Mycobacterium Dr Gh Hamzehloo Important Human Pathogens Mycobacterium
Mycobacterium Dr. Gh. Hamzehloo
Important Human Pathogens Mycobacterium tuberculosis Mycobacterium leprae (uncommon) Mycobacterium avium-intracellulaire Complex (MAC) or (M. avium)
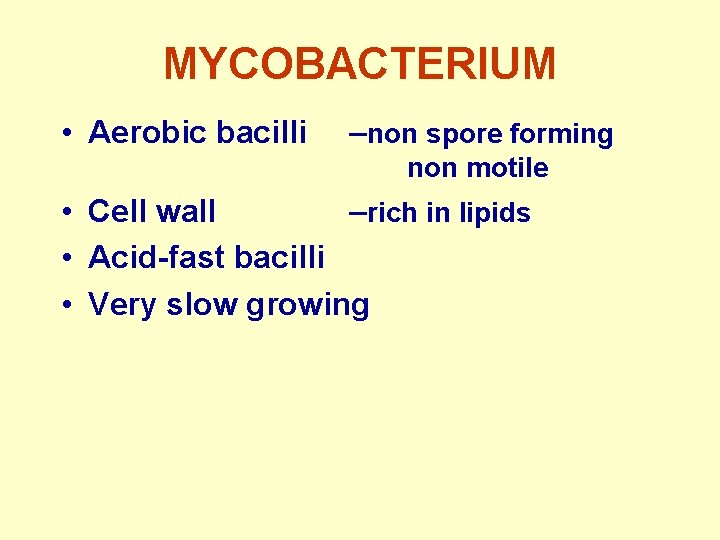
MYCOBACTERIUM • Aerobic bacilli –non spore forming non motile • Cell wall –rich in lipids • Acid-fast bacilli • Very slow growing
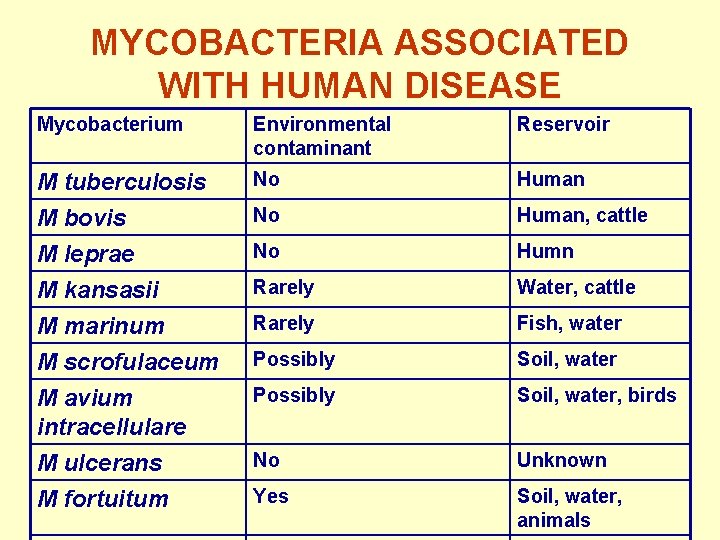
MYCOBACTERIA ASSOCIATED WITH HUMAN DISEASE Mycobacterium Environmental contaminant Reservoir M tuberculosis M bovis No Human, cattle M leprae M kansasii M marinum M scrofulaceum M avium intracellulare No Humn Rarely Water, cattle Rarely Fish, water Possibly Soil, water, birds M ulcerans M fortuitum No Unknown Yes Soil, water, animals
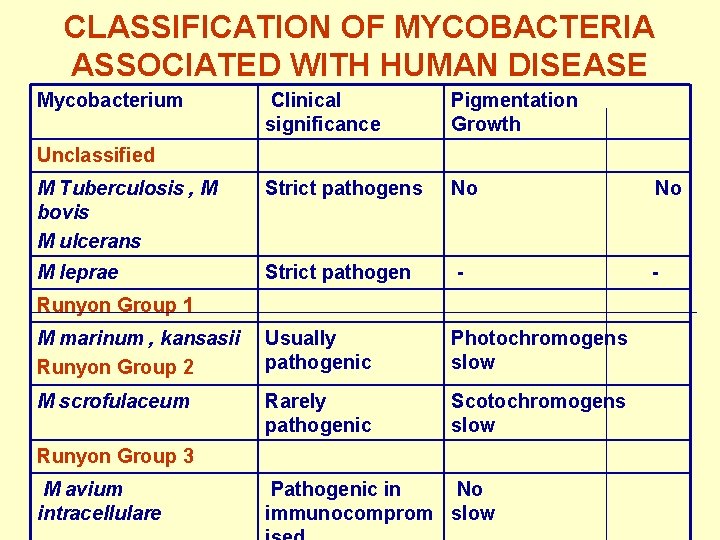
CLASSIFICATION OF MYCOBACTERIA ASSOCIATED WITH HUMAN DISEASE Mycobacterium Clinical significance Pigmentation Growth M Tuberculosis , M bovis M ulcerans Strict pathogens No No M leprae Strict pathogen - - M marinum , kansasii Runyon Group 2 Usually pathogenic Photochromogens slow M scrofulaceum Rarely pathogenic Scotochromogens slow Unclassified Runyon Group 1 Runyon Group 3 M avium intracellulare Pathogenic in No immunocomprom slow
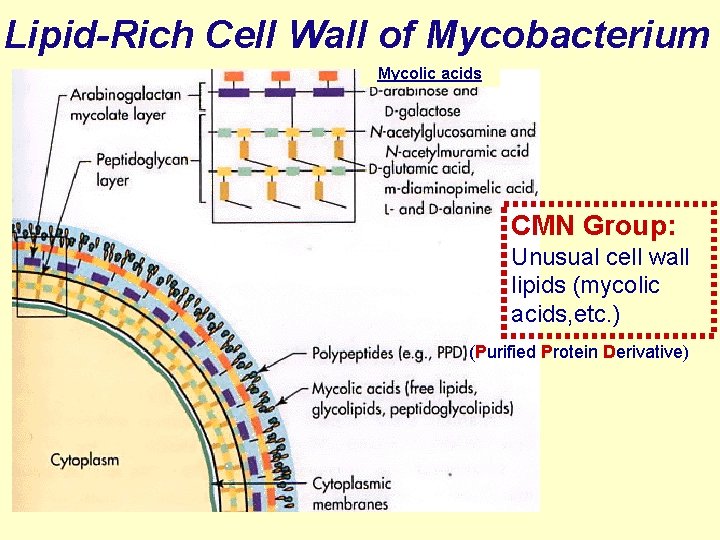
Lipid-Rich Cell Wall of Mycobacterium Mycolic acids CMN Group: Unusual cell wall lipids (mycolic acids, etc. ) (Purified Protein Derivative)
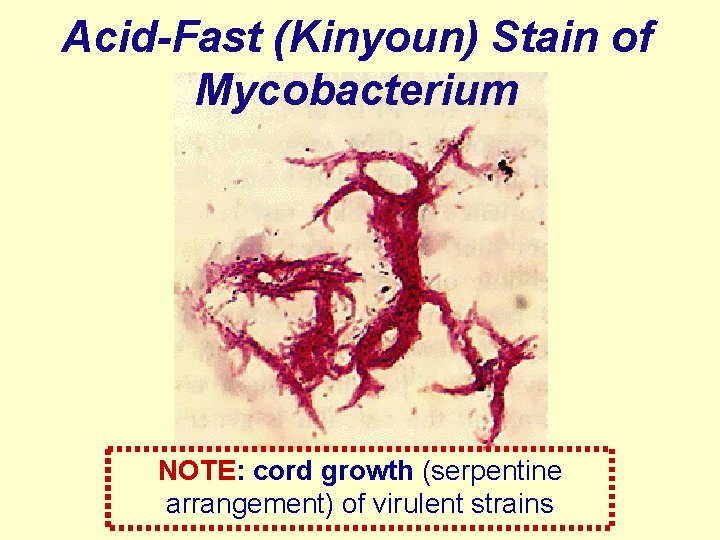
Acid-Fast (Kinyoun) Stain of Mycobacterium NOTE: cord growth (serpentine arrangement) of virulent strains
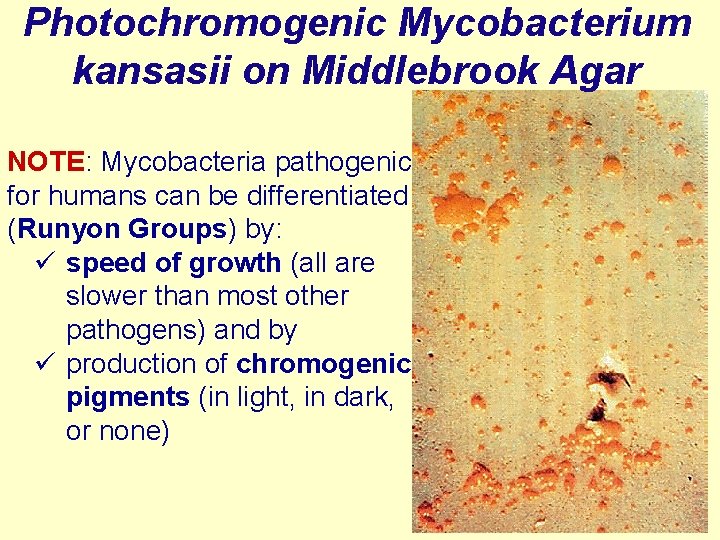
Photochromogenic Mycobacterium kansasii on Middlebrook Agar NOTE: Mycobacteria pathogenic for humans can be differentiated (Runyon Groups) by: ü speed of growth (all are slower than most other pathogens) and by ü production of chromogenic pigments (in light, in dark, or none)
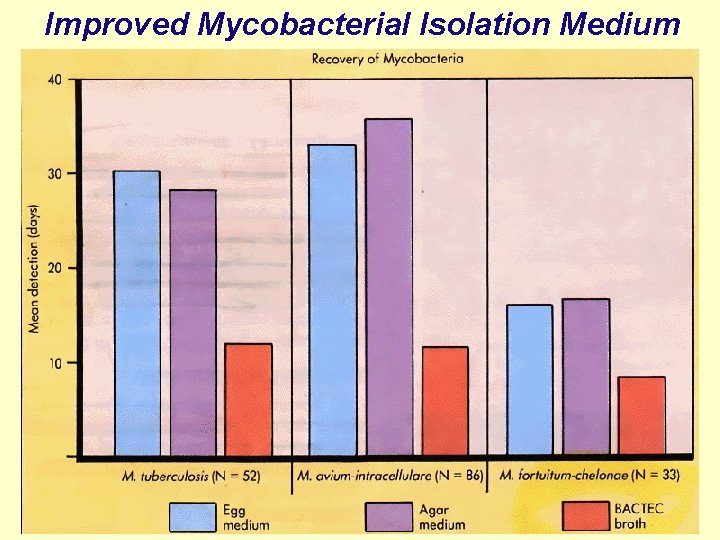
Improved Mycobacterial Isolation Medium
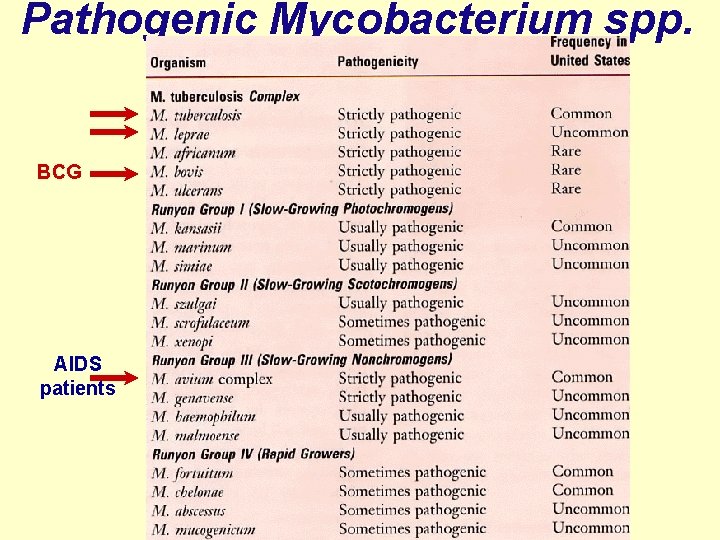
Pathogenic Mycobacterium spp. BCG AIDS patients
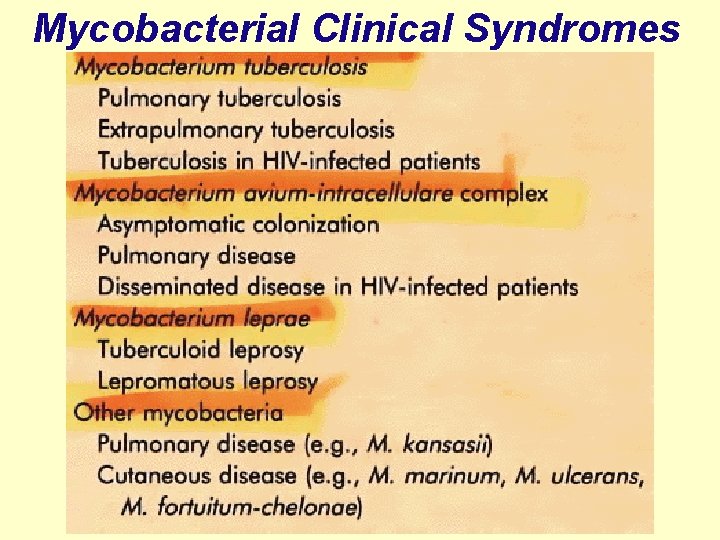
Mycobacterial Clinical Syndromes
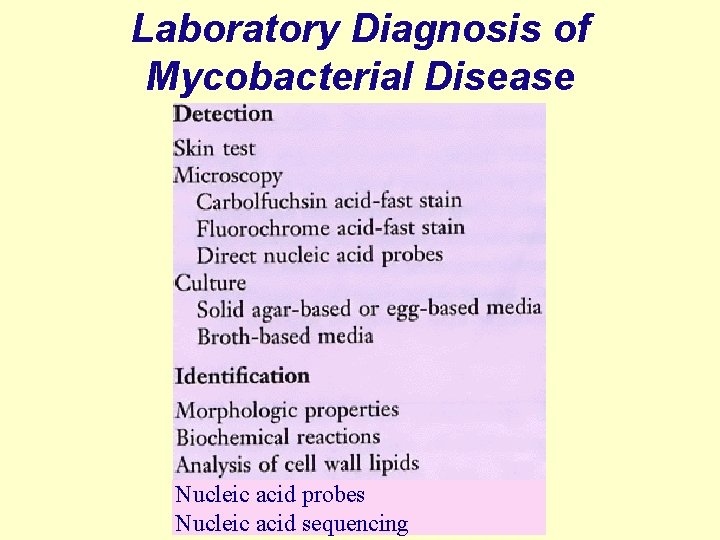
Laboratory Diagnosis of Mycobacterial Disease Nucleic acid probes Nucleic acid sequencing
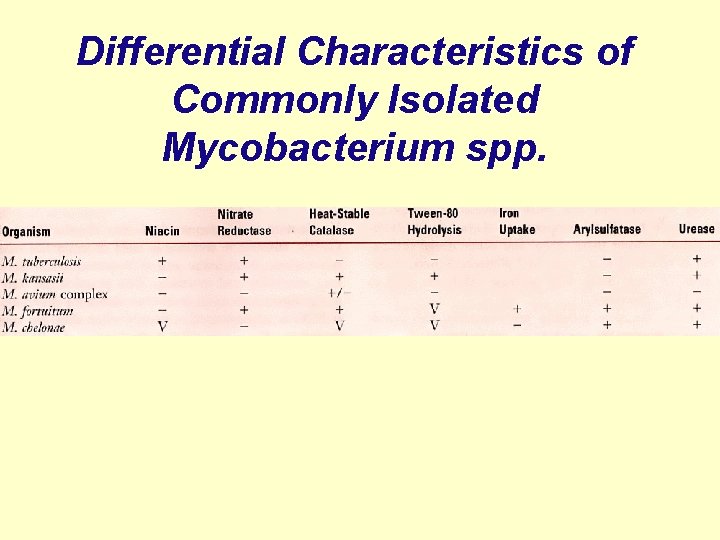
Differential Characteristics of Commonly Isolated Mycobacterium spp.
Mycobacterium tuberculosis
Mycobacterium tuberculosis • • Causes tuberculosis Classic human disease Pathogenesis Transmission Clinical presentations Diagnosis Treatment Prevention
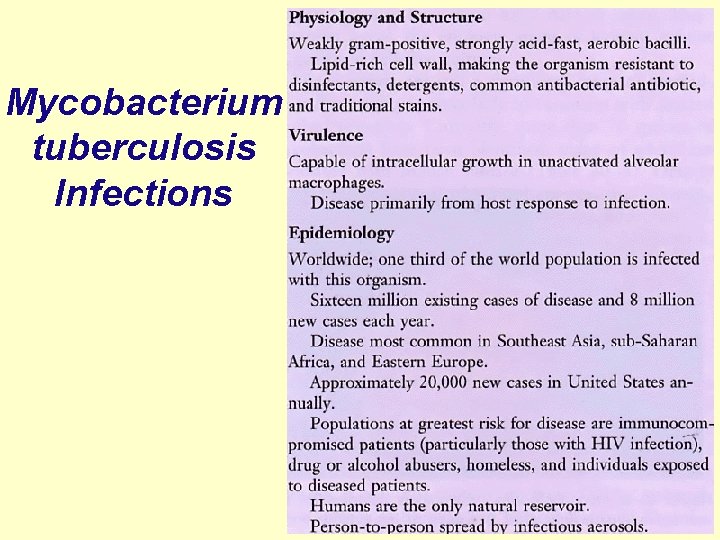
Mycobacterium tuberculosis Infections
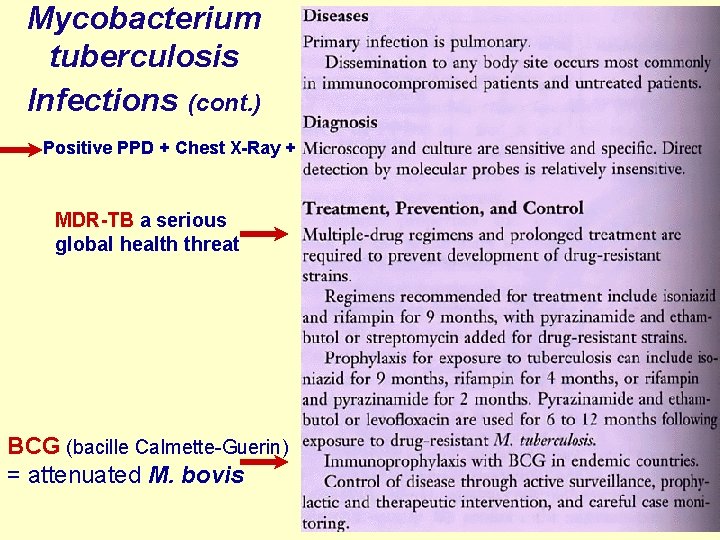
Mycobacterium tuberculosis Infections (cont. ) Positive PPD + Chest X-Ray + MDR-TB a serious global health threat BCG (bacille Calmette-Guerin) = attenuated M. bovis
Typical Progression of Pulmonary Tuberculosis Ø Pneumonia Ø Granuloma formation with fibrosis Ø Caseous necrosis • Tissue becomes dry & amorphous (resembling cheese) • Mixture of protein & fat (assimilated very slowly) Ø Calcification • Ca++ salts deposited Ø Cavity formation • Center liquefies & empties into bronchi
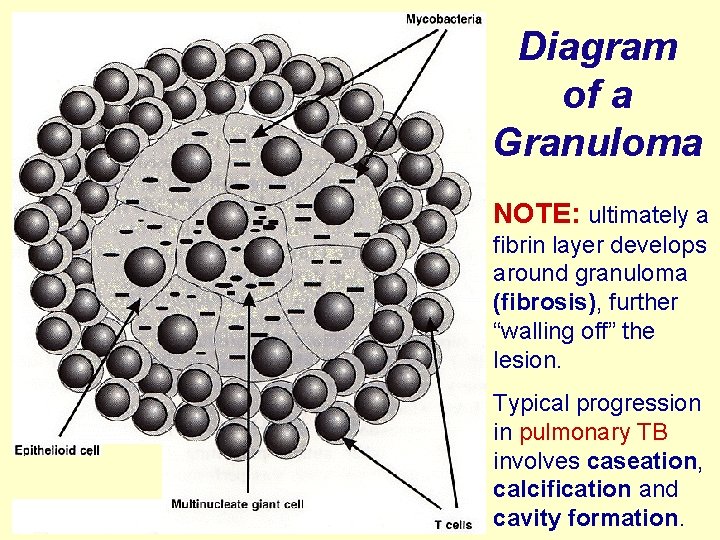
Diagram of a Granuloma NOTE: ultimately a fibrin layer develops around granuloma (fibrosis), further “walling off” the lesion. Typical progression in pulmonary TB involves caseation, calcification and cavity formation.
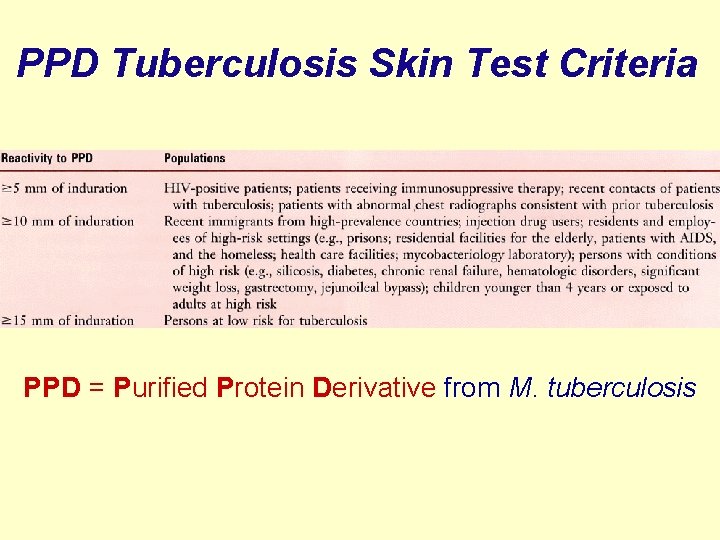
PPD Tuberculosis Skin Test Criteria PPD = Purified Protein Derivative from M. tuberculosis
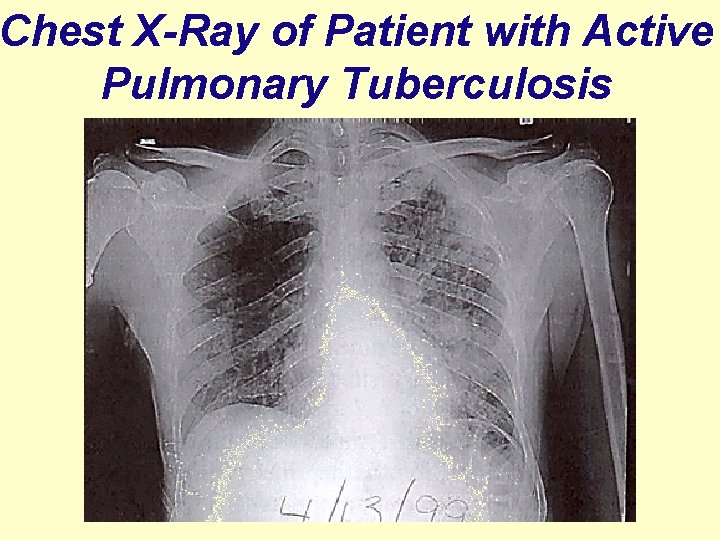
Chest X-Ray of Patient with Active Pulmonary Tuberculosis
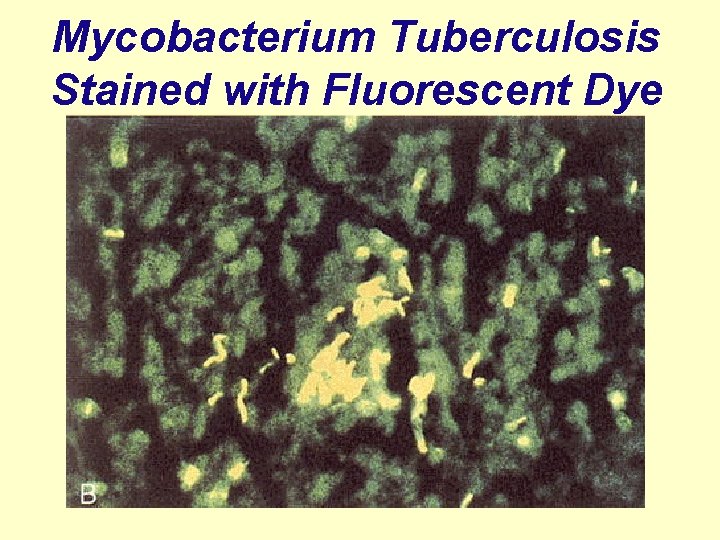
Mycobacterium Tuberculosis Stained with Fluorescent Dye
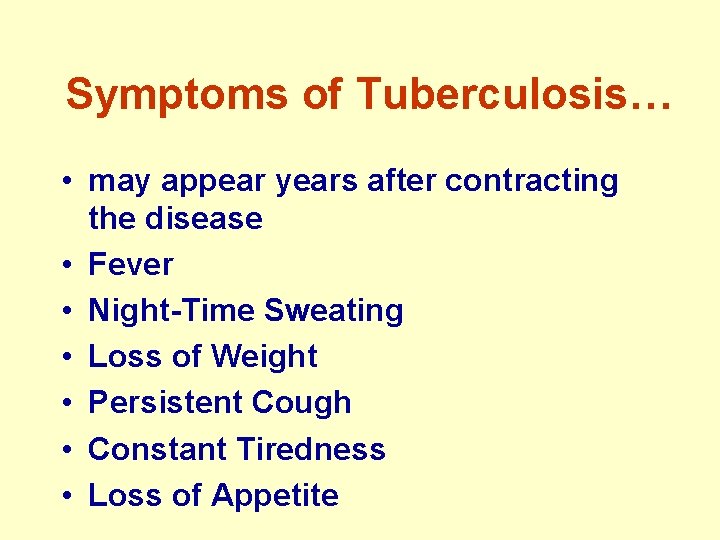
Symptoms of Tuberculosis… • may appear years after contracting the disease • Fever • Night-Time Sweating • Loss of Weight • Persistent Cough • Constant Tiredness • Loss of Appetite
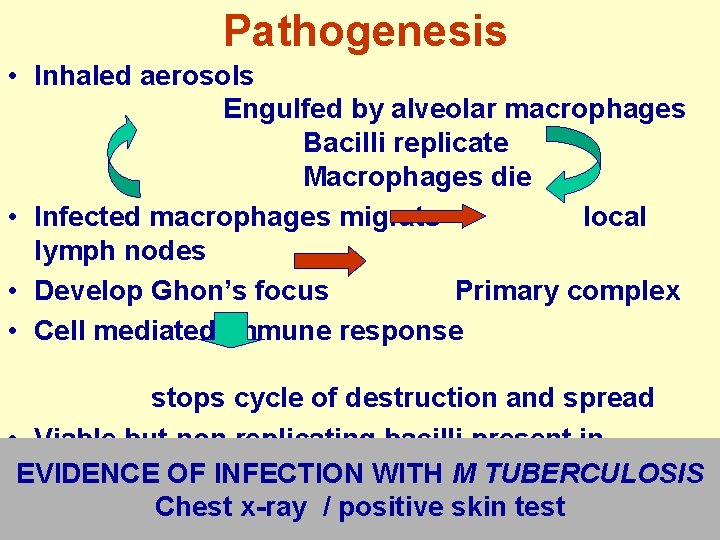
Pathogenesis • Inhaled aerosols Engulfed by alveolar macrophages Bacilli replicate Macrophages die • Infected macrophages migrate local lymph nodes • Develop Ghon’s focus Primary complex • Cell mediated immune response stops cycle of destruction and spread • Viable but non replicating bacilli present in macrophages EVIDENCE OF INFECTION WITH M TUBERCULOSIS Chest x-ray / positive skin test
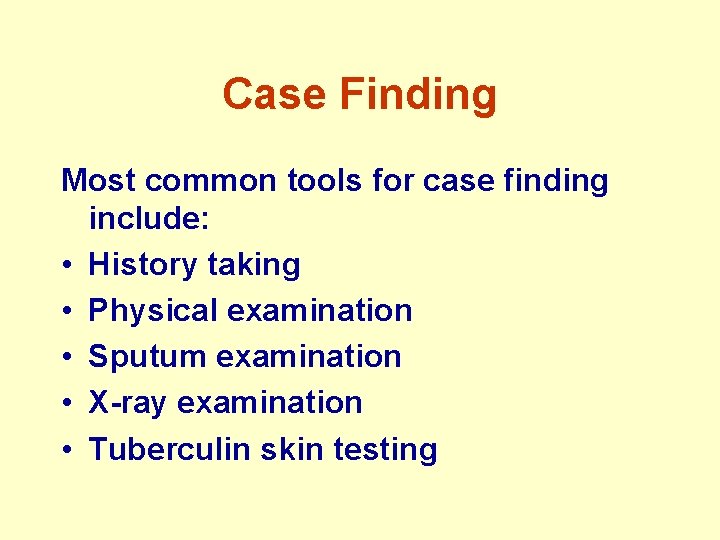
Case Finding Most common tools for case finding include: • History taking • Physical examination • Sputum examination • X-ray examination • Tuberculin skin testing
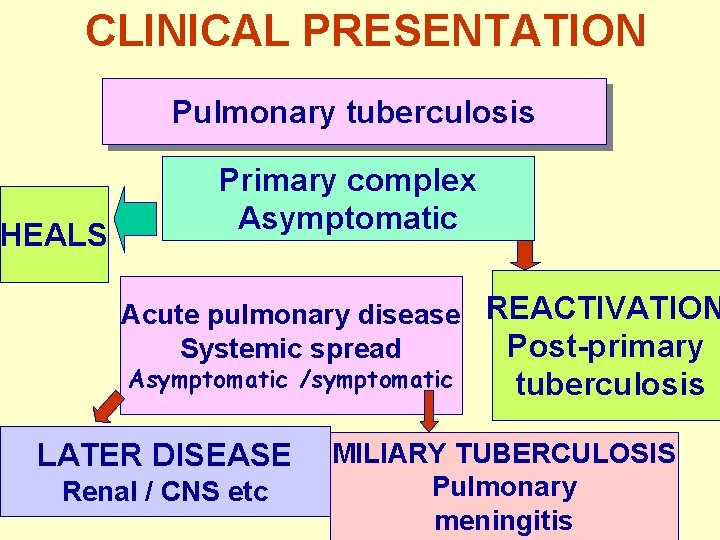
CLINICAL PRESENTATION Pulmonary tuberculosis HEALS Primary complex Asymptomatic Acute pulmonary disease REACTIVATION Post-primary Systemic spread Asymptomatic /symptomatic LATER DISEASE Renal / CNS etc tuberculosis MILIARY TUBERCULOSIS Pulmonary meningitis
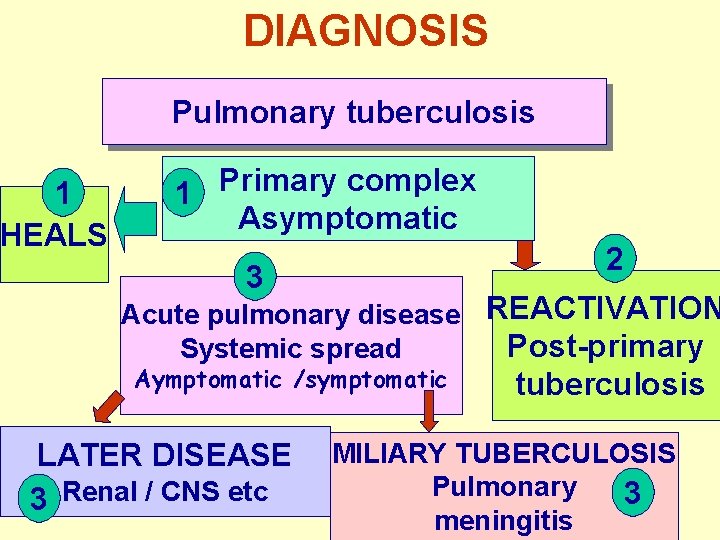
DIAGNOSIS Pulmonary tuberculosis 1 HEALS 1 Primary complex Asymptomatic 2 3 Acute pulmonary disease REACTIVATION Post-primary Systemic spread Aymptomatic /symptomatic LATER DISEASE 3 Renal / CNS etc tuberculosis MILIARY TUBERCULOSIS Pulmonary 3 meningitis
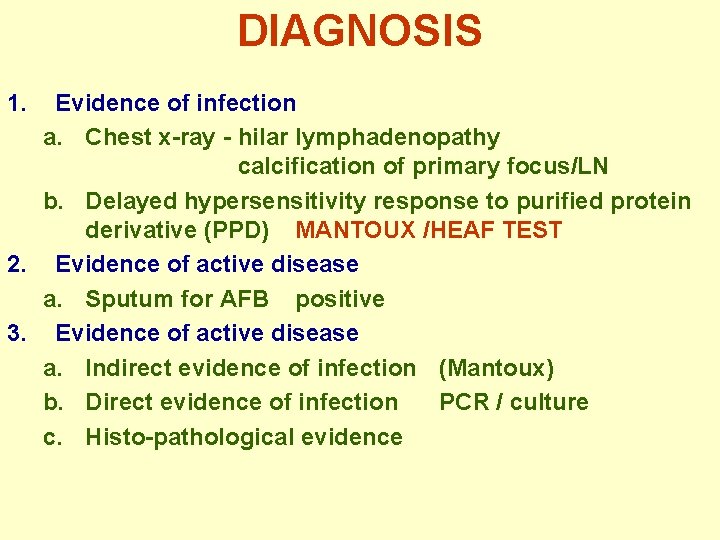
DIAGNOSIS 1. Evidence of infection a. Chest x-ray - hilar lymphadenopathy calcification of primary focus/LN b. Delayed hypersensitivity response to purified protein derivative (PPD) MANTOUX /HEAF TEST 2. Evidence of active disease a. Sputum for AFB positive 3. Evidence of active disease a. Indirect evidence of infection (Mantoux) b. Direct evidence of infection PCR / culture c. Histo-pathological evidence
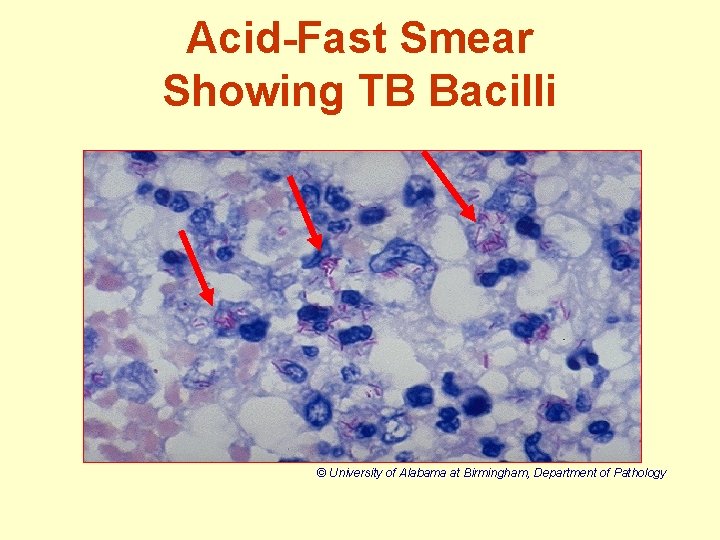
Acid-Fast Smear Showing TB Bacilli © University of Alabama at Birmingham, Department of Pathology
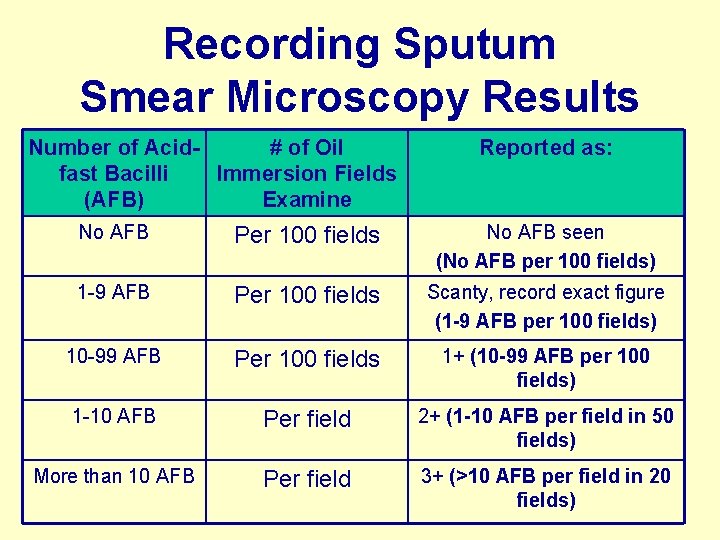
Recording Sputum Smear Microscopy Results Number of Acid# of Oil fast Bacilli Immersion Fields (AFB) Examine Reported as: No AFB Per 100 fields No AFB seen (No AFB per 100 fields) 1 -9 AFB Per 100 fields Scanty, record exact figure (1 -9 AFB per 100 fields) 10 -99 AFB Per 100 fields 1+ (10 -99 AFB per 100 fields) 1 -10 AFB Per field 2+ (1 -10 AFB per field in 50 fields) More than 10 AFB Per field 3+ (>10 AFB per field in 20 fields)
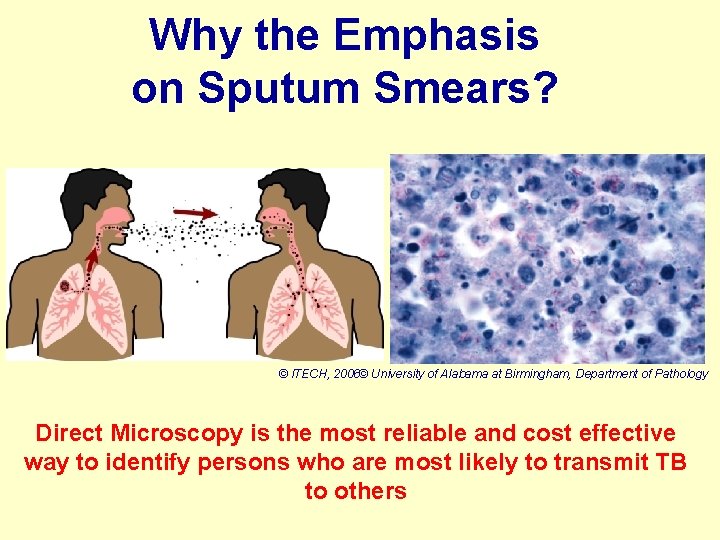
Why the Emphasis on Sputum Smears? © ITECH, 2006© University of Alabama at Birmingham, Department of Pathology Direct Microscopy is the most reliable and cost effective way to identify persons who are most likely to transmit TB to others
Primary and District Lab Services in TB control (Level 1) • • Receipt of specimens: from clinics Preparation and staining of smears ZN microscopy /recording Reporting of results Maintenance of lab register Management of reagents and supplies Internal Quality Control (QC) Collect specimen for culture and DST, send to NTRL • Participation in EQA
Nyangagbwe Referral lab (Level 2) • Activities: receive specimen for AFB and culture • Services to clinics: FM/ZN smear microscopy (smear microscopy and send results) • Support activities: (supply of reagents/ materials, training; EQA for smear microscopy including supervision) • Inoculate specimen and refer to NTRL for incubation and DST
Role of NTRL in TB Control • Identify mycobacterium other than MTB • DST of M. Tuberculosis • TB laboratory equipment services and maintenance • Develop TB Lab manuals and guidelines • Primary link with NTP • Supervision of intermediate QA of culture and microscopy • Operational and applied research • Provide EQA and monitor peripheral labs
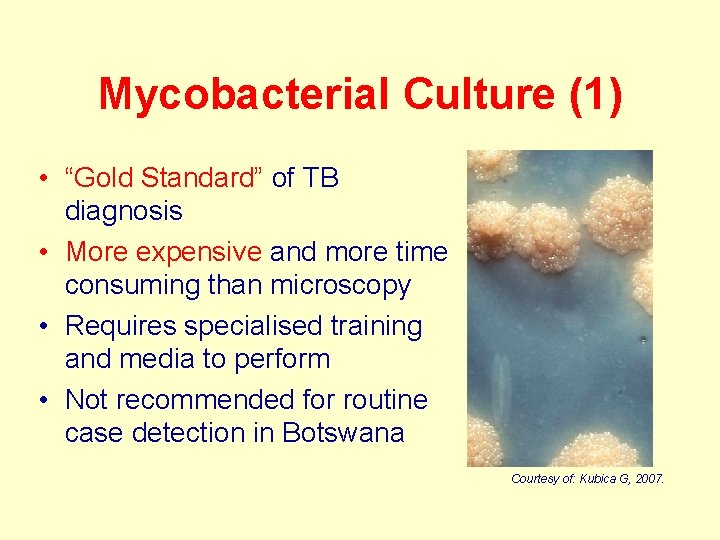
Mycobacterial Culture (1) • “Gold Standard” of TB diagnosis • More expensive and more time consuming than microscopy • Requires specialised training and media to perform • Not recommended for routine case detection in Botswana Courtesy of: Kubica G, 2007.
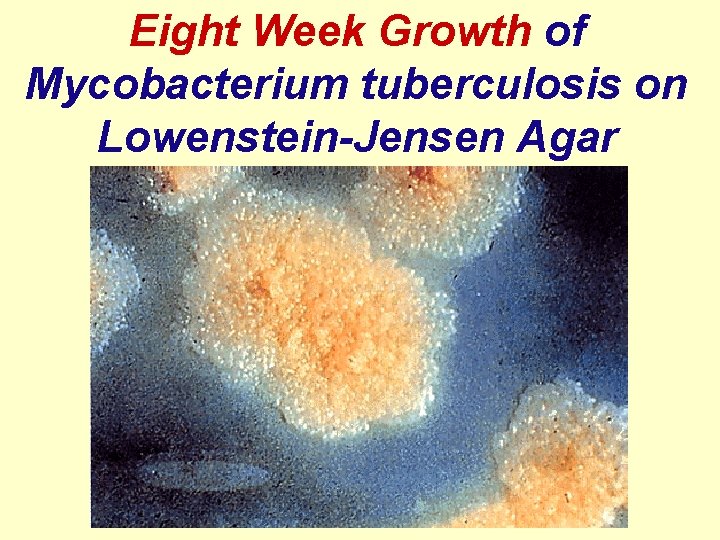
Eight Week Growth of Mycobacterium tuberculosis on Lowenstein-Jensen Agar
Mycobacterial Culture (2) Reasons to request mycobacterial culture: • Patient previously on anti-TB treatment • Still smear-positive after intensive phase of treatment or after finishing treatment • Symptomatic and at high-risk of MDR-TB • To test fluids potentially infected with M. tuberculosis • Investigation of patients who develop active PTB during or after IPT • TB in health workers
TB Drug Susceptibility Testing (DST) • DST performed on all cultures – Tests for isoniazid, rifampicin, ethambutol, and streptomycin • If found to be multi-drug resistant, then send for additional testing for susceptibility to second-line medicines
TREATMENT • Anti-tuberculous drugs – INAH – Rifampicin – Ethambutol – Pyrazinamide • DOT • Multi-drug resistant tuberculosis
PREVENTION • Incidence declined before availability of antituberculous drugs • Improved social conditions - housing /nutrition • Case detection & treatment • Contact tracing • Evidence of infection / disease • Treatment of infected / diseased contacts ROLE OF IMMUNIZATION BCG (bacillus Calmette Guerin)

PLAN – DO – CHECK – ACT CYCLE Process Management 6/6/2021 ACT PLAN CHECK DO 44
- Slides: 44