Myasthenia Gravis Guo Yijing the Department of Neurology
- Slides: 55
Myasthenia Gravis Guo Yijing the Department of Neurology, Affiliated Zhong. Da Hospital of Southeast University Reference: Allan H. Ropper et al. ADAMS AND VICTOR'S PRINCIPLES OF NEUROLOGY - 8 th Ed. (2005)
Disorders of the Neuromuscular Junction n Disorders of the NMJ ¨ Myasthenia Gravis (MG) ¨ Lambert-Eaton Syndrome (LEMS) ¨ Myasthenic syndromes induced by drugs and toxins n Organophosphate poisoning n Botulism poisoning n …… ¨ Neonatal myasthenia ¨ The congenital myasthenic syndromes 2
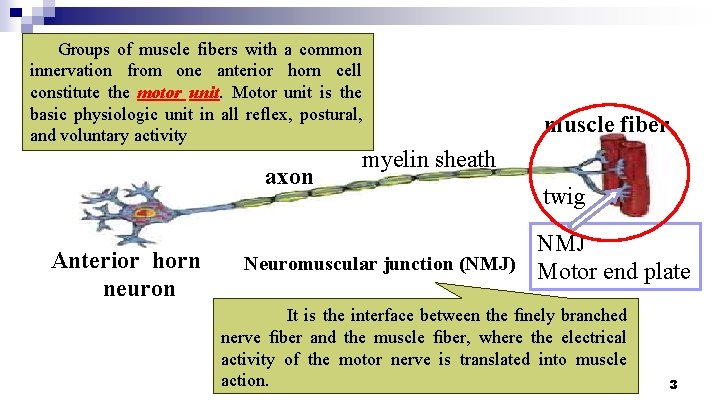
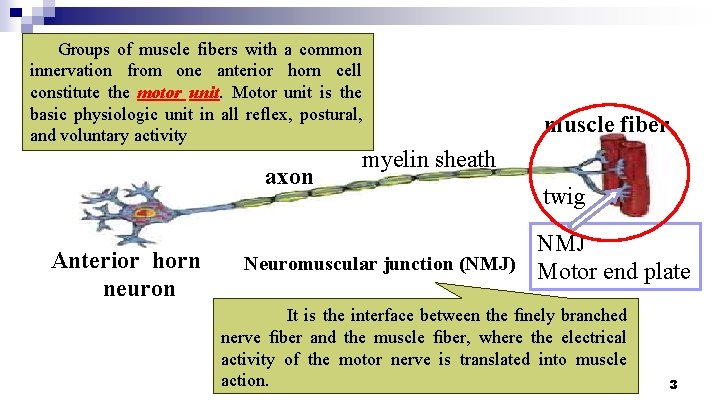
Groups of muscle fibers with a common innervation from one anterior horn cell constitute the motor unit. Motor unit is the basic physiologic unit in all reflex, postural, and voluntary activity axon Anterior horn neuron muscle fiber myelin sheath twig NMJ Neuromuscular junction (NMJ) Motor end plate It is the interface between the finely branched nerve fiber and the muscle fiber, where the electrical activity of the motor nerve is translated into muscle action. 3
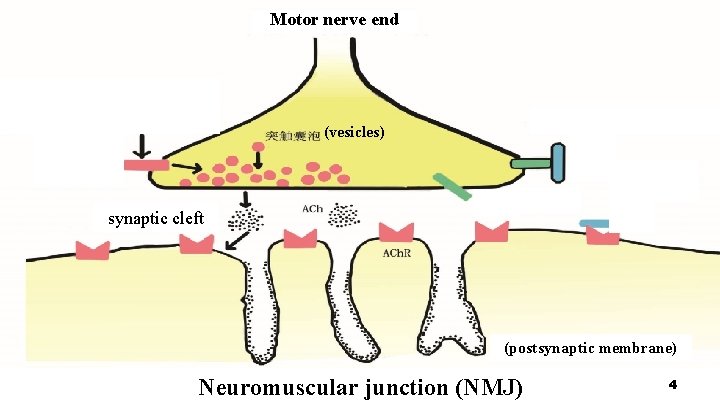
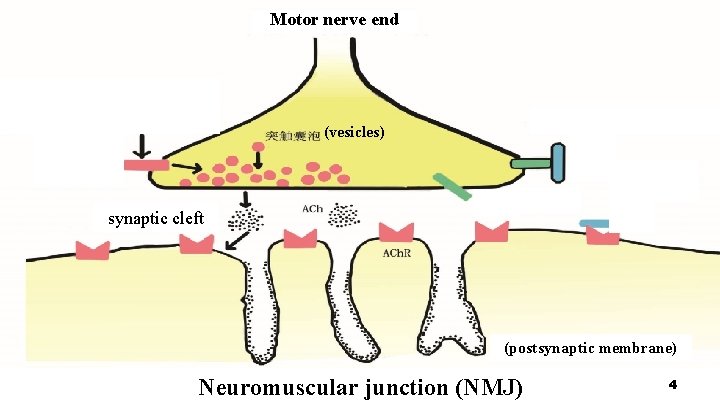
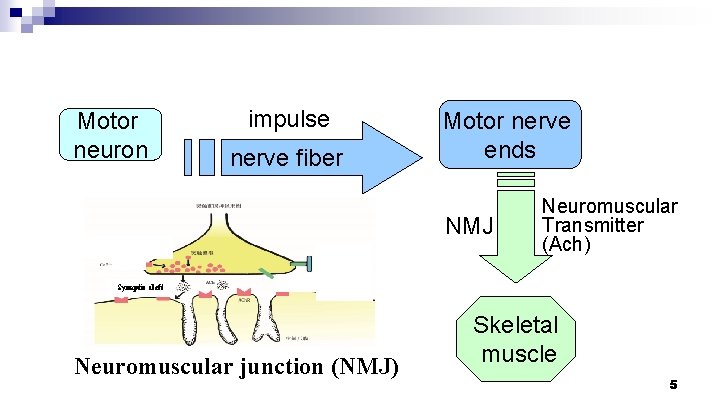
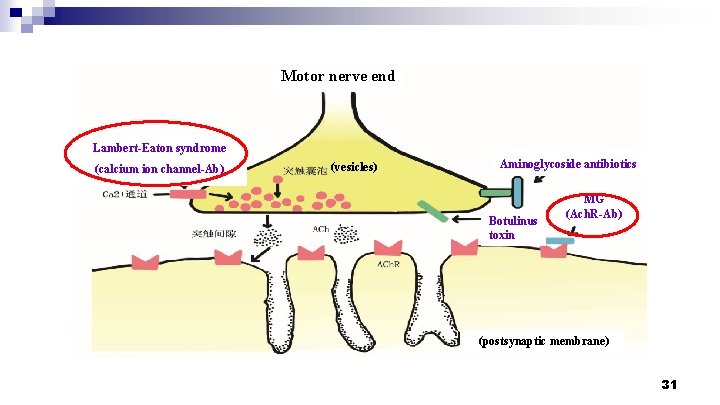
Motor nerve end (vesicles) synapticcleft synaptic (postsynaptic membrane) Neuromuscular junction (NMJ) 4
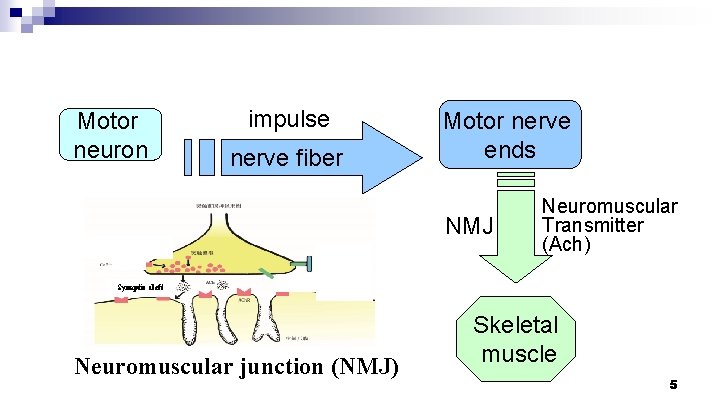
Motor neuron impulse nerve fiber Motor nerve ends NMJ Neuromuscular Transmitter (Ach) Synaptic cleft Neuromuscular junction (NMJ) Skeletal muscle 5
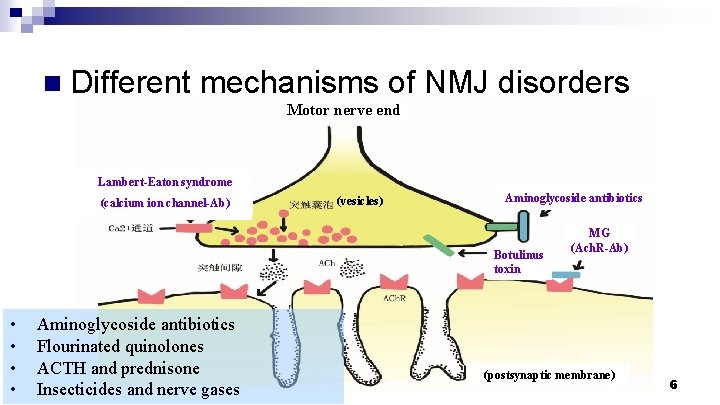
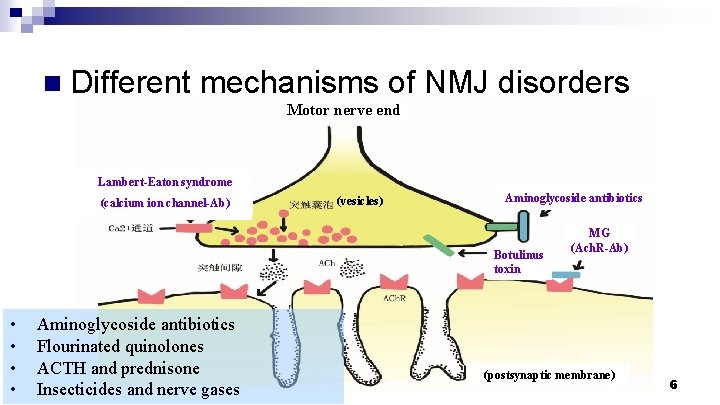
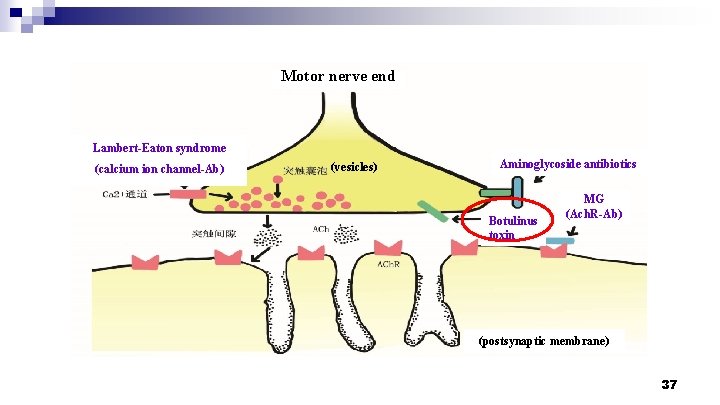
n Different mechanisms of NMJ disorders Motor nerve end Lambert-Eaton syndrome (calcium ion channel-Ab) (vesicles) Aminoglycoside antibiotics Botulinus toxin • • Aminoglycoside antibiotics Flourinated quinolones ACTH and prednisone Insecticides and nerve gases MG (Ach. R-Ab) (postsynaptic membrane) 6
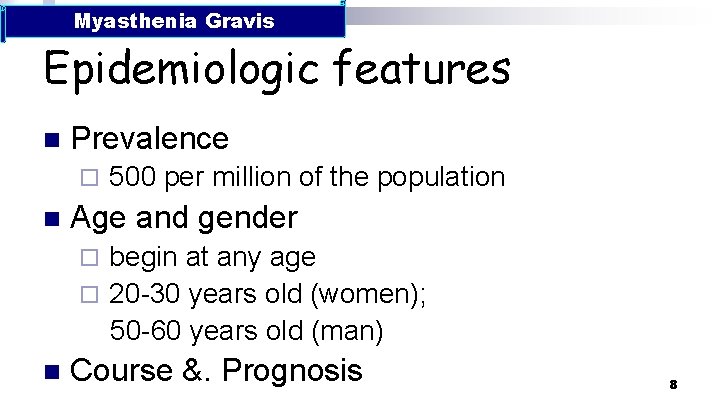
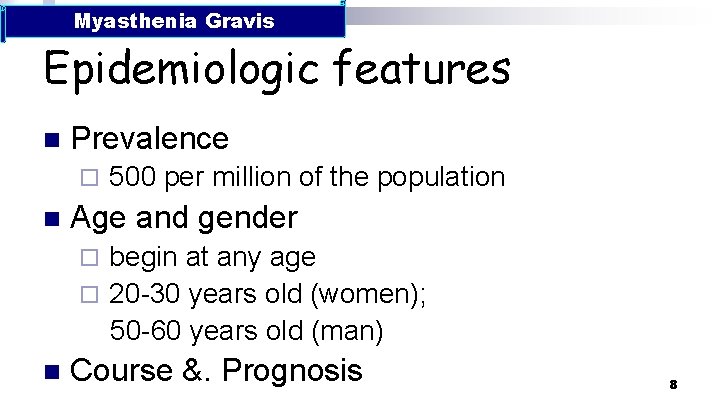
Myasthenia Gravis Epidemiologic features n Prevalence ¨ n 500 per million of the population Age and gender begin at any age ¨ 20 -30 years old (women); 50 -60 years old (man) ¨ n Course &. Prognosis 8
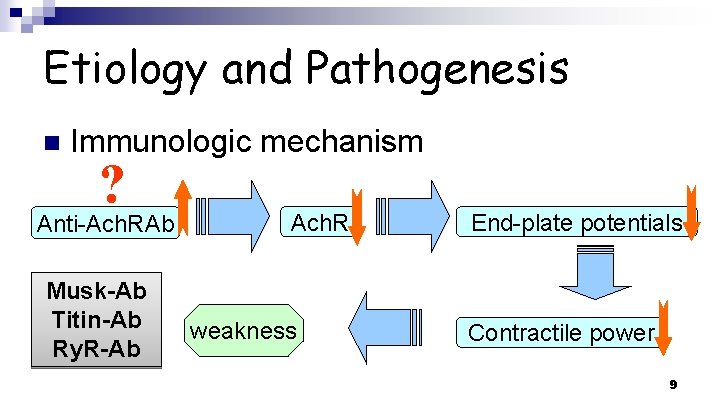
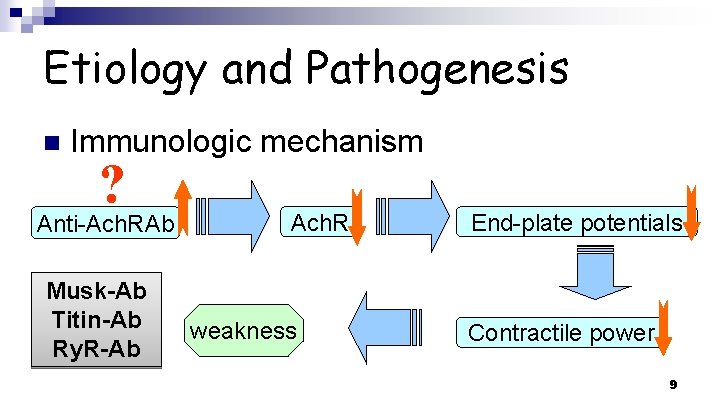
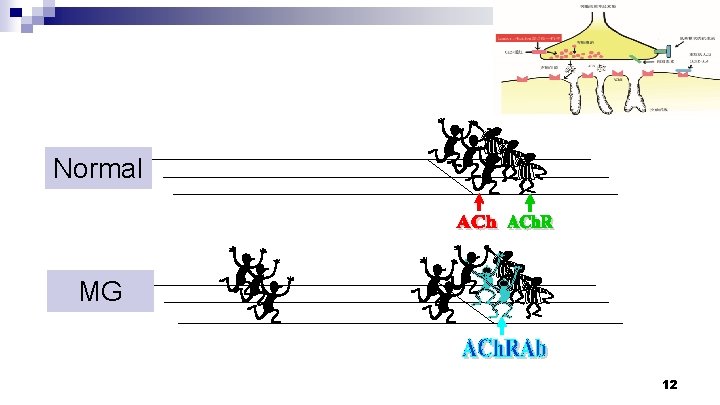
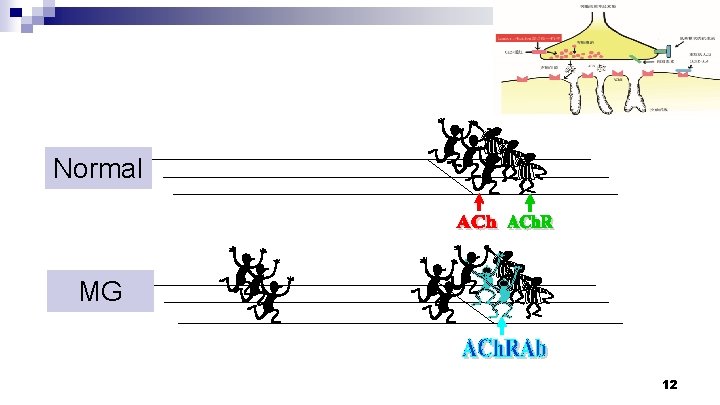
Etiology and Pathogenesis n Immunologic mechanism ? Anti-Ach. RAb Musk-Ab Titin-Ab Ry. R-Ab Ach. R weakness End-plate potentials Contractile power 9
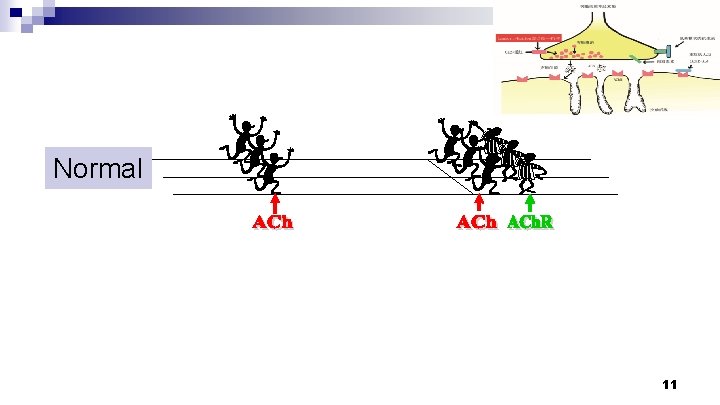
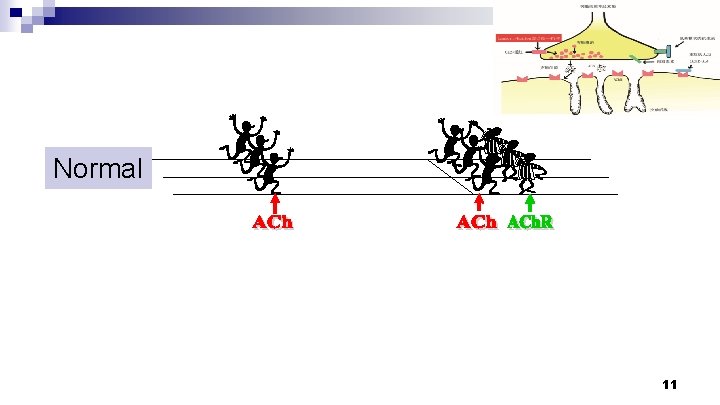
Normal 11
Normal MG 12
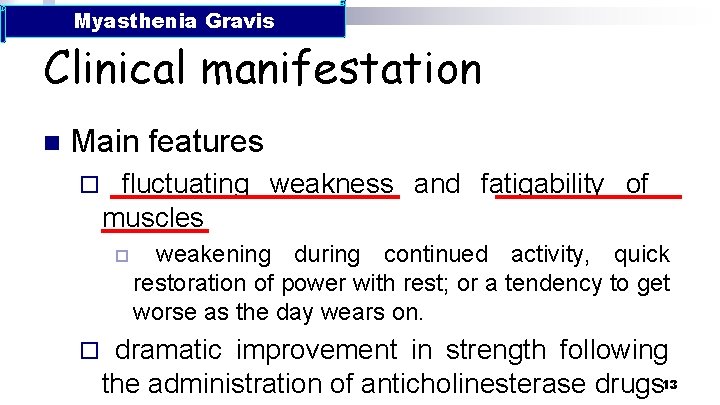
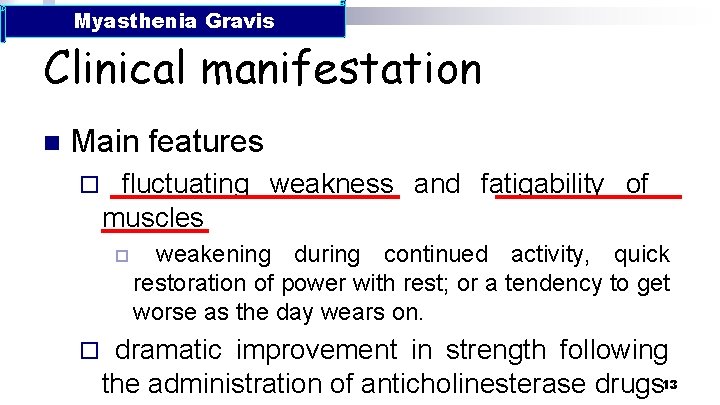
Myasthenia Gravis Clinical manifestation n Main features ¨ fluctuating weakness and fatigability of muscles p ¨ weakening during continued activity, quick restoration of power with rest; or a tendency to get worse as the day wears on. dramatic improvement in strength following the administration of anticholinesterase drugs 13
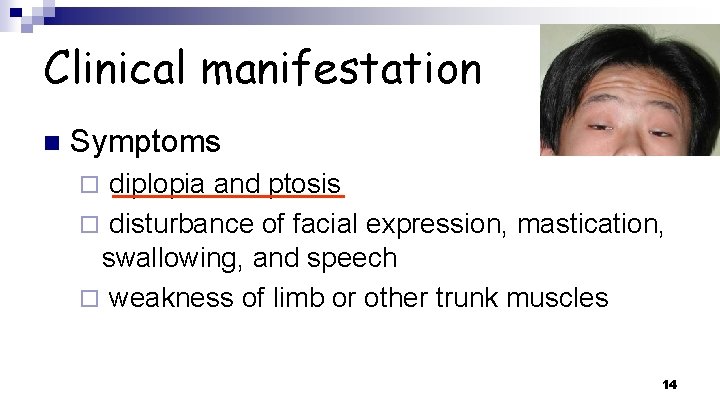
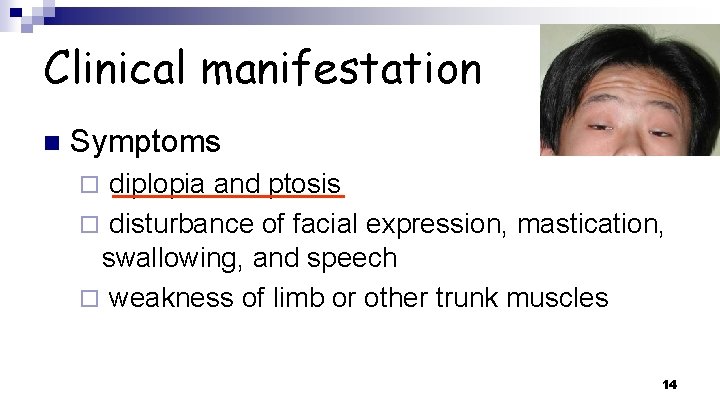
Clinical manifestation n Symptoms diplopia and ptosis ¨ disturbance of facial expression, mastication, swallowing, and speech ¨ weakness of limb or other trunk muscles ¨ 14
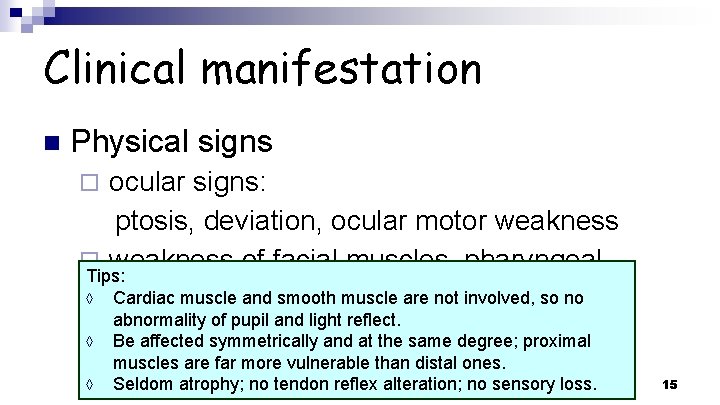
Clinical manifestation n Physical signs ocular signs: ptosis, deviation, ocular motor weakness ¨ weakness of facial muscles, pharyngeal Tips: and muscles ◊ muscles Cardiac muscle andlaryngeal smooth muscle are not involved, so no abnormality of pupil and light reflect. ¨ of limband axial ◊ weakness Be affected symmetrically at the samemuscles degree; proximal ¨ ◊ muscles are far more vulnerable than distal ones. Seldom atrophy; no tendon reflex alteration; no sensory loss. 15
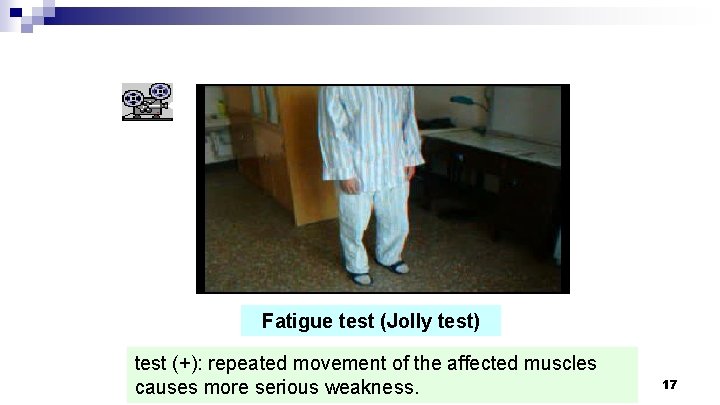
Clinical manifestation n Physical signs ocular signs: ptosis, deviation, ocular motor weakness ¨ weakness of facial muscles, pharyngeal muscle and laryngeal muscle ¨ weakness of limb and axial muscles ¨ Fatigue test 16
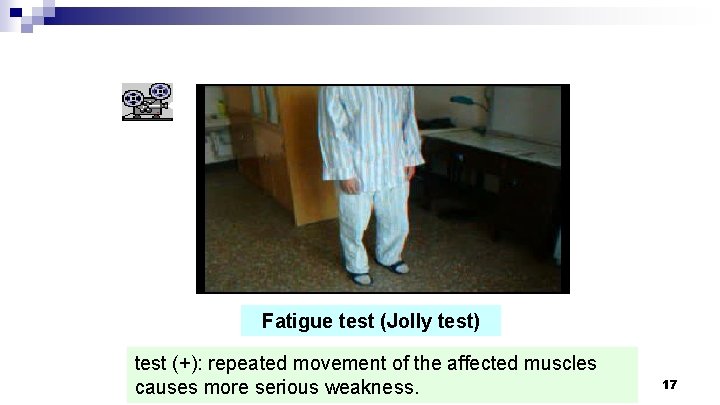
Fatigue test (Jolly test) test (+): repeated movement of the affected muscles causes more serious weakness. 17
Precipitating factors n n n an emotional upset infection (usually respiratory) overtiredness pregnancy or in the puerperium operation and/or anesthesia 18
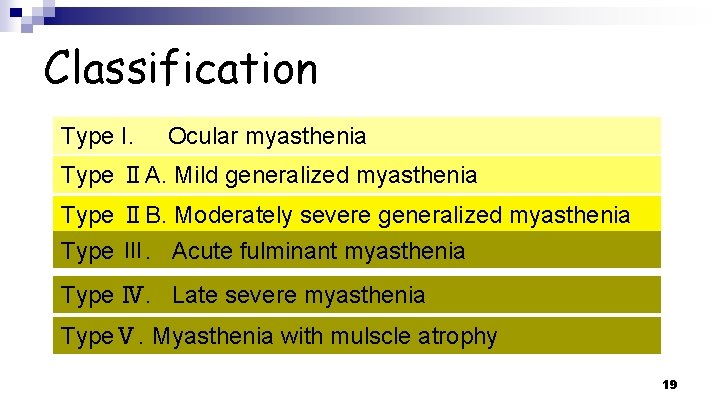
Classification Type I. Ocular myasthenia Type ⅡA. Mild generalized myasthenia Type ⅡB. Moderately severe generalized myasthenia Type Ⅲ. Acute fulminant myasthenia Type Ⅳ. Late severe myasthenia TypeⅤ. Myasthenia with mulscle atrophy 19
Auxiliary examinations Electrophysiologic testing n Tensilon or Neostigmine tests n Measurement of Ab in blood n CT scan of the chest n 20
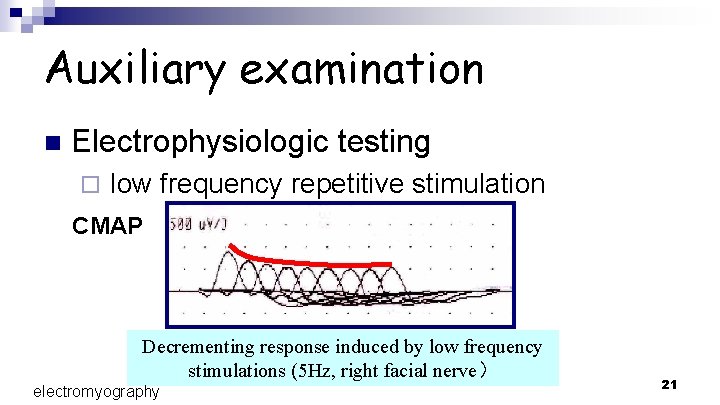
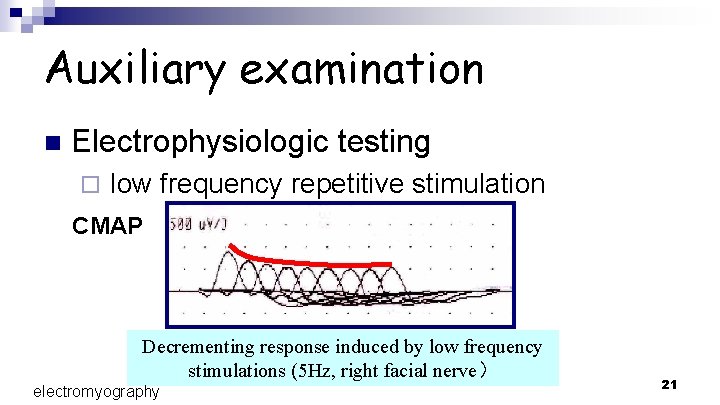
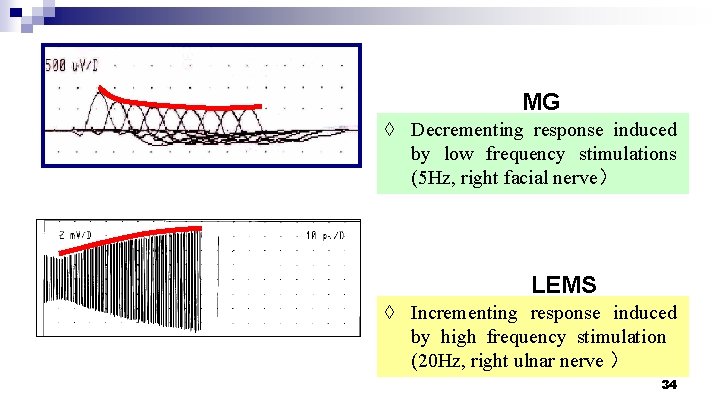
Auxiliary examination n Electrophysiologic testing ¨ low frequency repetitive stimulation CMAP Decrementing response induced by low frequency stimulations (5 Hz, right facial nerve) electromyography 21
Auxiliary examination n Electrophysiologic testing low frequency repeated stimulation ¨ single fiber electromyography ¨ ◊ This technique demonstrates an inconstancy of the normally invariant interval between the firing of fibers connected to the same motor unit ("jitter") or a blocking of successive discharges from single muscle fibers belonging to the same motor unit. 22
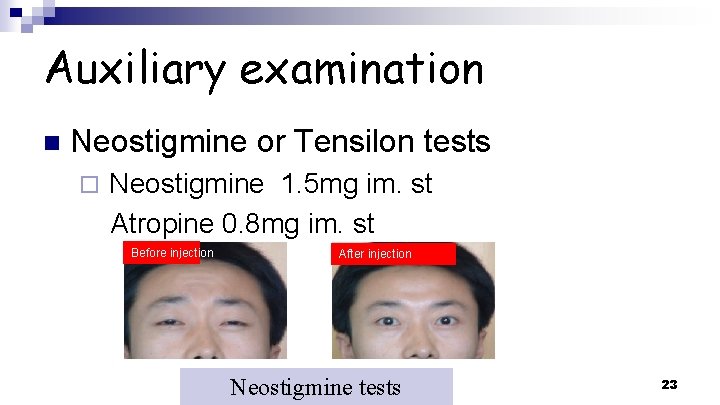
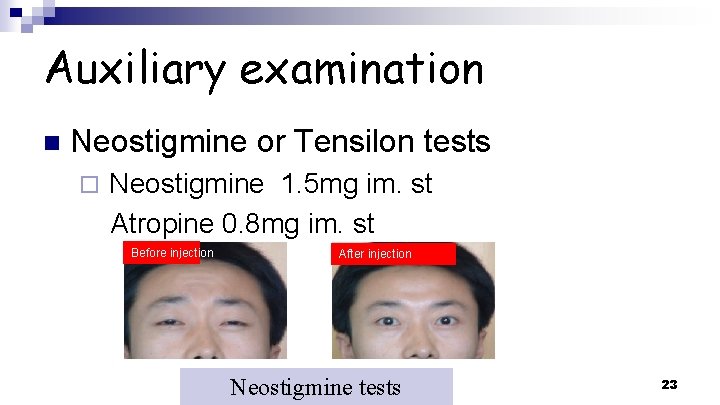
Auxiliary examination n Neostigmine or Tensilon tests ¨ Neostigmine 1. 5 mg im. st Atropine 0. 8 mg im. st Before injection After injection Neostigmine tests 23
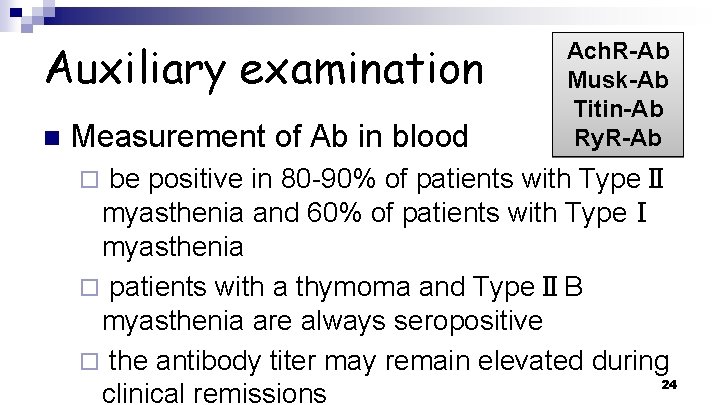
Auxiliary examination n Measurement of Ab in blood Ach. R-Ab Musk-Ab Titin-Ab Ry. R-Ab be positive in 80 -90% of patients with TypeⅡ myasthenia and 60% of patients with TypeⅠ myasthenia ¨ patients with a thymoma and TypeⅡB myasthenia are always seropositive ¨ the antibody titer may remain elevated during 24 clinical remissions ¨
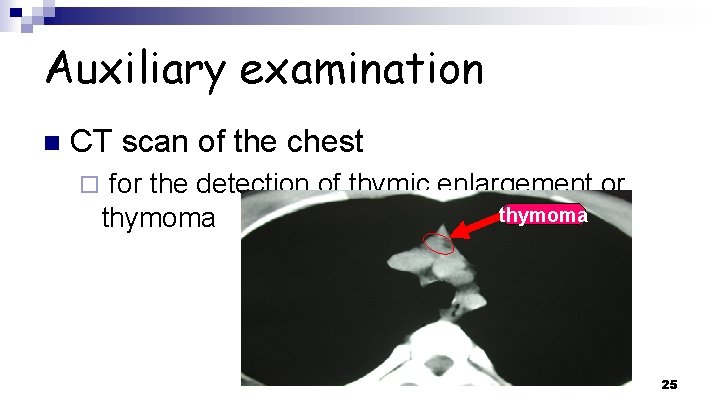
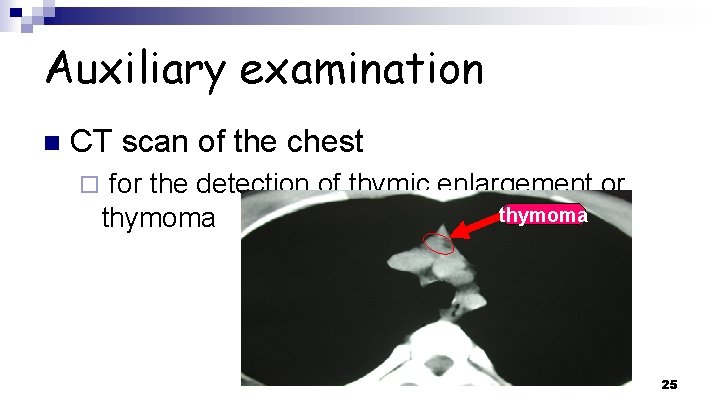
Auxiliary examination n CT scan of the chest ¨ for the detection of thymic enlargement or thymoma 25
Diagnosis n n n A fluctuating weakness, only involves skeletal muscles Remission if have a rest or treated by anticholinesterase drugs Positive results in Fatigue test, Neostigmine test, low frequency repeated stimulation and serum ACh. R antibody and other antibodies test. 26
Differential diagnosis n n n n Ophthalmoplegia Thyrotoxicosis and hypothyroidism Lambert-Eaton syndrome Botulism Polymyositis Midbrain stroke GBS 27
Differential diagnosis Ophthalmoplegia n Thyrotoxicosis and hypothyroidism n 28
Differential diagnosis Lambert-Eaton myasthenia syndrome n Botulism n Polymyositis n Midbrain stroke n GBS n 29
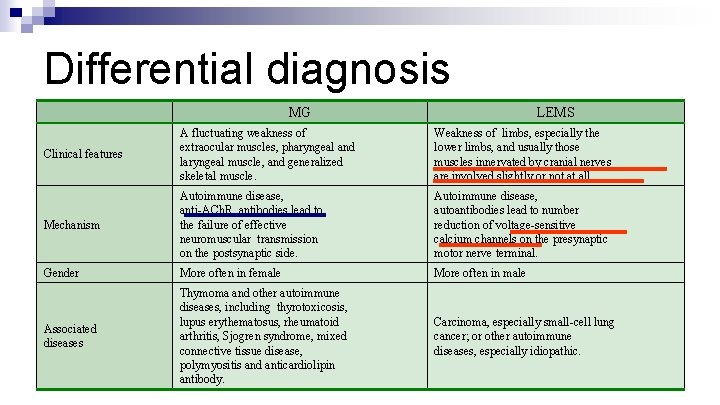
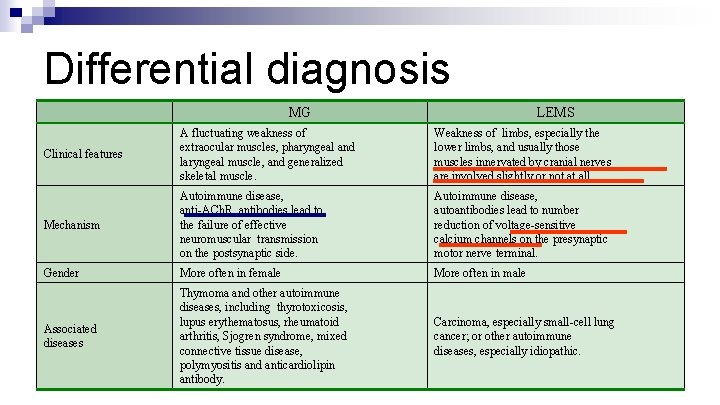
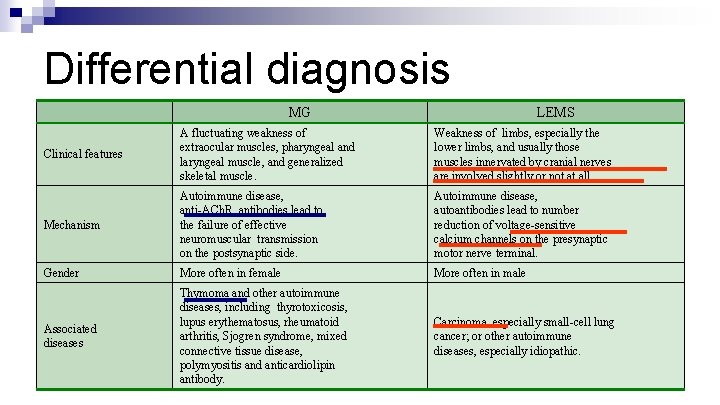
Differential diagnosis MG LEMS Clinical features A fluctuating weakness of extraocular muscles, pharyngeal and laryngeal muscle, and generalized skeletal muscle. Weakness of limbs, especially the lower limbs, and usually those muscles innervated by cranial nerves are involved slightly or not at all. Mechanism Autoimmune disease, anti-ACh. R antibodies lead to the failure of effective neuromuscular transmission on the postsynaptic side. Autoimmune disease, autoantibodies lead to number reduction of voltage-sensitive calcium channels on the presynaptic motor nerve terminal. Gender More often in female More often in male Associated diseases Thymoma and other autoimmune diseases, including thyrotoxicosis, lupus erythematosus, rheumatoid arthritis, Sjogren syndrome, mixed connective tissue disease, polymyositis and anticardiolipin antibody. Carcinoma, especially small-cell lung cancer; or other autoimmune diseases, especially idiopathic. 30
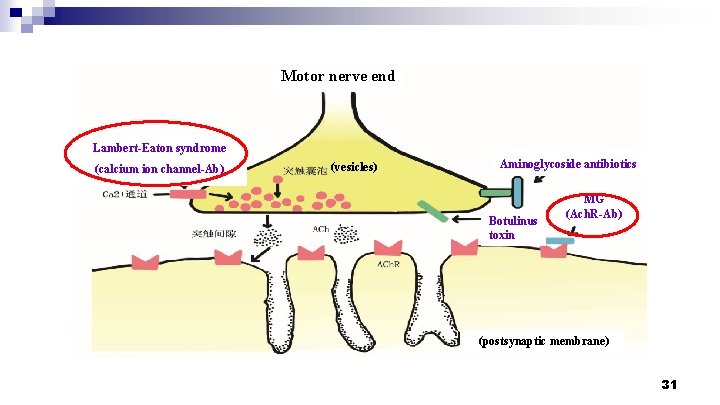
Motor nerve end Lambert-Eaton syndrome (calcium ion channel-Ab) (vesicles) Aminoglycoside antibiotics Botulinus toxin MG (Ach. R-Ab) (postsynaptic membrane) 31
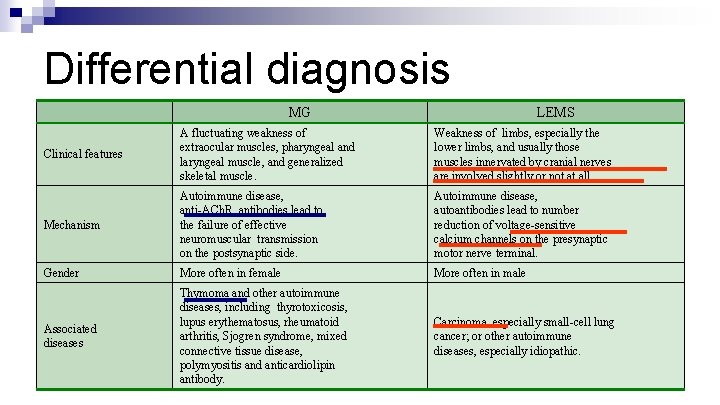
Differential diagnosis MG LEMS Clinical features A fluctuating weakness of extraocular muscles, pharyngeal and laryngeal muscle, and generalized skeletal muscle. Weakness of limbs, especially the lower limbs, and usually those muscles innervated by cranial nerves are involved slightly or not at all. Mechanism Autoimmune disease, anti-ACh. R antibodies lead to the failure of effective neuromuscular transmission on the postsynaptic side. Autoimmune disease, autoantibodies lead to number reduction of voltage-sensitive calcium channels on the presynaptic motor nerve terminal. Gender More often in female More often in male Associated diseases Thymoma and other autoimmune diseases, including thyrotoxicosis, lupus erythematosus, rheumatoid arthritis, Sjogren syndrome, mixed connective tissue disease, polymyositis and anticardiolipin antibody. Carcinoma, especially small-cell lung cancer; or other autoimmune diseases, especially idiopathic. 32
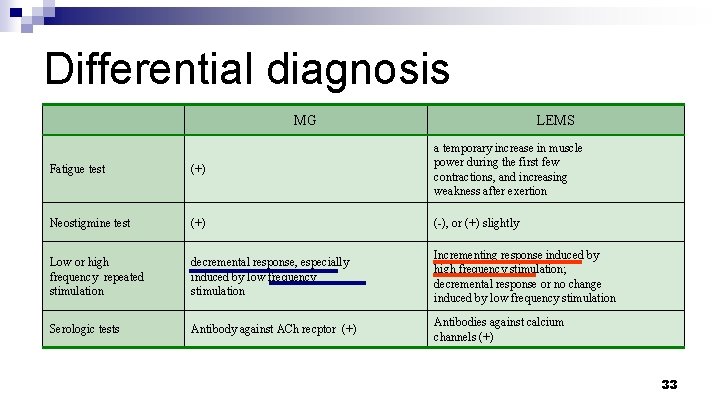
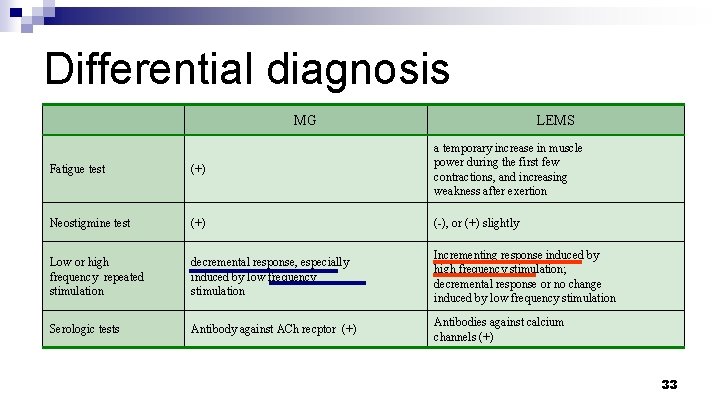
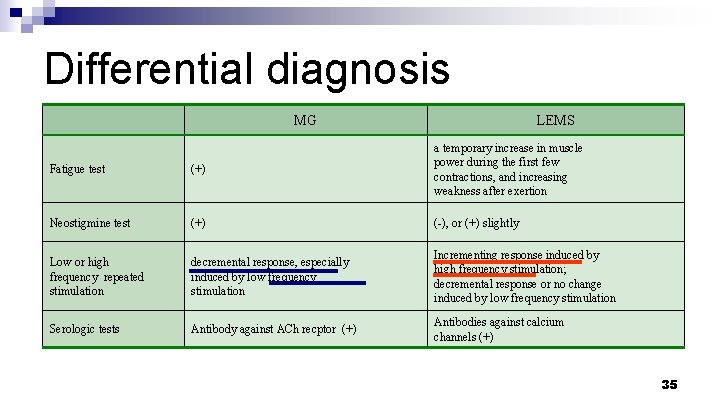
Differential diagnosis MG LEMS Fatigue test (+) a temporary increase in muscle power during the first few contractions, and increasing weakness after exertion Neostigmine test (+) (-), or (+) slightly Low or high frequency repeated stimulation decremental response, especially induced by low frequency stimulation Incrementing response induced by high frequency stimulation; decremental response or no change induced by low frequency stimulation Serologic tests Antibody against ACh recptor (+) Antibodies against calcium channels (+) 33
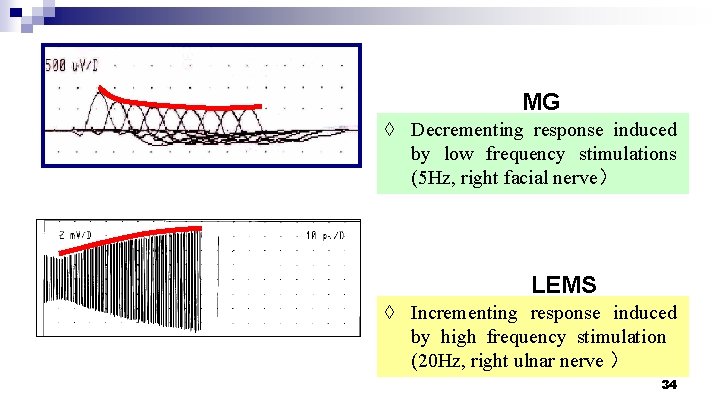
MG ◊ Decrementing response induced by low frequency stimulations (5 Hz, right facial nerve) LEMS ◊ Incrementing response induced by high frequency stimulation (20 Hz, right ulnar nerve ) 34
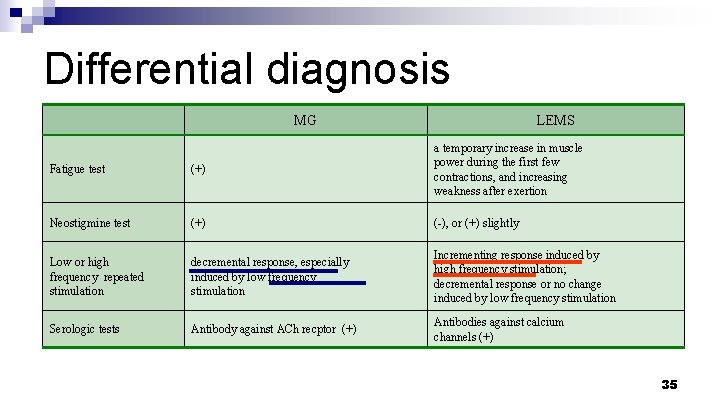
Differential diagnosis MG LEMS Fatigue test (+) a temporary increase in muscle power during the first few contractions, and increasing weakness after exertion Neostigmine test (+) (-), or (+) slightly Low or high frequency repeated stimulation decremental response, especially induced by low frequency stimulation Incrementing response induced by high frequency stimulation; decremental response or no change induced by low frequency stimulation Serologic tests Antibody against ACh recptor (+) Antibodies against calcium channels (+) 35
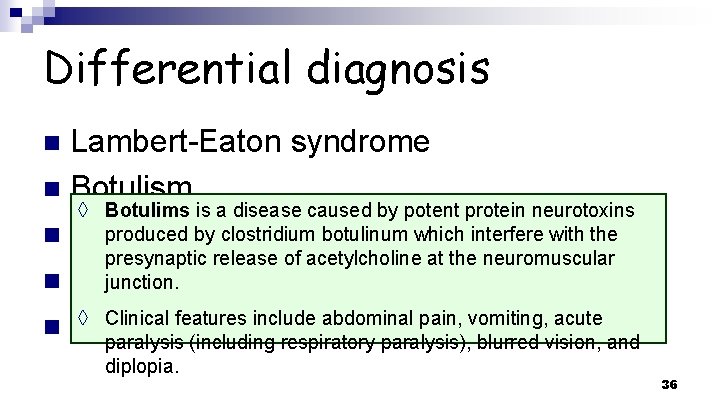
Differential diagnosis Lambert-Eaton syndrome n Botulism ◊ Botulims is a disease caused by potent protein neurotoxins produced by clostridium botulinum which interfere with the n Polymyositis presynaptic release of acetylcholine at the neuromuscular junction. stroke n Midbrain ◊ Clinical features include abdominal pain, vomiting, acute n GBS paralysis (including respiratory paralysis), blurred vision, and n diplopia. 36
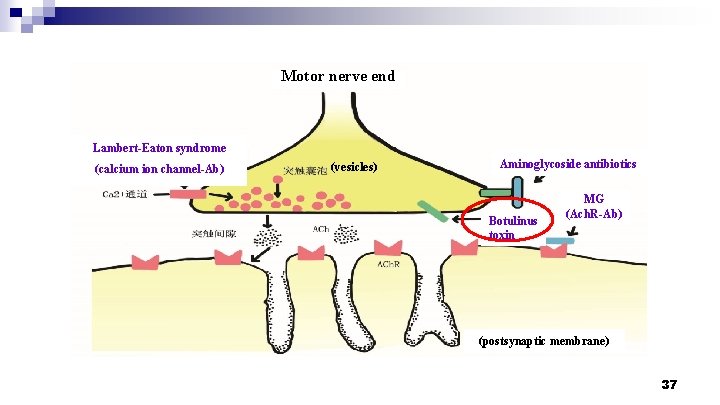
Motor nerve end Lambert-Eaton syndrome (calcium ion channel-Ab) (vesicles) Aminoglycoside antibiotics Botulinus toxin MG (Ach. R-Ab) (postsynaptic membrane) 37
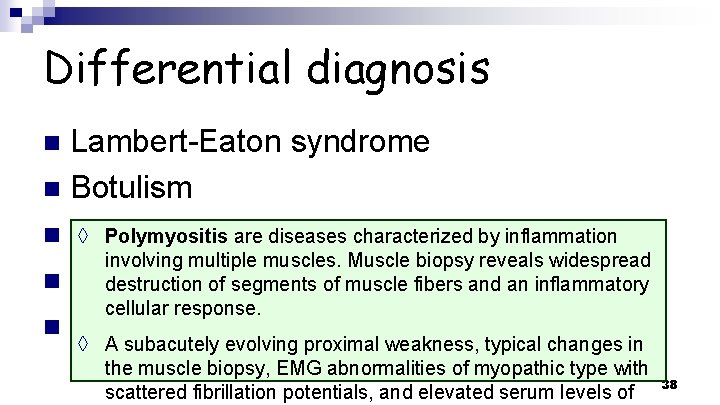
Differential diagnosis Lambert-Eaton syndrome n Botulism ◊ Polymyositis are diseases characterized by inflammation n Polymyositis involving multiple muscles. Muscle biopsy reveals widespread n Midbrain destructionstroke of segments of muscle fibers and an inflammatory cellular response. n GBS ◊ A subacutely evolving proximal weakness, typical changes in n the muscle biopsy, EMG abnormalities of myopathic type with scattered fibrillation potentials, and elevated serum levels of 38
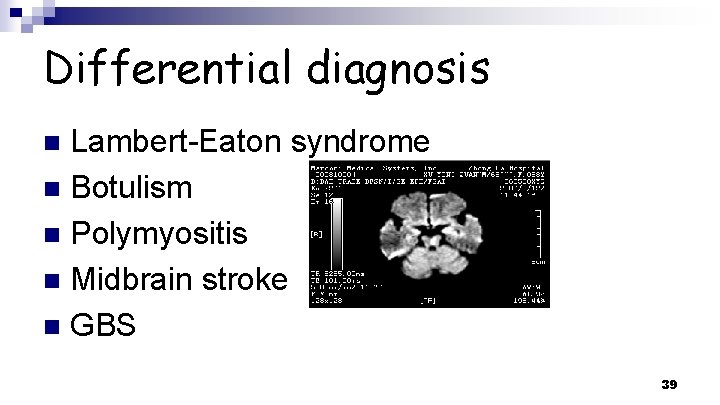
Differential diagnosis Lambert-Eaton syndrome n Botulism n Polymyositis n Midbrain stroke n GBS n 39
Differential diagnosis Lambert-Eaton syndrome n Botulism n Polymyositis ◊ GBS (Guillain-Barre syndrome), or Acute Inflammatory n Midbrain stroke Polyneuropathy (AIDP). The major clinical manifestation are symmetrical weakness and slight numbness in the toes and n GBS fingers. Reduced or absent tendon reflexes and sensory are n consistent findings. ◊ The most important laboratory aids are the electrodiagnostic 40
Therapy Anticholinesterase drugs n Corticosteroids n Immunosuppressive drugs n Plasma exchange n Intravenous immune globulin n Thymectomy n 41
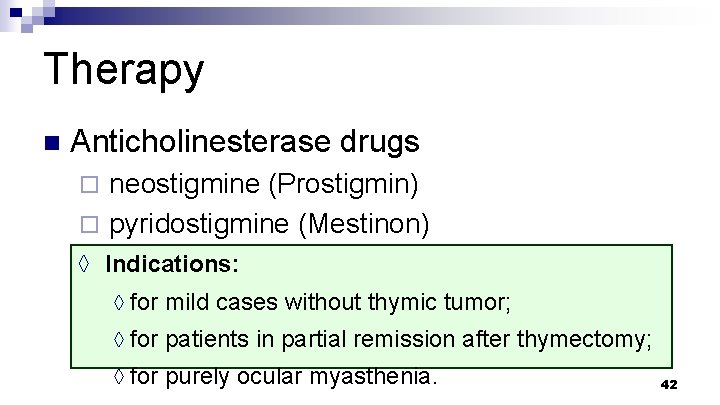
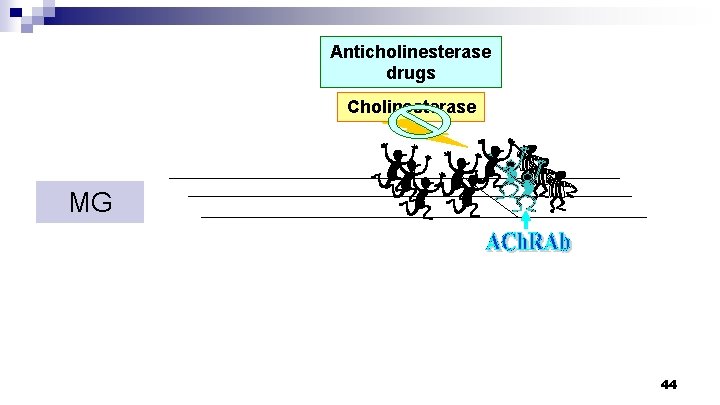
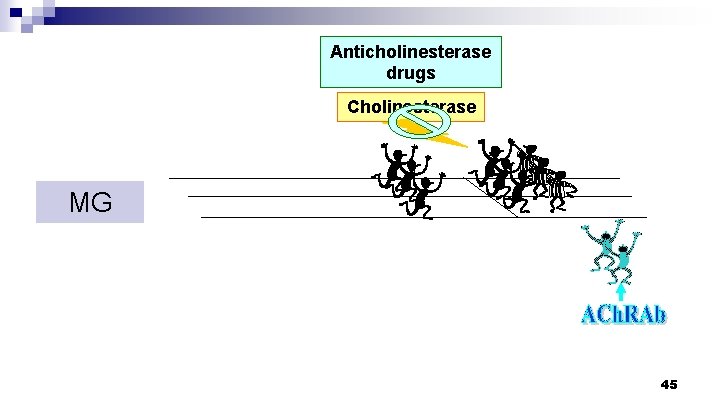
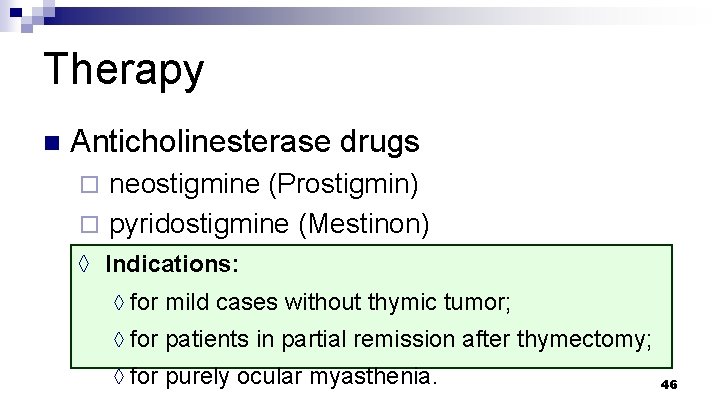
Therapy n Anticholinesterase drugs neostigmine (Prostigmin) ¨ pyridostigmine (Mestinon) ¨ n 30 -90 mg po. q 6 h ◊ Indications: ◊ for mild cases without thymic tumor; ◊ for patients in partial remission after thymectomy; ◊ for purely ocular myasthenia. 42
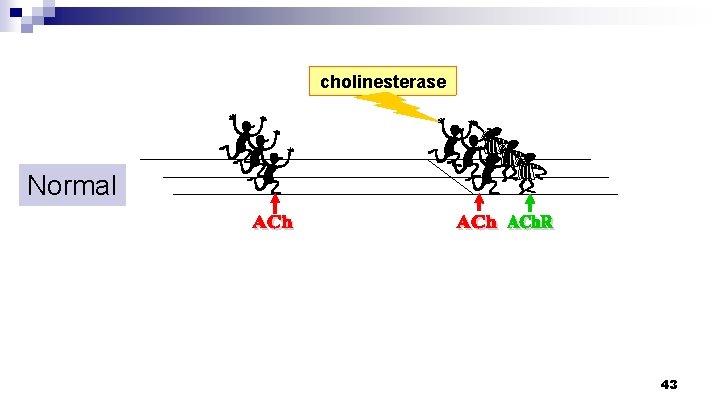
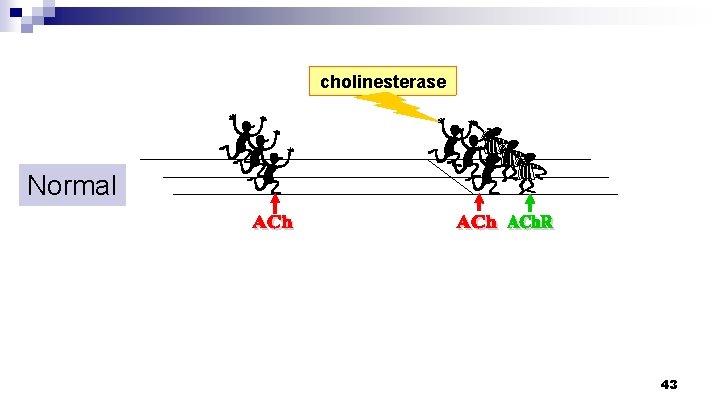
cholinesterase Normal 43
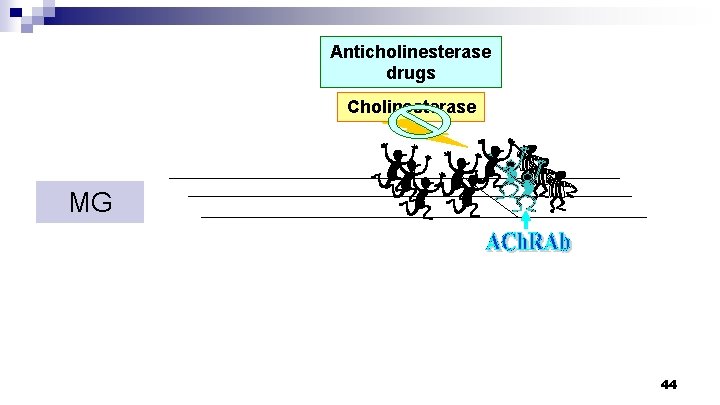
Anticholinesterase drugs Cholinesterase MG 44
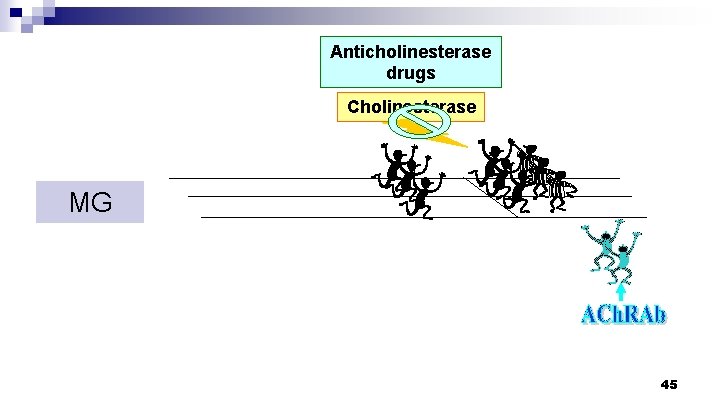
Anticholinesterase drugs Cholinesterase MG 45
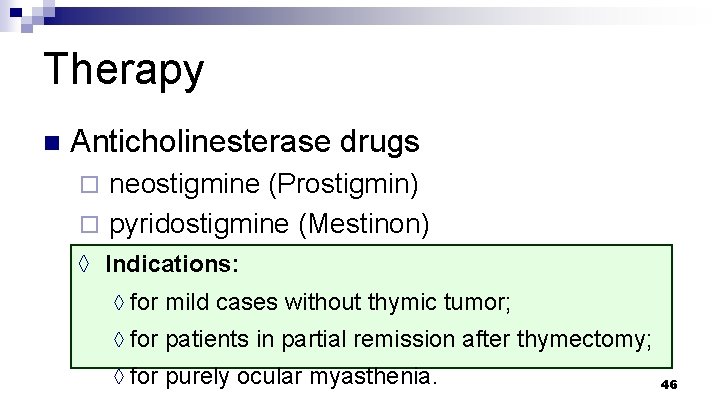
Therapy n Anticholinesterase drugs neostigmine (Prostigmin) ¨ pyridostigmine (Mestinon) ¨ n 30 -90 mg po. q 6 h ◊ Indications: ◊ for mild cases without thymic tumor; ◊ for patients in partial remission after thymectomy; ◊ for purely ocular myasthenia. 46
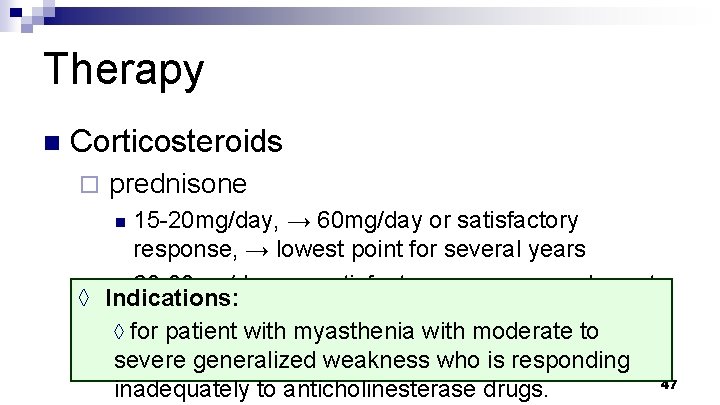
Therapy n Corticosteroids ¨ prednisone 15 -20 mg/day, → 60 mg/day or satisfactory response, → lowest point for several years n 60 -80 mg/day, → satisfactory response, → lowest ◊ Indications: point for several years ◊ for patient with myasthenia with moderate to severe generalized weakness who is responding 47 inadequately to anticholinesterase drugs. n
Therapy n Immunosuppressive drugs ¨ Azathioprine n 50 mg po. bid, → 75 -125 mg po. bid Cyclophosphamide ¨ Mycophenolate ¨ 48
Therapy n Plasma exchange 2 -3. 5 L each time, 1 -3 times per week, 3 -8 times totally ¨ The removed plasma is replaced with plasma ◊ of Indications: healthy human, or with albumin and saline. ¨ for severe myasthenia that is refractory to treatment with anticholinesterase drugs and prednisone, or during an acute worsening, especially those in 49 ◊
Therapy n Intravenous immune globulin ¨ 2 g/kg per day, over 3 to 5 days. 50
Therapy n Thymectomy ◊ Indications: ◊ for almost all patients with uncomplicated myasthenia gravis between puberty to 55 years of age. 51
Myasthenic Crisis n Definition ¨A rapid and severe deterioration of the myasthenia itself, just because it spreads to the respiratory muscles and results in dyspnea; usually assisted ventilation is a necessary treatment at this time. 52
Myasthenic Crisis n Classification ¨ ¨ ¨ . 53
Myasthenic Crisis n Precipitating factors respiratory infection ¨ excessive use of sedative drugs ¨ operations, including thymectomy ¨ mental stress ¨ 54
Myasthenic Crisis n Treatment mechanical ventilation ¨ withdrawing of anticholinergic drugs ¨ high-dose corticosteroid infusions or introvenous gamma globulin, or plasma exchange ¨ control of respiratory infection ¨ 55
Questions How to make a diagnosis of MG? n How to make differential diagnosis between MG and Lambert-Eaton syndrome? n What is MG crisis and how to treat it? n 56
The end! 57