Musculoskeletal System Types of Muscle Contraction Tone partial


![(From Beare, P. G. , Myers, J. L. [1998]. Adult health nursing. [3 rd (From Beare, P. G. , Myers, J. L. [1998]. Adult health nursing. [3 rd](https://slidetodoc.com/presentation_image_h2/8425dd93939498660769ecd30d3ebb35/image-36.jpg)

- Slides: 69
Musculoskeletal System
Types of Muscle Contraction Tone- partial contraction even when not in use, for constant readiness Isotonic- muscle gets shorter, thicker Work is produced: walking, running, weight lifting Isometric- no change in muscle length No movement produced Pushing against immovable objects
Effects of Aging on Muscle About age 40 Loss of muscle cells, size Loss of power (hunchback/kyphosis develops) Decrease in height Exercise (weight training) can delay progression of aging on muscles
Musculoskeletal Trauma Strains Sprains Dislocations Fractures Compartment Syndrome
Strain Injury to muscle or tendon due to overuse or overstretching Chronic strain-repeated use of muscles Acute strain-sudden severe pain Rest, possibly immobilization Ice, 20 -30 minutes on, 1 hr off, for 24 hrs Heat for comfort after 1 st 24 hrs Rupture may require surgery

Sprain Injury to ligaments surrounding a joint Caused by sudden twist, wrench, or fall Symptoms: Pain, edema, loss of motion, ecchymosis Treatment Rest Ice Compression Elevation After edema decreases, a cast may be applied
Dislocation Articular surfaces of joints no longer in contact May hinder blood supply, damage nerves, tear ligaments, rupture muscle attachments Traumatic-can be orthopedic emergency Congenital-present at birth Pathologic-caused by disease
Dislocation Symptoms Local joint pain Loss of function Change in length of extremity Change in contour of joint
Fracture Break in continuity of bone Usually involve soft tissue damage Blood vessels, nerves, tendons Caused by Trauma Disease process High risk Tumors, osteoporosis, poor coordination or vision, syncope, general weakness
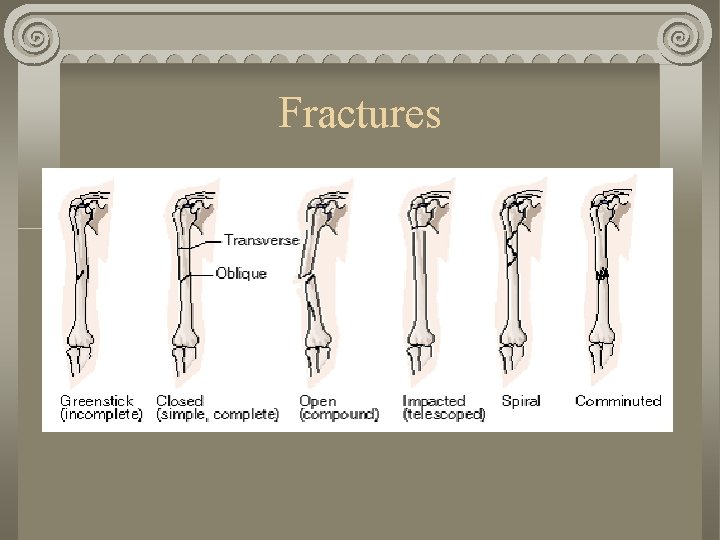
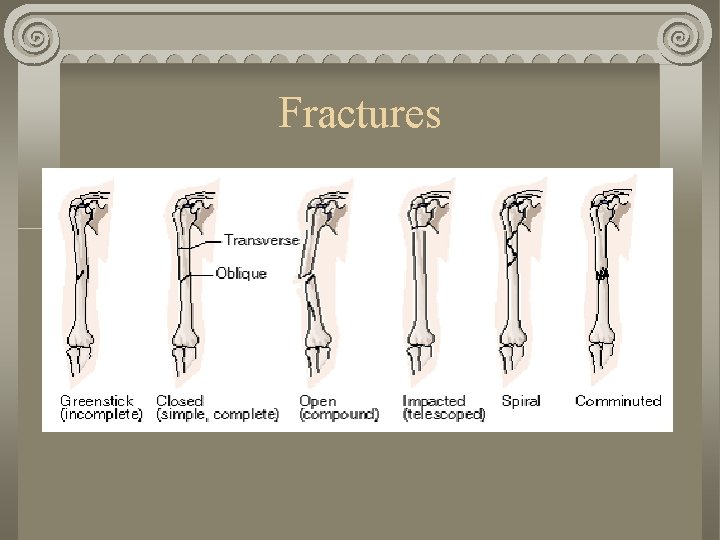
Types of Fractures Greenstick (incomplete) Closed (simple, complete) Open (compound) Impacted (telescope) Spiral Comminuted
Fractures
Greenstick Most often in children Break not all way through Splinters on one side, bends on other
Closed Uncomplicated Break complete through bone Skin in tact
Open/Compound Bone broken completely Skin also broken, allows bone to protrude through skin Greater risk of infection
Impacted/Telescoping One part of the bone is driven into another
Spiral Twists around the shaft of the bone From a twisting force
Comminuted Bone splintered into many unaligned fragments
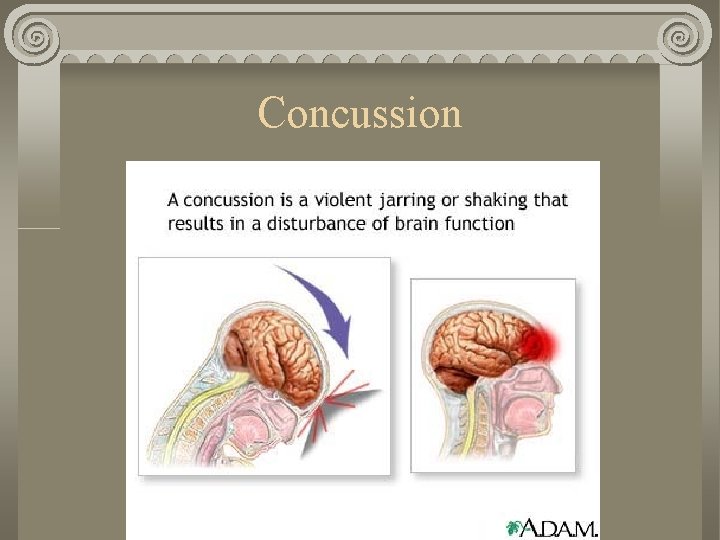
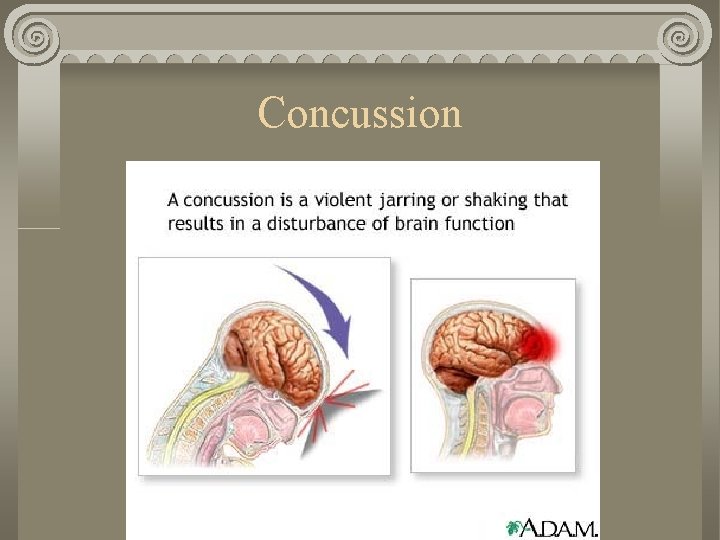
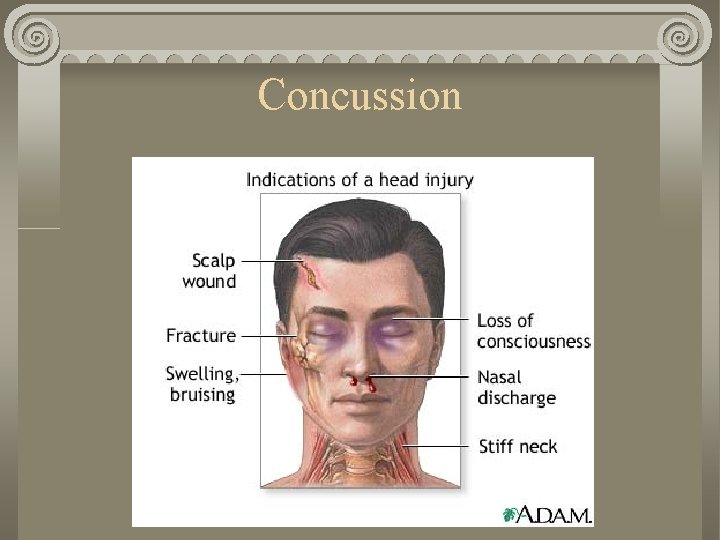
Concussion
The brain can be affected directly by damage to the nervous system tissue and bleeding. It can be affected indirectly by blood clots which form under the skull, but compress the underlying brain tissue (subdural or epidural hematoma).
A simple fracture is a break in the bone without damage to the skin. A linear skull fracture is a break in a cranial bone resembling a thin line, without splintering, depression, or distortion of bone.
A depressed skull fracture is a break in a cranial bone (or "crushed" portion of skull) with depression of the bone in toward the brain. A compound fracture involves a break in, or loss of skin and splintering of the bone.
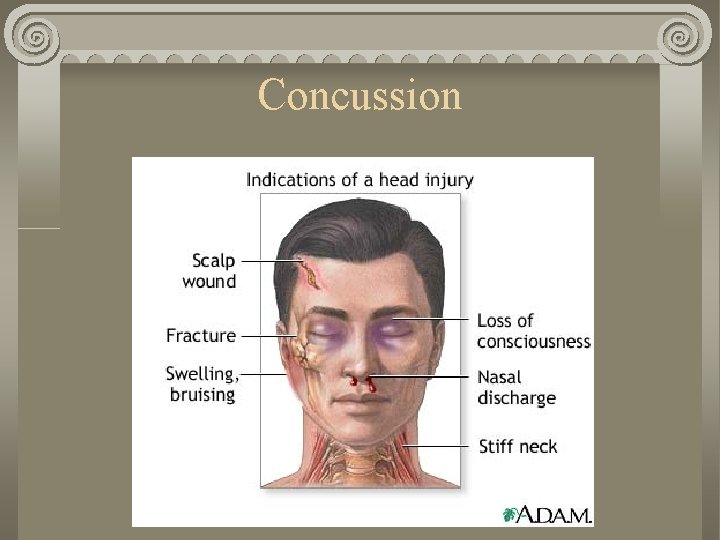
Concussion
Concussion Prevention Attention to safety, including the use of appropriate athletic gear, such as bike helmets and seat belts, reduces the risk of head injury.
Skull Fracture: Prevention 1. Use car seats or seat belts whenever in a motor vehicle. 2. Use helmets whenever biking, skating, climbing, or playing contact sports. 3. Use equipment designed specifically for the type of sport or recreation in which you are participating.
4. Provide appropriate supervision for children of any age. 5. Do not allow children to bike or skate at night. 6. Provide highly visible clothing. 7. Teach children to obey traffic rules and signals. 8. Educate individuals about risks of various work, recreational, or sport activities and how to avoid injury.
Healing Determined by Age of client Type of injury or disease process May take weeks, months, or years to heal
Healing Sequence Hematoma forms Granulation tissue formation Soft callous formation-temporary splint Callous ossification-calcium salt deposits form rigid bone and bind ends together Remodeling-excess bone removed by osteoclastic activity

Fracture Complications Can delay healing or be life threatening Infection open skin or hardware placed Fat embolism fat from bone marrow travels to lung or heart Compartment syndrome Neurovascular impairment
Fat Embolism Usually occurs within 24 -72 hours post injury Can occur up to a week post injury Small lung area involved Pain, tachycardia, dyspnea Large lung area involved Severe pain, dyspnea, cyanosis, restlessness, shock
Fat Embolism Treatment Bed rest Gentle handling Oxygen IV fluids
Complications of Fractures Fat embolism Cause Clinical manifestations/assessment Medical management/nursing interventions
Compartment Syndrome Progressive constriction of blood vessels and nerves can lead to permanent damage Can occur with any orthopedic injury Untreated
Compartment Syndrome Emergency Pain not relieved by narcotic analgesics Paresthesia (numbness, tingling) Paralysis Treatment is to relieve pressure Remove cast/dressing Fasciotomy
Complications of Fractures Compartment syndrome Cause Clinical manifestations/assessment Medical management/nursing interventions
![From Beare P G Myers J L 1998 Adult health nursing 3 rd (From Beare, P. G. , Myers, J. L. [1998]. Adult health nursing. [3 rd](https://slidetodoc.com/presentation_image_h2/8425dd93939498660769ecd30d3ebb35/image-36.jpg)
(From Beare, P. G. , Myers, J. L. [1998]. Adult health nursing. [3 rd ed. ]. St. Louis: Mosby. ) Compartment syndrome.
Other Complications of Fractures Shock Cause Clinical manifestations/assessment Medical management/nursing interventions
Other Complications of Fractures Gas gangrene Cause Clinical manifestations/assessment Medical management/nursing interventions
Other Complications of Fractures Thromboembolus Cause Clinical manifestations/assessment Medical management/nursing interventions

Medical-Surgical Management Treatment of a Fracture Immediate Realign the fracture Maintain the alignment Regain function
Method of Treatment Depends on First aid given Location of injury Severity Type of fracture Age and condition of client
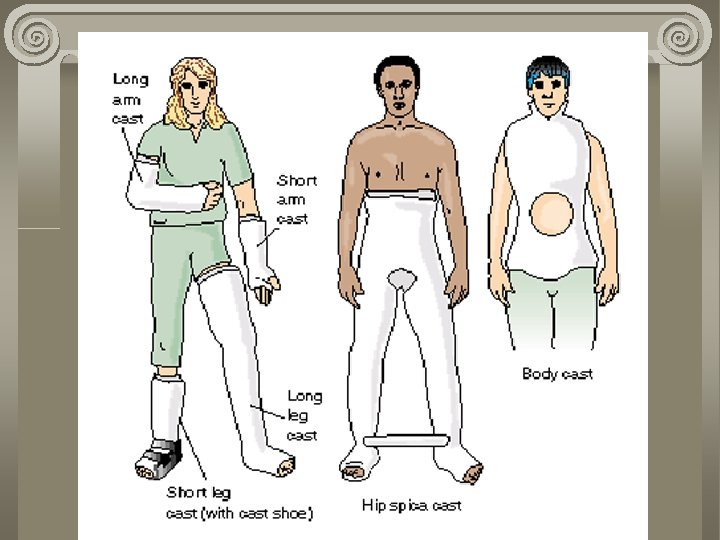
Casts For stabilization, immobilization, support, and protection Plaster or synthetic/fiberglass Synthetics, non-weight bearing parts of body Casts should extend to joints above and below affected part
Casts Continued Cast should by dry, odorless, shiny, resonant Underlying moisture causes cast to feel cool, smell musty, and sound dull on percussion
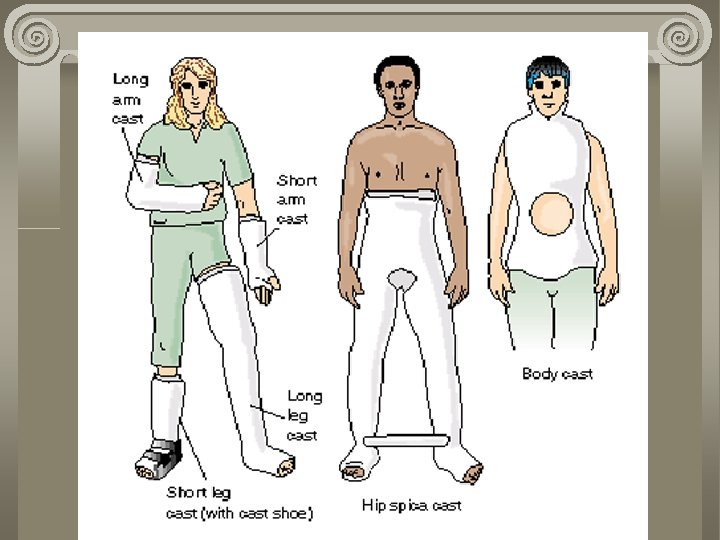
Types of Casts Long and short leg Spica cast, treats part or all of one or more extremities Walking cast Body cast Windowing-cut a hole over a body area to relieve pressure, such as for abdominal distention
Client Teaching - Casts Plaster casts should dry from inside out DO NOT USE A HAIR DRYER or Heat Lamp Heat during application is normal and will subside, 10 -15 minutes Avoid indentation, rest on pillow to dry Synthetic casts dry in minutes
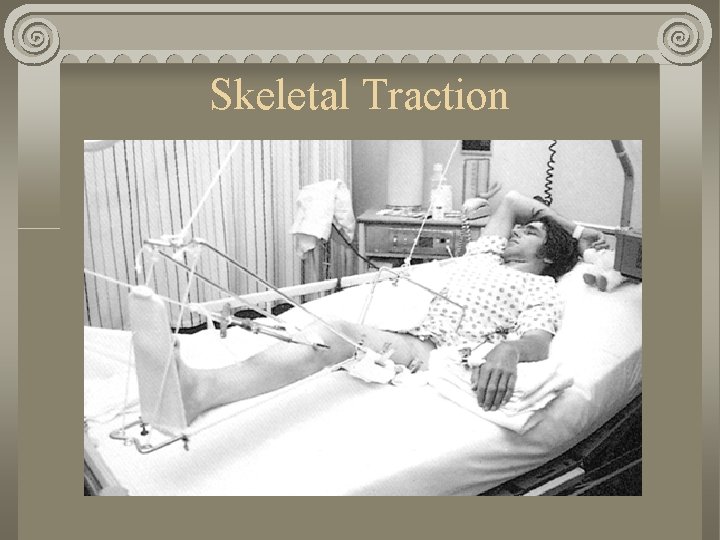
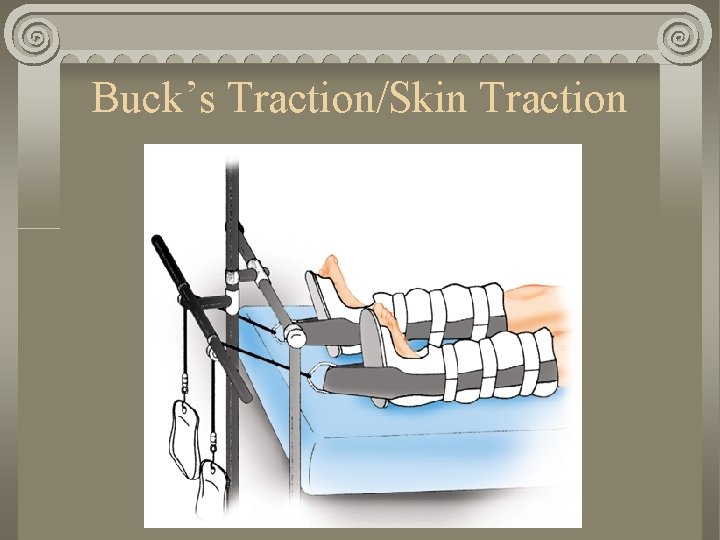
Traction Two forces pulling in opposite directions Consists of weights and counterweights Can be used to reduce a fracture, immobilize an extremity, decrease muscle spams, correct or prevent deformity
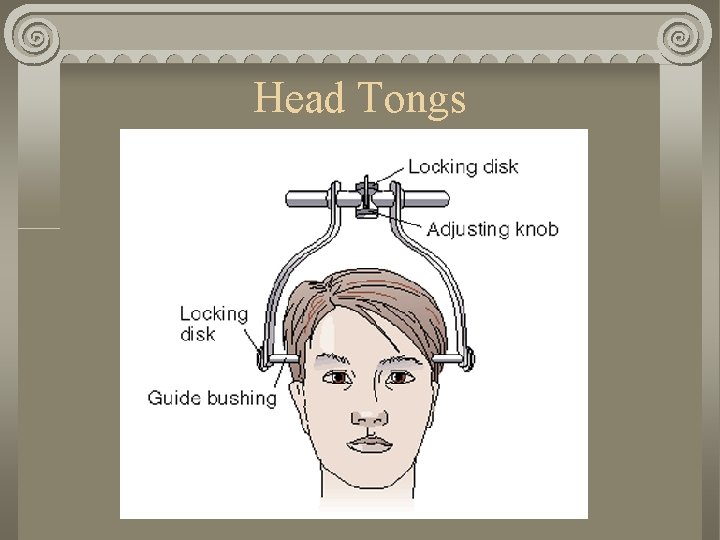
Types of Traction Skeletal Requires surgical insertion of pins or wires through bones Continuous Fx of femur, tibia, cervical spine (Head tongs) Skin Non-surgical Shorter period of time Tapes, traction strips, cervical halters, pelvic belts Manual
You Need to Know Which type traction What it is being used for How it works Associated complications Extent of the injury Movements and positions allowed
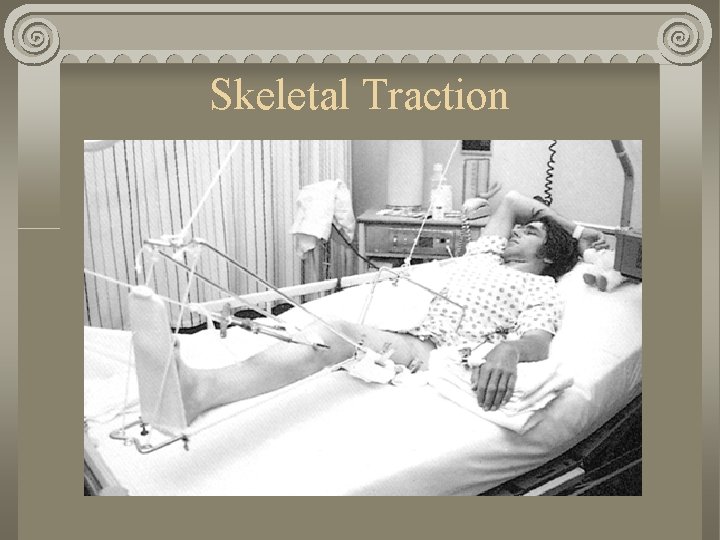
Skeletal Traction
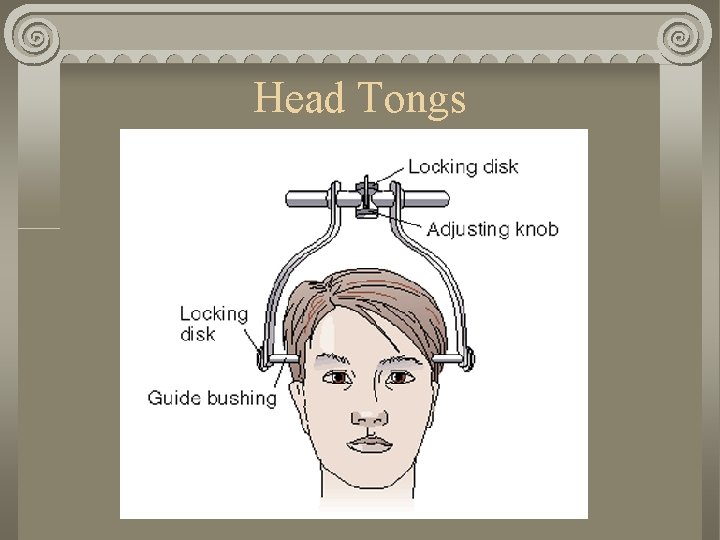
Head Tongs
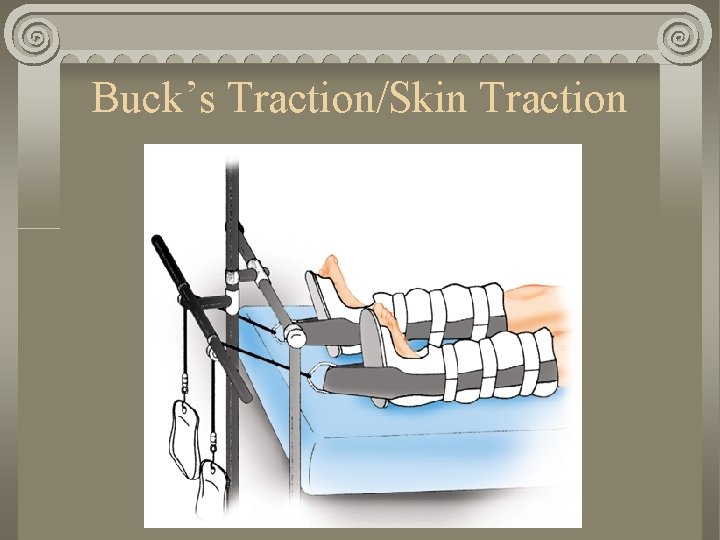
Buck’s Traction/Skin Traction
Nursing Care Dressing care Pin care Body alignment Alignment of traction apparatus ROM for allowed joints Client education
Devices Canes Walkers Crutches
Ambulation Devices Canes Full weight bearing Aid with balance and support Held in hand opposite affected extemity Opposite arm and leg move together Walkers Limited weight bearing Provide more stability
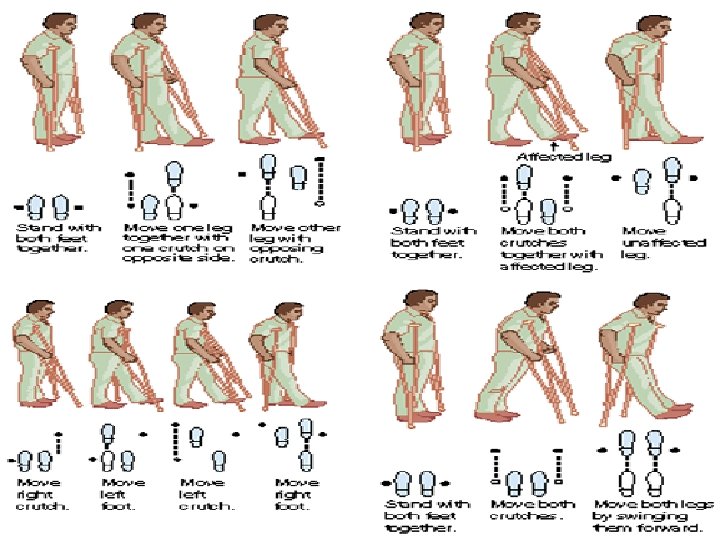
Crutchwalking Crutch pad 1. 5 – 2” below axilla (avoid nerve damage) Elbows bent 30 degrees Apply gait belt
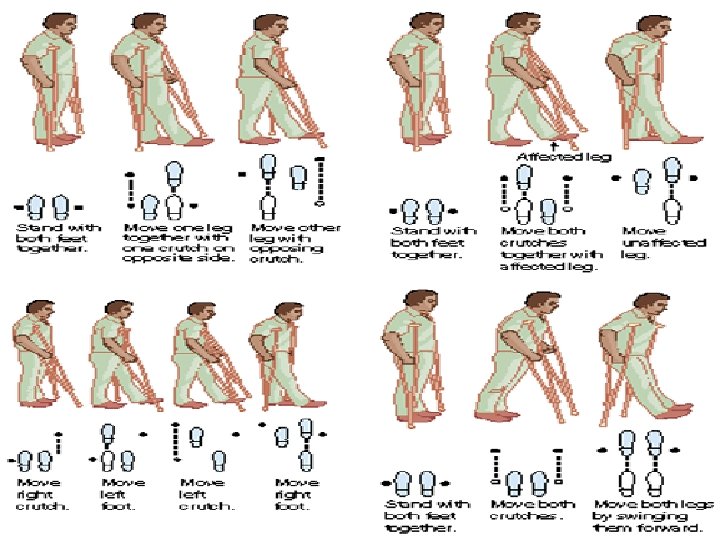
Four-Point Gait Move right foot and left crutch forward 4 -6 inches Move left foot and right crutch forward 4 -6 inches Repeat Client must be weight-bearing in both legs
Three-Point Gait Advance both crutches and weaker leg together 4 -6 inches Move strong leg forward Repeat Can be used for one weak or non-weight bearing leg
Two-Point Gait Move left crutch and right leg forward 4 -6 inches Move right crutch and left leg forward 4 -6 inches Repeat Client must be weight bearing on both legs Faster than four-point gait
Swing Through Gait Move both crutches forward 4 -6 inches Move both legs forward even with crutches Repeat Requires greater balance and more strength
Surgical Reduction ORIF-Open Reduction Internal Fixation Hardware placed to maintain the reduction Disadvantages
Pharmacology for Fractures Analgesics – pain Muscle relaxants- spasms Stool softeners-constipation
General Fracture, Sprain, & Strain Prevention Muscle and Bone strengthening Minimize high-risk behavior Helmets Appropriate protective sports equipment Slow down, use caution Vitamin D, Calcium Warm-up prior to strenuous exercise
Diet Fiber Protein Calcium Phosphorus Fluids Vitamin & mineral supplements
Activity Exercise joints that are not immobilized Isometric exercises (constant resistive force) help maintain muscle strength
Nursing Process Subjective Data Pain, especially on movement Muscle spasms Paresthesia (numbness, tingling) Neurovascular /CMS check Circulation Movement sensation
5 P’s Check 5 P’s Assessment Pain Pallor (slow capillary refill) Paresthesia (numbness or tingling) Puffyness (edema) Pulselessness
Objective Data Edema, shortening, deformity Pulses in affected limb Compare pulse in non-affected limb Vital signs Check skin for color and temperature Check cast edges for smoothness Traction weights should hang free