Musculoskeletal System Inflammatory Disorders Presentations Rheumatoid Arthritis Ankylosing



- Slides: 35
Musculoskeletal System
Inflammatory Disorders Presentations Rheumatoid Arthritis Ankylosing spondylitis Osteomyelitis Bursitis
Degenerative Disorders Osteoporosis Osteoarthritis DJD/Degenerative Joint Disease Total Joint Arthroplasty
Osteoporosis Increased porosity in the bone Common disorder of bone metabolism Decreased mineral and protein matrix Bone brittle, fragile Prone to fractures
Osteoporosis 10 million people in United States have Osteoporosis Another 34 million have low bone density, which puts them at risk for Osteoporosis 80% of affected are women 1. 5 million fractures occur each year related to Osteoporosis

Osteoporosis Silent disease No symptoms of bone loss May have 50% loss prior to diagnosis Multiple fractures may cause decrease in height Only diagnosed by BMD Bone Mineral Density Painless Non-invasive safe
Osteoporosis Risk Factors Small bones Advanced age Family history Post-menopause with out estrogen replacement Eating disorders Low calcium diet Inactive activity Smoking Increased alcohol consumption Use of corticosteroids or anticonvulsant medications
Medical-Surgical Management Pharmacological four medications – Estrogen Fosamax Miacalcin Testosterone No cure Prevention
Osteoporsis Diet Activity
Nursing Process Assessment Subjective Data
Objective Data
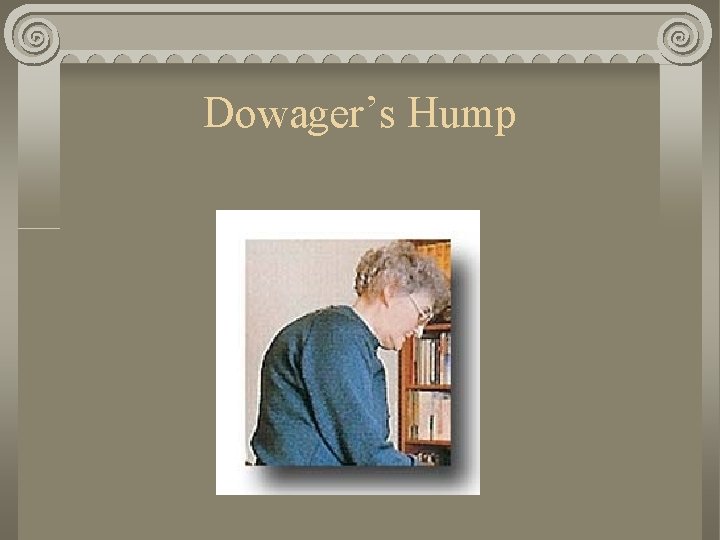
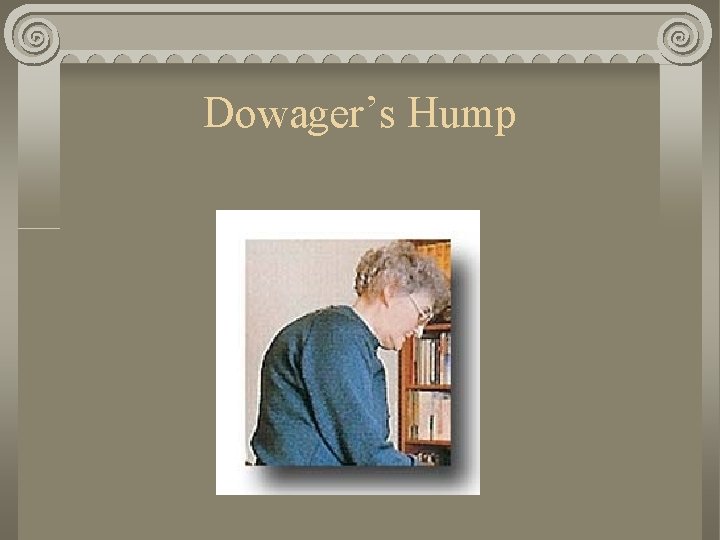
Dowager’s Hump
Degenerative Joint Disease/DJD Osteoarthritis NOT inflammatory Wear and tear disease Slow, steady, progressive destruction of the joint Etiology unknown Most common form of arthritis
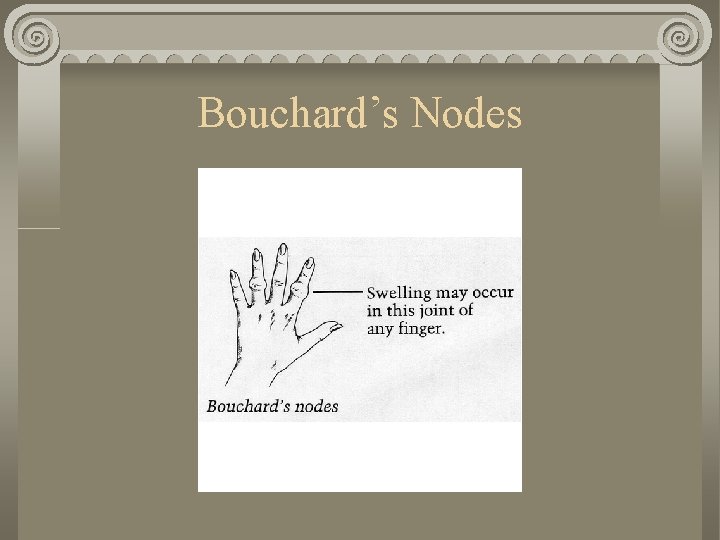
Osteoarthritis or DJD Symptoms Early morning stiffness Pain after physical activity Joint enlargement Bouchard’s nodes Heberden’s nodes Hypertrophic spurs – Distal interphalanges – Hard, painless
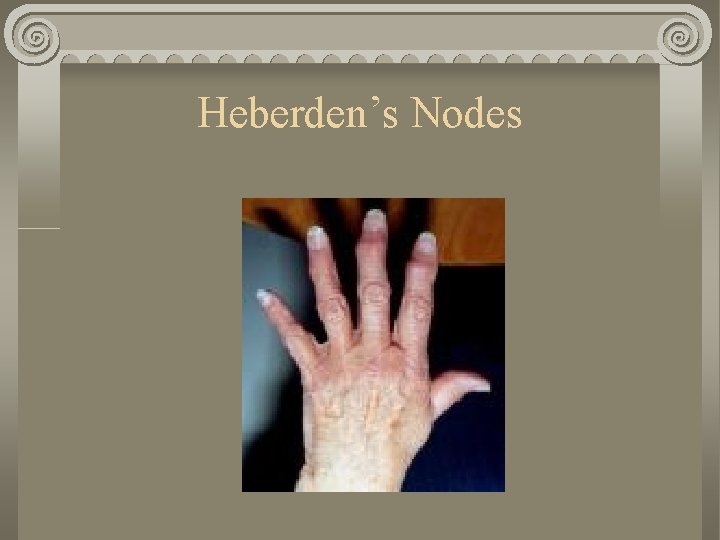
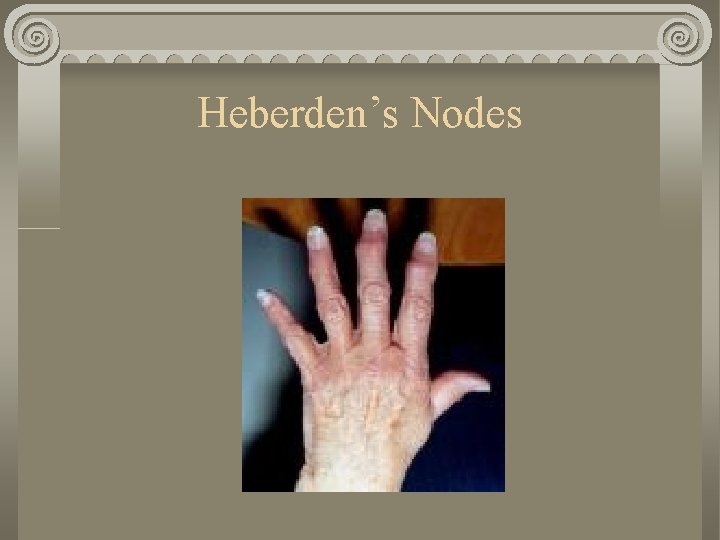
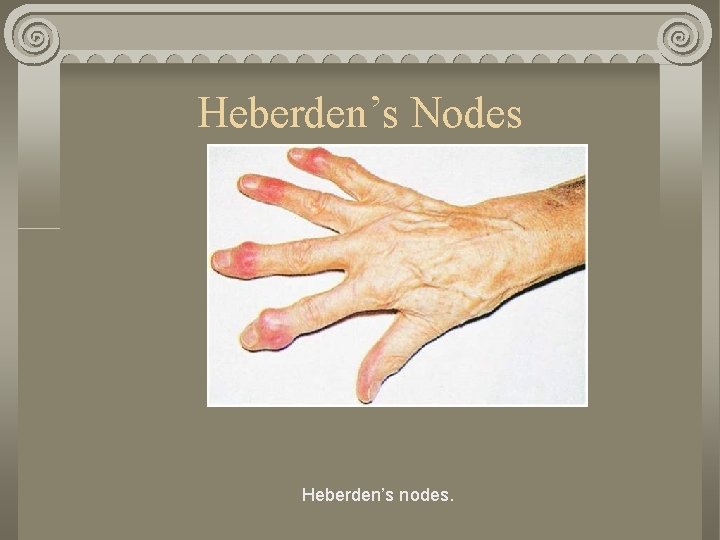
Heberden’s Nodes
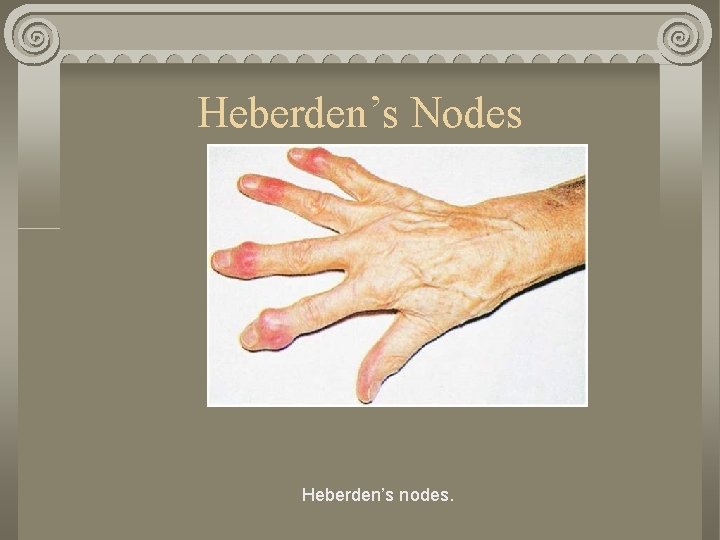
Heberden’s Nodes Heberden’s nodes.
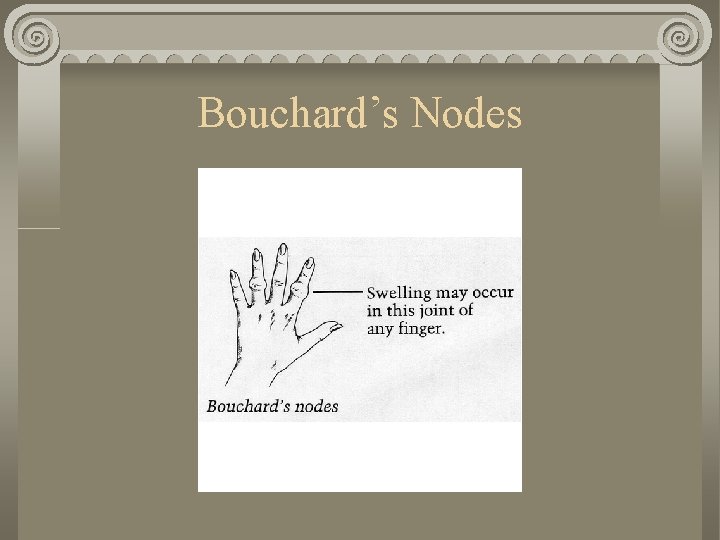
Bouchard’s Nodes
Osteoarthritis Diagnostic tests Radiographic studies Arthroscopy Synovial fluid examination Bone scans
Osteoarthritis Medical management/nursing interventions Surgery
Total Joint Arthroplasty Joint replacement Replacement of both articular surfaces with in a joint capsule Hip, knee, shoulder and fingers are most common sites Replacement consist of metal and polyethylene
Total Joint Arthroplasty Older method of cemented in prepared bone is not used as often New technology uses porous coated cementless artificial joint component. This allows bone to grow into the joint and less prosthesis failure noted.
Total Hip Replacement of severely damaged hip with an artificial joint Usually people over 60 years Severe pain, irreversible damage to hip joints
Hip Replacement Potential problems Dislocation of prosthesis Excessive wound drainage Infection
Following Hip Replacement Client’s hip and leg to be kept in position of adduction and extension Knees are apart by abductor pillow or by using foam wedges Entire leg to be supported when turning side to side AVOID ACUTE FLEXION OF THE HIP
Following Hip Replacement Fracture bed pan should be used Raised toilet seat in bathroom Vital signs, circulation, movement and sensation checks (CMS) to be done frequently Inspect dressing frequently Monitor drainage from portable suction device (JP Drainage) can be as high as 200 -500 cc. With in 48 hours should be less than 30 cc and suction devices can be removed.
Client Goals after Hip Replacement Ambulate independently Out of bed the night of the surgery or the next day Gait training begins so that client can use crutches or cane FLEXION OF KNEE TO BE AVOIDED No more than 90 degrees No stair climbing for three months
Total Knee Replacement Severe pain and functional disability related to joint destruction Following knee replacement clients may use CPM continuous passive motion machine which helps increase circulation to operative area and promotes flexibility with in he knee joint.

Knee Replacement Following surgery…. Knee to be imoblized Firm compression dressing Adjustable soft knee immobilizer Transfer to chair ok, but NO WEIGHT BEARING is allowed on knee until ordered my MD
Total knee replacement SCD – Sequential Compression Device may be used or TED hose – Anti embolism stocking worn to minimize the development of thrombophlebitis Rehabilitation starts second day When patient is sitting knee should be elevated Weight bearing should start with in 1 - 2 days

Nursing Management Cough and deep breathe Use trapeze to raise hips off bed for bedpan use
Nursing. Assessment Nursing Assessment should include… Neurovascular assessment of affected extremity Incision assessment Vital signs Lung sounds Pedal pulses Intake and output
Nursing Assessment Irritablity Restlessness Orientation Neurovascular assessment for pain, numbness, tingling and paresthesia
Objective Assessment Incision assessment for Approximation Redness Drainage Skin color
Assessment Other assessments Tachypnea Dyspnea Hypoxia Crackles and wheezes ( s/s of fat embolism) Position of affected part
Care Plans Divide in to groups and create care plans