Musculoskeletal MRI Pulse Sequences A Review for Residents
- Slides: 62
Musculoskeletal MRI Pulse Sequences: A Review for Residents and Fellows Stephanie Jo, MD, Ph. D, Steffen Sammet, MD, Ph. D, Stephen Thomas, MD, G. Scott Stacy, MD
Author affiliations: From the Department of Radiology, University of Pennsylvania, Philadelphia, Pa (S. J. ); and Department of Radiology, University of Chicago, Ill (S. S. , S. T. , G. S. S. ). Address correspondence to S. J: Penn University City, 3737 Market St Mailbox 4, Philadelphia, PA 19104 S (email: stephanie. jo@pennmedicine. upenn. edu). This material was partly presented as an electronic exhibit at the 2018 RSNA Annual Meeting (ID 18004613). All authors have disclosed no relevant relationships.
Abbreviations 2 D = two dimensional, 3 D = three dimensional, ABER = abduction – external rotation, ADC = apparent diffusion coefficient, CHESS = chemical shift selective fat suppression, DWI = diffusion weighted imaging, EPI = echo planar imaging, ETL = echo train length, FABS = flexion, abduction and supination, FSE = Fast Spin Echo, Gd = Gadolinium, GRE = gradient echo, i. v. = intravenous, MAA = magic angle artifact, MR = magnetic resonance, MRI = magnetic resonance imaging, MSK = musculoskeletal, PD = proton density, RF = radiofrequency, SE = spin echo, SNR = signal to noise ratio, STIR = short-T 1 inversion recovery, TE = echo time, TI = inversion time, TR = repetition time, TSE = Turbo Spin Echo
Learning Objectives At the end of this presentation, the viewer should be able to: 1. Understand the basic MR physics principles used for creation of common musculoskeletal MRI pulse sequences 2. Describe the fundamental differences between spin-echo and gradient-echo pulse sequences 3. Describe the application and appropriate selection of various pulse sequences used for musculoskeletal MR imaging 4. Describe various methods of fat suppression 5. Understand the basics of motion, susceptibility, and magic angle artifacts
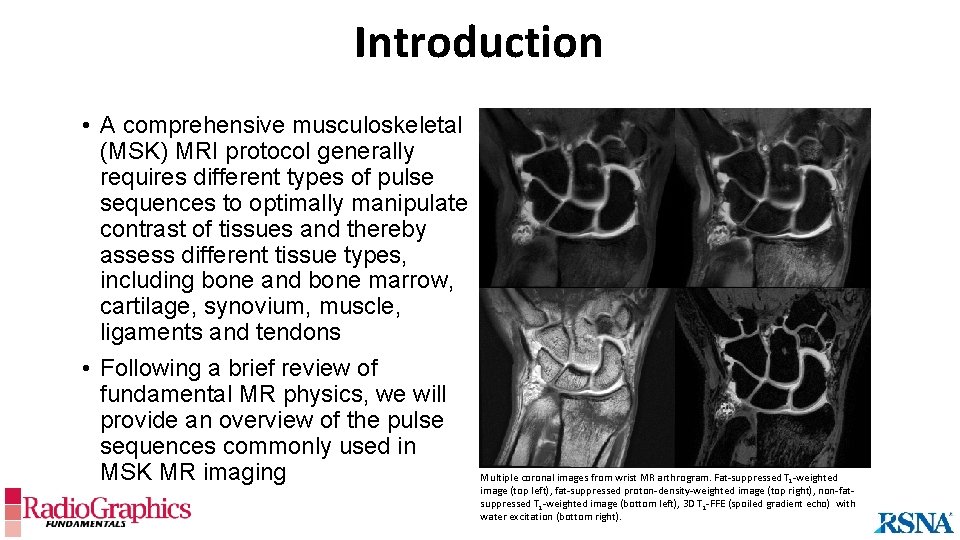
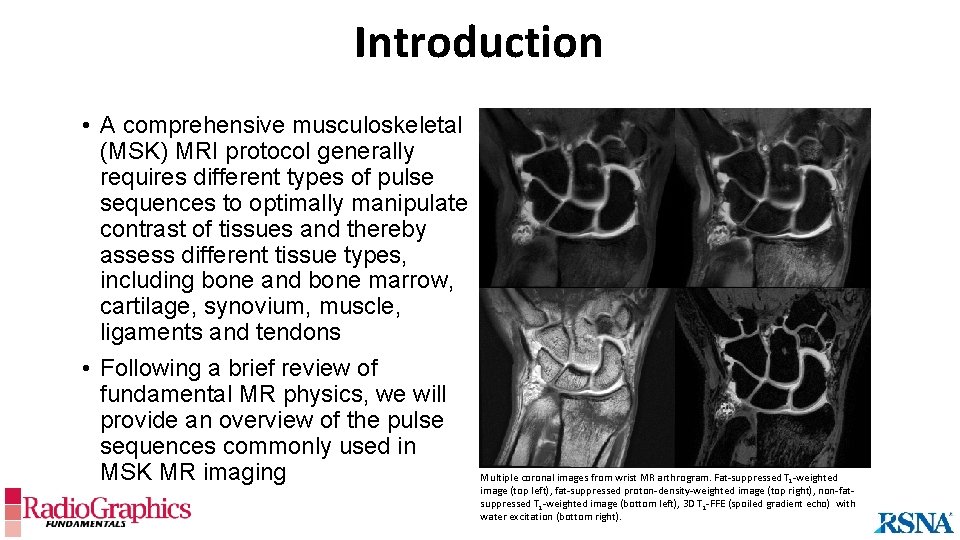
Introduction • A comprehensive musculoskeletal (MSK) MRI protocol generally requires different types of pulse sequences to optimally manipulate contrast of tissues and thereby assess different tissue types, including bone and bone marrow, cartilage, synovium, muscle, ligaments and tendons • Following a brief review of fundamental MR physics, we will provide an overview of the pulse sequences commonly used in MSK MR imaging Multiple coronal images from wrist MR arthrogram. Fat-suppressed T 1 -weighted image (top left), fat-suppressed proton-density-weighted image (top right), non-fatsuppressed T 1 -weighted image (bottom left), 3 D T 1 -FFE (spoiled gradient echo) with water excitation (bottom right).
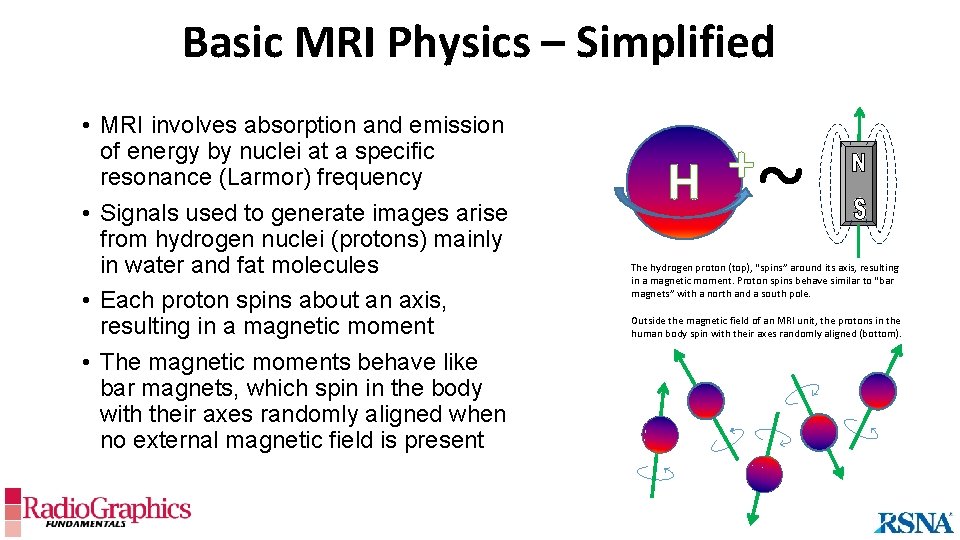
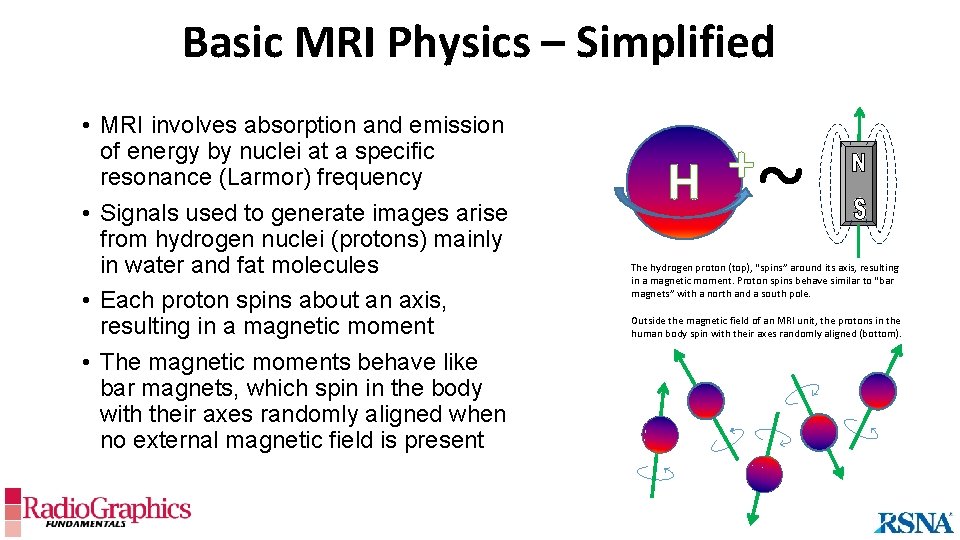
Basic MRI Physics – Simplified • MRI involves absorption and emission of energy by nuclei at a specific resonance (Larmor) frequency • Signals used to generate images arise from hydrogen nuclei (protons) mainly in water and fat molecules • Each proton spins about an axis, resulting in a magnetic moment • The magnetic moments behave like bar magnets, which spin in the body with their axes randomly aligned when no external magnetic field is present + H ~ The hydrogen proton (top), “spins” around its axis, resulting in a magnetic moment. Proton spins behave similar to “bar magnets” with a north and a south pole. Outside the magnetic field of an MRI unit, the protons in the human body spin with their axes randomly aligned (bottom).
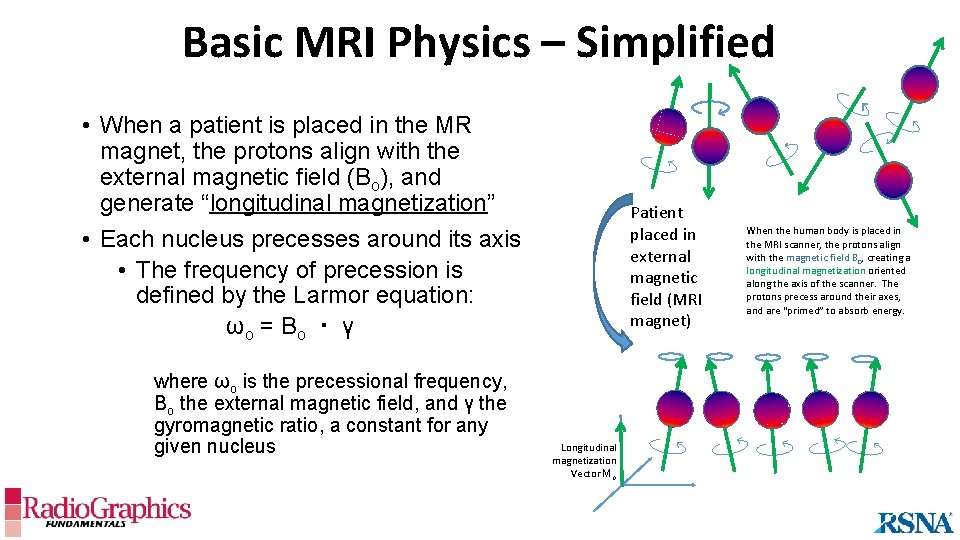
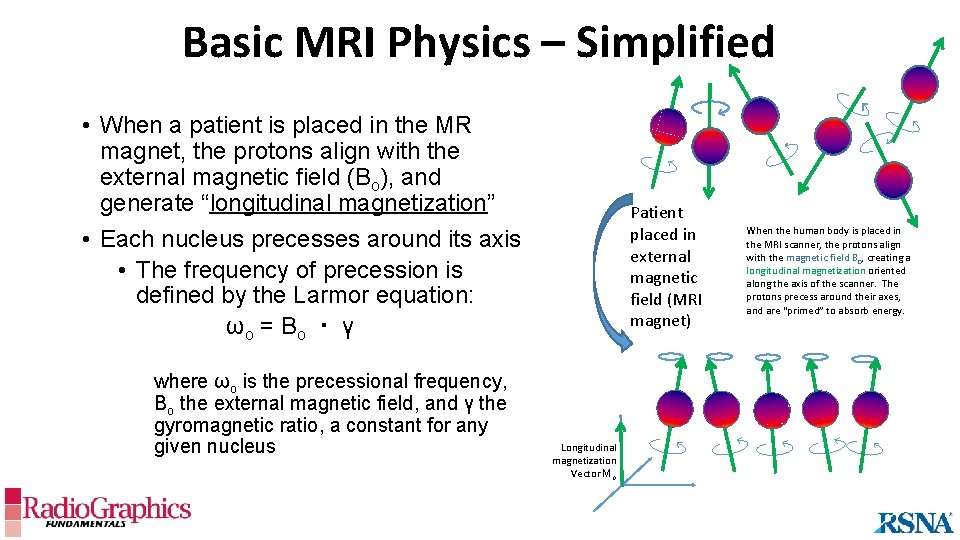
Basic MRI Physics – Simplified • When a patient is placed in the MR magnet, the protons align with the external magnetic field (Bo), and generate “longitudinal magnetization” • Each nucleus precesses around its axis • The frequency of precession is defined by the Larmor equation: ωo = B o ・ γ where ωo is the precessional frequency, Bo the external magnetic field, and γ the gyromagnetic ratio, a constant for any given nucleus Patient placed in external magnetic field (MRI magnet) Longitudinal magnetization Vector Mo When the human body is placed in the MRI scanner, the protons align with the magnetic field B 0, creating a longitudinal magnetization oriented along the axis of the scanner. The protons precess around their axes, and are “primed” to absorb energy.
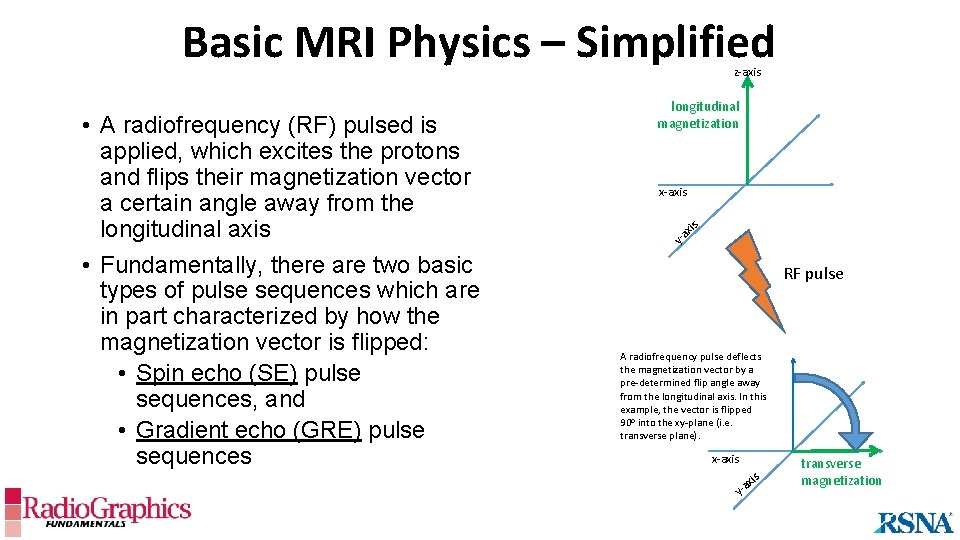
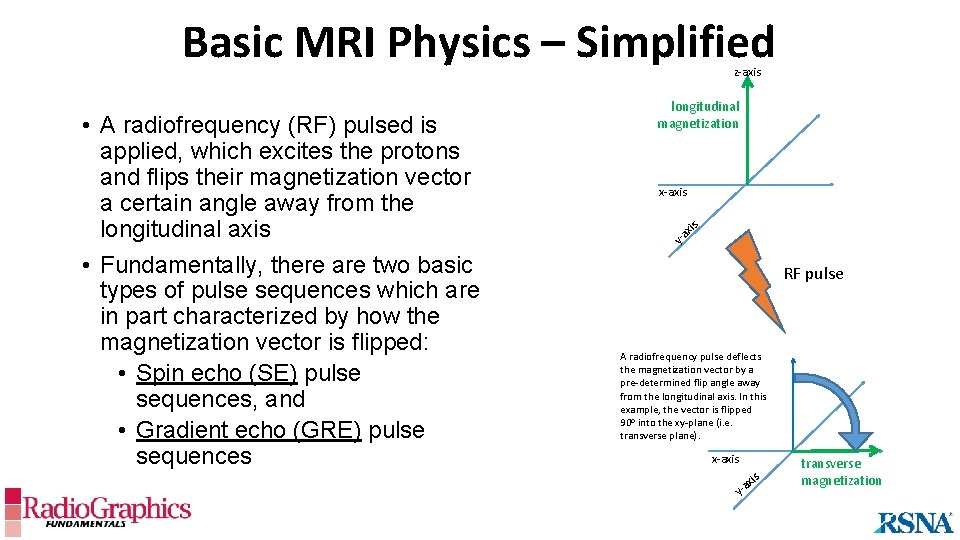
Basic MRI Physics – Simplified z-axis • A radiofrequency (RF) pulsed is applied, which excites the protons and flips their magnetization vector a certain angle away from the longitudinal axis • Fundamentally, there are two basic types of pulse sequences which are in part characterized by how the magnetization vector is flipped: • Spin echo (SE) pulse sequences, and • Gradient echo (GRE) pulse sequences longitudinal magnetization x-axis is ax y RF pulse A radiofrequency pulse deflects the magnetization vector by a pre-determined flip angle away from the longitudinal axis. In this example, the vector is flipped 90 o into the xy-plane (i. e. transverse plane). x-axis y- is ax transverse magnetization
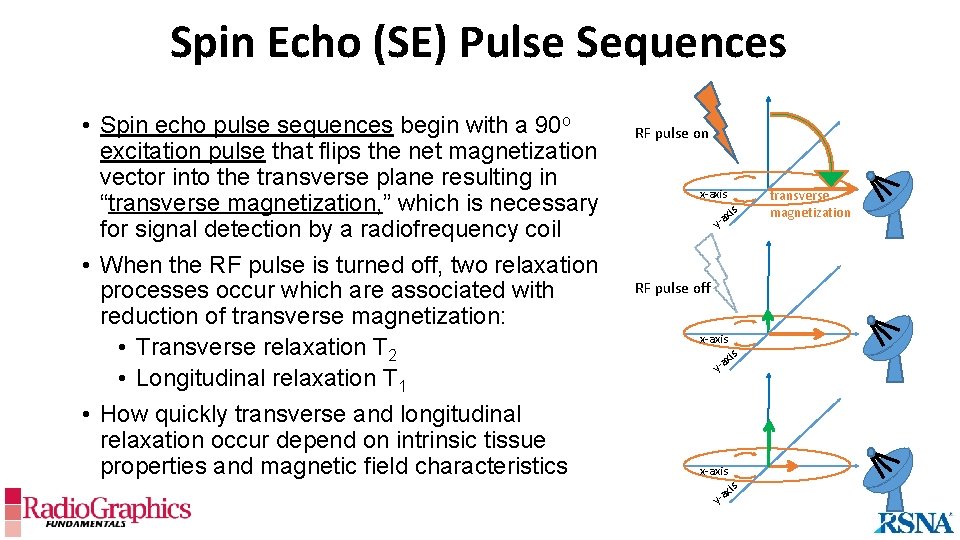
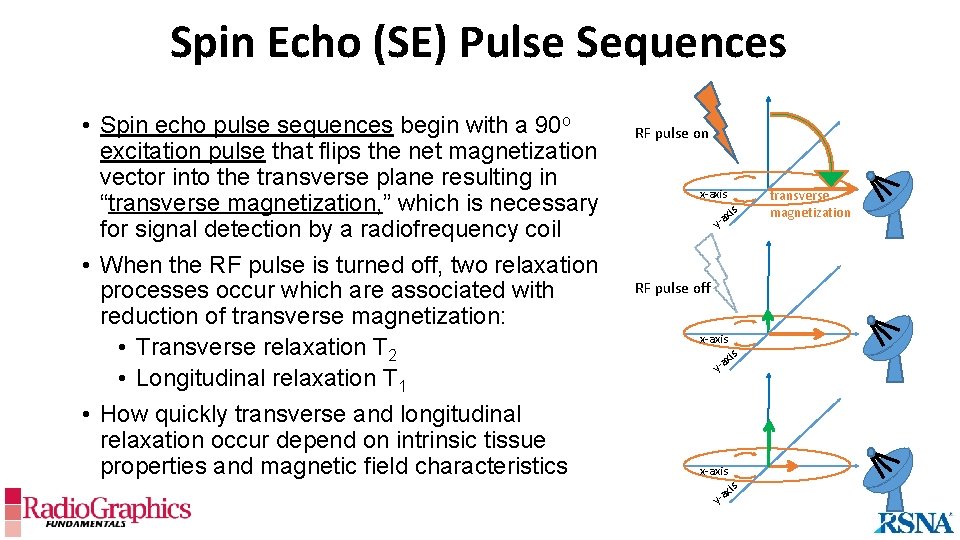
Spin Echo (SE) Pulse Sequences • Spin echo pulse sequences begin with a 90 o excitation pulse that flips the net magnetization vector into the transverse plane resulting in “transverse magnetization, ” which is necessary for signal detection by a radiofrequency coil • When the RF pulse is turned off, two relaxation processes occur which are associated with reduction of transverse magnetization: • Transverse relaxation T 2 • Longitudinal relaxation T 1 • How quickly transverse and longitudinal relaxation occur depend on intrinsic tissue properties and magnetic field characteristics RF pulse on x-axis y-a RF pulse off x-axis xis y-a transverse magnetization
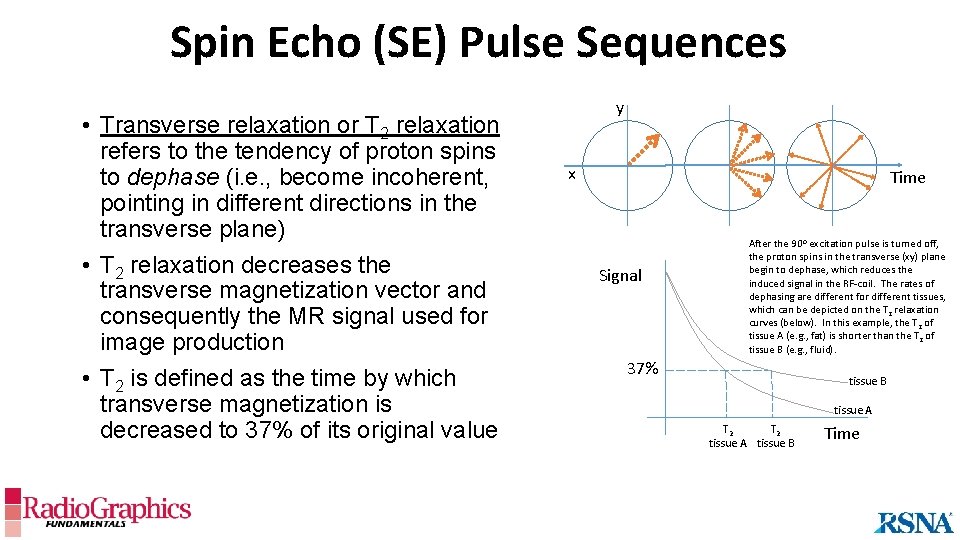
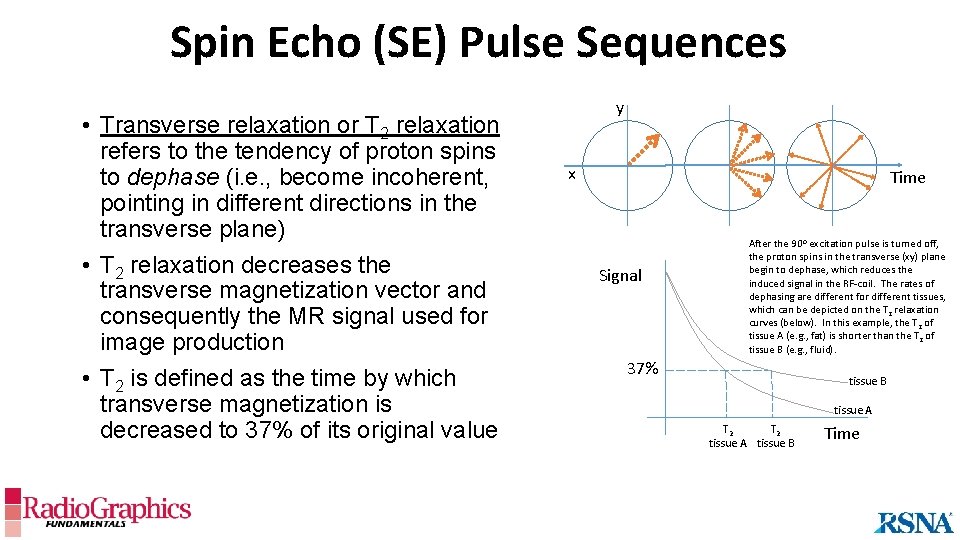
Spin Echo (SE) Pulse Sequences • Transverse relaxation or T 2 relaxation refers to the tendency of proton spins to dephase (i. e. , become incoherent, pointing in different directions in the transverse plane) • T 2 relaxation decreases the transverse magnetization vector and consequently the MR signal used for image production • T 2 is defined as the time by which transverse magnetization is decreased to 37% of its original value y x Time Signal After the 90 o excitation pulse is turned off, the proton spins in the transverse (xy) plane begin to dephase, which reduces the induced signal in the RF-coil. The rates of dephasing are different for different tissues, which can be depicted on the T 2 relaxation curves (below). In this example, the T 2 of tissue A (e. g. , fat) is shorter than the T 2 of tissue B (e. g. , fluid). 37% tissue B tissue A T 2 tissue A tissue B Time
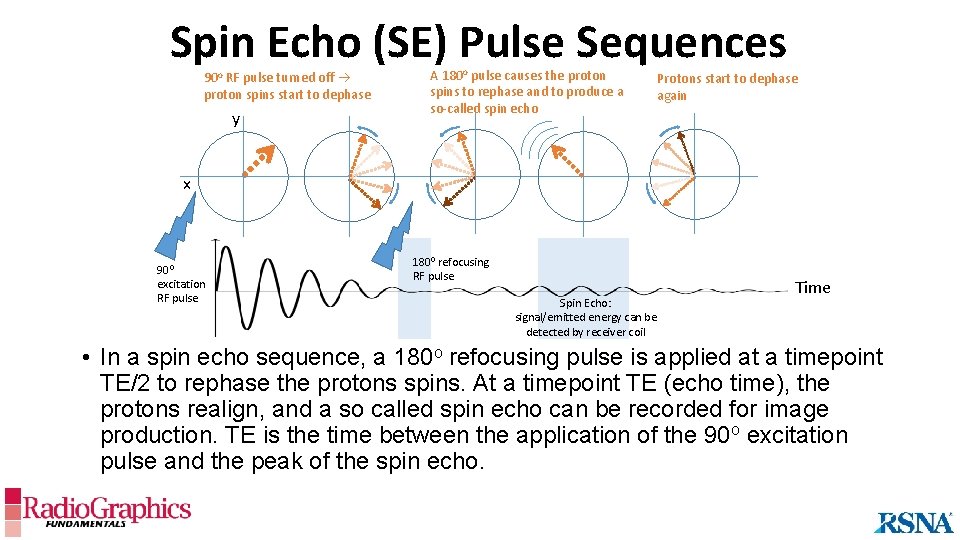
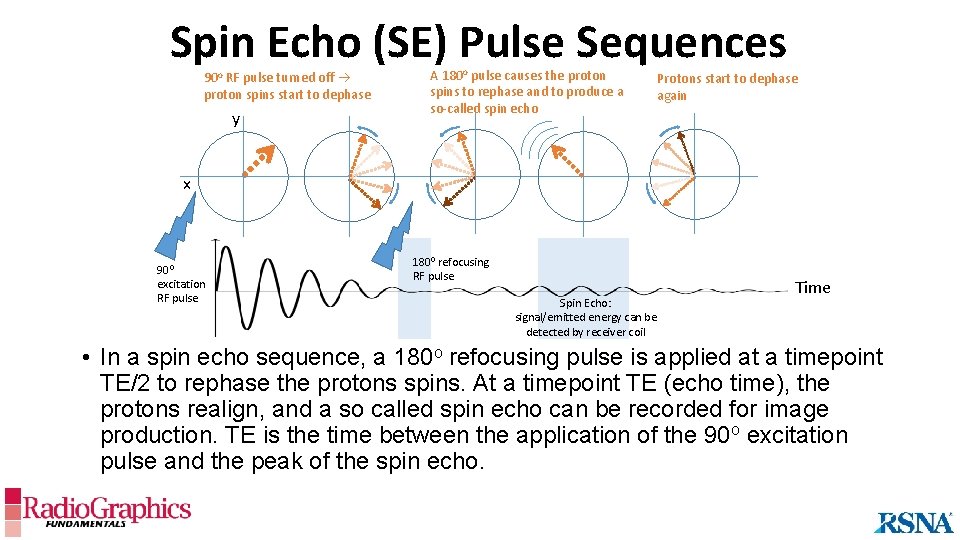
Spin Echo (SE) Pulse Sequences 90 o RF pulse turned off proton spins start to dephase y A 180 o pulse causes the proton spins to rephase and to produce a so-called spin echo Protons start to dephase again x 900 excitation RF pulse 1800 refocusing RF pulse Spin Echo: signal/emitted energy can be detected by receiver coil Time • In a spin echo sequence, a 180 o refocusing pulse is applied at a timepoint TE/2 to rephase the protons spins. At a timepoint TE (echo time), the protons realign, and a so called spin echo can be recorded for image production. TE is the time between the application of the 90 o excitation pulse and the peak of the spin echo.
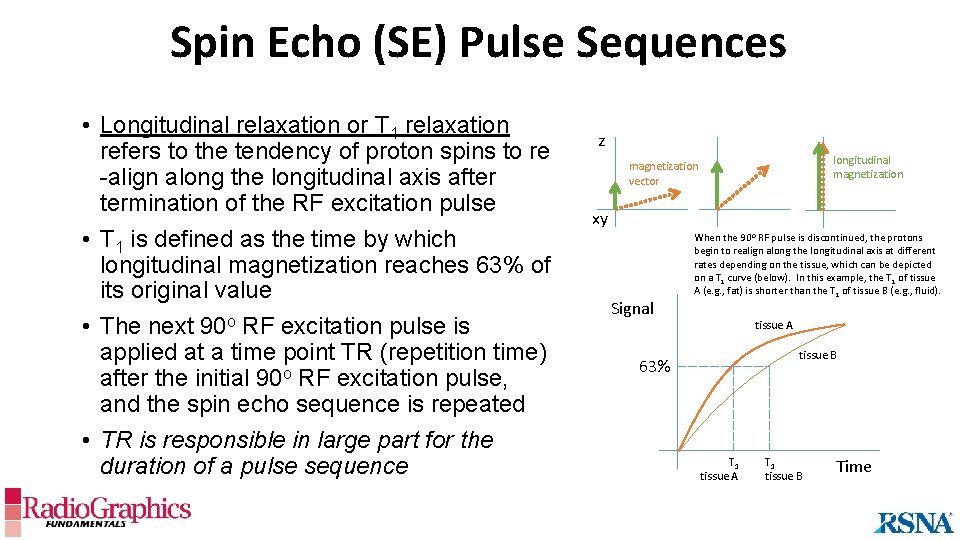
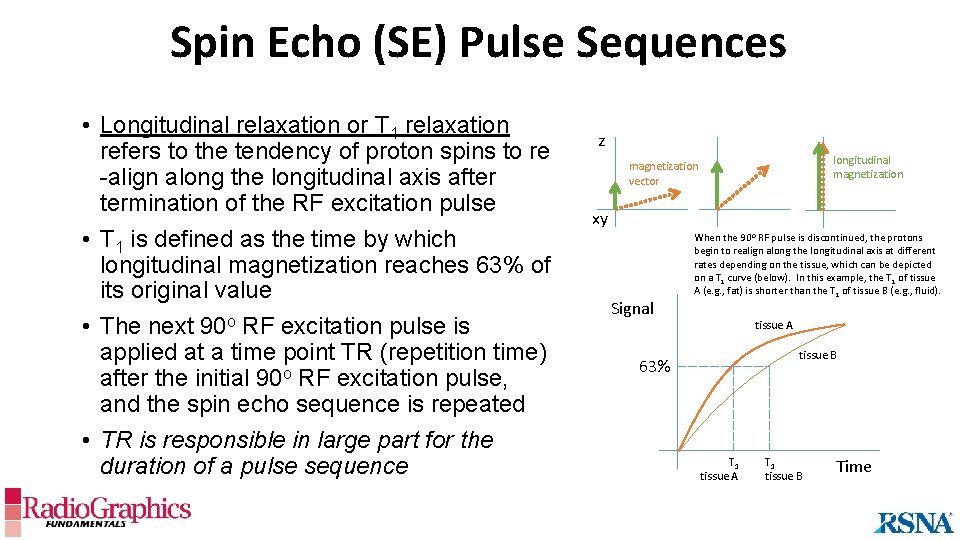
Spin Echo (SE) Pulse Sequences • Longitudinal relaxation or T 1 relaxation refers to the tendency of proton spins to re -align along the longitudinal axis after termination of the RF excitation pulse • T 1 is defined as the time by which longitudinal magnetization reaches 63% of its original value • The next 90 o RF excitation pulse is applied at a time point TR (repetition time) after the initial 90 o RF excitation pulse, and the spin echo sequence is repeated • TR is responsible in large part for the duration of a pulse sequence z longitudinal magnetization vector xy Signal When the 90 o RF pulse is discontinued, the protons begin to realign along the longitudinal axis at different rates depending on the tissue, which can be depicted on a T 1 curve (below). In this example, the T 1 of tissue A (e. g. , fat) is shorter than the T 1 of tissue B (e. g. , fluid). tissue A tissue B 63% T 1 tissue A T 1 tissue B Time
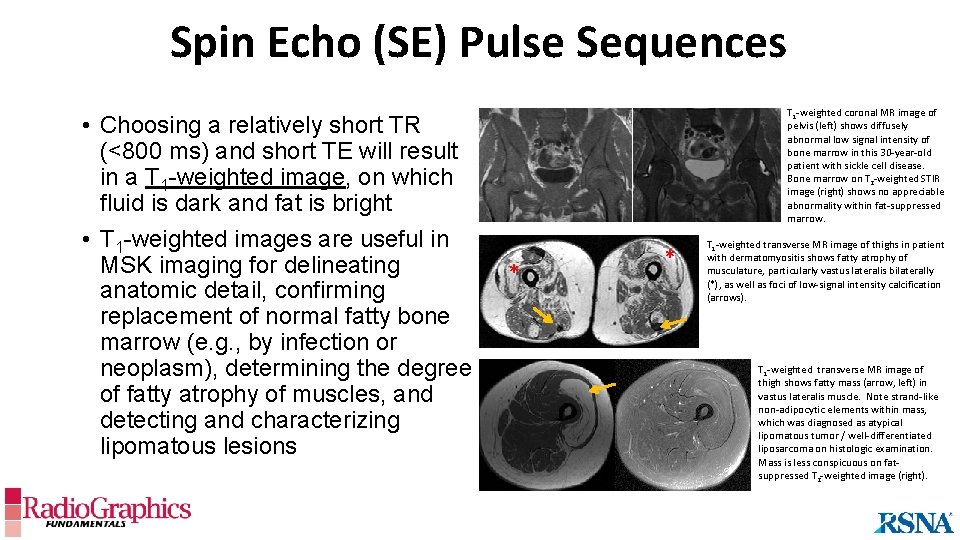
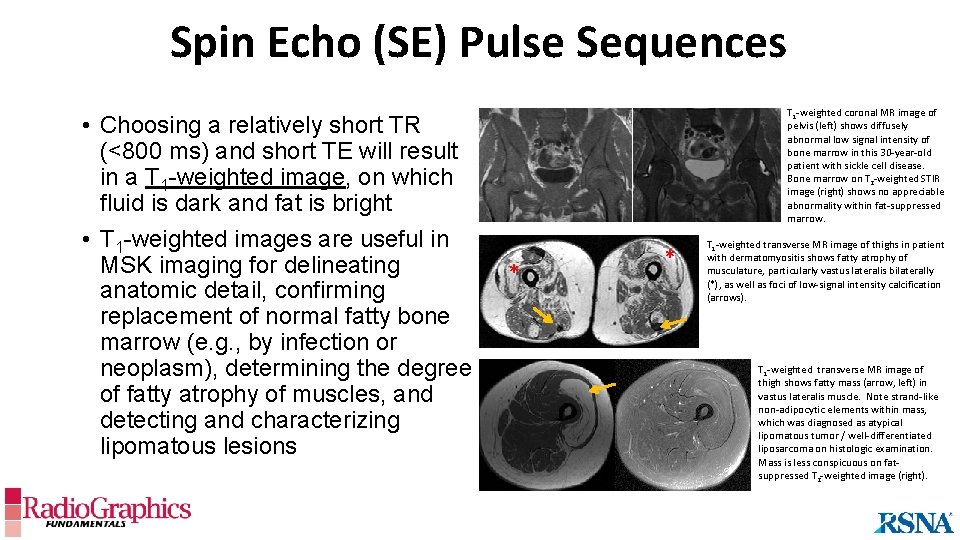
Spin Echo (SE) Pulse Sequences • Choosing a relatively short TR (<800 ms) and short TE will result in a T 1 -weighted image, on which fluid is dark and fat is bright • T 1 -weighted images are useful in MSK imaging for delineating anatomic detail, confirming replacement of normal fatty bone marrow (e. g. , by infection or neoplasm), determining the degree of fatty atrophy of muscles, and detecting and characterizing lipomatous lesions T 1 -weighted coronal MR image of pelvis (left) shows diffusely abnormal low signal intensity of bone marrow in this 30 -year-old patient with sickle cell disease. Bone marrow on T 2 -weighted STIR image (right) shows no appreciable abnormality within fat-suppressed marrow. * * T 1 -weighted transverse MR image of thighs in patient with dermatomyositis shows fatty atrophy of musculature, particularly vastus lateralis bilaterally (*), as well as foci of low-signal intensity calcification (arrows). T 1 -weighted transverse MR image of thigh shows fatty mass (arrow, left) in vastus lateralis muscle. Note strand-like non-adipocytic elements within mass, which was diagnosed as atypical lipomatous tumor / well-differentiated liposarcoma on histologic examination. Mass is less conspicuous on fatsuppressed T 2 -weighted image (right).
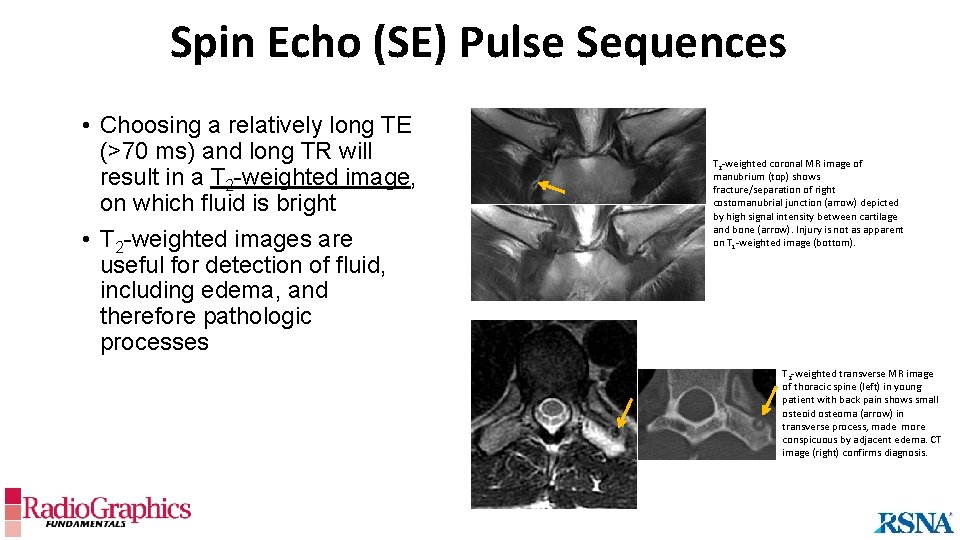
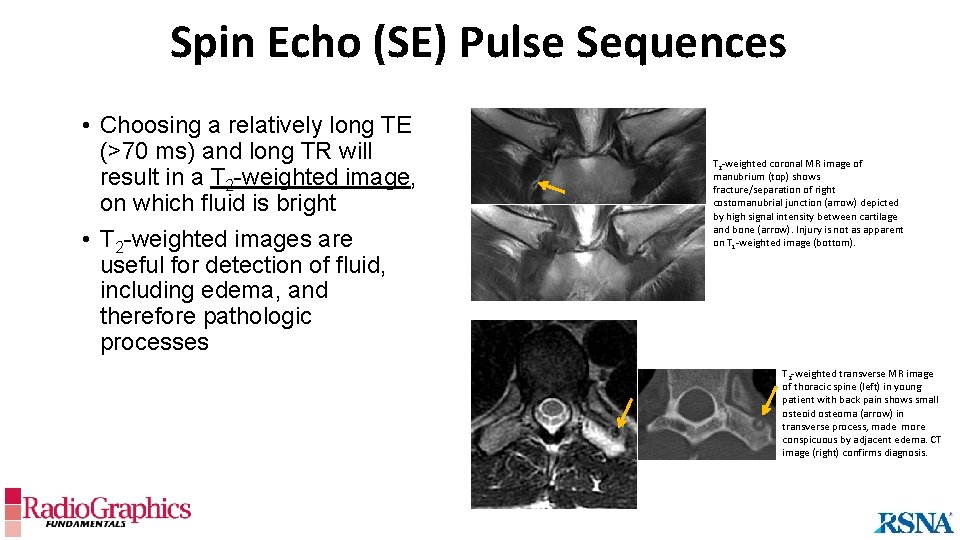
Spin Echo (SE) Pulse Sequences • Choosing a relatively long TE (>70 ms) and long TR will result in a T 2 -weighted image, on which fluid is bright • T 2 -weighted images are useful for detection of fluid, including edema, and therefore pathologic processes T 2 -weighted coronal MR image of manubrium (top) shows fracture/separation of right costomanubrial junction (arrow) depicted by high signal intensity between cartilage and bone (arrow). Injury is not as apparent on T 1 -weighted image (bottom). T 2 -weighted transverse MR image of thoracic spine (left) in young patient with back pain shows small osteoid osteoma (arrow) in transverse process, made more conspicuous by adjacent edema. CT image (right) confirms diagnosis.
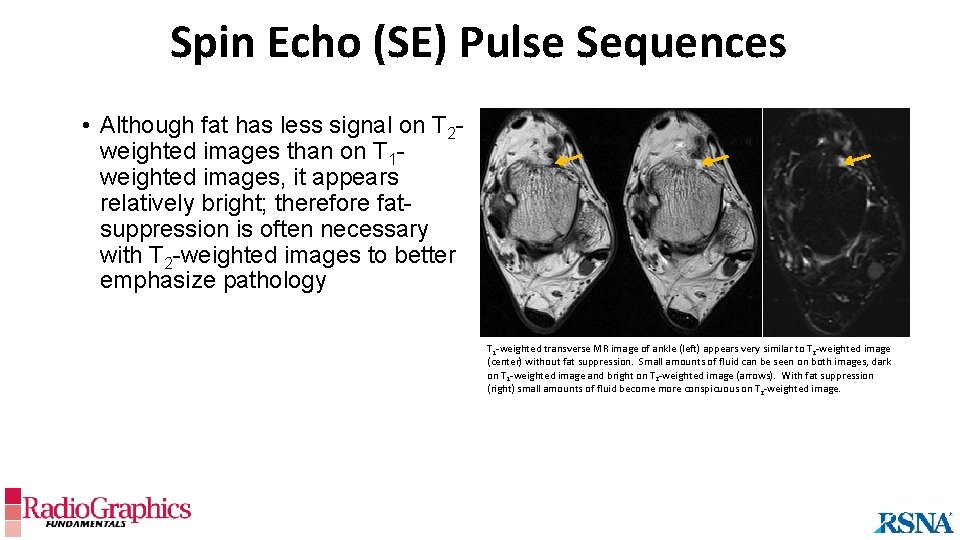
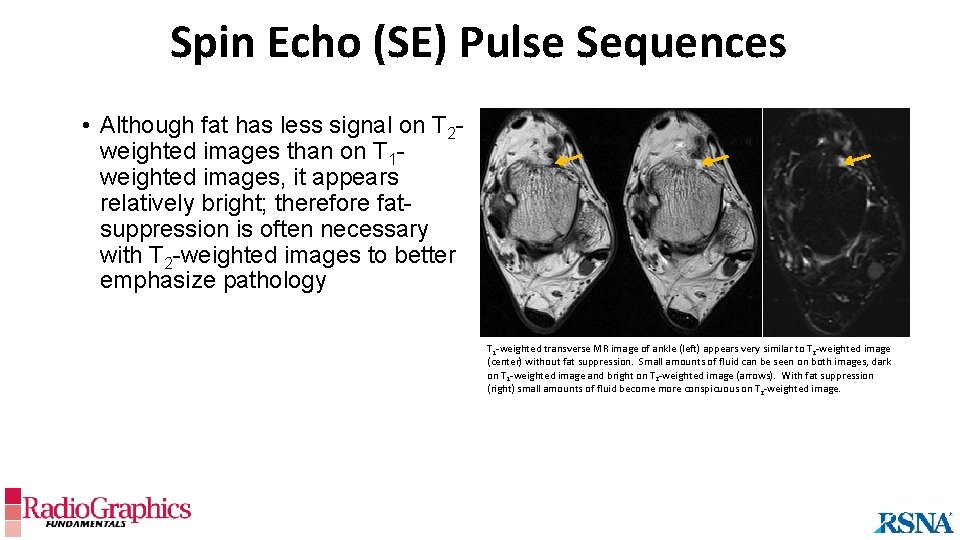
Spin Echo (SE) Pulse Sequences • Although fat has less signal on T 2 weighted images than on T 1 weighted images, it appears relatively bright; therefore fatsuppression is often necessary with T 2 -weighted images to better emphasize pathology T 1 -weighted transverse MR image of ankle (left) appears very similar to T 2 -weighted image (center) without fat suppression. Small amounts of fluid can be seen on both images, dark on T 1 -weighted image and bright on T 2 -weighted image (arrows). With fat suppression (right) small amounts of fluid become more conspicuous on T 2 -weighted image.
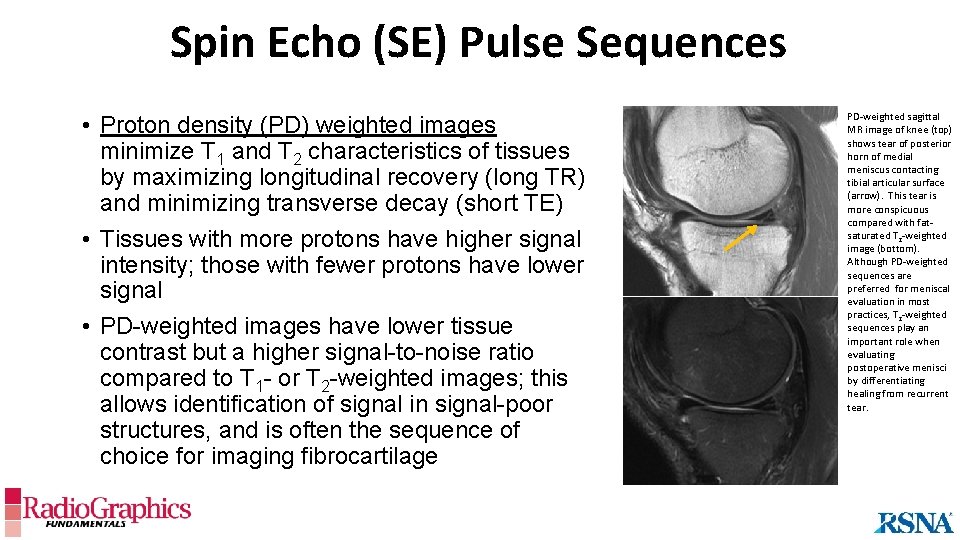
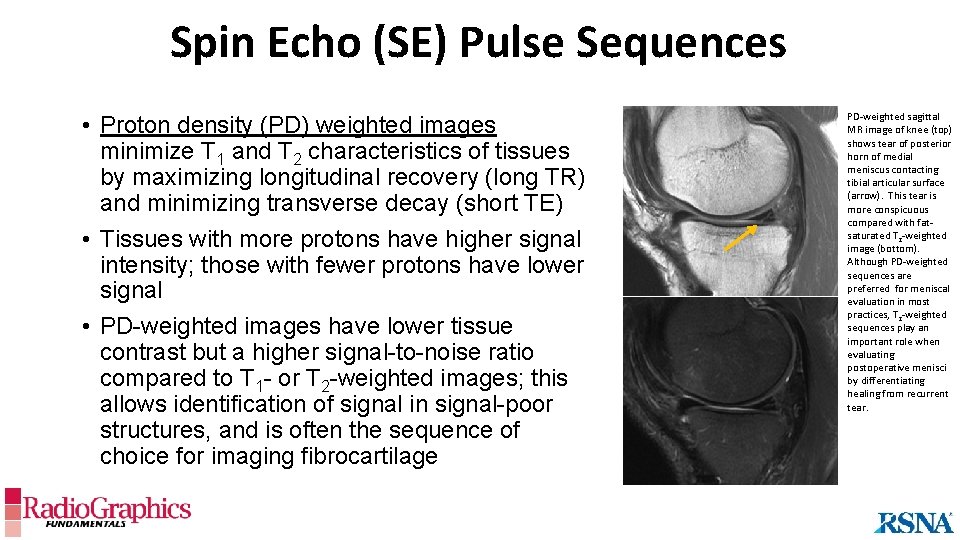
Spin Echo (SE) Pulse Sequences • Proton density (PD) weighted images minimize T 1 and T 2 characteristics of tissues by maximizing longitudinal recovery (long TR) and minimizing transverse decay (short TE) • Tissues with more protons have higher signal intensity; those with fewer protons have lower signal • PD-weighted images have lower tissue contrast but a higher signal-to-noise ratio compared to T 1 - or T 2 -weighted images; this allows identification of signal in signal-poor structures, and is often the sequence of choice for imaging fibrocartilage PD-weighted sagittal MR image of knee (top) shows tear of posterior horn of medial meniscus contacting tibial articular surface (arrow). This tear is more conspicuous compared with fatsaturated T 2 -weighted image (bottom). Although PD-weighted sequences are preferred for meniscal evaluation in most practices, T 2 -weighted sequences play an important role when evaluating postoperative menisci by differentiating healing from recurrent tear.
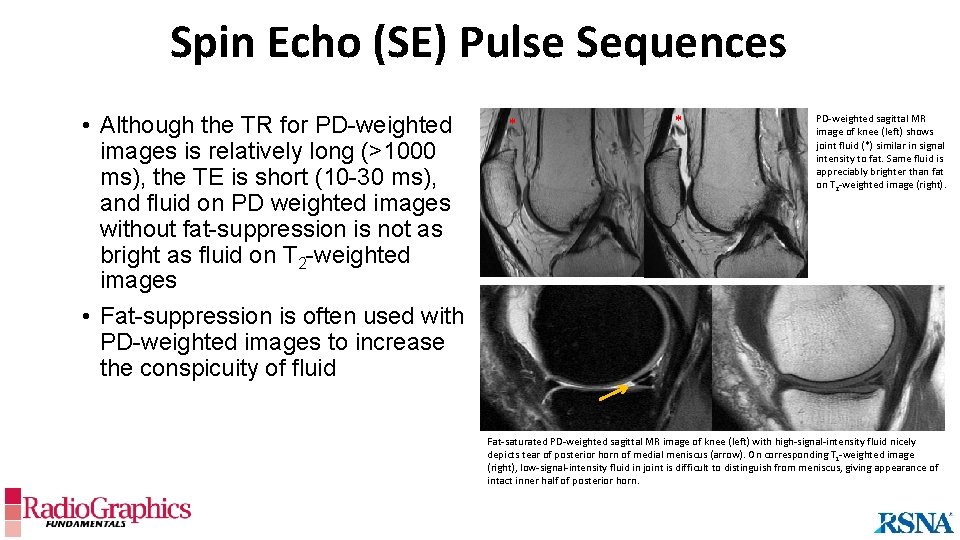
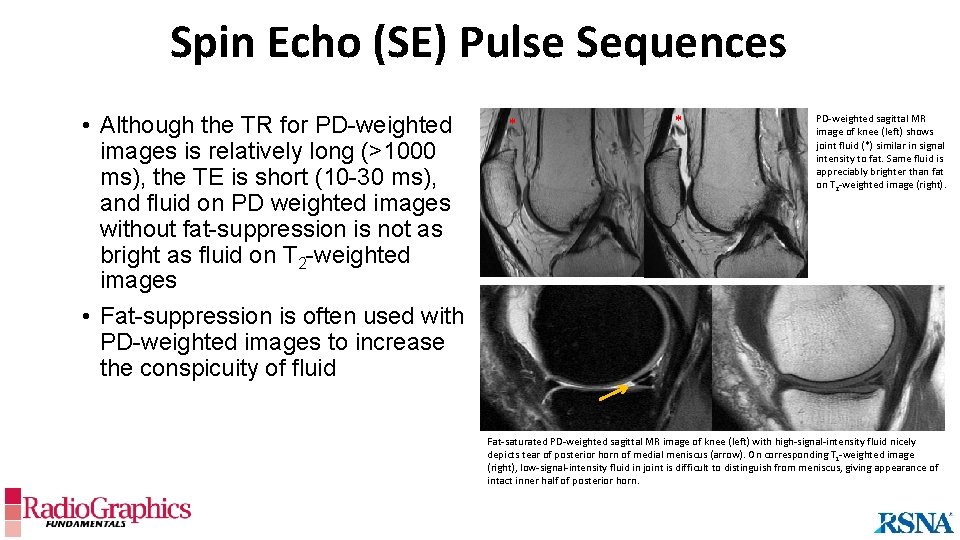
Spin Echo (SE) Pulse Sequences • Although the TR for PD-weighted images is relatively long (>1000 ms), the TE is short (10 -30 ms), and fluid on PD weighted images without fat-suppression is not as bright as fluid on T 2 -weighted images • Fat-suppression is often used with PD-weighted images to increase the conspicuity of fluid * * PD-weighted sagittal MR image of knee (left) shows joint fluid (*) similar in signal intensity to fat. Same fluid is appreciably brighter than fat on T 2 -weighted image (right). Fat-saturated PD-weighted sagittal MR image of knee (left) with high-signal-intensity fluid nicely depicts tear of posterior horn of medial meniscus (arrow). On corresponding T 1 -weighted image (right), low-signal-intensity fluid in joint is difficult to distinguish from meniscus, giving appearance of intact inner half of posterior horn.
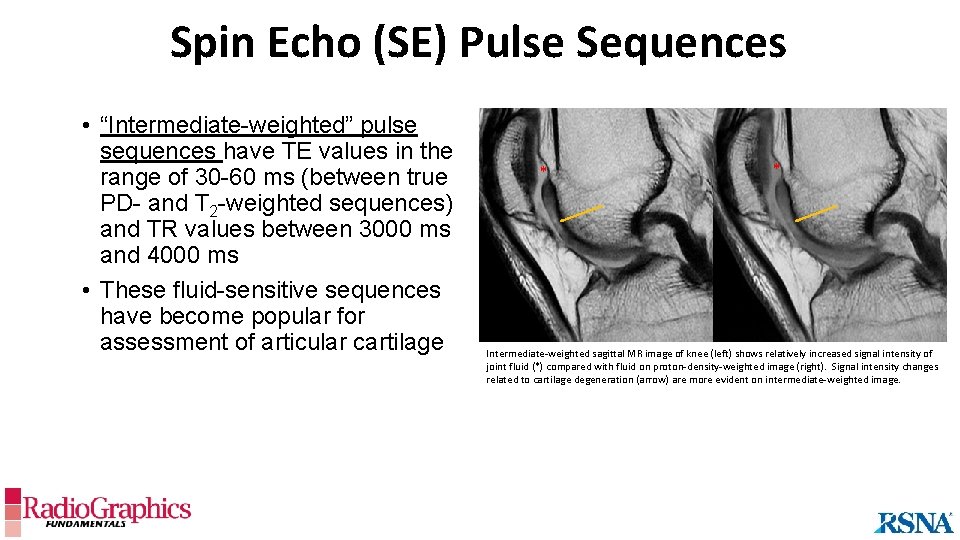
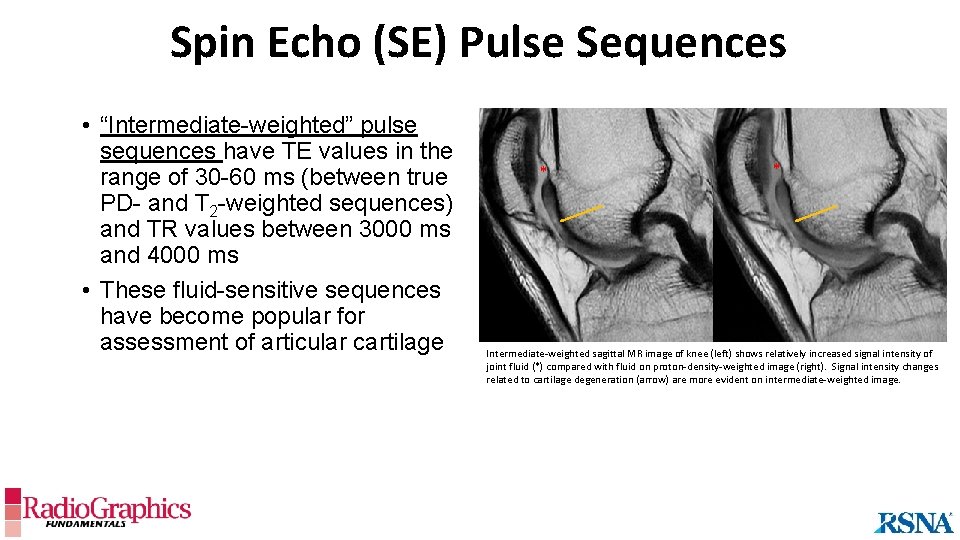
Spin Echo (SE) Pulse Sequences • “Intermediate-weighted” pulse sequences have TE values in the range of 30 -60 ms (between true PD- and T 2 -weighted sequences) and TR values between 3000 ms and 4000 ms • These fluid-sensitive sequences have become popular for assessment of articular cartilage * * Intermediate-weighted sagittal MR image of knee (left) shows relatively increased signal intensity of joint fluid (*) compared with fluid on proton-density-weighted image (right). Signal intensity changes related to cartilage degeneration (arrow) are more evident on intermediate-weighted image.
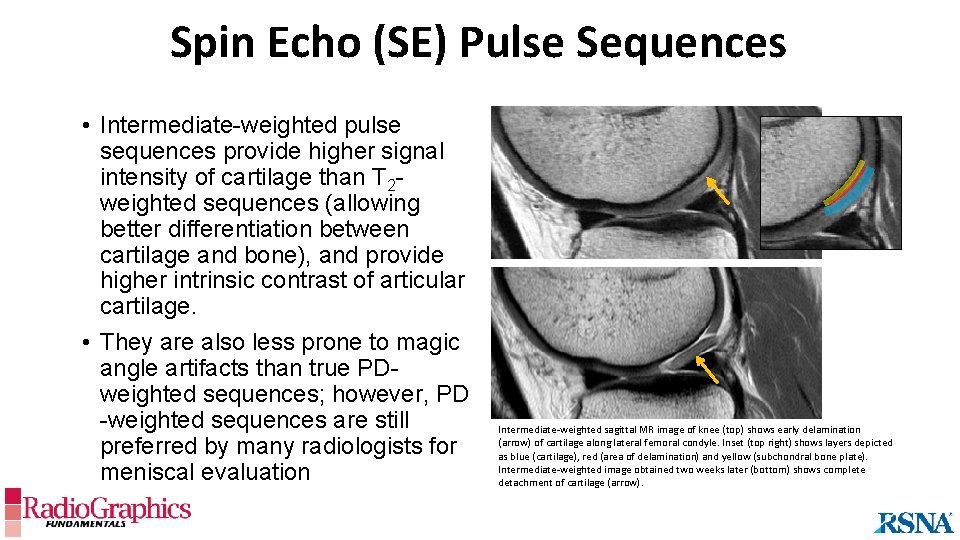
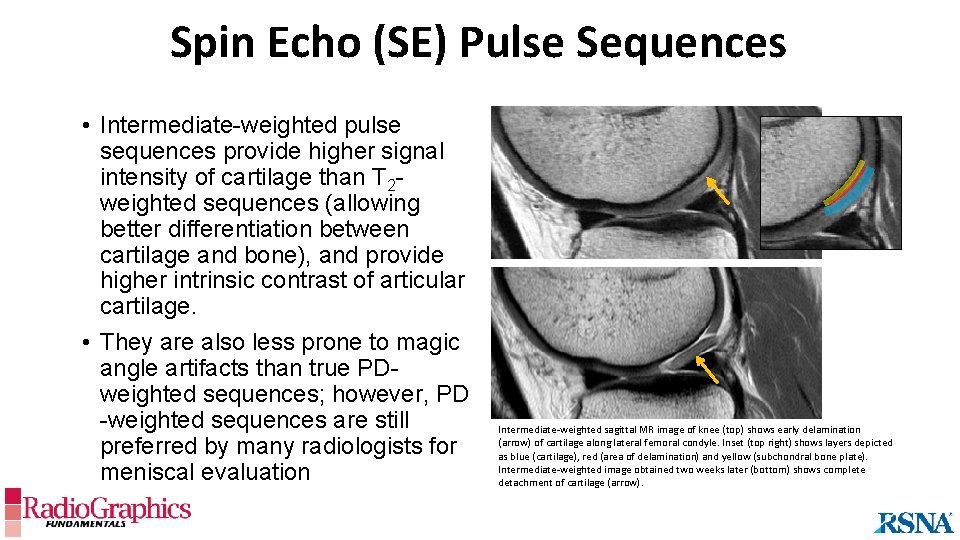
Spin Echo (SE) Pulse Sequences • Intermediate-weighted pulse sequences provide higher signal intensity of cartilage than T 2 weighted sequences (allowing better differentiation between cartilage and bone), and provide higher intrinsic contrast of articular cartilage. • They are also less prone to magic angle artifacts than true PDweighted sequences; however, PD -weighted sequences are still preferred by many radiologists for meniscal evaluation Intermediate-weighted sagittal MR image of knee (top) shows early delamination (arrow) of cartilage along lateral femoral condyle. Inset (top right) shows layers depicted as blue (cartilage), red (area of delamination) and yellow (subchondral bone plate). Intermediate-weighted image obtained two weeks later (bottom) shows complete detachment of cartilage (arrow).
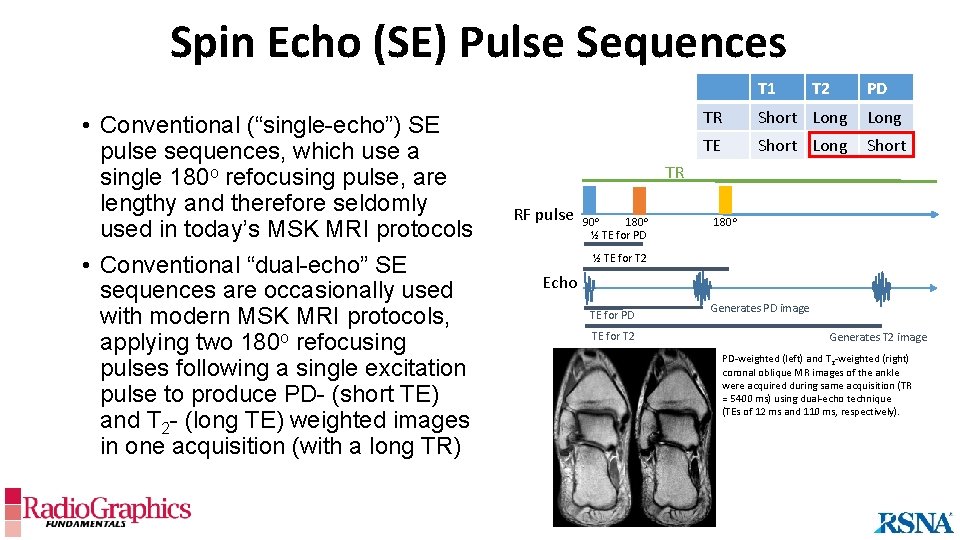
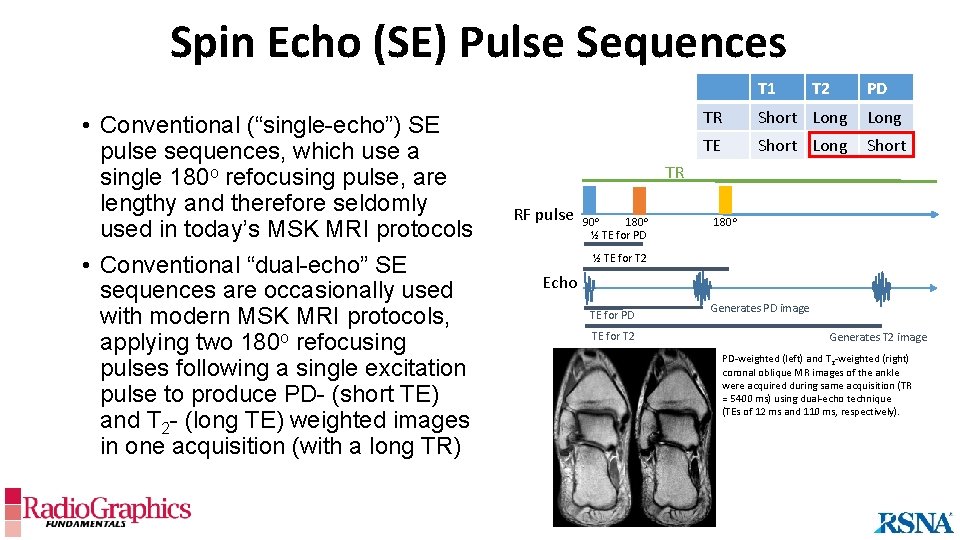
Spin Echo (SE) Pulse Sequences T 1 • Conventional (“single-echo”) SE pulse sequences, which use a single 180 o refocusing pulse, are lengthy and therefore seldomly used in today’s MSK MRI protocols • Conventional “dual-echo” SE sequences are occasionally used with modern MSK MRI protocols, applying two 180 o refocusing pulses following a single excitation pulse to produce PD- (short TE) and T 2 - (long TE) weighted images in one acquisition (with a long TR) T 2 PD TR Short Long TE Short Long Short TR RF pulse 90 o 180 o ½ TE for PD 180 o ½ TE for T 2 Echo TE for PD TE for T 2 Generates PD image Generates T 2 image PD-weighted (left) and T 2 -weighted (right) coronal oblique MR images of the ankle were acquired during same acquisition (TR = 5400 ms) using dual-echo technique (TEs of 12 ms and 110 ms, respectively).
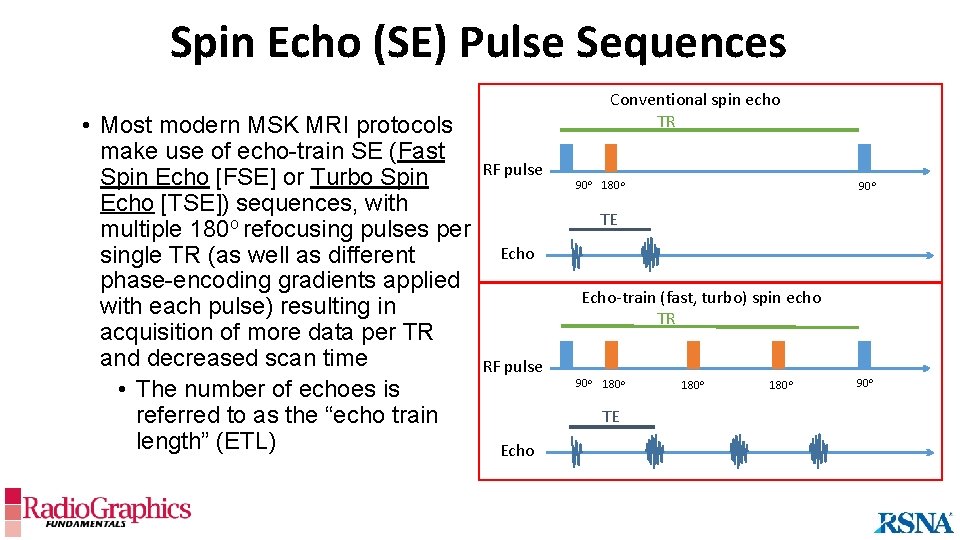
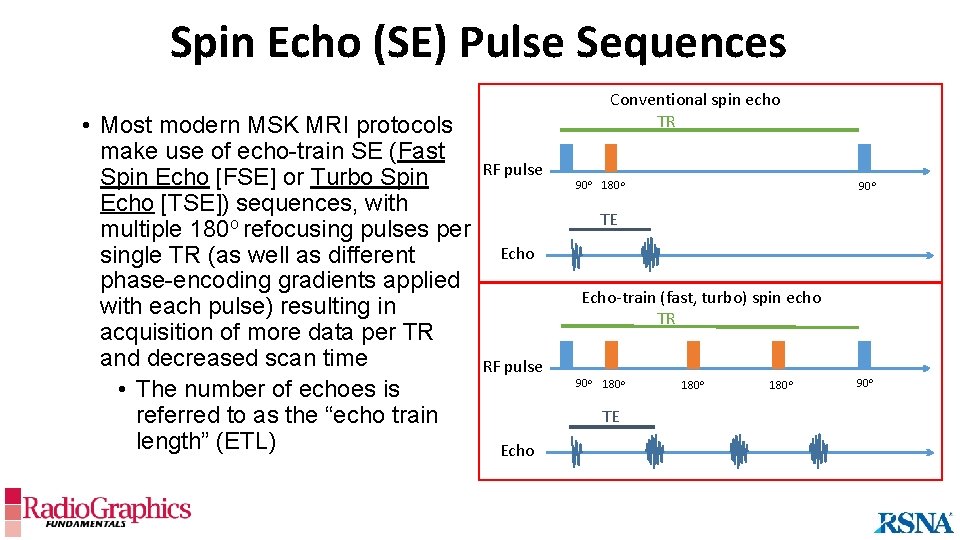
Spin Echo (SE) Pulse Sequences • Most modern MSK MRI protocols make use of echo-train SE (Fast Spin Echo [FSE] or Turbo Spin Echo [TSE]) sequences, with multiple 180 o refocusing pulses per single TR (as well as different phase-encoding gradients applied with each pulse) resulting in acquisition of more data per TR and decreased scan time • The number of echoes is referred to as the “echo train length” (ETL) Conventional spin echo TR RF pulse 90 o 180 o 90 o TE Echo-train (fast, turbo) spin echo TR RF pulse 90 o 180 o TE Echo 180 o 90 o
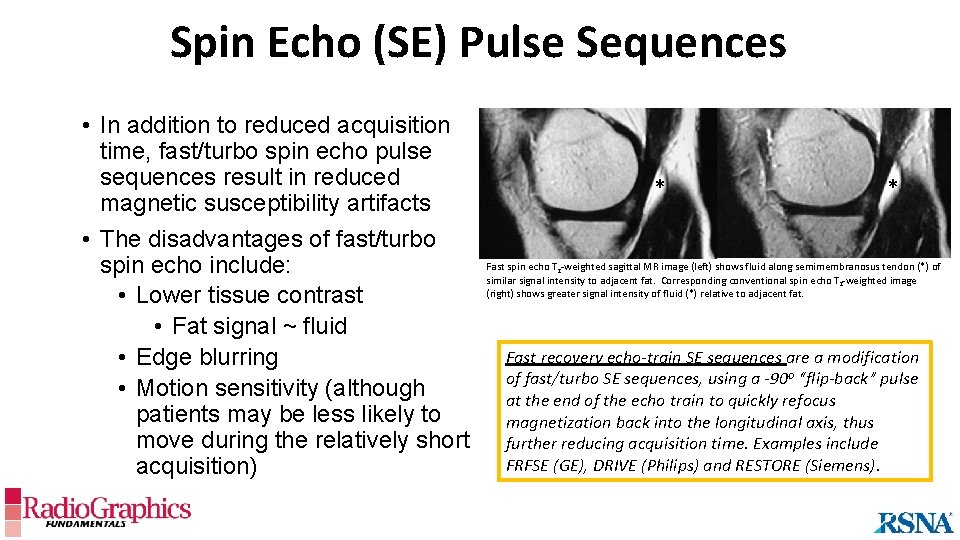
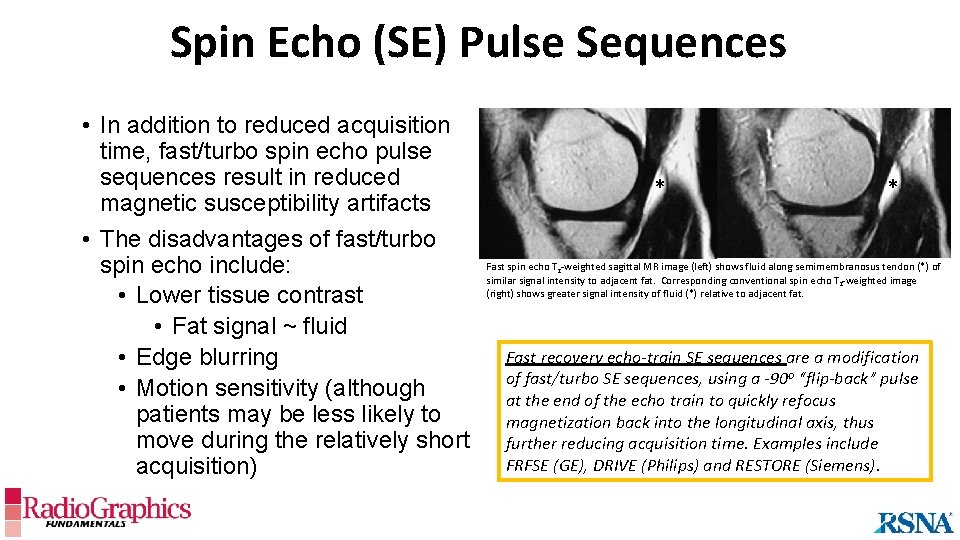
Spin Echo (SE) Pulse Sequences • In addition to reduced acquisition time, fast/turbo spin echo pulse sequences result in reduced magnetic susceptibility artifacts • The disadvantages of fast/turbo spin echo include: • Lower tissue contrast • Fat signal ~ fluid • Edge blurring • Motion sensitivity (although patients may be less likely to move during the relatively short acquisition) * * Fast spin echo T 2 -weighted sagittal MR image (left) shows fluid along semimembranosus tendon (*) of similar signal intensity to adjacent fat. Corresponding conventional spin echo T 2 -weighted image (right) shows greater signal intensity of fluid (*) relative to adjacent fat. Fast recovery echo-train SE sequences are a modification of fast/turbo SE sequences, using a -90 o “flip-back” pulse at the end of the echo train to quickly refocus magnetization back into the longitudinal axis, thus further reducing acquisition time. Examples include FRFSE (GE), DRIVE (Philips) and RESTORE (Siemens).
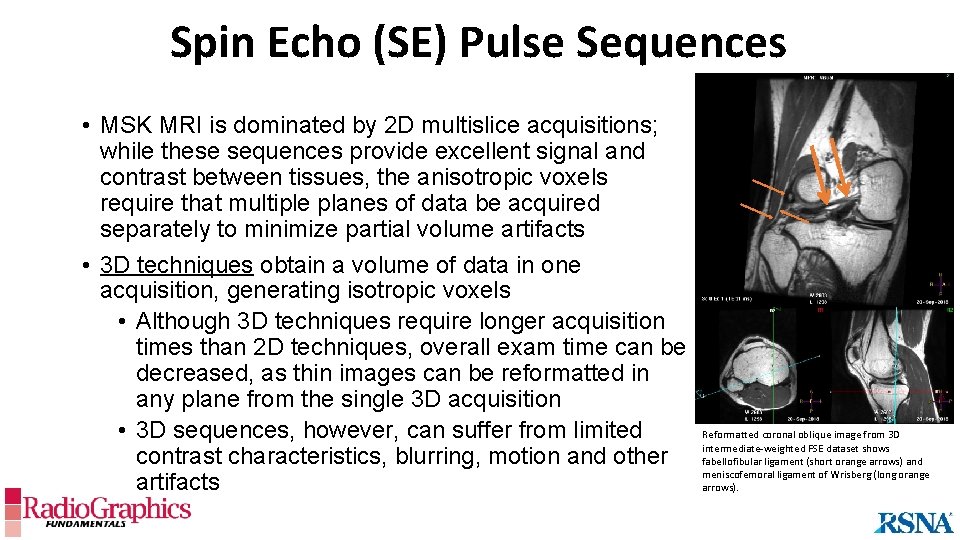
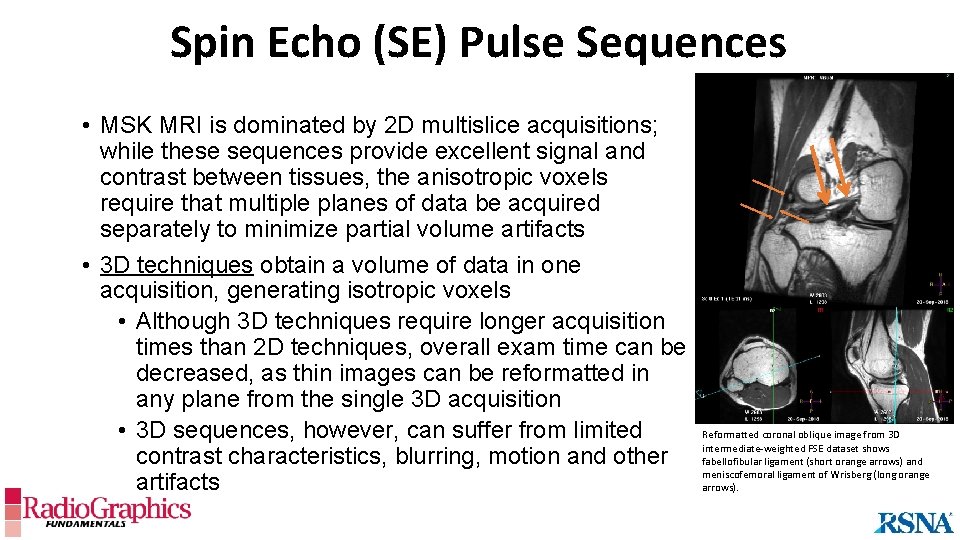
Spin Echo (SE) Pulse Sequences • MSK MRI is dominated by 2 D multislice acquisitions; while these sequences provide excellent signal and contrast between tissues, the anisotropic voxels require that multiple planes of data be acquired separately to minimize partial volume artifacts • 3 D techniques obtain a volume of data in one acquisition, generating isotropic voxels • Although 3 D techniques require longer acquisition times than 2 D techniques, overall exam time can be decreased, as thin images can be reformatted in any plane from the single 3 D acquisition • 3 D sequences, however, can suffer from limited contrast characteristics, blurring, motion and other artifacts Reformatted coronal oblique image from 3 D intermediate-weighted FSE dataset shows fabellofibular ligament (short orange arrows) and meniscofemoral ligament of Wrisberg (long orange arrows).
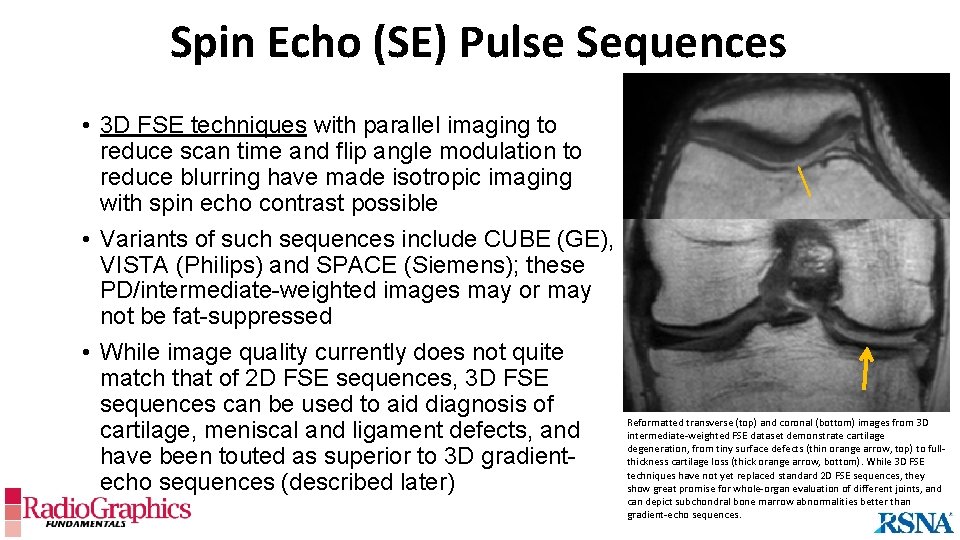
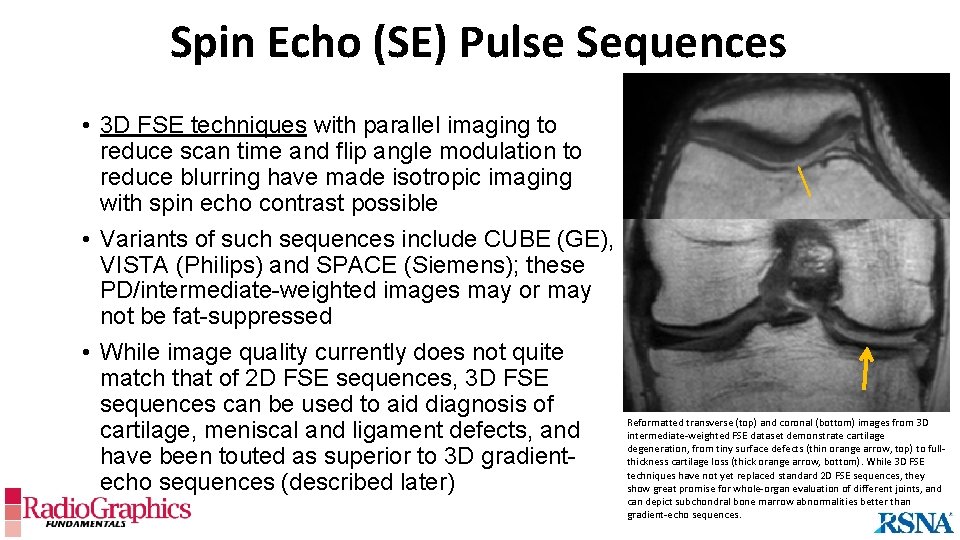
Spin Echo (SE) Pulse Sequences • 3 D FSE techniques with parallel imaging to reduce scan time and flip angle modulation to reduce blurring have made isotropic imaging with spin echo contrast possible • Variants of such sequences include CUBE (GE), VISTA (Philips) and SPACE (Siemens); these PD/intermediate-weighted images may or may not be fat-suppressed • While image quality currently does not quite match that of 2 D FSE sequences, 3 D FSE sequences can be used to aid diagnosis of cartilage, meniscal and ligament defects, and have been touted as superior to 3 D gradientecho sequences (described later) Reformatted transverse (top) and coronal (bottom) images from 3 D intermediate-weighted FSE dataset demonstrate cartilage degeneration, from tiny surface defects (thin orange arrow, top) to fullthickness cartilage loss (thick orange arrow, bottom). While 3 D FSE techniques have not yet replaced standard 2 D FSE sequences, they show great promise for whole-organ evaluation of different joints, and can depict subchondral bone marrow abnormalities better than gradient-echo sequences.
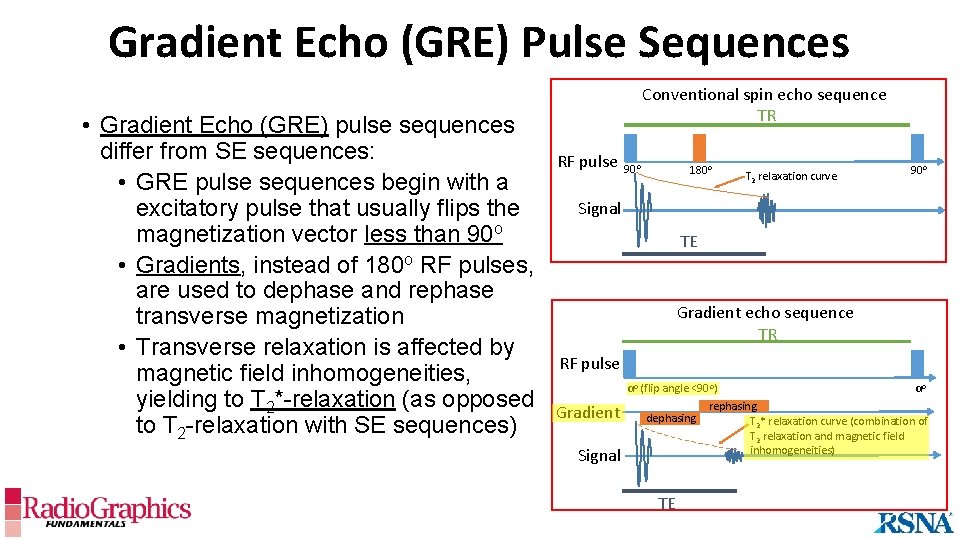
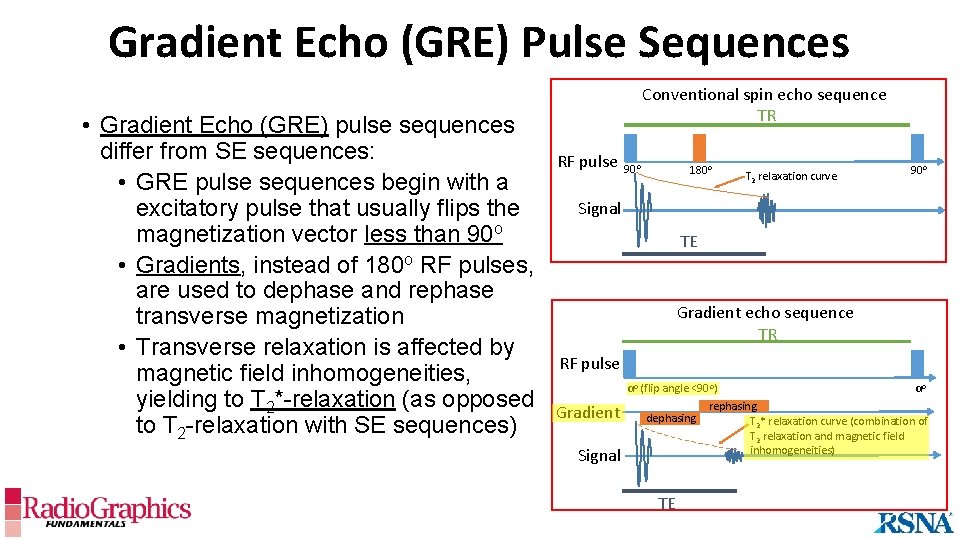
Gradient Echo (GRE) Pulse Sequences • Gradient Echo (GRE) pulse sequences differ from SE sequences: • GRE pulse sequences begin with a excitatory pulse that usually flips the magnetization vector less than 90 o • Gradients, instead of 180 o RF pulses, are used to dephase and rephase transverse magnetization • Transverse relaxation is affected by magnetic field inhomogeneities, yielding to T 2*-relaxation (as opposed to T 2 -relaxation with SE sequences) Conventional spin echo sequence TR RF pulse 90 o 180 o T 2 relaxation curve 90 o Signal TE Gradient echo sequence TR RF pulse Gradient Signal αo αo (flip angle <90 o) rephasing dephasing T 2* relaxation curve (combination of T 2 relaxation and magnetic field inhomogeneities) TE
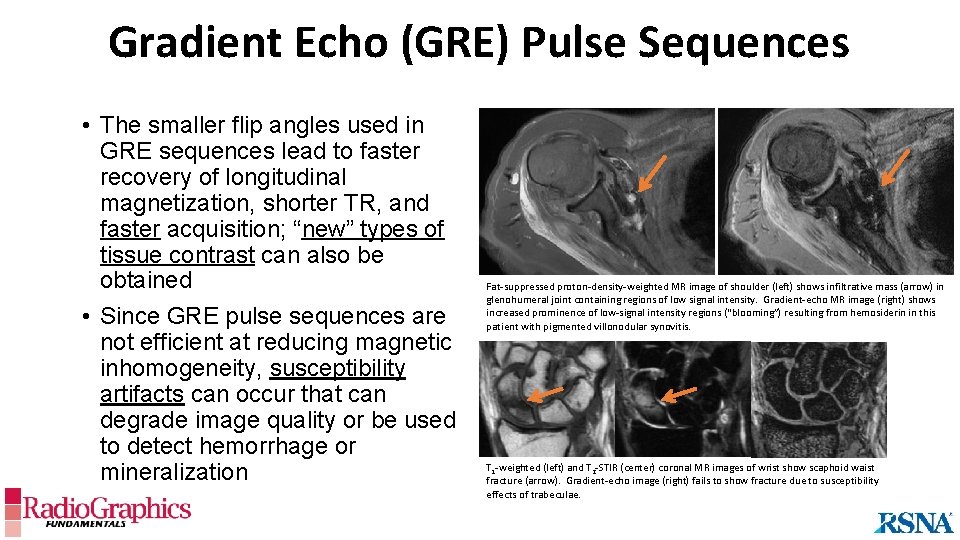
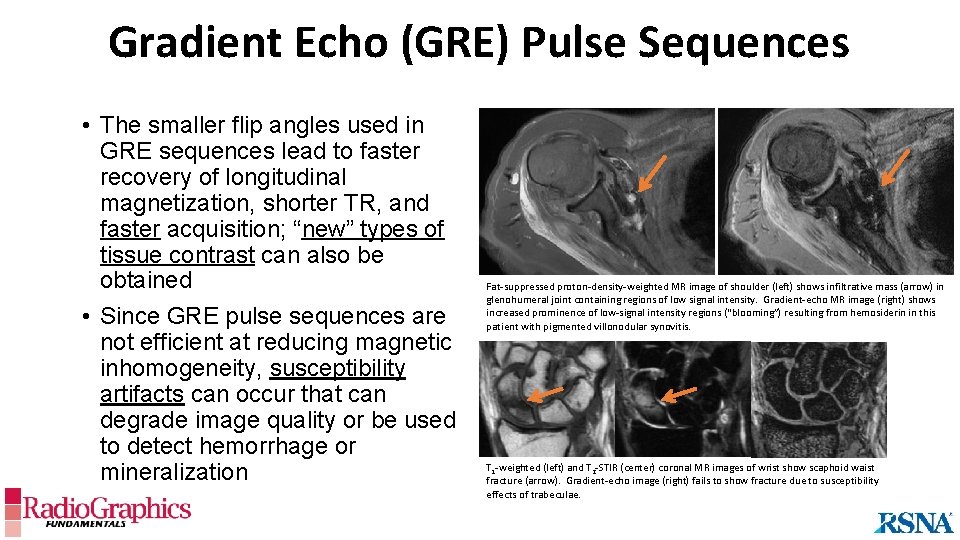
Gradient Echo (GRE) Pulse Sequences • The smaller flip angles used in GRE sequences lead to faster recovery of longitudinal magnetization, shorter TR, and faster acquisition; “new” types of tissue contrast can also be obtained • Since GRE pulse sequences are not efficient at reducing magnetic inhomogeneity, susceptibility artifacts can occur that can degrade image quality or be used to detect hemorrhage or mineralization Fat-suppressed proton-density-weighted MR image of shoulder (left) shows infiltrative mass (arrow) in glenohumeral joint containing regions of low signal intensity. Gradient-echo MR image (right) shows increased prominence of low-signal intensity regions (“blooming”) resulting from hemosiderin in this patient with pigmented villonodular synovitis. T 1 -weighted (left) and T 2 -STIR (center) coronal MR images of wrist show scaphoid waist fracture (arrow). Gradient-echo image (right) fails to show fracture due to susceptibility effects of trabeculae.
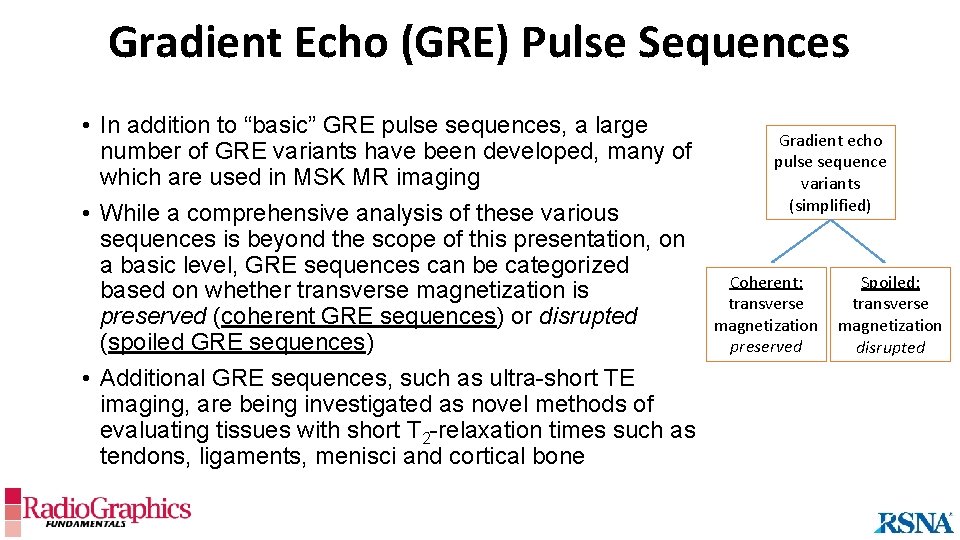
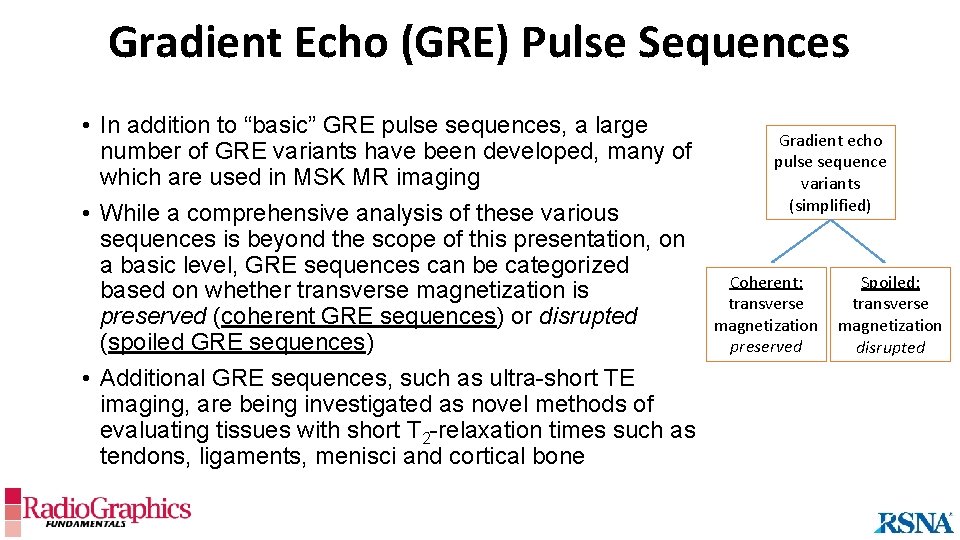
Gradient Echo (GRE) Pulse Sequences • In addition to “basic” GRE pulse sequences, a large number of GRE variants have been developed, many of which are used in MSK MR imaging • While a comprehensive analysis of these various sequences is beyond the scope of this presentation, on a basic level, GRE sequences can be categorized based on whether transverse magnetization is preserved (coherent GRE sequences) or disrupted (spoiled GRE sequences) • Additional GRE sequences, such as ultra-short TE imaging, are being investigated as novel methods of evaluating tissues with short T 2 -relaxation times such as tendons, ligaments, menisci and cortical bone Gradient echo pulse sequence variants (simplified) Coherent: transverse magnetization preserved Spoiled: transverse magnetization disrupted
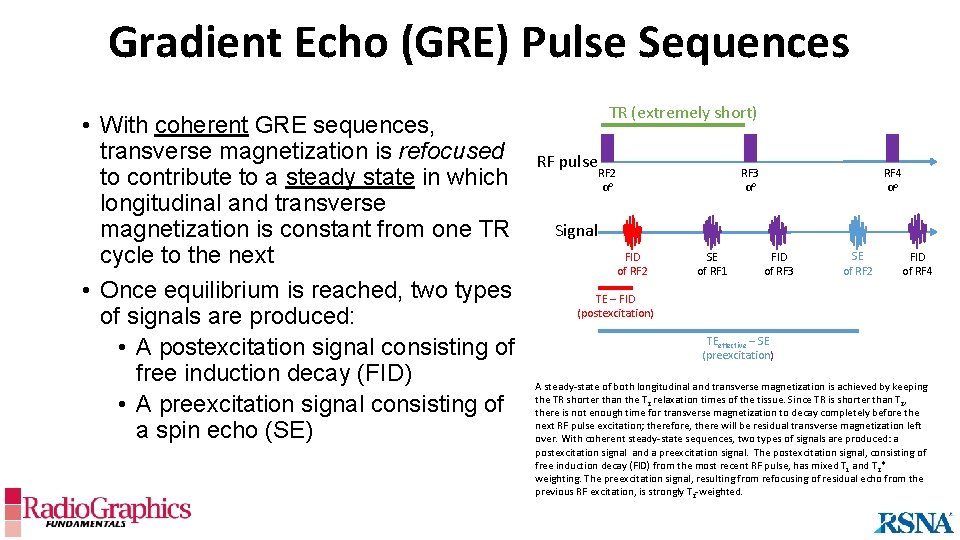
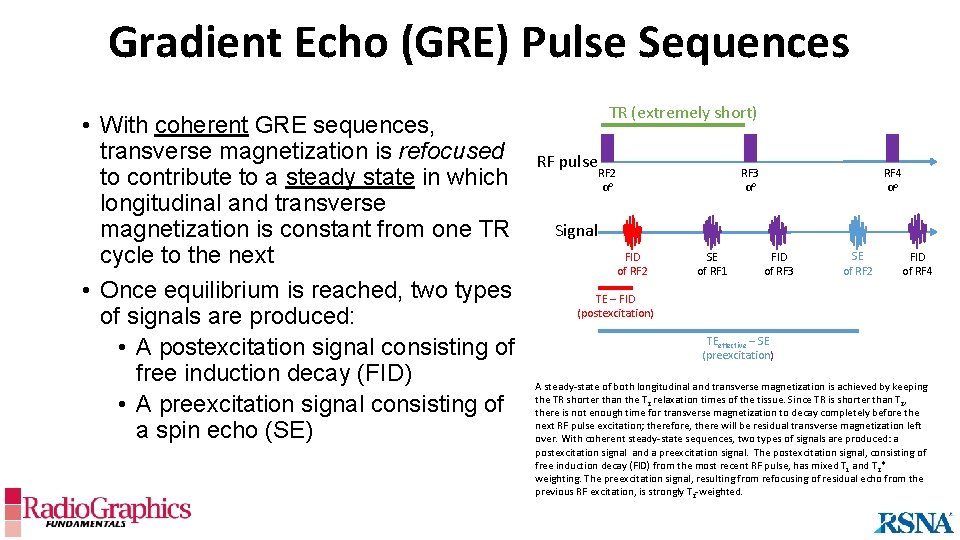
Gradient Echo (GRE) Pulse Sequences • With coherent GRE sequences, transverse magnetization is refocused to contribute to a steady state in which longitudinal and transverse magnetization is constant from one TR cycle to the next • Once equilibrium is reached, two types of signals are produced: • A postexcitation signal consisting of free induction decay (FID) • A preexcitation signal consisting of a spin echo (SE) TR (extremely short) RF pulse RF 3 αo RF 2 αo RF 4 αo Signal FID of RF 2 SE of RF 1 FID of RF 3 SE of RF 2 FID of RF 4 TE – FID (postexcitation) TEeffective – SE (preexcitation) A steady-state of both longitudinal and transverse magnetization is achieved by keeping the TR shorter than the T 2 relaxation times of the tissue. Since TR is shorter than T 2, there is not enough time for transverse magnetization to decay completely before the next RF pulse excitation; therefore, there will be residual transverse magnetization left over. With coherent steady-state sequences, two types of signals are produced: a postexcitation signal and a preexcitation signal. The postexcitation signal, consisting of free induction decay (FID) from the most recent RF pulse, has mixed T 1 and T 2* weighting. The preexcitation signal, resulting from refocusing of residual echo from the previous RF excitation, is strongly T 2 -weighted.
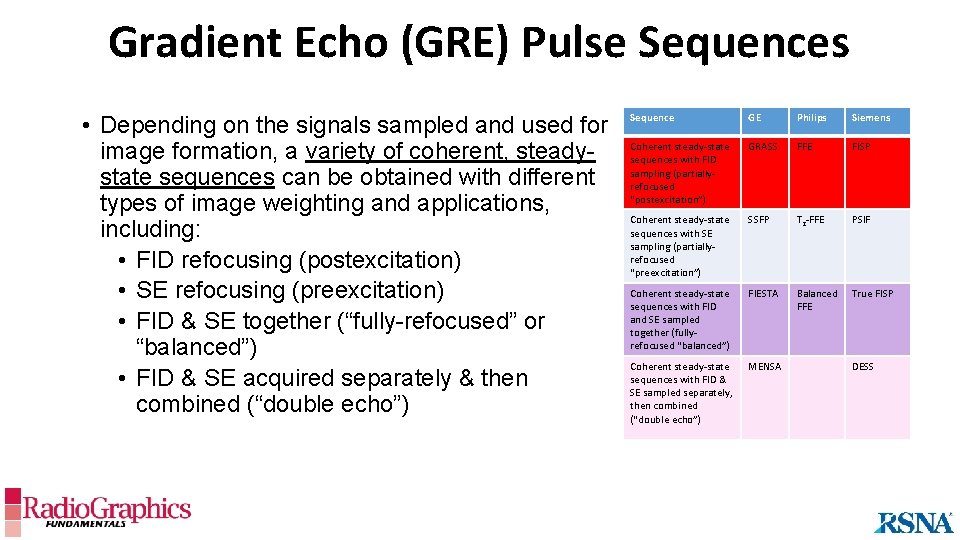
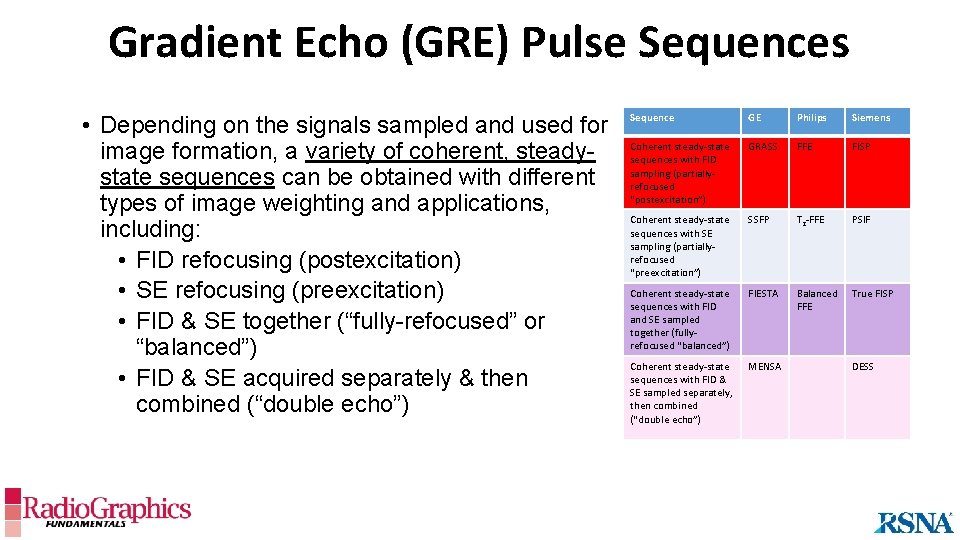
Gradient Echo (GRE) Pulse Sequences • Depending on the signals sampled and used for image formation, a variety of coherent, steadystate sequences can be obtained with different types of image weighting and applications, including: • FID refocusing (postexcitation) • SE refocusing (preexcitation) • FID & SE together (“fully-refocused” or “balanced”) • FID & SE acquired separately & then combined (“double echo”) Sequence GE Philips Siemens Coherent steady-state sequences with FID sampling (partiallyrefocused “postexcitation”) GRASS FFE FISP Coherent steady-state sequences with SE sampling (partiallyrefocused “preexcitation”) SSFP T 2 -FFE PSIF Coherent steady-state sequences with FID and SE sampled together (fullyrefocused “balanced”) FIESTA Balanced FFE True FISP Coherent steady-state sequences with FID & SE sampled separately, then combined (“double echo”) MENSA DESS
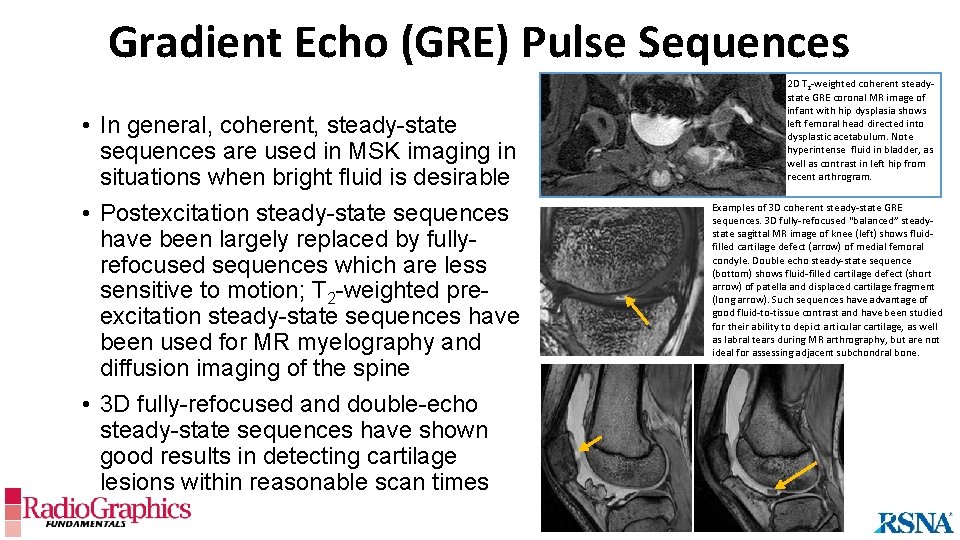
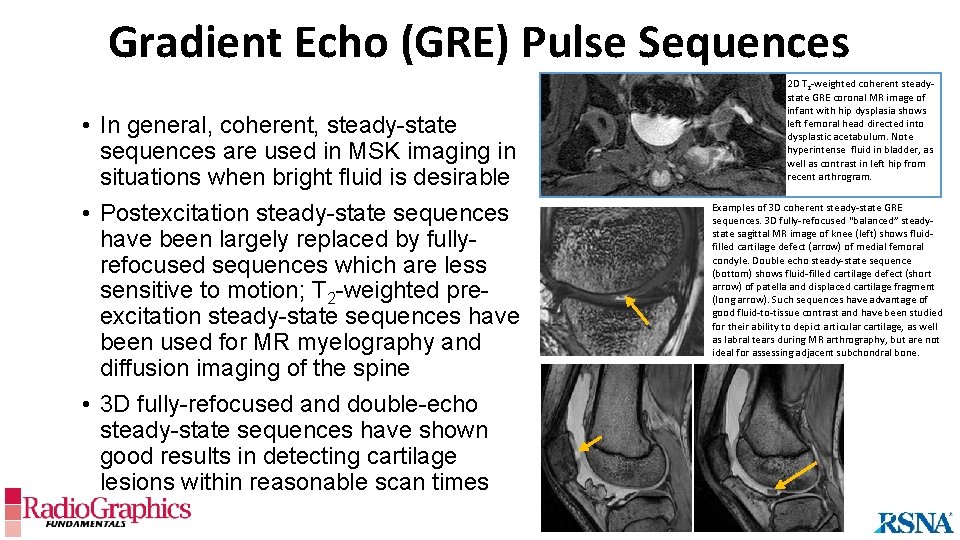
Gradient Echo (GRE) Pulse Sequences • In general, coherent, steady-state sequences are used in MSK imaging in situations when bright fluid is desirable • Postexcitation steady-state sequences have been largely replaced by fullyrefocused sequences which are less sensitive to motion; T 2 -weighted preexcitation steady-state sequences have been used for MR myelography and diffusion imaging of the spine • 3 D fully-refocused and double-echo steady-state sequences have shown good results in detecting cartilage lesions within reasonable scan times 2 D T 2 -weighted coherent steadystate GRE coronal MR image of infant with hip dysplasia shows left femoral head directed into dysplastic acetabulum. Note hyperintense fluid in bladder, as well as contrast in left hip from recent arthrogram. Examples of 3 D coherent steady-state GRE sequences. 3 D fully-refocused “balanced” steadystate sagittal MR image of knee (left) shows fluidfilled cartilage defect (arrow) of medial femoral condyle. Double echo steady-state sequence (bottom) shows fluid-filled cartilage defect (short arrow) of patella and displaced cartilage fragment (long arrow). Such sequences have advantage of good fluid-to-tissue contrast and have been studied for their ability to depict articular cartilage, as well as labral tears during MR arthrography, but are not ideal for assessing adjacent subchondral bone.
Gradient Echo (GRE) Pulse Sequences • Spoiled GRE sequences are those in which transverse magnetization is disrupted (“spoiled”) • There are different methods of “spoiling, ” and the terminology can be confusing: • The unqualified term “spoiled” usually refers to “RF-spoiling”; RF-spoiled sequences are often used to create T 1 -weighted images, and include SPGR (GE), T 1 -FFE (Philips) and FLASH (Siemens) • “Long TR spoiling” occurs when TR>>T 2*, allowing the transverse magnetization to decay to zero “naturally”; sequences that take advantage of this method include multiecho T 2*-weighted GRE • “Gradient spoiled” is a term occasionally used to refer to the previously described steady-state sequences: • Gradient-spoiled sequences (FID-refocusing): GRASS, FFE, FISP • Reversed gradient-spoiled echo (echo-refocusing): SSFP, T 2 -FFE, PSIF
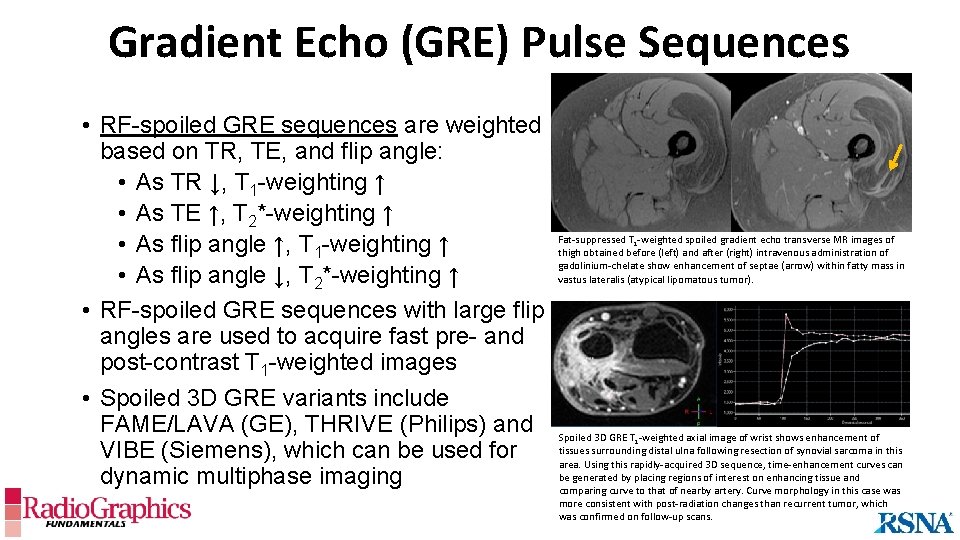
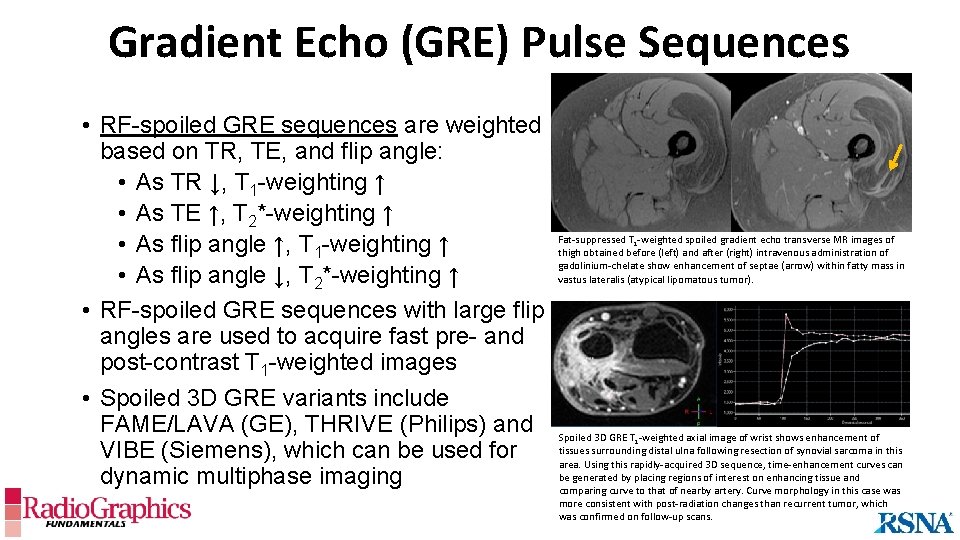
Gradient Echo (GRE) Pulse Sequences • RF-spoiled GRE sequences are weighted based on TR, TE, and flip angle: • As TR ↓, T 1 -weighting ↑ • As TE ↑, T 2*-weighting ↑ • As flip angle ↑, T 1 -weighting ↑ • As flip angle ↓, T 2*-weighting ↑ • RF-spoiled GRE sequences with large flip angles are used to acquire fast pre- and post-contrast T 1 -weighted images • Spoiled 3 D GRE variants include FAME/LAVA (GE), THRIVE (Philips) and VIBE (Siemens), which can be used for dynamic multiphase imaging Fat-suppressed T 1 -weighted spoiled gradient echo transverse MR images of thigh obtained before (left) and after (right) intravenous administration of gadolinium-chelate show enhancement of septae (arrow) within fatty mass in vastus lateralis (atypical lipomatous tumor). Spoiled 3 D GRE T 1 -weighted axial image of wrist shows enhancement of tissues surrounding distal ulna following resection of synovial sarcoma in this area. Using this rapidly-acquired 3 D sequence, time-enhancement curves can be generated by placing regions of interest on enhancing tissue and comparing curve to that of nearby artery. Curve morphology in this case was more consistent with post-radiation changes than recurrent tumor, which was confirmed on follow-up scans.
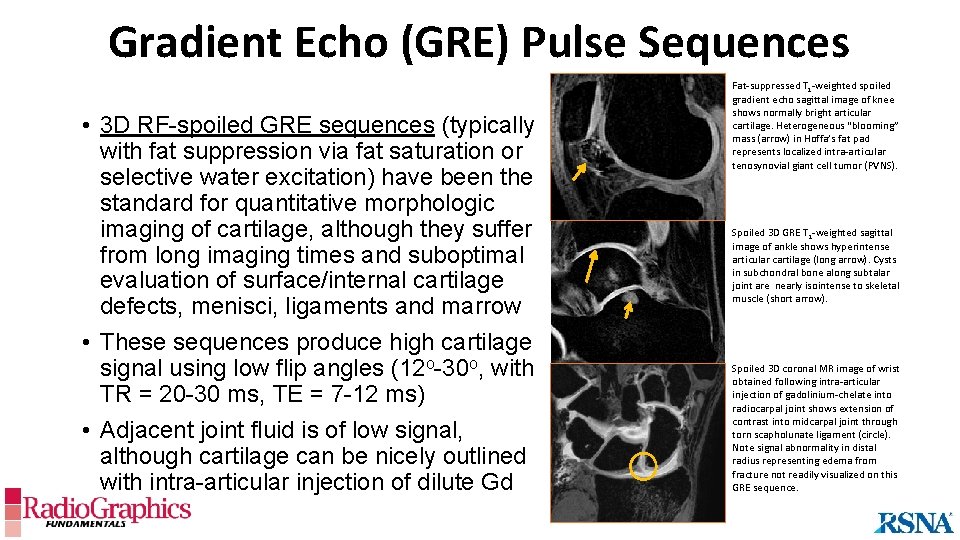
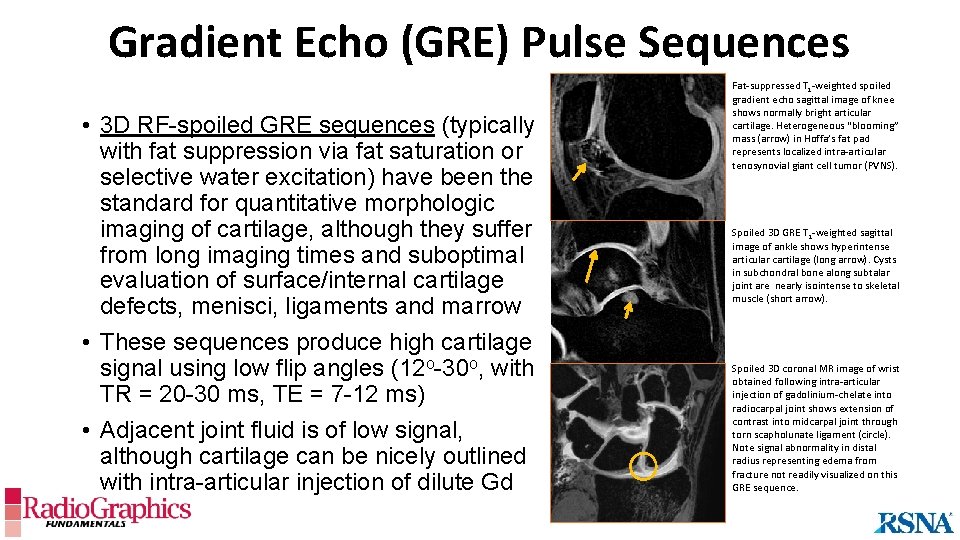
Gradient Echo (GRE) Pulse Sequences • 3 D RF-spoiled GRE sequences (typically with fat suppression via fat saturation or selective water excitation) have been the standard for quantitative morphologic imaging of cartilage, although they suffer from long imaging times and suboptimal evaluation of surface/internal cartilage defects, menisci, ligaments and marrow • These sequences produce high cartilage signal using low flip angles (12 o-30 o, with TR = 20 -30 ms, TE = 7 -12 ms) • Adjacent joint fluid is of low signal, although cartilage can be nicely outlined with intra-articular injection of dilute Gd Fat-suppressed T 1 -weighted spoiled gradient echo sagittal image of knee shows normally bright articular cartilage. Heterogeneous “blooming” mass (arrow) in Hoffa’s fat pad represents localized intra-articular tenosynovial giant cell tumor (PVNS). Spoiled 3 D GRE T 1 -weighted sagittal image of ankle shows hyperintense articular cartilage (long arrow). Cysts in subchondral bone along subtalar joint are nearly isointense to skeletal muscle (short arrow). Spoiled 3 D coronal MR image of wrist obtained following intra-articular injection of gadolinium-chelate into radiocarpal joint shows extension of contrast into midcarpal joint through torn scapholunate ligament (circle). Note signal abnormality in distal radius representing edema from fracture not readily visualized on this GRE sequence.
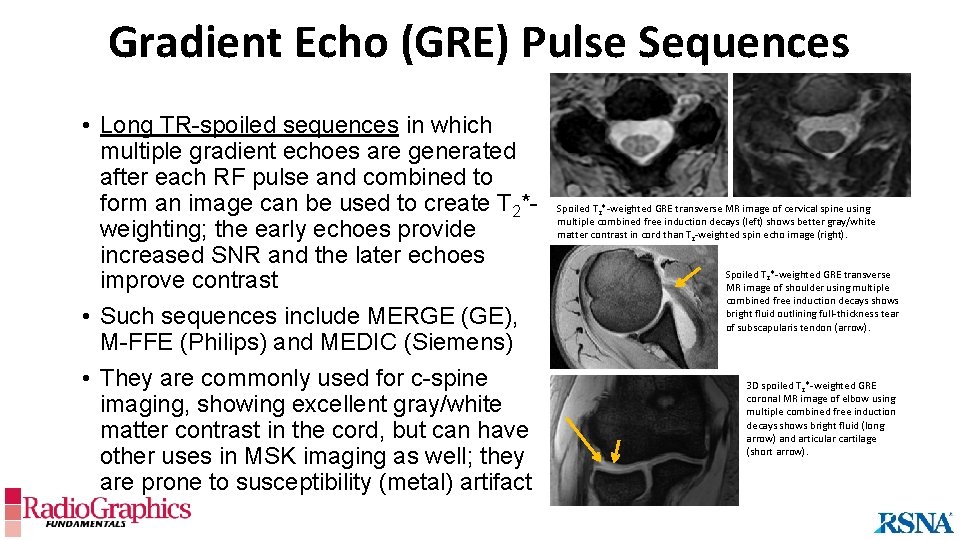
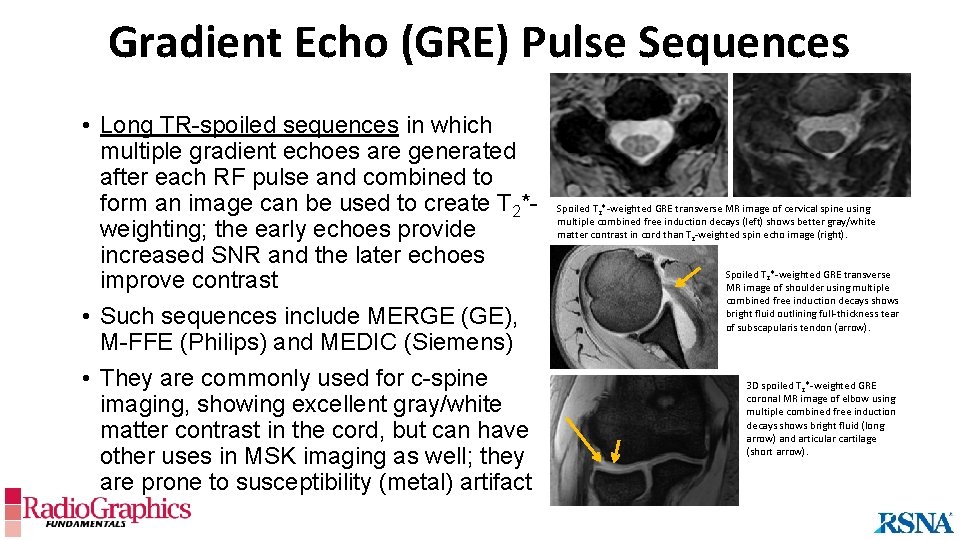
Gradient Echo (GRE) Pulse Sequences • Long TR-spoiled sequences in which multiple gradient echoes are generated after each RF pulse and combined to form an image can be used to create T 2*weighting; the early echoes provide increased SNR and the later echoes improve contrast • Such sequences include MERGE (GE), M-FFE (Philips) and MEDIC (Siemens) • They are commonly used for c-spine imaging, showing excellent gray/white matter contrast in the cord, but can have other uses in MSK imaging as well; they are prone to susceptibility (metal) artifact Spoiled T 2*-weighted GRE transverse MR image of cervical spine using multiple combined free induction decays (left) shows better gray/white matter contrast in cord than T 2 -weighted spin echo image (right). Spoiled T 2*-weighted GRE transverse MR image of shoulder using multiple combined free induction decays shows bright fluid outlining full-thickness tear of subscapularis tendon (arrow). 3 D spoiled T 2*-weighted GRE coronal MR image of elbow using multiple combined free induction decays shows bright fluid (long arrow) and articular cartilage (short arrow).
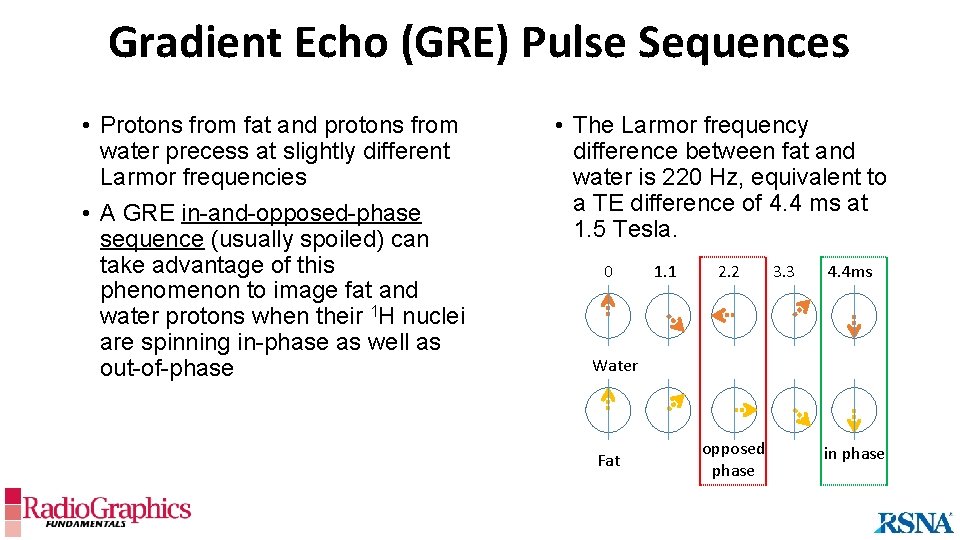
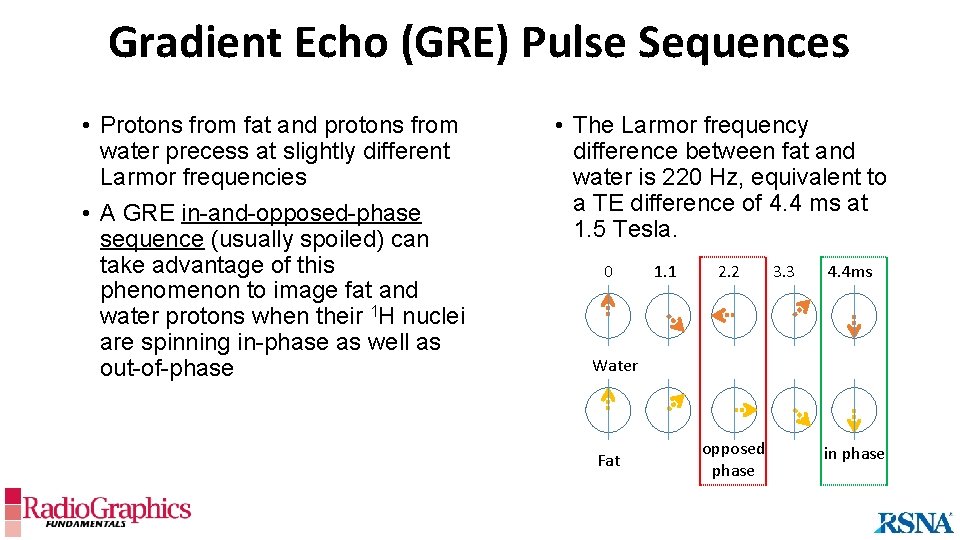
Gradient Echo (GRE) Pulse Sequences • Protons from fat and protons from water precess at slightly different Larmor frequencies • A GRE in-and-opposed-phase sequence (usually spoiled) can take advantage of this phenomenon to image fat and water protons when their 1 H nuclei are spinning in-phase as well as out-of-phase • The Larmor frequency difference between fat and water is 220 Hz, equivalent to a TE difference of 4. 4 ms at 1. 5 Tesla. 0 1. 1 2. 2 3. 3 4. 4 ms Water Fat opposed phase in phase
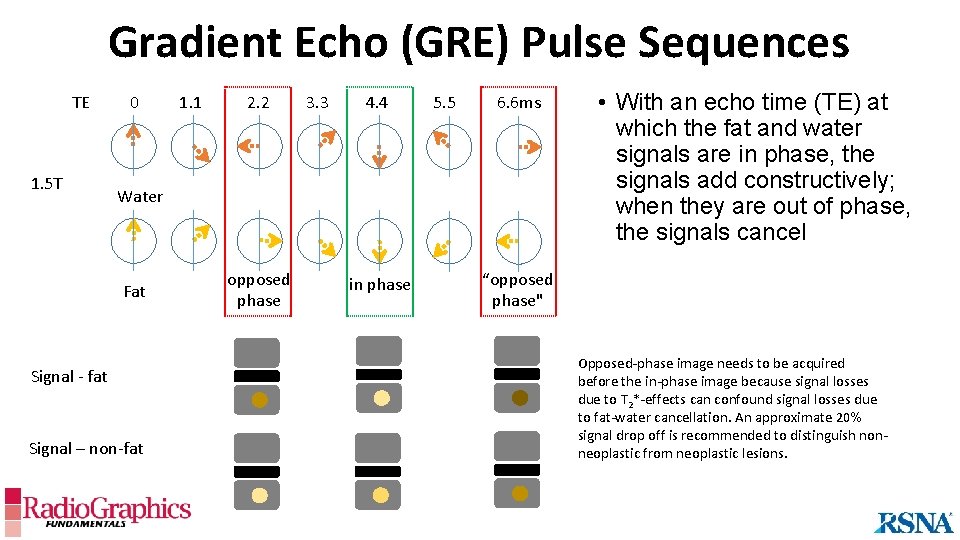
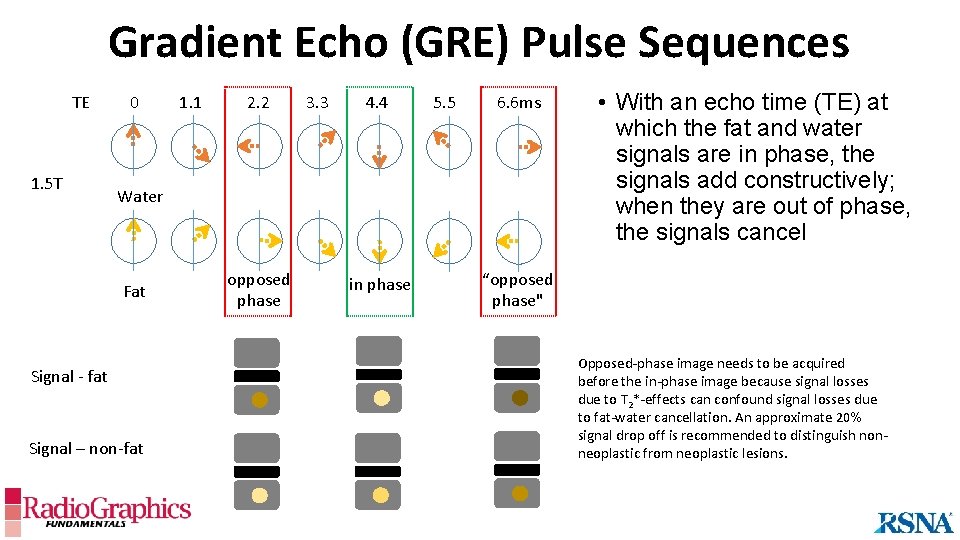
Gradient Echo (GRE) Pulse Sequences TE 1. 5 T 0 1. 1 2. 2 3. 3 4. 4 5. 5 6. 6 ms Water Fat Signal - fat Signal – non-fat opposed phase in phase • With an echo time (TE) at which the fat and water signals are in phase, the signals add constructively; when they are out of phase, the signals cancel “opposed phase" Opposed-phase image needs to be acquired before the in-phase image because signal losses due to T 2*-effects can confound signal losses due to fat-water cancellation. An approximate 20% signal drop off is recommended to distinguish nonneoplastic from neoplastic lesions.
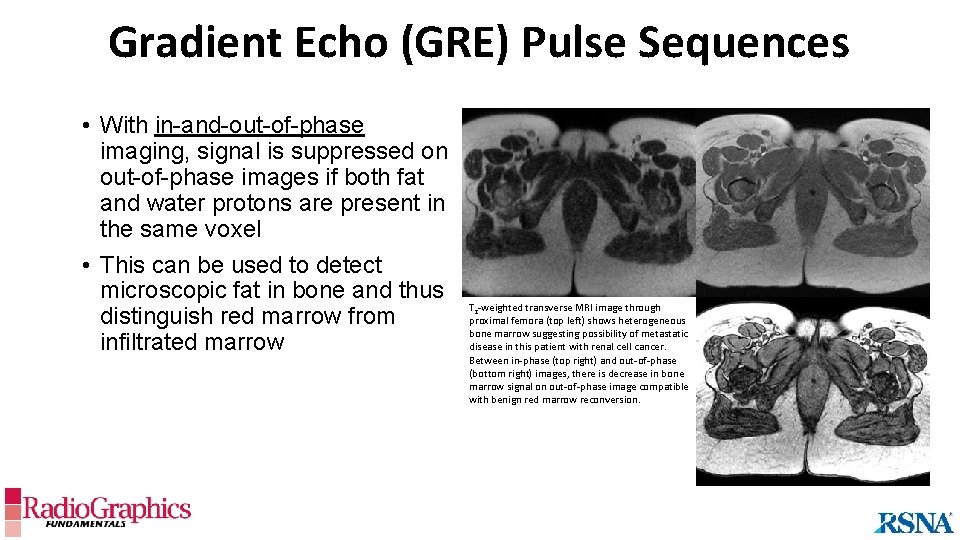
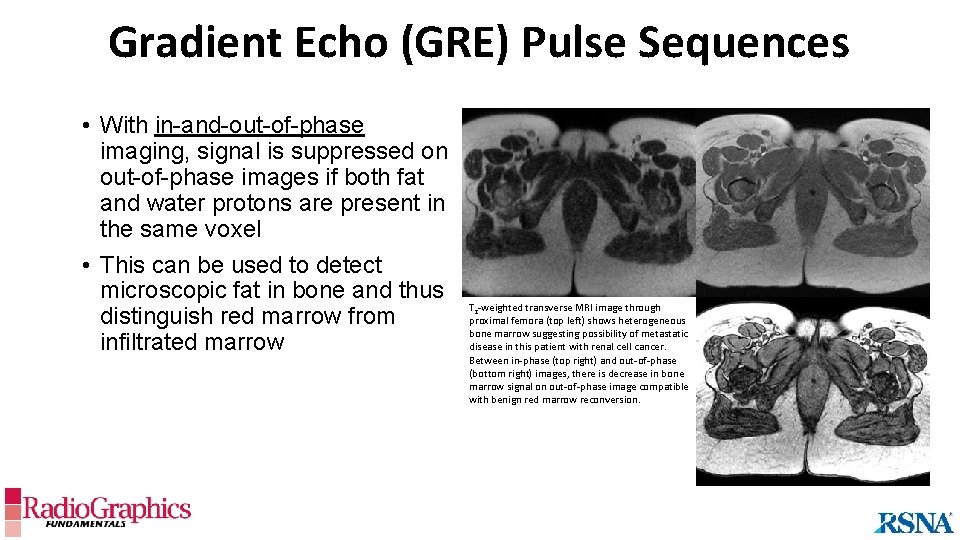
Gradient Echo (GRE) Pulse Sequences • With in-and-out-of-phase imaging, signal is suppressed on out-of-phase images if both fat and water protons are present in the same voxel • This can be used to detect microscopic fat in bone and thus distinguish red marrow from infiltrated marrow T 2 -weighted transverse MRI image through proximal femora (top left) shows heterogeneous bone marrow suggesting possibility of metastatic disease in this patient with renal cell cancer. Between in-phase (top right) and out-of-phase (bottom right) images, there is decrease in bone marrow signal on out-of-phase image compatible with benign red marrow reconversion.
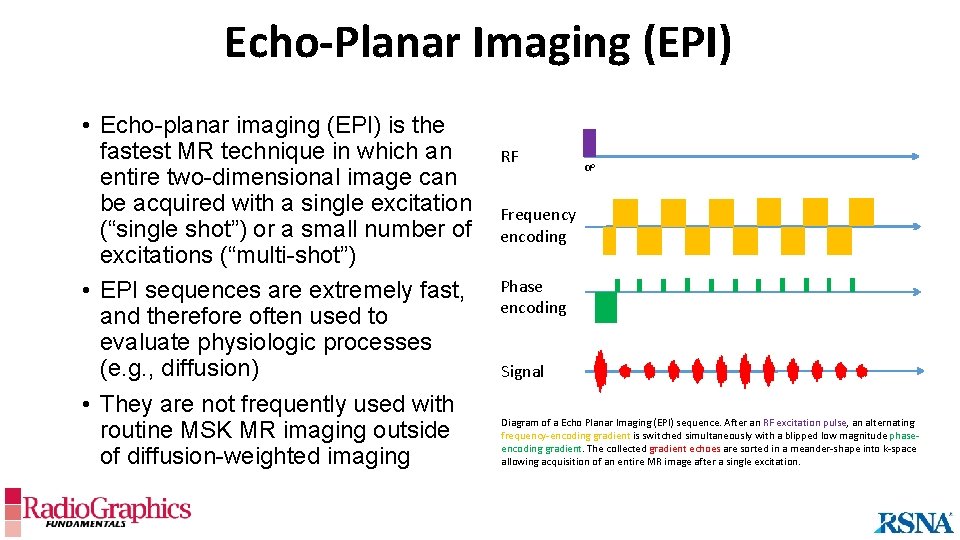
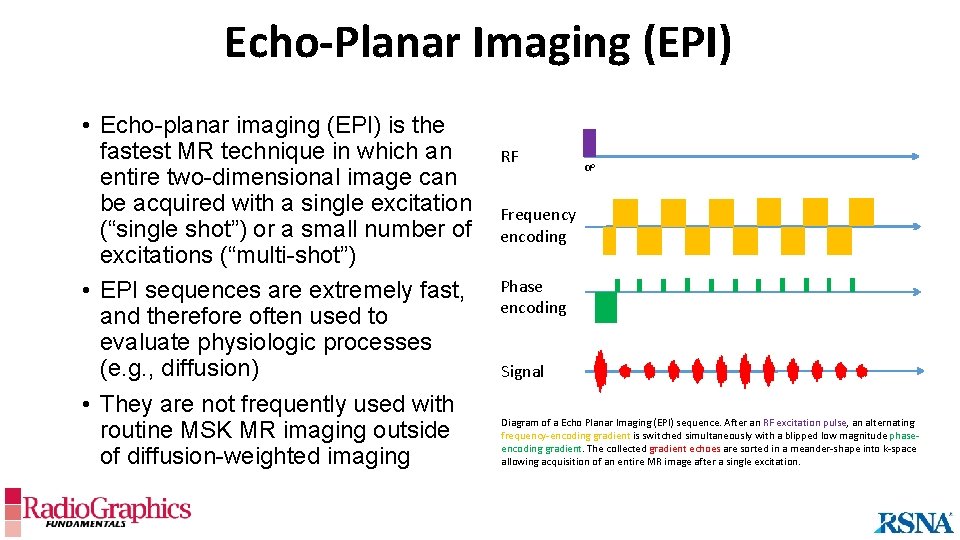
Echo-Planar Imaging (EPI) • Echo-planar imaging (EPI) is the fastest MR technique in which an entire two-dimensional image can be acquired with a single excitation (“single shot”) or a small number of excitations (“multi-shot”) • EPI sequences are extremely fast, and therefore often used to evaluate physiologic processes (e. g. , diffusion) • They are not frequently used with routine MSK MR imaging outside of diffusion-weighted imaging RF αo Frequency encoding Phase encoding Signal Diagram of a Echo Planar Imaging (EPI) sequence. After an RF excitation pulse, an alternating frequency-encoding gradient is switched simultaneously with a blipped low magnitude phaseencoding gradient. The collected gradient echoes are sorted in a meander-shape into k-space allowing acquisition of an entire MR image after a single excitation.
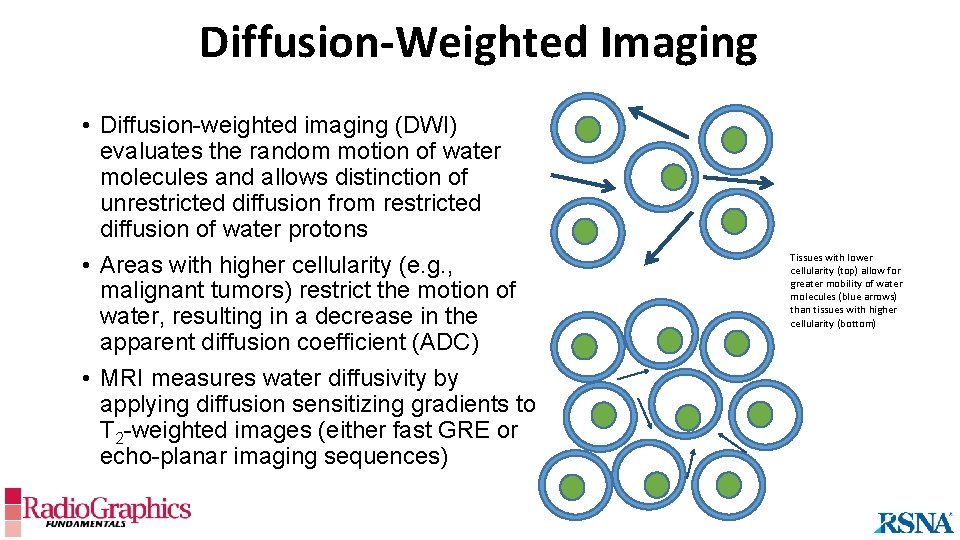
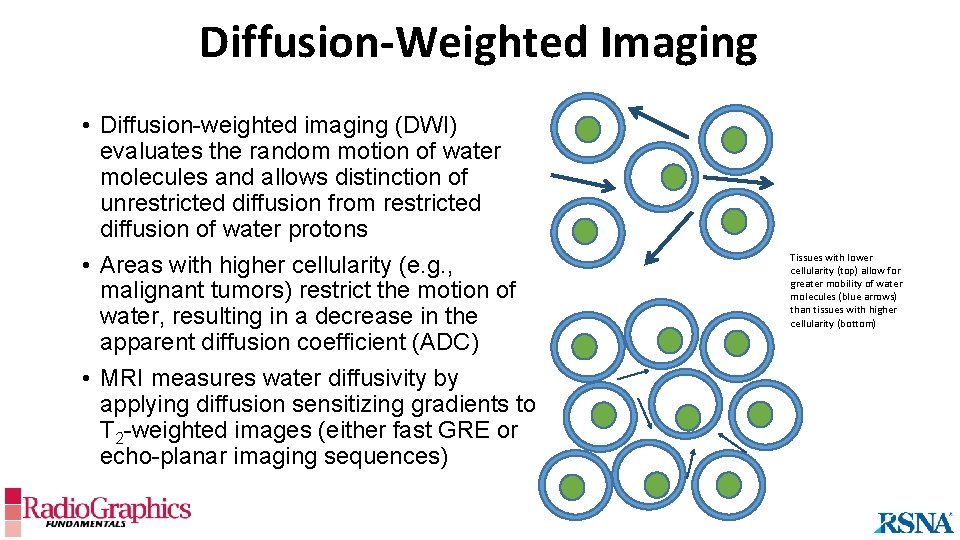
Diffusion-Weighted Imaging • Diffusion-weighted imaging (DWI) evaluates the random motion of water molecules and allows distinction of unrestricted diffusion from restricted diffusion of water protons • Areas with higher cellularity (e. g. , malignant tumors) restrict the motion of water, resulting in a decrease in the apparent diffusion coefficient (ADC) • MRI measures water diffusivity by applying diffusion sensitizing gradients to T 2 -weighted images (either fast GRE or echo-planar imaging sequences) Tissues with lower cellularity (top) allow for greater mobility of water molecules (blue arrows) than tissues with higher cellularity (bottom)
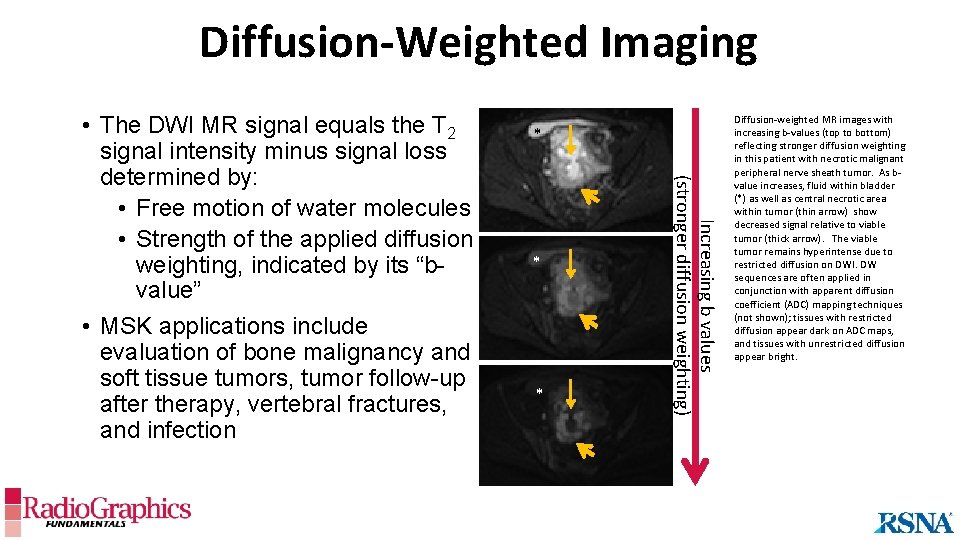
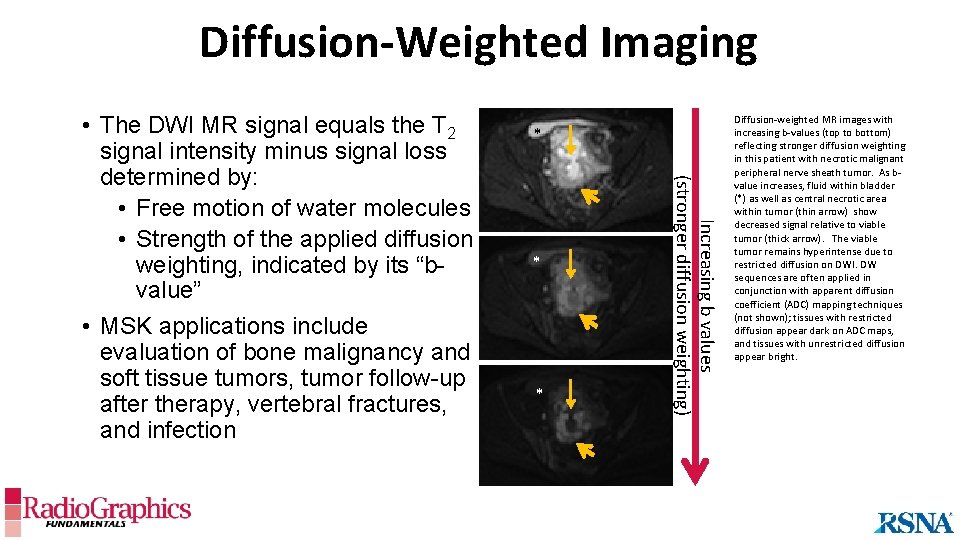
Diffusion-Weighted Imaging * * * Increasing b values (stronger diffusion weighting) • The DWI MR signal equals the T 2 signal intensity minus signal loss determined by: • Free motion of water molecules • Strength of the applied diffusion weighting, indicated by its “bvalue” • MSK applications include evaluation of bone malignancy and soft tissue tumors, tumor follow-up after therapy, vertebral fractures, and infection Diffusion-weighted MR images with increasing b-values (top to bottom) reflecting stronger diffusion weighting in this patient with necrotic malignant peripheral nerve sheath tumor. As bvalue increases, fluid within bladder (*) as well as central necrotic area within tumor (thin arrow) show decreased signal relative to viable tumor (thick arrow). The viable tumor remains hyperintense due to restricted diffusion on DWI. DW sequences are often applied in conjunction with apparent diffusion coefficient (ADC) mapping techniques (not shown); tissues with restricted diffusion appear dark on ADC maps, and tissues with unrestricted diffusion appear bright.
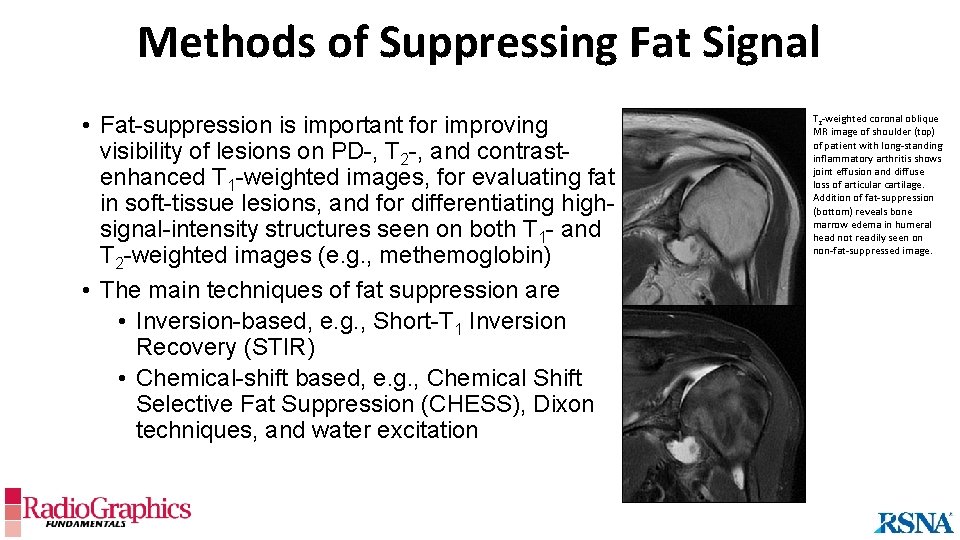
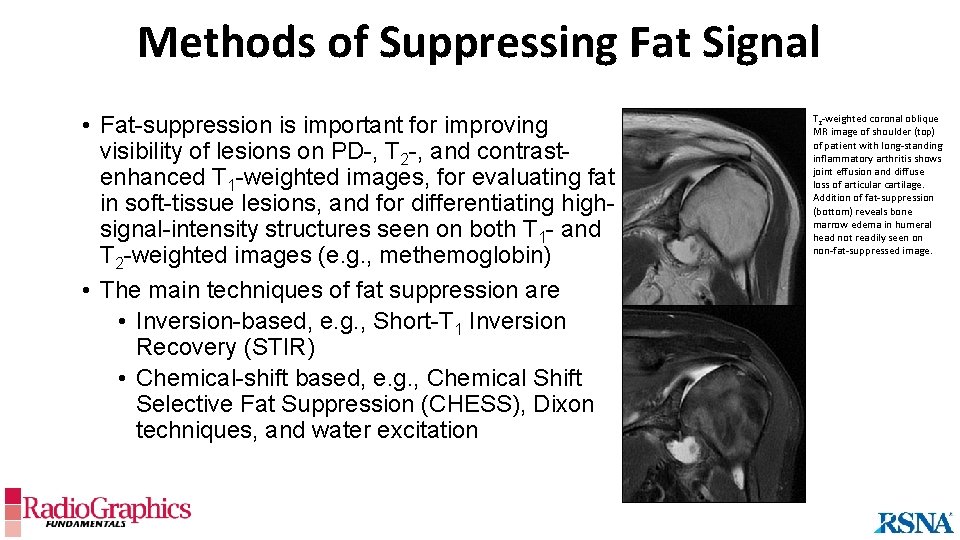
Methods of Suppressing Fat Signal • Fat-suppression is important for improving visibility of lesions on PD-, T 2 -, and contrastenhanced T 1 -weighted images, for evaluating fat in soft-tissue lesions, and for differentiating highsignal-intensity structures seen on both T 1 - and T 2 -weighted images (e. g. , methemoglobin) • The main techniques of fat suppression are • Inversion-based, e. g. , Short-T 1 Inversion Recovery (STIR) • Chemical-shift based, e. g. , Chemical Shift Selective Fat Suppression (CHESS), Dixon techniques, and water excitation T 2 -weighted coronal oblique MR image of shoulder (top) of patient with long-standing inflammatory arthritis shows joint effusion and diffuse loss of articular cartilage. Addition of fat-suppression (bottom) reveals bone marrow edema in humeral head not readily seen on non-fat-suppressed image.
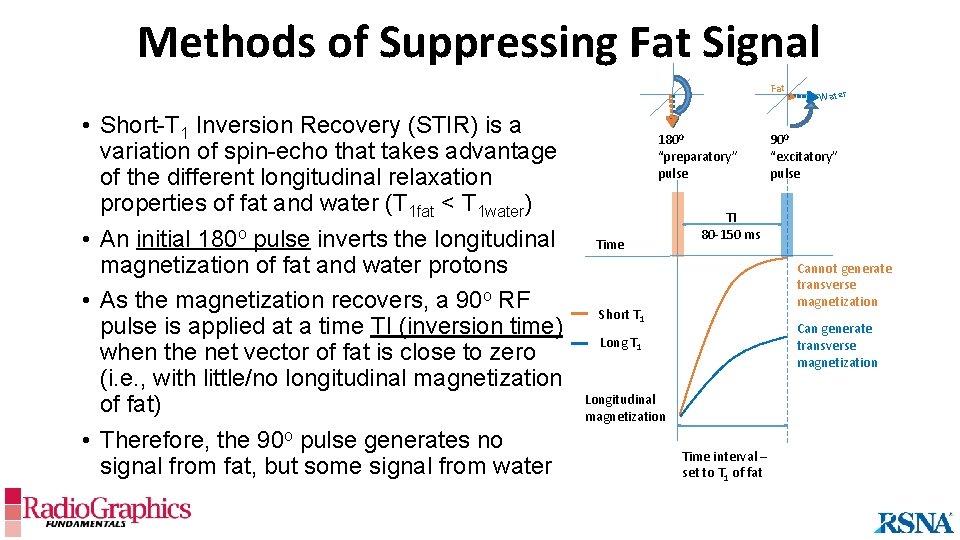
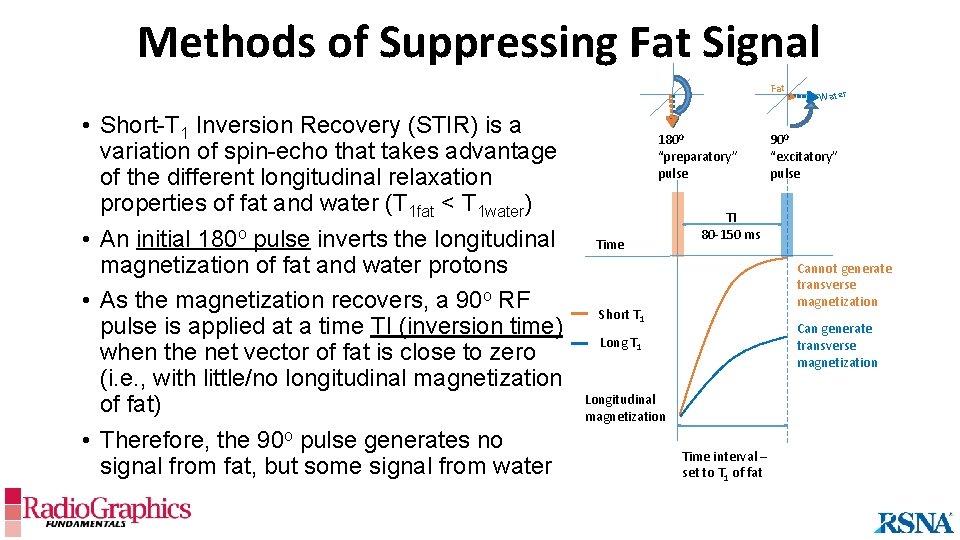
Methods of Suppressing Fat Signal Fat • Short-T 1 Inversion Recovery (STIR) is a variation of spin-echo that takes advantage of the different longitudinal relaxation properties of fat and water (T 1 fat < T 1 water) • An initial 180 o pulse inverts the longitudinal magnetization of fat and water protons • As the magnetization recovers, a 90 o RF pulse is applied at a time TI (inversion time) when the net vector of fat is close to zero (i. e. , with little/no longitudinal magnetization of fat) • Therefore, the 90 o pulse generates no signal from fat, but some signal from water 1800 “preparatory” pulse Time Water 900 “excitatory” pulse TI 80 -150 ms Cannot generate transverse magnetization Short T 1 Can generate transverse magnetization Long T 1 Longitudinal magnetization Time interval – set to T 1 of fat
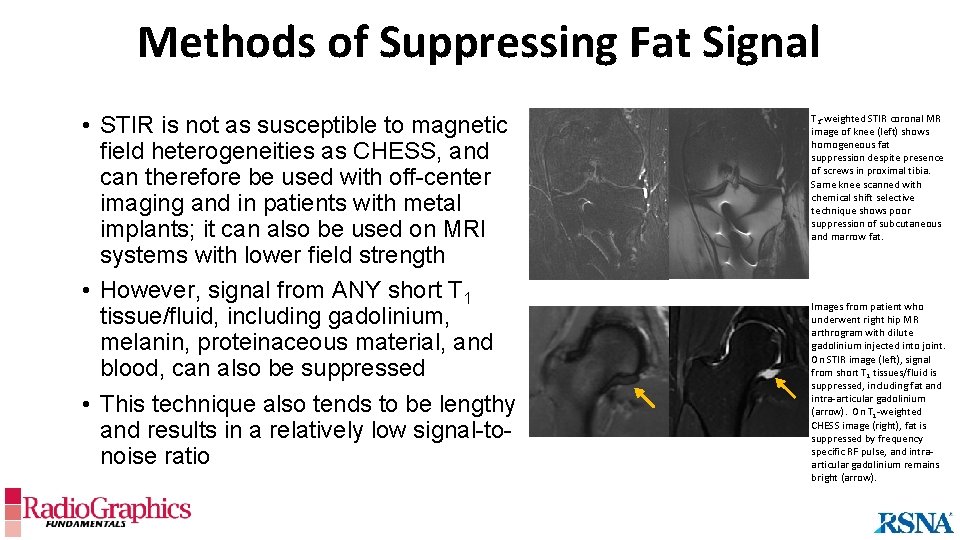
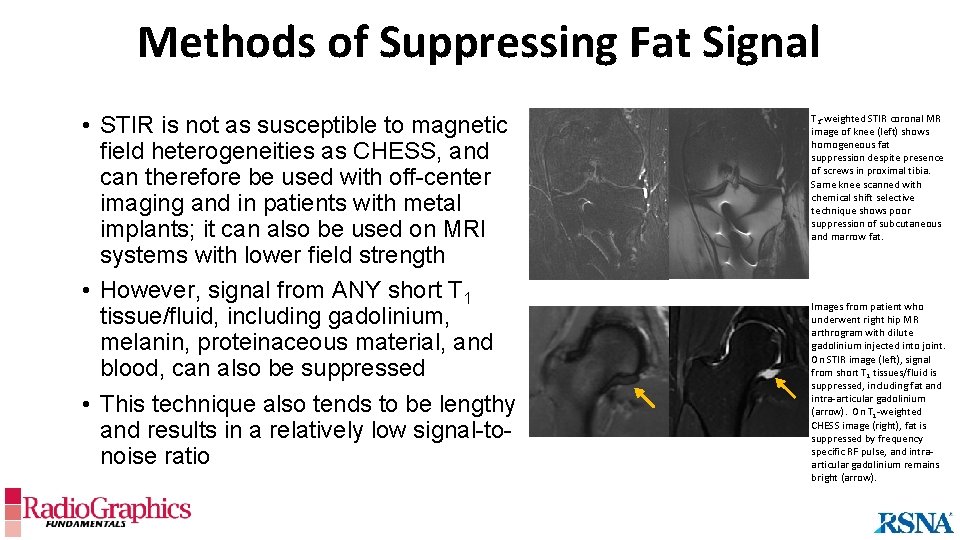
Methods of Suppressing Fat Signal • STIR is not as susceptible to magnetic field heterogeneities as CHESS, and can therefore be used with off-center imaging and in patients with metal implants; it can also be used on MRI systems with lower field strength • However, signal from ANY short T 1 tissue/fluid, including gadolinium, melanin, proteinaceous material, and blood, can also be suppressed • This technique also tends to be lengthy and results in a relatively low signal-tonoise ratio T 2 -weighted STIR coronal MR image of knee (left) shows homogeneous fat suppression despite presence of screws in proximal tibia. Same knee scanned with chemical shift selective technique shows poor suppression of subcutaneous and marrow fat. Images from patient who underwent right hip MR arthrogram with dilute gadolinium injected into joint. On STIR image (left), signal from short T 1 tissues/fluid is suppressed, including fat and intra-articular gadolinium (arrow). On T 1 -weighted CHESS image (right), fat is suppressed by frequency specific RF pulse, and intraarticular gadolinium remains bright (arrow).
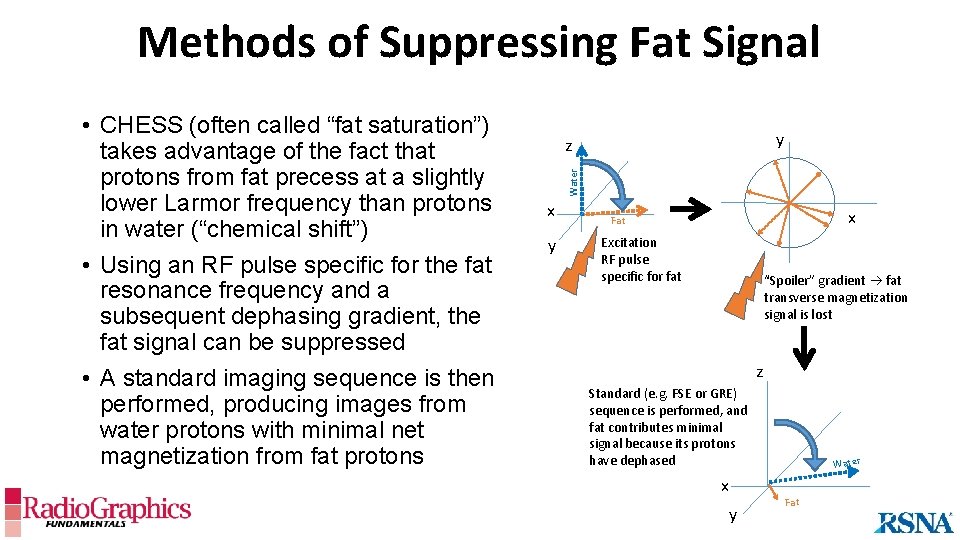
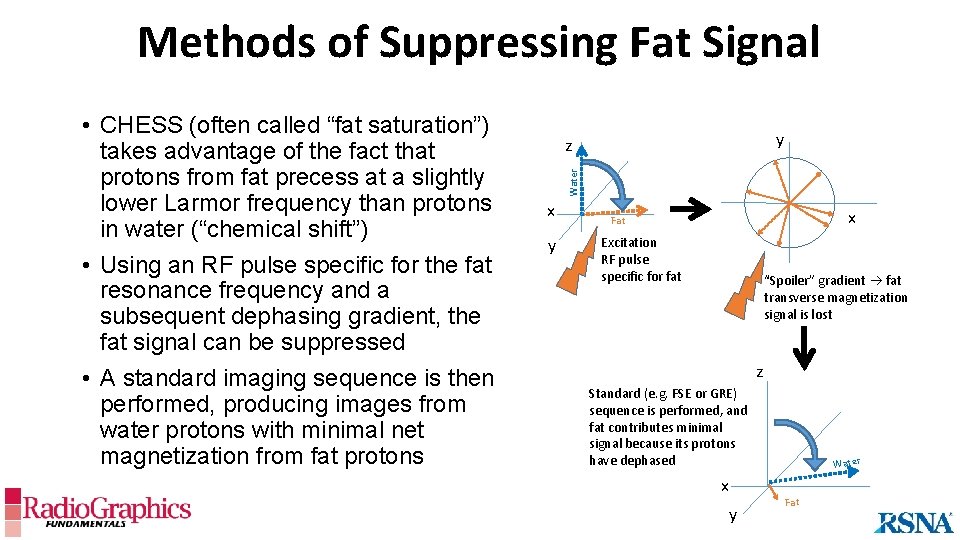
Methods of Suppressing Fat Signal y z Water • CHESS (often called “fat saturation”) takes advantage of the fact that protons from fat precess at a slightly lower Larmor frequency than protons in water (“chemical shift”) • Using an RF pulse specific for the fat resonance frequency and a subsequent dephasing gradient, the fat signal can be suppressed • A standard imaging sequence is then performed, producing images from water protons with minimal net magnetization from fat protons x y x Fat Excitation RF pulse specific for fat “Spoiler” gradient fat transverse magnetization signal is lost z Standard (e. g. FSE or GRE) sequence is performed, and fat contributes minimal signal because its protons have dephased x y Water Fat
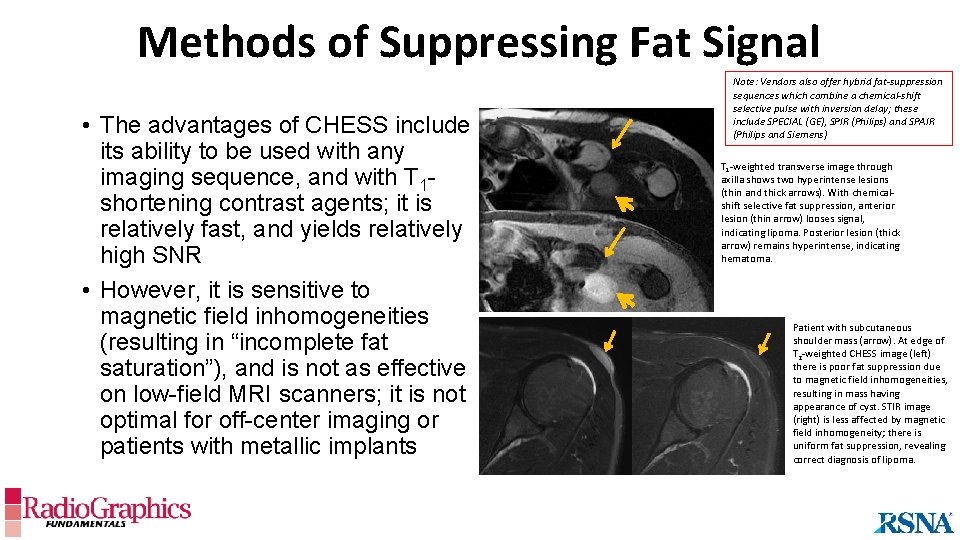
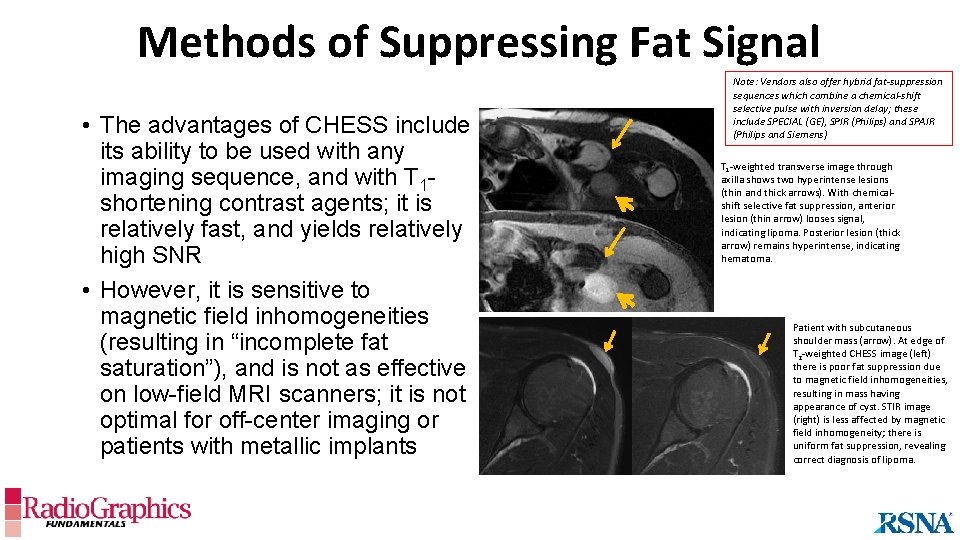
Methods of Suppressing Fat Signal • The advantages of CHESS include its ability to be used with any imaging sequence, and with T 1 shortening contrast agents; it is relatively fast, and yields relatively high SNR • However, it is sensitive to magnetic field inhomogeneities (resulting in “incomplete fat saturation”), and is not as effective on low-field MRI scanners; it is not optimal for off-center imaging or patients with metallic implants Note: Vendors also offer hybrid fat-suppression sequences which combine a chemical-shift selective pulse with inversion delay; these include SPECIAL (GE), SPIR (Philips) and SPAIR (Philips and Siemens) T 1 -weighted transverse image through axilla shows two hyperintense lesions (thin and thick arrows). With chemicalshift selective fat suppression, anterior lesion (thin arrow) looses signal, indicating lipoma. Posterior lesion (thick arrow) remains hyperintense, indicating hematoma. Patient with subcutaneous shoulder mass (arrow). At edge of T 2 -weighted CHESS image (left) there is poor fat suppression due to magnetic field inhomogeneities, resulting in mass having appearance of cyst. STIR image (right) is less affected by magnetic field inhomogeneity; there is uniform fat suppression, revealing correct diagnosis of lipoma.
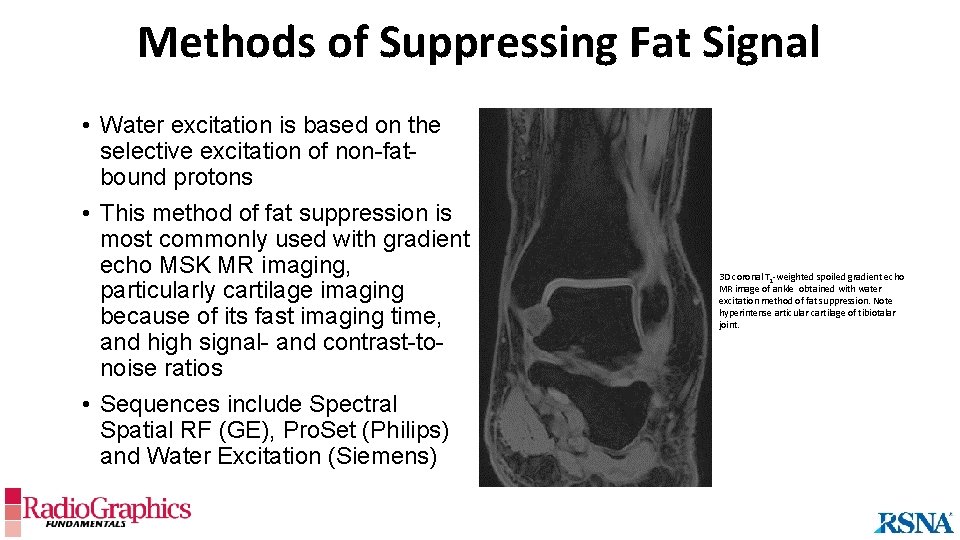
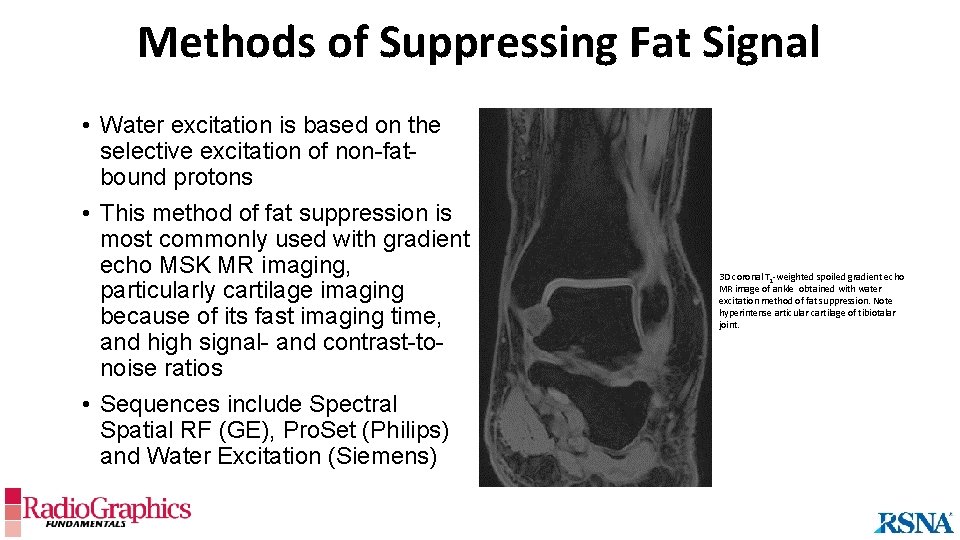
Methods of Suppressing Fat Signal • Water excitation is based on the selective excitation of non-fatbound protons • This method of fat suppression is most commonly used with gradient echo MSK MR imaging, particularly cartilage imaging because of its fast imaging time, and high signal- and contrast-tonoise ratios • Sequences include Spectral Spatial RF (GE), Pro. Set (Philips) and Water Excitation (Siemens) 3 D coronal T 1 -weighted spoiled gradient echo MR image of ankle obtained with water excitation method of fat suppression. Note hyperintense articular cartilage of tibiotalar joint.
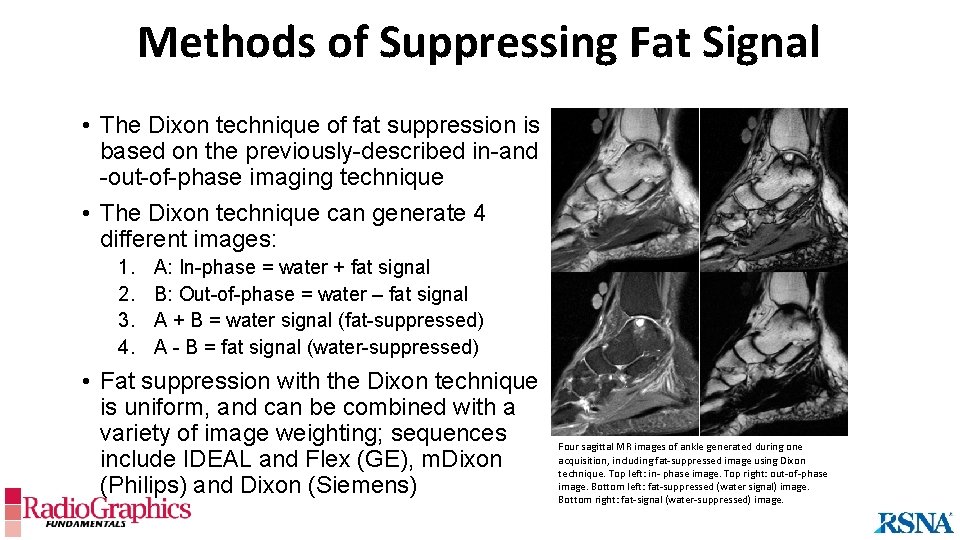
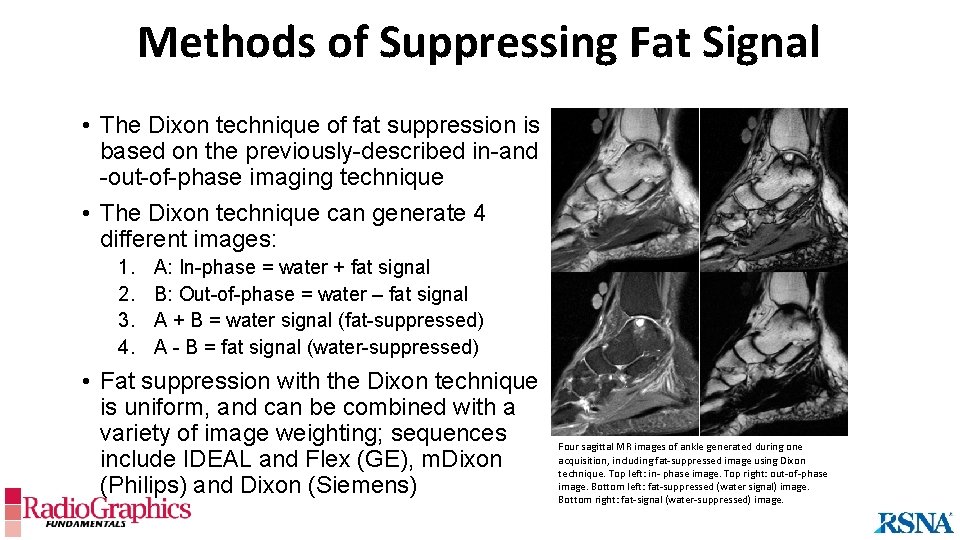
Methods of Suppressing Fat Signal • The Dixon technique of fat suppression is based on the previously-described in-and -out-of-phase imaging technique • The Dixon technique can generate 4 different images: 1. 2. 3. 4. A: In-phase = water + fat signal B: Out-of-phase = water – fat signal A + B = water signal (fat-suppressed) A - B = fat signal (water-suppressed) • Fat suppression with the Dixon technique is uniform, and can be combined with a variety of image weighting; sequences include IDEAL and Flex (GE), m. Dixon (Philips) and Dixon (Siemens) Four sagittal MR images of ankle generated during one acquisition, including fat-suppressed image using Dixon technique. Top left: in- phase image. Top right: out-of-phase image. Bottom left: fat-suppressed (water signal) image. Bottom right: fat-signal (water-suppressed) image.
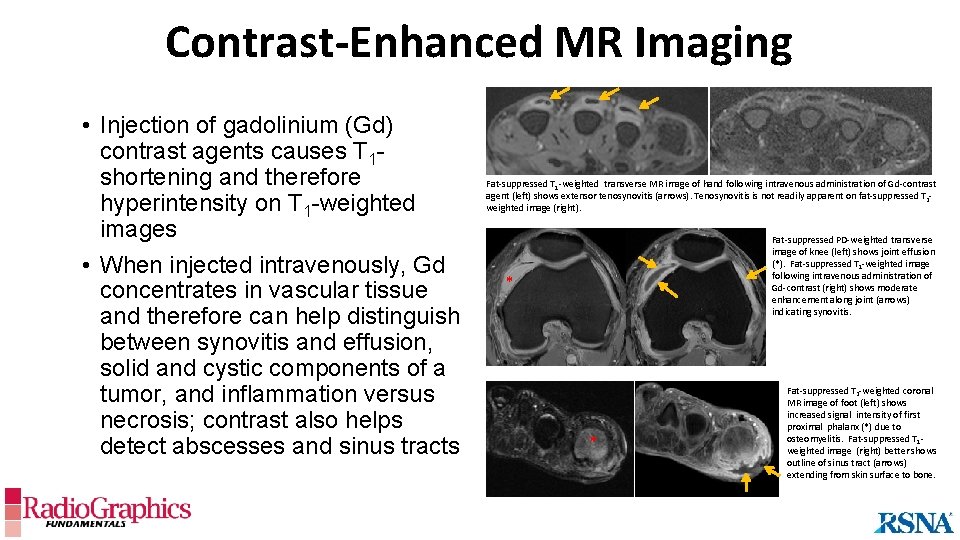
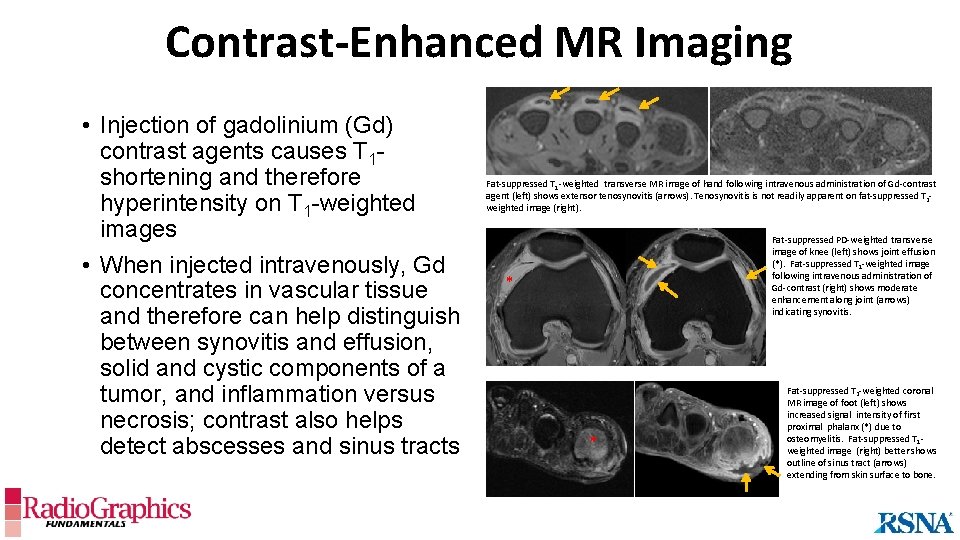
Contrast-Enhanced MR Imaging • Injection of gadolinium (Gd) contrast agents causes T 1 shortening and therefore hyperintensity on T 1 -weighted images • When injected intravenously, Gd concentrates in vascular tissue and therefore can help distinguish between synovitis and effusion, solid and cystic components of a tumor, and inflammation versus necrosis; contrast also helps detect abscesses and sinus tracts Fat-suppressed T 1 -weighted transverse MR image of hand following intravenous administration of Gd-contrast agent (left) shows extensor tenosynovitis (arrows). Tenosynovitis is not readily apparent on fat-suppressed T 2 weighted image (right). Fat-suppressed PD-weighted transverse image of knee (left) shows joint effusion (*). Fat-suppressed T 1 -weighted image following intravenous administration of Gd-contrast (right) shows moderate enhancement along joint (arrows) indicating synovitis. * * Fat-suppressed T 2 -weighted coronal MR image of foot (left) shows increased signal intensity of first proximal phalanx (*) due to osteomyelitis. Fat-suppressed T 1 weighted image (right) better shows outline of sinus tract (arrows) extending from skin surface to bone.
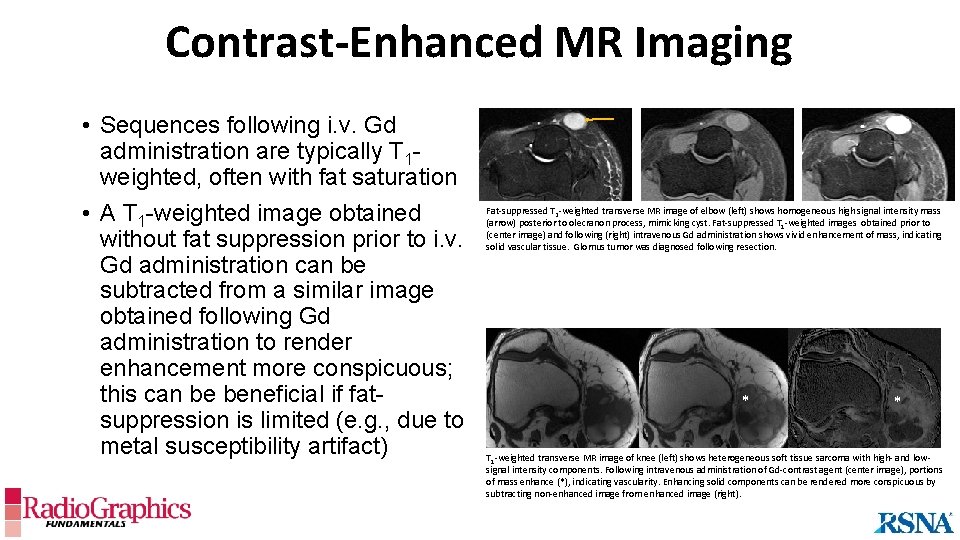
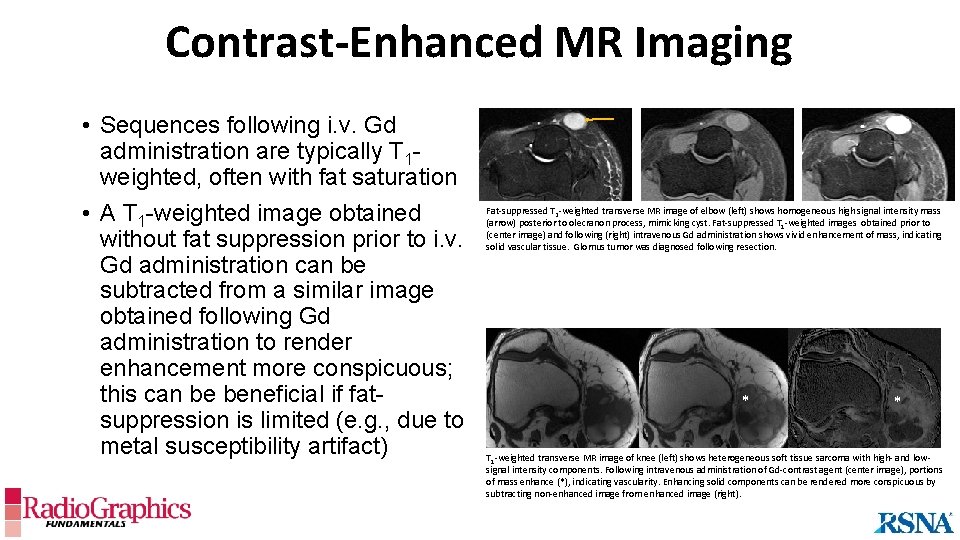
Contrast-Enhanced MR Imaging • Sequences following i. v. Gd administration are typically T 1 weighted, often with fat saturation • A T 1 -weighted image obtained without fat suppression prior to i. v. Gd administration can be subtracted from a similar image obtained following Gd administration to render enhancement more conspicuous; this can be beneficial if fatsuppression is limited (e. g. , due to metal susceptibility artifact) Fat-suppressed T 2 -weighted transverse MR image of elbow (left) shows homogeneous high signal intensity mass (arrow) posterior to olecranon process, mimicking cyst. Fat-suppressed T 1 -weighted images obtained prior to (center image) and following (right) intravenous Gd administration shows vivid enhancement of mass, indicating solid vascular tissue. Glomus tumor was diagnosed following resection. * * T 1 -weighted transverse MR image of knee (left) shows heterogeneous soft tissue sarcoma with high- and lowsignal intensity components. Following intravenous administration of Gd-contrast agent (center image), portions of mass enhance (*), indicating vascularity. Enhancing solid components can be rendered more conspicuous by subtracting non-enhanced image from enhanced image (right).
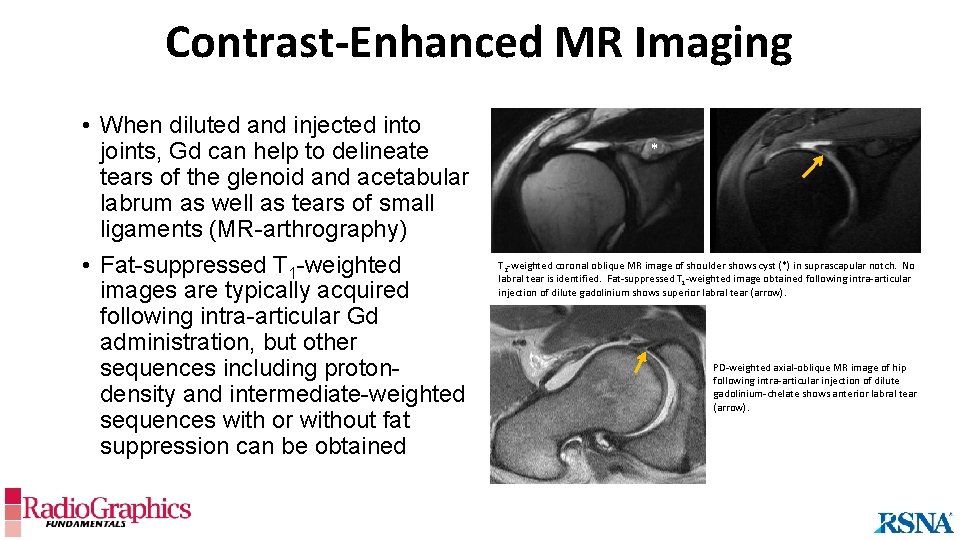
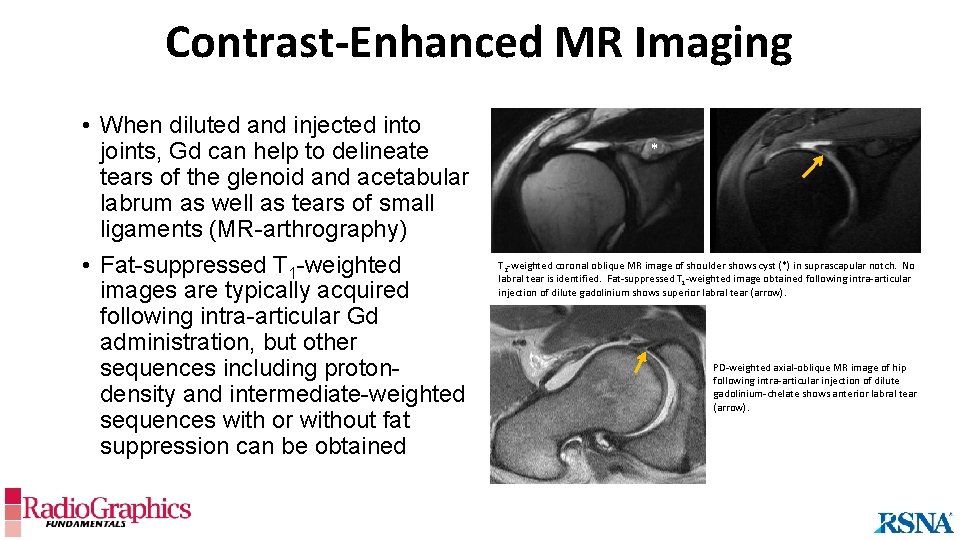
Contrast-Enhanced MR Imaging • When diluted and injected into joints, Gd can help to delineate tears of the glenoid and acetabular labrum as well as tears of small ligaments (MR-arthrography) • Fat-suppressed T 1 -weighted images are typically acquired following intra-articular Gd administration, but other sequences including protondensity and intermediate-weighted sequences with or without fat suppression can be obtained * T 2 -weighted coronal oblique MR image of shoulder shows cyst (*) in suprascapular notch. No labral tear is identified. Fat-suppressed T 1 -weighted image obtained following intra-articular injection of dilute gadolinium shows superior labral tear (arrow). PD-weighted axial-oblique MR image of hip following intra-articular injection of dilute gadolinium-chelate shows anterior labral tear (arrow).
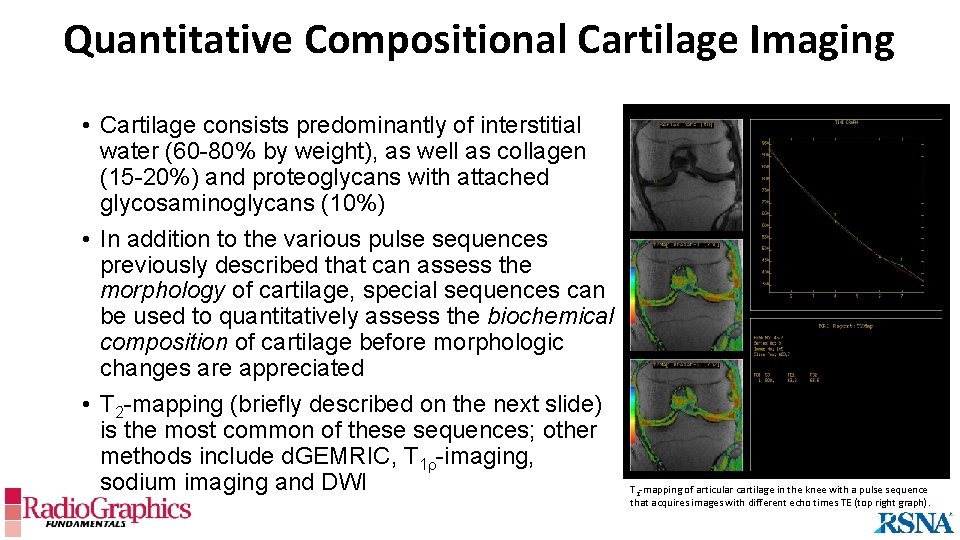
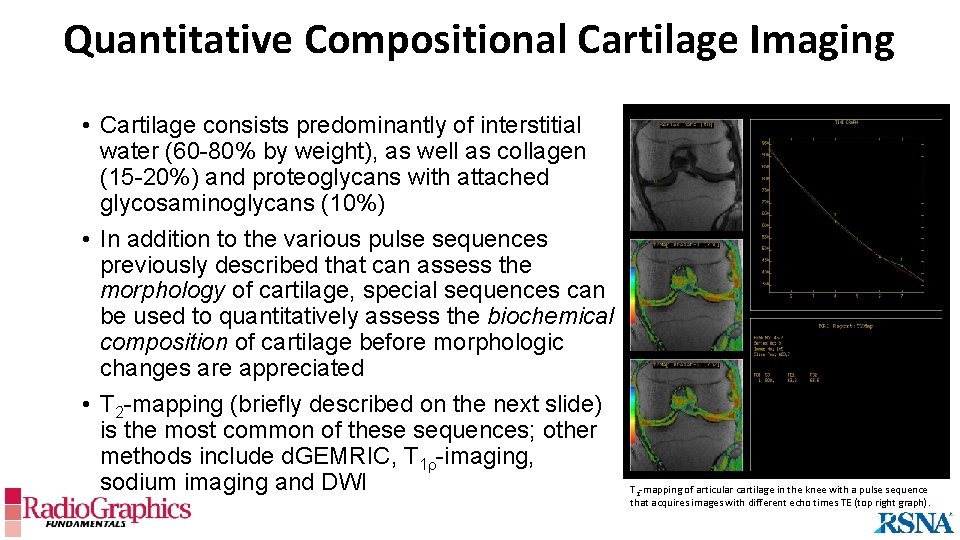
Quantitative Compositional Cartilage Imaging • Cartilage consists predominantly of interstitial water (60 -80% by weight), as well as collagen (15 -20%) and proteoglycans with attached glycosaminoglycans (10%) • In addition to the various pulse sequences previously described that can assess the morphology of cartilage, special sequences can be used to quantitatively assess the biochemical composition of cartilage before morphologic changes are appreciated • T 2 -mapping (briefly described on the next slide) is the most common of these sequences; other methods include d. GEMRIC, T 1 r-imaging, sodium imaging and DWI T 2 -mapping of articular cartilage in the knee with a pulse sequence that acquires images with different echo times TE (top right graph).
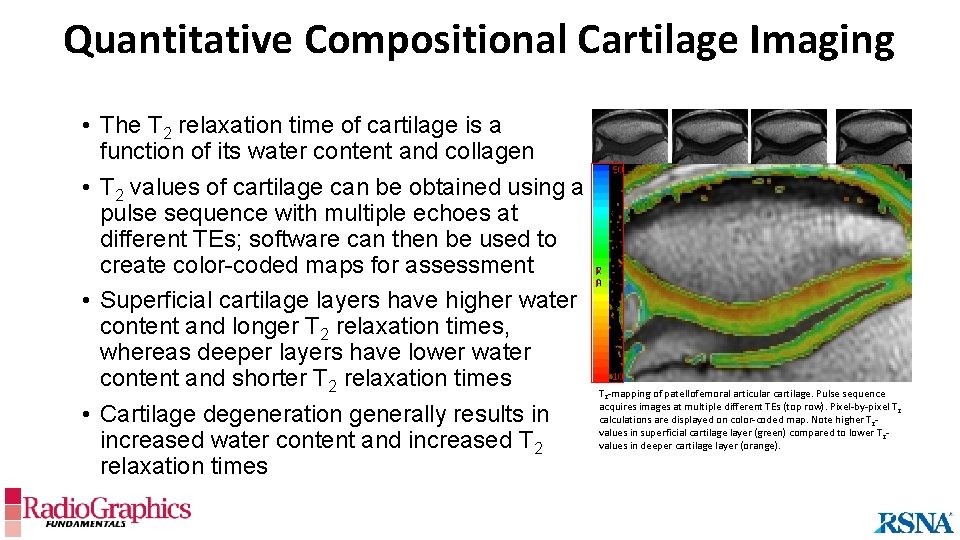
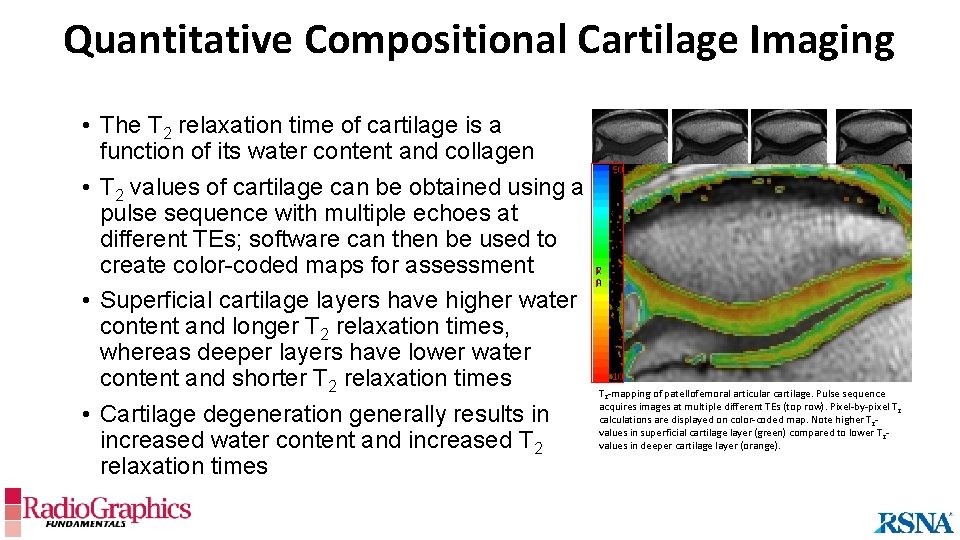
Quantitative Compositional Cartilage Imaging • The T 2 relaxation time of cartilage is a function of its water content and collagen • T 2 values of cartilage can be obtained using a pulse sequence with multiple echoes at different TEs; software can then be used to create color-coded maps for assessment • Superficial cartilage layers have higher water content and longer T 2 relaxation times, whereas deeper layers have lower water content and shorter T 2 relaxation times • Cartilage degeneration generally results in increased water content and increased T 2 relaxation times T 2 -mapping of patellofemoral articular cartilage. Pulse sequence acquires images at multiple different TEs (top row). Pixel-by-pixel T 2 calculations are displayed on color-coded map. Note higher T 2 values in superficial cartilage layer (green) compared to lower T 2 values in deeper cartilage layer (orange).
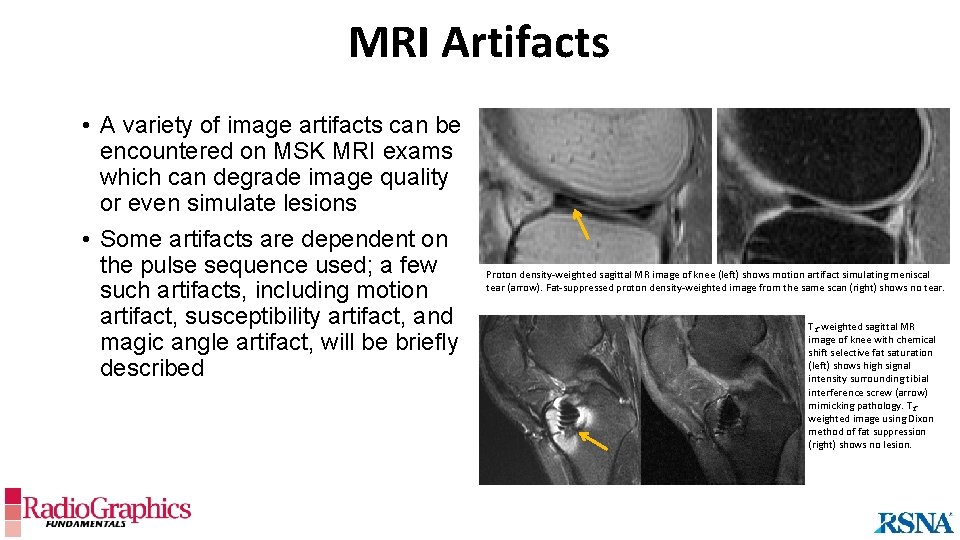
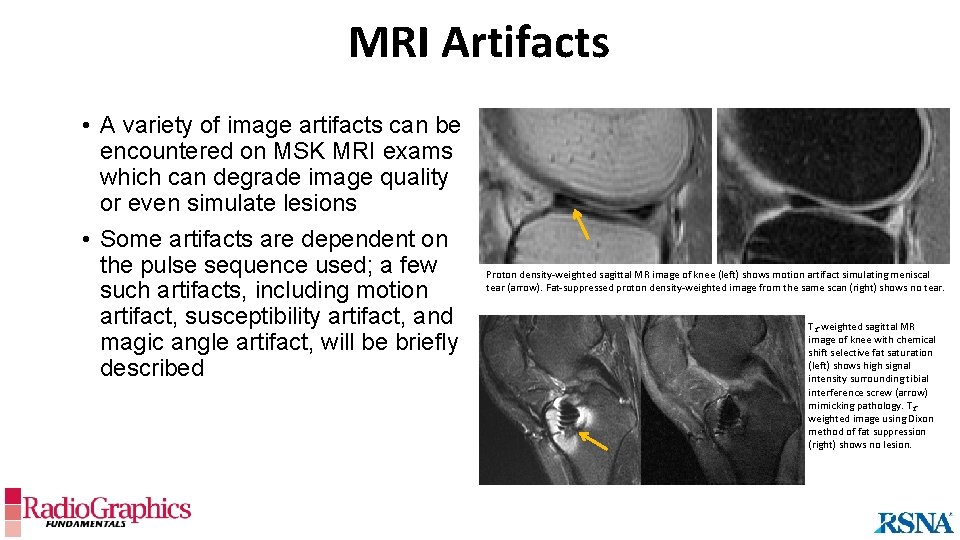
MRI Artifacts • A variety of image artifacts can be encountered on MSK MRI exams which can degrade image quality or even simulate lesions • Some artifacts are dependent on the pulse sequence used; a few such artifacts, including motion artifact, susceptibility artifact, and magic angle artifact, will be briefly described Proton density-weighted sagittal MR image of knee (left) shows motion artifact simulating meniscal tear (arrow). Fat-suppressed proton density-weighted image from the same scan (right) shows no tear. T 2 -weighted sagittal MR image of knee with chemical shift selective fat saturation (left) shows high signal intensity surrounding tibial interference screw (arrow) mimicking pathology. T 2 weighted image using Dixon method of fat suppression (right) shows no lesion.
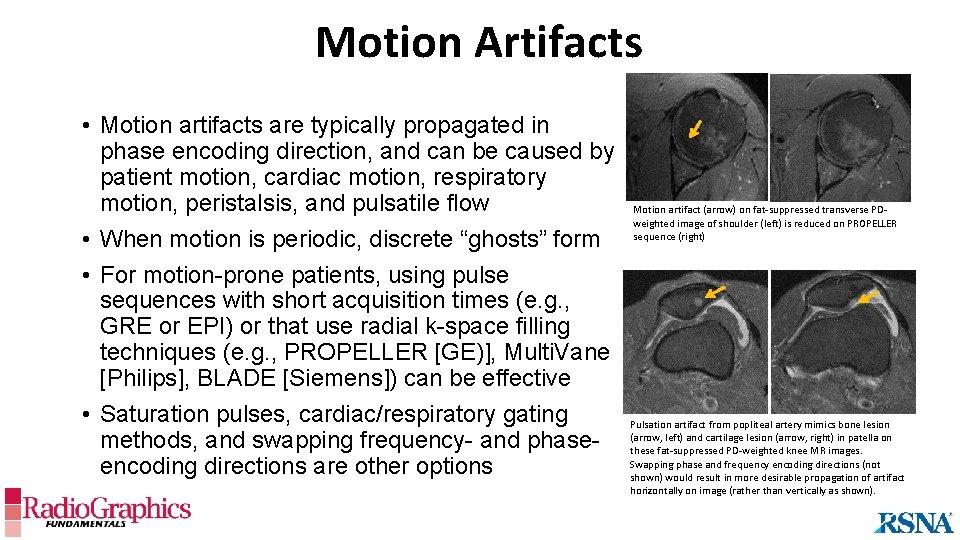
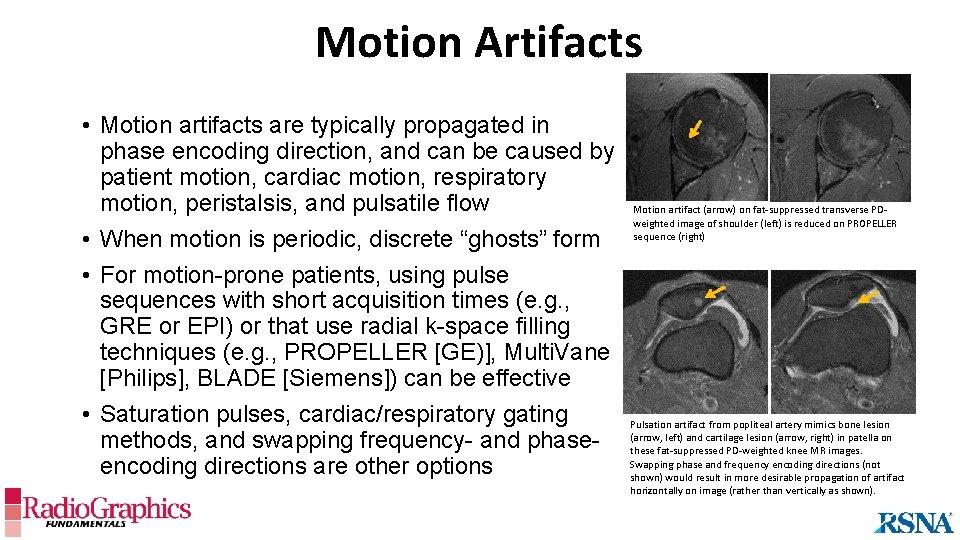
Motion Artifacts • Motion artifacts are typically propagated in phase encoding direction, and can be caused by patient motion, cardiac motion, respiratory motion, peristalsis, and pulsatile flow • When motion is periodic, discrete “ghosts” form • For motion-prone patients, using pulse sequences with short acquisition times (e. g. , GRE or EPI) or that use radial k-space filling techniques (e. g. , PROPELLER [GE)], Multi. Vane [Philips], BLADE [Siemens]) can be effective • Saturation pulses, cardiac/respiratory gating methods, and swapping frequency- and phaseencoding directions are other options Motion artifact (arrow) on fat-suppressed transverse PDweighted image of shoulder (left) is reduced on PROPELLER sequence (right) Pulsation artifact from popliteal artery mimics bone lesion (arrow, left) and cartilage lesion (arrow, right) in patella on these fat-suppressed PD-weighted knee MR images. Swapping phase and frequency encoding directions (not shown) would result in more desirable propagation of artifact horizontally on image (rather than vertically as shown).
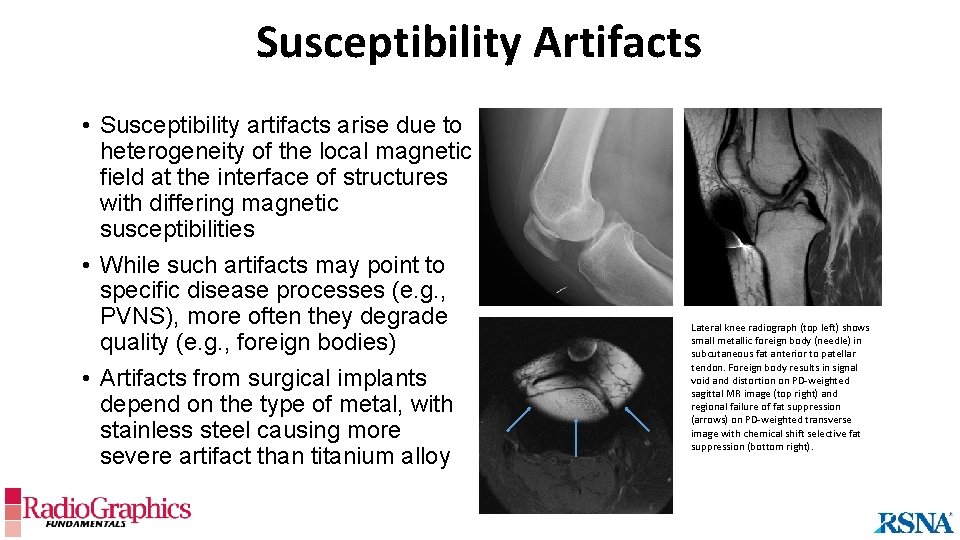
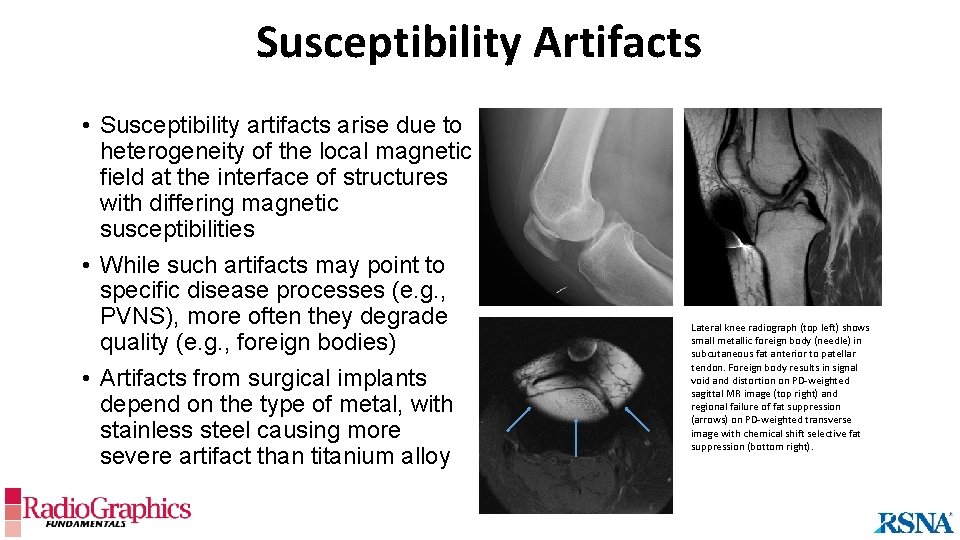
Susceptibility Artifacts • Susceptibility artifacts arise due to heterogeneity of the local magnetic field at the interface of structures with differing magnetic susceptibilities • While such artifacts may point to specific disease processes (e. g. , PVNS), more often they degrade quality (e. g. , foreign bodies) • Artifacts from surgical implants depend on the type of metal, with stainless steel causing more severe artifact than titanium alloy Lateral knee radiograph (top left) shows small metallic foreign body (needle) in subcutaneous fat anterior to patellar tendon. Foreign body results in signal void and distortion on PD-weighted sagittal MR image (top right) and regional failure of fat suppression (arrows) on PD-weighted transverse image with chemical shift selective fat suppression (bottom right).
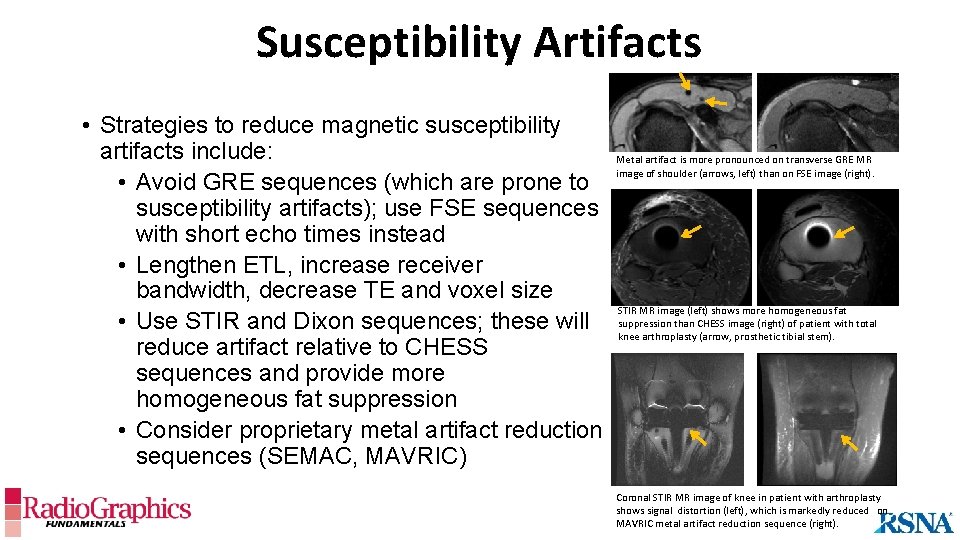
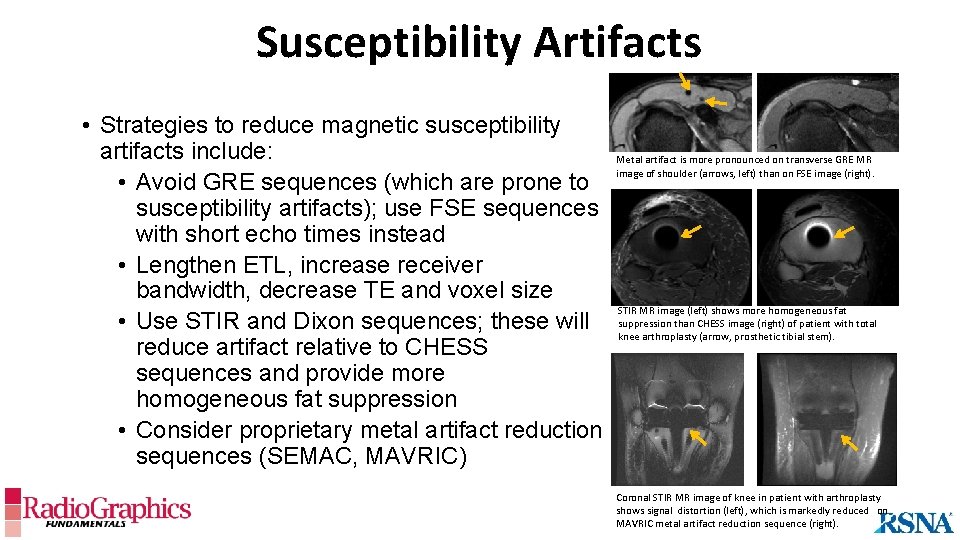
Susceptibility Artifacts • Strategies to reduce magnetic susceptibility artifacts include: • Avoid GRE sequences (which are prone to susceptibility artifacts); use FSE sequences with short echo times instead • Lengthen ETL, increase receiver bandwidth, decrease TE and voxel size • Use STIR and Dixon sequences; these will reduce artifact relative to CHESS sequences and provide more homogeneous fat suppression • Consider proprietary metal artifact reduction sequences (SEMAC, MAVRIC) Metal artifact is more pronounced on transverse GRE MR image of shoulder (arrows, left) than on FSE image (right). STIR MR image (left) shows more homogeneous fat suppression than CHESS image (right) of patient with total knee arthroplasty (arrow, prosthetic tibial stem). Coronal STIR MR image of knee in patient with arthroplasty shows signal distortion (left), which is markedly reduced on MAVRIC metal artifact reduction sequence (right).
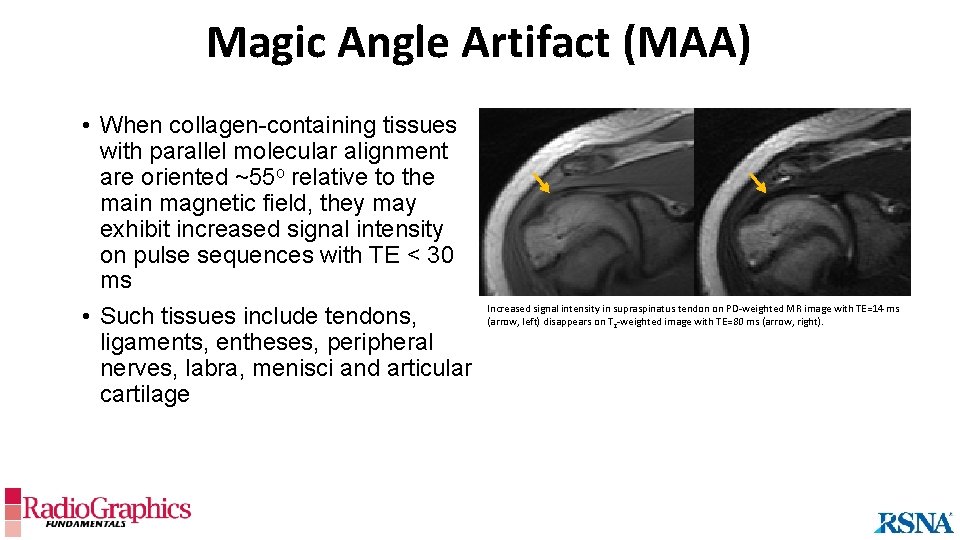
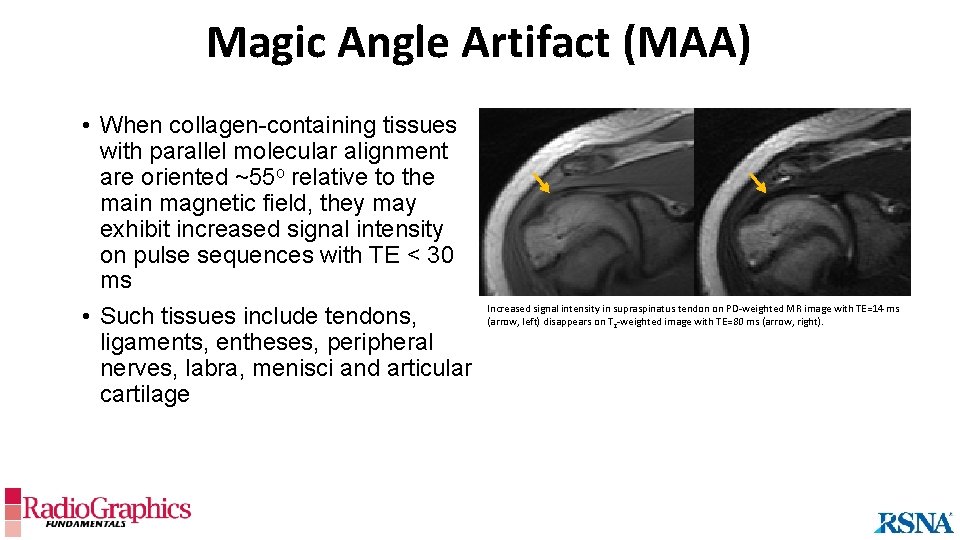
Magic Angle Artifact (MAA) • When collagen-containing tissues with parallel molecular alignment are oriented ~55 o relative to the main magnetic field, they may exhibit increased signal intensity on pulse sequences with TE < 30 ms • Such tissues include tendons, ligaments, entheses, peripheral nerves, labra, menisci and articular cartilage Increased signal intensity in supraspinatus tendon on PD-weighted MR image with TE=14 ms (arrow, left) disappears on T 2 -weighted image with TE=80 ms (arrow, right).
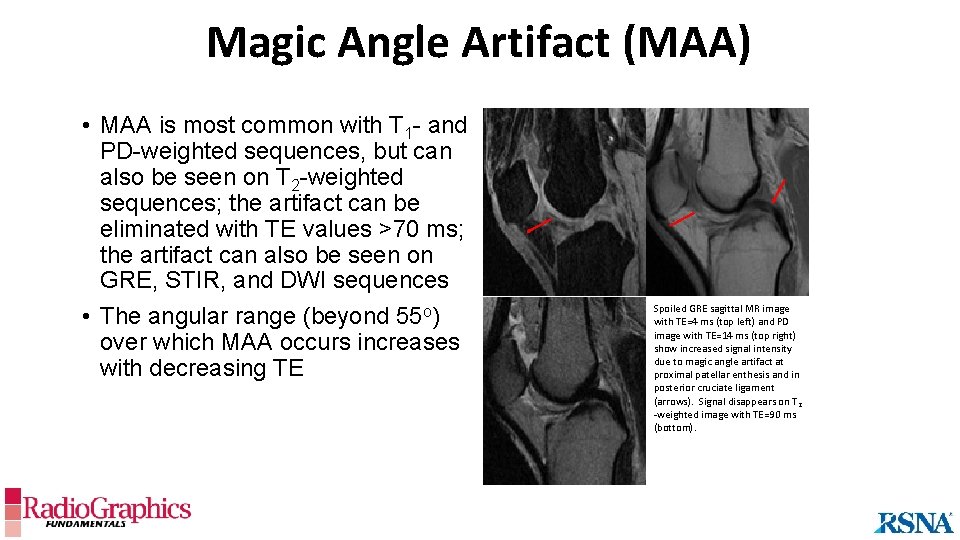
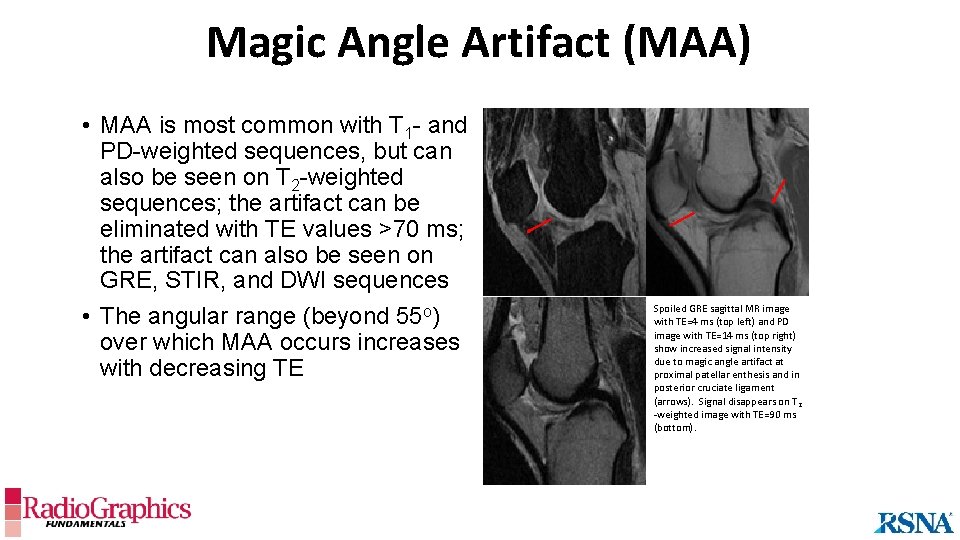
Magic Angle Artifact (MAA) • MAA is most common with T 1 - and PD-weighted sequences, but can also be seen on T 2 -weighted sequences; the artifact can be eliminated with TE values >70 ms; the artifact can also be seen on GRE, STIR, and DWI sequences • The angular range (beyond 55 o) over which MAA occurs increases with decreasing TE Spoiled GRE sagittal MR image with TE=4 ms (top left) and PD image with TE=14 ms (top right) show increased signal intensity due to magic angle artifact at proximal patellar enthesis and in posterior cruciate ligament (arrows). Signal disappears on T 2 -weighted image with TE=90 ms (bottom).
In Conclusion • A basic knowledge of MR pulse sequences is essential for planning diagnostic musculoskeletal magnetic resonance imaging examinations • Understanding fundamental MR physics allows better appreciation of the properties of various pulse sequences and methods of fat suppression • Fast/turbo spin echo pulse sequences remain the most common pulse sequences used in typical MSK MR imaging protocols; however, gradient echo pulse sequences have the advantage of rapid acquisition and therefore are frequently used to create 3 D datasets • Chemical shift selective fat saturation is a commonly used method of fat suppression, but is more sensitive to magnetic field heterogeneity than inversion-based techniques
In Conclusion • Some artifacts, such as motion artifacts, susceptibility artifacts, and magic angle artifacts, are dependent upon the pulse sequence used; these artifacts often can be minimized with forethought • We hope that this presentation has served as a useful introduction and/or review for residents and fellows studying musculoskeletal MRI
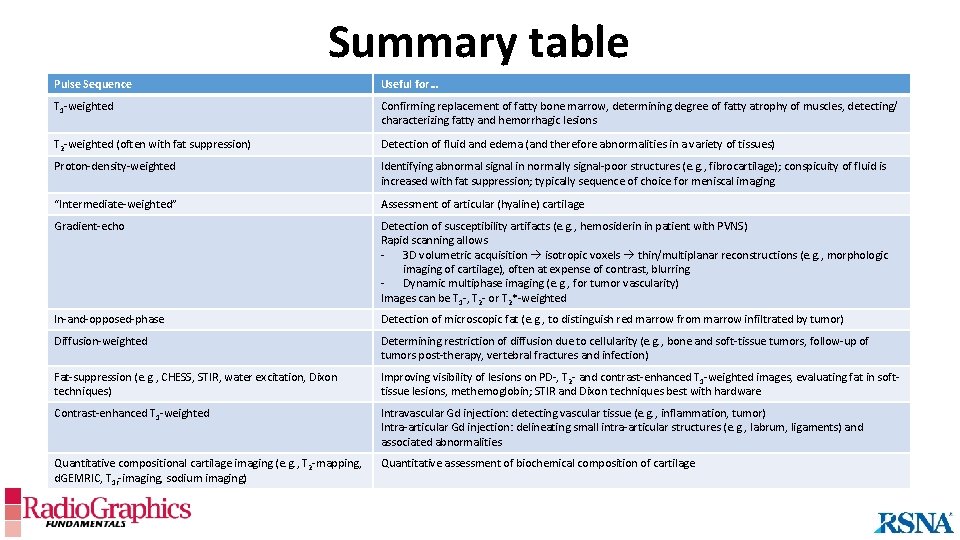
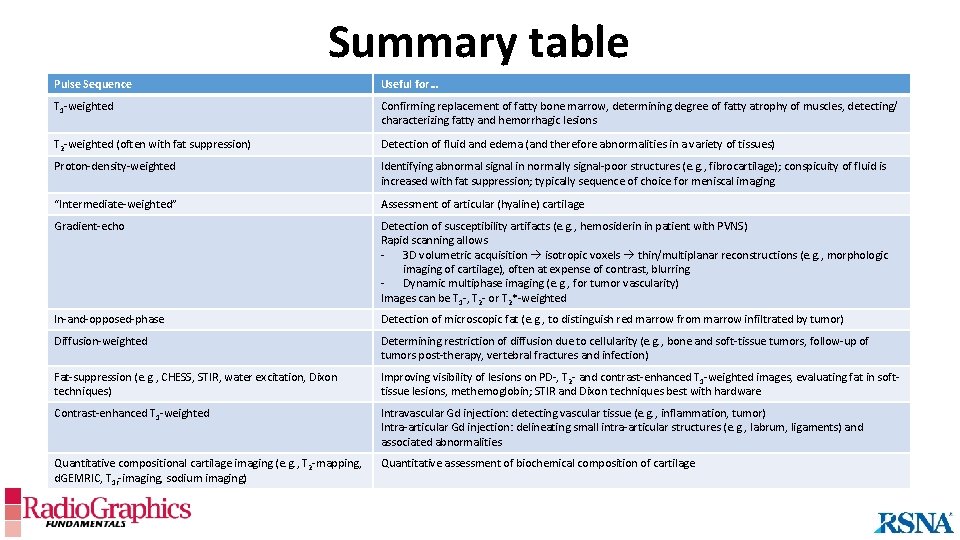
Summary table Pulse Sequence Useful for… T 1 -weighted Confirming replacement of fatty bone marrow, determining degree of fatty atrophy of muscles, detecting/ characterizing fatty and hemorrhagic lesions T 2 -weighted (often with fat suppression) Detection of fluid and edema (and therefore abnormalities in a variety of tissues) Proton-density-weighted Identifying abnormal signal in normally signal-poor structures (e. g. , fibrocartilage); conspicuity of fluid is increased with fat suppression; typically sequence of choice for meniscal imaging “Intermediate-weighted” Assessment of articular (hyaline) cartilage Gradient-echo Detection of susceptibility artifacts (e. g. , hemosiderin in patient with PVNS) Rapid scanning allows - 3 D volumetric acquisition isotropic voxels thin/multiplanar reconstructions (e. g. , morphologic imaging of cartilage), often at expense of contrast, blurring - Dynamic multiphase imaging (e. g. , for tumor vascularity) Images can be T 1 -, T 2 - or T 2*-weighted In-and-opposed-phase Detection of microscopic fat (e. g. , to distinguish red marrow from marrow infiltrated by tumor) Diffusion-weighted Determining restriction of diffusion due to cellularity (e. g. , bone and soft-tissue tumors, follow-up of tumors post-therapy, vertebral fractures and infection) Fat-suppression (e. g. , CHESS, STIR, water excitation, Dixon techniques) Improving visibility of lesions on PD-, T 2 - and contrast-enhanced T 1 -weighted images, evaluating fat in softtissue lesions, methemoglobin; STIR and Dixon techniques best with hardware Contrast-enhanced T 1 -weighted Intravascular Gd injection: detecting vascular tissue (e. g. , inflammation, tumor) Intra-articular Gd injection: delineating small intra-articular structures (e. g. , labrum, ligaments) and associated abnormalities Quantitative compositional cartilage imaging (e. g. , T 2 -mapping, d. GEMRIC, T 1 r-imaging, sodium imaging) Quantitative assessment of biochemical composition of cartilage
Suggested Readings • • • • • • Berger A. Magnetic resonance imaging. BMJ 2002; 324: 35. Bitar R et al. MR pulse sequences: what every radiologist wants to know but is afraid to ask. Radiographics. 2006; 265: 13 -37 Chavhan GB. Appropriate selection of MRI sequences for common scenarios in clinical practice. Pediatr Radiol 2016; 46: 740 -747 Chavhan GB et al. Steady-state MR imaging sequences: physics, classification, and clinical applications. Radio. Graphics 2008; 28: 1147 -1160 Chen et al. Cartilage morphology at 3. 0 T: assessment of three-dimensional magnetic resonance imaging techniques. J Magn Reson Imaging 2010; 32: 173 -183 Crema et al. Articular cartilage in the knee: current MR imaging techniques and applications in clinical practice and research. Radio. Graphics 2011; 31: 37 -62 Del Grande F et al. Fat-suppression techniques for 3 -T MR imaging of the musculoskeletal system. Radio. Graphics 2014; 34: 217 -233 Del Grande F et al. Bone marrow lesions: A systematic diagnostic approach. Indian J Radiol Imaging. 2014 Jul-Sep; 24(3): 279– 287. Elster AD. Gradient-echo MR imaging: techniques and acronyms. Radiology 1993; 186: 1 -8 Gold et al. Recent advances in MRI of articular cartilage. AJR 2009; 193: 628 -638 Hargreaves BA. Rapid gradient-echo imaging. J Magn Reson Imaging 2012; 36: 1300 -1313 Hesper T et al. T 2* mapping for articular cartilage assessment: principles, current applications, and future prospects. Skeletal Radiol 2014; 43: 1429 -1445. Huda W. (2016) Review of radiologic physics. LWW. Link TM. MR imaging in osteoarthritis: hardware, coils, and sequences. Magn Reson Imaging Clin N Am 2010; 18: 95 -110 Morelli JN et al. An Image-based Approach to Understanding the Physics of MR Artifacts. Radiographics. 2011 31: 849 -66 Pezeshk P et al. Role of chemical shift and Dixon based techniques in musculoskeletal MR imaging. Eur J Radiol 2017; 94: 93 -100. Pooley RA. AAPM/RSNA physics tutorial for residents: fundamental physics of MR imaging. Radiographics 2005; 25: 1087 -99. Richardson ML et al. Some new angles on the magic angle: what MSK radiologists know and don’t know about this phenomenon. Skeletal Radiol 2018; 47: 1673 -1681 Schild HH. (1994) MRI made easy (…well almost). Berlex Laboratories. Shakoor D et al. Diagnosis of knee meniscal injuries by using three-dimensional MRI: a systematic review and meta-analysis of diagnostic performance. Radiology 2019; 290: 435 -445 Singh DR et al. Artifacts in musculoskeletal MR imaging. Semin Musculoskelet Radiol 2014; 18: 12 -22 Tanitame N et al. Clinical utility of optimized three-dimensional T 1 -, T 2 -, and T 2*-weighted sequences in spinal magnetic resonance imaging. Jpn J Radiol 2017; 35: 135 -144 We also suggest the web site www. mriquestions. com by Allen D. Elster (© 2018) as a comprehensive but easily digestible resource for material pertaining to general MRI physics.