Muscles Muscle Tissue Chapter 10 Functions of Skeletal



















- Slides: 140
Muscles &Muscle Tissue Chapter 10
Functions of Skeletal Muscles 1. 2. 3. 4. 5. Produce skeletal movement Maintain body position Support soft tissues Guard body openings Maintain body temperature
Functional Characteristics of Muscle • Excitability (irritability) – Can receive and respond to stimuli. • Stimuli can include nerve impulses, stretch, hormones or changes in the chemical environment. • Contractility – the ability to shorten with increasing tension. • Extensibility – the ability to stretch. • Elasticity – the ability to snap back (recoil) to their resting length after being stretched.
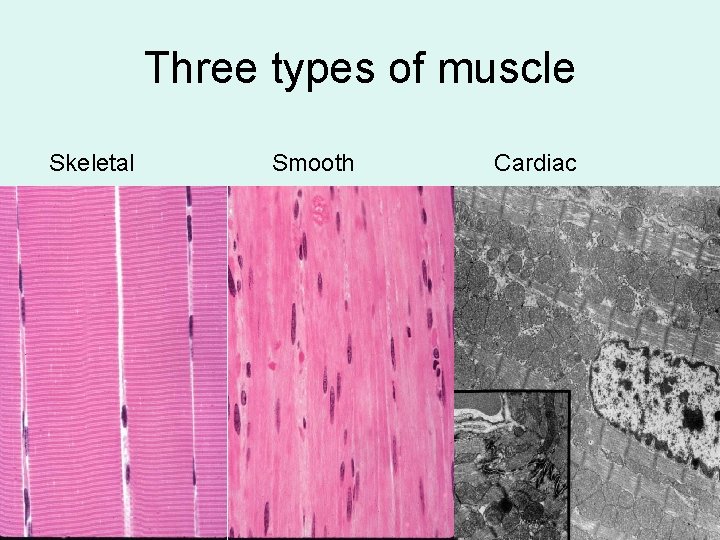
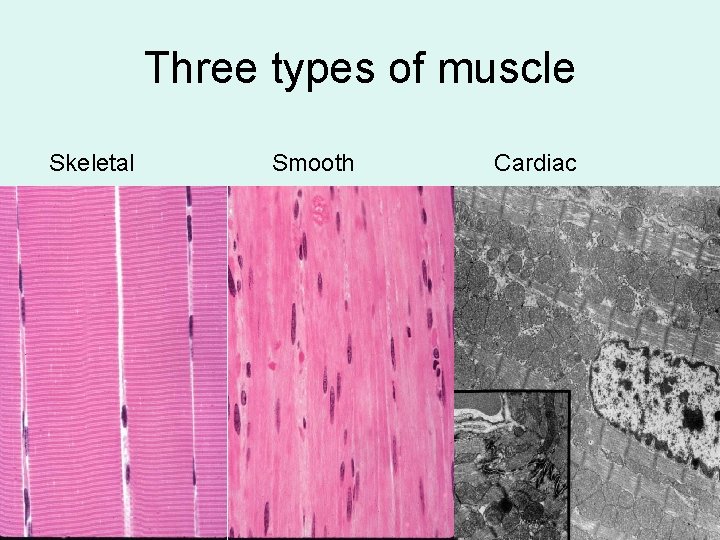
Three types of muscle Skeletal Smooth Cardiac

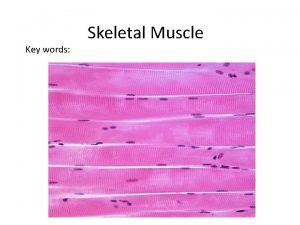
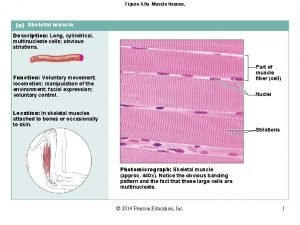
Characteristics of Skeletal Muscle • • Striated Multinucleate (it is a syncytium) Voluntary Parallel fibers
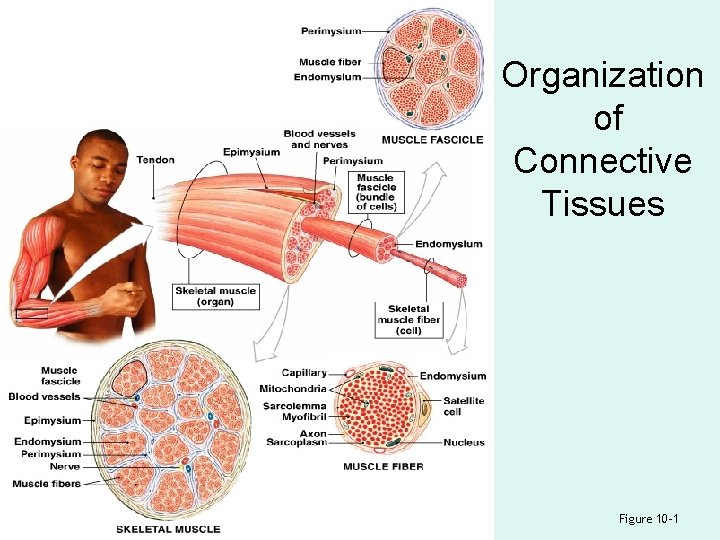
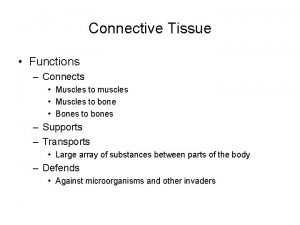
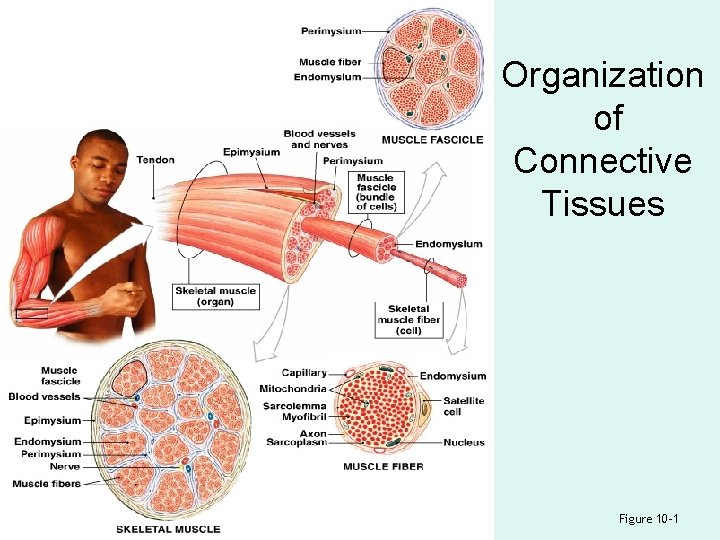
Organization of Connective Tissues Figure 10– 1
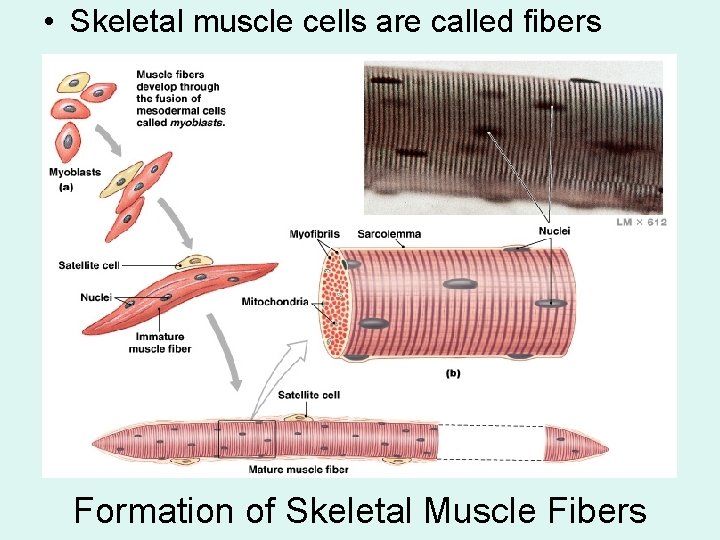
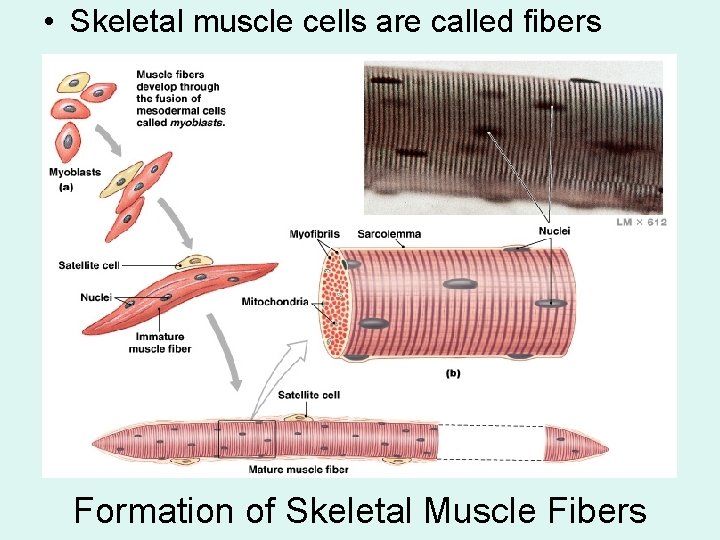
• Skeletal muscle cells are called fibers Formation of Skeletal Muscle Fibers
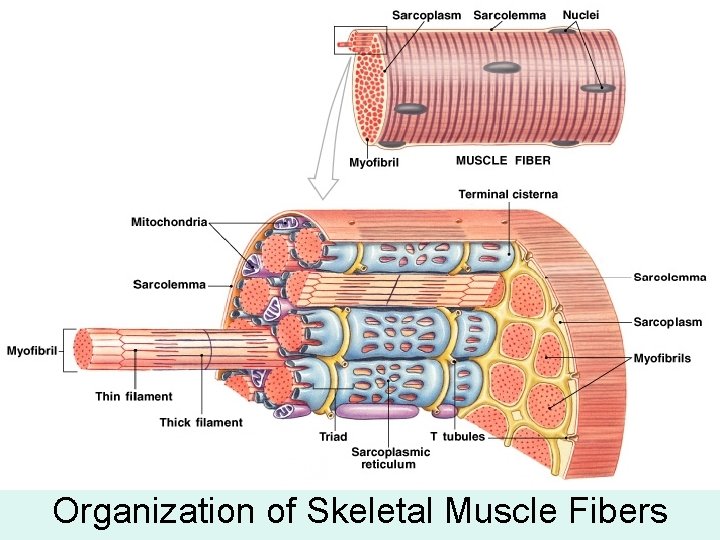
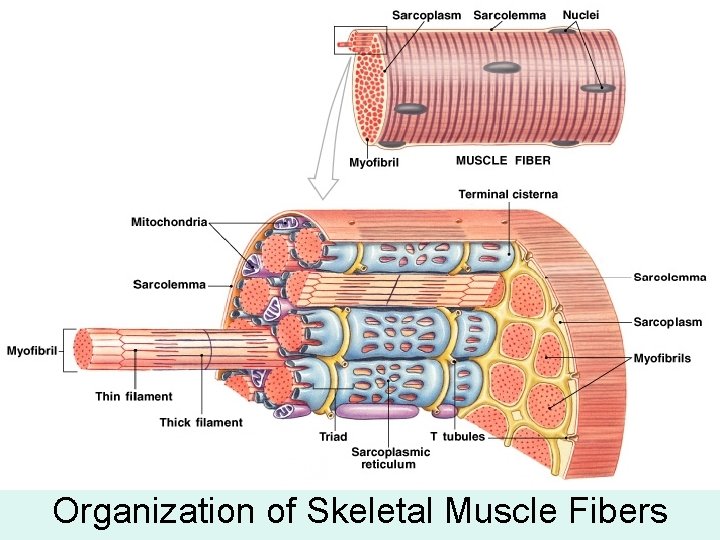
Organization of Skeletal Muscle Fibers
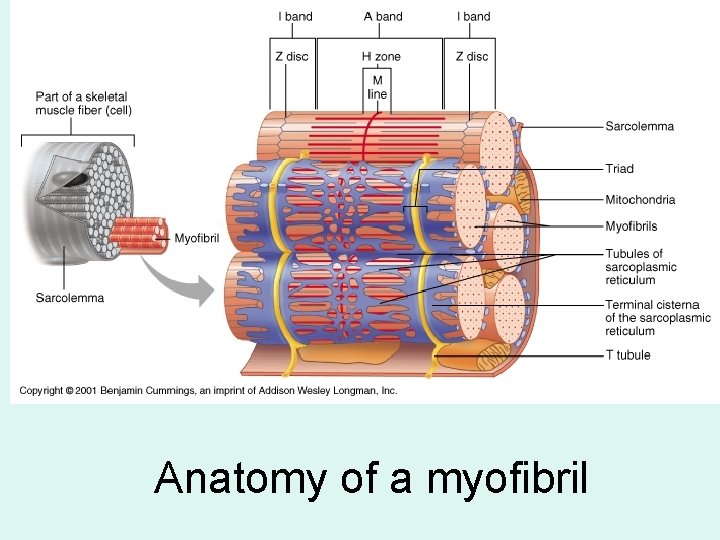
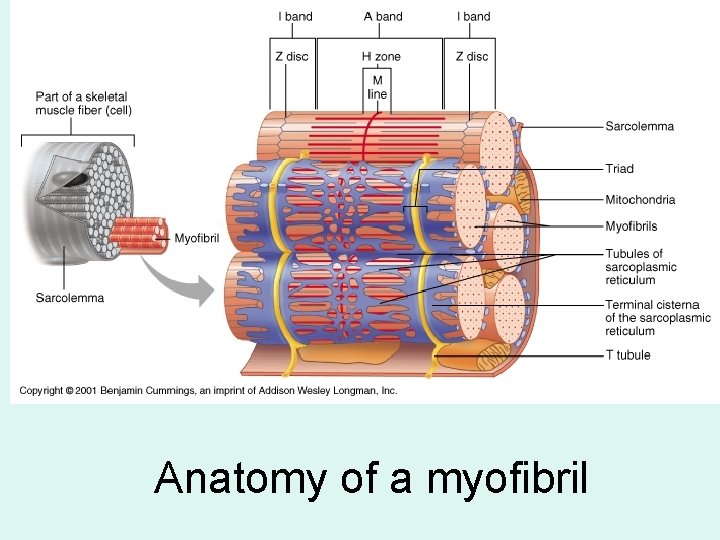
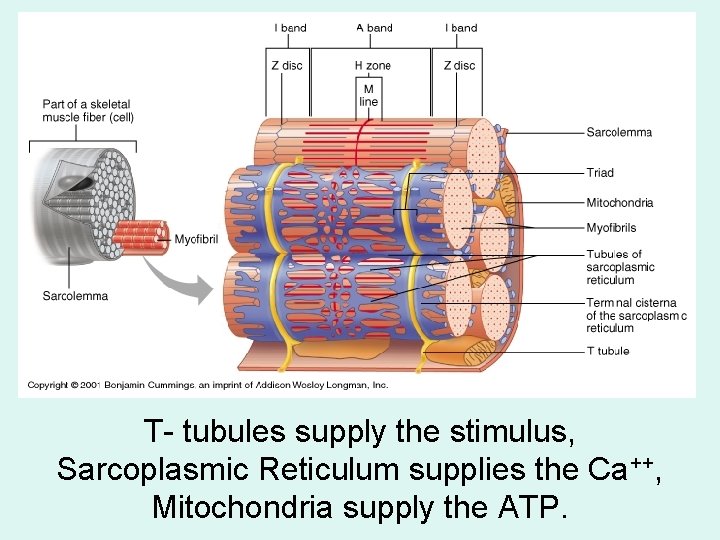
Anatomy of a myofibril
A Triad • Is formed by 1 T tubule and 2 terminal cisternae

Sarcomeres Figure 10– 4

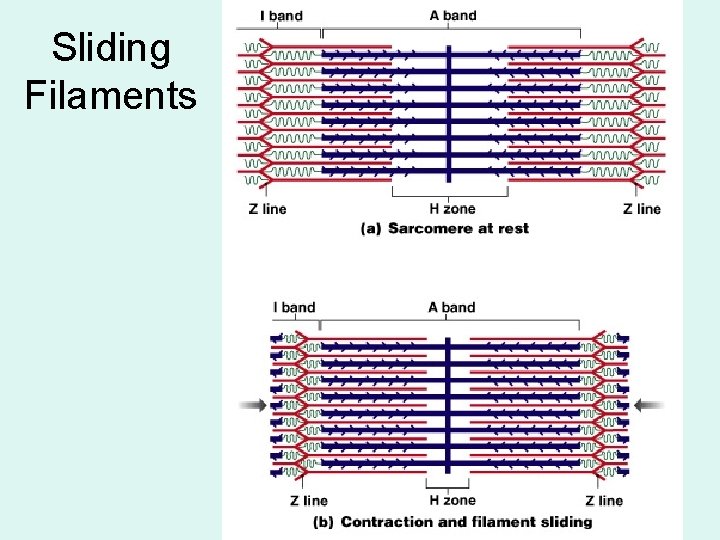
Muscle Striations • A striped or striated pattern within myofibrils: – alternating dark, thick filaments (A bands) and light, thin filaments (I bands)
M Lines and Z Lines • M line: – the center of the A band – at midline of sarcomere • Z lines: – the centers of the I bands – at 2 ends of sarcomere
Zone of Overlap • The densest, darkest area on a light micrograph • Where thick and thin filaments overlap
The H Zone • The area around the M line • Has thick filaments but no thin filaments
Titin • Are strands of protein • Reach from tips of thick filaments to the Z line • Stabilize the filaments

Sarcomere Structure

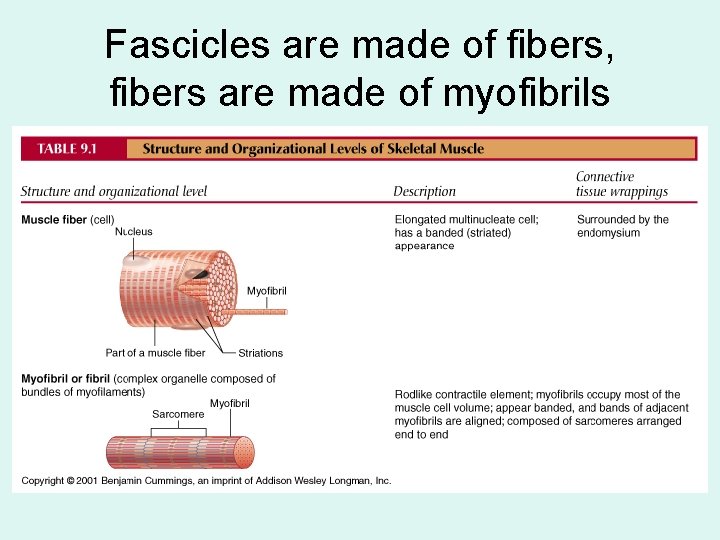
Summary of skeletal muscle anatomy: muscles are made of fascicles
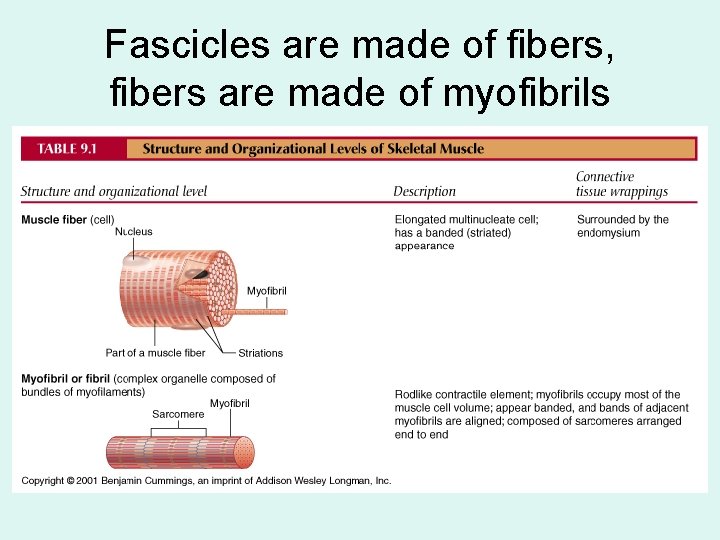
Fascicles are made of fibers, fibers are made of myofibrils
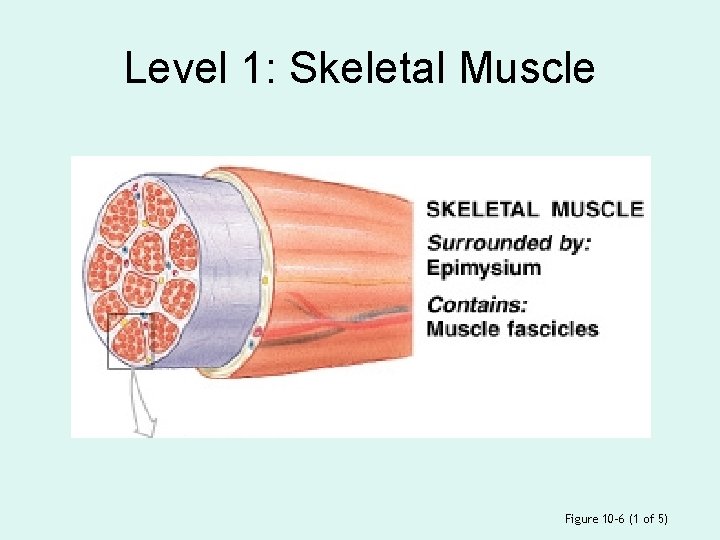
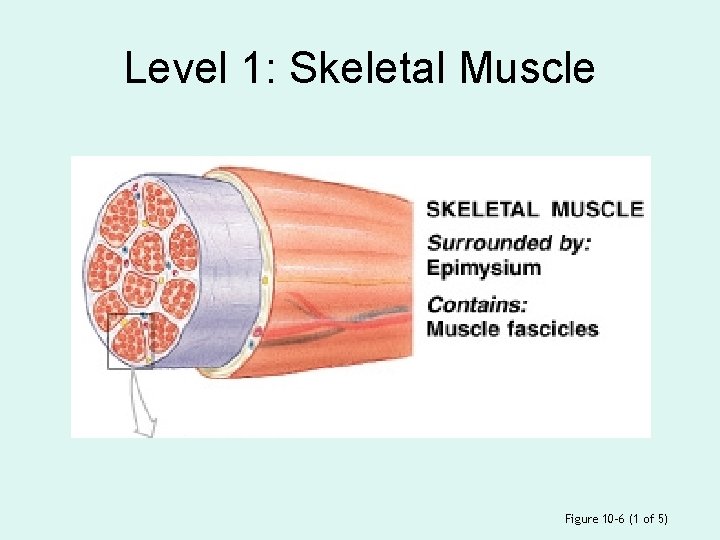
Level 1: Skeletal Muscle Figure 10– 6 (1 of 5)
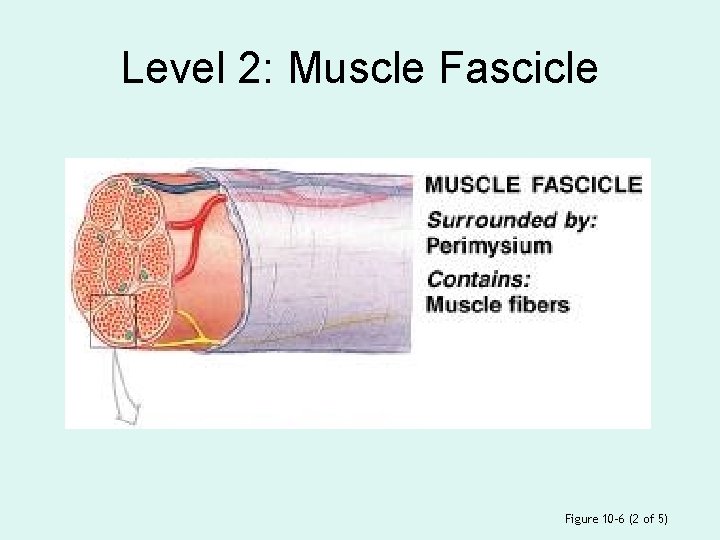
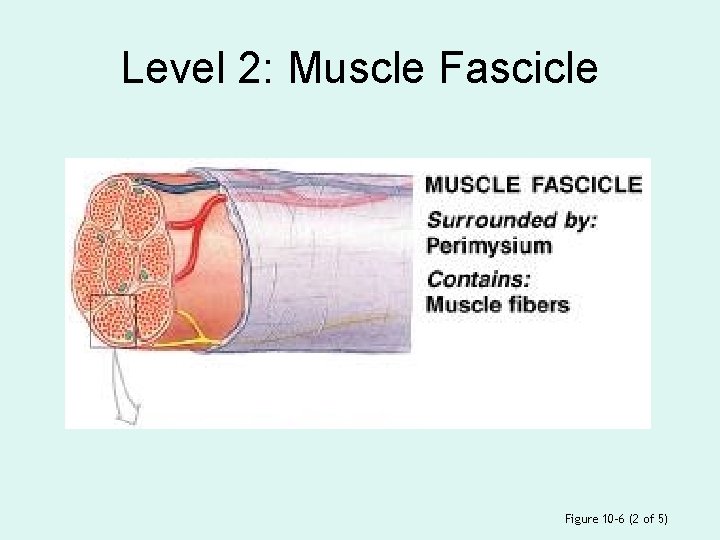
Level 2: Muscle Fascicle Figure 10– 6 (2 of 5)
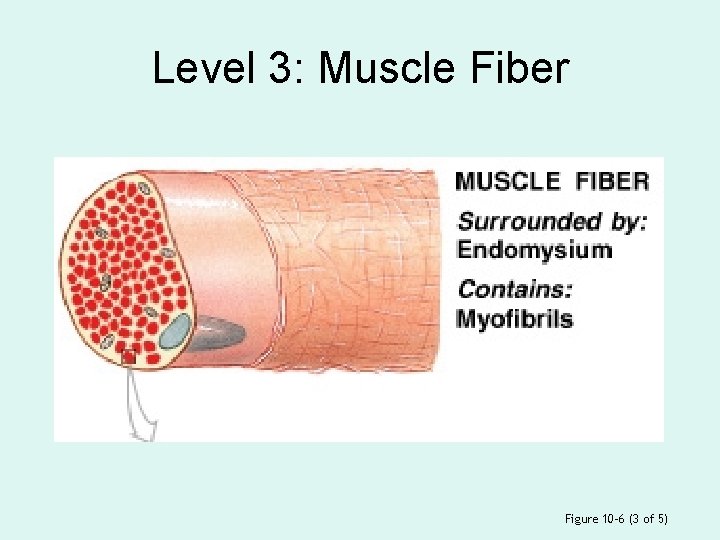
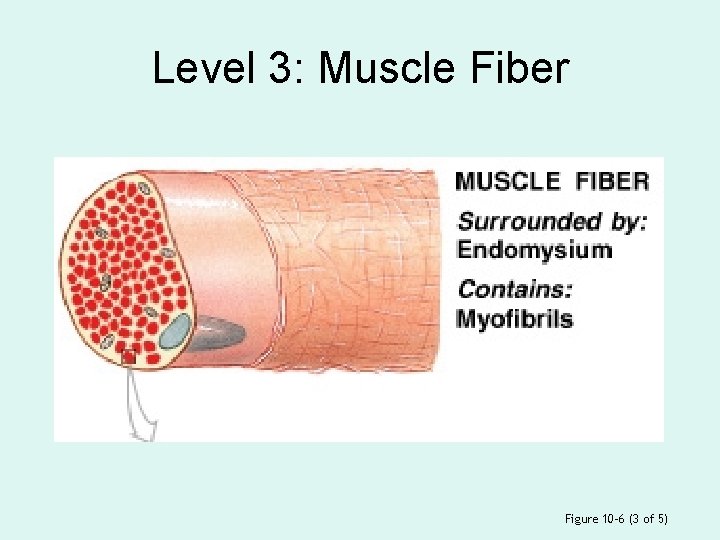
Level 3: Muscle Fiber Figure 10– 6 (3 of 5)
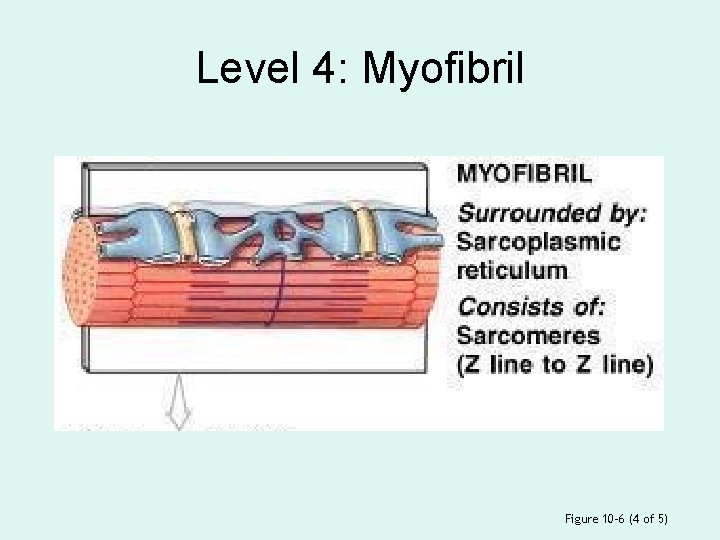
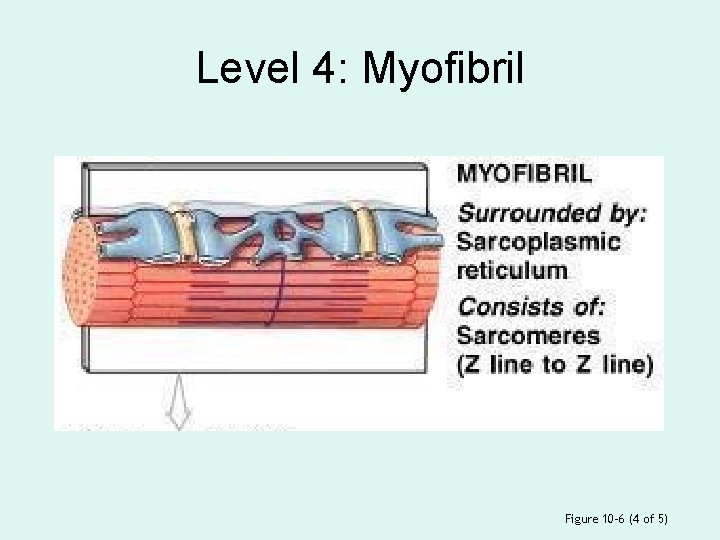
Level 4: Myofibril Figure 10– 6 (4 of 5)

Level 5: Sarcomere Figure 10– 6 (5 of 5)
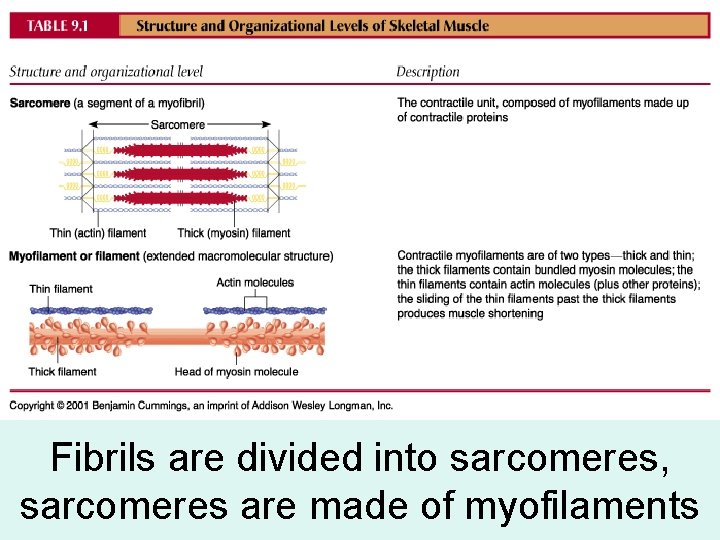
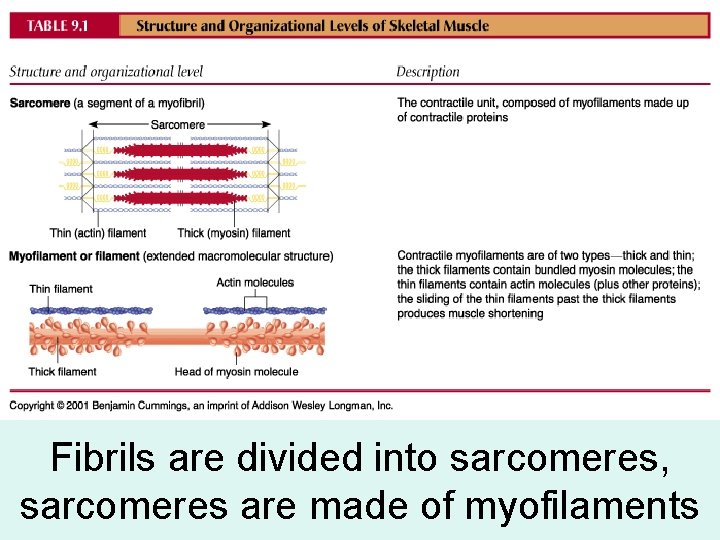
Fibrils are divided into sarcomeres, sarcomeres are made of myofilaments
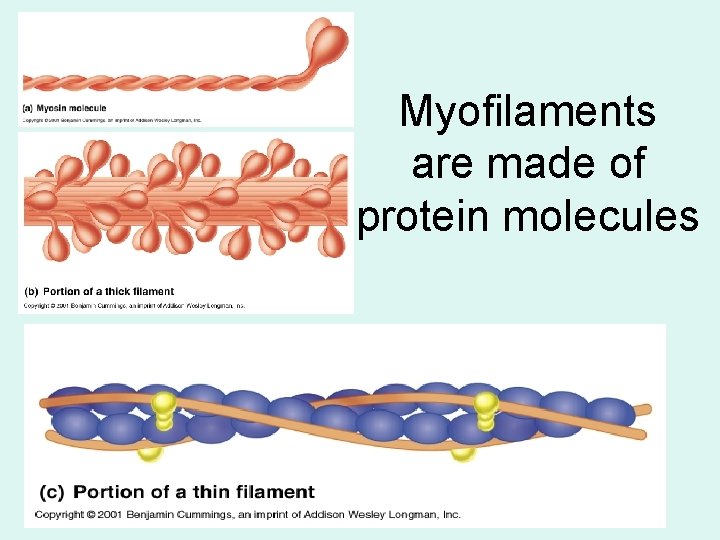
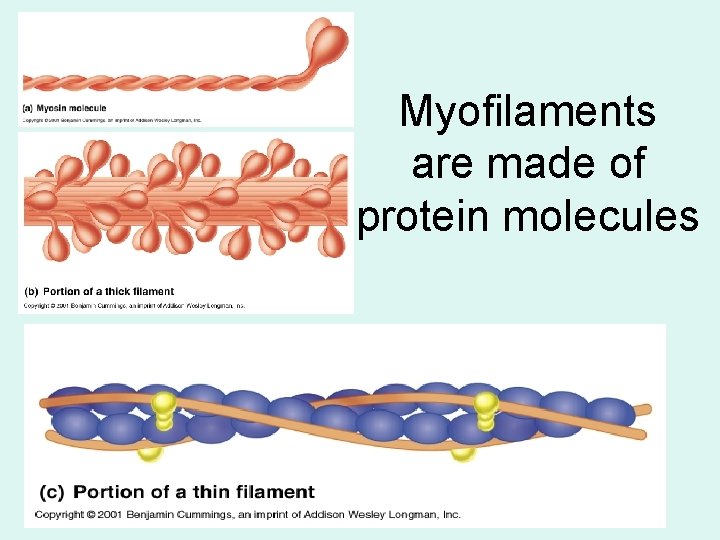
Myofilaments are made of protein molecules
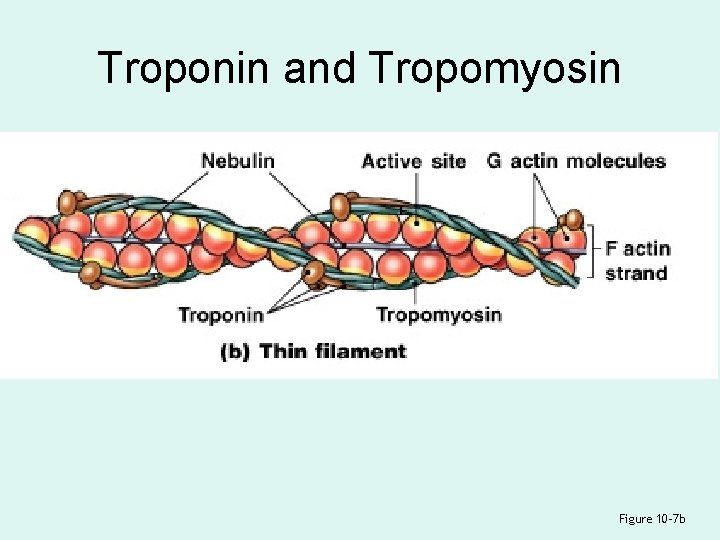
A Thin Filament
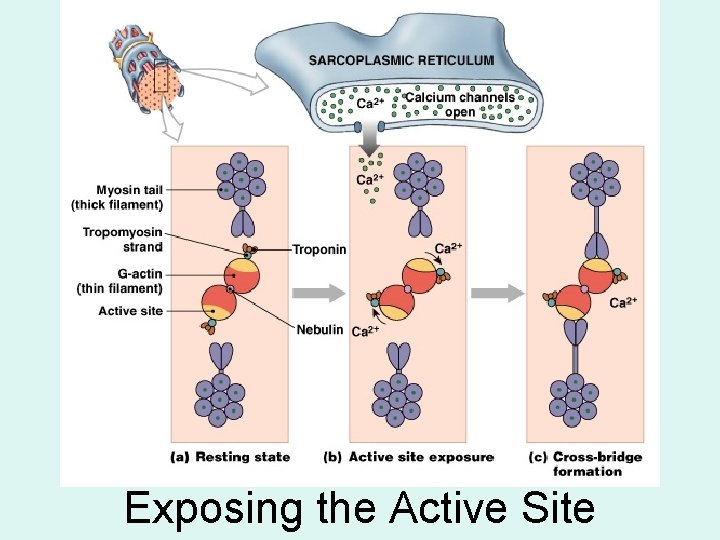
4 Thin Filament Proteins 1. F actin: – is 2 twisted rows of globular G actin – the active sites on G actin strands bind to myosin
4 Thin Filament Proteins 2. Nebulin: – holds F actin strands together
4 Thin Filament Proteins 3. Tropomyosin: – is a double strand – prevents actin–myosin interaction
4 Thin Filament Proteins 4. Troponin: – a globular protein – binds tropomyosin to G actin – controlled by Ca 2+
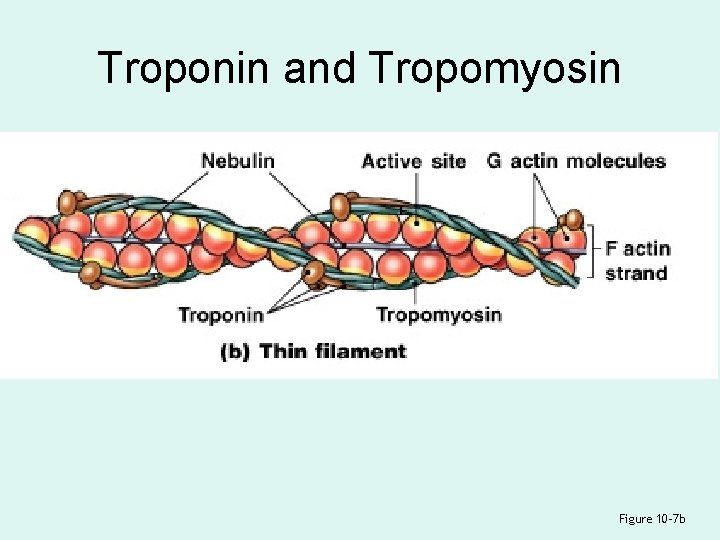
Troponin and Tropomyosin Figure 10– 7 b
A Thick Filament Figure 10– 7 c
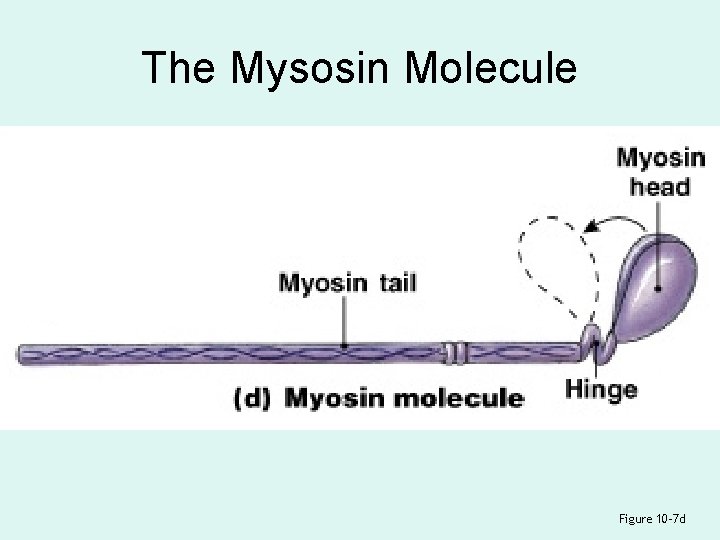
Thick Filaments • Contain twisted myosin subunits • Contain titin strands that recoil after stretching
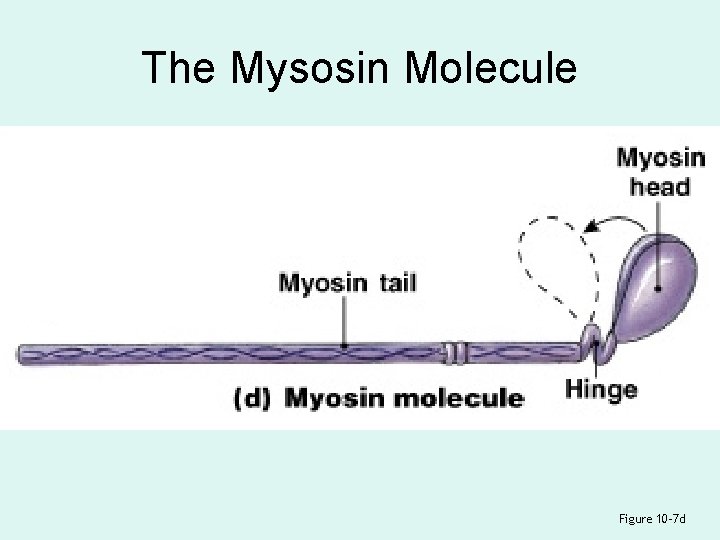
The Mysosin Molecule Figure 10– 7 d
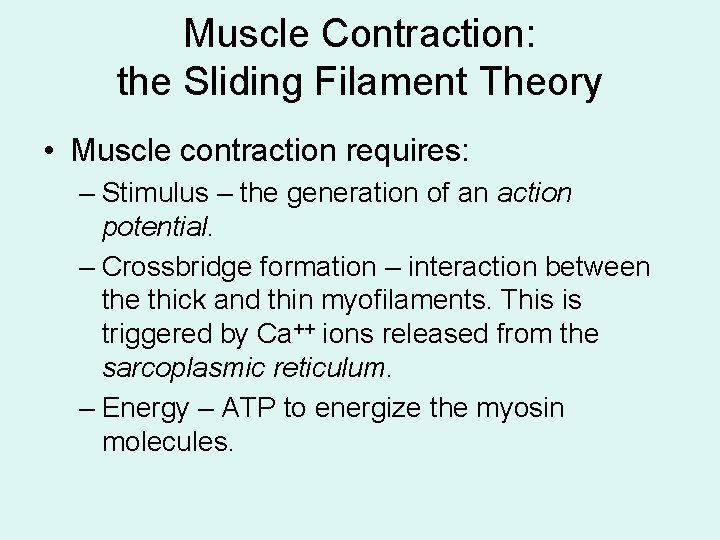
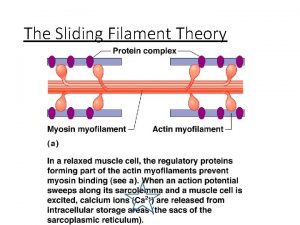
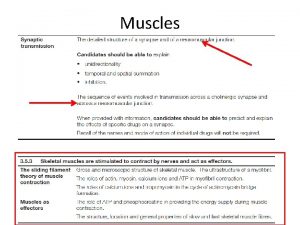
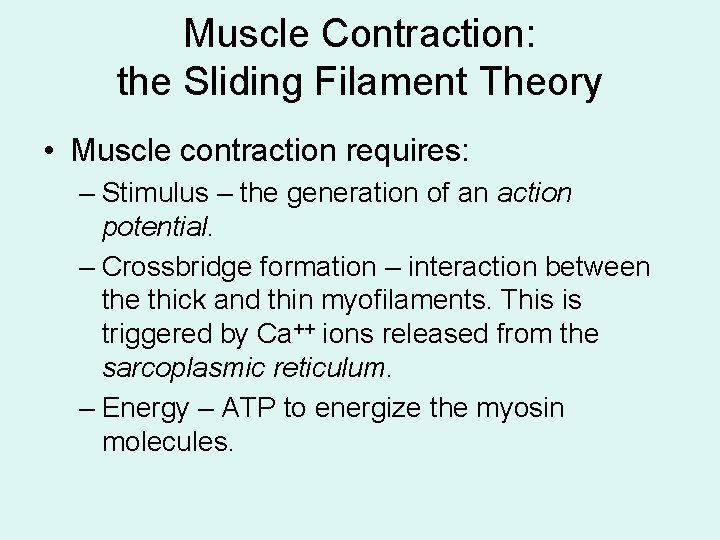
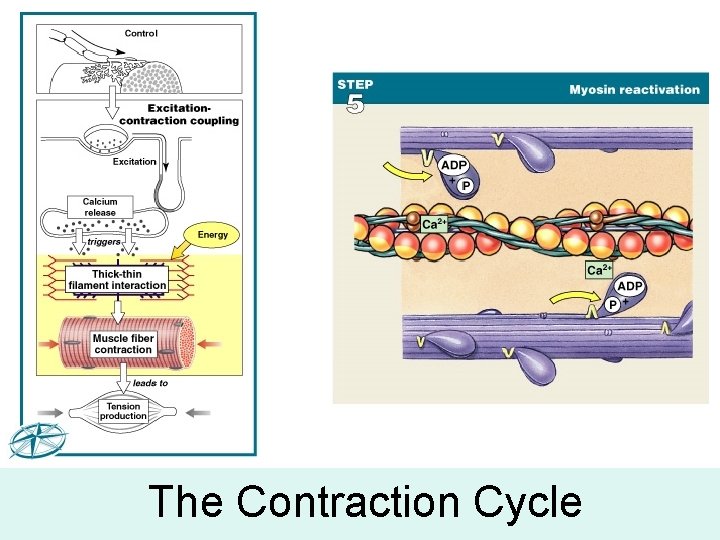
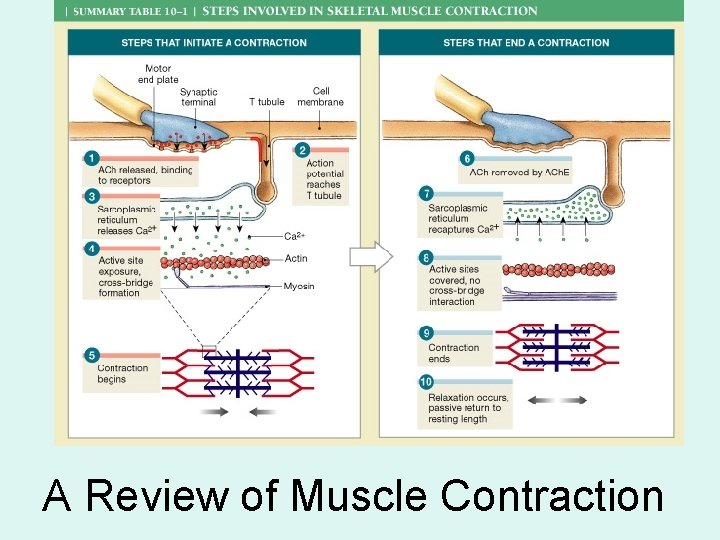
Muscle Contraction: the Sliding Filament Theory • Muscle contraction requires: – Stimulus – the generation of an action potential. – Crossbridge formation – interaction between the thick and thin myofilaments. This is triggered by Ca++ ions released from the sarcoplasmic reticulum. – Energy – ATP to energize the myosin molecules.
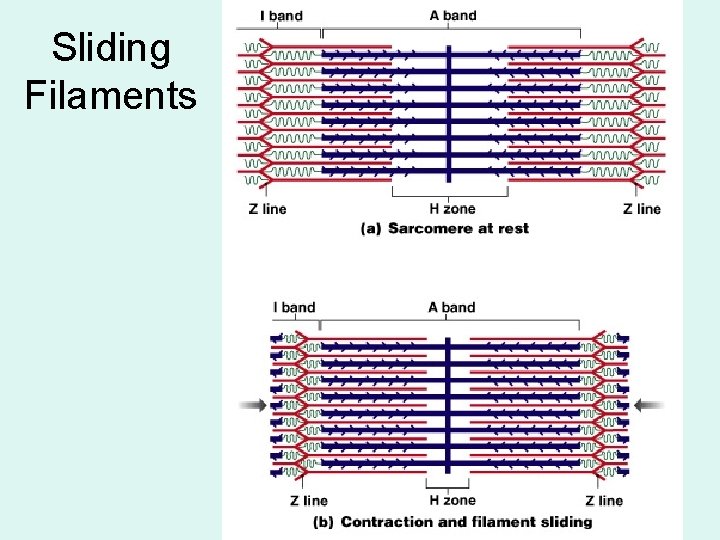
Sliding Filaments
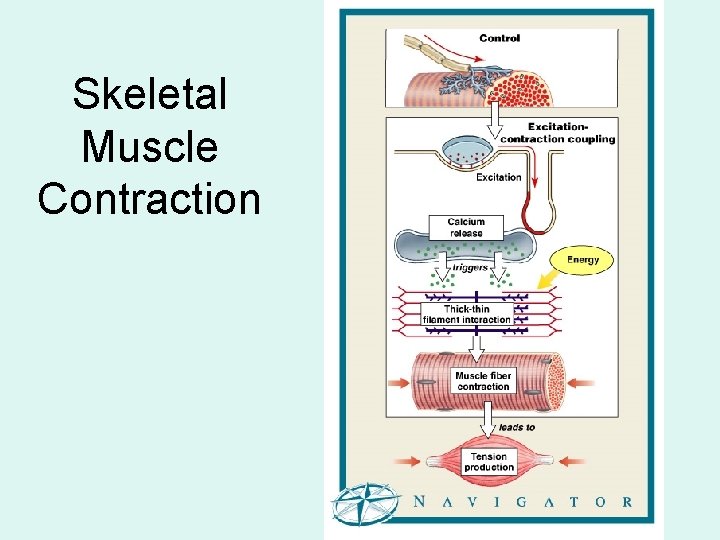
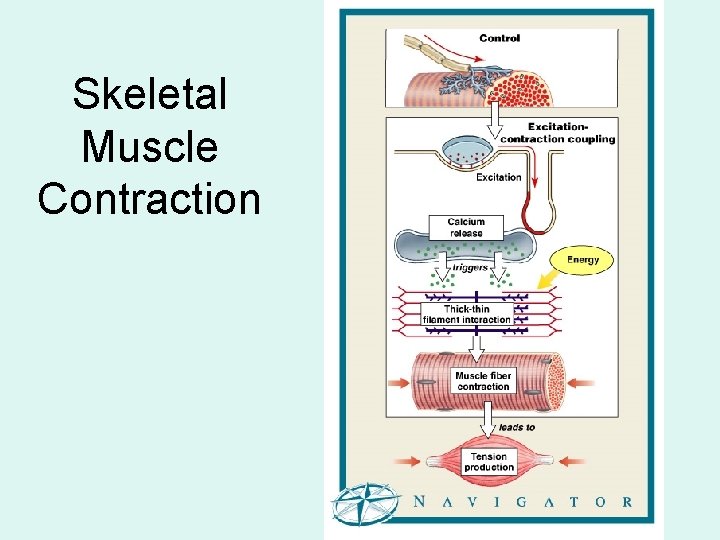
Skeletal Muscle Contraction
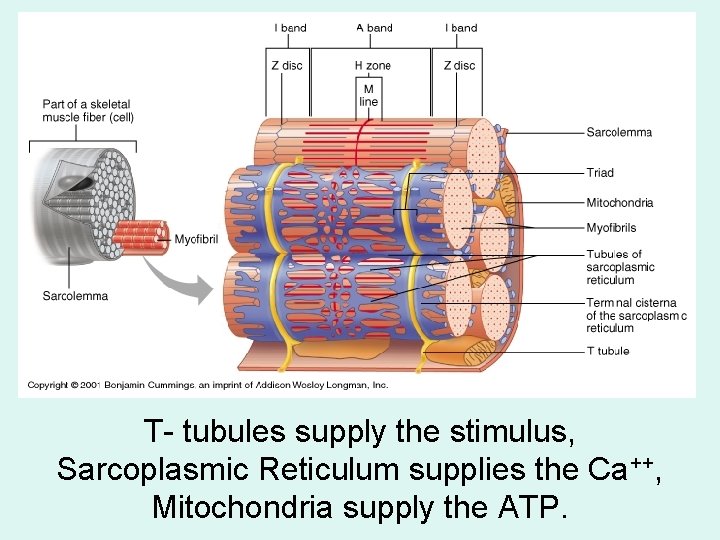
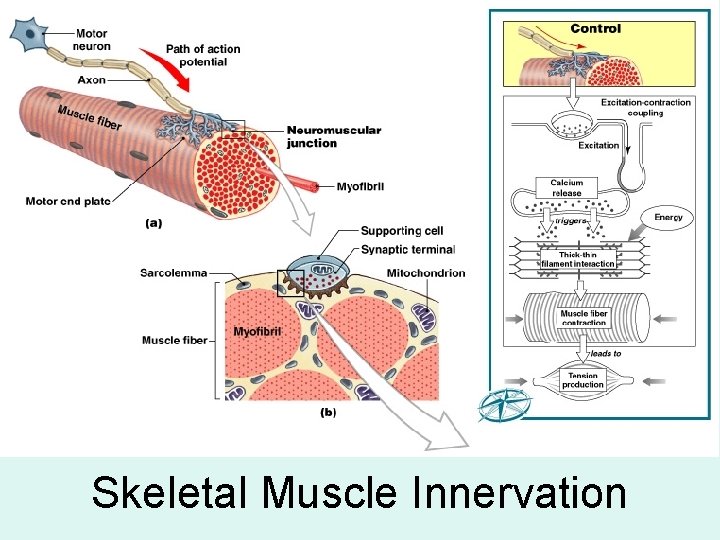
T- tubules supply the stimulus, Sarcoplasmic Reticulum supplies the Ca++, Mitochondria supply the ATP.
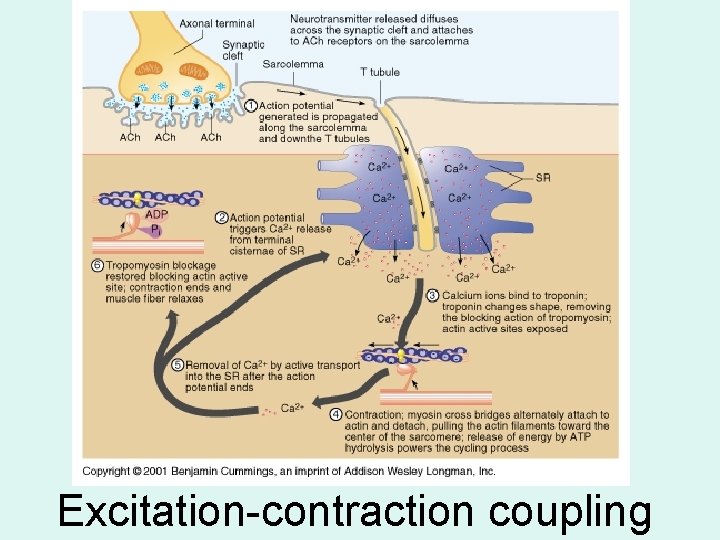
The Process of Contraction • Neural stimulation of sarcolemma: – causes excitation–contraction coupling • Cisternae of SR release Ca 2+: – which triggers interaction of thick and thin filaments – consuming ATP and producing tension
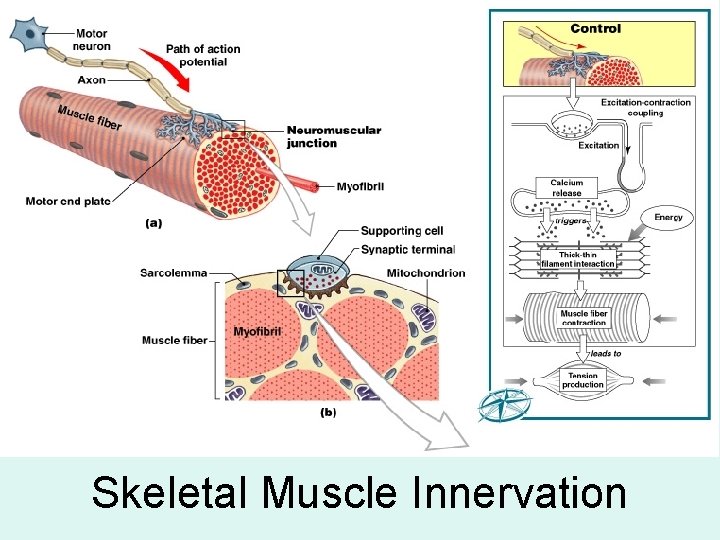
Skeletal Muscle Innervation

Skeletal Muscle Innervation Figure 10– 10 c
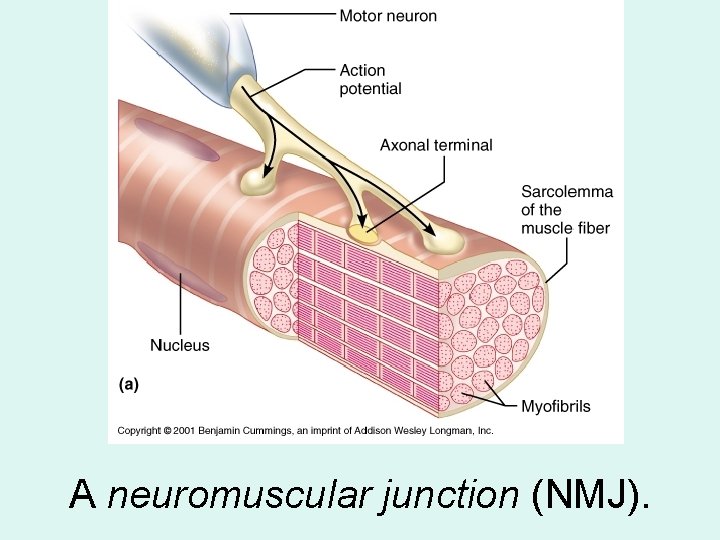
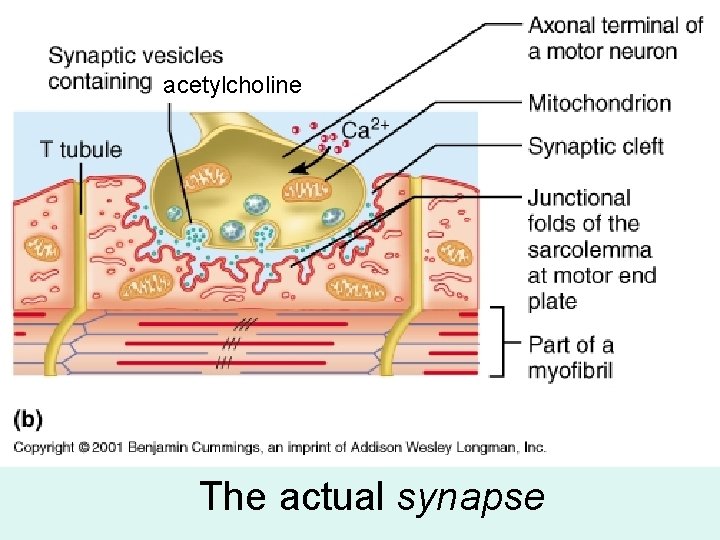
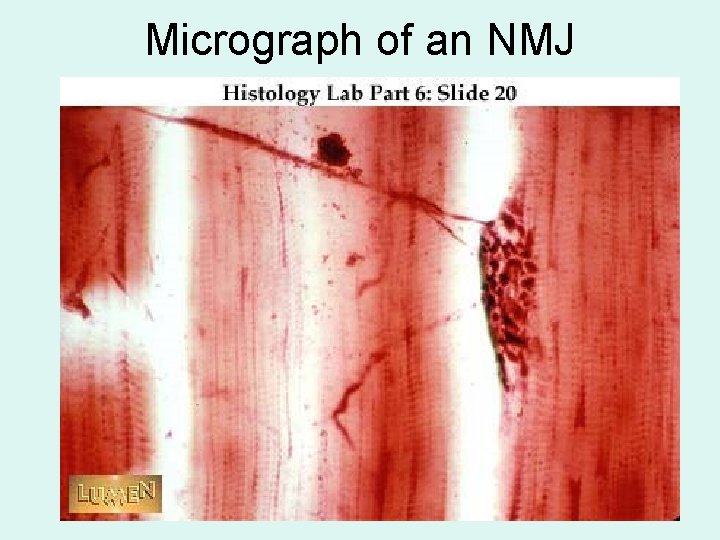
The Neuromuscular Junction • Is the location of neural stimulation • Action potential (electrical signal): – travels along nerve axon – ends at synaptic terminal
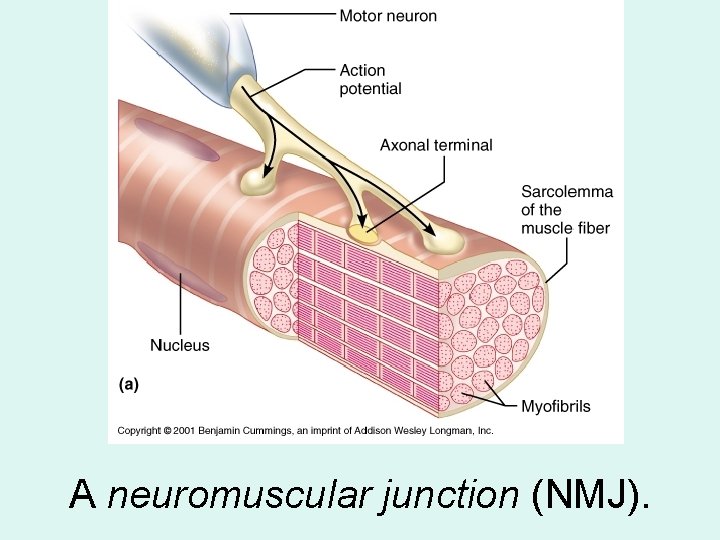
A neuromuscular junction (NMJ).
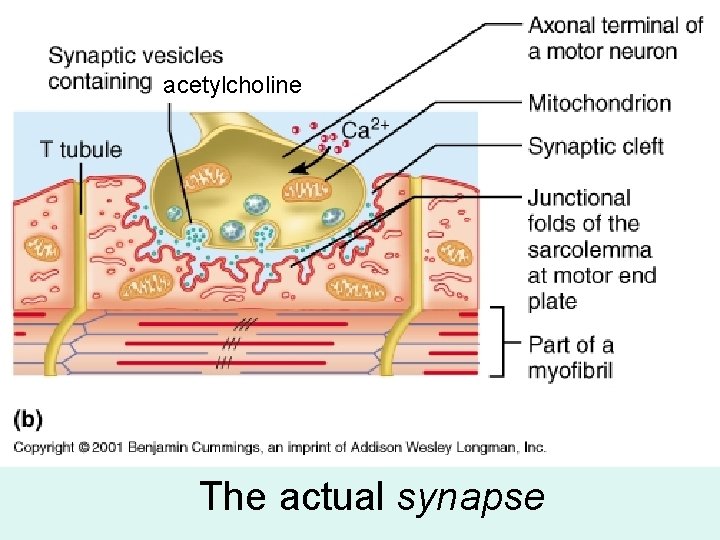
acetylcholine The actual synapse

Synaptic Terminal • Releases neurotransmitter (acetylcholine or ACh) • Into the synaptic cleft (gap between synaptic terminal and motor end plate)
The Neurotransmitter • Acetylcholine or ACh: – travels across the synaptic cleft – binds to membrane receptors on sarcolemma (motor end plate) – causes sodium–ion rush into sarcoplasm – is quickly broken down by enzyme (acetylcholinesterase or ACh. E)

Action Potential • Generated by increase in sodium ions in sarcolemma • Travels along the T tubules • Leads to excitation–contraction coupling
Excitation–Contraction Coupling • Action potential reaches a triad: – releasing Ca 2+ – triggering contraction • Requires myosin heads to be in “cocked” position: – loaded by ATP energy
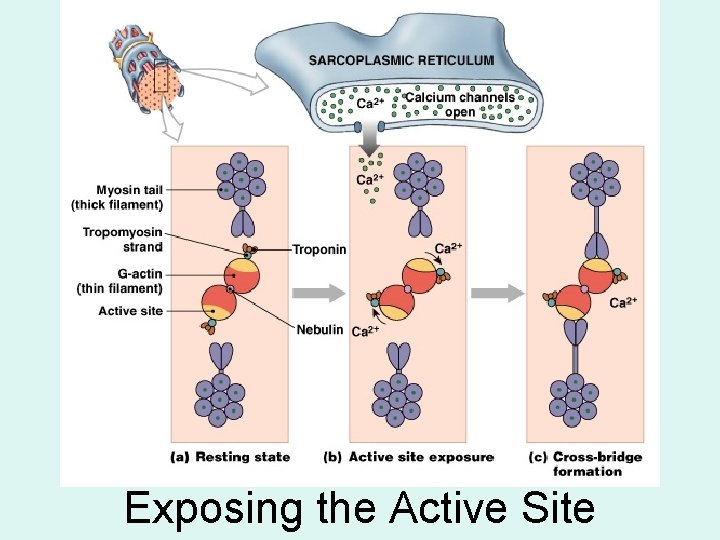
Exposing the Active Site
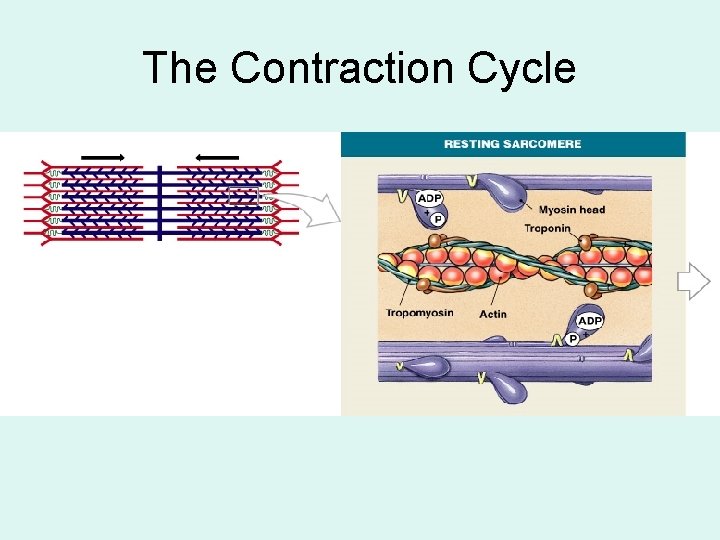
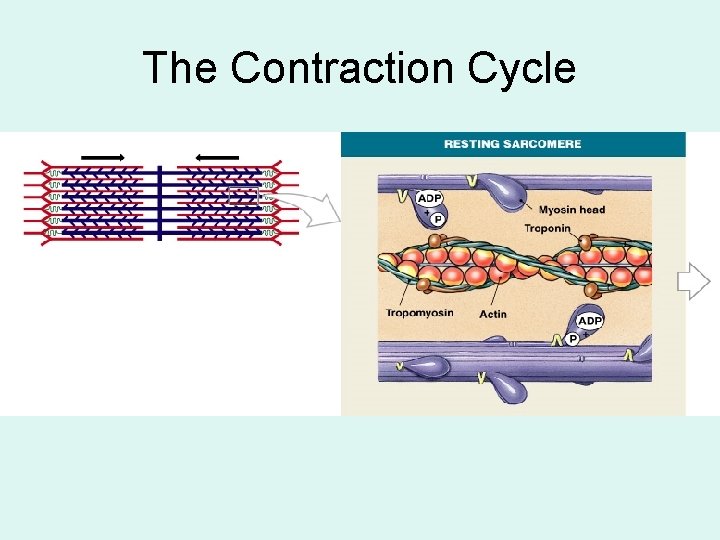
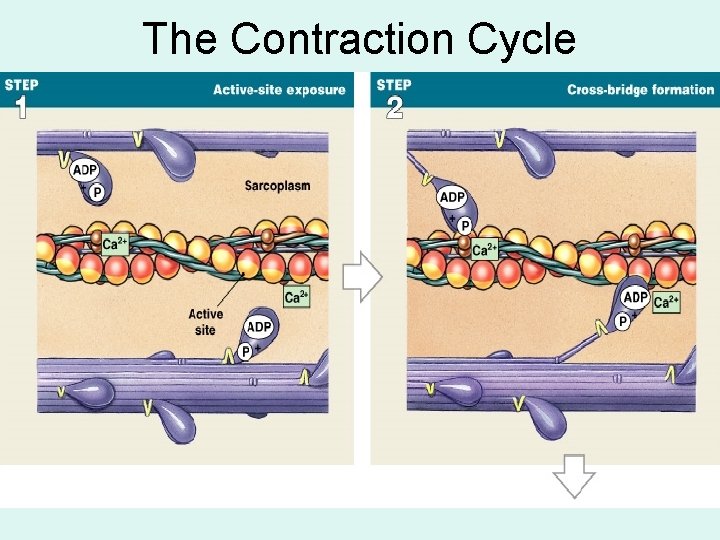
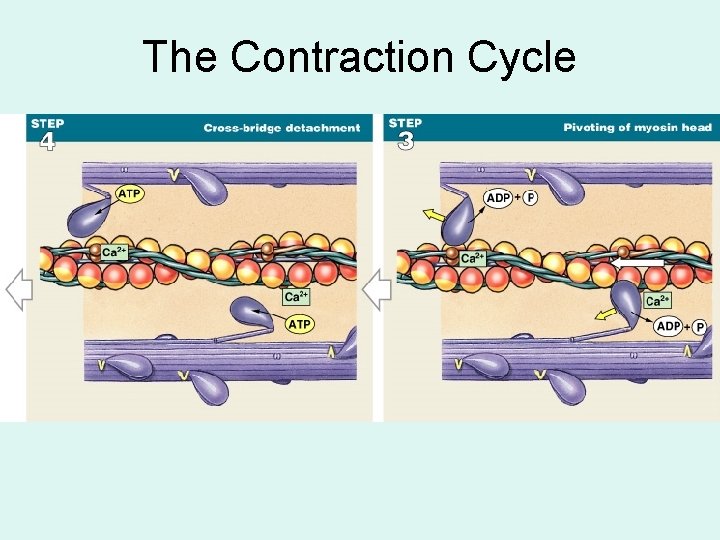
The Contraction Cycle
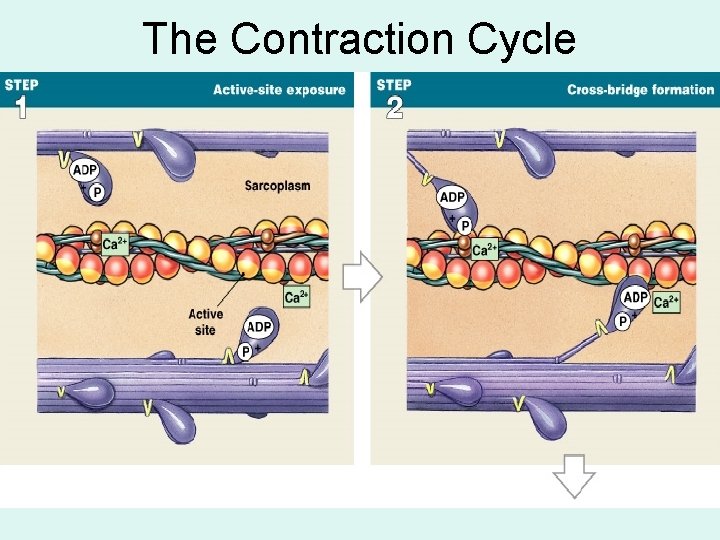
The Contraction Cycle
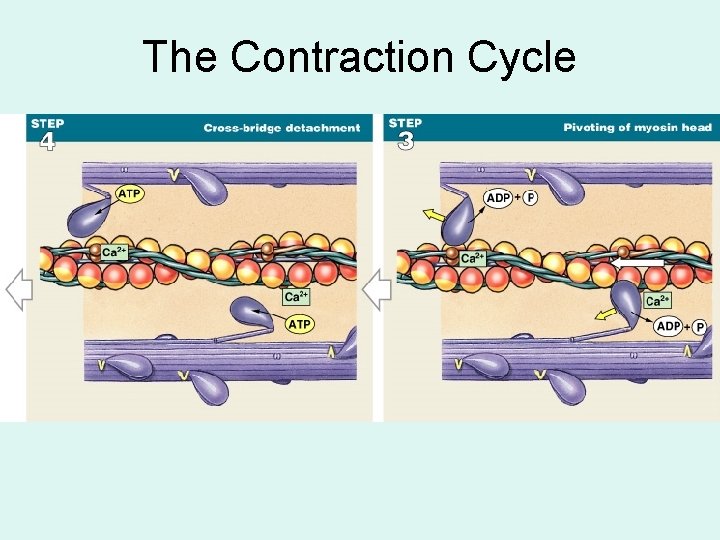
The Contraction Cycle
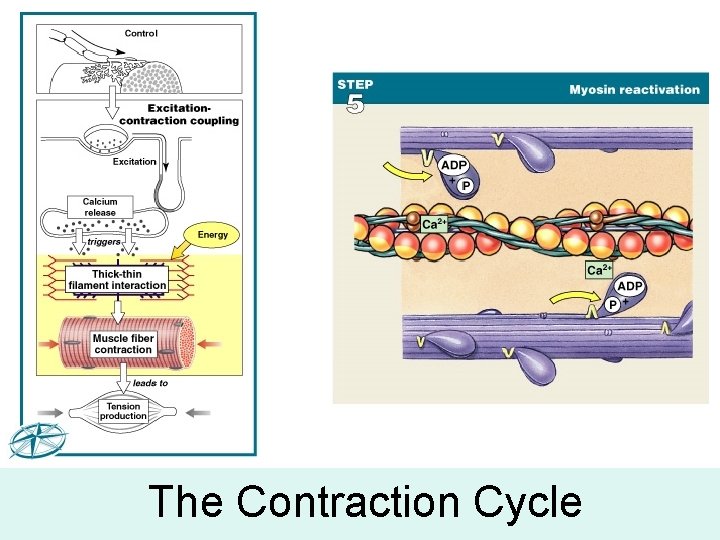
The Contraction Cycle
5 Steps of the Contraction Cycle 1. 2. 3. 4. 5. Exposure of active sites Formation of cross-bridges Pivoting of myosin heads Detachment of cross-bridges Reactivation of myosin
Show the animation
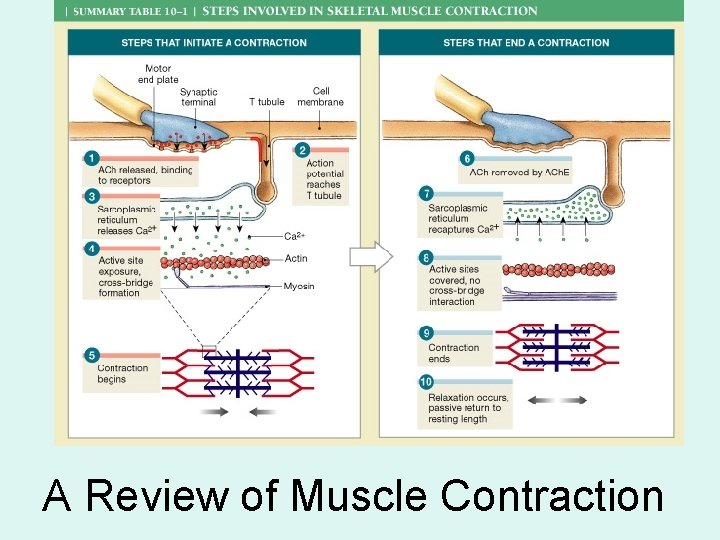
A Review of Muscle Contraction
Excitation-Contraction coupling • Stimulus or excitation is required for muscles to contract. • In skeletal muscle, the stimulus is from a motor neuron. • The stimulus is in the form of an action potential. • This action potential starts at the neuromuscular junction (NMJ).
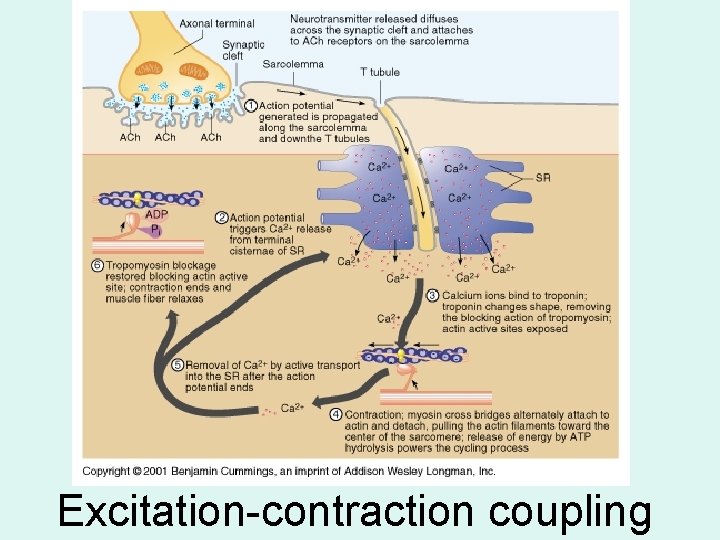
Excitation-contraction coupling
Show NMJ animation
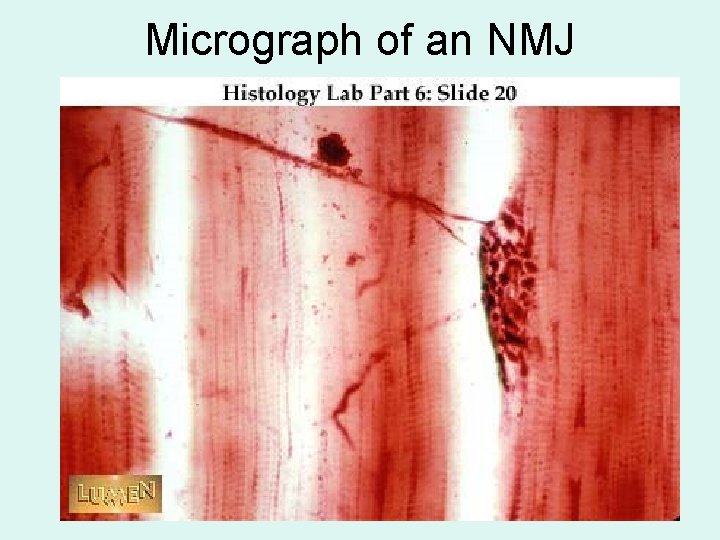
Micrograph of an NMJ

A Synapse Synaptic vesicles
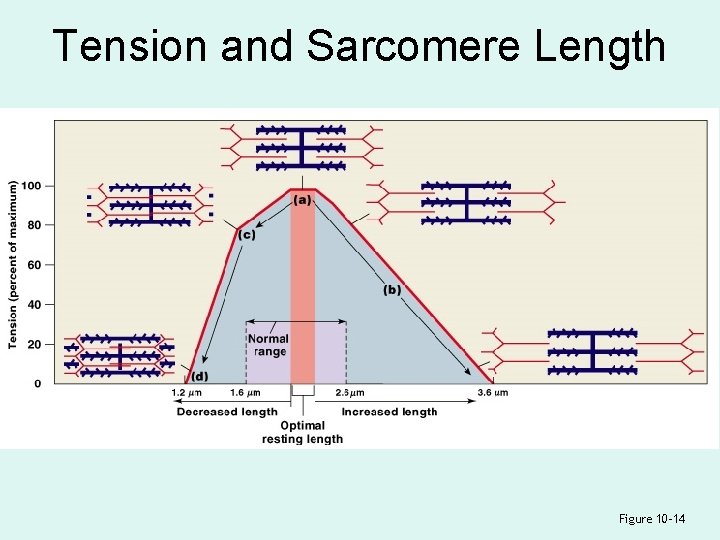
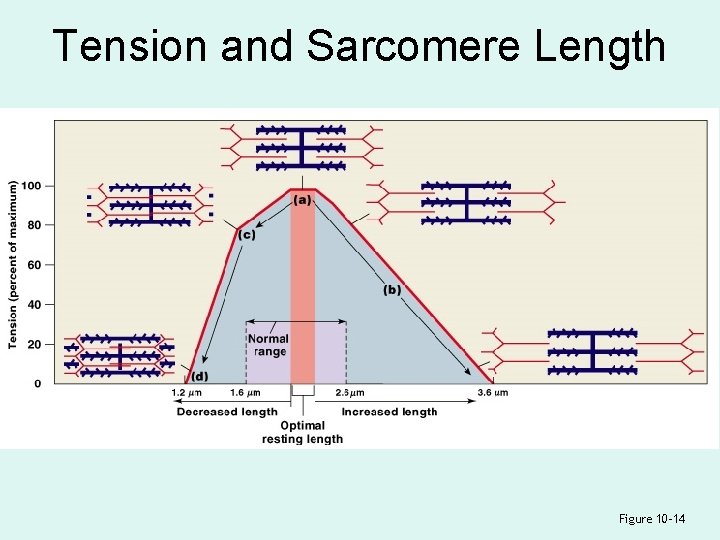
Tension and Sarcomere Length Figure 10– 14
Length–Tension Relationship • Number of pivoting cross-bridges depends on: – amount of overlap between thick and thin fibers • Optimum overlap produces greatest amount of tension: – too much or too little reduces efficiency
Length–Tension Relationship • Normal resting sarcomere length: – is 75% to 130% of optimal length
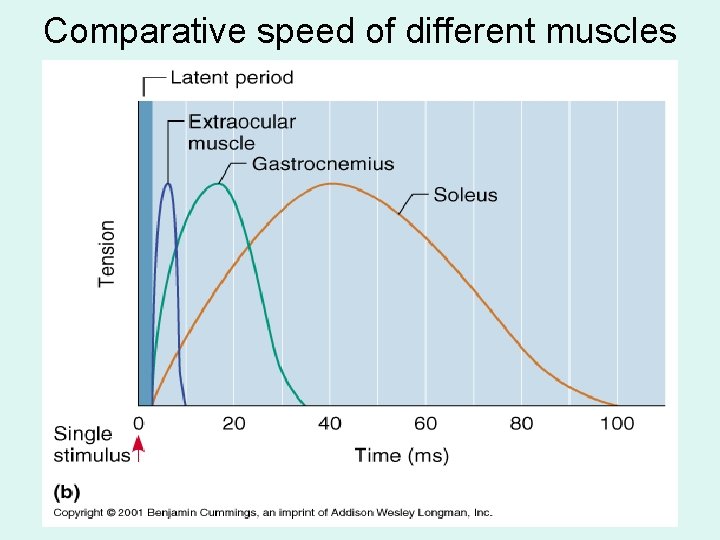
Frequency of Stimulation • A single neural stimulation produces: – a single contraction or twitch – which lasts about 7– 100 msec • Sustained muscular contractions: – require many repeated stimuli
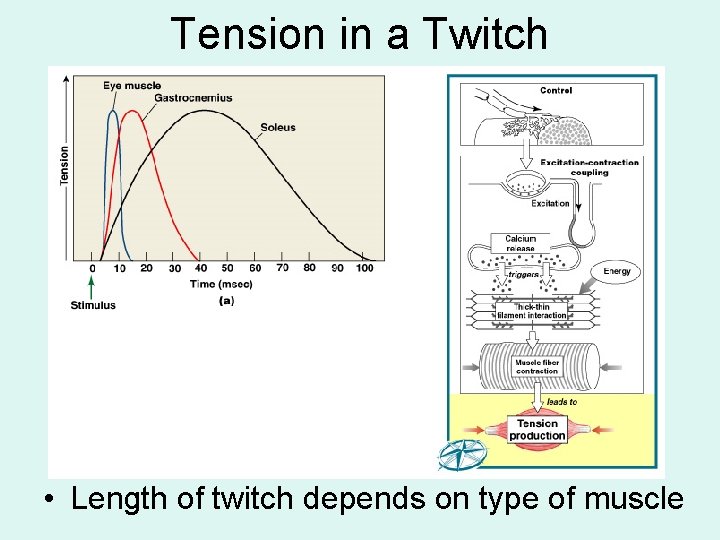
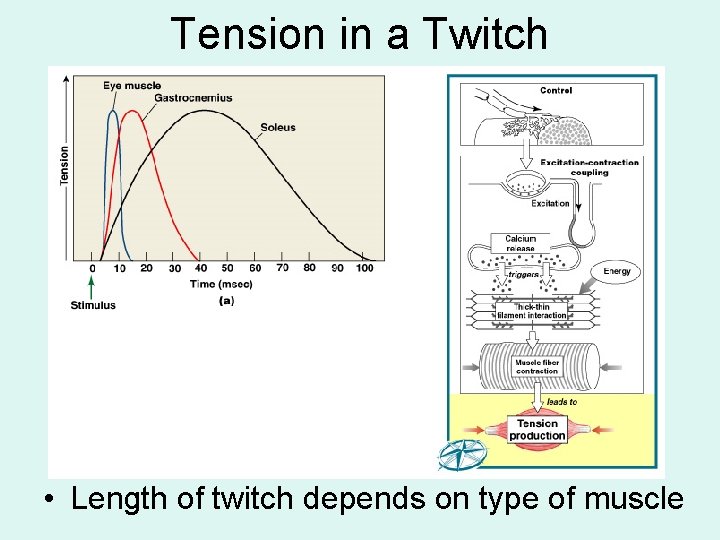
Tension in a Twitch • Length of twitch depends on type of muscle
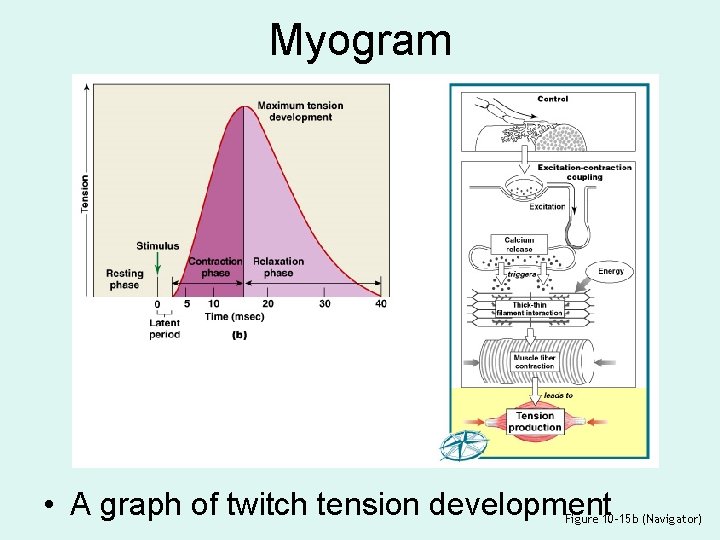
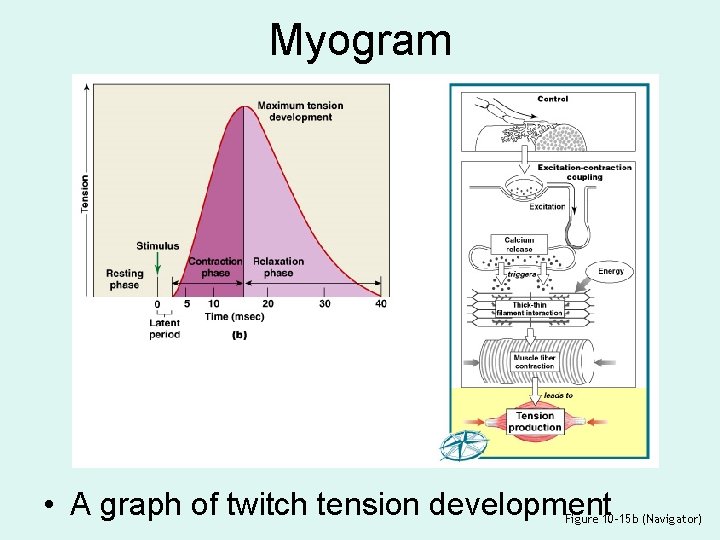
Myogram • A graph of twitch tension development Figure 10– 15 b (Navigator)
3 Phases of Twitch 1. Latent period before contraction: – the action potential moves through sarcolemma – causing Ca 2+ release
3 Phases of Twitch 2. Contraction phase: – calcium ions bind – tension builds to peak
3 Phases of Twitch 3. Relaxation phase: – Ca 2+ levels fall – active sites are covered – tension falls to resting levels
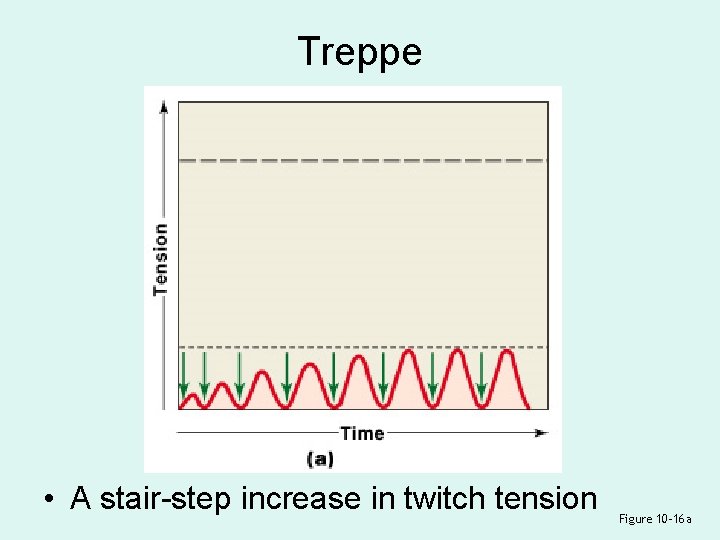
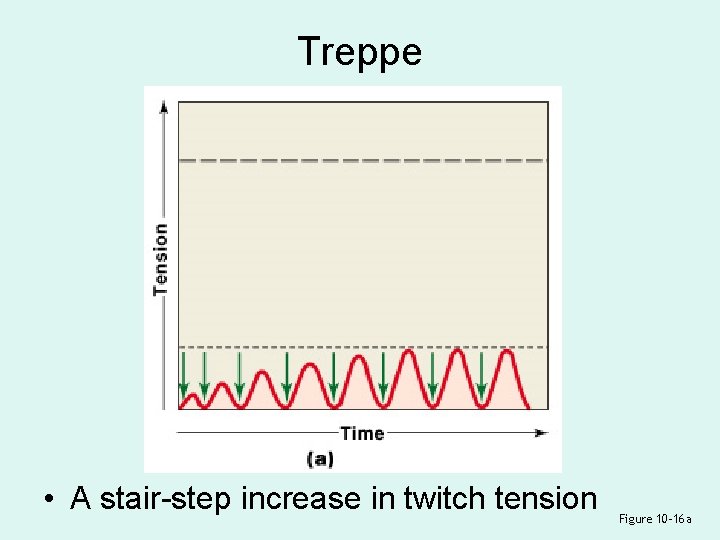
Treppe • A stair-step increase in twitch tension Figure 10– 16 a
Treppe • Repeated stimulations immediately after relaxation phase: – stimulus frequency < 50/second • Causes a series of contractions with increasing tension
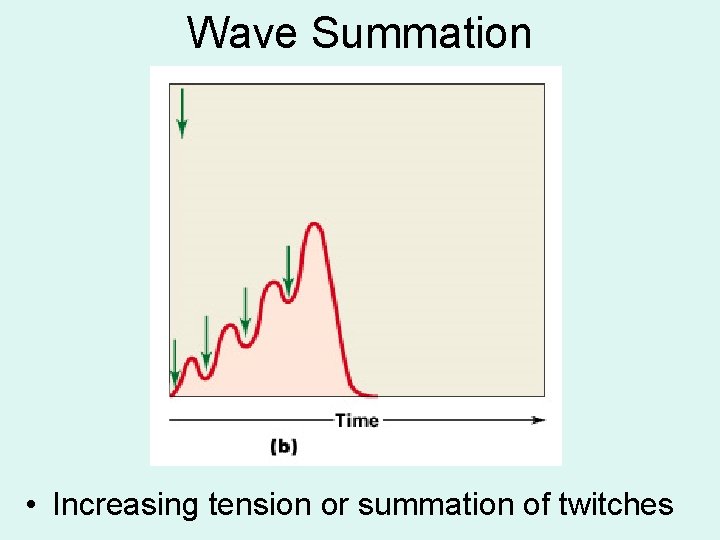
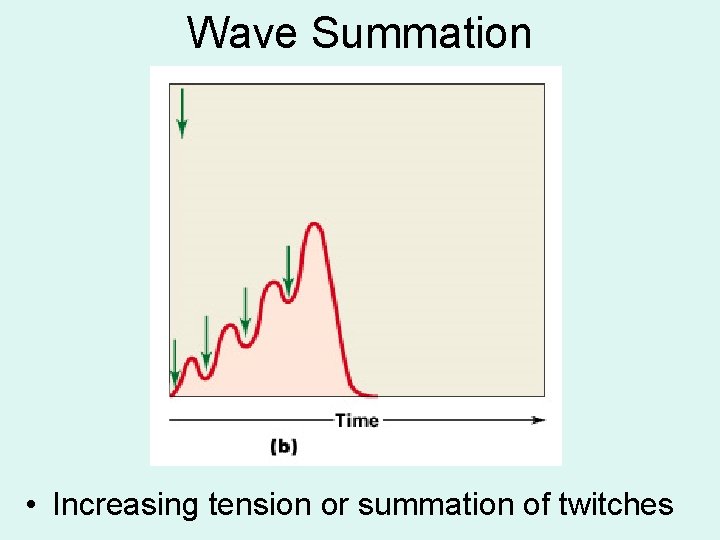
Wave Summation • Increasing tension or summation of twitches
Wave Summation • Repeated stimulations before the end of relaxation phase: – stimulus frequency > 50/second • Causes increasing tension or summation of twitches
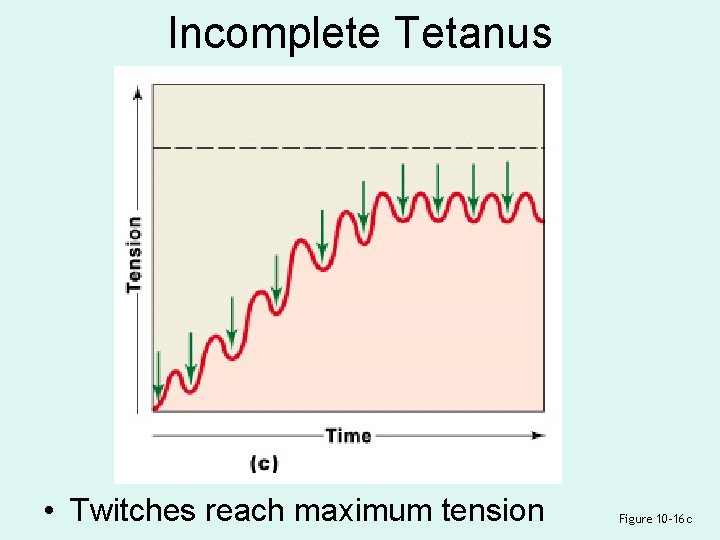
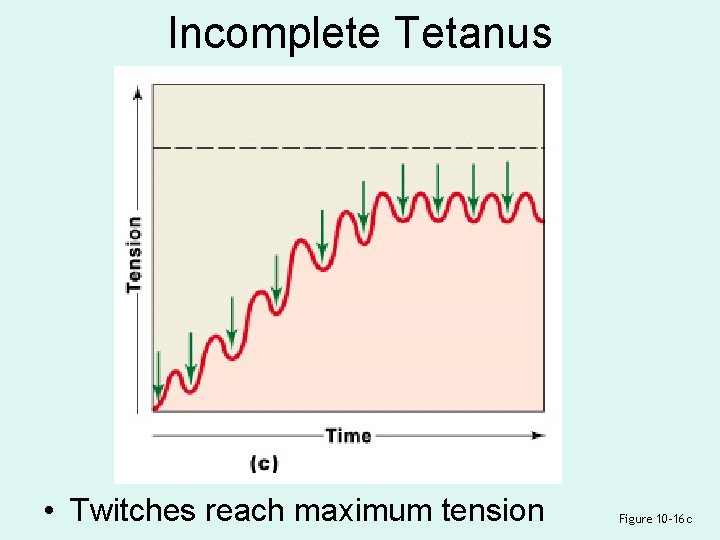
Incomplete Tetanus • Twitches reach maximum tension Figure 10– 16 c
Incomplete Tetanus • If rapid stimulation continues and muscle is not allowed to relax, twitches reach maximum level of tension
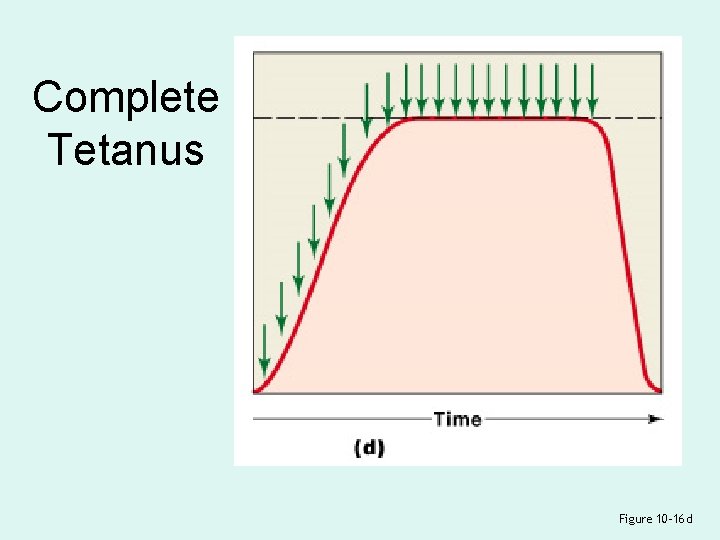
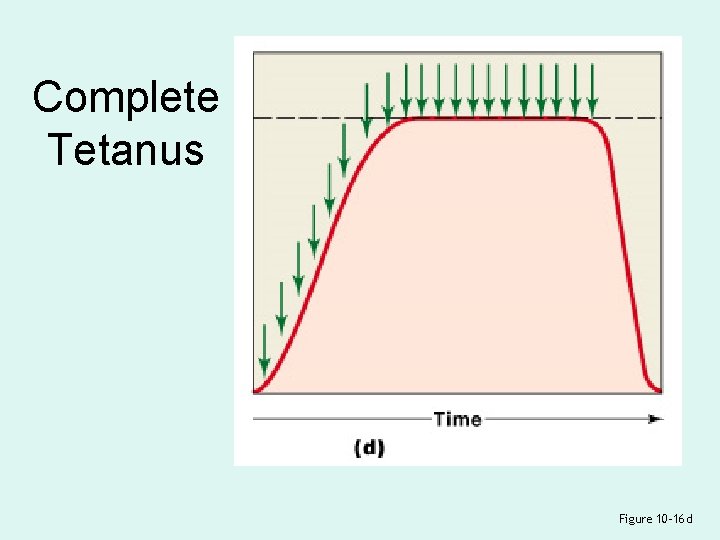
Complete Tetanus Figure 10– 16 d
Complete Tetanus • If stimulation frequency is high enough, muscle never begins to relax, and is in continuous contraction
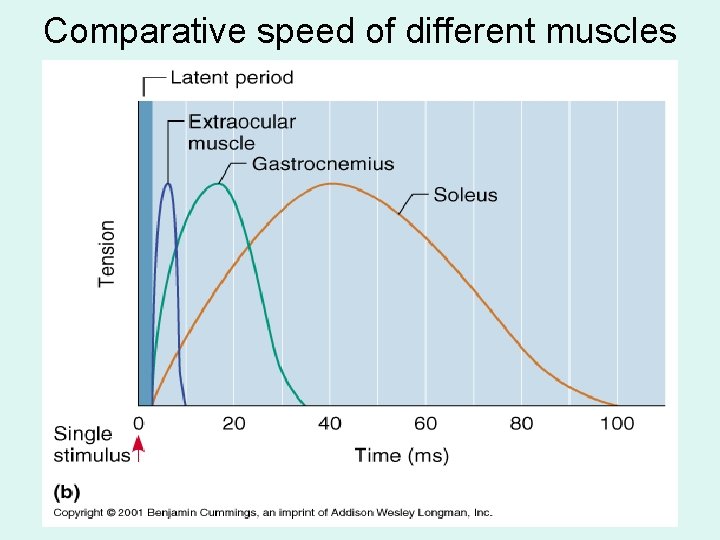
Comparative speed of different muscles
Tension Produced by Whole Skeletal Muscles • Depends on: – internal tension produced by muscle fibers – external tension exerted by muscle fibers on elastic extracellular fibers – total number of muscle fibers stimulated
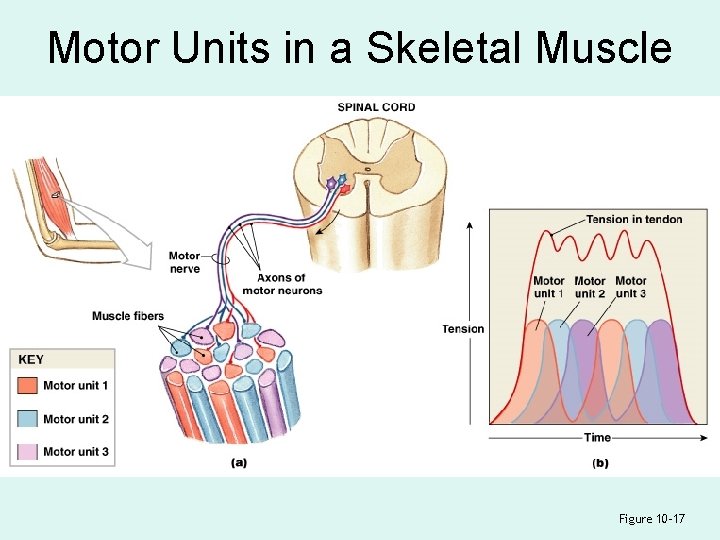
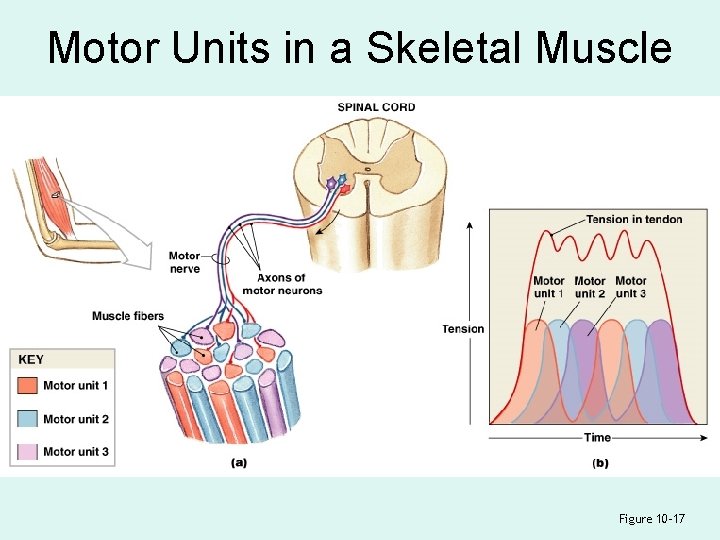
Motor Units in a Skeletal Muscle Figure 10– 17
Motor Units in a Skeletal Muscle • Contain hundreds of muscle fibers • That contract at the same time • Controlled by a single motor neuron
Recruitment (Multiple Motor Unit Summation) • In a whole muscle or group of muscles, smooth motion and increasing tension is produced by slowly increasing size or number of motor units stimulated
Maximum Tension • Achieved when all motor units reach tetanus • Can be sustained only a very short time
Sustained Tension • Less than maximum tension • Allows motor units to rest in rotation
2 Types of Skeletal Muscle Tension 1. Isotonic contraction 2. Isometric contraction
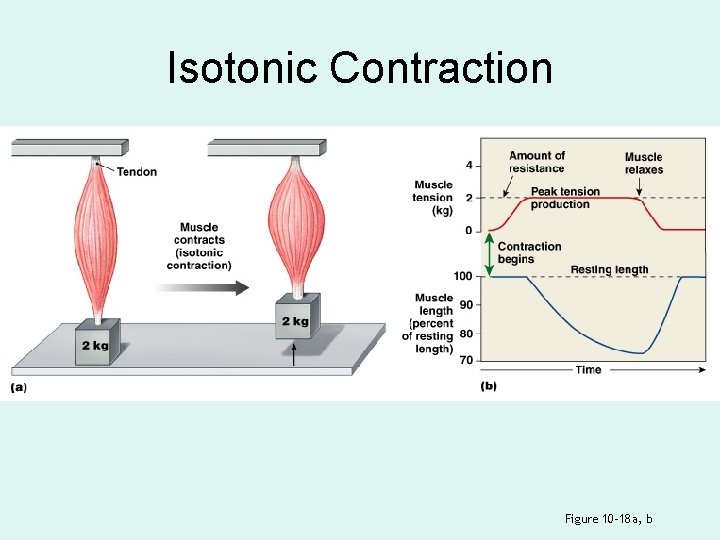
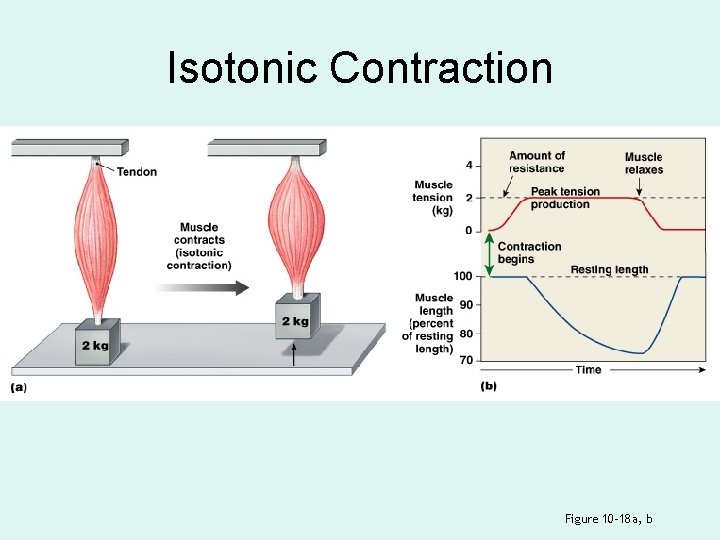
Isotonic Contraction Figure 10– 18 a, b

Isotonic Contraction • Skeletal muscle changes length: – resulting in motion • If muscle tension > resistance: – muscle shortens (concentric contraction) • If muscle tension < resistance: – muscle lengthens (eccentric contraction)
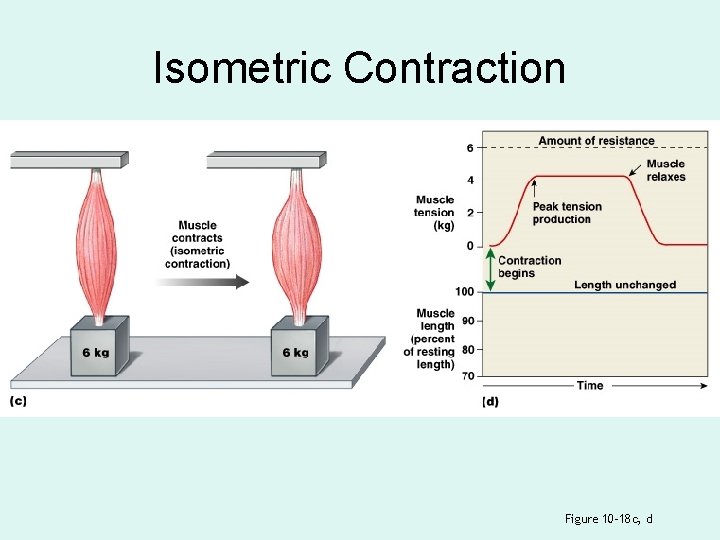
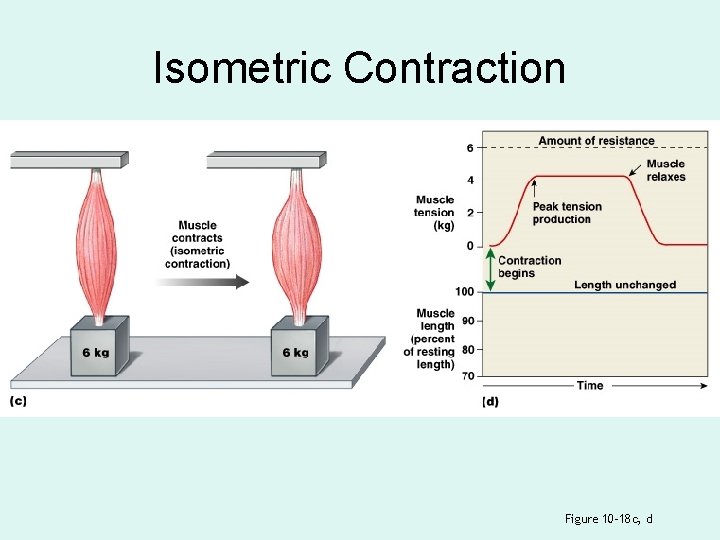
Isometric Contraction Figure 10– 18 c, d
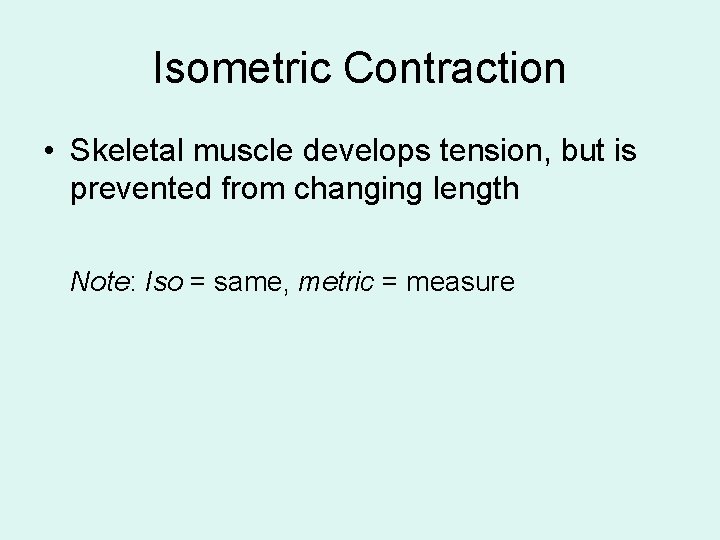
Isometric Contraction • Skeletal muscle develops tension, but is prevented from changing length Note: Iso = same, metric = measure
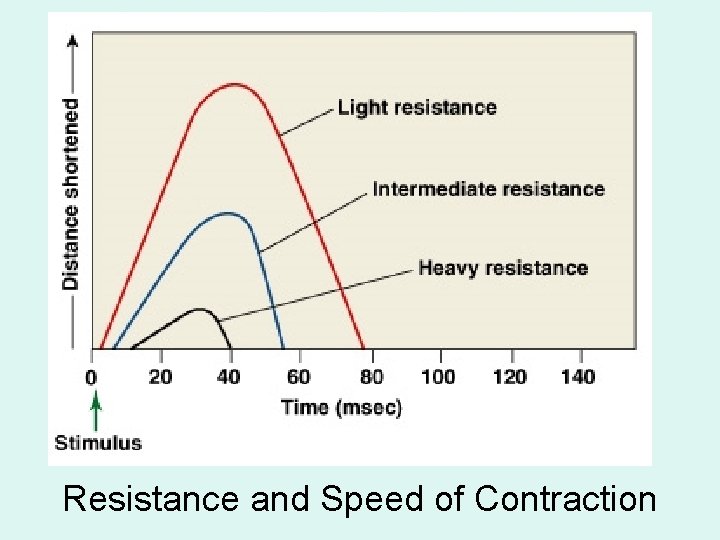
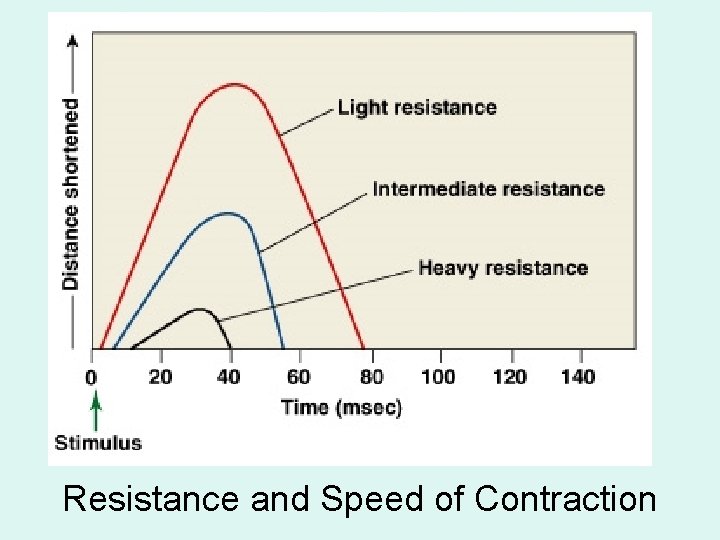
Resistance and Speed of Contraction
Resistance and Speed of Contraction • Are inversely related • The heavier the resistance on a muscle: – the longer it takes for shortening to begin – and the less the muscle will shorten
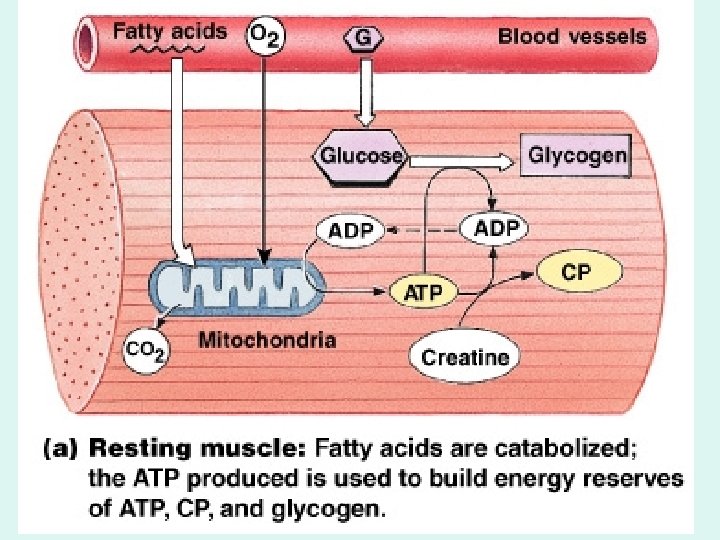
ATP and Muscle Contraction • Sustained muscle contraction uses a lot of ATP energy • Muscles store enough energy to start contraction • Muscle fibers must manufacture more ATP as needed
ATP and CP Reserves • Adenosine triphosphate (ATP): – the active energy molecule • Creatine phosphate (CP): – the storage molecule for excess ATP energy in resting muscle
Recharging ATP • Energy recharges ADP to ATP: – using the enzyme creatine phosphokinase (CPK) • When CP is used up, other mechanisms generate ATP

Energy Storage in Muscle Fiber Table 10– 2
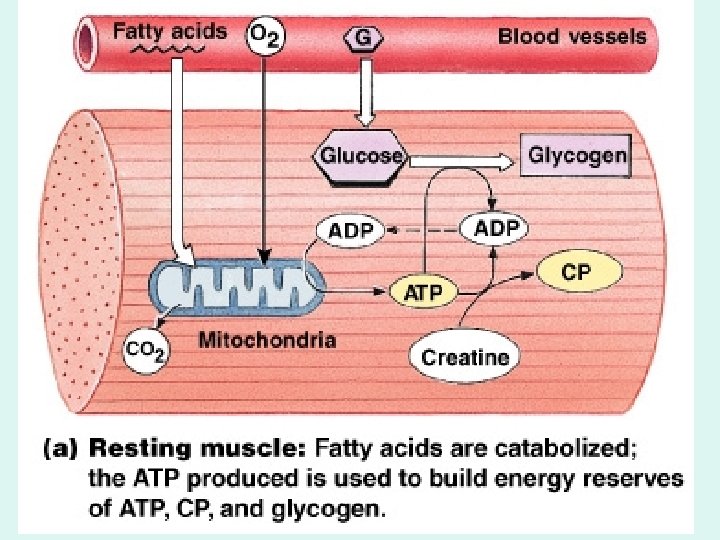
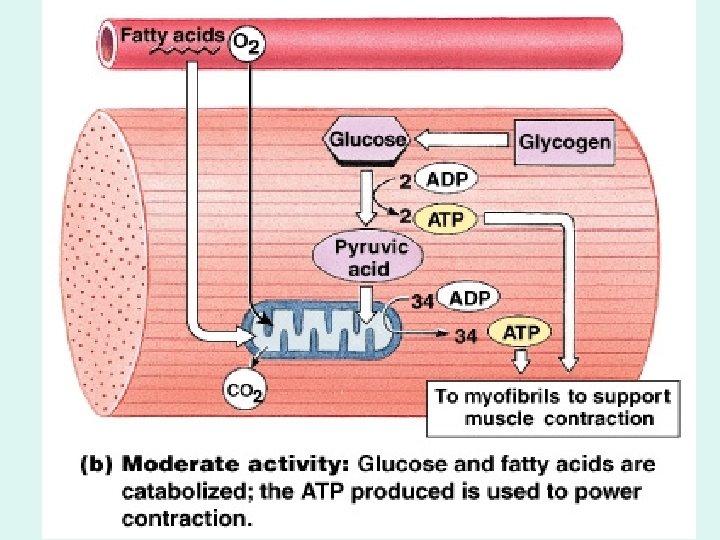
ATP Generation • Cells produce ATP in 2 ways: – aerobic metabolism of fatty acids in the mitochondria – anaerobic glycolysis in the cytoplasm
Aerobic Metabolism • Is the primary energy source of resting muscles • Breaks down fatty acids • Produces 34 ATP molecules per glucose molecule
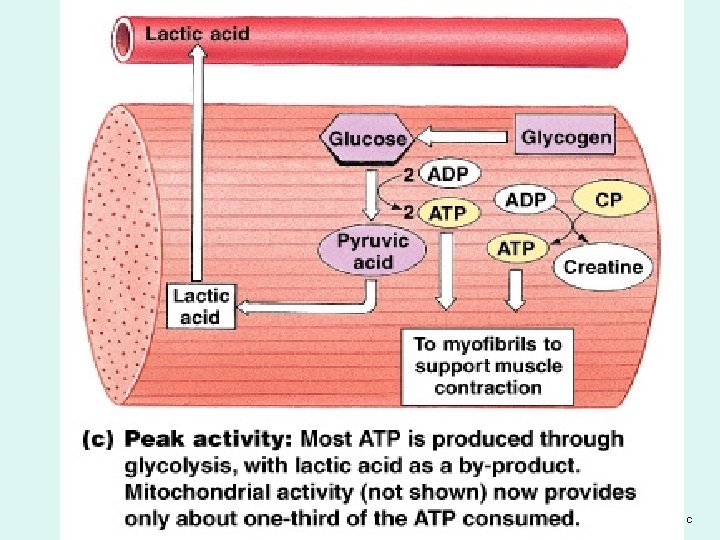
Anaerobic Glycolysis • Is the primary energy source for peak muscular activity • Produces 2 ATP molecules per molecule of glucose • Breaks down glucose from glycogen stored in skeletal muscles
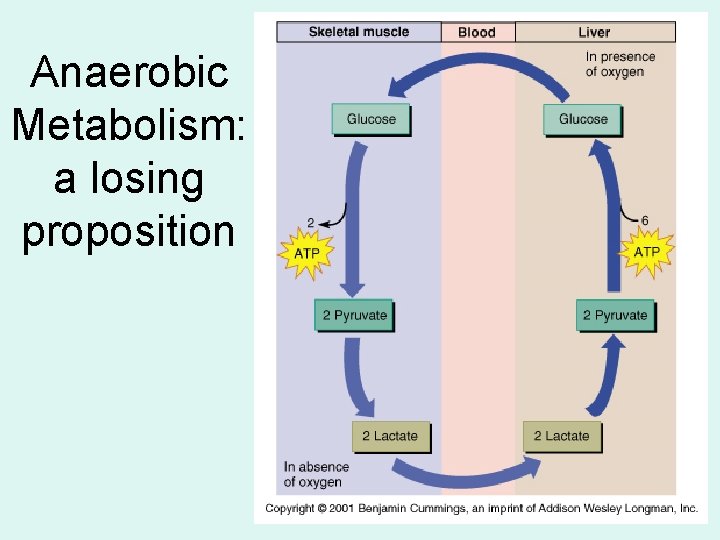
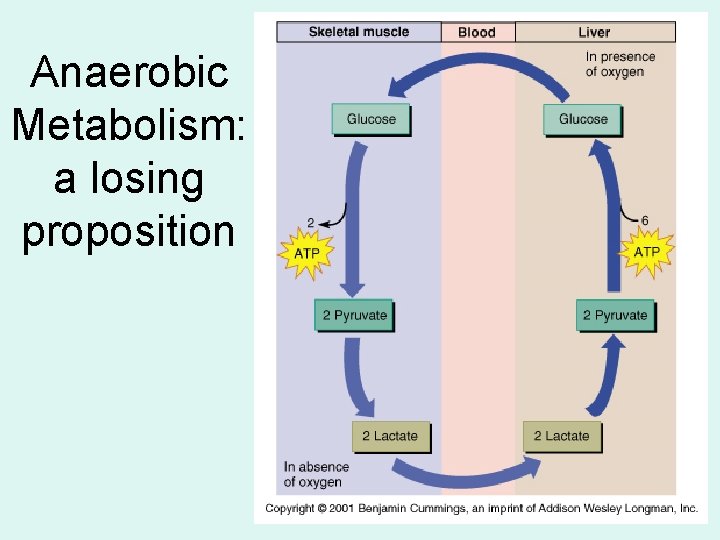
Anaerobic Metabolism: a losing proposition
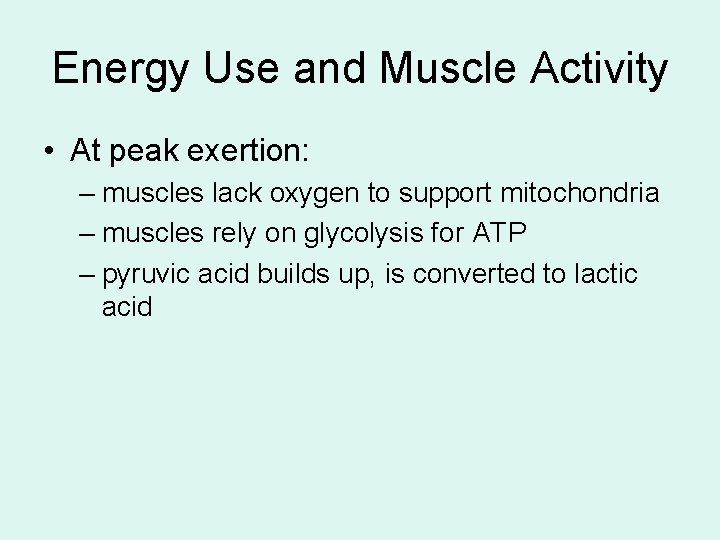
Energy Use and Muscle Activity • At peak exertion: – muscles lack oxygen to support mitochondria – muscles rely on glycolysis for ATP – pyruvic acid builds up, is converted to lactic acid
Muscle Metabolis m
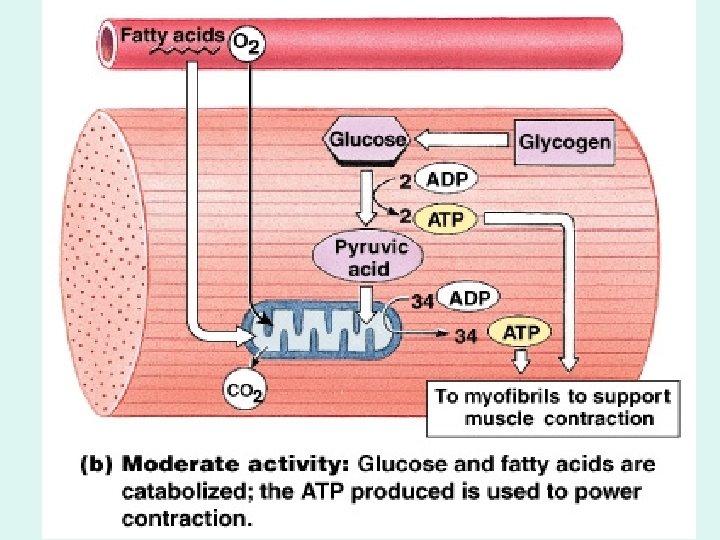
Muscle Metabolism Figure 10– 20 b
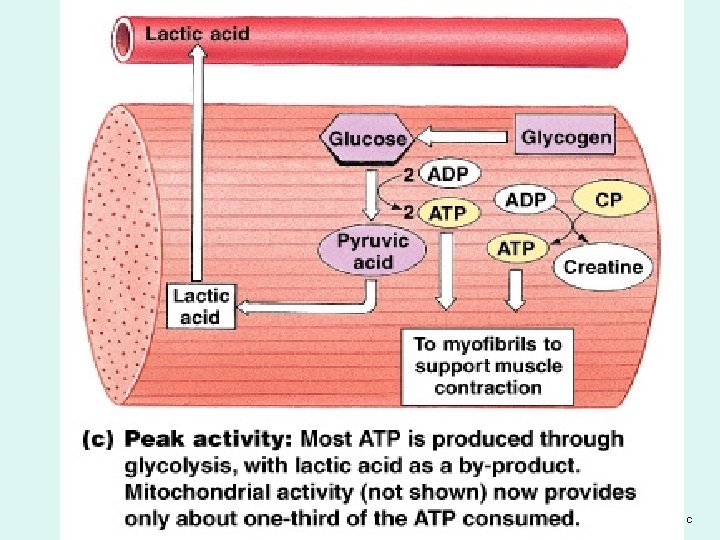
Muscle Metabolism Figure 10– 20 c
Results of Muscle Fatigue 1. Depletion of metabolic reserves 2. Damage to sarcolemma and sarcoplasmic reticulum 3. Low p. H (lactic acid) 4. Muscle exhaustion and pain
The Recovery Period • The time required after exertion for muscles to return to normal • Oxygen becomes available • Mitochondrial activity resumes

The Cori Cycle • The removal and recycling of lactic acid by the liver • Liver converts lactic acid to pyruvic acid • Glucose is released to recharge muscle glycogen reserves

Oxygen Debt • After exercise: – the body needs more oxygen than usual to normalize metabolic activities – resulting in heavy breathing
Muscle Performance • Power: – the maximum amount of tension produced • Endurance: – the amount of time an activity can be sustained • Power and endurance depend on: – the types of muscle fibers – physical conditioning

3 Types of Skeletal Muscle Fibers 1. Fast fibers 2. Slow fibers 3. Intermediate fibers
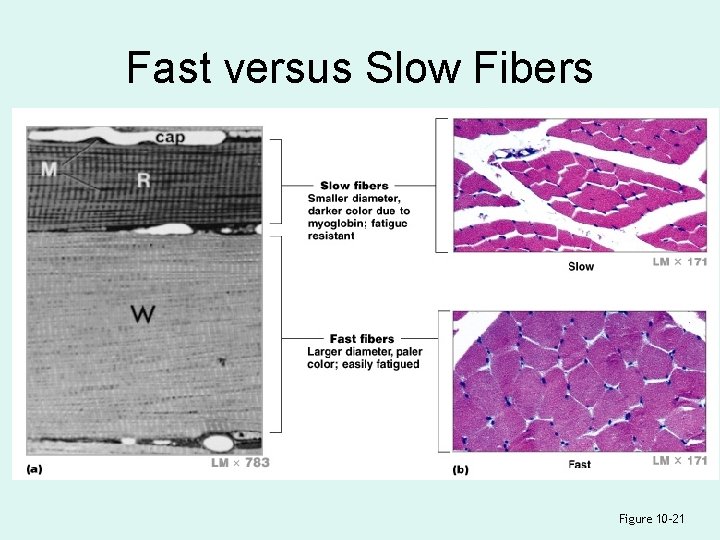
Fast Fibers • Contract very quickly • Have large diameter, large glycogen reserves, few mitochondria • Have strong contractions, fatigue quickly
Slow Fibers • • Are slow to contract, slow to fatigue Have small diameter, more mitochondria Have high oxygen supply Contain myoglobin (red pigment, binds oxygen)
Intermediate Fibers • Are mid-sized • Have low myoglobin • Have more capillaries than fast fiber, slower to fatigue
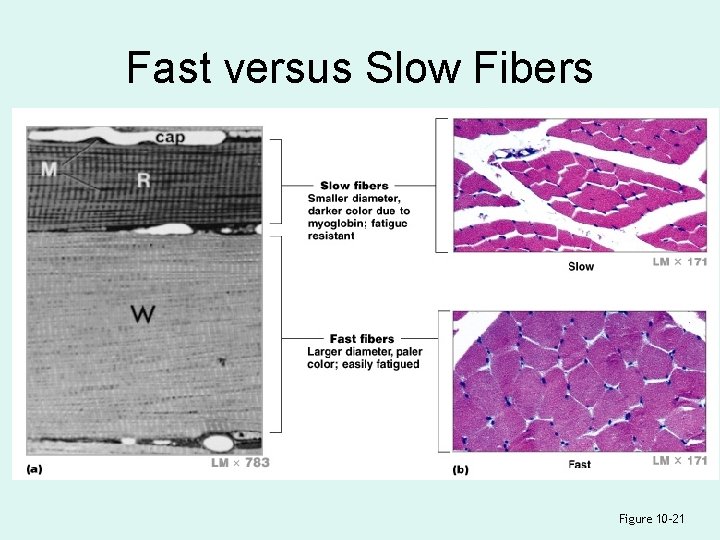
Fast versus Slow Fibers Figure 10– 21

Comparing Skeletal Muscle Fibers
Muscles and Fiber Types • White muscle: – mostly fast fibers – pale (e. g. , chicken breast) • Red muscle: – mostly slow fibers – dark (e. g. , chicken legs) • Most human muscles: – mixed fibers – pink
Muscle Hypertrophy • Muscle growth from heavy training: – increases diameter of muscle fibers – increases number of myofibrils – increases mitochondria, glycogen reserves
Muscle Atrophy • Lack of muscle activity: – reduces muscle size, tone, and power
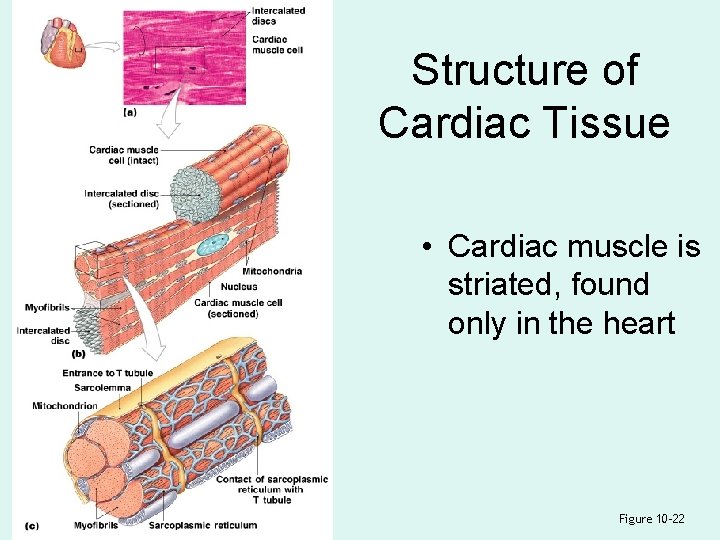
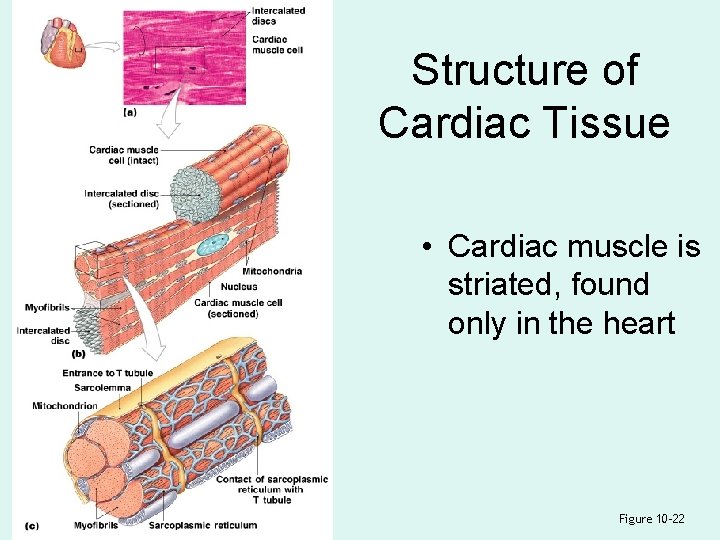
Structure of Cardiac Tissue • Cardiac muscle is striated, found only in the heart Figure 10– 22
7 Characteristics of Cardiocytes • Unlike skeletal muscle, cardiac muscle cells (cardiocytes): – are small – have a single nucleus – have short, wide T tubules
7 Characteristics of Cardiocytes – have no triads – have SR with no terminal cisternae – are aerobic (high in myoglobin, mitochondria) – have intercalated discs
Intercalated Discs • Are specialized contact points between cardiocytes • Join cell membranes of adjacent cardiocytes (gap junctions, desmosomes)
Functions of Intercalated Discs • Maintain structure • Enhance molecular and electrical connections • Conduct action potentials
Coordination of Cardiocytes • Because intercalated discs link heart cells mechanically, chemically, and electrically, the heart functions like a single, fused mass of cells
4 Functions of Cardiac Tissue 1. Automaticity: – contraction without neural stimulation – controlled by pacemaker cells 2. Variable contraction tension: – controlled by nervous system
4 Functions of Cardiac Tissue 3. Extended contraction time 4. Prevention of wave summation and tetanic contractions by cell membranes
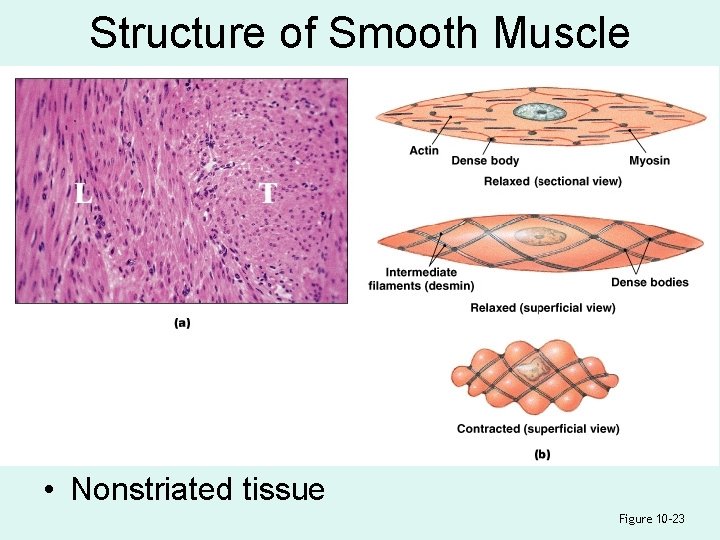
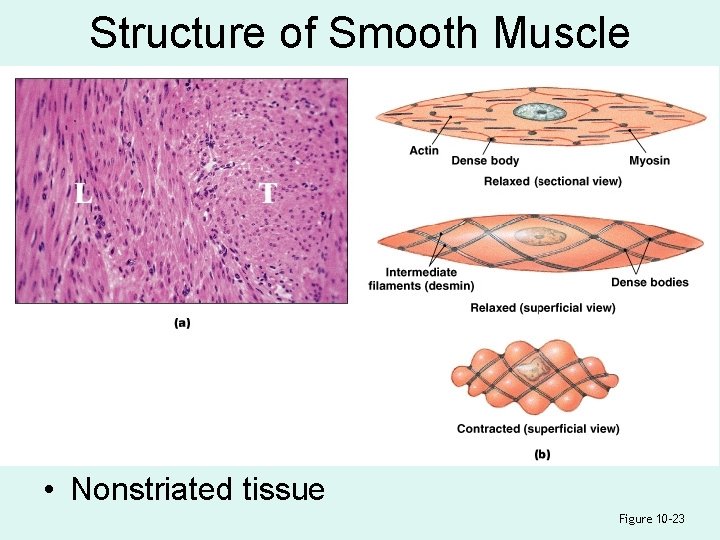
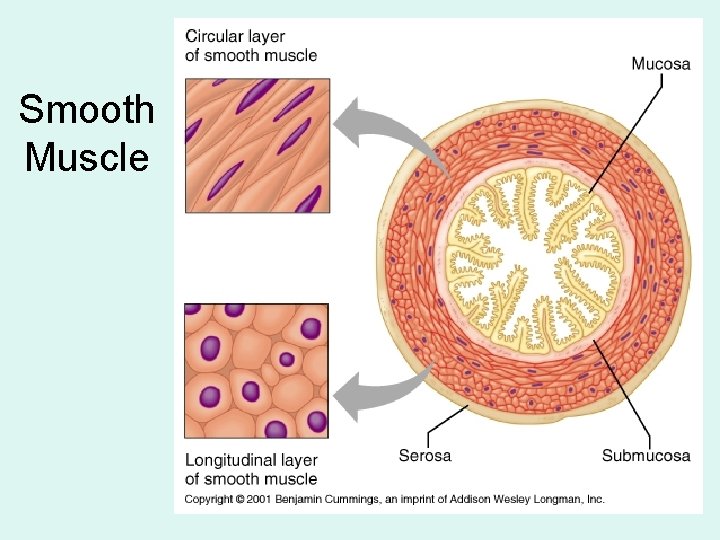
Structure of Smooth Muscle • Nonstriated tissue Figure 10– 23
Comparing Smooth and Striated Muscle • Different internal organization of actin and myosin • Different functional characteristics
8 Characteristics of Smooth Muscle Cells 1. Long, slender, and spindle shaped 2. Have a single, central nucleus 3. Have no T tubules, myofibrils, or sarcomeres 4. Have no tendons or aponeuroses
8 Characteristics of Smooth Muscle Cells 5. Have scattered myosin fibers 6. Myosin fibers have more heads per thick filament 7. Have thin filaments attached to dense bodies 8. Dense bodies transmit contractions from cell to cell
Functional Characteristics of Smooth Muscle 1. 2. 3. 4. Excitation–contraction coupling Length–tension relationships Control of contractions Smooth muscle tone

Excitation–Contraction Coupling 2+ • Free Ca in cytoplasm triggers contraction • Ca 2+ binds with calmodulin: – in the sarcoplasm – activates myosin light chain kinase • Enzyme breaks down ATP, initiates contraction
Length–Tension Relationships • Thick and thin filaments are scattered • Resting length not related to tension development • Functions over a wide range of lengths (plasticity)
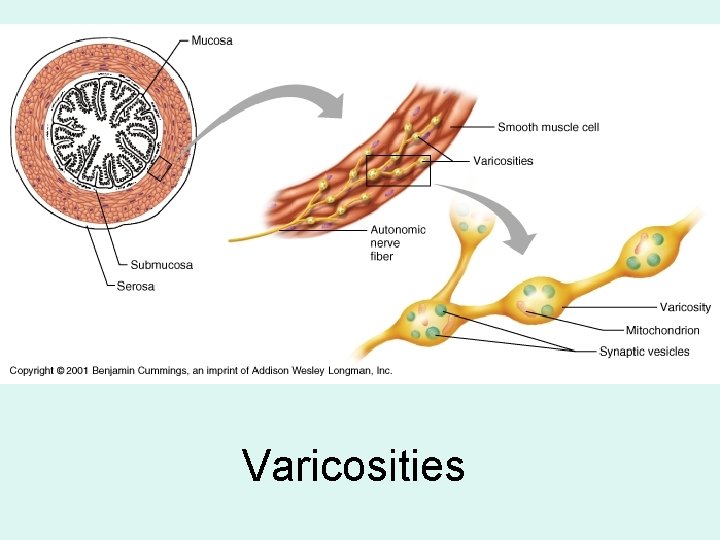
Control of Contractions • Subdivisions: – multiunit smooth muscle cells: • connected to motor neurons – visceral smooth muscle cells: • not connected to motor neurons • rhythmic cycles of activity controlled by pacesetter cells
Smooth Muscle Tone • Maintains normal levels of activity • Modified by neural, hormonal, or chemical factors
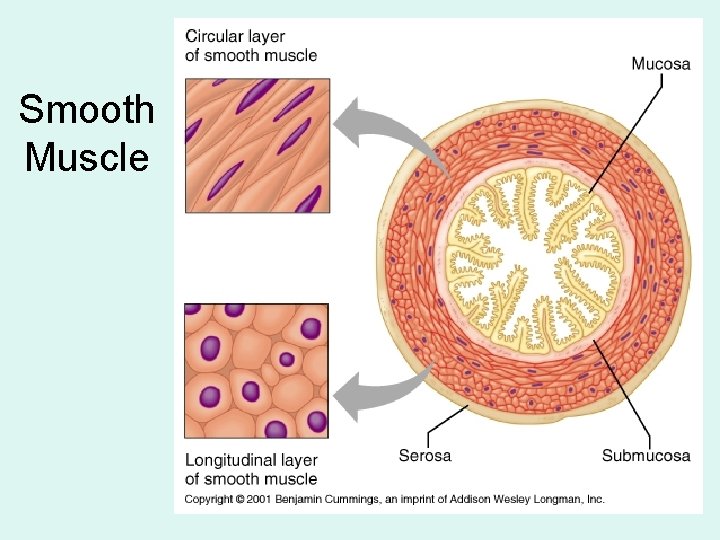
Smooth Muscle
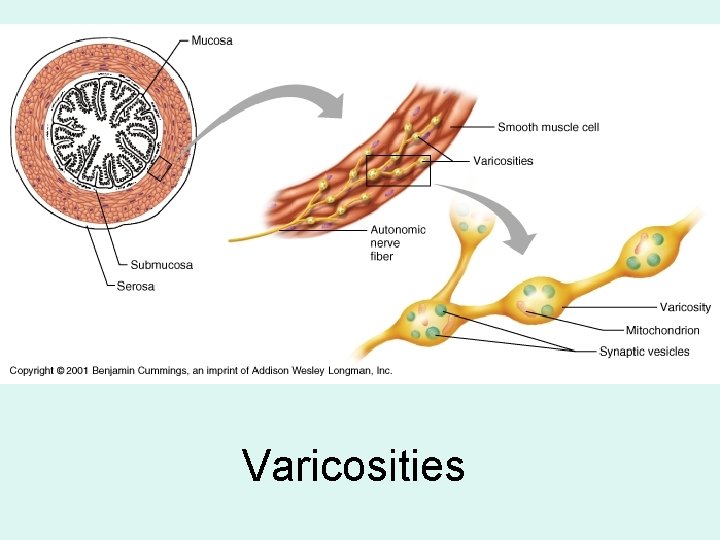
Varicosities

Skeletal Smooth Diameter 10 - 100 m 3 - 8 m Connective tissue Epi-, Peri- & Endomysium only Endomysium SR Yes, complex Barely, simple T - tubules yes no Sarcomeres yes no Gap Junctions no yes voluntary yes no Neurotransmitters Acetylcholine Ach, epinephrine, (Ach) norepinephrine, et al Regeneration Very little Lots, for muscle

Future governors of Califorina?
 Muscles and muscle tissue chapter 9
Muscles and muscle tissue chapter 9 Skeletal muscle
Skeletal muscle Skeletal muscle tissue
Skeletal muscle tissue Skeletal muscle tissue structure
Skeletal muscle tissue structure Structure of muscle cell
Structure of muscle cell Smooth muscle fibers
Smooth muscle fibers 5 functions skeletal system
5 functions skeletal system Function of muscular tissue
Function of muscular tissue Thin
Thin Microscopic anatomy of skeletal muscles
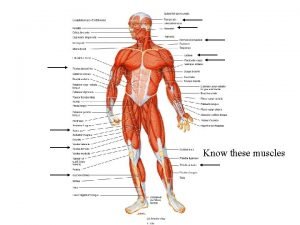
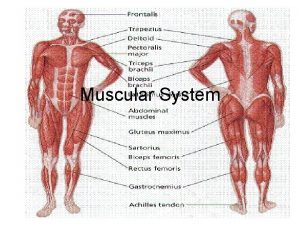
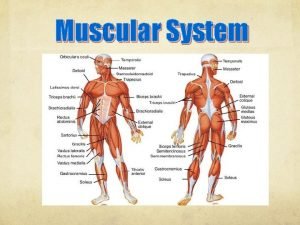
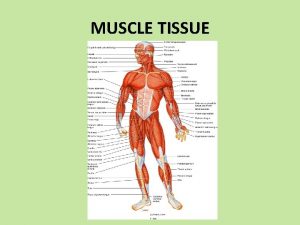
Microscopic anatomy of skeletal muscles Major skeletal muscles
Major skeletal muscles Skeletal muscles anterior view
Skeletal muscles anterior view Skeletal muscle organization
Skeletal muscle organization Fascicle
Fascicle What tissue forms membranes
What tissue forms membranes Major skeletal muscles
Major skeletal muscles Naming muscles
Naming muscles Human muscles anterior
Human muscles anterior Skeletal muscles
Skeletal muscles Naming skeletal muscles
Naming skeletal muscles Naming skeletal muscles
Naming skeletal muscles John wiley
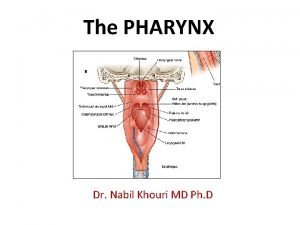
John wiley Pharyngeal tubercle
Pharyngeal tubercle 5 golden rules of skeletal muscle activity
5 golden rules of skeletal muscle activity Centrally acting skeletal muscle relaxants
Centrally acting skeletal muscle relaxants Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Chlorzoxone
Chlorzoxone Endo peri epi
Endo peri epi Sarcoplasmic
Sarcoplasmic Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Macro structure of muscle
Macro structure of muscle Skeletal muscle pump
Skeletal muscle pump Spleen histology slide labeled
Spleen histology slide labeled A&p flix activity: resting membrane potential
A&p flix activity: resting membrane potential Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Microscopic anatomy of skeletal muscle figure 6-2
Microscopic anatomy of skeletal muscle figure 6-2 Microscopic anatomy of skeletal muscle figure 6-2
Microscopic anatomy of skeletal muscle figure 6-2 Nerve supply to muscles
Nerve supply to muscles Skeletal muscle belly
Skeletal muscle belly Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Function of skeletal muscle
Function of skeletal muscle Skeletal muscle cylindrical
Skeletal muscle cylindrical Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Lesson 5.1 the organization of a skeletal muscle
Lesson 5.1 the organization of a skeletal muscle Cross bridge cycle
Cross bridge cycle Lesson 5.1 the organization of a skeletal muscle
Lesson 5.1 the organization of a skeletal muscle Site:slidetodoc.com
Site:slidetodoc.com Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Starter which muscles do you already know
Starter which muscles do you already know Cardiac muscle tissue
Cardiac muscle tissue When unstretched transitional epithelium
When unstretched transitional epithelium Microscopic anatomy of skeletal muscle
Microscopic anatomy of skeletal muscle 5 golden rules of skeletal muscle activity
5 golden rules of skeletal muscle activity What are t tubules in muscles
What are t tubules in muscles Is skeletal muscle an organ
Is skeletal muscle an organ Autonomic nervous system skeletal muscle
Autonomic nervous system skeletal muscle Is skeletal muscle an organ
Is skeletal muscle an organ What tissue is this
What tissue is this Types of muscle tissue
Types of muscle tissue Heart muscles are
Heart muscles are Main function of muscular system
Main function of muscular system Girdl
Girdl Myosin in smooth muscle
Myosin in smooth muscle Anatomy of skeletal muscle
Anatomy of skeletal muscle Function of skeletal muscle
Function of skeletal muscle Parallel skeletal muscle
Parallel skeletal muscle Adductor pollicis longus tendon
Adductor pollicis longus tendon Function of skeletal muscle
Function of skeletal muscle Skeletal muscle
Skeletal muscle Skeletal muscle origin
Skeletal muscle origin Figure 10-1 skeletal muscle fiber
Figure 10-1 skeletal muscle fiber Perforation plates
Perforation plates What are the five functions of the skeletal system
What are the five functions of the skeletal system What are the five functions of the skeletal system?
What are the five functions of the skeletal system? Arms movement
Arms movement 5 functions of skeletal system
5 functions of skeletal system Sagittal suture
Sagittal suture Muscle tissue
Muscle tissue Cardiac muscle
Cardiac muscle Eccentric movement
Eccentric movement Muscle tissue ppt
Muscle tissue ppt Classification of muscle tissue
Classification of muscle tissue Epithelium location
Epithelium location Latent phase muscle contraction
Latent phase muscle contraction Muscle tissue
Muscle tissue Muscle tissue
Muscle tissue Muscle tissue parts
Muscle tissue parts Inner quads
Inner quads Axial muscles
Axial muscles Types of muscle
Types of muscle Tissue that connects muscle to bone
Tissue that connects muscle to bone Myalgia is abnormal softening of muscle tissue
Myalgia is abnormal softening of muscle tissue Connective tissue disease adalah
Connective tissue disease adalah Muscle tissue parts
Muscle tissue parts Cardiac muscle tissue parts
Cardiac muscle tissue parts What makes up muscle tissue
What makes up muscle tissue What are the characteristics of nervous tissue
What are the characteristics of nervous tissue Muscle tissue function
Muscle tissue function Cardiac muscle tissue
Cardiac muscle tissue What muscle fibers run in circles around your eye
What muscle fibers run in circles around your eye Adipose connective tissue function
Adipose connective tissue function Chapter 5 the skeletal system
Chapter 5 the skeletal system The skeletal system chapter 3
The skeletal system chapter 3 Chapter 7 4 skeletal system
Chapter 7 4 skeletal system Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Chapter 6 the skeletal system answer key
Chapter 6 the skeletal system answer key Site:slidetodoc.com
Site:slidetodoc.com Chapter 36 skeletal muscular and integumentary systems
Chapter 36 skeletal muscular and integumentary systems Chapter 32 section 2 the skeletal system answer key
Chapter 32 section 2 the skeletal system answer key Chapter 14 lesson 3 the nervous system
Chapter 14 lesson 3 the nervous system Chapter 8 skeletal system
Chapter 8 skeletal system Chapter 7 4 skeletal system
Chapter 7 4 skeletal system Chapter 6 bones and skeletal tissues
Chapter 6 bones and skeletal tissues Chapter 5 axial skeleton worksheet answers
Chapter 5 axial skeleton worksheet answers Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Human skull superior view
Human skull superior view Chapter 5 the skeletal system
Chapter 5 the skeletal system Chapter 5 the skeletal system axial skeleton skull
Chapter 5 the skeletal system axial skeleton skull Chapter 3 the skeletal system labeling exercises
Chapter 3 the skeletal system labeling exercises Hollow portions of bones surrounding the nasal cavity
Hollow portions of bones surrounding the nasal cavity Tissue examples
Tissue examples Chapter 8 skeletal system
Chapter 8 skeletal system Male vs female skeleton pelvis
Male vs female skeleton pelvis All about bones
All about bones Emr chapter 15 injuries to muscles and bones
Emr chapter 15 injuries to muscles and bones Absolute value as a piecewise function
Absolute value as a piecewise function How to solve evaluating functions
How to solve evaluating functions Evaluating functions and operations on functions
Evaluating functions and operations on functions Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Chapter 4 tissue the living fabric
Chapter 4 tissue the living fabric Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Mrs skeletal
Mrs skeletal Medical terminology skeletal system
Medical terminology skeletal system Hardware skinning
Hardware skinning Section 36-1 the skeletal system
Section 36-1 the skeletal system