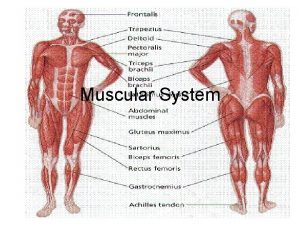
Muscle Tissue Types of Muscle Tissue Skeletal muscle
- Slides: 48
Muscle Tissue
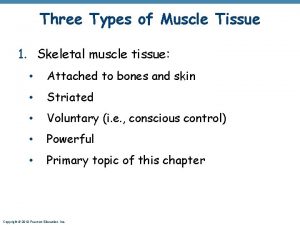
Types of Muscle Tissue Skeletal muscle tissue Cardiac muscle tissue Autorhythmicity - pacemaker Smooth muscle tissue
Functions of Muscle Tissue Producing body movements Stabilizing body positions Storing and moving substances within the body Sphincters – sustained contractions of ringlike bands prevent outflow of the contents of a hollow organ Cardiac muscle pumps nutrients and wastes through Smooth muscle moves food, bile, gametes, and urine Skeletal muscle contractions promote flow of lymph and return blood to the heart Generating heat - thermogenesis
Properties of Muscle Tissue Electrical excitability Produces electrical signals – action potentials Contractility Isometric contraction – tension without muscle shortening Isotonic contraction – constant tension with muscle shortening
Properties of Muscle Tissue Extensibility – ability of a muscle to stretch without being damaged Elasticity Ability of a muscle to return to its original length
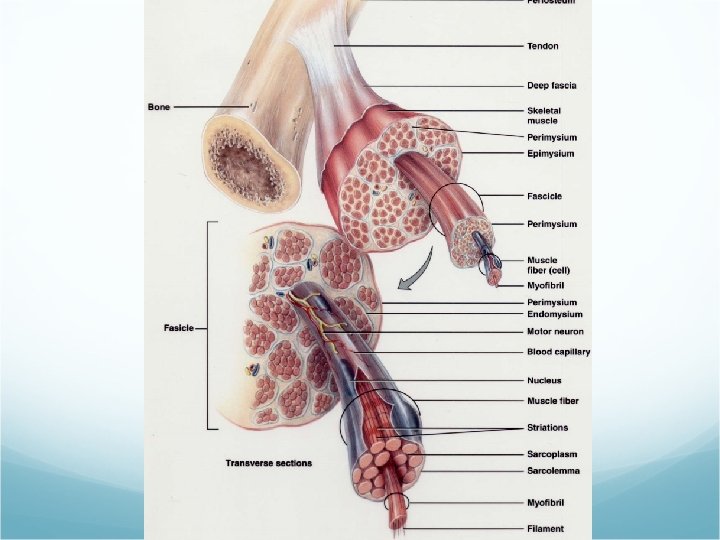
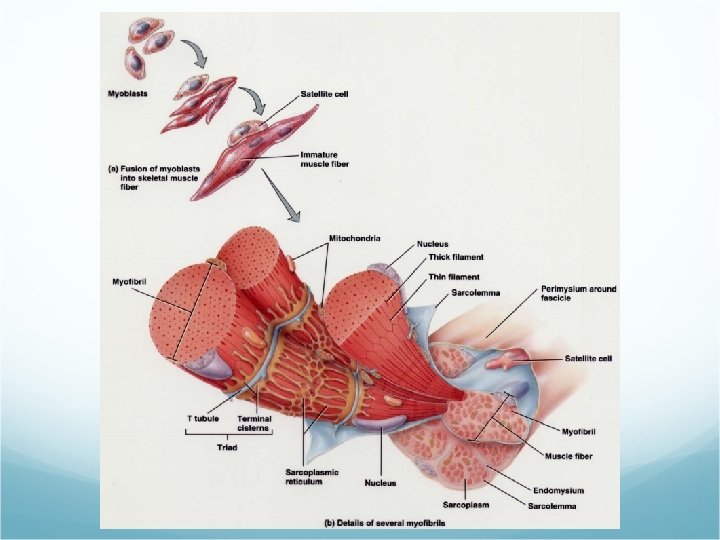
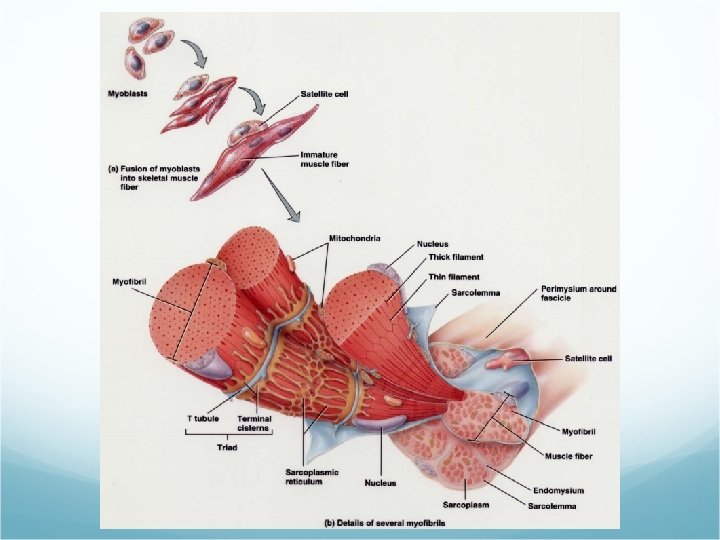
Connective Tissue Components Fascia – a sheet of fibrous CT that supports or surrounds muscles and other organs Superficial fascia (subcutaneous layer) – separates muscle from skin Deep fascia – holds muscles with similar functions together Epimysium – outermost layer – encircles whole muscles Perimysium Surrounds groups of 10 – 100 individual muscle fibers separating them into bundles called fascicles
Connective Tissue Components Endomysium Separates individual muscle fibers within the fascicle Tendon All 3 CT layers may extend beyond the muscle to form a cord of dense regular CT that attaches muscle to the periosteum of bone Aponeurosis A broad, flat layer of CT
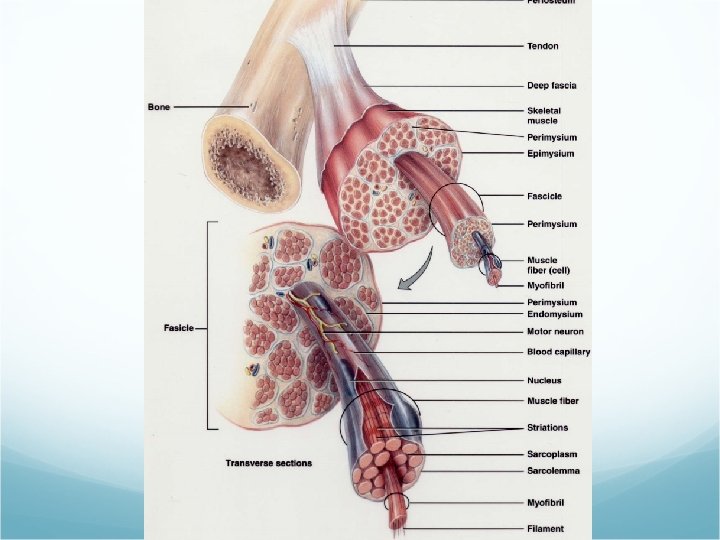
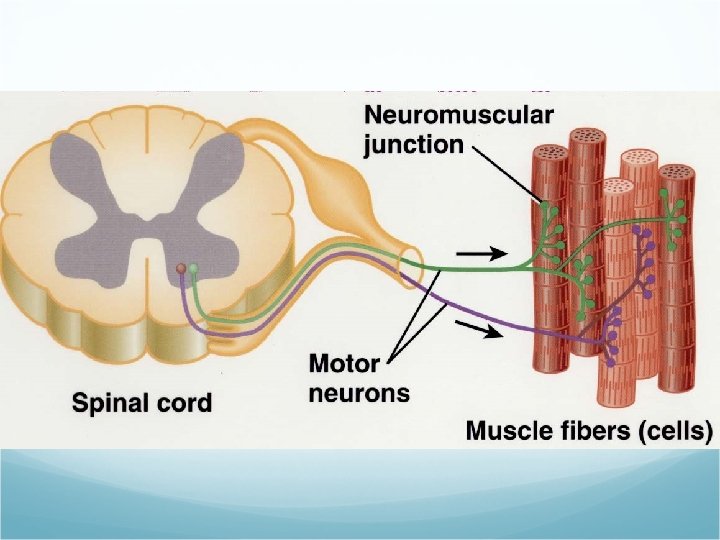
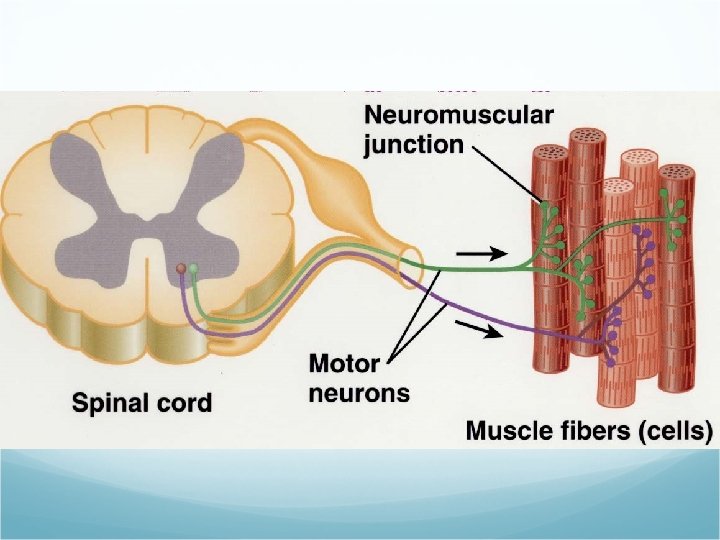
Nerve and Blood Supply Skeletal muscles are well supplied with nerves and blood vessels Neuromuscular junction – the structural point of contact and the functional site of communication between a nerve and the muscle fiber Capillaries are abundant – each muscle fiber comes into contact with 1 or more
Sarcolemma, T Tubules, and Sarcoplasm Sarcolemma – the plasma membrane of a muscle cell T (transverse) tubules – Propogate action potentials – extend to the outside of the muscle fiber Sarcoplasm – cytoplasm of the muscle fiber Contains myoglobin – protein that binds with oxygen
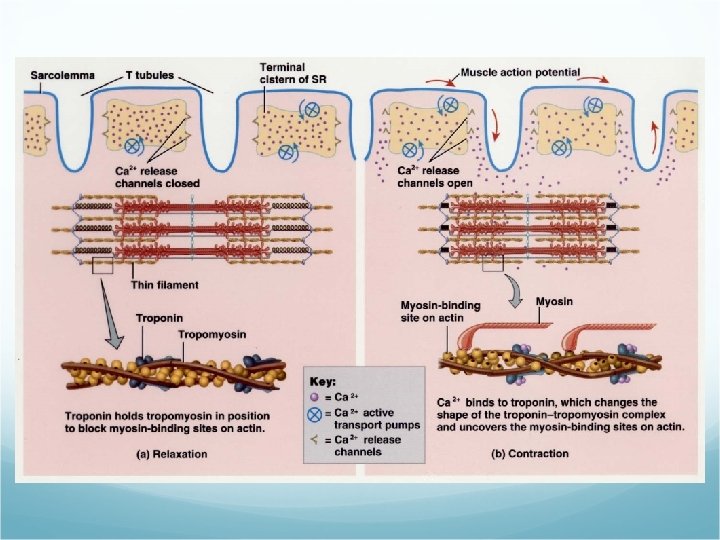
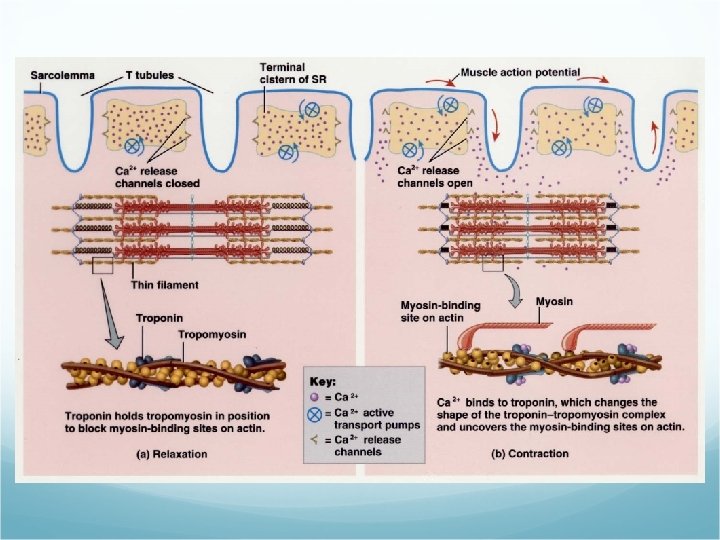
Myofibrils and Sarcoplasmic Reticulum Myofibril – the contractile elements of skeletal muscle Sarcoplasmic reticulum (SR) – encircles each myofibril – stores CA 2+ (its release triggers muscle contractions)
Atrophy and Hypertrophy Muscular atrophy – wasting away of muscles Disuse Denervation Muscular hypertrophy – an excessive increase in the diameter of muscle fibers
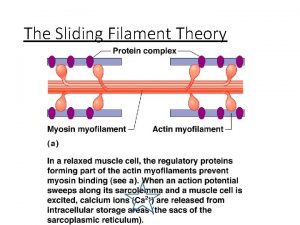
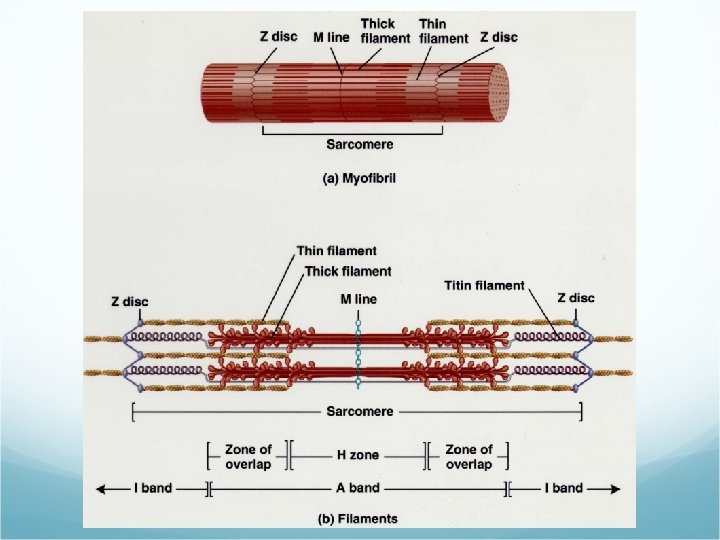
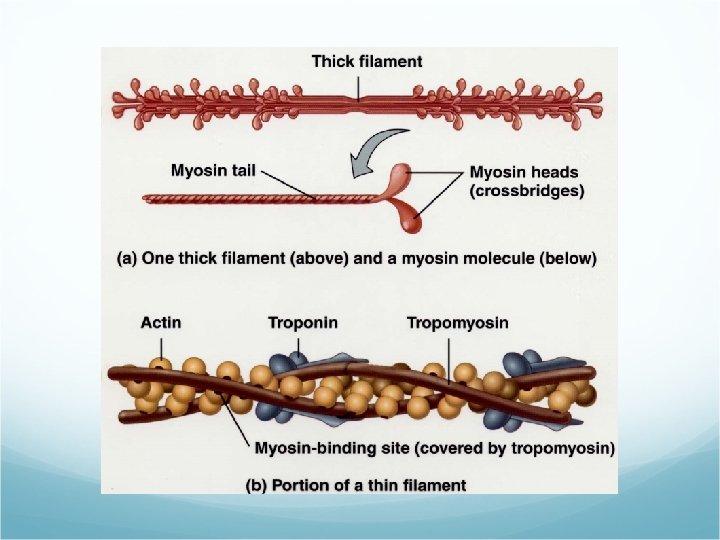
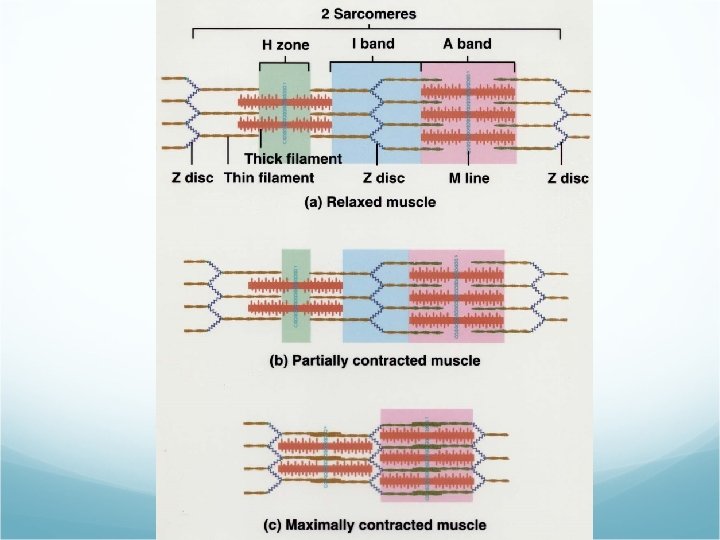
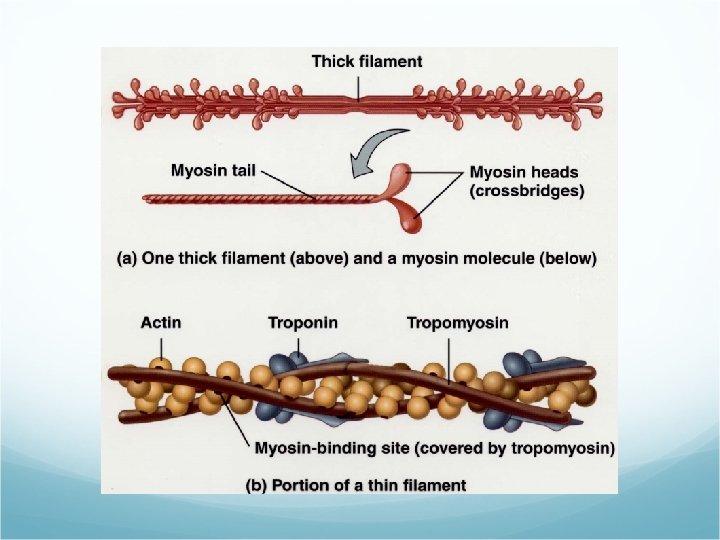
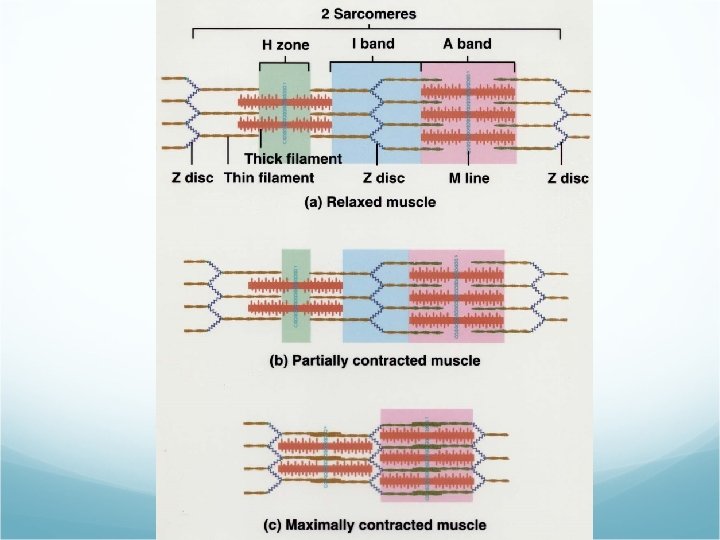
Filaments and the Sarcomere Filaments – structures within the myofibril Thin Thick Sarcomere – basic functional unit of a myofibril Z discs – separate one sarcomere from the next
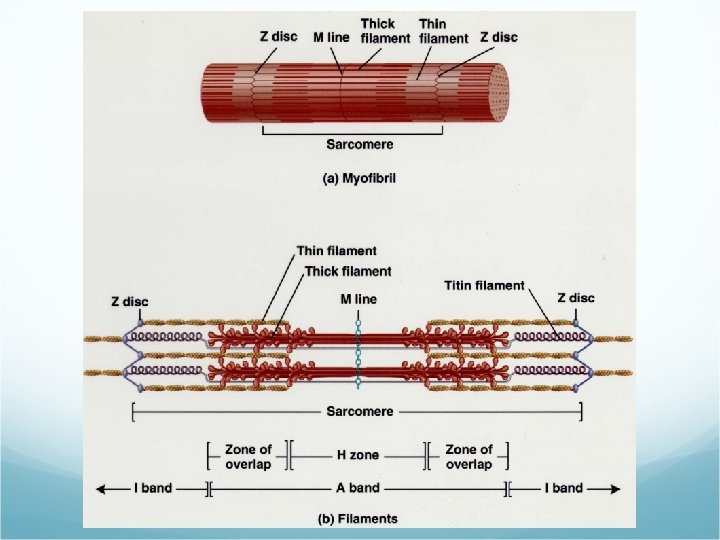
Filaments and the Sarcomere A band – predominantly thick filaments Zone of overlap at the ends of the A bands H zone – contains thick, but no thin filaments I band – thin filaments M-line – middle of the sarcomere
Muscle Proteins Contractile proteins – generate force Myosin Actin Regulatory proteins – switch contraction on and off Structural proteins
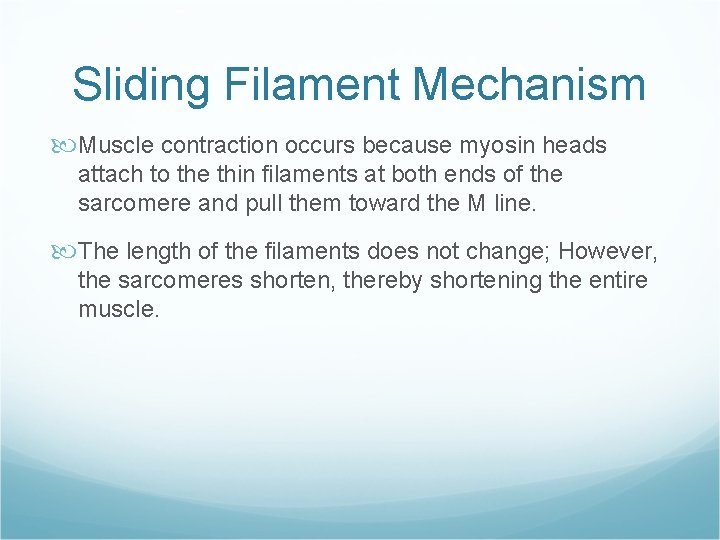
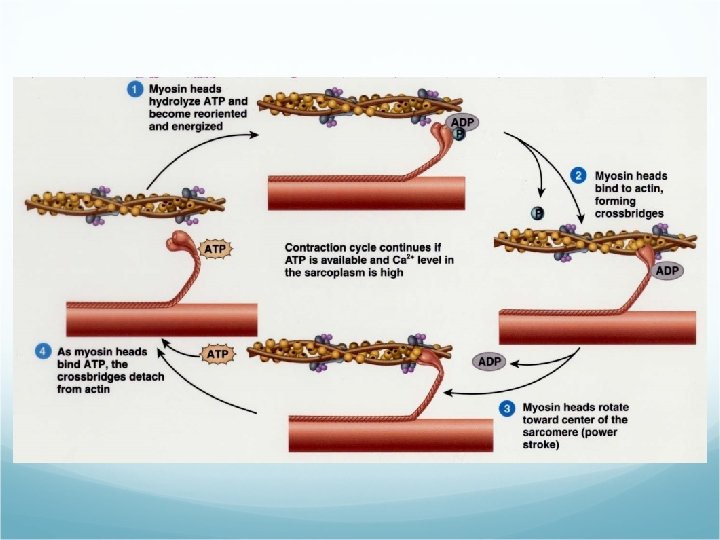
Sliding Filament Mechanism Muscle contraction occurs because myosin heads attach to the thin filaments at both ends of the sarcomere and pull them toward the M line. The length of the filaments does not change; However, the sarcomeres shorten, thereby shortening the entire muscle.
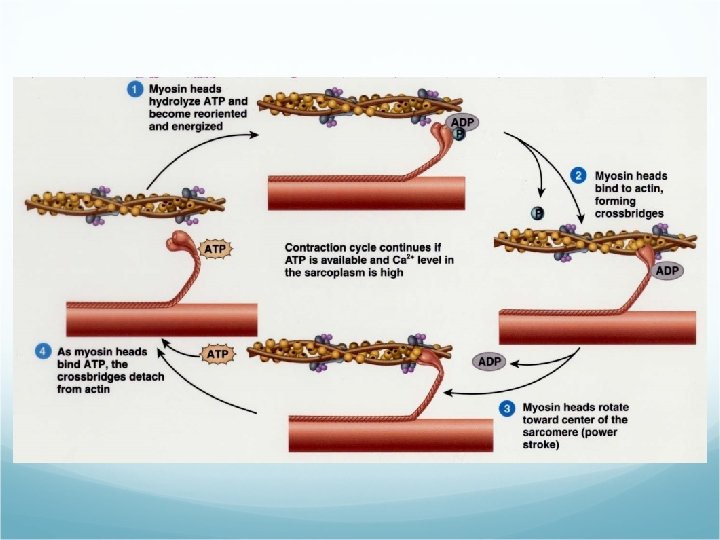
Role of Ca 2+ in Contraction An increase in calcium ion concentration in the cytosol initiates muscle contraction and a decrease in calcium ions stops it.
Rigor Mortis After death the cellular membranes become leaky. Calcium ions are released and cause muscular contraction. The muscles are in a state of rigidity called rigor mortis. It begins 3 -4 hours after death and lasts about 24 hours, until proteolytic enzymes break down (digest) the cross-bridges.
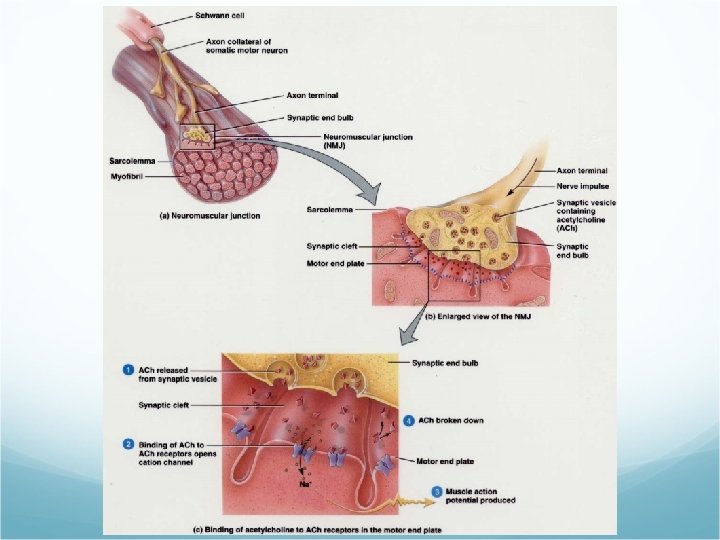
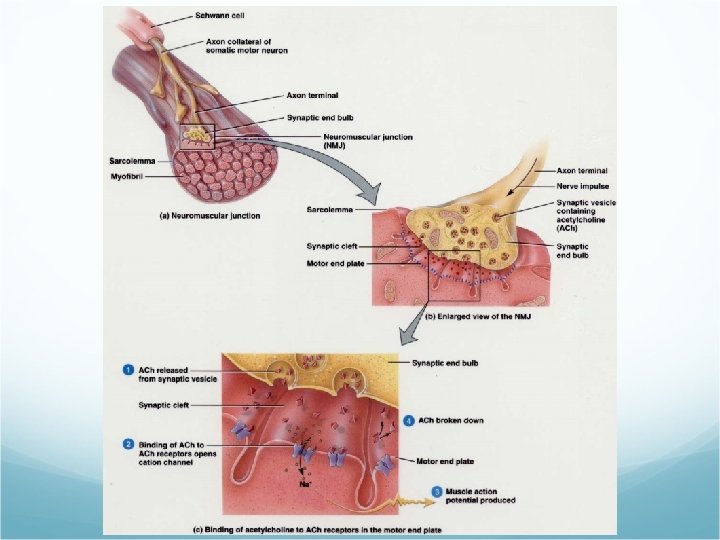
Neuromuscular Junction (NMJ) Muscle action potentials arise at the NMJ. The NMJ is the site at which the motor neuron contacts the skeletal muscle fiber. A synapse is the region where communication occurs.
Neuromuscular Juntcion (NMJ) The neuron cell communicates with the second by releasing a chemical called a neurotransmitter. Synaptic vesicles containing the neurotransmitter acetylcholine (ach) are released at the NMJ. The motor end plate is the muscular part of the NMJ. It contains acetylcholine receptors. The enzyme acetlycholineesterase (ACh. E) breaks down ACh.
Production of ATP 1. From creatine phosphate. When muscle fibers are relaxed they produce more ATP than they need. This excess is used to synthesize creatine phosphate (an energy rich compound).
Production of ATP 2. Anaerobic cellular respiration. Glucose undergoes glycolysis, yielding ATP and 2 molecules of pyruvic acid. Does not require oxygen.
Production of ATP 3. Aerobic cellular respiration. The pyruvic acid enters the mitochondria where it is broken down to form more ATP. Slower than anaerobic respiration, but yields more ATP. Utilizes oxygen. 2 sources of oxygen. Diffuses from bloodstream. Oxygen released from myoglobin.
Muscle Fatigue Muscle fatigue is the inability of a muscle to contract forcefully after prolonged activity. Central fatigue – a person may develop feelings of tiredness before actual muscle fatigue.
Oxygen Debt or Recovery Oxygen Uptake Added oxygen, over and above resting oxygen consumption, taken in after exercise. Used to restore metabolic conditions. 1. To convert lactic acid back into glycogen stores in the liver. 2. To resynthesize creatine phosphate and ATP in muscle fibers. 3. To replace the oxygen removed from hemoglobin.
Motor Units A motor unit consists of the somatic motor neuron and all the skeletal muscle fibers it stimulates. A single motor neuron makes contact with an average of 150 muscle fibers. All muscle fibers in one motor unit contract in unison.
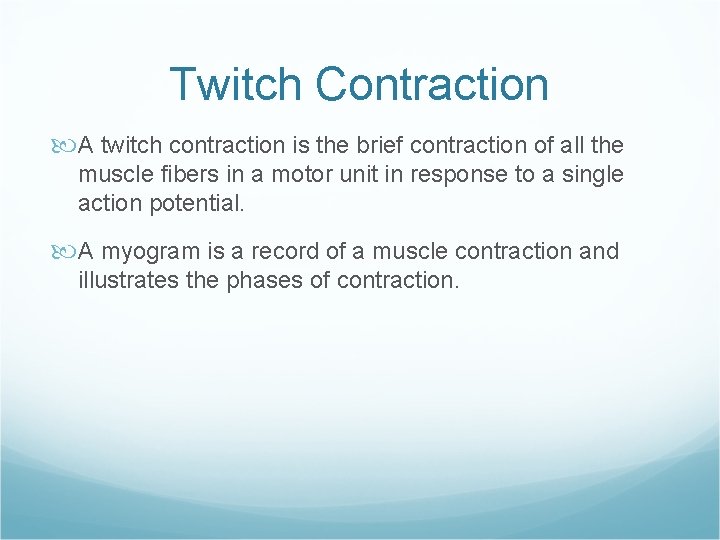
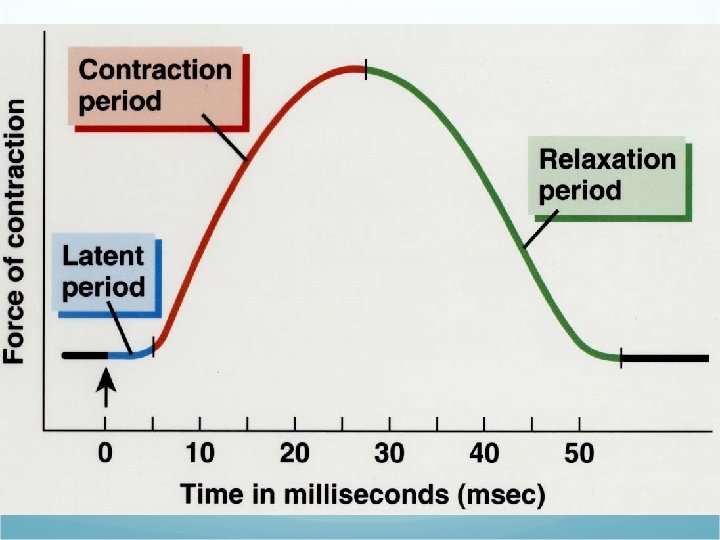
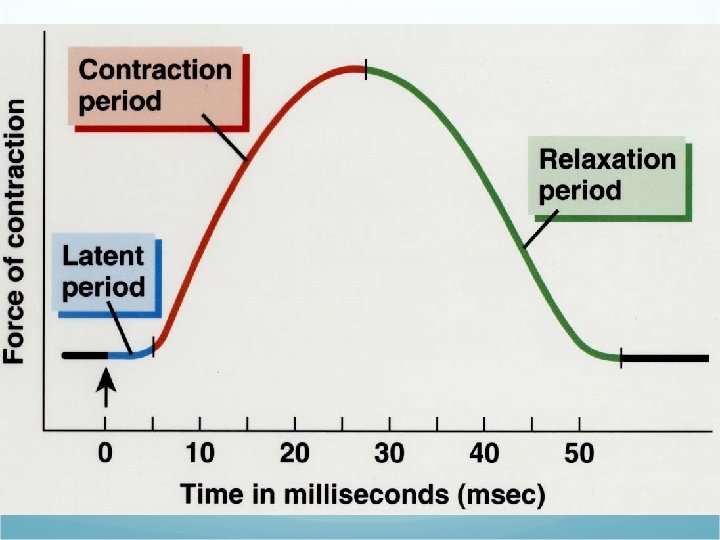
Twitch Contraction A twitch contraction is the brief contraction of all the muscle fibers in a motor unit in response to a single action potential. A myogram is a record of a muscle contraction and illustrates the phases of contraction.
Refractory Period A period of lost excitability during which a muscle fiber cannot respond to stimulation.
Motor Unit Recruitment The process in which the number of active motor units increases. The weakest motor units are recruited first, with progressively stronger units being added if the task requires more force.
Muscle Tone Even at rest a muscle exhibits a small amount of muscle tone – tension or tautness. Flaccid – when motor units serving a muscle are damaged or cut. Spastic – when motor units are over-stimulated.
Isotonic and Isometric Contractions Concentric isotonic contraction – a muscle shortens and pulls on another structure. Eccentric isotonic contraction – the length of a muscle increases during contraction. Isometric contraction – muscle tension is created; However, the muscle doesn’t shorten or lengthen.
Types of Skeletal Muscle Fibers Slow oxidative (SO) fibers. Smallest of the fibers. Least powerful. Appear dark red – much myoglobin and many capillaries. Resistant to fatigue.
Types of Skeletal Muscle Fibers Fast oxidative-Glycolytic (FOG) fibers. Intermediate in diameter. Appear dark red – much myoglobin and many capillaries. High level of intracellular glycogen. Resistant to fatigue.
Types of Skeletal Muscle Fibers Fast Glycolitic (FG) fibers. Largest in diameter. Contain the most myofibrils, therefore more powerful contractions. Appear white – low myoglobin and few capillaries. Large amounts of glycogen – anaerobic respiration. Fatigue quickly.
Distribution and Recruitment of Different Types of Fibers Most skeletal muscles are a mixture of all three types. The continually active postural muscles have a high concentration of SO fibers.
Distribution and Recruitment of Different Types of Fibers Muscles of the shoulders and arms are used briefly and for quick actions, therefore they have many FG fibers. Muscle of the legs support the body and participate in quick activities, therefore they have many SO and FOG fibers.
Cardiac Muscle Tissue The principle tissue in the heart is cardiac muscle tissue. Cardiac muscle fibers have intercalated discs, which connect the ends of the cardiac muscle fibers together. Cardiac muscle tissue remains contracted 10 to 15 times longer than skeletal muscle. Requires a constant supply of oxygen and contains larger and more numerous mitochondria.
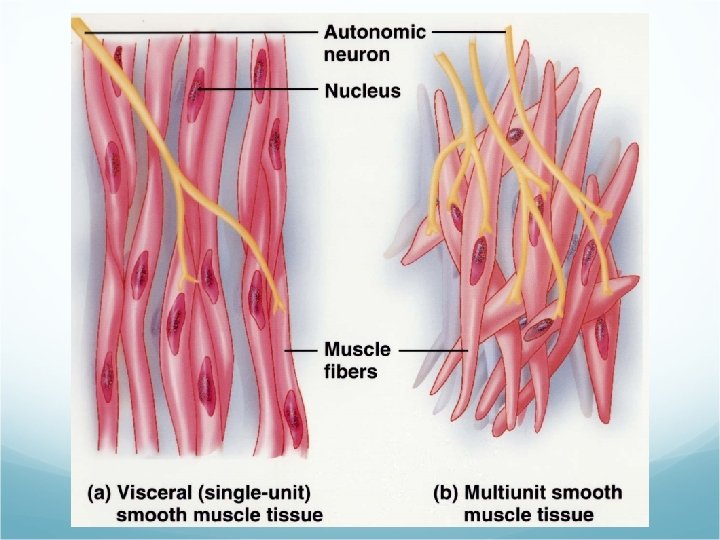
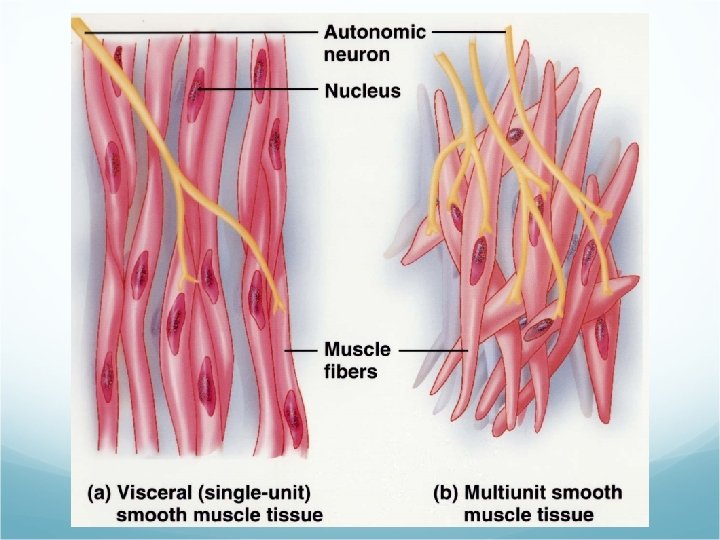
Smooth Muscle Tissue Activated involuntarily. Two types. Visceral (single-unit) smooth muscle. Walls of small blood vessels and walls of hollow organs (I. E. Stomach, intestines, uterus, and urinary bladder). Multi-unti smooth muscle. Walls of large ateries, in the airways of lungs, in arrector pili muscles.
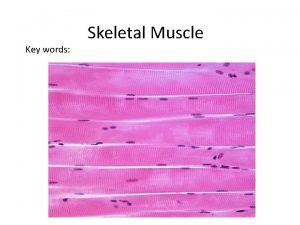
 Skeletal muscle tissue description
Skeletal muscle tissue description Skeletal muscle tissue
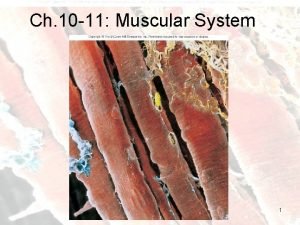
Skeletal muscle tissue Skeletal muscle tissue structure
Skeletal muscle tissue structure Smooth mucle
Smooth mucle Smooth muscle contraction vs skeletal muscle contraction
Smooth muscle contraction vs skeletal muscle contraction Dark a
Dark a Types of muscle tissue
Types of muscle tissue Skeletal muscle location
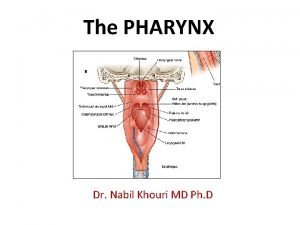
Skeletal muscle location Layers of the pharynx
Layers of the pharynx 5 golden rules of skeletal muscle activity
5 golden rules of skeletal muscle activity Centrally acting skeletal muscle relaxants
Centrally acting skeletal muscle relaxants Dantrolene
Dantrolene Classification of skeletal muscle relaxant
Classification of skeletal muscle relaxant Chlorzoxone
Chlorzoxone Epi peri endo
Epi peri endo Sarcoplasmic
Sarcoplasmic Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Microscopic anatomy of skeletal muscles
Microscopic anatomy of skeletal muscles Epimysium
Epimysium Organization of muscle
Organization of muscle Skeletal muscle pump
Skeletal muscle pump Cardiac muscle cross section
Cardiac muscle cross section Multinucleated muscle cells
Multinucleated muscle cells 5 functions of skeletal system
5 functions of skeletal system Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Microscopic anatomy of skeletal muscle figure 6-2
Microscopic anatomy of skeletal muscle figure 6-2 Chapter 6 the muscular system figure 6-9
Chapter 6 the muscular system figure 6-9 Nerve supply skeletal muscle
Nerve supply skeletal muscle Skeletal muscle belly
Skeletal muscle belly Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Trunk muscles
Trunk muscles Skeletal muscle cylindrical
Skeletal muscle cylindrical Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Lesson 5.1 the organization of a skeletal muscle
Lesson 5.1 the organization of a skeletal muscle Cross bridge myosin head
Cross bridge myosin head Lesson 5.1 the organization of a skeletal muscle
Lesson 5.1 the organization of a skeletal muscle Contraction
Contraction Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Starter which muscles do you already know
Starter which muscles do you already know Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Simple cuboidal epithelium function
Simple cuboidal epithelium function Microscopic anatomy of skeletal muscle figure 6-2
Microscopic anatomy of skeletal muscle figure 6-2 5 golden rules of skeletal muscle activity
5 golden rules of skeletal muscle activity What are t tubules in muscles
What are t tubules in muscles Is skeletal muscle an organ
Is skeletal muscle an organ Skeletal muscle autonomic nervous system
Skeletal muscle autonomic nervous system Skeletal muscle tone
Skeletal muscle tone Cardiac muscle cell vs skeletal
Cardiac muscle cell vs skeletal