MULTIPLE SYSTEM ATROPHY STUDENT INSERVICE BY KELLIE ADAMS
MULTIPLE SYSTEM ATROPHY STUDENT INSERVICE BY KELLIE ADAMS
LEARNING OBJECTIVES The rehabilitation specialist will be able to identify the two different types of Multiple System Atrophy and the distinguishing characteristics of each type to ensure proper rehabilitation treatment based on impairment The rehabilitation specialist will be able to identify the three distinguishable clinical signs for diagnosis of Multiple System Atrophy to allow contribution to diagnosis in a multidisciplinary team The rehabilitation specialist will be able to discuss the neurodegenerative changes in the brain that cause the clinical symptoms associated with Multiple System Atrophy to allow formation of a focused plan of care in rehabilitation The rehabilitation specialist will be able to describe appropriate physical therapy interventions at each stage of mobility decline in MSA: preserved mobility, impaired mobility, and severely compromised mobility to ensure maintenance of patient independence and quality, patient centered care
HISTORY OF MULTIPLE SYSTEMS ATROPHY First described in 1960 by Dr. Milton Shy and Dr. Glen Drager, leading to the less common title of Shy- Drager Syndrome 1 The term “Multiple System Atrophy” was first used in 1969 to include three previously described neurologic disorders: olivopontocerebellar atrophy, autonomic dysfunction, and striatonigral degeneration 2
TYPES OF MULTIPLE SYSTEM ATROPHY 3 MSA- P: MSA- C: Primary characteristics similar to Parkinson’s § Primary characteristics due to cerebellar Disease: dysfunction: Tremors § Ataxia Stiffness § Difficulty swallowing Balance problems § Speech abnormalities Incoordination § Abnormal eye movements ANS dysfunction § ANS dysfunction
DIAGNOSIS OF MULTIPLE SYSTEM ATROPHY Key distinguishing clinical signs at diagnosis include 4: Autonomic failure Poor response to Levodopa Akinetic rigid Parkinsonism OR cerebellar ataxia Presence of widespread Glial Cytoplasmic inclusions are the only reliable criteria for the definitive diagnosis of MSA Diagnosis proposed from clinical history and brief neurological screen 5 Autonomic testing Bladder function screen MRI PET scan Levodopa trial
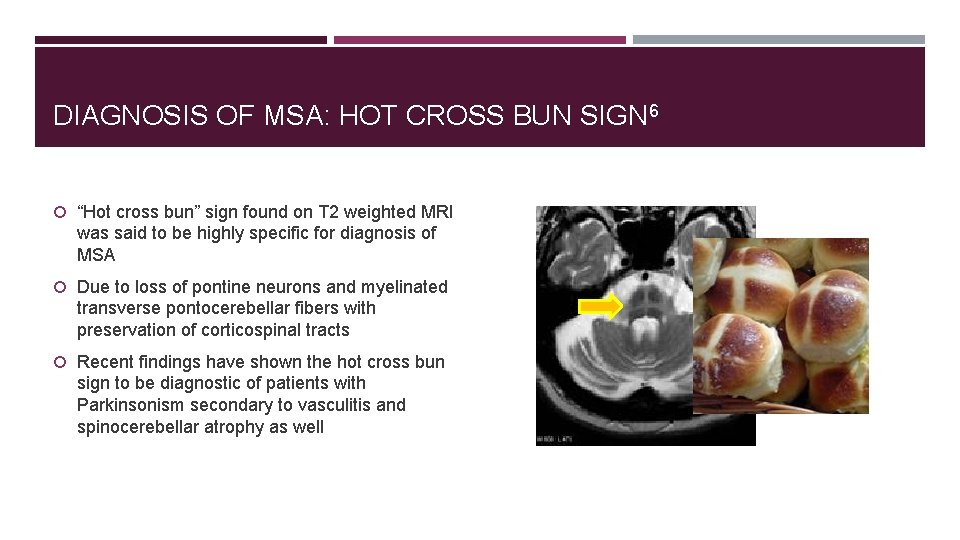
DIAGNOSIS OF MSA: HOT CROSS BUN SIGN 6 “Hot cross bun” sign found on T 2 weighted MRI was said to be highly specific for diagnosis of MSA Due to loss of pontine neurons and myelinated transverse pontocerebellar fibers with preservation of corticospinal tracts Recent findings have shown the hot cross bun sign to be diagnostic of patients with Parkinsonism secondary to vasculitis and spinocerebellar atrophy as well
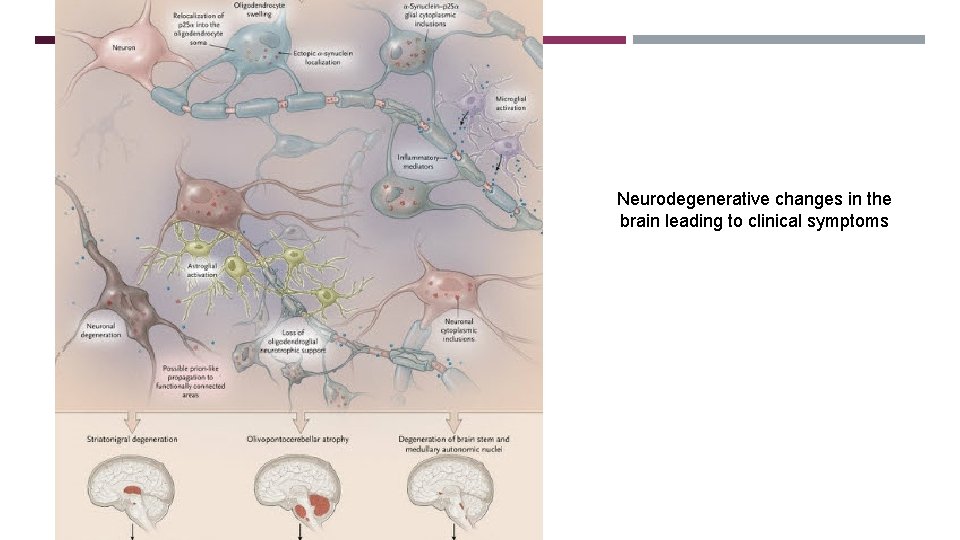
GLIAL CYTOPLASMIC INCLUSIONS Neurodegenerative changes in the brain leading to clinical symptoms
SIGNS AND SYMPTOMS OF MSA 3 Autonomic Symptoms: Motor Symptoms: Fainting spells Loss of muscle control and movement Difficulty controlling heart rate Tremor Bladder control Rigidity Erectile dysfunction Muscle incoordination Orthostatic hypotension Speech difficulties Gait abnormalities Contractures Antecollis Pisa syndrome

PREVALENCE OF MSA 15, 000 -50, 000 Americans suffer from MSA 3 1, 900 new cases per year in the U. S. 7 Incidence of 0. 6 per 100, 000 people worldwide 2 Affects men and women equally across all racial groups 3

ETIOLOGY OF MSA Unknown etiology Nicotine and alcohol consumption are less common among patients with MSA as well as Parkinson’s Disease Majority of cases are sporadic with no known cause In some reported European and Japanese families, MSA has been transmitted in an autosomal recessive or autosomal dominant inheritance pattern 2 Study hypothesized that increased expression of the gene ABCA 8 played a role in pathogenesis of MSA 8: ABCA 8 is a protein encoded by the ABCA 8 gene and was found to be highly expressed in oligodendrocyte-rich white matter regions of the brain Measured expression of ABCA 8, alpha synuclein and p 25 a in MSA brains in disease affected gray matter, disease affected white matter, and an unaffected brain region Findings suggested direct relationship between the levels of ABCA 8 and expression of alpha synuclein and p 25 a; therefore, increased ABCA 8 may precipitate MSA pathology

PROGNOSIS OF MSA Onset is typically in the 50 s with a rapid decline over 5 -10 years with loss of motor function 3 Some patients reported to live as long as 18 years after diagnosis, with majority of patients with MSA passing away 6 -10 years after diagnosis 9 50% of patients require an assistive device for walking within 3 years of diagnosis, 60% require a wheelchair after 6 years, with patients bedridden at a median time after diagnosis of 6 -8 years Negative prognostic factors: older age at onset, MSA-P phenotype, and early development of severe autonomic failure 2
TREATMENTS FOR MSA There are currently no medications to slow the progression of MSA or treat the disease, only medications to treat symptoms 3 Drugs that are used to treat Parkinson’s Disease, such as Levodopa, may be prescribed; however, in many cases patient’s respond poorly and effectiveness decreases over time 7 Physical therapy Occupational therapy Speech language pathology
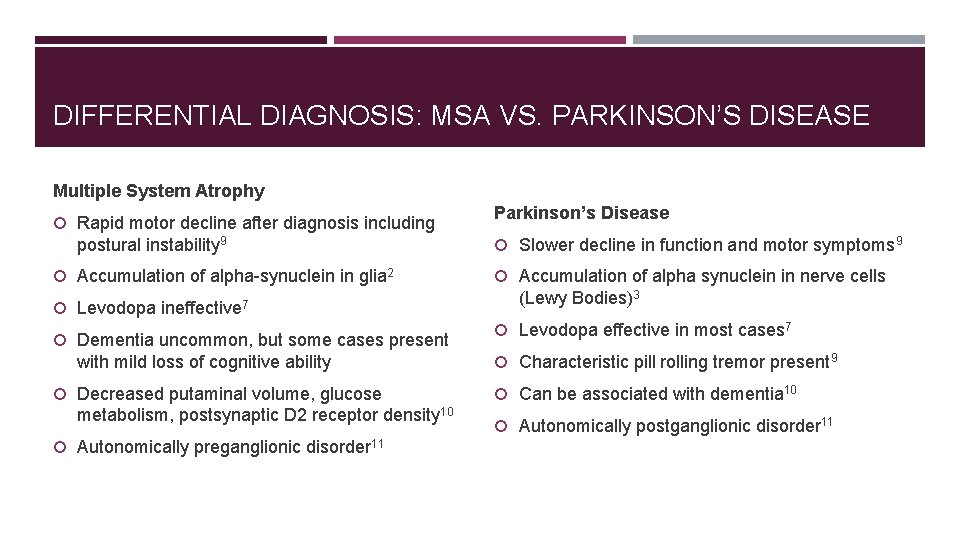
DIFFERENTIAL DIAGNOSIS: MSA VS. PARKINSON’S DISEASE Multiple System Atrophy Rapid motor decline after diagnosis including postural instability 9 Accumulation of alpha-synuclein in glia 2 Levodopa ineffective 7 Dementia uncommon, but some cases present with mild loss of cognitive ability Decreased putaminal volume, glucose metabolism, postsynaptic D 2 receptor density 10 Autonomically preganglionic disorder 11 Parkinson’s Disease Slower decline in function and motor symptoms 9 Accumulation of alpha synuclein in nerve cells (Lewy Bodies)3 Levodopa effective in most cases 7 Characteristic pill rolling tremor present 9 Can be associated with dementia 10 Autonomically postganglionic disorder 11
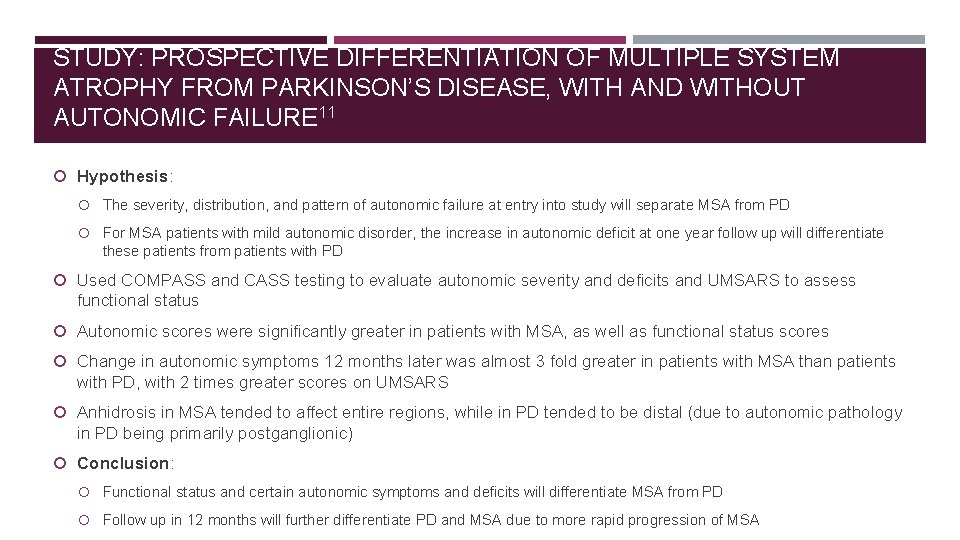
STUDY: PROSPECTIVE DIFFERENTIATION OF MULTIPLE SYSTEM ATROPHY FROM PARKINSON’S DISEASE, WITH AND WITHOUT AUTONOMIC FAILURE 11 Hypothesis: The severity, distribution, and pattern of autonomic failure at entry into study will separate MSA from PD For MSA patients with mild autonomic disorder, the increase in autonomic deficit at one year follow up will differentiate these patients from patients with PD Used COMPASS and CASS testing to evaluate autonomic severity and deficits and UMSARS to assess functional status Autonomic scores were significantly greater in patients with MSA, as well as functional status scores Change in autonomic symptoms 12 months later was almost 3 fold greater in patients with MSA than patients with PD, with 2 times greater scores on UMSARS Anhidrosis in MSA tended to affect entire regions, while in PD tended to be distal (due to autonomic pathology in PD being primarily postganglionic) Conclusion: Functional status and certain autonomic symptoms and deficits will differentiate MSA from PD Follow up in 12 months will further differentiate PD and MSA due to more rapid progression of MSA
PARKINSON PLUS DISORDERS 12 Multiple System Atrophy considered to be a “Parkinson Plus Syndrome” Group of heterogeneous neurological disorders Differ from idiopathic Parkinson’s disease in clinical features, poor response to levodopa, distinctive pathological characteristics, and poor prognosis Dementia with Lewy Body Disease Multiple System Atrophy Progressive Supranuclear Palsy Final diagnosis based on autopsy study

REHABILITATION STRATEGIES FOR PATIENTS WITH MSA Multiple System Atrophy Coalition https: //www. multiplesystematrophy. org
PHYSICAL THERAPY 4 Stage 1: Preserved Mobility Management of autonomic symptoms Encourage active lifestyle and exercise: pilates, tai chi, walking the dog Exercise should focus on high level balance, strength, aerobic training Identify falls risk Avoid compensatory motor patterns at this stage MSA-C: focus on posture, balance, and gait while considering role of vision
PHYSICAL THERAPY Stage II: Impaired Mobility Encourage maintenance of activity May include compensations and/or assistive devices Remove causes of falls including creating a safer environment Stretching and assess for contractures Gait training: focus on taking large steps and heel strike, safe turns while avoiding pivoting and crossing one foot over the other Orthotics Seated exercises
PHYSICAL THERAPY Stage III: Severely Compromised Mobility Wheelchair assessment Skills for transfer and bed mobility Positioning Caregiver support and education Breathing techniques, assisted cough if appropriate

PHYSICAL THERAPY LSVT Big Program 13 Increased amplitude movements in limb and body centered around patients with PD Documented improvements in amplitude and speed of movement, balance, and quality of life 16 sessions over a 1 month period- 4 hour long sessions per week May help patients with Multiple System Atrophy in the short term
OCCUPATIONAL THERAPY 14 Teach compensatory strategies as needed: Adaptive devices Arm positioning when eating Educate on placing less blankets or using satin sheets in the bed to allow for easier bed mobility Dress affected limb first Sit when dressing, bathing, self-care Supporting with one hand on sturdy surface while reaching Side step when working at the counter-space or sink
OUTCOME MEASURE: UNIFIED MULTIPLE SYSTEM ATROPHY RATING SCALE 15 UMSARS Assesses 4 domains: impairment and functional tasks, motor ability, autonomic function, global disability Good psychometric properties including: internal consistency, interrater reliability, and criterion validity Scores range from 0 -104 with higher score= greater impairment https: //www. movementdisorders. org/MDS-Files 1/PDFs/MDS-UPDRS-Rating-Scales/scale_UMSARS. pdf
PATIENT CASE: MR. S 64 years old Diagnosed in 2013 at 59 years old Worked as a nuclear physicist for the CIA for 23 years Retired early due to progression of disease- having difficulty driving, walking, typing
PATIENT CASE: MR. S Signs and symptoms began prior to diagnosis: Difficulty swimming (collegiate swimmer, swam regularly for exercise) Swayed to the right when walking Grabbed onto sturdy objects for stability- poor balance Erectile dysfunction Bladder control problems at night
PATIENT CASE: MR. S Evaluated by neurologists, movement disorder specialists Sought numerous opinions from specialists at John Hopkins, Georgetown, NIH Multiple specialists suspected a Parkinson Plus syndrome, came to eventual diagnosis of MSA
PATIENT CASE: MR. S Current: No longer to negotiate stairs- moved to a single-story home Primary form of mobility is a manual wheelchair with others pushing him Gait is very slow with poor balance, uncoordination Requires assistance eating, bathing, shaving, dressing, using the bathroom No longer able to self-cath- uses a supra-pubic catheter Suffers from orthostatic hypotension- dizziness, fainting, falling

PATIENT CASE- MR. S Caregiver comes daily for 4 hours Lives with wife, 3 sons live close by and come over daily to check on him Receives home health PT, OT, SLP twice weekly- focus on functional mobility and preserving strength

PATIENT CASE- MR. S Challenges: Mr. S is very angry about his circumstances, “his world has become very small” Personality has changed- has become self-absorbed and doesn’t always recognize what his family members do for him on a daily basis Hobbies: watches movies, playing chess, listens to podcasts about physics
REFERENCES 1. History of Multiple System Atrophy (MSA), A Neurodegenerative Disorder. Multiple System Atrophy: The MSA Coalition. https: //www. multiplesystematrophy. org/about-msa/history-of-msa. Accessed April 19, 2018. 2. Longo DL, Fanciulli A, Wenning GK. Multiple-system atrophy. N Engl J Med. 2015; 372(3): 249 -263. http: //libproxy. lib. unc. edu/login? url=https: //search-proquestcom. libproxy. lib. unc. edu/docview/1645924181? accountid=14244. 3. Multiple System Atrophy Fact Sheet. National Institute of Neurological Disorders and Stroke. https: //www. ninds. nih. gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Multiple-System-Atrophy. Modified January 23, 2018. Accessed April 19, 2018. 4. Lord S, Mhiripiri D. A Guide to Multiple System Atrophy for: Physiotherapists. Multiple System Atrophy Trust. https: //www. msatrust. org. uk/wp-content/uploads/2015/11/FS 830 -Guide-for-Physiotherapists_v 1. 2. pdf. Published November 2014. Accessed April 19, 2018. 5. Ciolli L, Krismer F, Nicoletti F, Wenning GK. An update on the cerebellar subtype of multiple system atrophy. Cerebellum & Ataxias. https: //cerebellumandataxias. biomedcentral. com/articles/10. 1186/s 40673 -014 -0014 -7. Published October 10, 2014. Accessed April 19, 2018.
REFERENCES 6. Muqit MM, Mort D, Miszkiel KA, Shakir RA. "Hot cross bun" sign in a patient with parkinsonism secondary to presumed vasculitis. Journal of Neurology, Neurosurgery & Psychiatry. http: //jnnp. bmj. com/content/71/4/565. Published October 1, 2001. Accessed April 19, 2018. 7. Multiple System Atrophy. NORD (National Organization for Rare Disorders). https: //rarediseases. org/rare- diseases/multiple-system-atrophy/. Accessed April 19, 2018. 8. Bleasel JM, Hsiao JH, Halliday GM, Kim WS. Increased expression of ABCA 8 in multiple system atrophy brain is associated with changes in pathogenic proteins. Journal of Parkinson's disease. https: //www. ncbi. nlm. nih. gov/pubmed/23948991. Published January 1, 2013. Accessed April 19, 2018. 9. Differential Diagnosis for Multiple System Atrophy, a Disorder Similar to Parkinson's Disease. Multiple System Atrophy: The MSA Coalition. https: //www. multiplesystematrophy. org/about-msa/differential-diagnosis. Accessed April 19, 2018. 10. Ghaemi M, Hilker R, Rudolf J, Subesky J, Heiss WD. Differentiating multiple system atrophy from Parkinson's disease: contribution of striatal and midbrain MRI volumetry and multi-tracer PET imaging. Journal of Neurology, Neurosurgery & Psychiatry. http: //jnnp. bmj. com/content/73/5/517? utm_source=Trend. MD&utm_medium=cpc&utm_campaign=J_Neurol_N eurosurg_Psychiatry_Trend. MD_1. Published November 1, 2002. Accessed April 19, 2018.

REFERENCES 11. Lipp A, Sandroni P, Ahlskog JE, et al. Prospective Differentiation of Multiple System Atrophy from Parkinson's Disease, with and without Autonomic Failure. Archives of neurology. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 2838493/. Published June 2009. Accessed April 19, 2018. 12. Mitra K. Parkinson plus syndrome- a review. Neurology India. 2003; 51(2): 183 -188. doi: 10. 1075/ps. 5. 3. 02 chi. audio. 2 f. 13. What is LSVT BIG? LSVT Global - What is LSVT BIG? https: //www. lsvtglobal. com/patient- resources/what-is-lsvt-big. Accessed April 19, 2018. 14. A Guide to Multiple System Atrophy for: Occupational Therapists. Multiple System Atrophy Trust. https: //www. msatrust. org. uk/wp-content/uploads/2015/11/FS 810 -Guide-to-MSA-for-Occupational. Therapists. pdf. Published February 2016. Accessed April 19, 2018. 15. Wenning G, et al. Development and Validation of the Unified Multiple System Atrophy Rating Scale (UMSARS). Movement Disorderes. 2004; 19: 1391 -1402. https: //www. movementdisorders. org/MDSFiles 1/PDFs/Rating-Scales/umsars. pdf.

Questions?
- Slides: 32