Multiple Sclerosis Overview for Dentists What does MS

- Slides: 41
Multiple Sclerosis: Overview for Dentists
What does MS look like? • Julia—a 35 yo white married mother of 3 who is exhausted all the time and can’t drive because of vision problems and numbness in her feet • Jackson—a 25 yo African-American man who stopped working because he can’t control his bladder or remember what he read in the morning paper • Maria—a 10 yo Hispanic girl who falls down a lot and whose parents just told her she has MS • Loretta—a 47 yo white single woman who moved into a nursing home because she can no longer care for herself
What else does MS look like? • Sam—a 45 yo divorced white man who has looked and felt fine since he was diagnosed seven years ago • Karen—a 24 yo single white woman who is severely depressed and worried about losing her job because of her diagnosis of MS • Sandra—a 30 yo single mother of two who experiences severe burning pain in her legs and feet • Richard—who was found on autopsy at age 76 to have MS but never knew it • Jeannette—whose tremors are so severe that she cannot feed herself
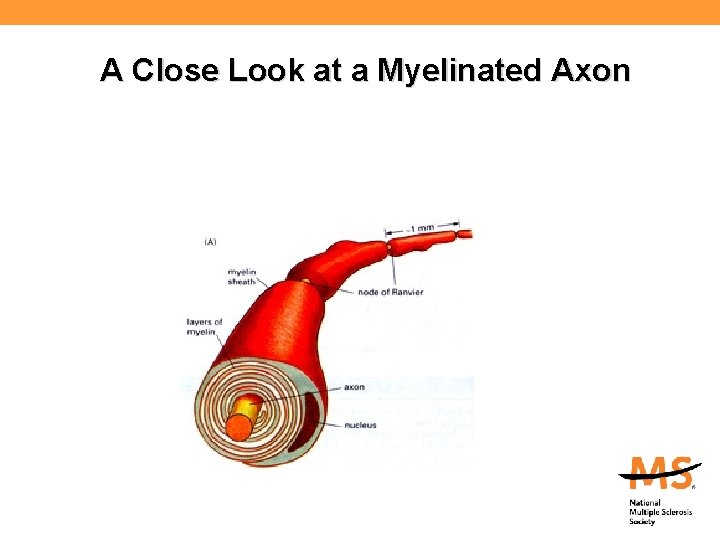
What MS Is: • MS is thought to be a disease of the immune system— possibly autoimmune. • The primary targets of the immune attack are the myelin coating around the nerves in the central nervous system (CNS—brain, spinal cord, and optic nerves) and the nerve fibers themselves. • Its name comes from the scarring caused by inflammatory attacks at multiple sites in the central nervous system.
What MS Is Not: • MS is not: – Contagious – Directly inherited – Always severely disabling – Fatal—except in fairly rare instances • Being diagnosed with MS is not a reason to: – Stop working – Stop doing things that one enjoys – Not have children
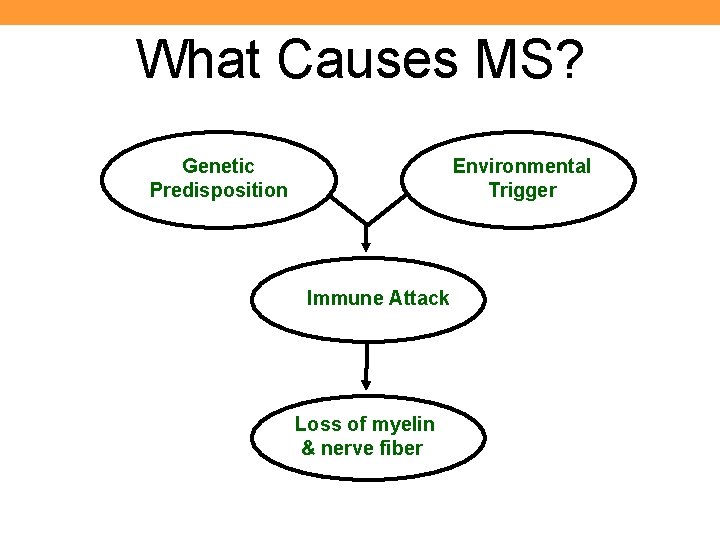
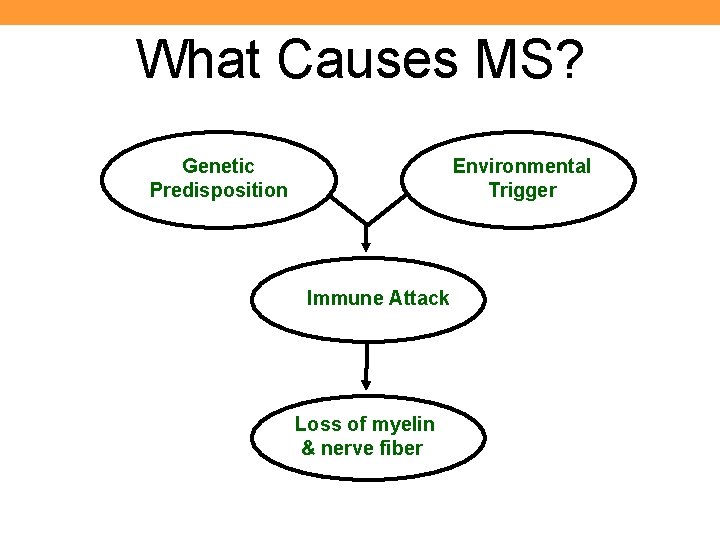
What Causes MS? Genetic Predisposition Environmental Trigger Immune Attack Loss of myelin & nerve fiber
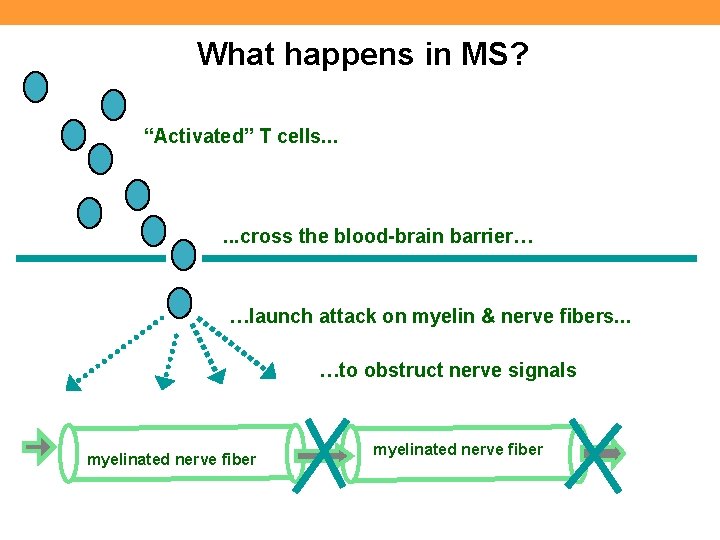
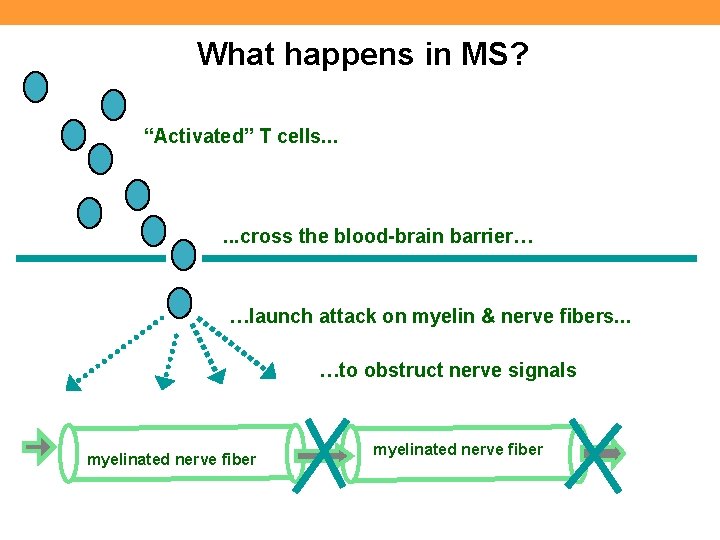
What happens in MS? “Activated” T cells. . . cross the blood-brain barrier… …launch attack on myelin & nerve fibers. . . …to obstruct nerve signals myelinated nerve fiber
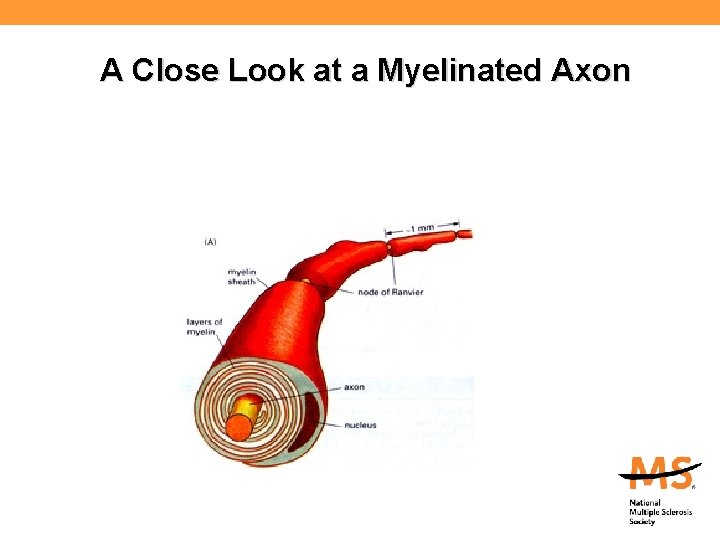
A Close Look at a Myelinated Axon
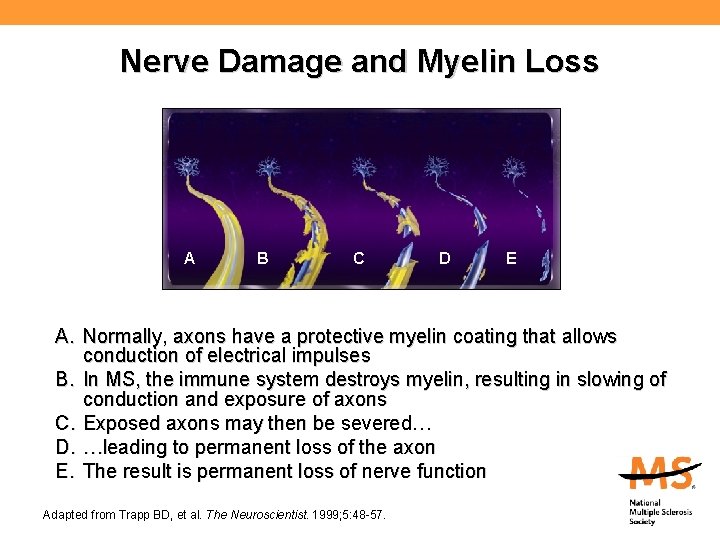
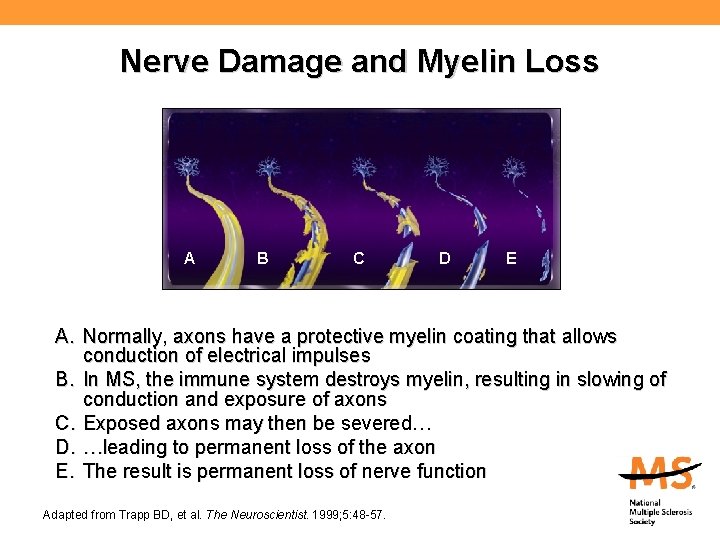
Nerve Damage and Myelin Loss A B C D E A. Normally, axons have a protective myelin coating that allows conduction of electrical impulses B. In MS, the immune system destroys myelin, resulting in slowing of conduction and exposure of axons C. Exposed axons may then be severed… D. …leading to permanent loss of the axon E. The result is permanent loss of nerve function Adapted from Trapp BD, et al. The Neuroscientist. 1999; 5: 48 -57.
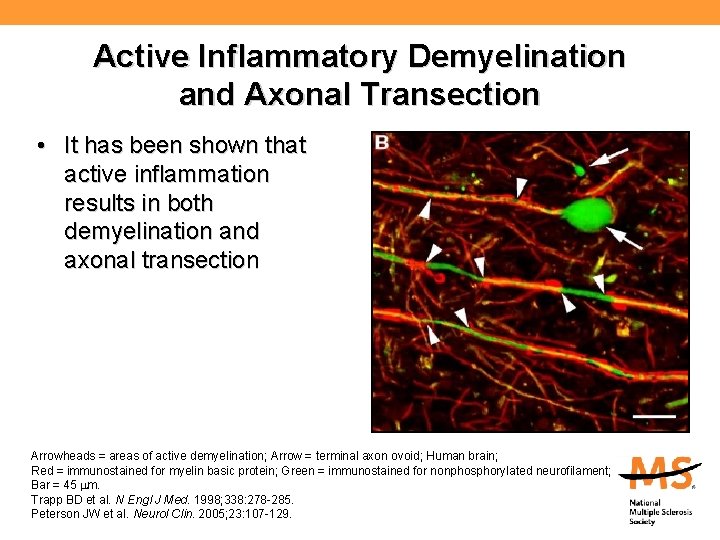
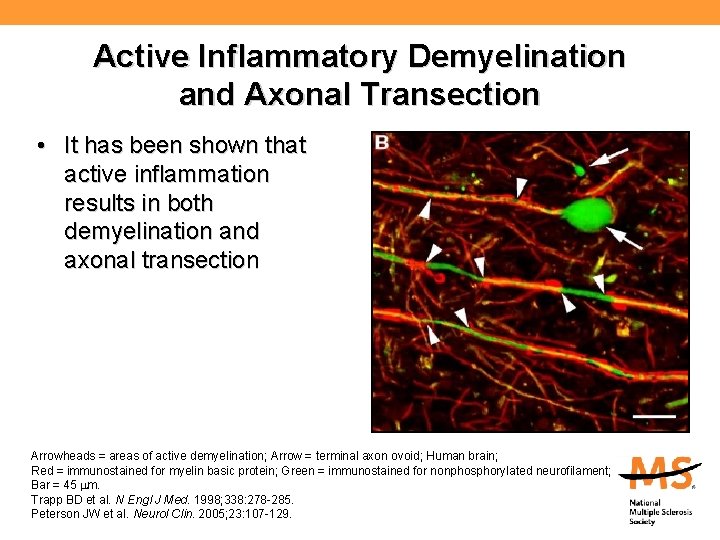
Active Inflammatory Demyelination and Axonal Transection • It has been shown that active inflammation results in both demyelination and axonal transection Arrowheads = areas of active demyelination; Arrow = terminal axon ovoid; Human brain; Red = immunostained for myelin basic protein; Green = immunostained for nonphosphorylated neurofilament; Bar = 45 m. Trapp BD et al. N Engl J Med. 1998; 338: 278 -285. Peterson JW et al. Neurol Clin. 2005; 23: 107 -129.
How is MS diagnosed? • MS is a clinical diagnosis: – Signs and symptoms – Medical history – Laboratory tests • Requires dissemination in time and space: – Space: Evidence of scarring (plaques) in at least two separate areas of the CNS (space) – Time: Evidence that the plaques occurred at different points in time • There must be no other explanation
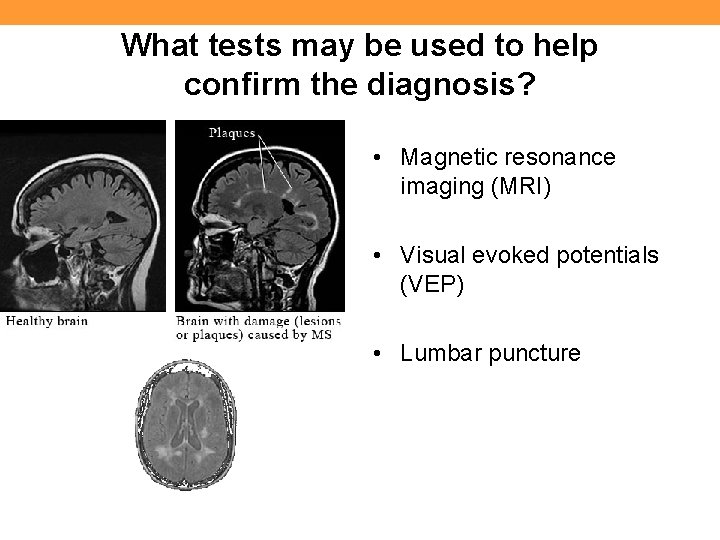
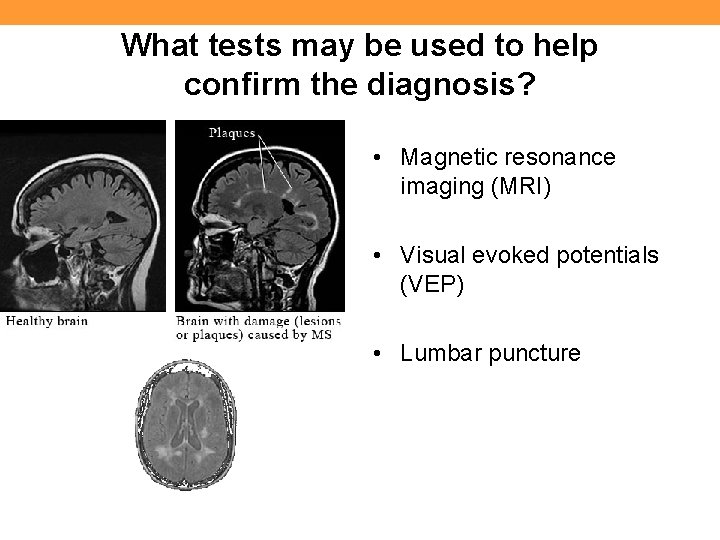
What tests may be used to help confirm the diagnosis? • Magnetic resonance imaging (MRI) • Visual evoked potentials (VEP) • Lumbar puncture
Who gets MS? • Usually diagnosed between 20 and 50 – Occasionally diagnosed in young children and older adults • More common in women than men (>2 -3: 1) • Most common in those of Northern European ancestry – More common in Caucasians than Hispanics or African Americans; rare among Asians • More common in temperate areas of the world
The genetic factor in MS • The risk of getting MS is approximately: – 1/750 for the general population (0. 1%) – 1/40 for person with a close relative with MS (3%) – 1/4 for an identical twin (25%) • 20% of people with MS have a blood relative with MS The risk is higher in any family in which there are several family members with the disease (multiplex families)
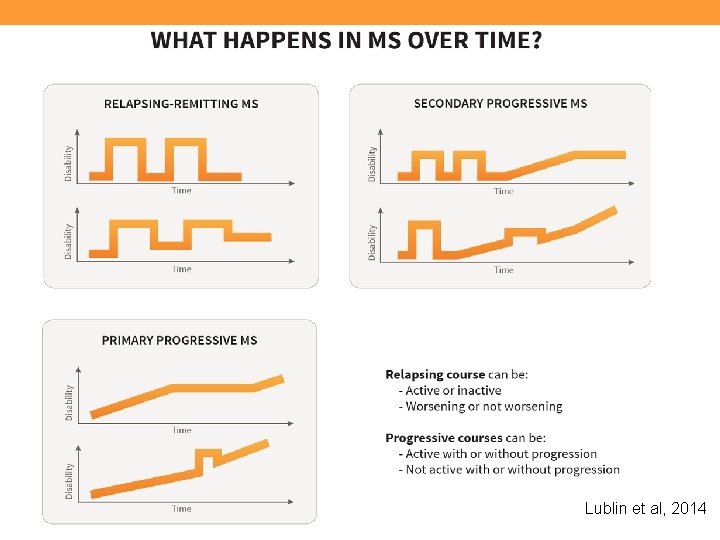
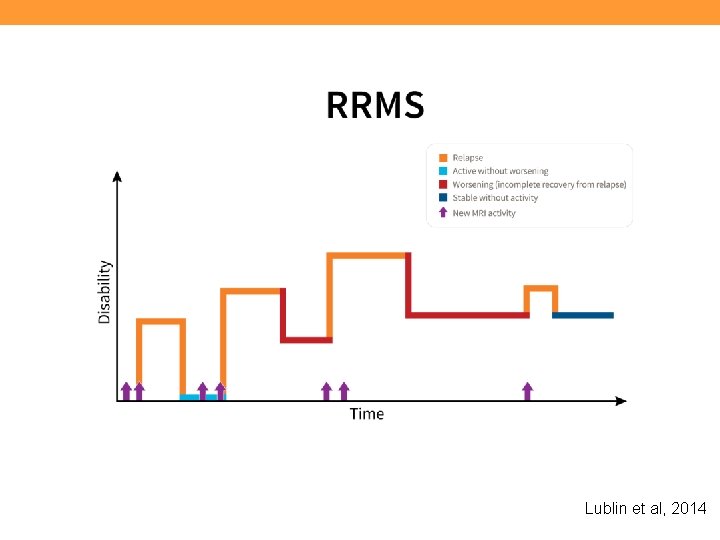
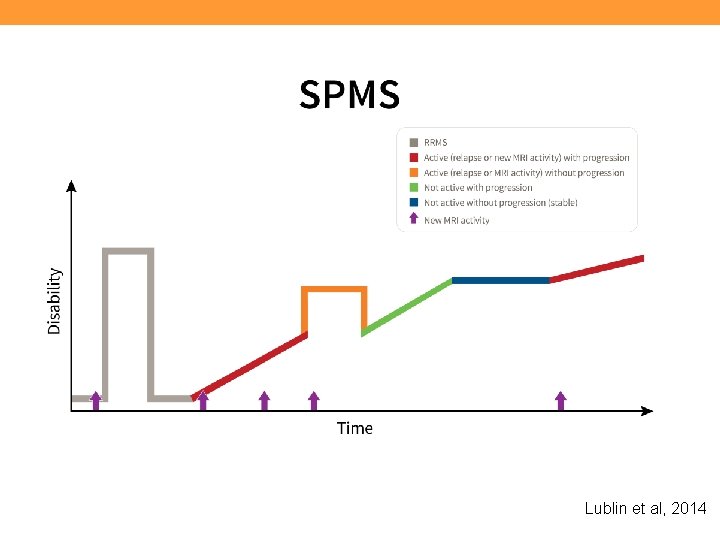
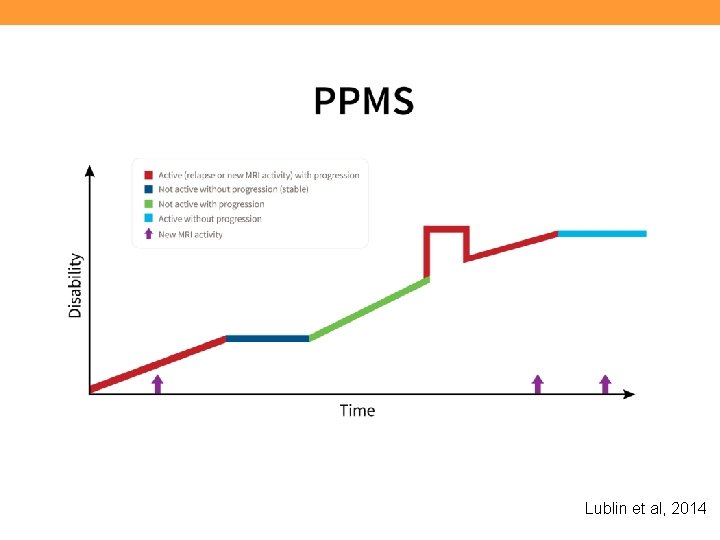
Disease Types • Clinically isolated syndrome (CIS) • Relapsing-remitting MS (RRMS) – About 85% of people are diagnosed with RRMS • Primary progressive MS (PPMS) – About 15% of people experience this course • Secondary progressive – Most people diagnosed with RRMS will eventually transition to SPMS Lublin et al, 2014
Clinically Isolated Syndrome (CIS) • A first neurologic event suggestive of demyelination • Individuals with CIS are at high risk for developing clinically definite MS if the neurologic event is accompanied by multiple, clinically silent (asymptomatic) lesions on MRI typical of MS
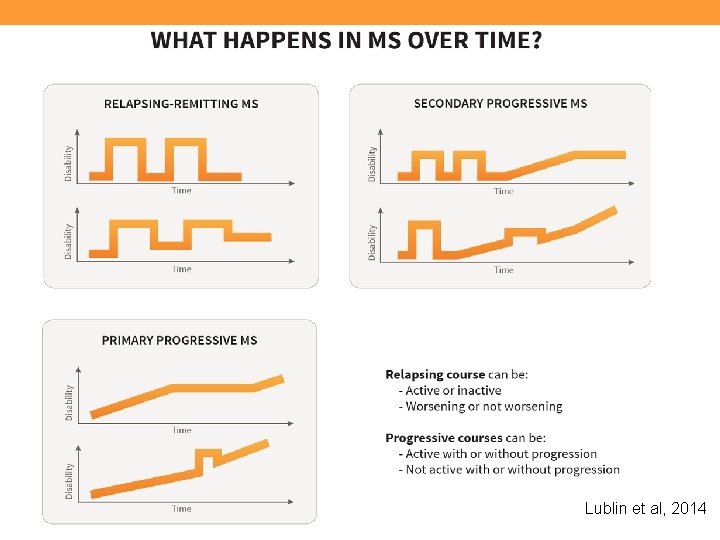
Lublin et al, 2014
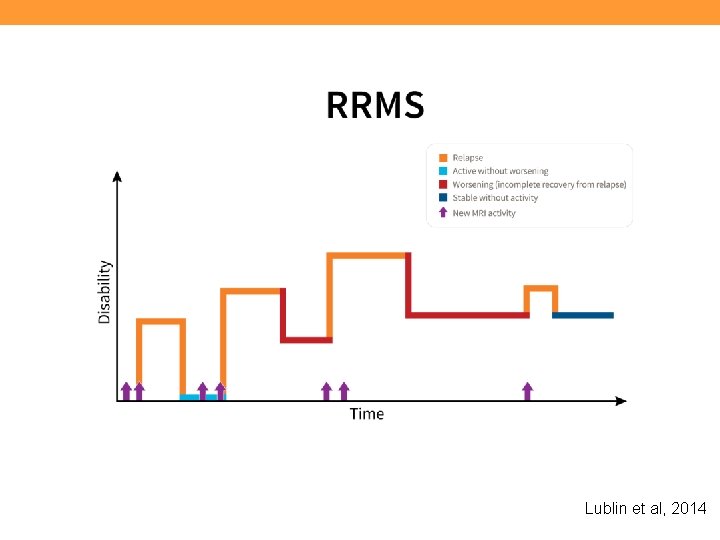
Lublin et al, 2014
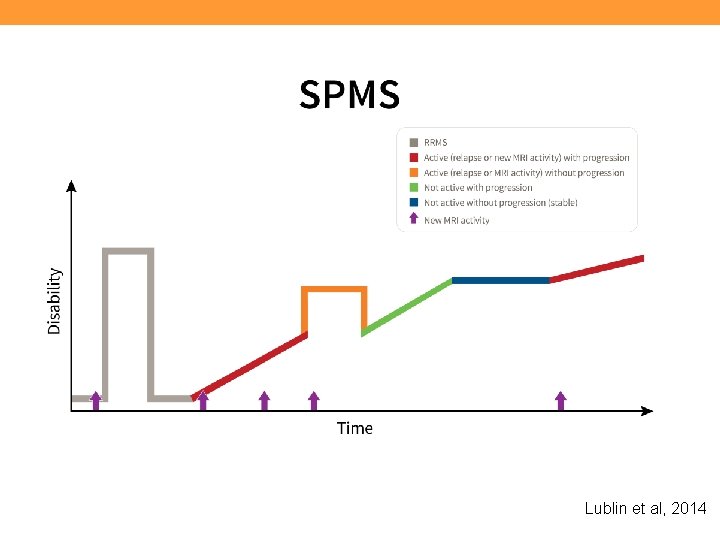
Lublin et al, 2014
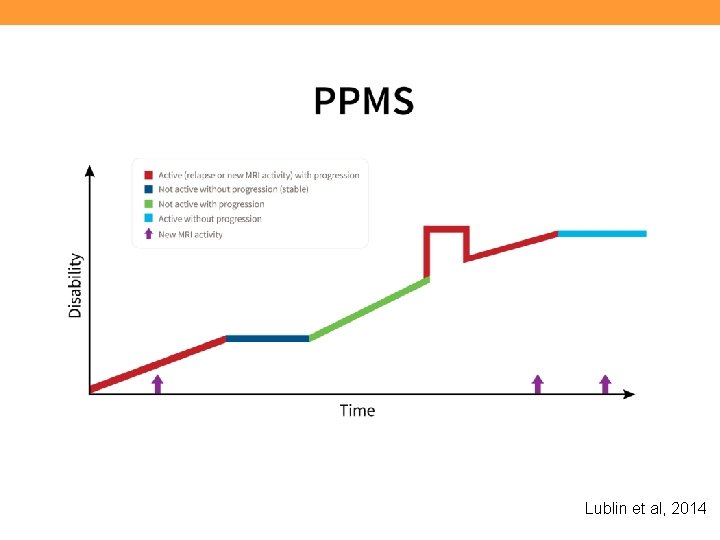
Lublin et al, 2014
Managing Multiple Sclerosis • A complex disease requiring a multi-pronged approach that involves many clinical disciplines: – Disease Management – Relapse Management – Symptom Management – Rehabilitation – Psychosocial Support
Management of Multiple Sclerosis The MS “Treatment Team”: • • Neurologist Urologist Nurse Primary care physician Physiatrist Physical therapist Occupational therapist Speech/language pathologist • • Psychiatrist Psychotherapist Neuropsychologist Social worker/Care manager • Pharmacist

FDA-Approved Disease-Modifying Drugs Drug Origin Dosage Freq Route Glatiramer acetate Random polypeptides 20 mg/40 mg Every day/3 x/wk SC IFNb-1 b Recombinant protein 0. 25 mg Every other day SC IFNb-1 a IM Recombinant protein 30 mcg 1 x/wk IM IFNb-1 a SC Recombinant protein 22 mcg 44 mcg 125 mg 3 x/wk IFNb-1 a SC SC 2 x/mo Dimethyl fumarate Oral formulation of dimethyl fumarate rapidly hydrolyzed to monomethyl fumarate 24 o mg Twice daily Oral Fingolimod Sphingosine 1 -phosphate receptor modulator 0. 5 mg Every day Oral Teriflunomide De novo pyrimidine synthesis inhibitor of the DHO-DH enzyme 7 mg or 14 mg Daily Oral Alemtuzumab CD 52 -directed cytolytic Mab 12 mg/day 5 consecutive days 3 consecutive days 12 mos. later IV infusion Mitoxantrone Chemotherapy 12 mg/m 2 (cumulative lifetime dose < 140 mg/m 2) Every 3 months IV infusion
Managing Progressive MS • Azathiorpine (Imuran) • Methotrexate • Mitoxantrone (Novantrone) • Monthly administration of methylprednisolone • IVIg. G • Cladribine • Cytoxan • Bone marrow transplantation
Relapse Management • Relapse = new symptom or sudden worsening of old symptom lasting at least 24 hours, and usually accompanied by a finding • Treatment with corticosteroids recommended if relapse significantly interferes with everyday functioning – 3 -5 day course of high-dose intravenous methylprednisolone with or without oral taper – High-dose oral steroids may also be used • Rehabilitation can help restore function following a relapse
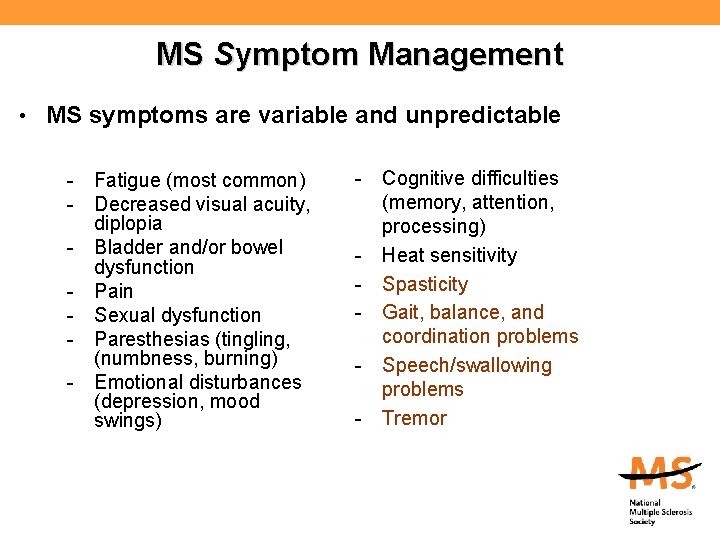
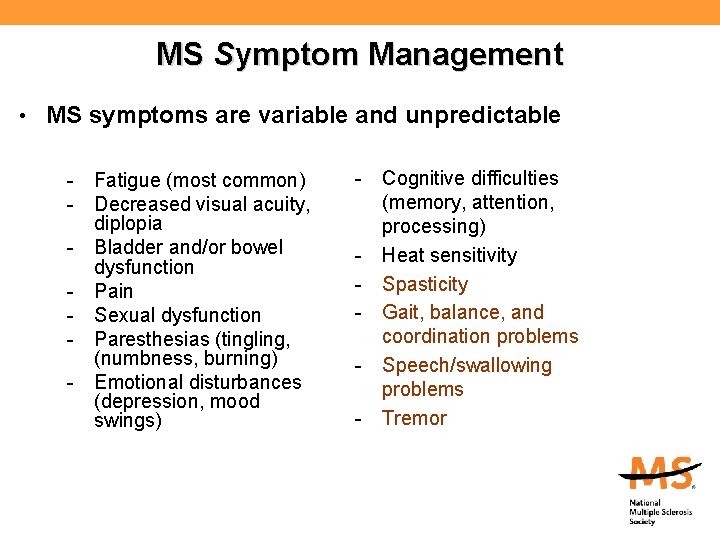
MS Symptom Management • MS symptoms are variable and unpredictable - Fatigue (most common) - Decreased visual acuity, diplopia - Bladder and/or bowel dysfunction - Pain - Sexual dysfunction - Paresthesias (tingling, (numbness, burning) - Emotional disturbances (depression, mood swings) - Cognitive difficulties (memory, attention, processing) - Heat sensitivity - Spasticity - Gait, balance, and coordination problems - Speech/swallowing problems - Tremor
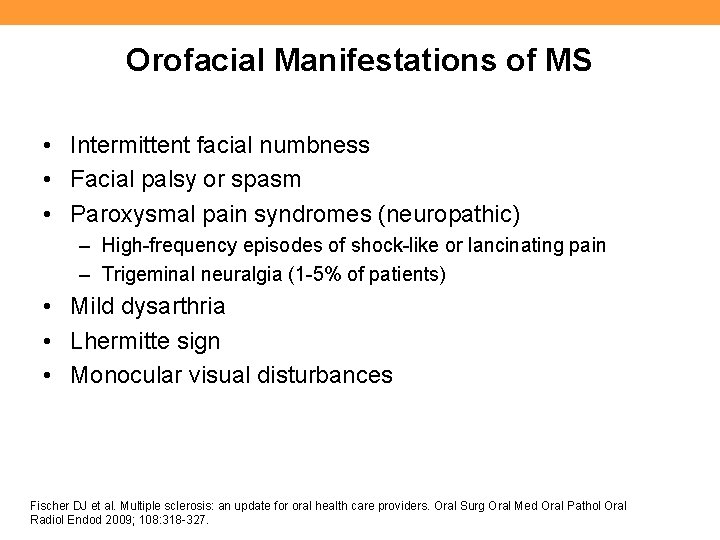
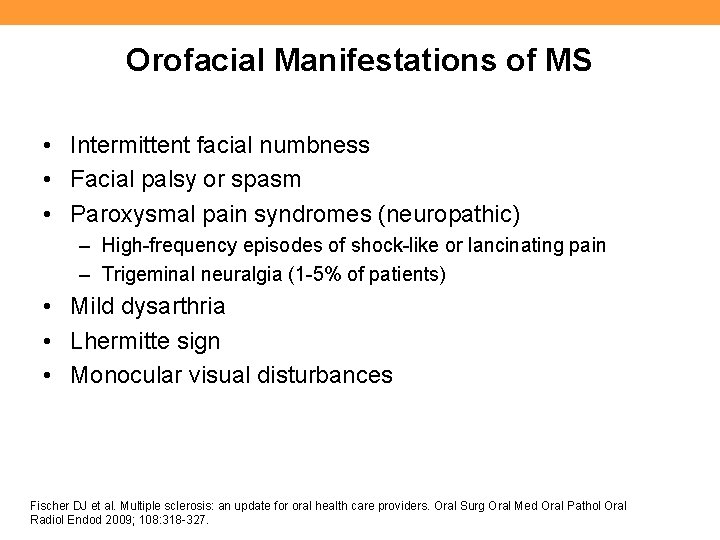
Orofacial Manifestations of MS • Intermittent facial numbness • Facial palsy or spasm • Paroxysmal pain syndromes (neuropathic) – High-frequency episodes of shock-like or lancinating pain – Trigeminal neuralgia (1 -5% of patients) • Mild dysarthria • Lhermitte sign • Monocular visual disturbances Fischer DJ et al. Multiple sclerosis: an update for oral health care providers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 318 -327.
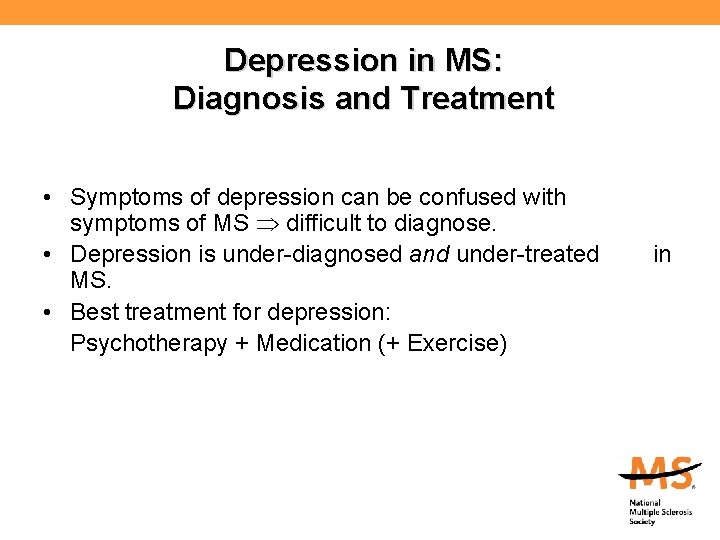
Depression in MS: Diagnosis and Treatment • Symptoms of depression can be confused with symptoms of MS difficult to diagnose. • Depression is under-diagnosed and under-treated MS. • Best treatment for depression: Psychotherapy + Medication (+ Exercise) in
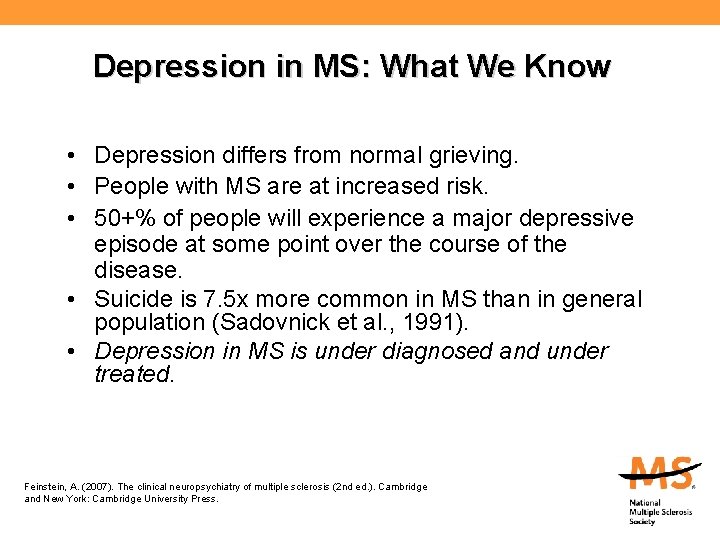
Depression in MS: What We Know • Depression differs from normal grieving. • People with MS are at increased risk. • 50+% of people will experience a major depressive episode at some point over the course of the disease. • Suicide is 7. 5 x more common in MS than in general population (Sadovnick et al. , 1991). • Depression in MS is under diagnosed and under treated. Feinstein, A. (2007). The clinical neuropsychiatry of multiple sclerosis (2 nd ed. ). Cambridge and New York: Cambridge University Press.
Cognitive Functions Affected in MS • • • Memory - acquisition and retrieval Attention & concentration - working memory Speed of information processing Executive Functioning Visual/spatial organization Verbal fluency - word finding De. Luca, J. What we know about cognitive changes in multiple sclerosis. In La. Rocca, N & Kalb, R (eds. ) Multiple sclerosis: understanding the cognitive challenges. New York: Demos Medical Publishing, 2006.
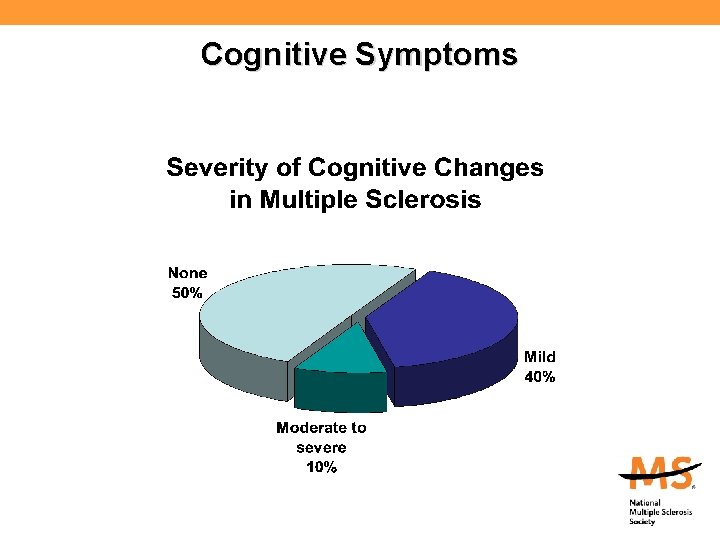
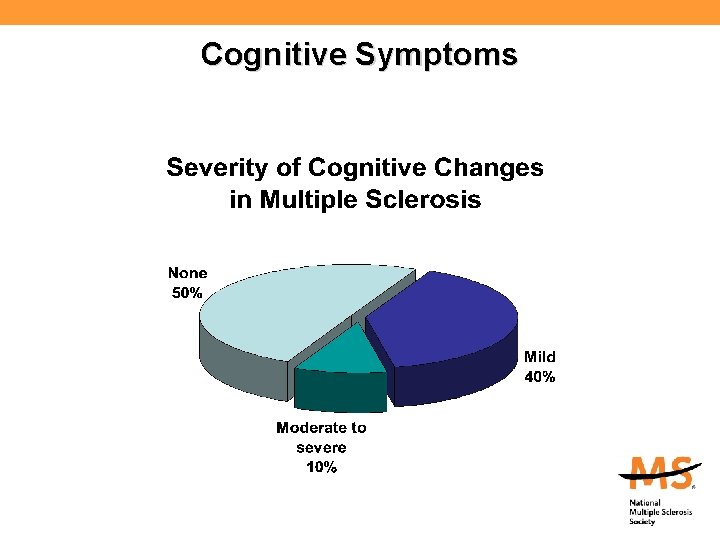
Cognitive Symptoms
Cognitive Functions Unaffected in MS • • • General intellect Long-term (remote) memory Recognition memory Conversational skill Reading comprehension
Common Misconceptions about MS and cognition • Cognitive impairment (CI) is rare in MS. • CI only occurs in late stage MS or severe MS. • MS is a white-matter disease and does not affect: 1) brain volume, 2) gray matter, 3) the cerebral cortex. • If an MS patient can pass the mental status exam, everything is OK. • Memory problems reported by MS patients are caused by stress, anxiety, and/or depression. • Discussing CI will upset MS patients/families.
Cognition and Other Disease Characteristics • Cognitive function correlates with lesion load and brain atrophy. • Cognitive dysfunction can occur at any time (even as a first symptom) but is more common later on. • Cognitive dysfunction can occur with any disease course, but is more likely in progressive MS. • Being in an exacerbation is a risk factor for cognitive dysfunction. • Depression can worsen cognition, particularly executive functions (Arnett et al. , 1999). La. Rocca N, Kalb R. Multiple Sclerosis: Understanding the Cognitive Challenges. New York: Demos Medical Publishing, 2006.
MS-Related Stresses for Patients and Families • MS is a chronic disease that many will live with for decades. • The unpredictability from day to day and year to year is difficult for patients and families to handle • MS is a disease characterized by change and loss. • Treatment costs and loss of income threaten patient and family well-being. • With more options available and choices to make, patients and families worry about making “wrong” choices.
Dental Management of MS Patients: Special Considerations • • • Office accessibility Mobility impairment (getting to appointments; transfers) Fatigue (self-care; getting to appointments) Weakness/incoordination (self-care) Possible cognitive impairment (self-care; remembering appointments, remembering instructions) • Possible mood changes (self-care) • Possible facial pain • Medication side effects (xerostomia)
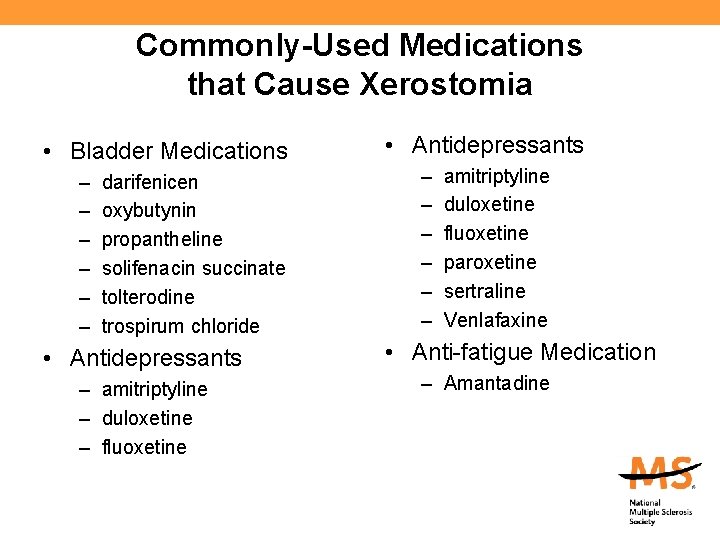
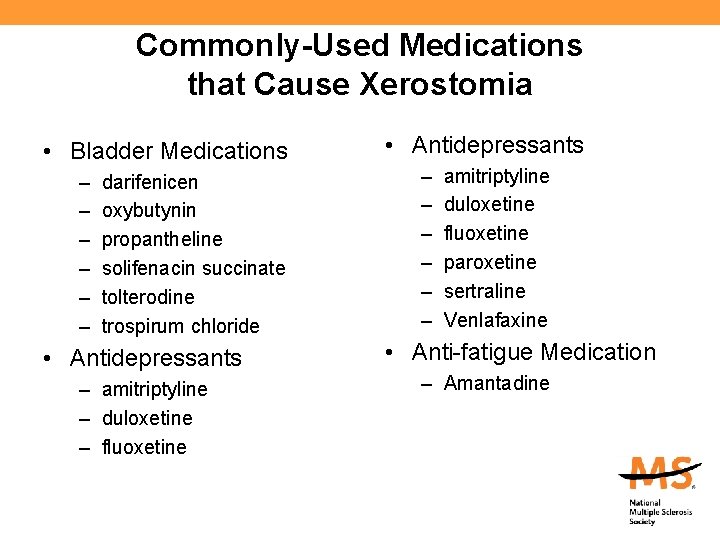
Commonly-Used Medications that Cause Xerostomia • Bladder Medications – – – darifenicen oxybutynin propantheline solifenacin succinate tolterodine trospirum chloride • Antidepressants – amitriptyline – duloxetine – fluoxetine • Antidepressants – – – amitriptyline duloxetine fluoxetine paroxetine sertraline Venlafaxine • Anti-fatigue Medication – Amantadine
Where do we go from here?
Current Treatment Priorities • Better understanding of MS pathogenesis and heterogeneity to guide development of better therapies and monitoring methods • Additional treatment options for relapsing-remitting MS RRMS) that are more effective, convenient, and/or tolerable • Effective therapies for purely progressive MS • Neuroprotective and repair strategies • More effective treatments for common symptoms such as fatigue, pain, tremor, and cognitive impairment • More effective psychosocial suport Cohen J. Arch Neurol. 2009; 66(7): 821 -828
NMSS Resources for Your Patients • Nationwide network of chapters around the country • Web site (www. national. MSsociety. org) • Access to information, referrals, and support (1 -800 -344 -4867) • Educational programs (in-person, online) • Support programs (self-help groups, peer and professional counseling, friendly visitors) • Consultation (legal, employment, insurance, long-term care) • Financial assistance
National MS Society Resources for Clinicians • Professional Resource Center (www. national. MSsociety. org/PRC; healthprof_info@nmss. org) – Clinical consultations with MS specialist physicians – Literature search services – Professional publications (Clinical Bulletins; Expert Opinion Papers; Talking with Your MS Patients about Difficult Topics; Pamela Cavallo Education Series for nurses, rehab professionals, mental health professionals, and pharmacists – Quarterly e-newsletter for healthcare professionals – Professional Education Programs (Nursing, Rehab, Mental Health) – Consultation on insurance and long-term care issues