Multiple Sclerosis Multiple Sclerosis Chronic progressive degenerative disorder


- Slides: 33
Multiple Sclerosis
Multiple Sclerosis • Chronic, progressive, degenerative disorder of the CNS characterized by disseminated demyelination of nerve fibers of the brain and spinal cord
Multiple Sclerosis • Usually affects young to middle- aged adults, with onset between 15 and 50 years of age • Women affected more than men
Multiple Sclerosis Etiology • Unknown cause • Related to infectious, immunologic, and genetic factors
Multiple Sclerosis Etiology • Possible precipitating factors include Ø Infection Ø Physical injury Ø Emotional stress Ø Excessive fatigue Ø Pregnancy Ø Poor state of health
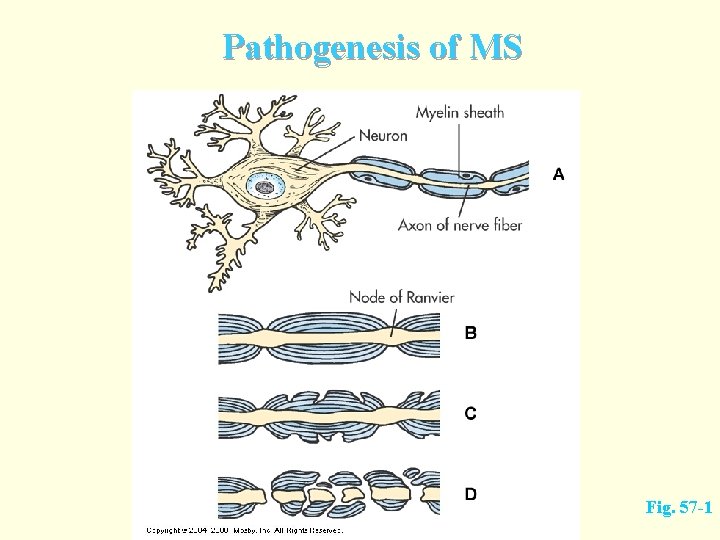
Multiple Sclerosis Pathophysiology • Mylelin sheath • • • Segmented lamination that wraps axons of many nerve cells Increases velocity of nerve impulse conduction in the axons Composed of myelin, a substance with high lipid content
Multiple Sclerosis Pathophysiology • Characterized by chronic inflammation, • • demyelination, and gliosis (scarring) in the CNS Initially triggered by a virus in genetically susceptible individuals Subsequent antigen-antibody reaction leads to demyelination of axons
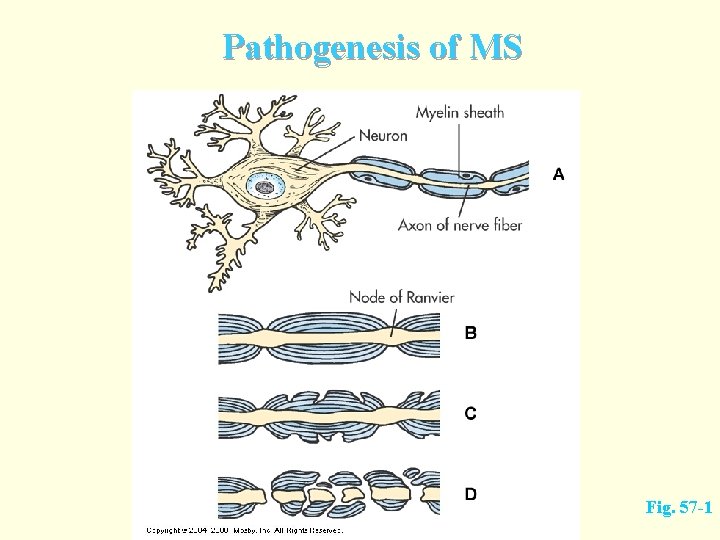
Pathogenesis of MS Fig. 57 -1
Multiple Sclerosis Pathophysiology • Disease process consists of loss of myelin, disappearance of oligodendrocytes, and proliferation of astrocytes • Changes result in plaque formation with plaques scattered throughout the CNS
Multiple Sclerosis Pathophysiology • Initially the myelin sheaths of the neurons • • in the brain and spinal cord are attacked, but the nerve fiber is not affected Patient may complain of noticeable impairment of function Myelin can regenerate, and symptoms disappear, resulting in a remission
Multiple Sclerosis Etiology and Pathophysiology • Myelin can be replaced by glial scar tissue • Without myelin, nerve impulses slow down • With destruction of axons, impulses are totally blocked • Results in permanent loss of nerve function
Multiple Sclerosis Clinical Manifestations • Vague symptoms occur intermittently over months and years • MS may not be diagnosed until long after the onset of the first symptom
Multiple Sclerosis Clinical Manifestations • Characterized by • • Chronic, progressive deterioration in some Remissions and exacerbations in others
Multiple Sclerosis Clinical Manifestations • Common signs and symptoms include motor, sensory, cerebellar, and emotional problems
Multiple Sclerosis Clinical Manifestations • Motor manifestations • • Weakness or paralysis of limbs, trunk, and head Diplopia (double vision) Scanning speech Spasticity of muscles
Multiple Sclerosis Clinical Manifestations • Sensory manifestations • • • Numbness and tingling Blurred vision Vertigo and tinnitus Decreased hearing Chronic neuropathic pain
Multiple Sclerosis Clinical Manifestations • Cerebellar manifestations • Nystagmus • • • Ataxia Dysarthria • • Involuntary eye movements Lack of coordination in articulating speech Dysphagia • Difficulty swallowing
Multiple Sclerosis Clinical Manifestations • Emotional manifestations • • • Anger Depression Euphoria
Multiple Sclerosis Other Clinical Manifestations • Bowel and bladder functions • • Constipation Spastic bladder: small capacity for urine results in incontinence. Flaccid bladder: large capacity for urine and no sensation to urinate
Multiple Sclerosis Other Clinical Manifestations • Sexual dysfunction Ø Erectile dysfunction Ø Decreased libido Ø Difficulty with orgasmic response Ø Painful intercourse Ø Decreased lubrication

Multiple Sclerosis Diagnostic Studies • Based primarily on history, clinical manifestations, and presence of multiple lesions over time measured by MRI • Certain laboratory tests are used as adjuncts to clinical exam
Multiple Sclerosis Diagnostic Studies • Diagnosis based primarily on: history and clinical manifestations • ruling out other causes of symptoms • No definitive diagnostic test • MRI – demonstrates presence of plaques •
Multiple Sclerosis Collaborative Care Drug Therapy • Corticosteroids • • Treat acute exacerbations by reducing edema and inflammation at the site of demyelination Do not affect the ultimate outcome or degree of residual neurologic impairment from exacerbation
Multiple Sclerosis Collaborative Care • Immunosuppressive Therapy • • Because MS is considered an autoimmune disease Potential benefits counterbalanced against potentially serious side effects
Multiple Sclerosis Collaborative Care • Antispasmotics (muscle relaxants)
Multiple Sclerosis Collaborative Care • Physical therapy helps Relieve spasticity Ø Increase coordination Ø Train the patient to substitute unaffected muscles for impaired ones Ø
Multiple Sclerosis Collaborative Care • Nutritional therapy includes megavitamins and diets consisting of lowfat, gluten-free food, and raw vegetables • High-protein diet with supplementary vitamins is often prescribed
Multiple Sclerosis Nursing Assessment • Health History Ø Risk factors Ø Precipitation factors Ø Clinical manifestations
Multiple Sclerosis Nursing Diagnoses • Impaired physical mobility • Dressing/grooming self-care deficit • Risk for impaired skin integrity • Impaired urinary elimination pattern • Sexual dysfunction • Interrupted family processes
Multiple Sclerosis Nursing Planning • Maximize neuromuscular function • Maintain independence in activities of • • • daily living for as long as possible Optimize psychosocial well-being Adjust to the illness Reduce factors that precipitate exacerbations
Multiple Sclerosis Nursing Implementation • Help identify triggers and develop ways • • • to avoid them or minimize their effects Reassure patient during diagnostic phase Assist in dealing with anxiety caused by diagnosis Prevent major complications of immobility
Multiple Sclerosis Nursing Implementation • Focus teaching on building general resistance to illness Ø Avoiding fatigue, extremes of hot and cold, exposure to infection • Teach good balance of exercise and rest, nutrition, avoidance of hazards of immobility

Multiple Sclerosis Nursing Implementation • Teach self-catheterization if necessary • Teach adequate intake of fiber to aid in regular bowel habits