MULTIPLE SCLEROSIS MS CASE STUDY 30 year old

- Slides: 41
MULTIPLE SCLEROSIS (MS)
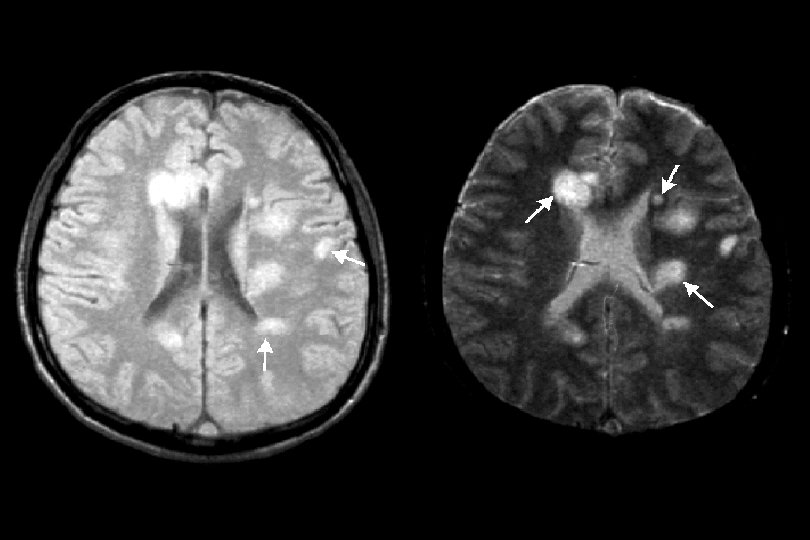
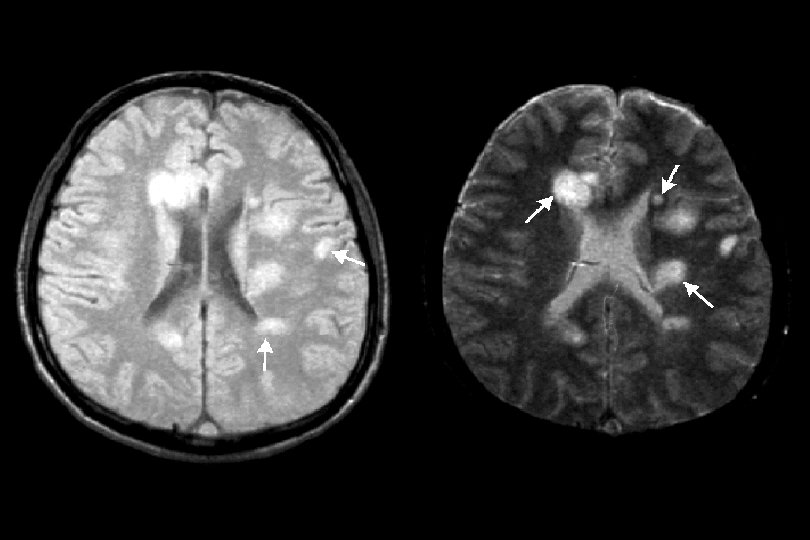
CASE STUDY • 30 year old white female presents to family physician with acute loss of vision in left eye • Referred to neurologist > Diagnosis of optic neuritis > Treated with IV corticosteroids for 5 days – Normal vision over next 3 weeks > Family history (mother) > Magnetic resonance imaging (MRI) – Multiple lesions in white matter of brain under cortex and around ventricles
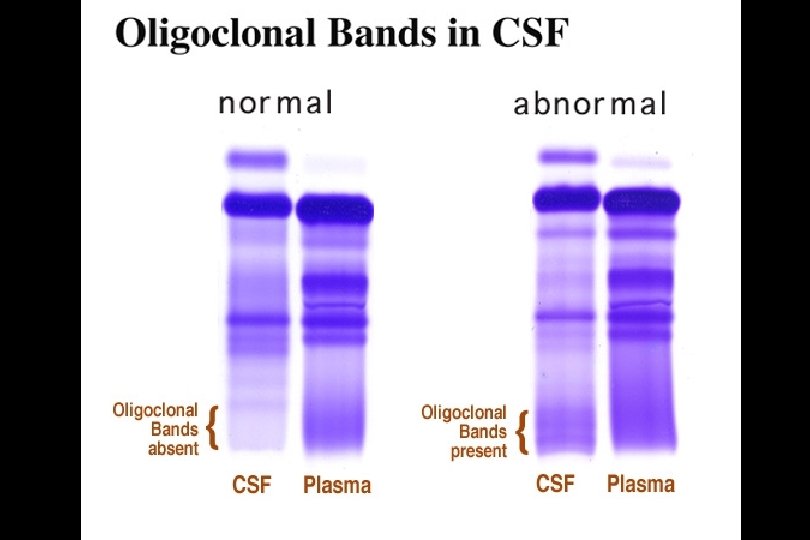
CASE STUDY • 3 years later > Muscle weakness on left side of face and fatigue > Radiology (MRI with gadolinium) – New lesions in left middle cerebellar peduncle and pons > Laboratory (CSF from lumbar puncture) – 12 lymphocytes/u. L – Ig. G index of 1. 2 – Oligoclonal bands (high resolution protein electrophoresis) • 2 bands in gamma region of CSF and no bands in gamma region of serum > Diagnosis of MS > Treatment with 5 day course of IV methylprednisolone and weekly IM interferon-beta (Avonex)
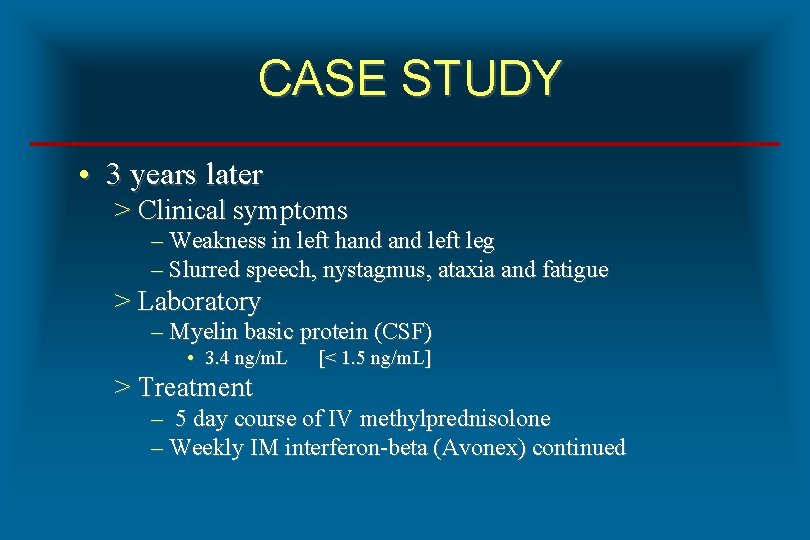
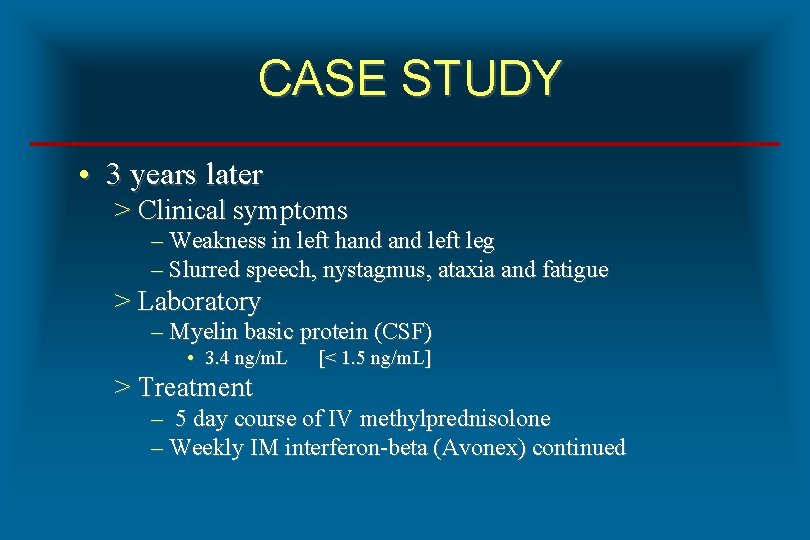
CASE STUDY • 3 years later > Clinical symptoms – Weakness in left hand left leg – Slurred speech, nystagmus, ataxia and fatigue > Laboratory – Myelin basic protein (CSF) • 3. 4 ng/m. L [< 1. 5 ng/m. L] > Treatment – 5 day course of IV methylprednisolone – Weekly IM interferon-beta (Avonex) continued
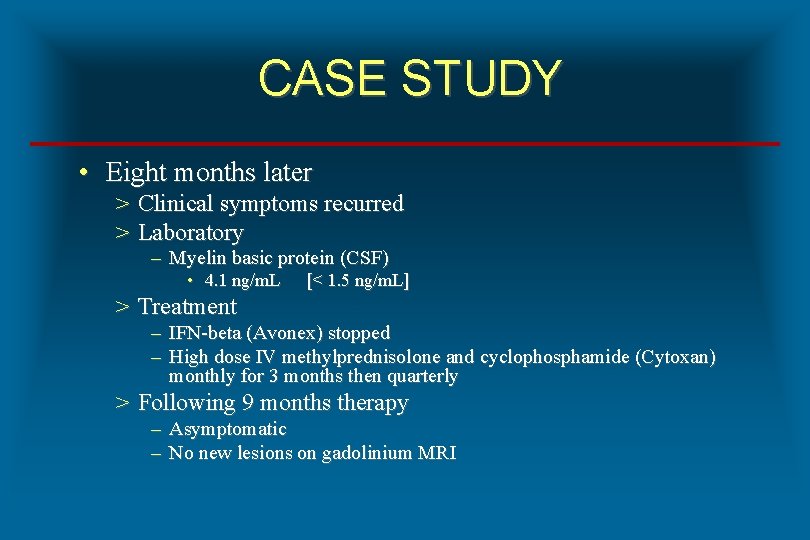
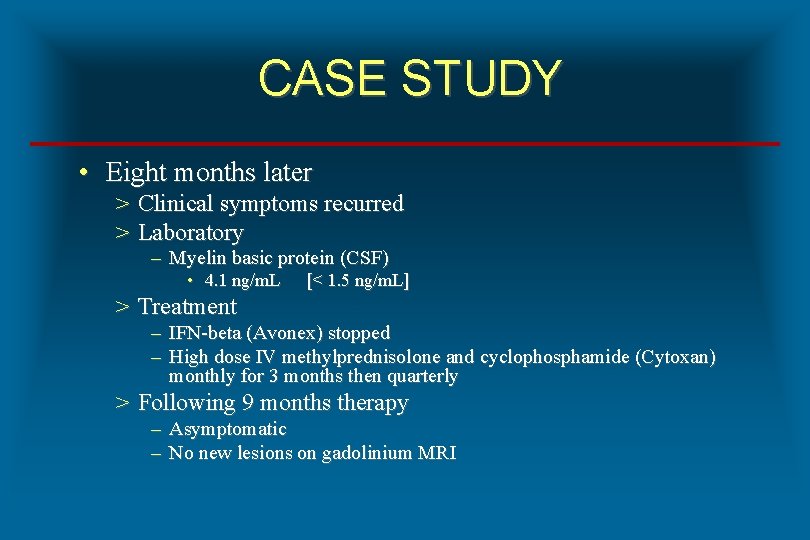
CASE STUDY • Eight months later > Clinical symptoms recurred > Laboratory – Myelin basic protein (CSF) • 4. 1 ng/m. L [< 1. 5 ng/m. L] > Treatment – IFN-beta (Avonex) stopped – High dose IV methylprednisolone and cyclophosphamide (Cytoxan) monthly for 3 months then quarterly > Following 9 months therapy – Asymptomatic – No new lesions on gadolinium MRI
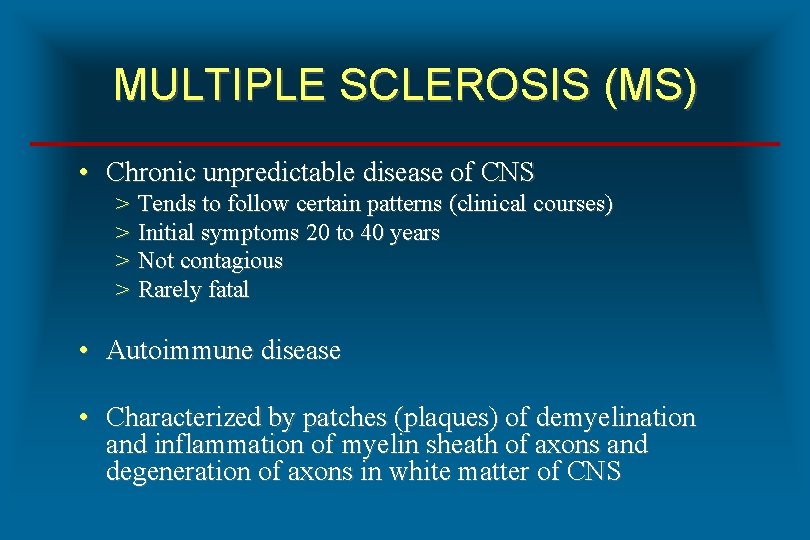
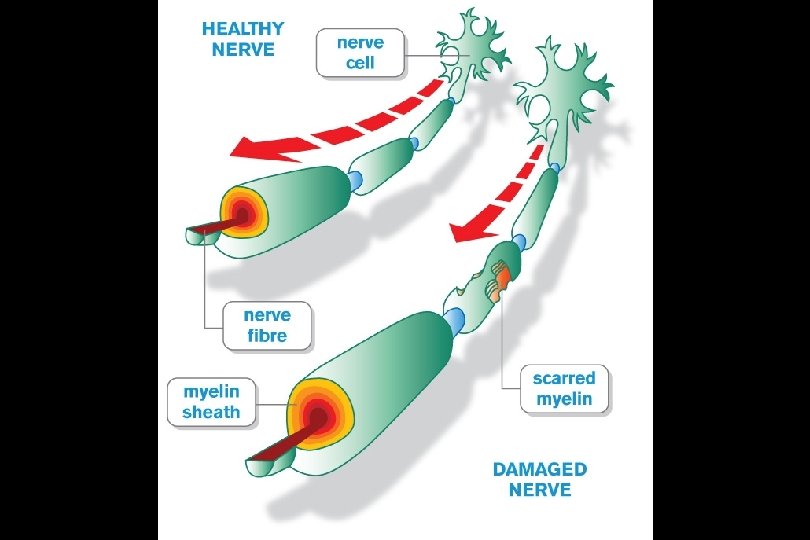
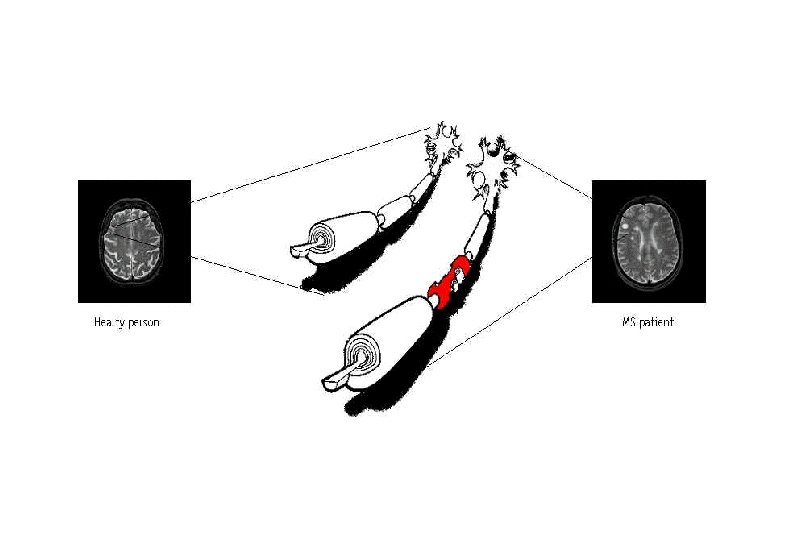
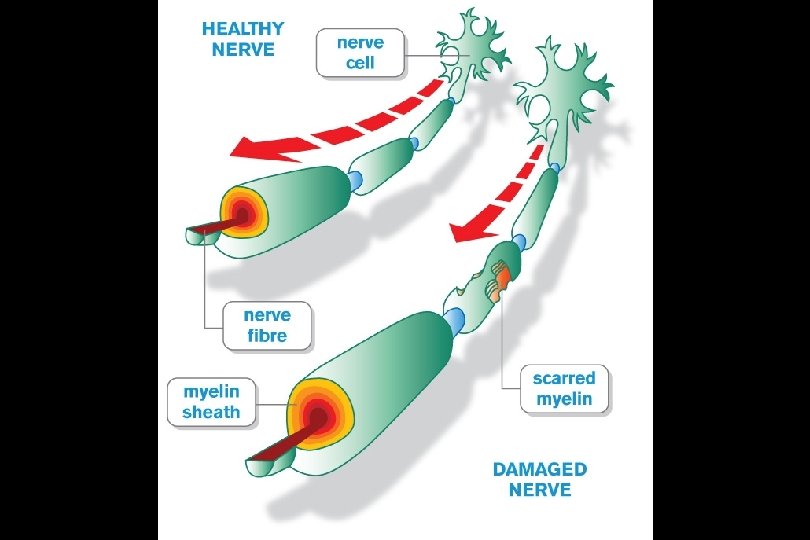
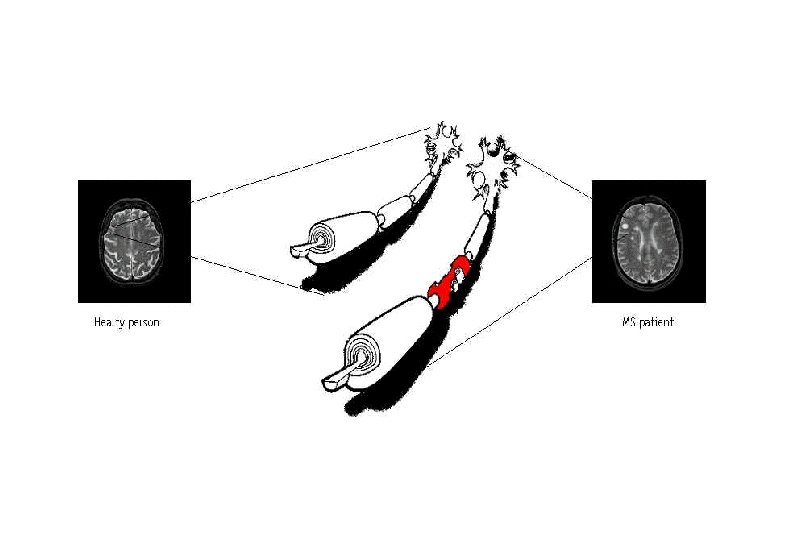
MULTIPLE SCLEROSIS (MS) • Chronic unpredictable disease of CNS > > Tends to follow certain patterns (clinical courses) Initial symptoms 20 to 40 years Not contagious Rarely fatal • Autoimmune disease • Characterized by patches (plaques) of demyelination and inflammation of myelin sheath of axons and degeneration of axons in white matter of CNS
ETIOLOGY OF MULTIPLE SCLEROSIS (MS) • Complex with multiple causal factors > Environmental agents – Chemicals (organic solvents) – UV light > Infectious agents – Viruses • EBV, HHV-6, measles virus, CDV, HERV – Bacteria • Chlamydophila pneumoniae > Genetic predisposition – HLA-DR 2 – IL-2 R and IL-7 receptor mutations
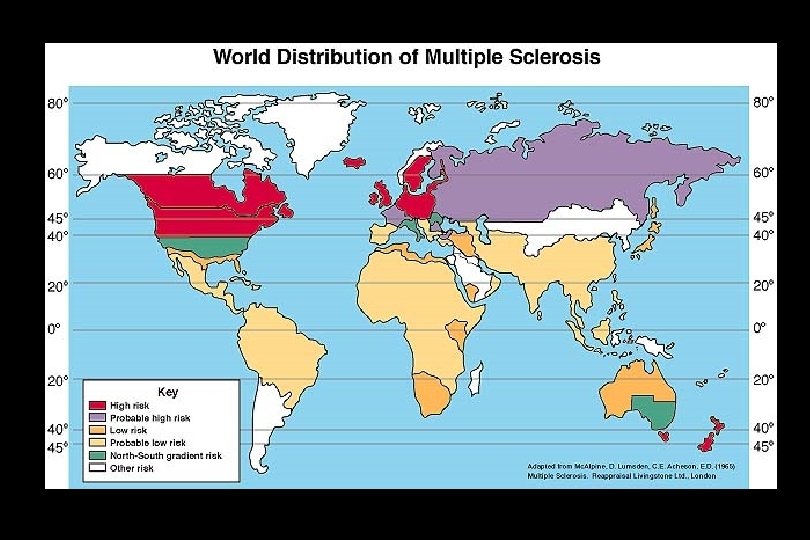
EPIDEMIOLOGY OF MULTIPLE SCLEROSIS • Female to male ratio of 2: 1 • Prevalence of 1 case per 750/1000 population > Northern Europe > Continental North America – 350, 000 to 400, 000 in US > Australia (SE) and New Zealand • Incidence in US of 200 to 300 cases/week • Disease prevalence > Caucasians > African Americans > Asians
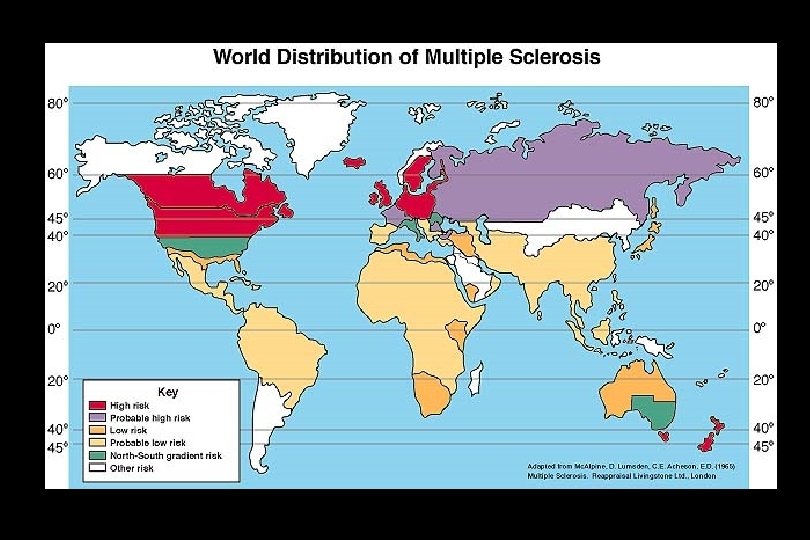
EPIDEMIOLOGY OF MULTIPLE SCLEROSIS (MS) • Hemisphere gradients for prevalence > North to south in northern hemisphere > South to north in southern hemisphere • Prevalence gradients in Northern Hemisphere > North of 37 th parallel (125 cases/100, 000 population) > South of 37 th parallel (70 cases/100, 000 population) • Migration risk > Geographic move and risk for developing disease • Disease rare or not seen in > Inuit, Lapps, American Indians, Aborigines, Maoris
RISK OF MULTIPLE SCLEROSIS (MS) • A 12 year old female > Moves from Rochester, Minnesota to Miami, Florida Risk for MS is: Increased Decreased Same • An 18 year old female > Moves from Rochester, Minnesota to Miami, Florida Risk for MS is: Increased Decreased Same
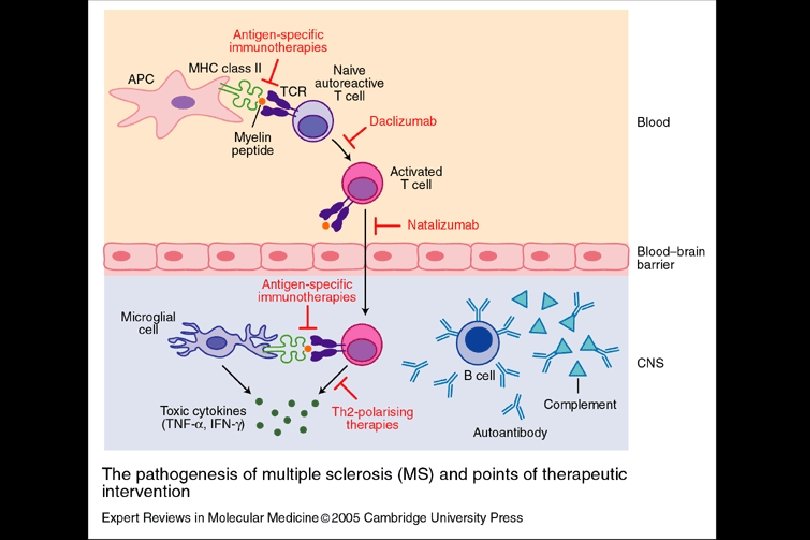
PATHOPHYSIOLOGY OF MULTIPLE SCLEROSIS • Destruction of > Myelin, oligodendrocytes, nerve axons • Hypothesis of molecular mimicry • Antigens > > Myelin basic protein (MBP) Myelin oligodendrocyte glycoprotein (MOG) Proteolipid protein (PLP) Myelin associated glycoprotein (MAG)
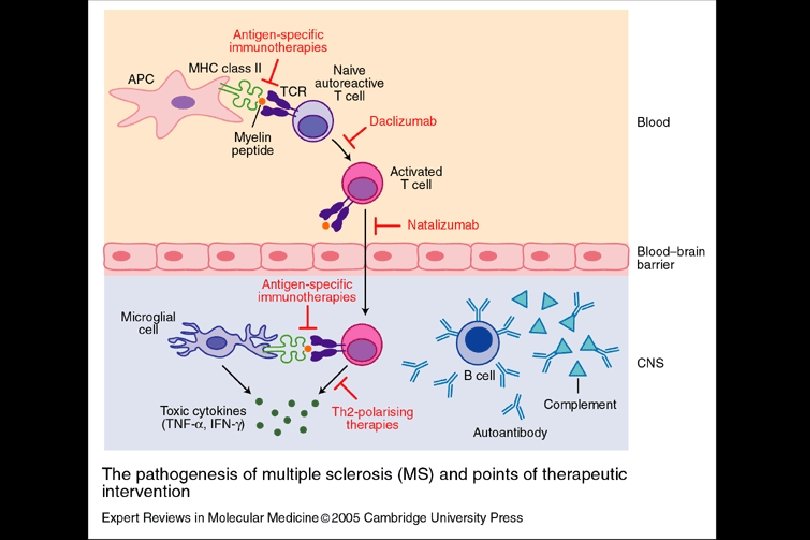
PATHOPHYSIOLOGY OF MULTIPLE SCLEROSIS • Cells > > CD 4 TH 1, CD 4 TH 2 and CD 8 T cells Macrophages and microglial cells Mast cells B cells • Cytokines, chemokines and adhesion molecules – IL-12 – IFN-gamma – ALCAM (Activated leukocyte cell adhesion molecule)
DIAGNOSIS OF MULTIPLE SCLEROSIS (MS) • Mc. Donald Criteria (2005 Revision) > History and clinical symptoms > Radiology – Magnetic resonance imaging (MRI) with and without gadolinium enhancement • Head and spinal column > Laboratory – MS panel
CLINICAL SYMPTOMS OF MULTIPLE SCLEROSIS (MS) • Fatigue • Visual disturbances > Blurred vision, diplopia, nystagmus, red-green color desaturation • Motor > Spasticity, paresis, dysarthria, spasms, ataxia, muscle weakness • Sensory changes > Paraesthesia, neuralgia • Cognitive deficits > Memory loss • Bladder / bowel urgency and incontinence
CLINICAL CONDITIONS ASSOCIATED WITH MS • Optic neuritis > Inflammation of optic nerve • Internuclear ophthalmoplegia > Paraylsis of ocular muscles • Transverse myelitis > Inflammation of spinal cord

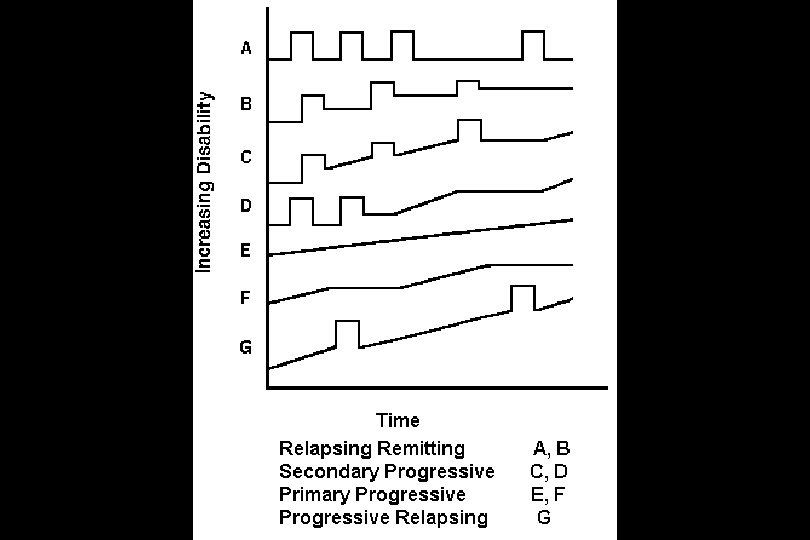
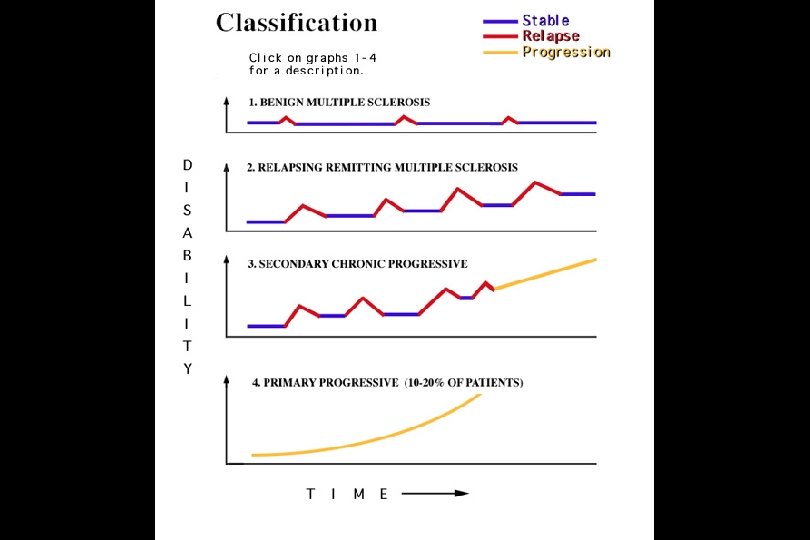
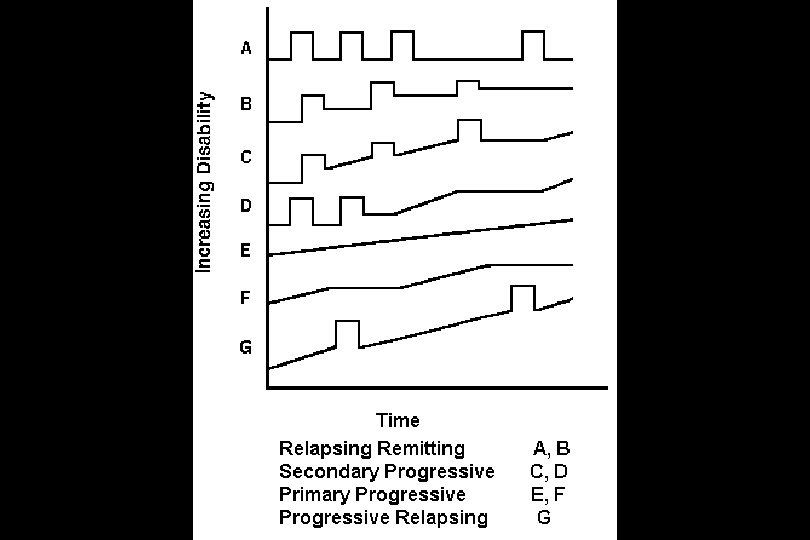
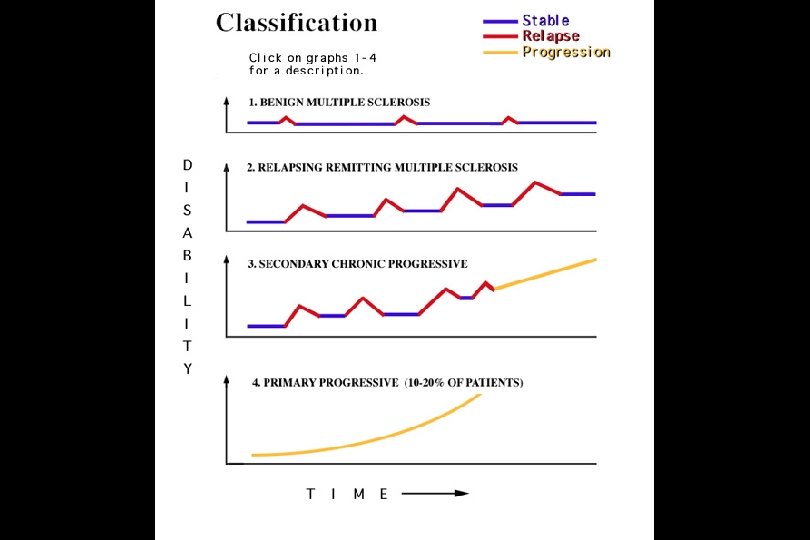
PATTERNS (CLINICAL COURSES) OF MULTIPLE SCLEROSIS • Relapsing-Remitting (85%) > Relaspes (attacks, exacerbations) followed by remission (rest periods) > Attack symptoms (old may flare, new may appear) • Secondary Progressive (50%) • Primary Progressive (10%) • Progressive-Relapsing (5%)
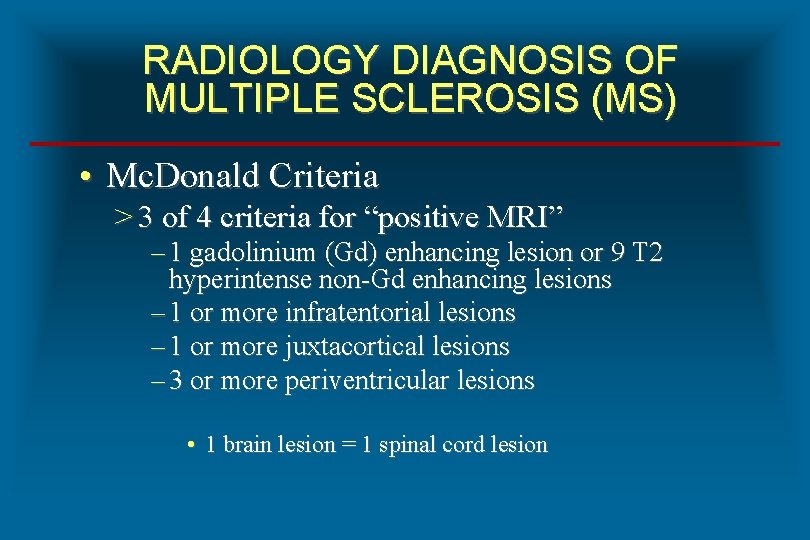
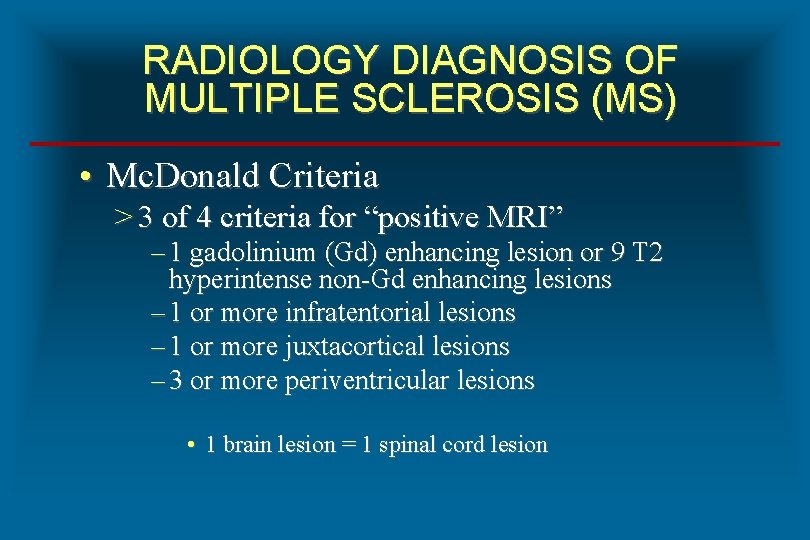
RADIOLOGY DIAGNOSIS OF MULTIPLE SCLEROSIS (MS) • Mc. Donald Criteria > 3 of 4 criteria for “positive MRI” – 1 gadolinium (Gd) enhancing lesion or 9 T 2 hyperintense non-Gd enhancing lesions – 1 or more infratentorial lesions – 1 or more juxtacortical lesions – 3 or more periventricular lesions • 1 brain lesion = 1 spinal cord lesion
LABORATORY DIAGNOSIS OF MULTIPLE SCLEROSIS (MS) • Oligoclonal bands > High resolution protein electrophoresis > Isoelectric focusing (IEF) • CSF Ig. G Index • Myelin basic protein (MBP) > Primary protein component (30%) of myelin > Elevated level indicates active demyelination > CSF reference range of < 1. 5 ng/m. L
LABORATORY DIAGNOSIS OF MS (OLIGOCLONAL BANDS) • Marker for intrathecal antibody synthesis • Associated with > MS, Sjogrens syndrome, SLE > AIDS, Creutzfeldt-Jakob disease (CJD), Lyme disease, Syphilis > Subacute sclerosing panencephalitis (SSPE) > Guillain-Barre syndrome (GBS) > Neoplasms
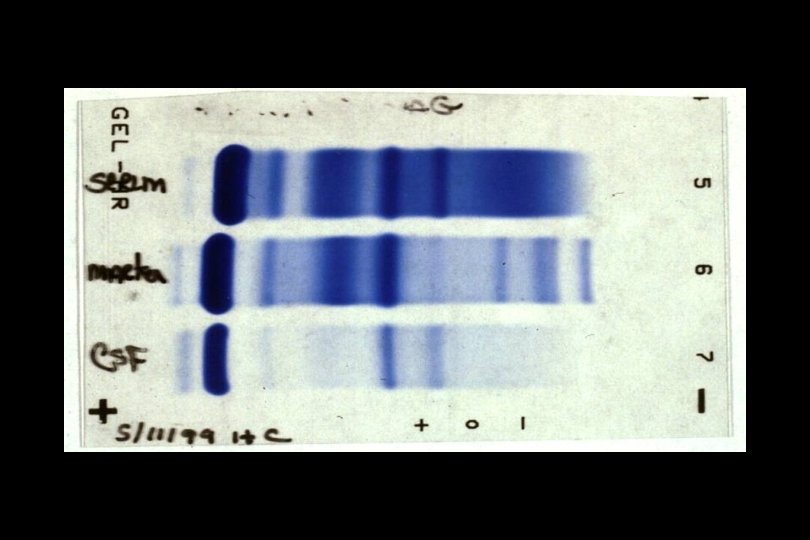
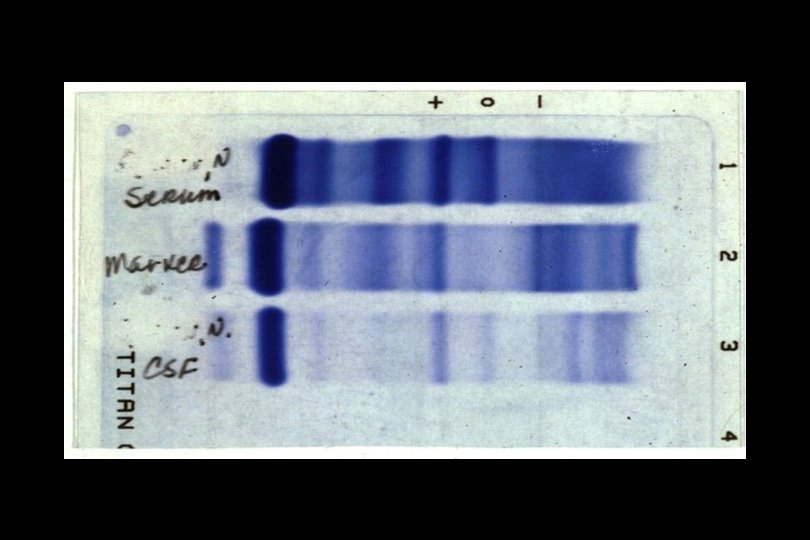
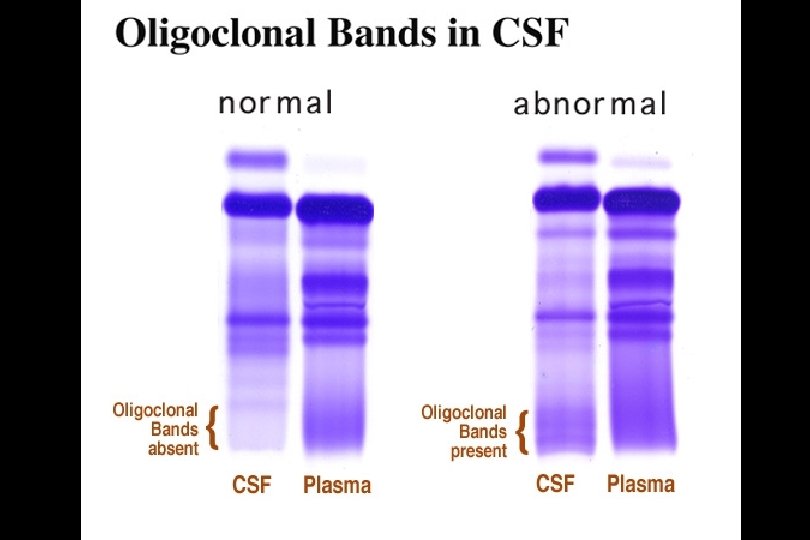
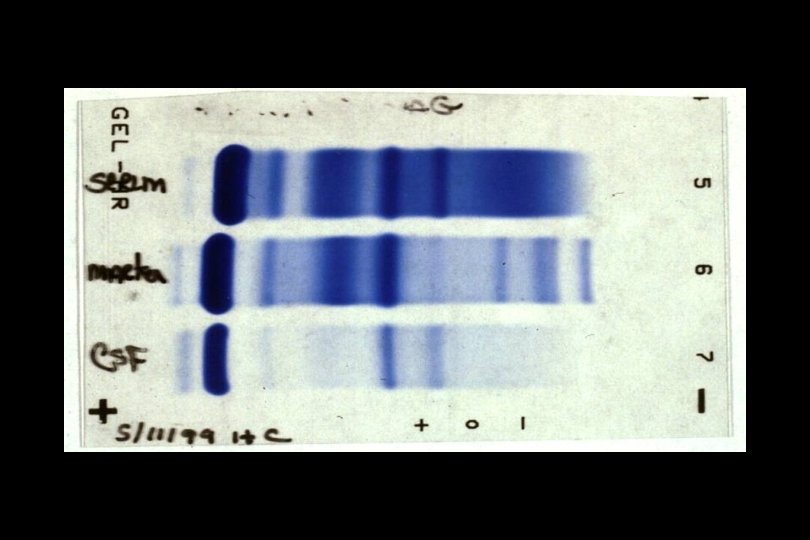
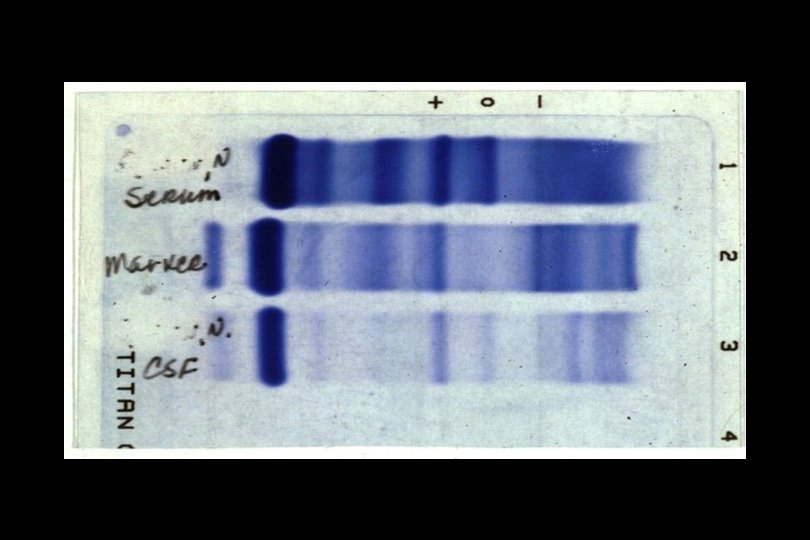
LABORATORY DIAGNOSIS OF MS (OLIGOCLONAL BANDS) • Specimens > CSF and serum • Method > High resolution protein electrophoresis – – Concentration of CSF (80 -100 X) Agarose gel 250 V for 20 minutes Coomassie brilliant blue stain • Interpretation > 2 or more bands in gamma region of CSF and no bands in gamma region of serum
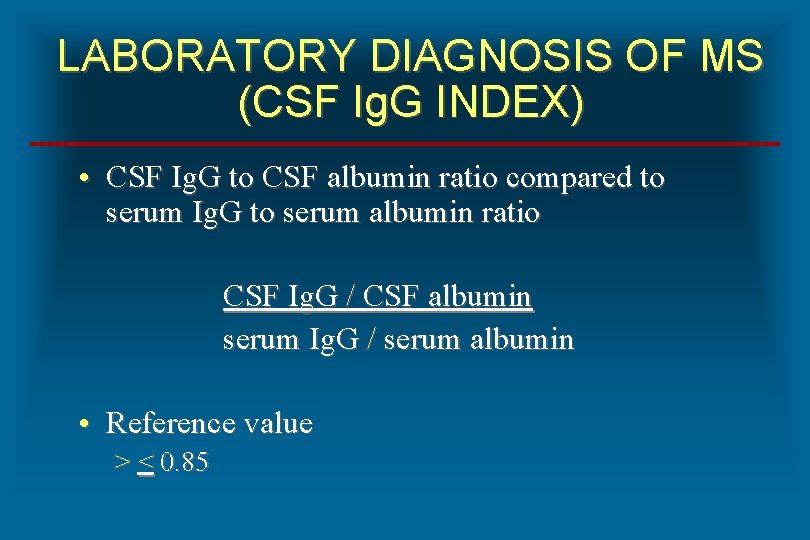
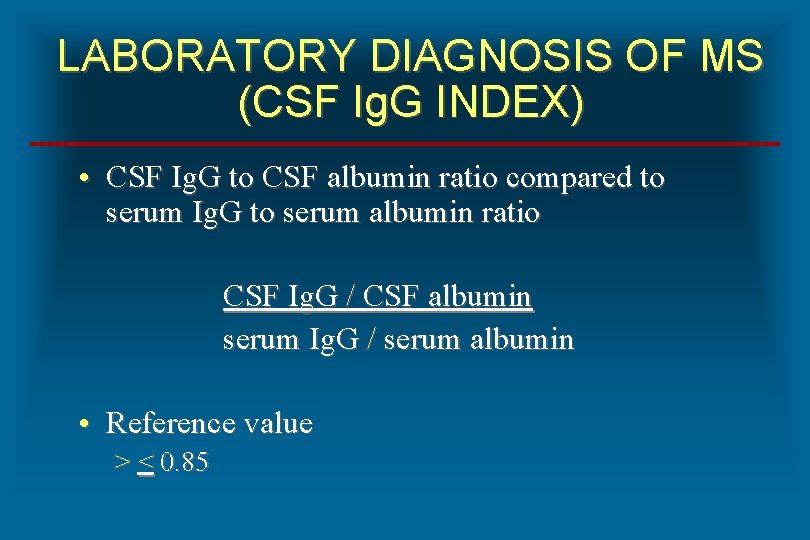
LABORATORY DIAGNOSIS OF MS (CSF Ig. G INDEX) • CSF Ig. G to CSF albumin ratio compared to serum Ig. G to serum albumin ratio CSF Ig. G / CSF albumin serum Ig. G / serum albumin • Reference value > < 0. 85
TREATMENT OF MULTIPLE SCLEROSIS • Two categories > Symptom management agents > Disease modifying agents • Symptom management agents > Corticosteroids – Prednisone, methylprednisolone, dexamethasone – Indicated for acute exacerbations
TREATMENT OF MULTIPLE SCLEROSIS • Disease modifying agents > Immunomodulating – Interferon beta-1 b (Betaseron) – Interferon beta-1 a (Avonex) – Interferon beta-1 a (Rebif) – Glatiramer acetate (Copaxone) – Natalizumab (Tysabri) > Immunosuppressant – Mitoxantrone (Novantrone)
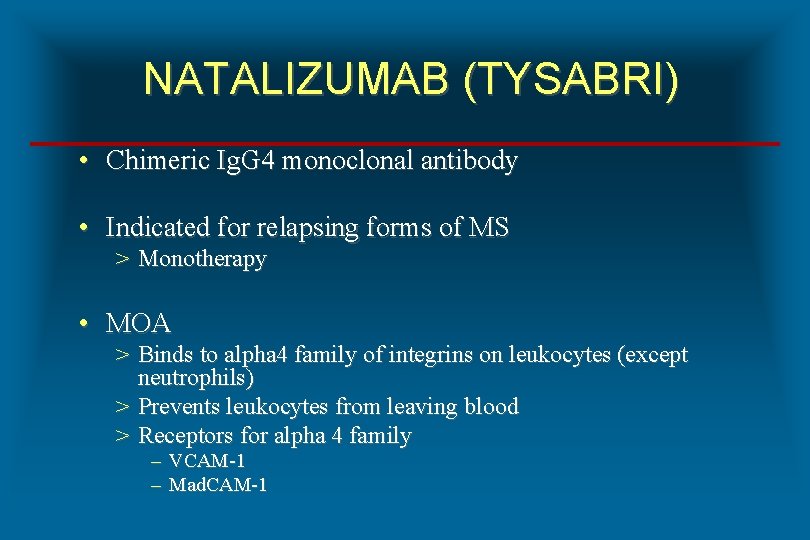
NATALIZUMAB (TYSABRI) • Chimeric Ig. G 4 monoclonal antibody • Indicated for relapsing forms of MS > Monotherapy • MOA > Binds to alpha 4 family of integrins on leukocytes (except neutrophils) > Prevents leukocytes from leaving blood > Receptors for alpha 4 family – – VCAM-1 Mad. CAM-1
NATALIZUMAB (TYSABRI) • FDA approval in November, 2004 • Manufacturer withdrawal in February, 2005 • Adverse event (Boxed Warning) > Increased risk of – Progressive multifocal leukoencephalopathy (PML) • PML > Viral encephalitis caused by JC virus • FDA reapproval in March, 2006
INTERFERON BETA-1 b (BETASERON) • Protein from human interferon beta-1 b gene on plasmid in Escherichia coli > Serine for cysteine at 17 • Indications > Relapsing forms > Initial clinical episode with MRI • Mechanism of action is unknown • Administration > Subcutaneous injection every other day
INTERFERON BETA – 1 a (AVONEX) • Glycoprotein from human interferon beta-1 a gene in Chinese Hamster Ovary Cells • Indications > Relapsing forms • Mechanism of action is unknown > Beta 2 microglobulin > Neopterin • Dose and administration > 30 mcg IM / week
INTERFERON BETA – 1 a (REBIF) • Glycoprotein from human interferon beta-1 a gene in Chinese Hamster Ovary Cells • Indications > Relapsing forms • Mechanism of action is unknown > Beta 2 microglobulin > Neopterin • Dose and administration > 22 mcg or 44 mcg SC 3 x /week
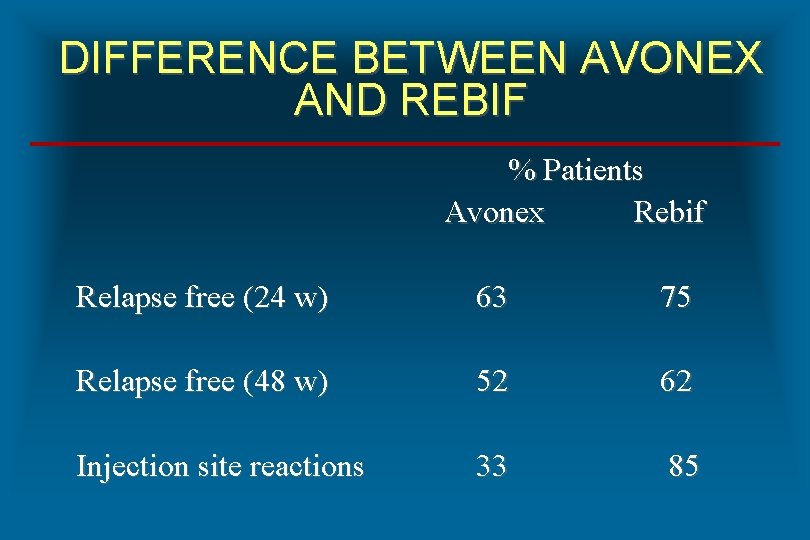
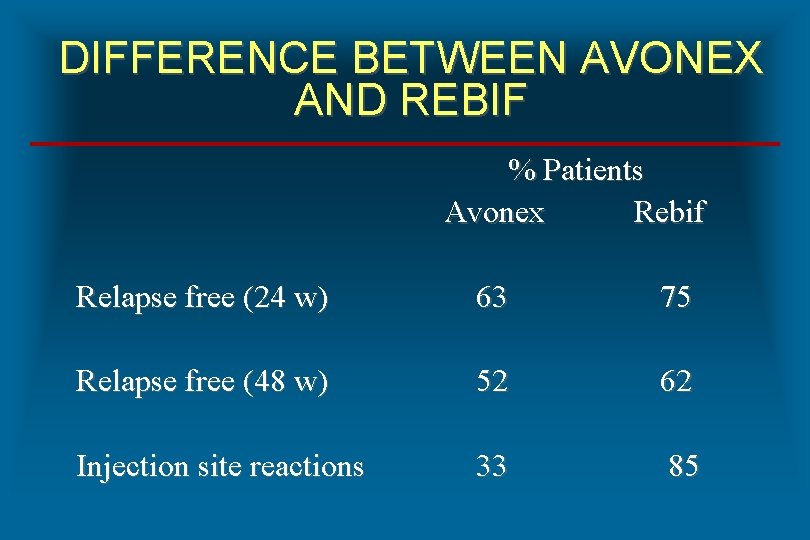
DIFFERENCE BETWEEN AVONEX AND REBIF % Patients Avonex Rebif Relapse free (24 w) 63 75 Relapse free (48 w) 52 62 Injection site reactions 33 85