Multiple Organ Dysfunction Syndrome Definition Diagnosis Management Definitions


- Slides: 51
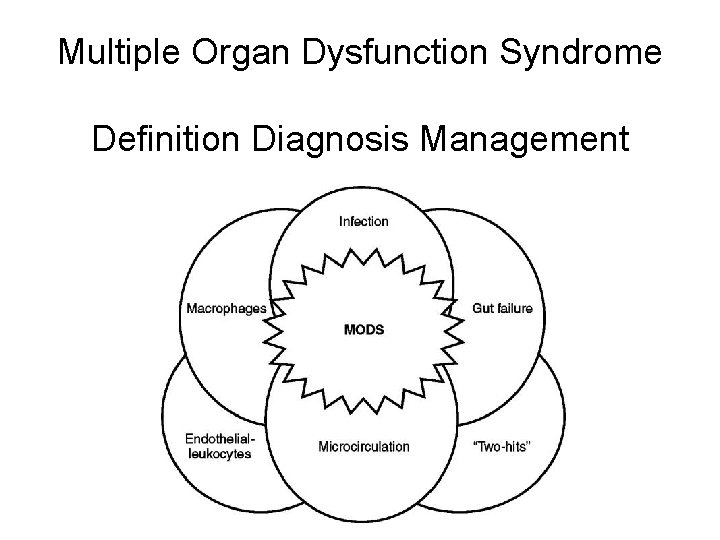
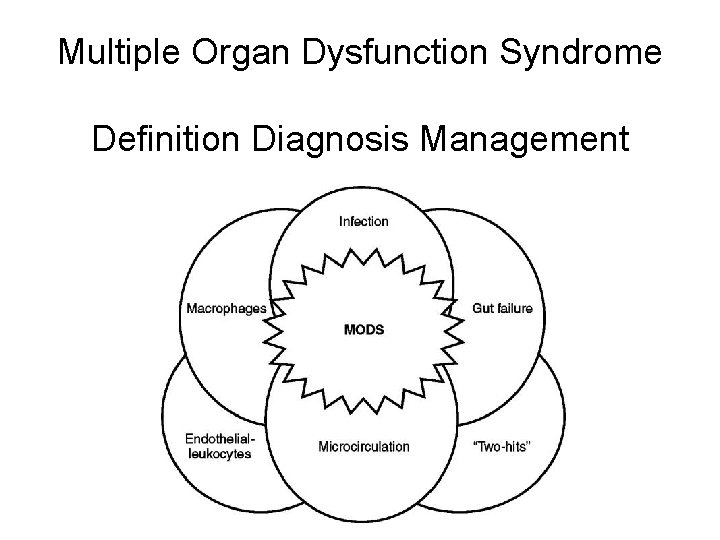
Multiple Organ Dysfunction Syndrome Definition Diagnosis Management
Definitions • Multiple Organ Dysfunction Syndrome “MODS” – 1991 Consensus conference of the American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM) • Dysfunction replaced failure to accentuate the reversible nature of the condition • Underlying concept – Sepsis, systemic inflammatory response syndrome (SIRS), acute respiratory distress syndrome (ARDS), and MODS are closely related phenomena
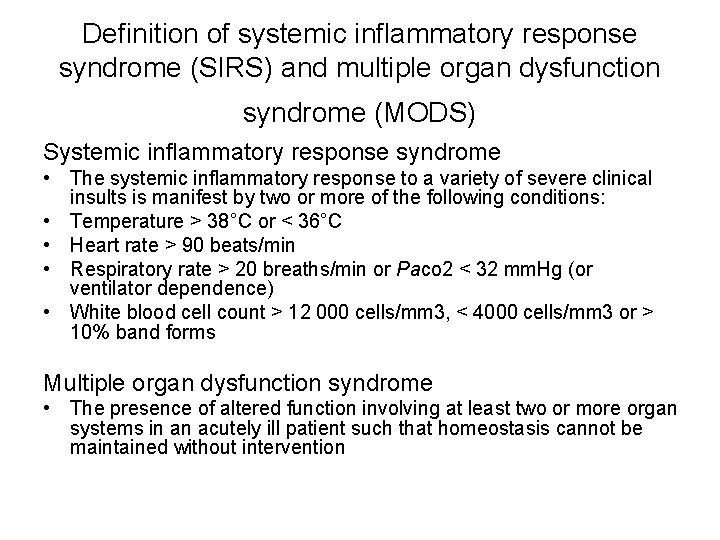
Definition of systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome (MODS) Systemic inflammatory response syndrome • The systemic inflammatory response to a variety of severe clinical insults is manifest by two or more of the following conditions: • Temperature > 38°C or < 36°C • Heart rate > 90 beats/min • Respiratory rate > 20 breaths/min or Paco 2 < 32 mm. Hg (or ventilator dependence) • White blood cell count > 12 000 cells/mm 3, < 4000 cells/mm 3 or > 10% band forms Multiple organ dysfunction syndrome • The presence of altered function involving at least two or more organ systems in an acutely ill patient such that homeostasis cannot be maintained without intervention
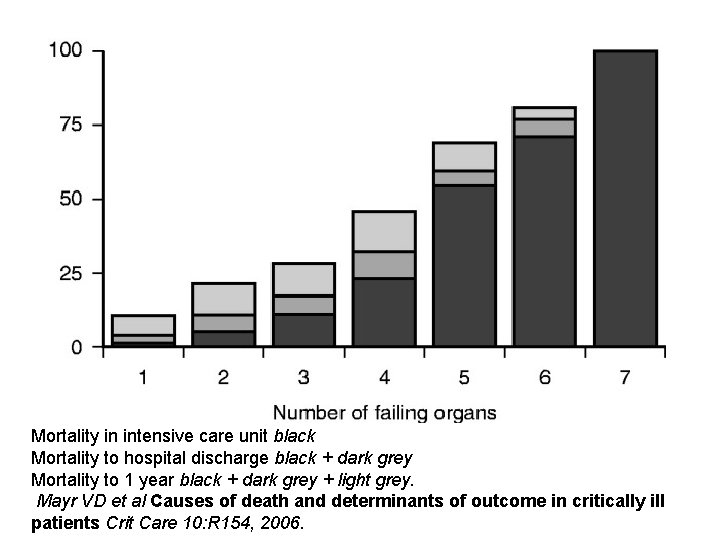
• MODS is the most common cause of late trauma deaths • Approximately 50% of ICU patients will develop MODS (estimates 25 -80+%) • Estimates of 20% to up to 75% mortality in patients having at least two-organ failure • As each organ fails the average risk of death increased 11 to 23 percent Ulvik A, Kvale R, Wentzel-Larsen T, et al. Multiple organ failure after trauma affects even long-term survival and functional status. Crit Care 2007; 11: R 95.
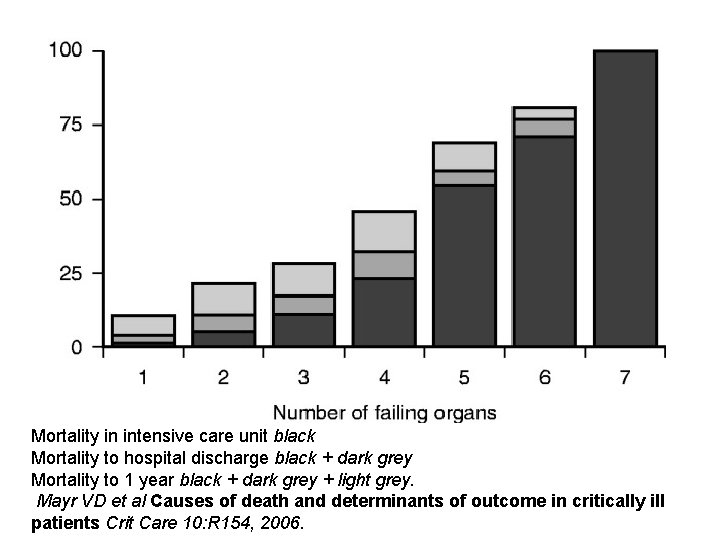
Mortality in intensive care unit black Mortality to hospital discharge black + dark grey Mortality to 1 year black + dark grey + light grey. Mayr VD et al Causes of death and determinants of outcome in critically ill patients Crit Care 10: R 154, 2006.
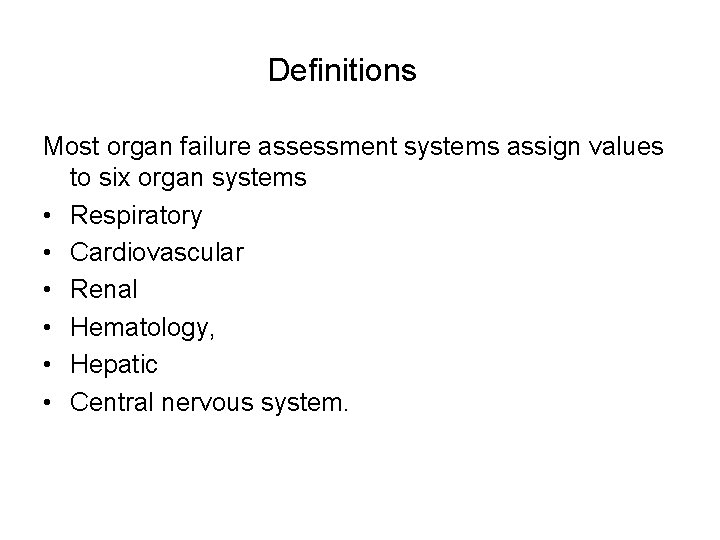
Definitions Most organ failure assessment systems assign values to six organ systems • Respiratory • Cardiovascular • Renal • Hematology, • Hepatic • Central nervous system.
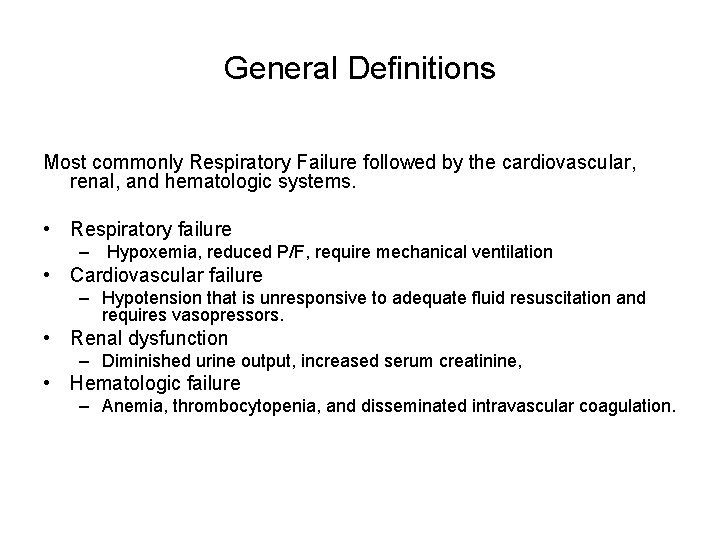
General Definitions Most commonly Respiratory Failure followed by the cardiovascular, renal, and hematologic systems. • Respiratory failure – Hypoxemia, reduced P/F, require mechanical ventilation • Cardiovascular failure – Hypotension that is unresponsive to adequate fluid resuscitation and requires vasopressors. • Renal dysfunction – Diminished urine output, increased serum creatinine, • Hematologic failure – Anemia, thrombocytopenia, and disseminated intravascular coagulation.
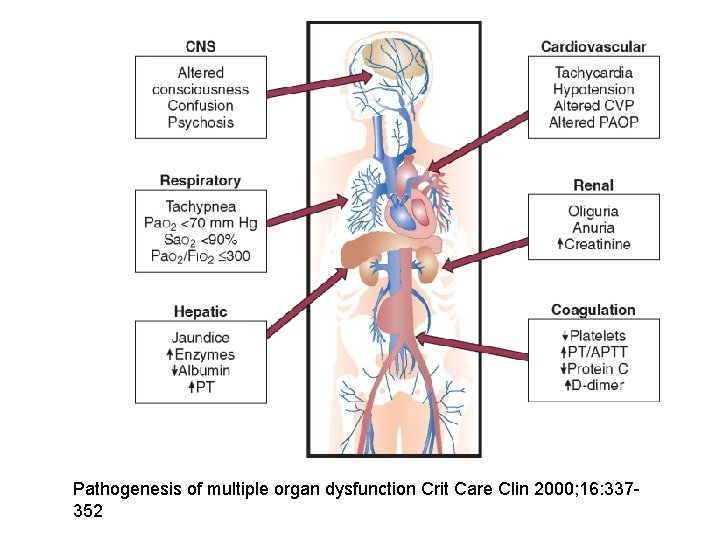
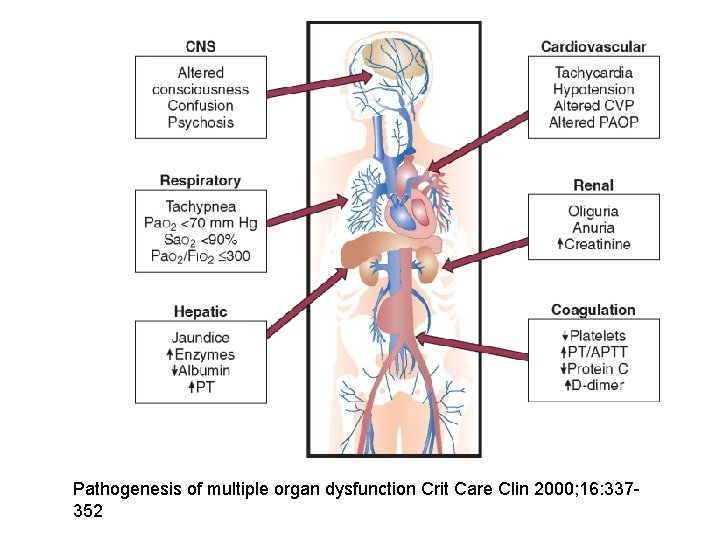
Pathogenesis of multiple organ dysfunction Crit Care Clin 2000; 16: 337352
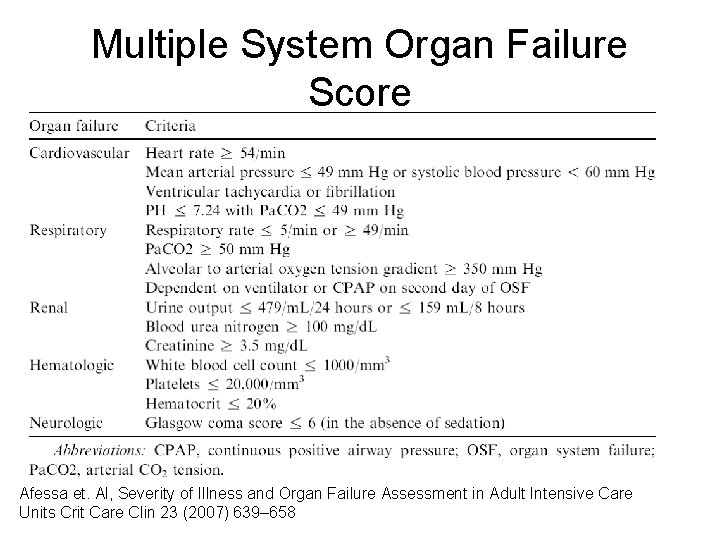
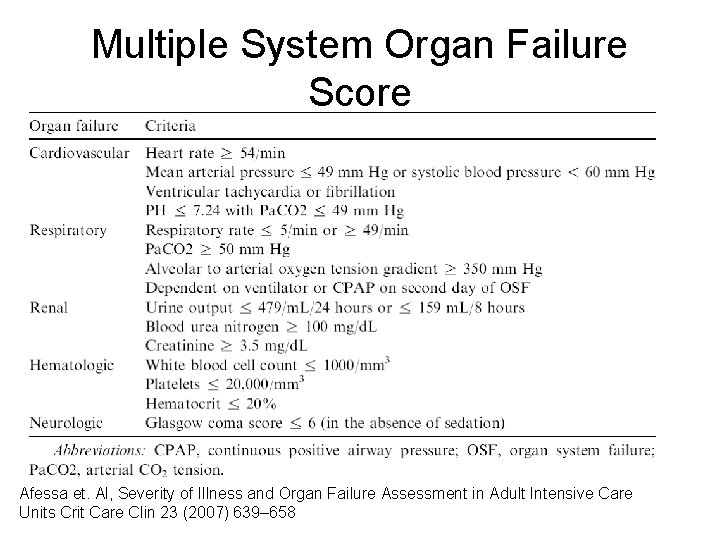
Multiple System Organ Failure Score Afessa et. Al, Severity of Illness and Organ Failure Assessment in Adult Intensive Care Units Crit Care Clin 23 (2007) 639– 658
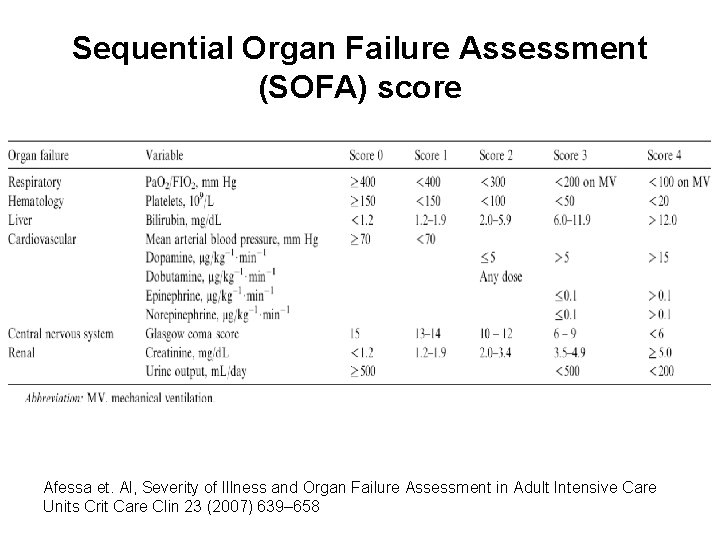
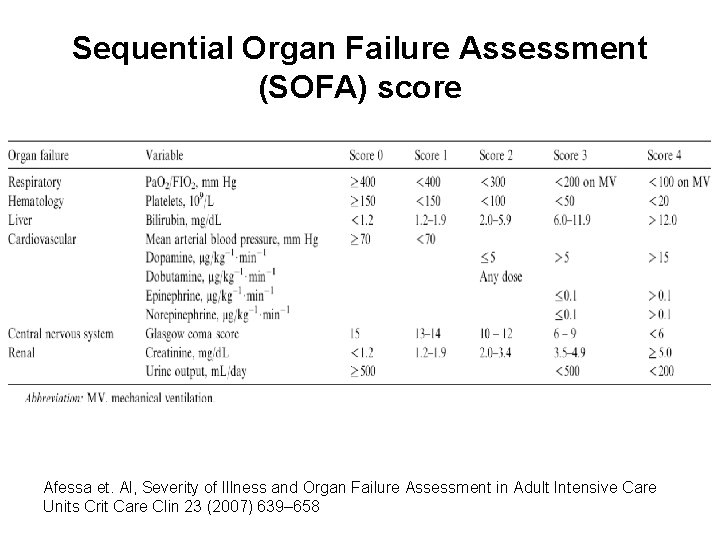
Sequential Organ Failure Assessment (SOFA) score Afessa et. Al, Severity of Illness and Organ Failure Assessment in Adult Intensive Care Units Crit Care Clin 23 (2007) 639– 658
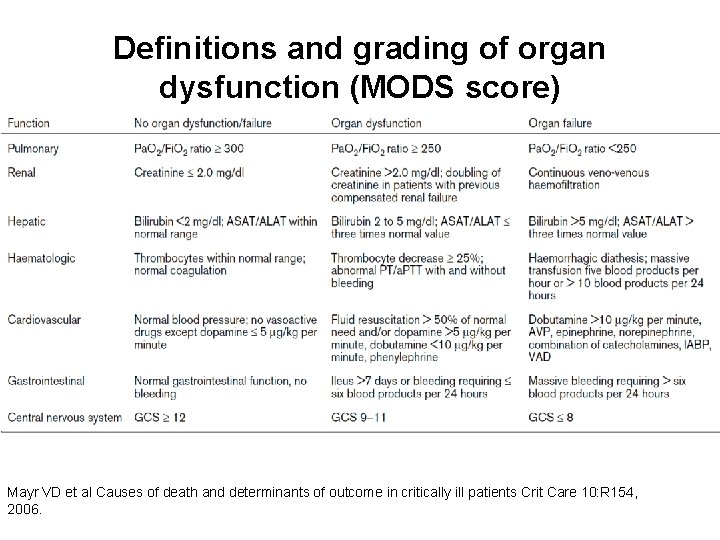
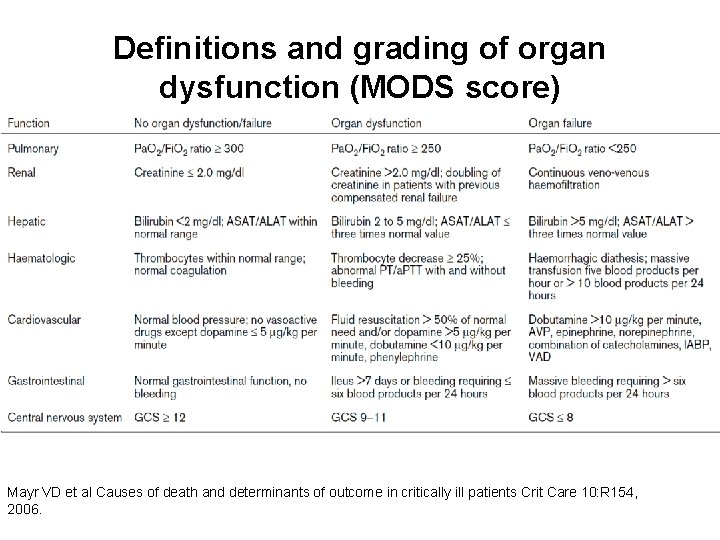
Definitions and grading of organ dysfunction (MODS score) Mayr VD et al Causes of death and determinants of outcome in critically ill patients Crit Care 10: R 154, 2006.
Denver Postinjury MOF Score Ciesla et al, The role of the lung in postinjury multiple organ failure Surgery 01 -OCT-2005; 138(4): 749 -57
Diagnosis by Definition • Syndrome – wide spectrum of pathophysiology under one term believed to be related by common cascade of events culminating in organ dysfunction • Heterogeneous collection – Approximately 50%– 70% of patients with MODS do not have an identifiable focus of infection – Approximately 1/3 do not have lung involvement – Trauma patients may form a distinct subset
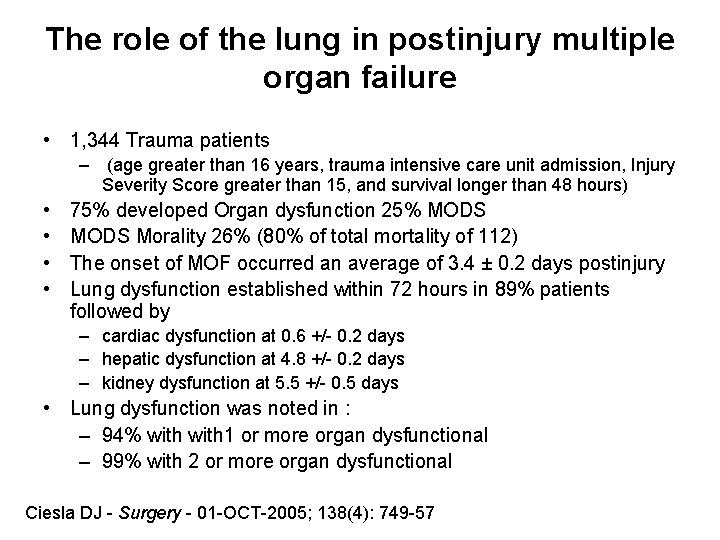
The role of the lung in postinjury multiple organ failure • 1, 344 Trauma patients – (age greater than 16 years, trauma intensive care unit admission, Injury Severity Score greater than 15, and survival longer than 48 hours) • • 75% developed Organ dysfunction 25% MODS Morality 26% (80% of total mortality of 112) The onset of MOF occurred an average of 3. 4 ± 0. 2 days postinjury Lung dysfunction established within 72 hours in 89% patients followed by – cardiac dysfunction at 0. 6 +/- 0. 2 days – hepatic dysfunction at 4. 8 +/- 0. 2 days – kidney dysfunction at 5. 5 +/- 0. 5 days • Lung dysfunction was noted in : – 94% with 1 or more organ dysfunctional – 99% with 2 or more organ dysfunctional Ciesla DJ - Surgery - 01 -OCT-2005; 138(4): 749 -57
Potential Pathophysiologic Mechanisms Producing MODS • • Circulating immune/inflammatory mediators Primary cellular injury Mitochondrial Injury/ down-regulation Inadequate tissue/organ perfusion – Hypoperfusion – Ischemia/reperfusion – Microaggregation and/or DIC • • • Diffuse endothelial cell injury Circulating humoral factors Protein calorie malnutrition Bacterial-toxin translocation Adverse effect of directed treatment or medication
Models Meakins “two-hit” model of postinjury MOF. • The first hit (trauma / shock ) primes neutrophils and macrophages • The second hit (nosocomial infection/complication) results in detrimental inflammatory response
Inflammatory Model • MODS is caused by an overwhelming imbalance between systemic inflammatory response and counter regulation (anti-inflammatory) response. • May be activated by a number of external and internal factors, including pro-inflammatory (e. g. , infection, sepsis, shock, and trauma) and immunosuppression (e. g. , Blood transfusion, infection, and steroids). • The imbalance in favor of inflammatory response causes loss of the host's ability to localize the inflammation to ijnitial inciting factor, leading to systemic inflammation and tissue damage.
Bioenergetics Model • Multiple organ dysfunction is the results of the dysregulation of mitochondria • Mitochondrial activity is down-regulated as a protective reflex to inciting factors • Failure to recover mitochondrial function results in self perpetuating cycle of cell damage furthering shutdown of mitochondria • Mervyn Singer, Mitochondrial function in sepsis: Acute phase versus multiple organ failure (Crit Care Med 2007; 35[Suppl. ]: S 441–S 448)
Bioenergetics and Sepsis Mervyn Singer, Cellular Dysfunction in Sepsis Clin Chest Med 29 (2008) 655– 660
Progression of Bioenergetics Dysfunction Mervyn Singer, Mitochondrial function in sepsis: Acute phase versus multiple organ failure (Crit Care Med 2007; 35[Suppl. ]: S 441–S 448)
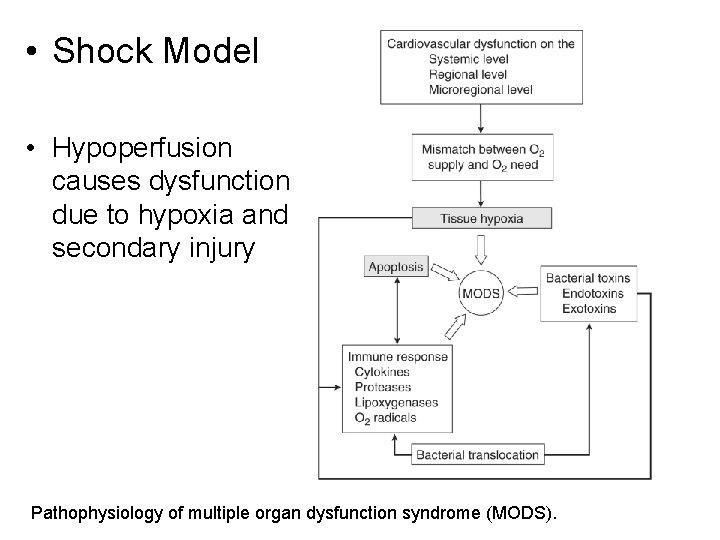
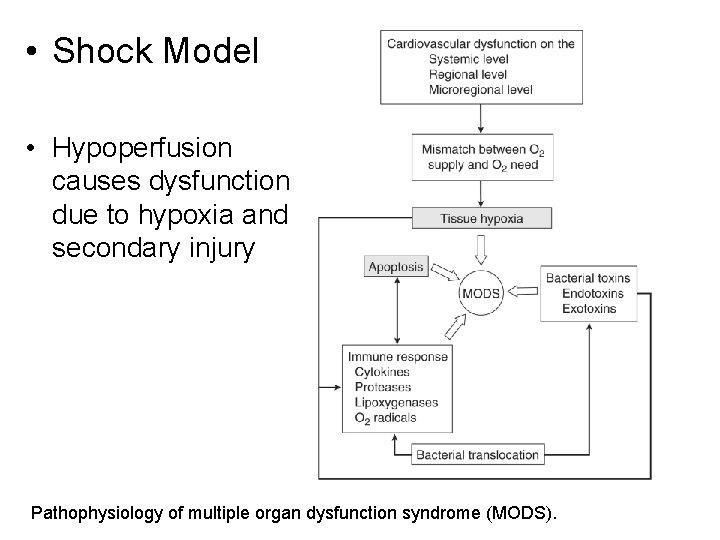
• Shock Model • Hypoperfusion causes dysfunction due to hypoxia and secondary injury Pathophysiology of multiple organ dysfunction syndrome (MODS).
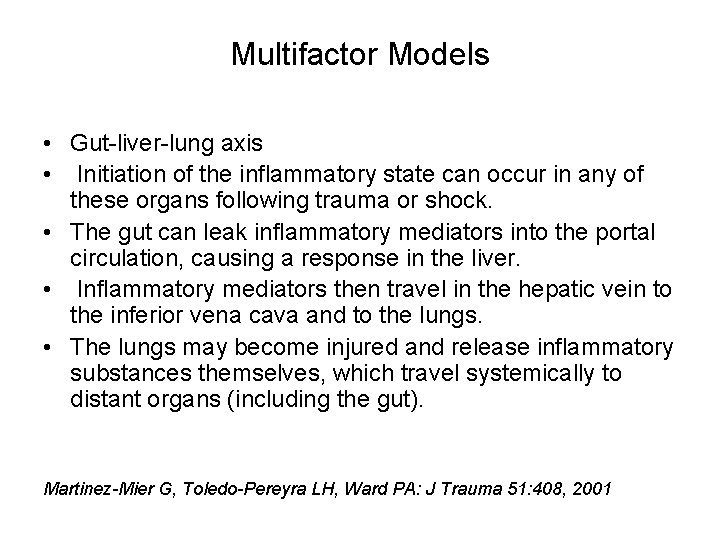
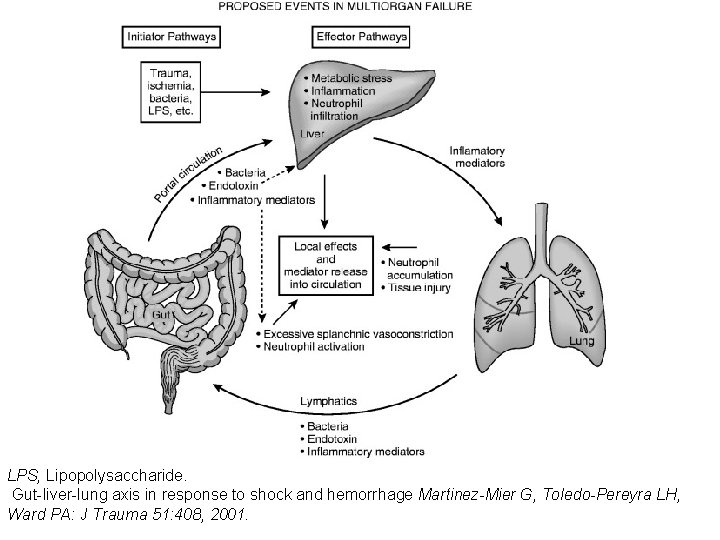
Multifactor Models • Gut-liver-lung axis • Initiation of the inflammatory state can occur in any of these organs following trauma or shock. • The gut can leak inflammatory mediators into the portal circulation, causing a response in the liver. • Inflammatory mediators then travel in the hepatic vein to the inferior vena cava and to the lungs. • The lungs may become injured and release inflammatory substances themselves, which travel systemically to distant organs (including the gut). Martinez-Mier G, Toledo-Pereyra LH, Ward PA: J Trauma 51: 408, 2001
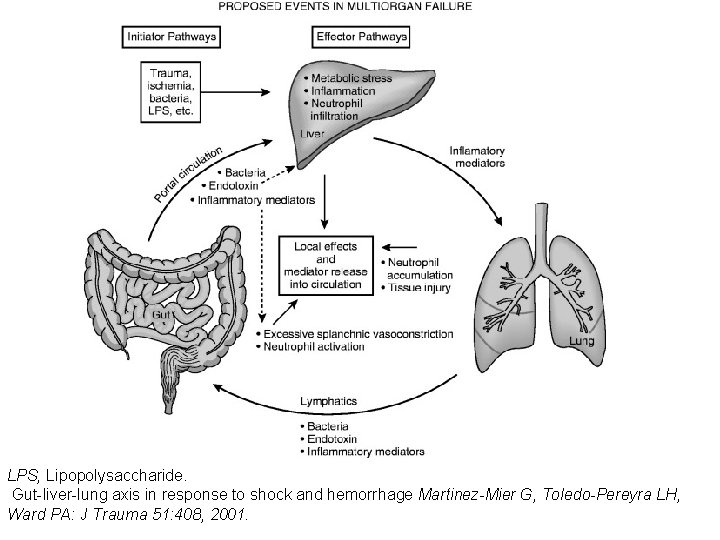
LPS, Lipopolysaccharide. Gut-liver-lung axis in response to shock and hemorrhage Martinez-Mier G, Toledo-Pereyra LH, Ward PA: J Trauma 51: 408, 2001.
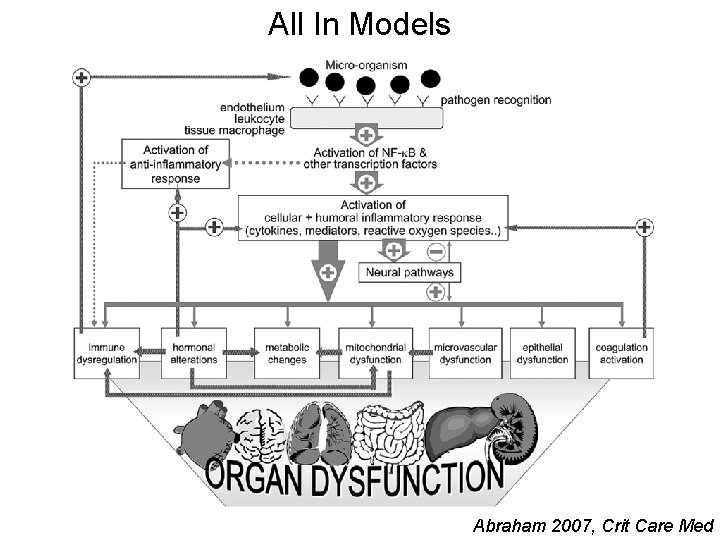
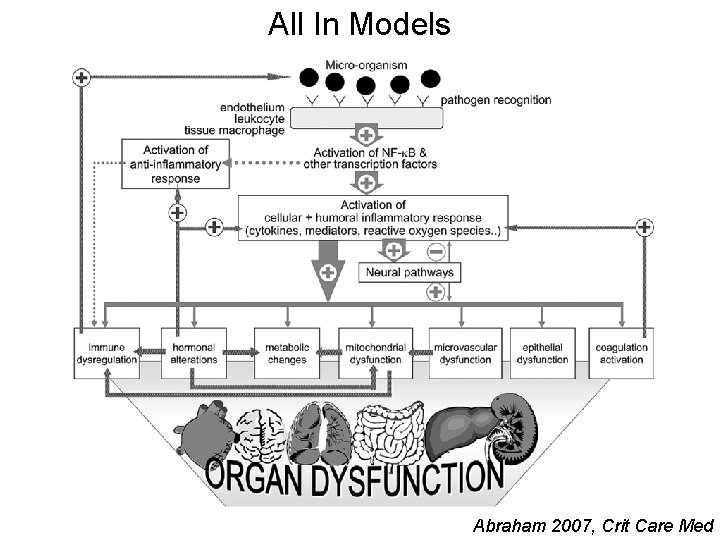
All In Models Abraham 2007, Crit Care Med
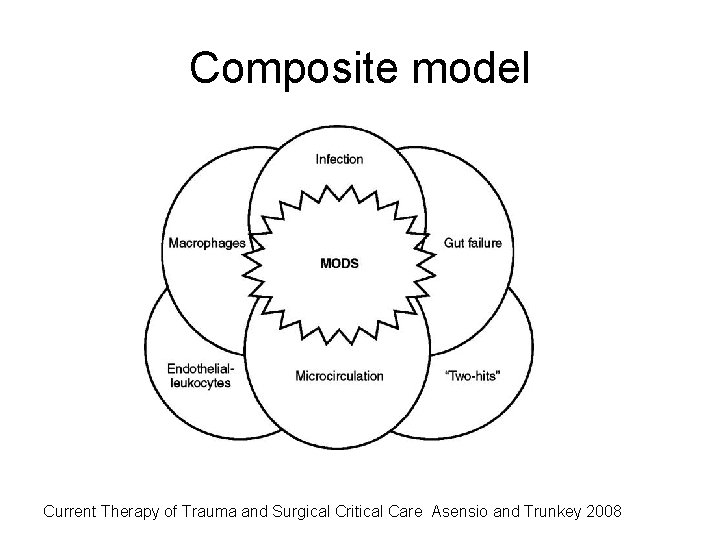
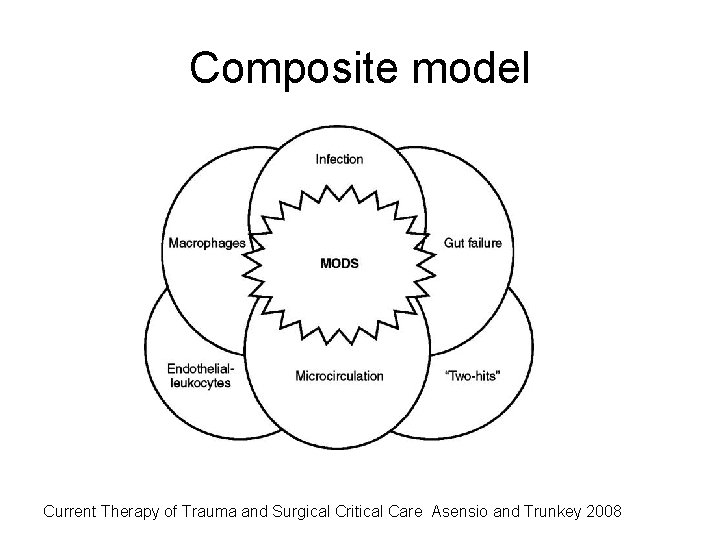
Composite model Current Therapy of Trauma and Surgical Critical Care Asensio and Trunkey 2008

Therapy
Targeted therapy • Activated Protein C – Modulating the systemic inflammatory, procoagulant, and fibrinolytic host responses • Vasopressin Therapy – Replacing falling plasma levels of vasopressin seen in shock • Steriods – Replacement reversible failure of the hypothalamic-pituitary-Adrenal (HPA) axis
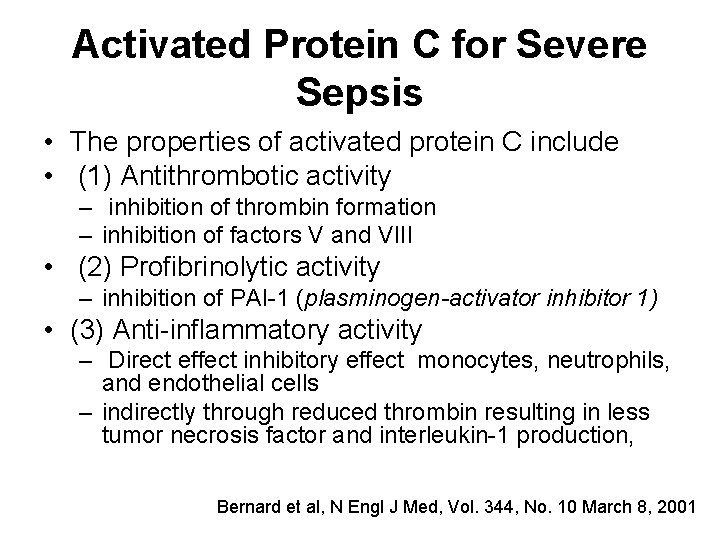
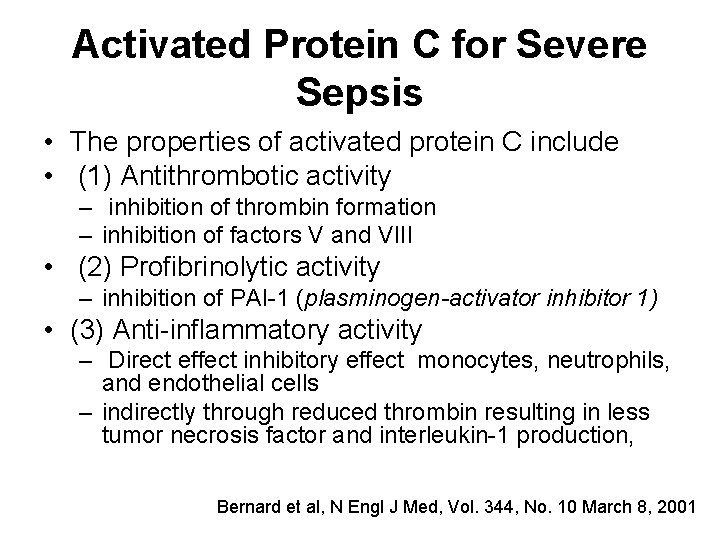
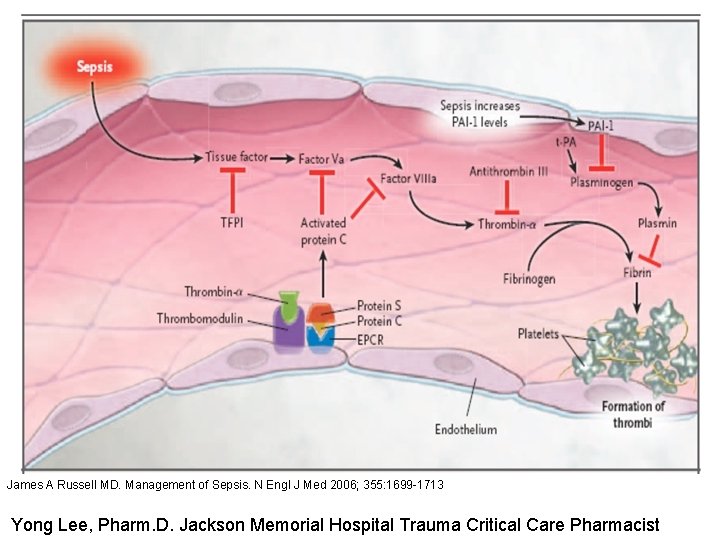
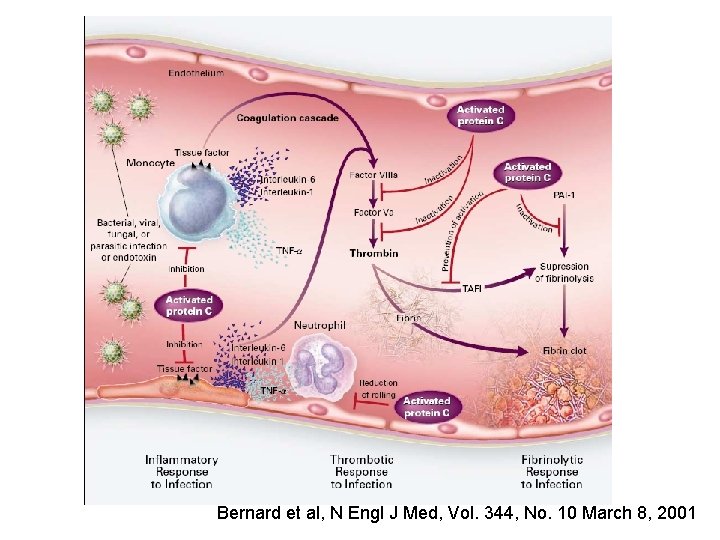
Activated Protein C for Severe Sepsis • The properties of activated protein C include • (1) Antithrombotic activity – inhibition of thrombin formation – inhibition of factors V and VIII • (2) Profibrinolytic activity – inhibition of PAI-1 (plasminogen-activator inhibitor 1) • (3) Anti-inflammatory activity – Direct effect inhibitory effect monocytes, neutrophils, and endothelial cells – indirectly through reduced thrombin resulting in less tumor necrosis factor and interleukin-1 production, Bernard et al, N Engl J Med, Vol. 344, No. 10 March 8, 2001
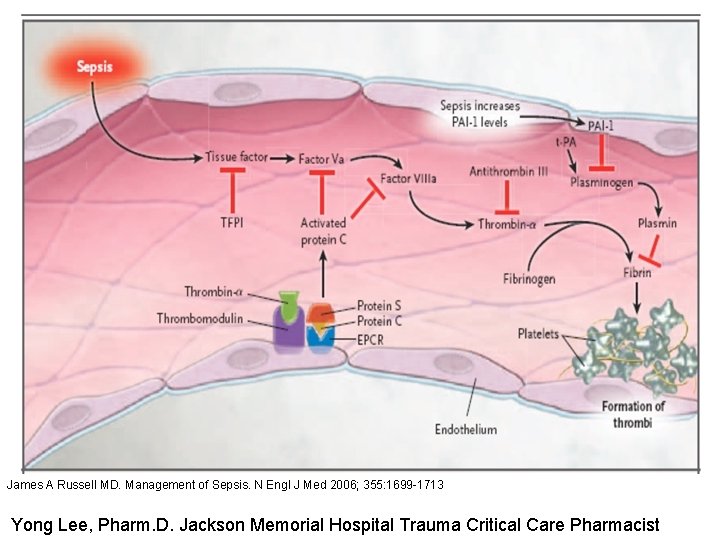
James A Russell MD. Management of Sepsis. N Engl J Med 2006; 355: 1699 -1713 Yong Lee, Pharm. D. Jackson Memorial Hospital Trauma Critical Care Pharmacist
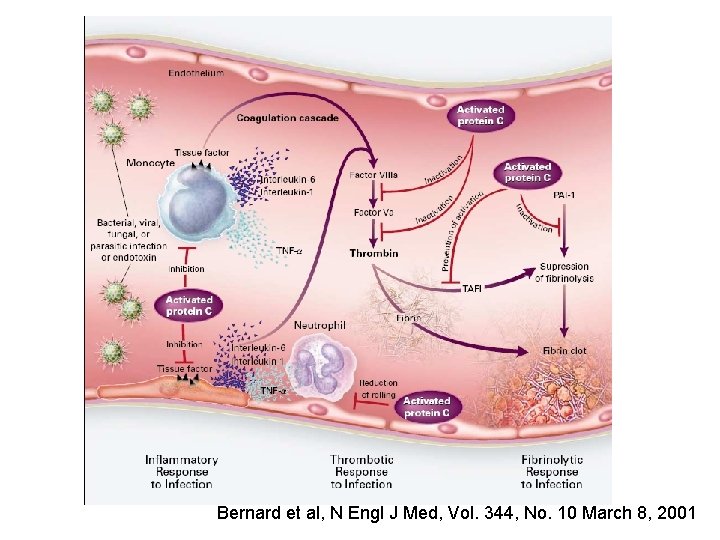
Bernard et al, N Engl J Med, Vol. 344, No. 10 March 8, 2001
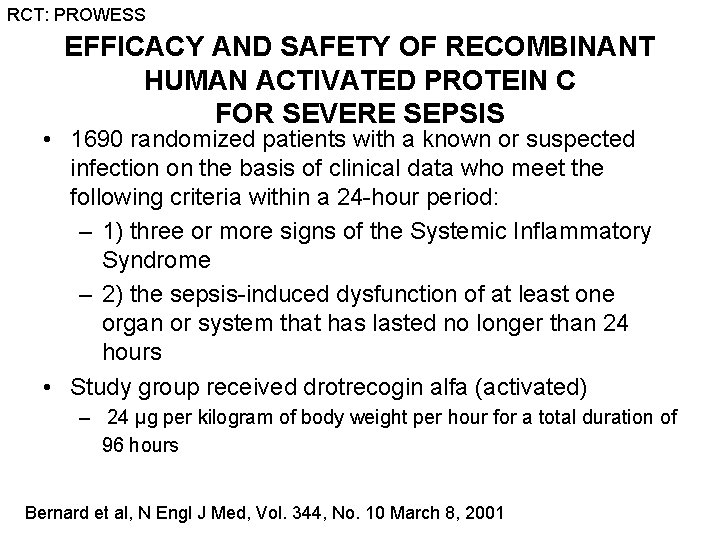
RCT: PROWESS EFFICACY AND SAFETY OF RECOMBINANT HUMAN ACTIVATED PROTEIN C FOR SEVERE SEPSIS • 1690 randomized patients with a known or suspected infection on the basis of clinical data who meet the following criteria within a 24 -hour period: – 1) three or more signs of the Systemic Inflammatory Syndrome – 2) the sepsis-induced dysfunction of at least one organ or system that has lasted no longer than 24 hours • Study group received drotrecogin alfa (activated) – 24 μg per kilogram of body weight per hour for a total duration of 96 hours Bernard et al, N Engl J Med, Vol. 344, No. 10 March 8, 2001
RCT: PROWESS Findings • Absolute reduction in the risk of death of 6. 1 percent • Mortality rate – 30. 8 percent in the placebo – 24. 7 percent in the drotrecogin alfa activated group Bernard et al, N Engl J Med, Vol. 344, No. 10 March 8, 2001
RCT: ADDRESS Drotrecogin Alfa (Activated) for Adults with Severe Sepsis and a Low Risk of Death • 2640 adults patients with severe sepsis and a low risk of death – (defined by an Acute Physiology and Chronic Health Evaluation [APACHE II] score <25 or single organ failure) – Randomized intravenous infusion Drot. AA (24 Μg per kilogram of body weight per hour) for 96 hours or placebo • Trial was terminated early – No benefit from treatment – Increased incidence of serious bleeding complications, • Conclusion Drot. AA should not be used in patients with severe sepsis who are at low risk for death Abraham, et al N Engl J Med 353; 13 Sept 29, 2005
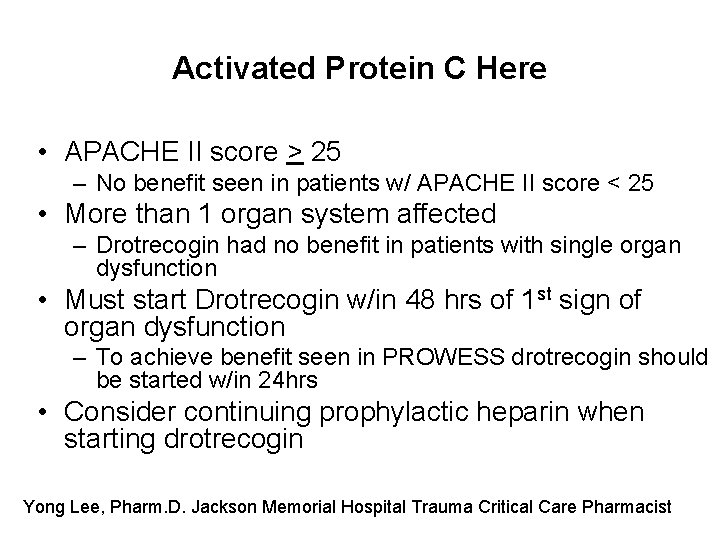
Activated Protein C Here • APACHE II score > 25 – No benefit seen in patients w/ APACHE II score < 25 • More than 1 organ system affected – Drotrecogin had no benefit in patients with single organ dysfunction • Must start Drotrecogin w/in 48 hrs of 1 st sign of organ dysfunction – To achieve benefit seen in PROWESS drotrecogin should be started w/in 24 hrs • Consider continuing prophylactic heparin when starting drotrecogin Yong Lee, Pharm. D. Jackson Memorial Hospital Trauma Critical Care Pharmacist
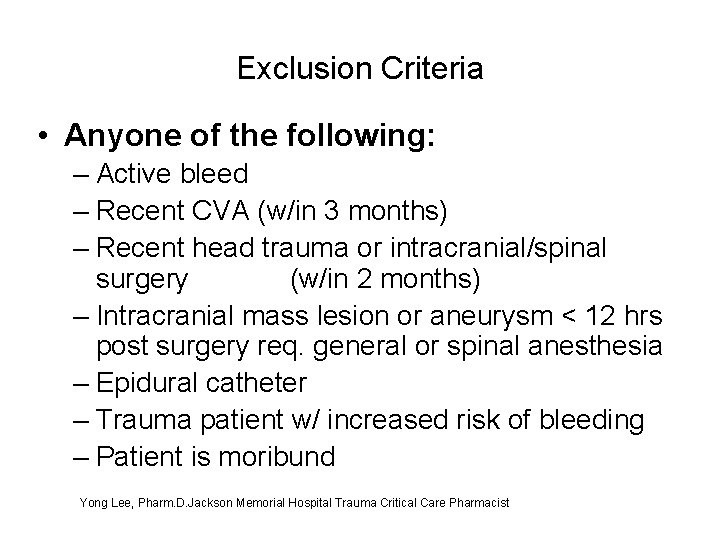
Exclusion Criteria • Anyone of the following: – Active bleed – Recent CVA (w/in 3 months) – Recent head trauma or intracranial/spinal surgery (w/in 2 months) – Intracranial mass lesion or aneurysm < 12 hrs post surgery req. general or spinal anesthesia – Epidural catheter – Trauma patient w/ increased risk of bleeding – Patient is moribund Yong Lee, Pharm. D. Jackson Memorial Hospital Trauma Critical Care Pharmacist
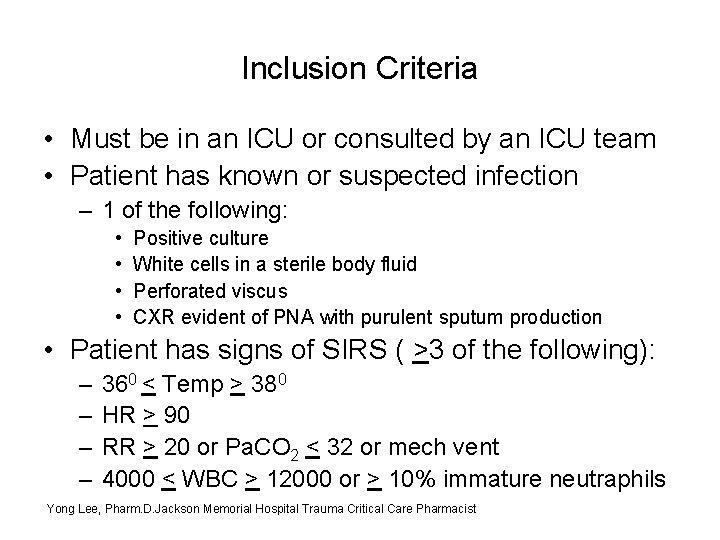
Inclusion Criteria • Must be in an ICU or consulted by an ICU team • Patient has known or suspected infection – 1 of the following: • • Positive culture White cells in a sterile body fluid Perforated viscus CXR evident of PNA with purulent sputum production • Patient has signs of SIRS ( >3 of the following): – – 360 < Temp > 380 HR > 90 RR > 20 or Pa. CO 2 < 32 or mech vent 4000 < WBC > 12000 or > 10% immature neutraphils Yong Lee, Pharm. D. Jackson Memorial Hospital Trauma Critical Care Pharmacist
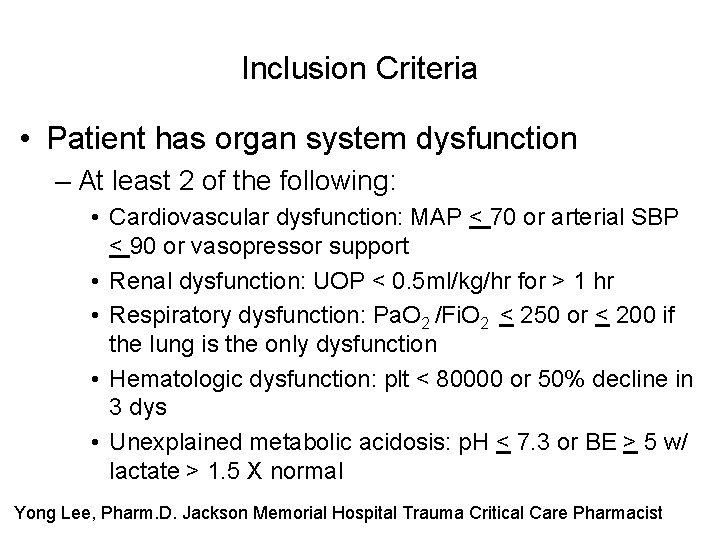
Inclusion Criteria • Patient has organ system dysfunction – At least 2 of the following: • Cardiovascular dysfunction: MAP < 70 or arterial SBP < 90 or vasopressor support • Renal dysfunction: UOP < 0. 5 ml/kg/hr for > 1 hr • Respiratory dysfunction: Pa. O 2 /Fi. O 2 < 250 or < 200 if the lung is the only dysfunction • Hematologic dysfunction: plt < 80000 or 50% decline in 3 dys • Unexplained metabolic acidosis: p. H < 7. 3 or BE > 5 w/ lactate > 1. 5 X normal Yong Lee, Pharm. D. Jackson Memorial Hospital Trauma Critical Care Pharmacist
Vasopressin Therapy for Septic Shock In early shock, appropriately high levels of vasopressin are produced to support organ perfusion. • As the shock state progresses, plasma vasopressin levels fall from: – depletion of pituitary stores of vasopressin exhaustive release in early septic shock – central inhibition from elevated norepinephrine levels (endogenous or exogenous) – central inhibition from increased nitric oxide release by vascular endothelium within the posterior pituitary during sepsis
Vasopressin and Septic Shock Trial (VASST) • Randomization trial of 778 patients with shock • 396 patients received vasopressin, and 382 norepinephrine • There was no significant difference : – 28 -day mortality rate (35. 4% and 39. 3%, respectively; P = 0. 26) – in 90 -day mortality (43. 9% and 49. 6%, respectively; P = 0. 11). – Overall rates of serious adverse events (10. 3% and 10. 5%, respectively; P = 1. 00). Russell et al, Vasopressin versus Norepinephrine Infusion in Patients with Septic Shock N Engl J Med 2008; 358: 877 -87
Hydrocortisone Therapy for Patients with Septic Shock • 499 patients multicenter • Randomized, double-blind, placebo-controlled trial • Concluded – Hydrocortisone did not improve survival or reversal of shock in patients with septic shock, either overall or in patients who did not have a response to corticotropin, although hydrocortisone hastened reversal of shock in patients in whom shock was reversed. Sprung et. Al N Engl J Med 358; 2 January 10, 2008
International task force by the American College of Critical Care Medicine • Review published literature concluded most of the research supports treatment with moderate-dose corticosteroids in patients with septic shock who have responded poorly to volume resuscitation and vasopressor agents • Tests of adrenal function are not routinely required in these patients. • Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: Consensus statements from an international task force by the American College of Critical Care Medicine Crit Care Med 2008 Vol. 36, No. 6
Management • Prevention • Removal of inciting factors • Support Recovery
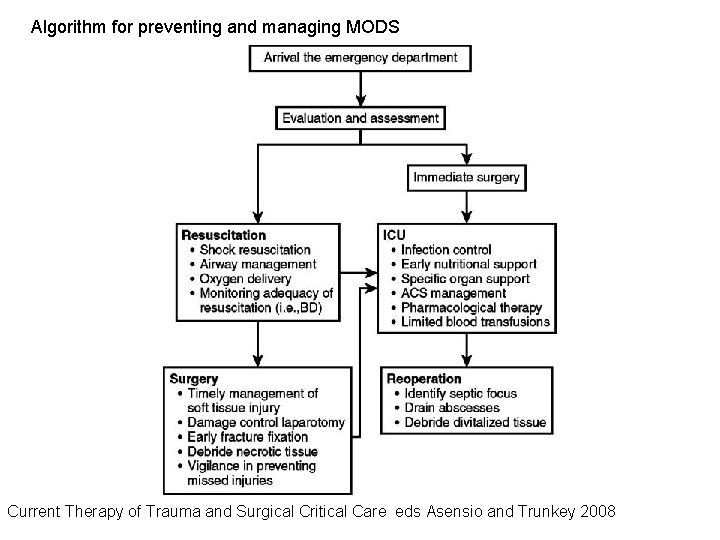
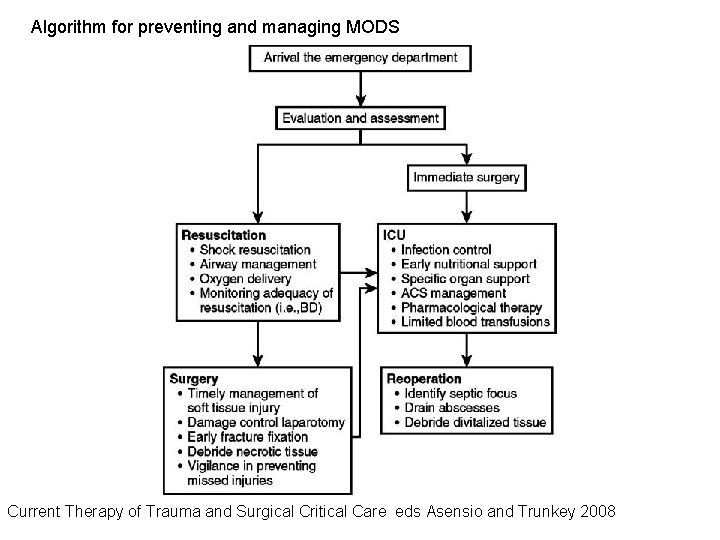
Algorithm for preventing and managing MODS Current Therapy of Trauma and Surgical Critical Care eds Asensio and Trunkey 2008
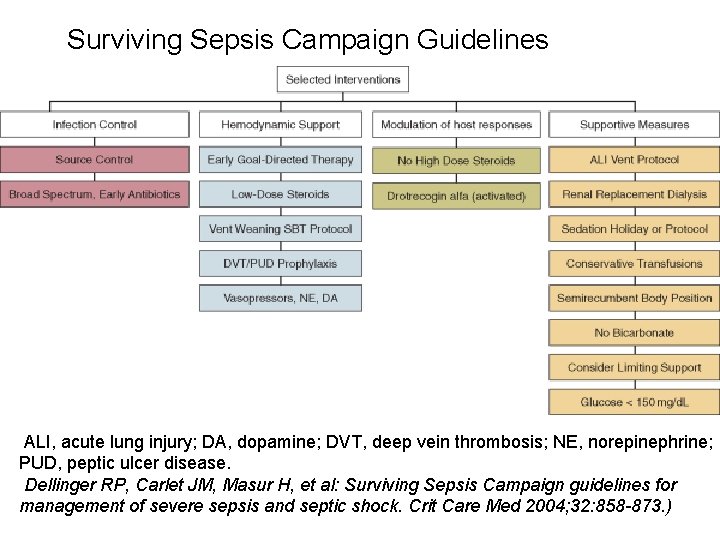
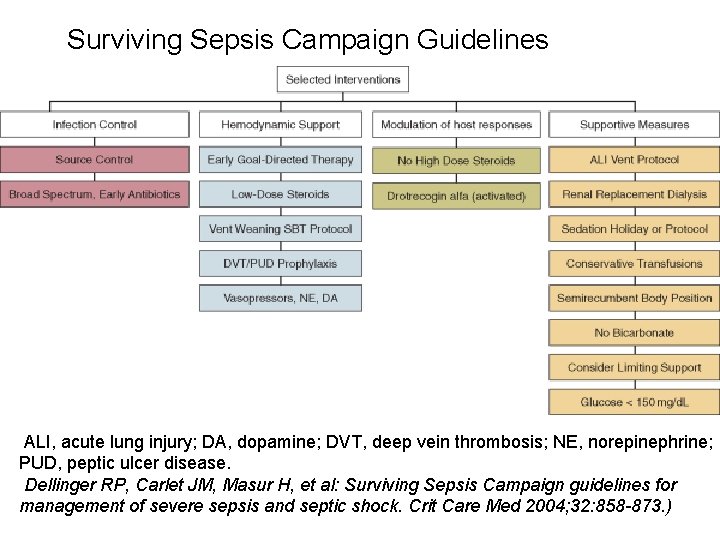
Surviving Sepsis Campaign Guidelines ALI, acute lung injury; DA, dopamine; DVT, deep vein thrombosis; NE, norepinephrine; PUD, peptic ulcer disease. Dellinger RP, Carlet JM, Masur H, et al: Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 2004; 32: 858 -873. )
Hemodynamic Support • Early Goal directed therapy • 1. Preload – Monitor/Support central venous pressure 8 - 12 mm Hg 12 - 15 mm Hg in mechanically ventilated patients • 2. After-load – Monitor/Support Mean arterial pressure >65 mm Hg – Urine output >0. 5 m. L/Kg/h • 4. Balance oxygen delivery and oxygen demand – Monitor/Support Oxygen balance – Central venous or mixed venous oxygen saturation >70%
Hemodynamic Support • Low-dose steroids administered for nonresponders to fluid and vasopressors – Hydrocortisone dose should be < 300 mg/day – Steroid therapy may be weaned once vasopressors are no longer required • Activated Protein C administered in accordance policy here
Infection Control Source Control • Early Identification abscess, infection with imaging/studies – ID treatable causes e. g. , necrotizing fasciitis, diffuse peritonitis, cholangitis, intestinal infarction • Early intervention – – • • Drainage of infected fluid collection Surgery to control /eliminate source if appropriate Debridement of infected solid tissue Removal of devices or foreign bodies Monitor/Address abdominal compartment syndrome Remove intravascular access devices if potentially infected Systemic Antibiotics • Broad-spectrum antibiotic therapy started within the first hour • Cultures (blood, urine, sputum, tissue) preferable prior, • Therapy adapted to most appropriate single drug as soon as antibiogram available. • Combination therapy for patients with known or suspected Pseudomonas infections and neutropenic patients with severe sepsis
Sepsis Resuscitation Bundle • 1. Serum lactate measured at clinical presentation • 2. Blood cultures obtained before antibiotics administered • 3. Broad-spectrum antibiotics within 3 hours • 4. In the event of hypotension or lactate >4 mmol/L (36 mg/d. L) – a. deliver an initial minimum of 20 m. L/kg of crystalloid (or colloid equivalent) – b. apply vasopressors for ongoing hypotension • 5. In the event of persistent hypotension despite fluid resuscitation or lactate >4 mmol/L (36 mg/d. L) – a. achieve central venous pressure of >8 mm Hg – b. Achieve central venous oxygen saturation > 70% The Role of Bundles in Sepsis Care Crit Care Clin 22 (2006) 521– 529
On Going Intensive Care Support • • DVT/PE prevention Ulcer Prevention Nutritional Support Glucose Control/Insulin therapy as needed Specific organ Support Minimize Blood Transfusion Infection control – Avoidance of Ventilator Associated Pneumonia – Avoidance of Catheter (any type) Related Infection
Long-term Outcome • Follow up 322 patients Trauma related organ failure • 47% had multiple organ failure (MOF), 28% had single organ failure. • Long-term survival and functional status were the same for patients suffering single organ failure and no organ failure. • MOF increased the overall risk of death 6. 0 times. • Complete recovery occurred in 52% of survivors 87% were able to look after themselves • MOF had 3. 9 times greater odds for requiring personal assistance in activities of daily living Ulvik A, Kvale R, Wentzel-Larsen T, et al. Multiple organ failure after trauma affects even long-term survival and functional status. Crit Care 2007; 11: R 95.
