Multimodality Imaging Overview of Common and Uncommon Solid



- Slides: 38
Multimodality Imaging Overview of Common and Uncommon Solid Parotid Space Masses e. Ed. E-139 Whitney Finke, MD, Nicholas Koontz, MD, Stephen Kralik, MD Department of Radiology & Imaging Sciences Indiana University School of Medicine Indianapolis, IN
Disclosures • None
Abbreviations • • • BMT = Benign Mixed Tumor • Tx = Treatment CECT = Contrast enhanced CT • +C = Contrast enhanced DCF = Deep cervical fascia EAC = External auditory canal FS = Fat-saturated MMT = Malignant Mixed Tumor NECT = Non-contrast enhanced CT PNT = Perineural tumor SCM = Sternocleidomastoid T 1 WI = T 1 weighted image T 2 WI = T 2 weighted image
Purpose • Provide a comprehensive overview of imaging characteristics of pathology-proven common & uncommon solid parotid space masses • Modalities • US • CT • MRI • FDG-PET/CT
Approach/Methods • We performed a HIPAA-compliant retrospective review of our institution's electronic medical record (radiology and pathology databases) for illustrative cases of histopathologically-proven parotid masses • Included cases with multimodality imaging when possible • Additionally, a review of the current medical literature was performed
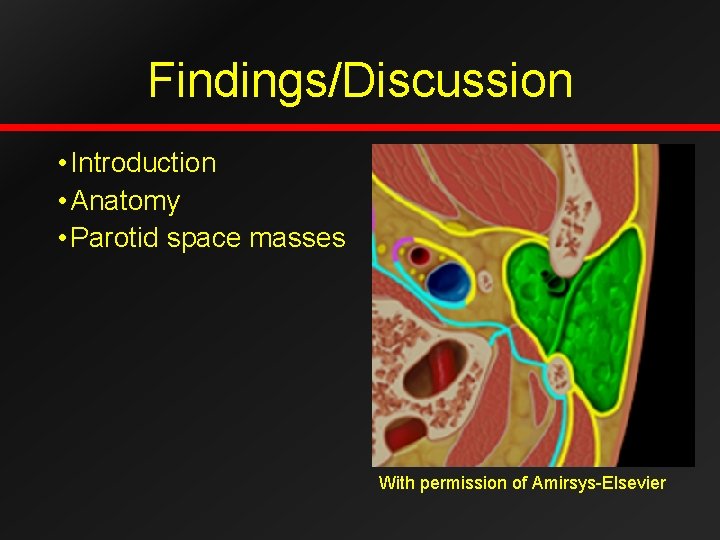
Findings/Discussion • Introduction • Anatomy • Parotid space masses With permission of Amirsys-Elsevier
Introduction • Largest salivary gland • Superficial “lobe” • 80% of glandular volume • Superficial to the plane of facial nerve • Overlies ramus and angle of mandible, superficial to masseter • Deep “lobe” • 20% of glandular volume • Medial extent through stylomandibular tunnel
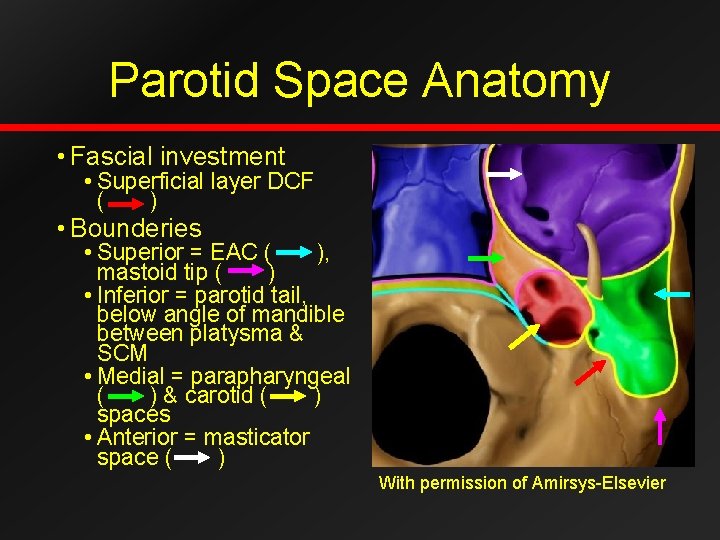
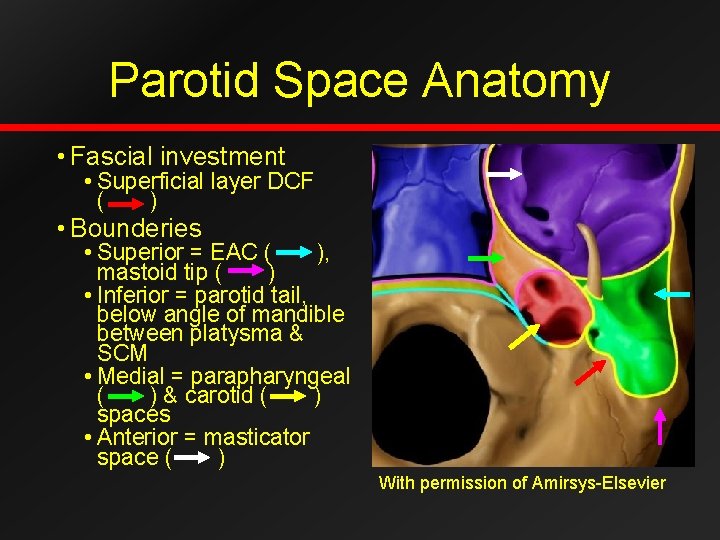
Parotid Space Anatomy • Fascial investment • Superficial layer DCF ( ) • Bounderies • Superior = EAC ( ), mastoid tip ( ) • Inferior = parotid tail, below angle of mandible between platysma & SCM • Medial = parapharyngeal ( ) & carotid ( ) spaces • Anterior = masticator space ( ) With permission of Amirsys-Elsevier
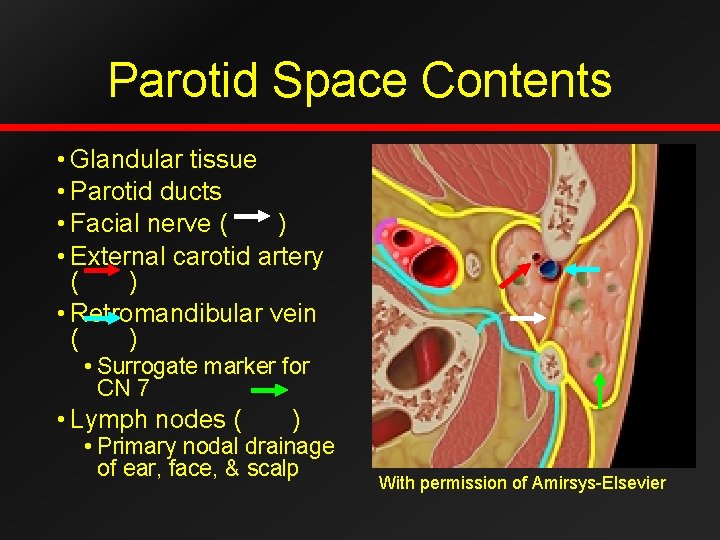
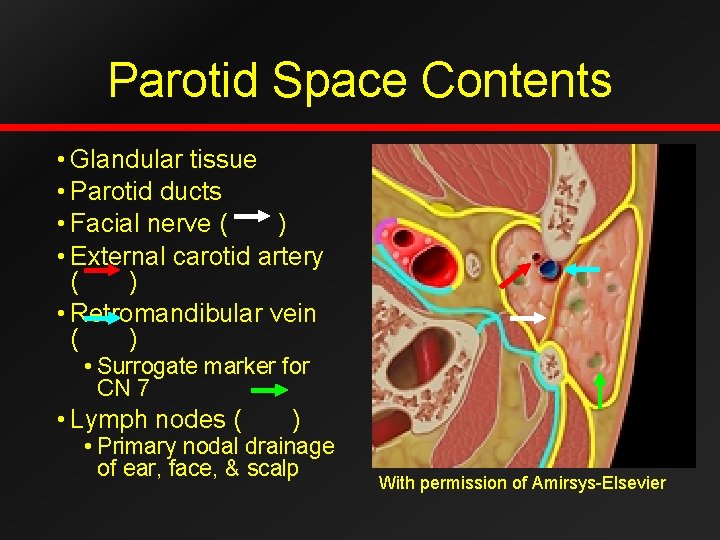
Parotid Space Contents • Glandular tissue • Parotid ducts • Facial nerve ( ) • External carotid artery ( ) • Retromandibular vein ( ) • Surrogate marker for CN 7 • Lymph nodes ( ) • Primary nodal drainage of ear, face, & scalp With permission of Amirsys-Elsevier
Parotid Masses • 80% of salivary gland masses • 80% benign (adults) • Pediatric masses higher rate of malignancy • Staging of malignant parotid masses • Weighted heavily based upon size • Subdivided based upon local extension • Skin • Soft tissues • Bone • Lingual or facial nerve • Nodal or distant metastases
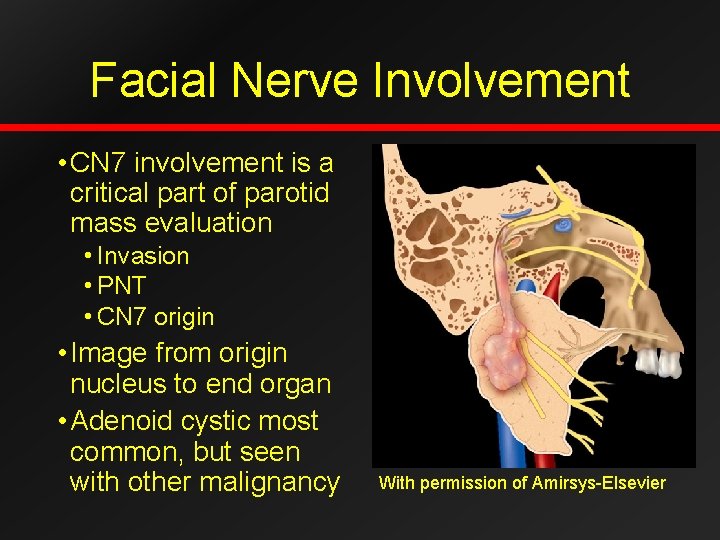
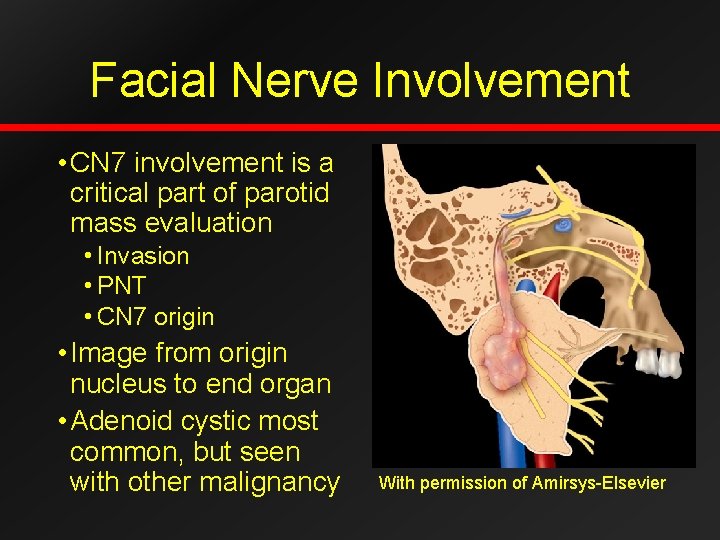
Facial Nerve Involvement • CN 7 involvement is a critical part of parotid mass evaluation • Invasion • PNT • CN 7 origin • Image from origin nucleus to end organ • Adenoid cystic most common, but seen with other malignancy With permission of Amirsys-Elsevier
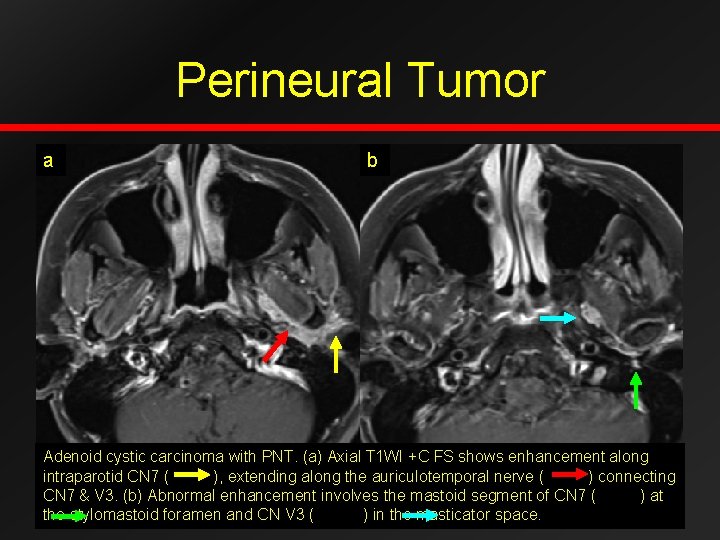
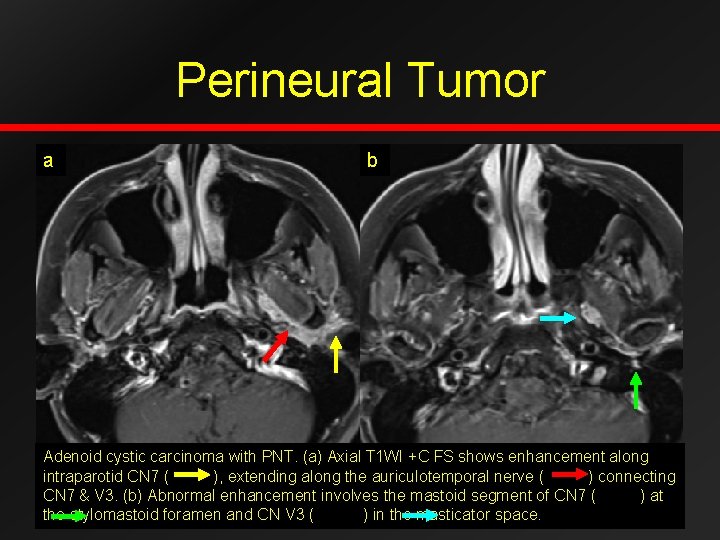
Perineural Tumor a b Adenoid cystic carcinoma with PNT. (a) Axial T 1 WI +C FS shows enhancement along intraparotid CN 7 ( ), extending along the auriculotemporal nerve ( ) connecting CN 7 & V 3. (b) Abnormal enhancement involves the mastoid segment of CN 7 ( ) at the stylomastoid foramen and CN V 3 ( ) in the masticator space.
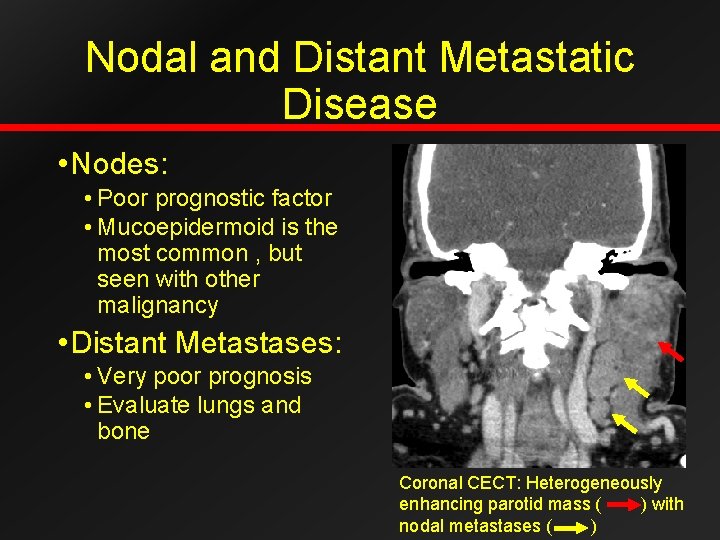
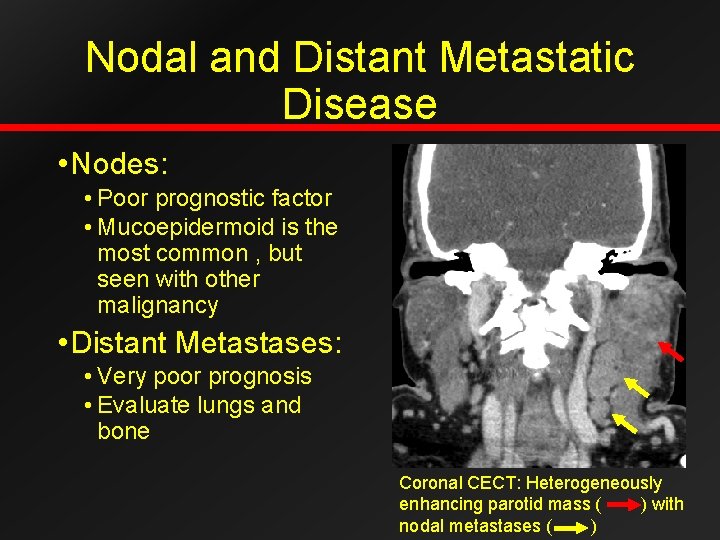
Nodal and Distant Metastatic Disease • Nodes: • Poor prognostic factor • Mucoepidermoid is the most common , but seen with other malignancy • Distant Metastases: • Very poor prognosis • Evaluate lungs and bone Coronal CECT: Heterogeneously enhancing parotid mass ( ) with nodal metastases ( )
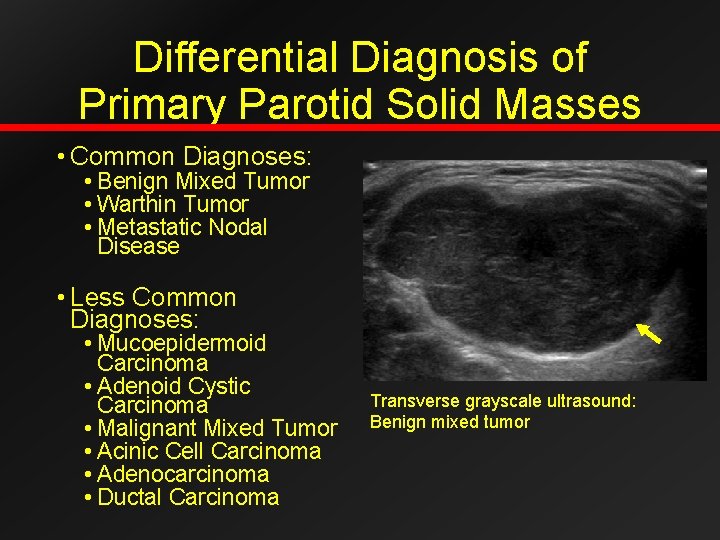
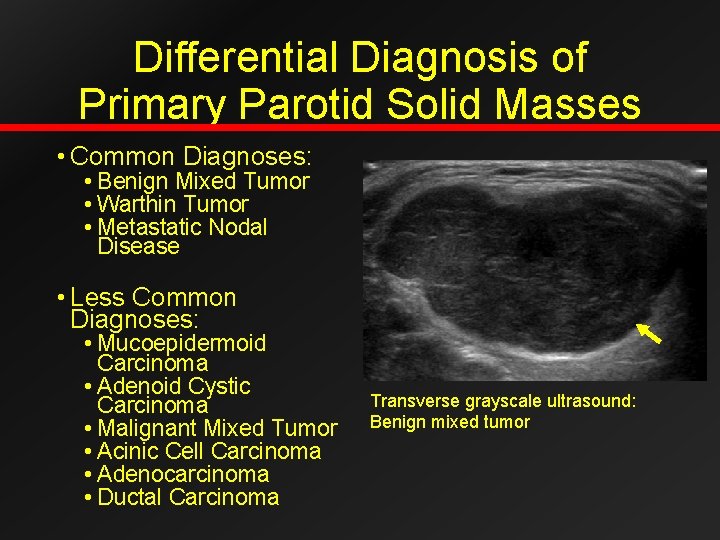
Differential Diagnosis of Primary Parotid Solid Masses • Common Diagnoses: • Benign Mixed Tumor • Warthin Tumor • Metastatic Nodal Disease • Less Common Diagnoses: • Mucoepidermoid Carcinoma • Adenoid Cystic Carcinoma • Malignant Mixed Tumor • Acinic Cell Carcinoma • Adenocarcinoma • Ductal Carcinoma Transverse grayscale ultrasound: Benign mixed tumor
General Imaging Overview: • Imaging is nonspecific. • 80% benign • 80% are benign mixed tumors. • Look for clues to suggest malignancy such as invasive margins, perineural spread, and lymphadenopathy. • FDG uptake does not always correspond with tumor grading. • Ultimately biopsy and excision are needed for definitive diagnosis.
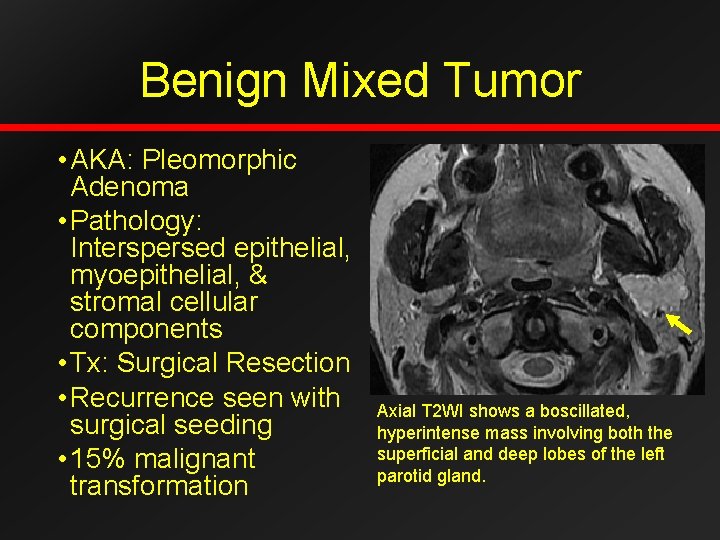
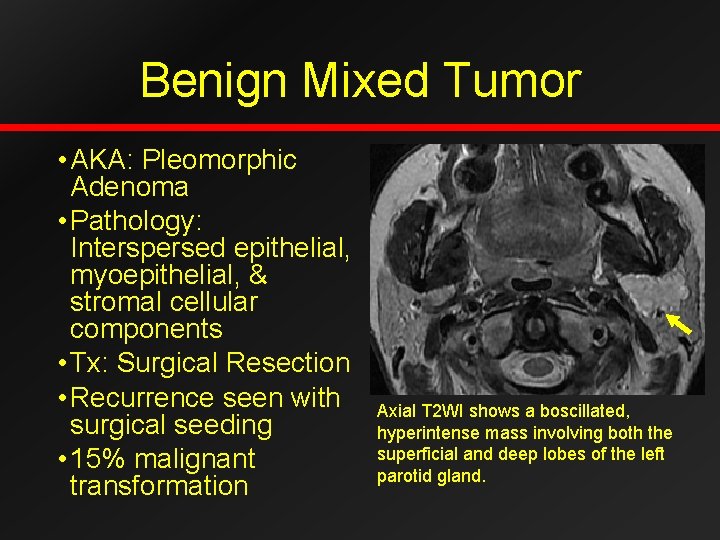
Benign Mixed Tumor • AKA: Pleomorphic Adenoma • Pathology: Interspersed epithelial, myoepithelial, & stromal cellular components • Tx: Surgical Resection • Recurrence seen with surgical seeding • 15% malignant transformation Axial T 2 WI shows a boscillated, hyperintense mass involving both the superficial and deep lobes of the left parotid gland.
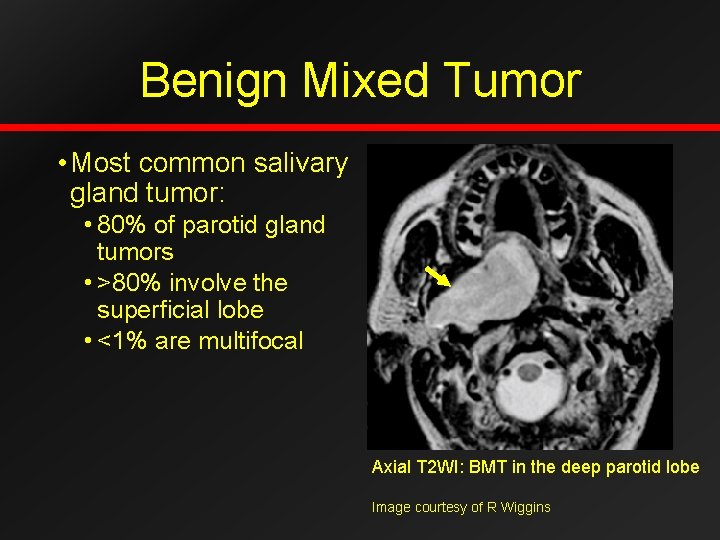
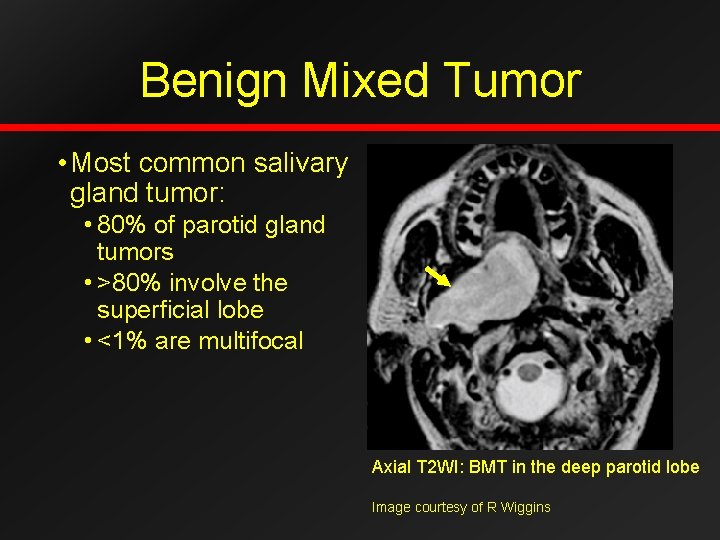
Benign Mixed Tumor • Most common salivary gland tumor: • 80% of parotid gland tumors • >80% involve the superficial lobe • <1% are multifocal Axial T 2 WI: BMT in the deep parotid lobe Image courtesy of R Wiggins
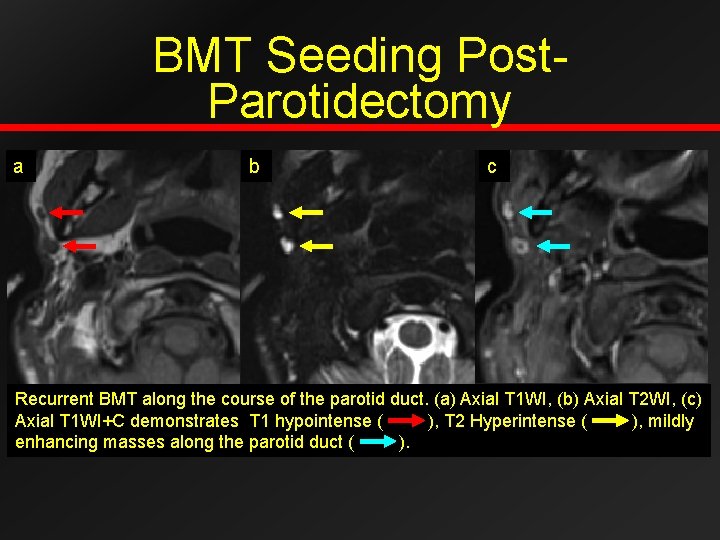
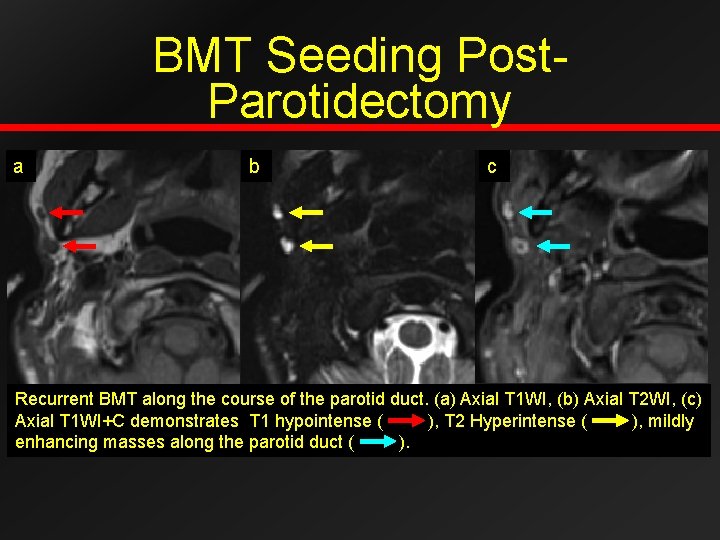
BMT Seeding Post. Parotidectomy a b c Recurrent BMT along the course of the parotid duct. (a) Axial T 1 WI, (b) Axial T 2 WI, (c) Axial T 1 WI+C demonstrates T 1 hypointense ( ), T 2 Hyperintense ( ), mildly enhancing masses along the parotid duct ( ).
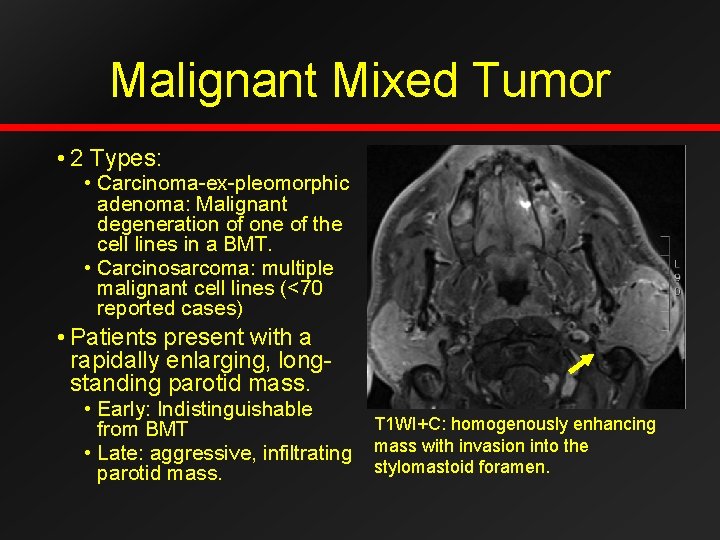
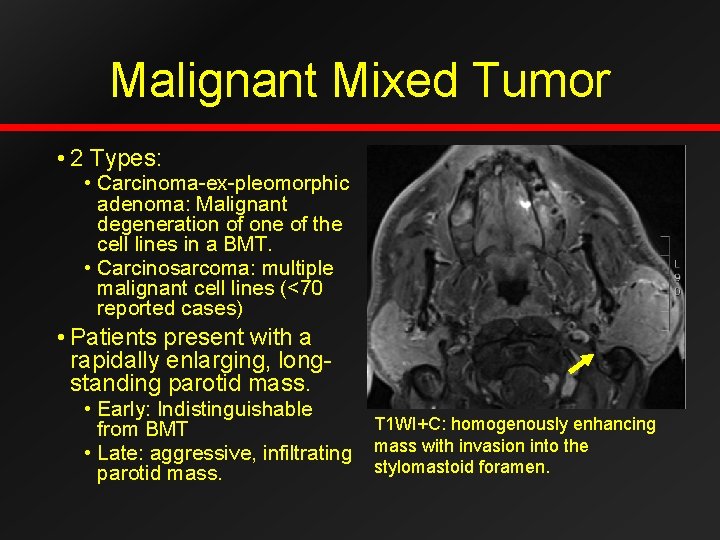
Malignant Mixed Tumor • 2 Types: • Carcinoma-ex-pleomorphic adenoma: Malignant degeneration of one of the cell lines in a BMT. • Carcinosarcoma: multiple malignant cell lines (<70 reported cases) • Patients present with a rapidally enlarging, longstanding parotid mass. • Early: Indistinguishable from BMT • Late: aggressive, infiltrating parotid mass. T 1 WI+C: homogenously enhancing mass with invasion into the stylomastoid foramen.
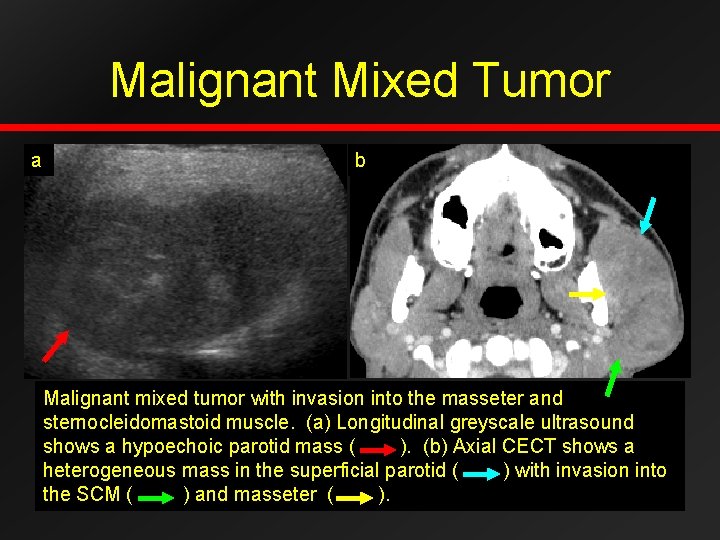
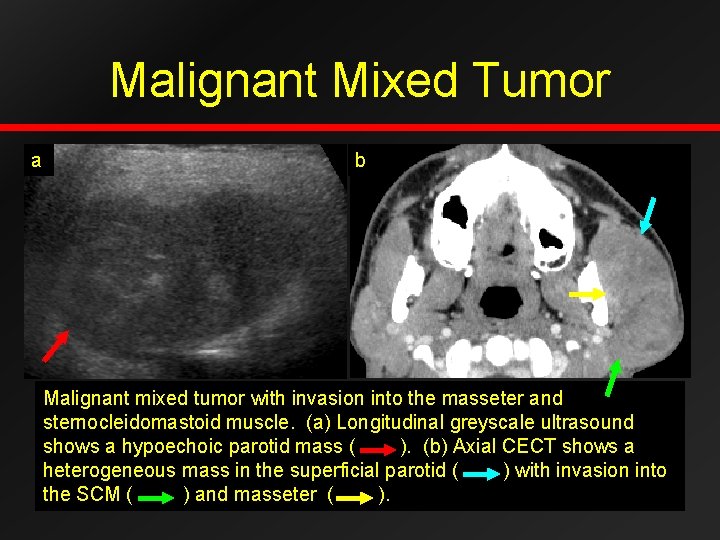
Malignant Mixed Tumor a b Malignant mixed tumor with invasion into the masseter and sternocleidomastoid muscle. (a) Longitudinal greyscale ultrasound shows a hypoechoic parotid mass ( ). (b) Axial CECT shows a heterogeneous mass in the superficial parotid ( ) with invasion into the SCM ( ) and masseter ( ).

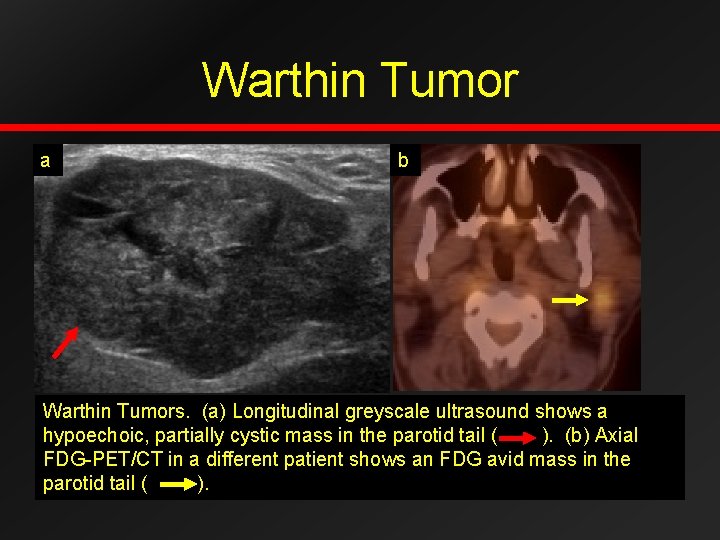
Warthin Tumor • Smoking associated • Arises from salivarylymphoid tissue • 2 nd most common benign parotid tumor • 2 -10% of parotid tumors • Most common parotid tail mass • 20% multifocal • 30% cystic component • FDG and Tc avid • Tx: excision (<1% malignant transformation) Axial CECT: hyperenhancing masses in the bilateral parotid tails.
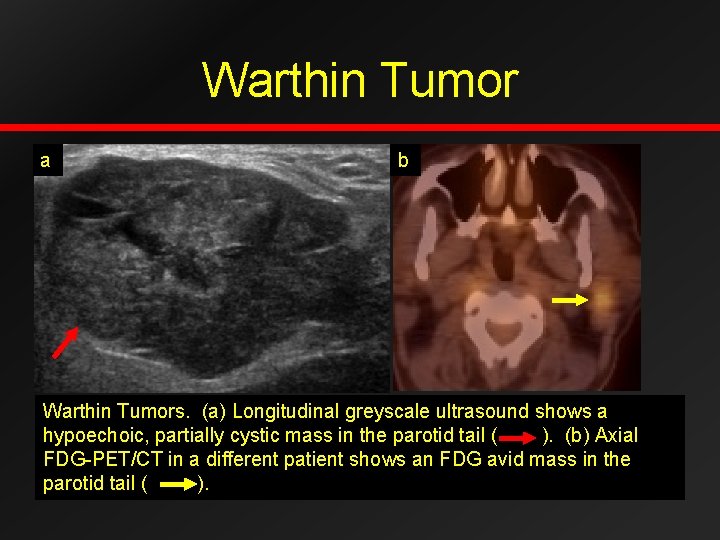
Warthin Tumor a b Warthin Tumors. (a) Longitudinal greyscale ultrasound shows a hypoechoic, partially cystic mass in the parotid tail ( ). (b) Axial FDG-PET/CT in a different patient shows an FDG avid mass in the parotid tail ( ).
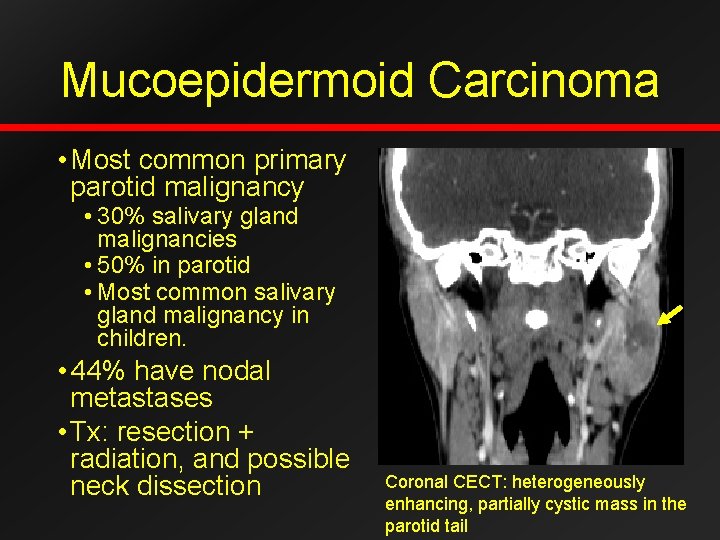
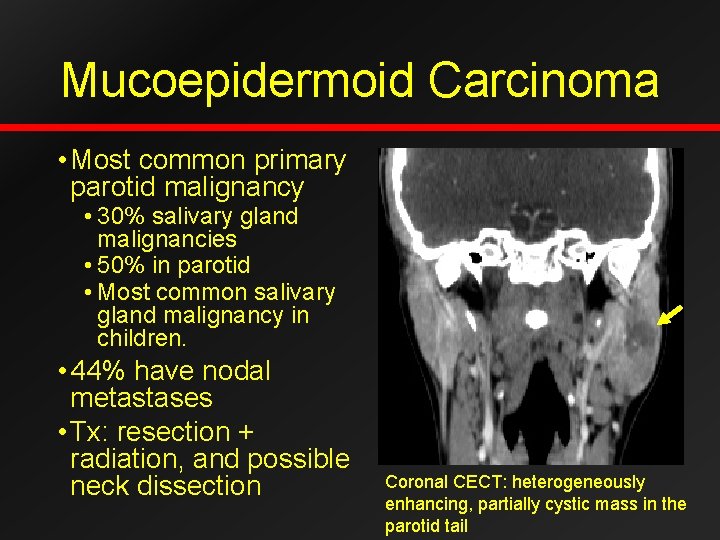
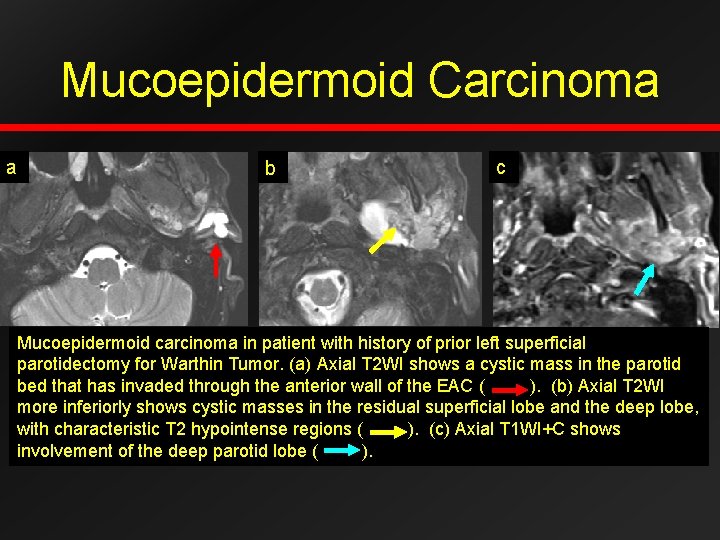
Mucoepidermoid Carcinoma • Most common primary parotid malignancy • 30% salivary gland malignancies • 50% in parotid • Most common salivary gland malignancy in children. • 44% have nodal metastases • Tx: resection + radiation, and possible neck dissection Coronal CECT: heterogeneously enhancing, partially cystic mass in the parotid tail
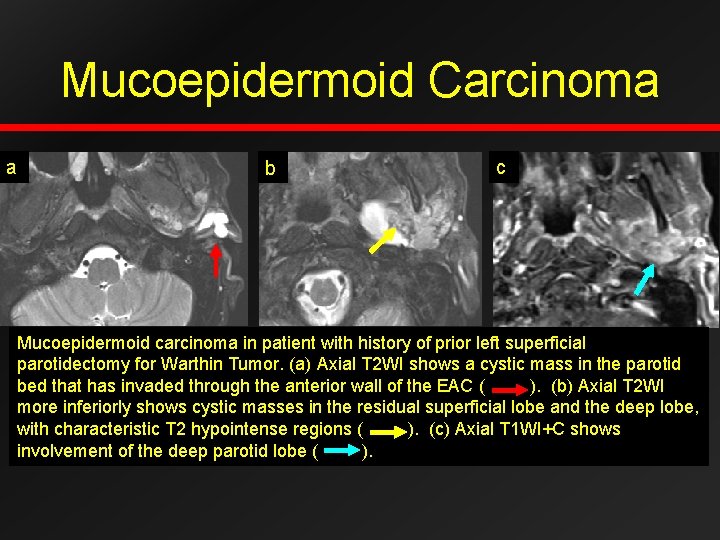
Mucoepidermoid Carcinoma a b c Mucoepidermoid carcinoma in patient with history of prior left superficial parotidectomy for Warthin Tumor. (a) Axial T 2 WI shows a cystic mass in the parotid bed that has invaded through the anterior wall of the EAC ( ). (b) Axial T 2 WI more inferiorly shows cystic masses in the residual superficial lobe and the deep lobe, with characteristic T 2 hypointense regions ( ). (c) Axial T 1 WI+C shows involvement of the deep parotid lobe ( ).
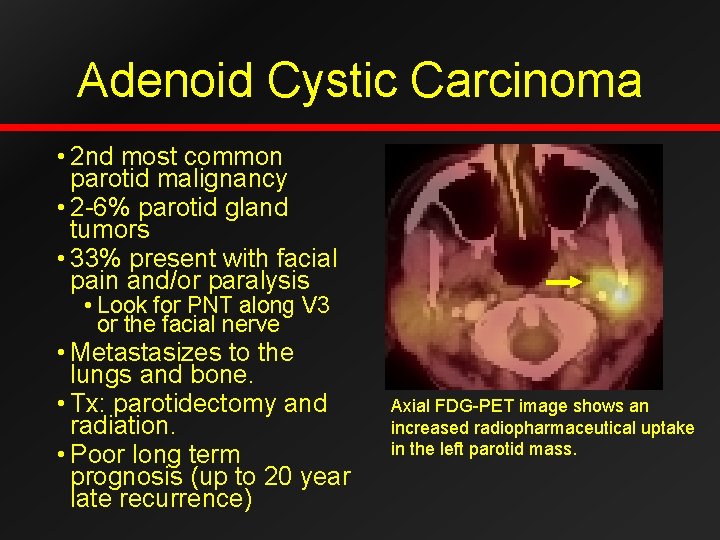
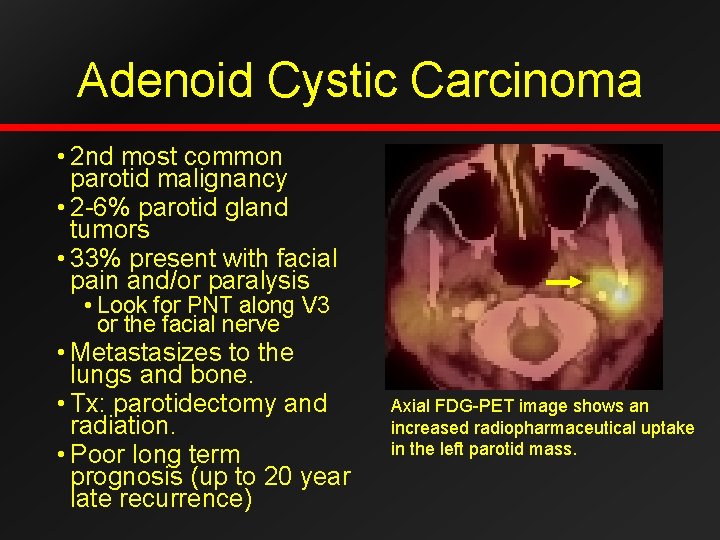
Adenoid Cystic Carcinoma • 2 nd most common parotid malignancy • 2 -6% parotid gland tumors • 33% present with facial pain and/or paralysis • Look for PNT along V 3 or the facial nerve • Metastasizes to the lungs and bone. • Tx: parotidectomy and radiation. • Poor long term prognosis (up to 20 year late recurrence) Axial FDG-PET image shows an increased radiopharmaceutical uptake in the left parotid mass.
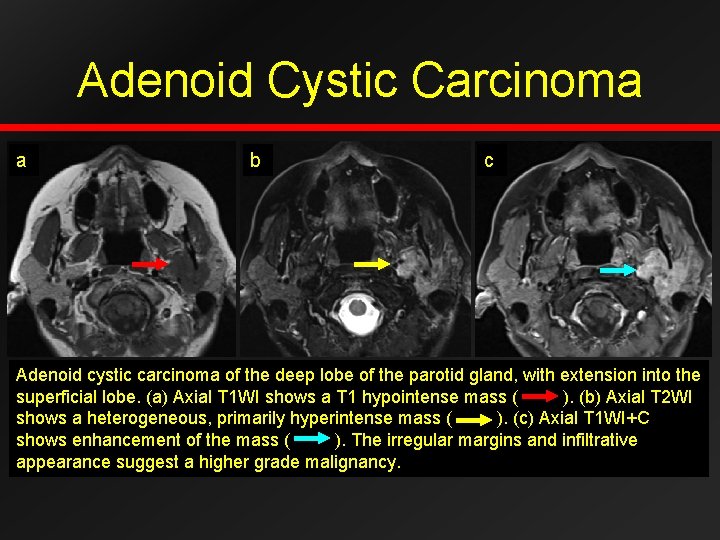
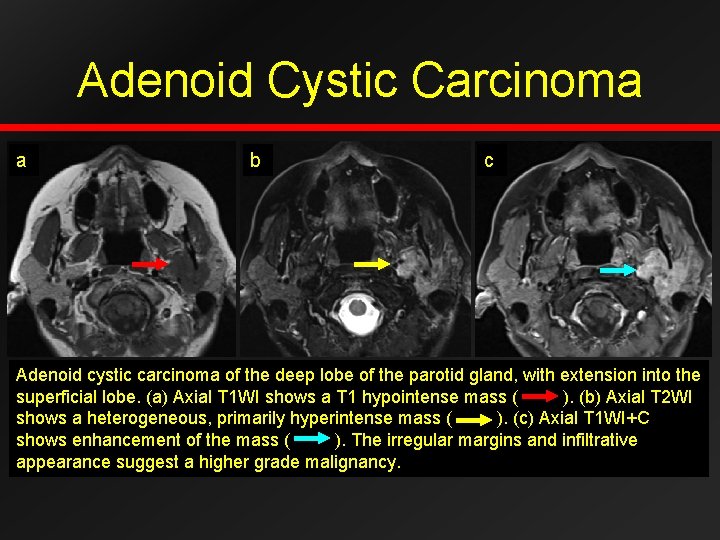
Adenoid Cystic Carcinoma a b c Adenoid cystic carcinoma of the deep lobe of the parotid gland, with extension into the superficial lobe. (a) Axial T 1 WI shows a T 1 hypointense mass ( ). (b) Axial T 2 WI shows a heterogeneous, primarily hyperintense mass ( ). (c) Axial T 1 WI+C shows enhancement of the mass ( ). The irregular margins and infiltrative appearance suggest a higher grade malignancy.
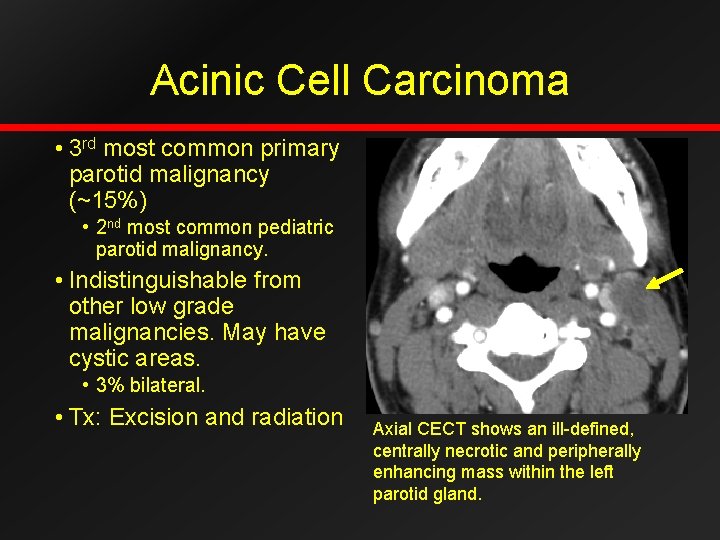
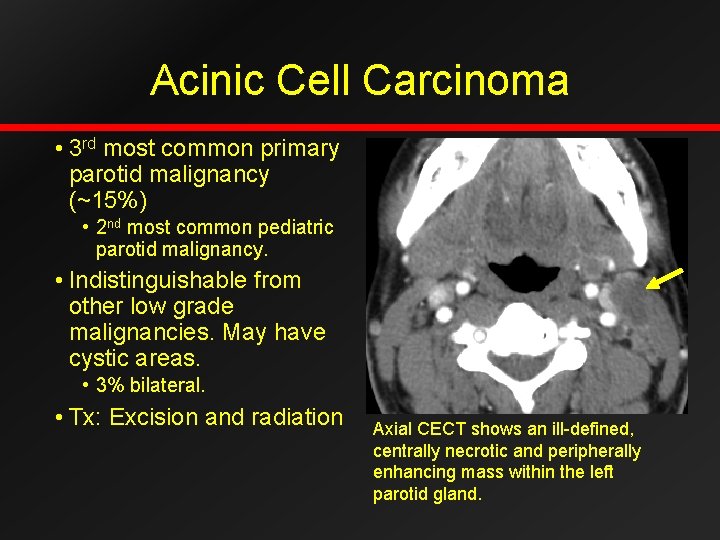
Acinic Cell Carcinoma • 3 rd most common primary parotid malignancy (~15%) • 2 nd most common pediatric parotid malignancy. • Indistinguishable from other low grade malignancies. May have cystic areas. • 3% bilateral. • Tx: Excision and radiation Axial CECT shows an ill-defined, centrally necrotic and peripherally enhancing mass within the left parotid gland.
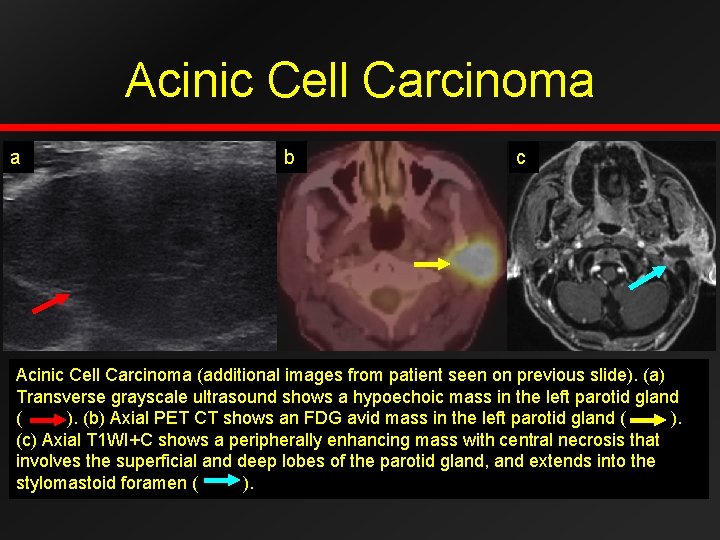
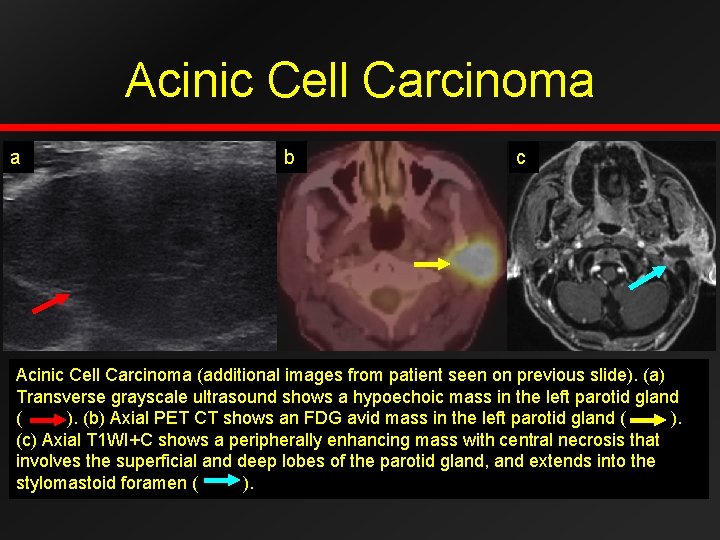
Acinic Cell Carcinoma a b c Acinic Cell Carcinoma (additional images from patient seen on previous slide). (a) Transverse grayscale ultrasound shows a hypoechoic mass in the left parotid gland ( ). (b) Axial PET CT shows an FDG avid mass in the left parotid gland ( ). (c) Axial T 1 WI+C shows a peripherally enhancing mass with central necrosis that involves the superficial and deep lobes of the parotid gland, and extends into the stylomastoid foramen ( ).
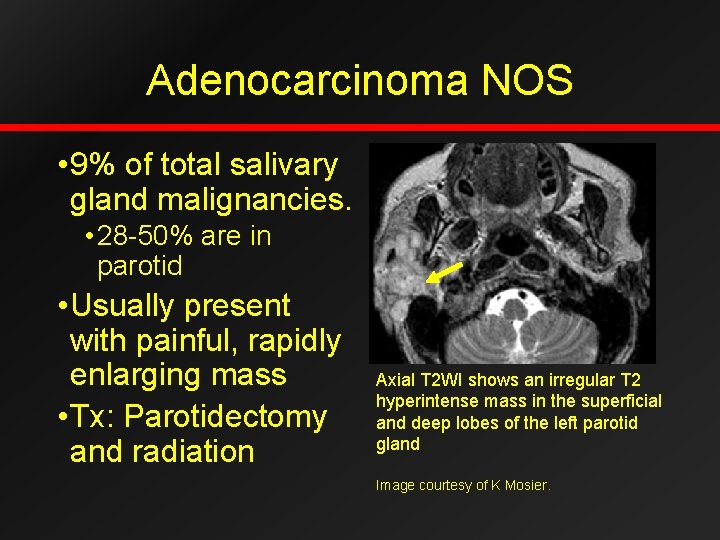
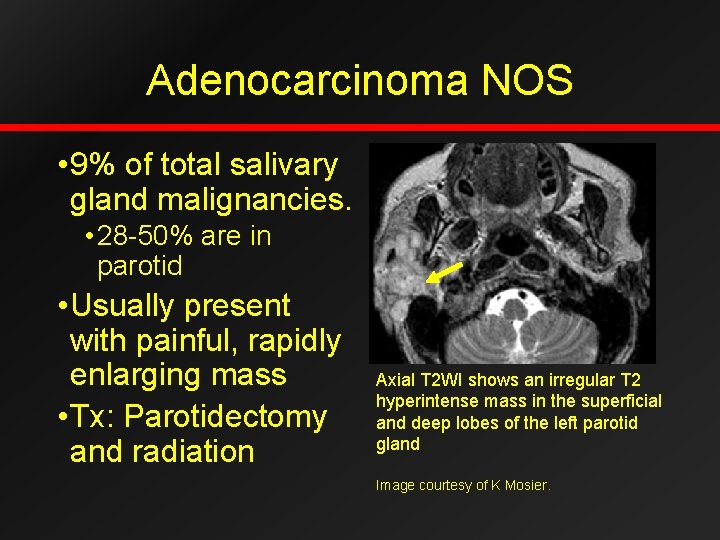
Adenocarcinoma NOS • 9% of total salivary gland malignancies. • 28 -50% are in parotid • Usually present with painful, rapidly enlarging mass • Tx: Parotidectomy and radiation Axial T 2 WI shows an irregular T 2 hyperintense mass in the superficial and deep lobes of the left parotid gland Image courtesy of K Mosier.

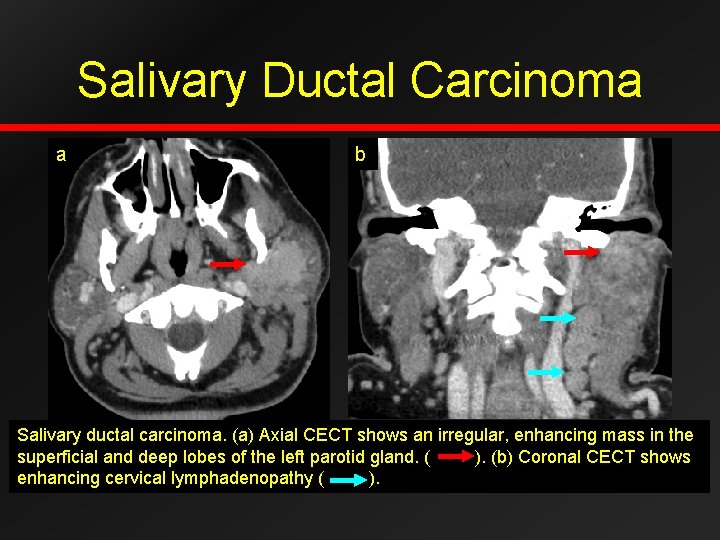
Salivary Ductal Carcinoma • Pathology: Similar to invasive ductal carcinoma of the breast. • Uncommon, extremely aggressive malignancy • Perineural spread is common • Cervical nodal metastasis in 70% • Distant metastasis to lung, bone, brain Axial CECT shows an ill defined enhancing mass in the superficial and deep lobes of the left parotid gland, with extension into the stylomandibular tunnel
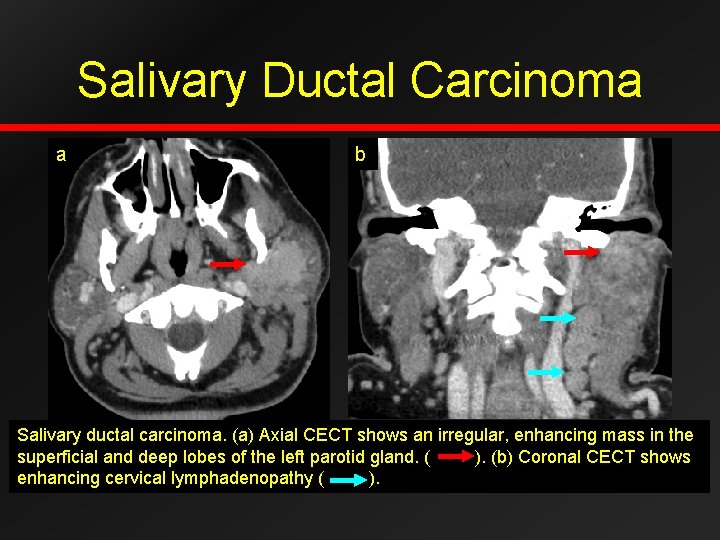
Salivary Ductal Carcinoma a b Salivary ductal carcinoma. (a) Axial CECT shows an irregular, enhancing mass in the superficial and deep lobes of the left parotid gland. ( ). (b) Coronal CECT shows enhancing cervical lymphadenopathy ( ).

Squamous Cell Carcinoma • Rare • 0. 1 -0. 5% parotid tumors • 3 -10% malignant parotid tumors • Squamous metaplasia develops secondary to chronic inflammation • Must exclude metastatic disease from skin • Metastasizes to regional nodes, lungs, and liver. Axial CECT shows an ill defined enhancing mass in the right parotid gland with areas of necrosis. Patient had a history of long standing chronic sialadenitis
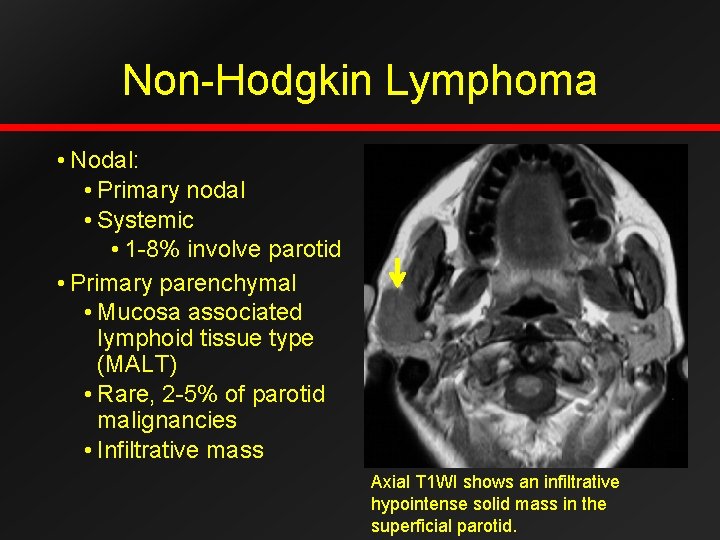
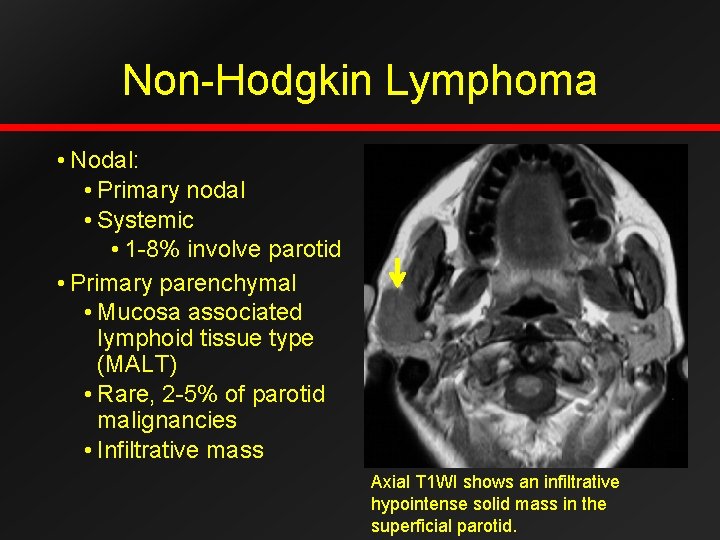
Non-Hodgkin Lymphoma • Nodal: • Primary nodal • Systemic • 1 -8% involve parotid • Primary parenchymal • Mucosa associated lymphoid tissue type (MALT) • Rare, 2 -5% of parotid malignancies • Infiltrative mass Axial T 1 WI shows an infiltrative hypointense solid mass in the superficial parotid.
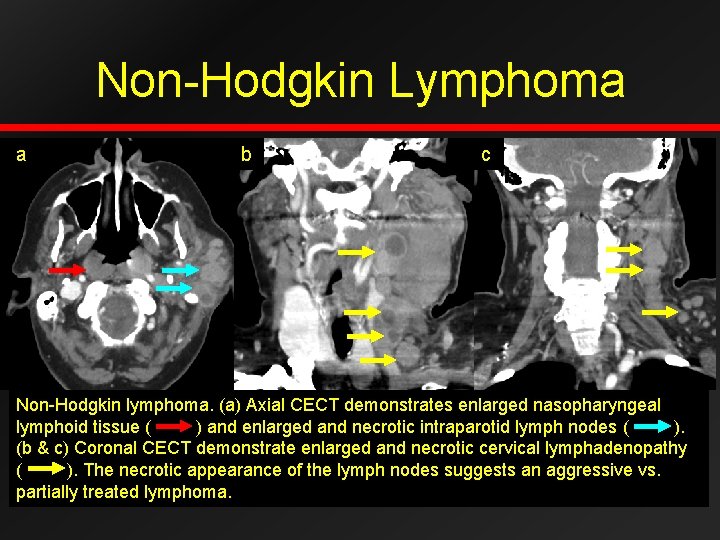
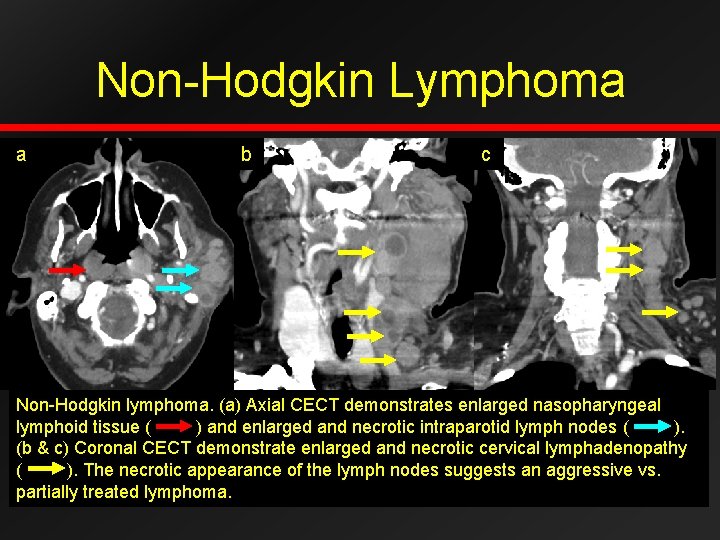
Non-Hodgkin Lymphoma a b c Non-Hodgkin lymphoma. (a) Axial CECT demonstrates enlarged nasopharyngeal lymphoid tissue ( ) and enlarged and necrotic intraparotid lymph nodes ( ). (b & c) Coronal CECT demonstrate enlarged and necrotic cervical lymphadenopathy ( ). The necrotic appearance of the lymph nodes suggests an aggressive vs. partially treated lymphoma.
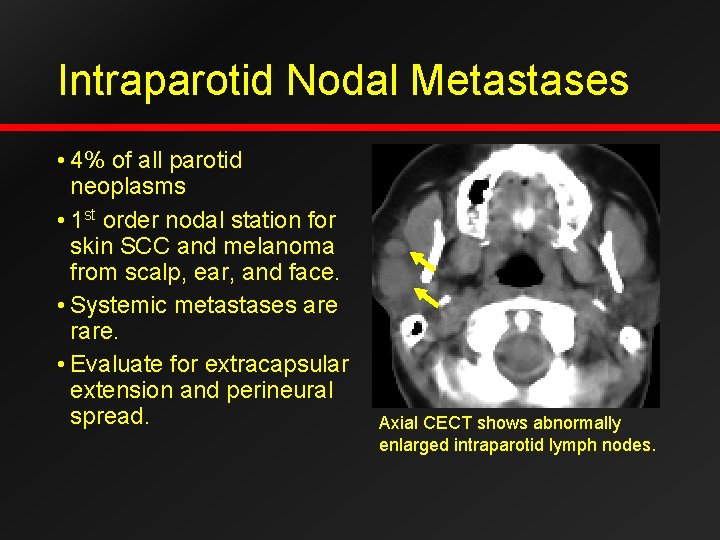
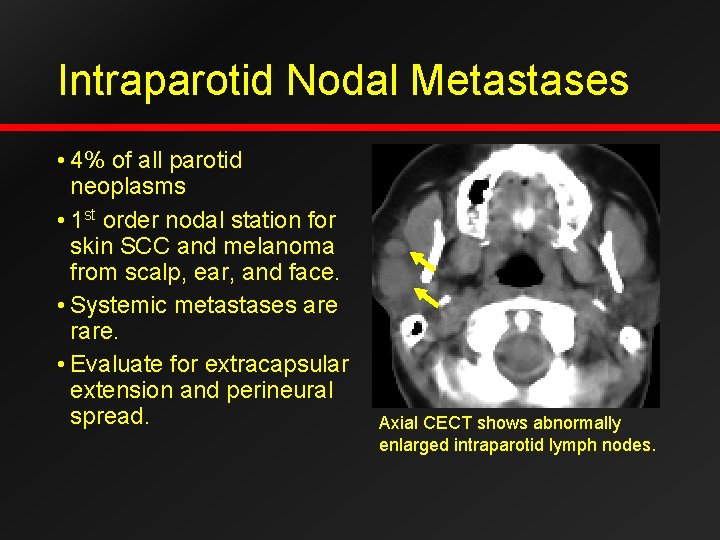
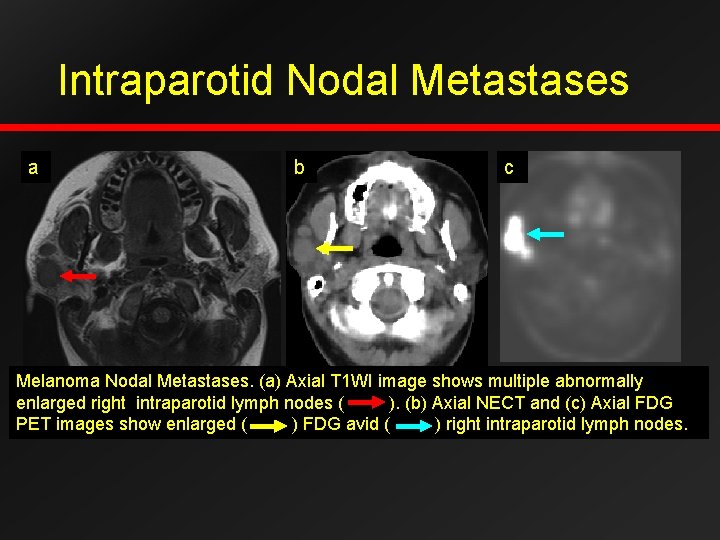
Intraparotid Nodal Metastases • 4% of all parotid neoplasms • 1 st order nodal station for skin SCC and melanoma from scalp, ear, and face. • Systemic metastases are rare. • Evaluate for extracapsular extension and perineural spread. Axial CECT shows abnormally enlarged intraparotid lymph nodes.
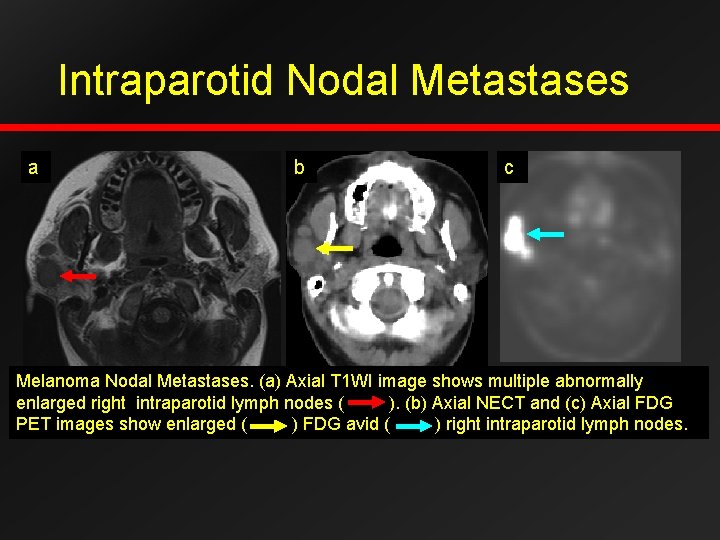
Intraparotid Nodal Metastases a b c Melanoma Nodal Metastases. (a) Axial T 1 WI image shows multiple abnormally enlarged right intraparotid lymph nodes ( ). (b) Axial NECT and (c) Axial FDG PET images show enlarged ( ) FDG avid ( ) right intraparotid lymph nodes.
Conclusion: • Imaging is nonspecific. • Look for clues such as invasive margins, perineural spread, lymphadenopathy, and multifocality. • 80% benign • 80% are benign mixed tumors. • Invasive margins suggest a more aggressive tumor. • Ultimately biopsy and excision are needed for definitive diagnosis.
References • Aiken AH et al: Imaging Hodgkin and non-Hodgkin lymphoma in the head and neck. Radiol Clin North Am. 46(2): 363 -78, ix-x, 2008 • Christe, A, Waldherr, C, Hallet, R, et al. MR Imaging of Parotid Tumors: Typical Lesion Characteristics in MR Imaging Improve Discrmination between Benign and Malignant Disease. AJNR Am J Neuroradiol 2011 32: 1202 -1207. • Freling NJ et al: Malignant parotid tumors: clinical use of MR imaging and histologic correlation. Radiology. 1992. 185(3): 691 -696. • Guzzo M et al: Major and minor salivary gland tumors. Crit Rev Oncol Hematol. 74(2): 134 -48, 2010 • Habermann CR et al: Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol. 30(3): 591 -6, 2009. • Hamilton BE, Salzman KL, Wiggins RH, et al. Earring lesions of the parotid tail. AJNR Am J Neuroradiol 2003; 24: 1757 -64. • Kato H et al: Carcinoma ex pleomorphic adenoma of the parotid gland: radiologic-pathologic correlation with MR imaging including diffusion-weighted imaging. AJNR Am J Neuroradiol. 29(5): 8657, 2008. • Lee YY et al: Imaging of salivary gland tumours. Eur J Radiol. 66(3): 419 -36, 2008. • Maroldi R et al: Perineural tumor spread. Neuroimaging Clin N Am. 18(2): 413 -29, xi, 2008 • Mlika, Mona, Kourda, Nadia, Zidi, YSH, et al. Salivary duct carcinoma of the parotid gland. J Oral Maxillofac Pathol 2012; 16 (1): 134 -136.