MUAC 120 mm AS A SIMPLE SAFE AND

- Slides: 12

MUAC ≥ 120 mm AS A SIMPLE, SAFE AND EFFECTIVE DISCHARGE CRITERIA FOR SAM IN BIHAR, INDIA MSF SPAIN
Structure of the session 1. Background 2. Methods 3. Programme outcomes 4. Long-term outcomes 5. Conclusions
Background • India has 40% of the worldwide burden of childhood SAM. • WHO currently recommends admission using MUAC<115 mm and/or WHZ<-3 SD, and discharge when 15% body-weight has increased. Although this 15% increase has been discredited, debate is ongoing regarding using different MUAC and/or W/H cut-offs for discharge. • MUAC has been shown to be an effective method for screening and admitting SAM children, and much simpler than W/H. • MSF in Bihar is one of the only and longest running CMAM programmes worldwide routinely using exclusively MUAC+/-oedema for admission (<115 mm) and discharge (≥ 120 mm) • This presentation describes the programmatic results and long-term outcomes of using exclusively MUAC≥ 120 mm for discharge for children 659 months of age.
Methods • Data from all children cured (defined as MUAC≥ 120 mm) from July 2010 -September 2011 (n=2288) were retrospectively analyzed. – Children with oedema (0. 3%, n=8), length of stay<14 days (3. 8%, n=95) and >140 days (2. 9%, n=71) were excluded. • During a targeted follow-up study, children discharged as cured from the programme were traced up to 18 months post -discharge (n=1036). • These results were then matched.
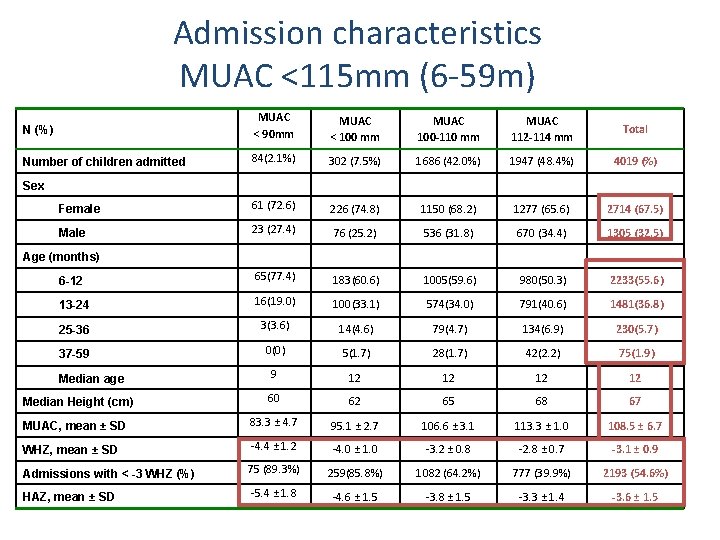
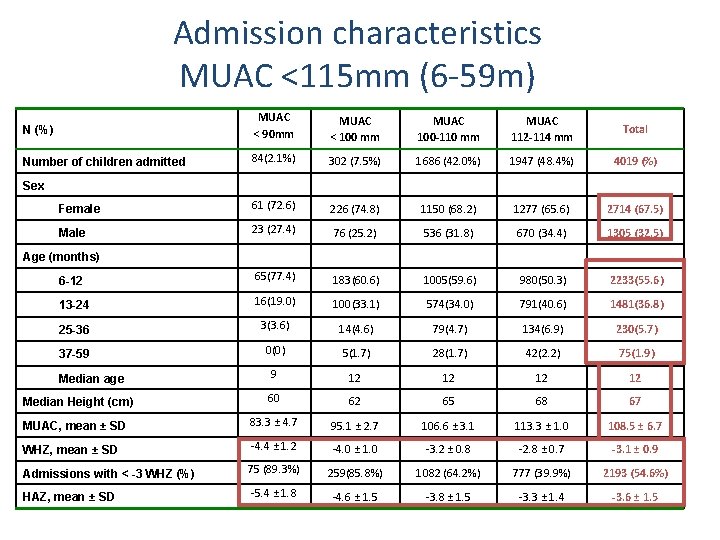
Admission characteristics MUAC <115 mm (6 -59 m) N (%) MUAC < 90 mm MUAC < 100 mm MUAC 100 -110 mm MUAC 112 -114 mm Total Number of children admitted 84(2. 1%) 302 (7. 5%) 1686 (42. 0%) 1947 (48. 4%) 4019 (%) Female 61 (72. 6) 226 (74. 8) 1150 (68. 2) 1277 (65. 6) 2714 (67. 5) Male 23 (27. 4) 76 (25. 2) 536 (31. 8) 670 (34. 4) 1305 (32. 5) 6 -12 65(77. 4) 183(60. 6) 1005(59. 6) 980(50. 3) 2233(55. 6) 13 -24 16(19. 0) 100(33. 1) 574(34. 0) 791(40. 6) 1481(36. 8) 25 -36 3(3. 6) 14(4. 6) 79(4. 7) 134(6. 9) 230(5. 7) 37 -59 0(0) 5(1. 7) 28(1. 7) 42(2. 2) 75(1. 9) 9 12 12 Median Height (cm) 60 62 65 68 67 MUAC, mean ± SD 83. 3 ± 4. 7 95. 1 ± 2. 7 106. 6 ± 3. 1 113. 3 ± 1. 0 108. 5 ± 6. 7 WHZ, mean ± SD -4. 4 ± 1. 2 -4. 0 ± 1. 0 -3. 2 ± 0. 8 -2. 8 ± 0. 7 -3. 1 ± 0. 9 Admissions with < -3 WHZ (%) 75 (89. 3%) 259(85. 8%) 1082 (64. 2%) 777 (39. 9%) 2193 (54. 6%) HAZ, mean ± SD -5. 4 ± 1. 8 -4. 6 ± 1. 5 -3. 8 ± 1. 5 -3. 3 ± 1. 4 -3. 6 ± 1. 5 Sex Age (months) Median age
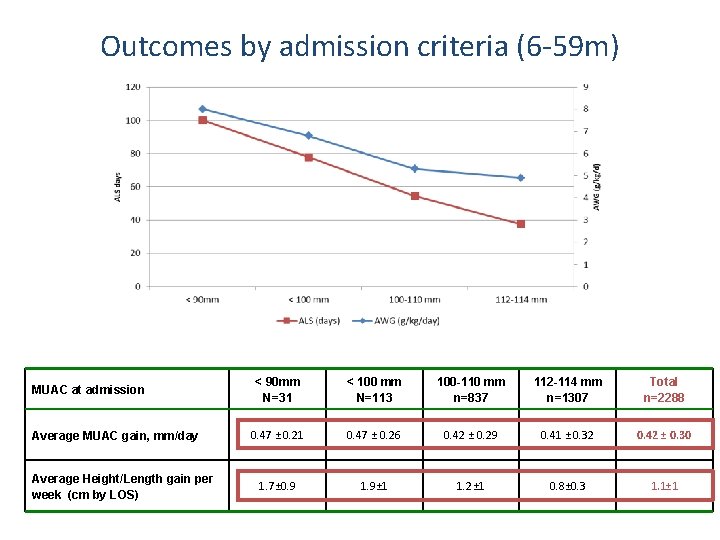
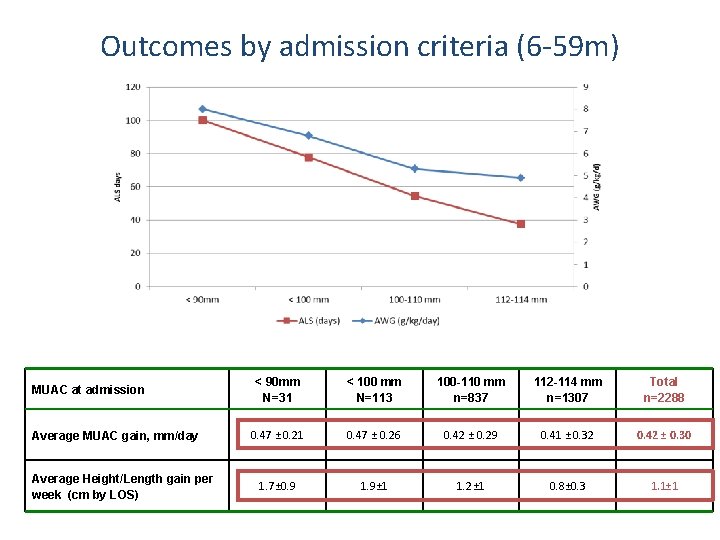
Outcomes by admission criteria (6 -59 m) MUAC at admission Average MUAC gain, mm/day Average Height/Length gain per week (cm by LOS) < 90 mm N=31 < 100 mm N=113 100 -110 mm n=837 112 -114 mm n=1307 Total n=2288 0. 47 ± 0. 21 0. 47 ± 0. 26 0. 42 ± 0. 29 0. 41 ± 0. 32 0. 42 ± 0. 30 1. 7± 0. 9 1. 9± 1 1. 2± 1 0. 8± 0. 3 1. 1± 1
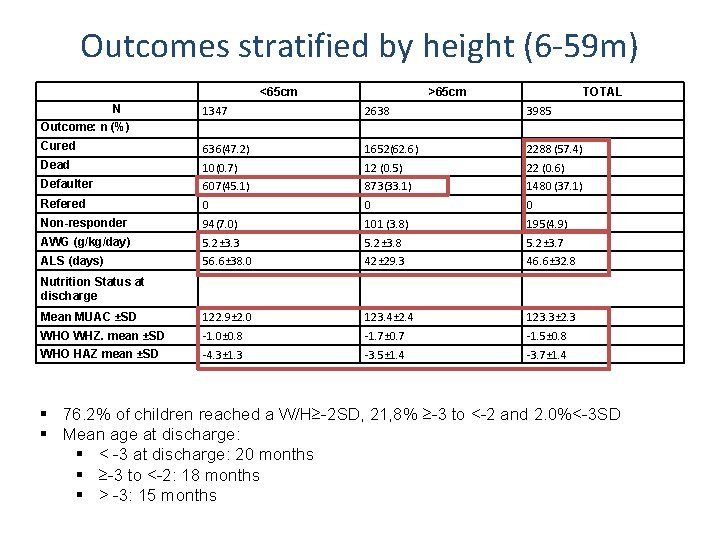
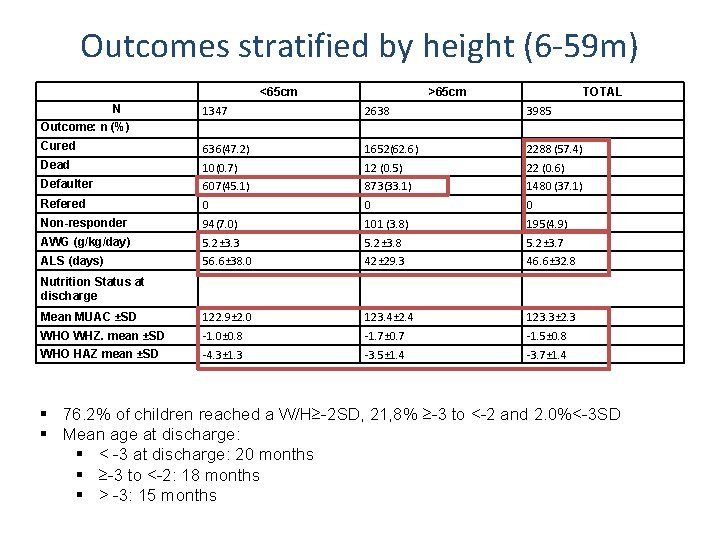
Outcomes stratified by height (6 -59 m) <65 cm N >65 cm TOTAL 1347 2638 3985 Cured 636(47. 2) 1652(62. 6) 2288 (57. 4) Dead 10(0. 7) 12 (0. 5) 22 (0. 6) Defaulter 607(45. 1) 873(33. 1) 1480 (37. 1) Refered 0 0 0 Non-responder 94(7. 0) 101 (3. 8) 195(4. 9) AWG (g/kg/day) 5. 2± 3. 3 5. 2± 3. 8 5. 2± 3. 7 ALS (days) 56. 6± 38. 0 42± 29. 3 46. 6± 32. 8 Mean MUAC ±SD 122. 9± 2. 0 123. 4± 2. 4 123. 3± 2. 3 WHO WHZ. mean ±SD -1. 0± 0. 8 -1. 7± 0. 7 -1. 5± 0. 8 WHO HAZ mean ±SD -4. 3± 1. 3 -3. 5± 1. 4 -3. 7± 1. 4 Outcome: n (%) Nutrition Status at discharge § 76. 2% of children reached a W/H≥-2 SD, 21, 8% ≥-3 to <-2 and 2. 0%<-3 SD § Mean age at discharge: § < -3 at discharge: 20 months § ≥-3 to <-2: 18 months § > -3: 15 months
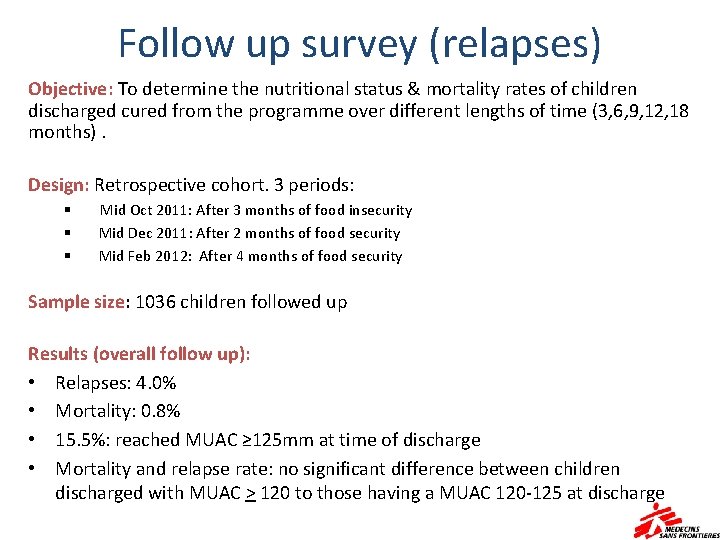
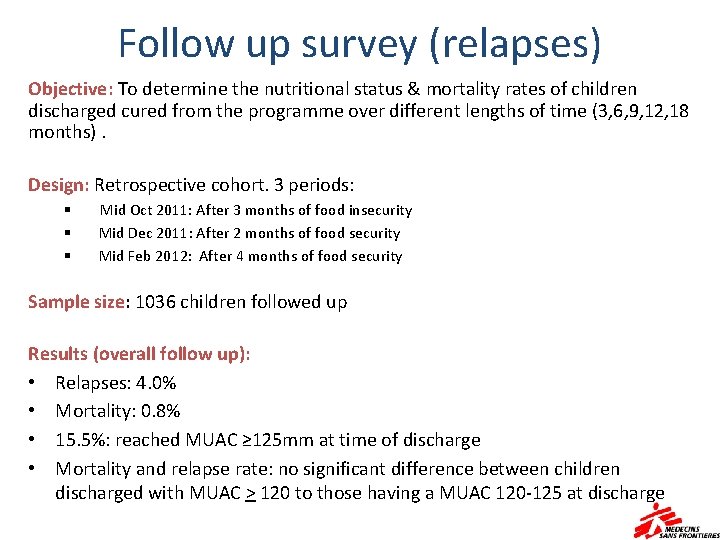
Follow up survey (relapses) Objective: To determine the nutritional status & mortality rates of children discharged cured from the programme over different lengths of time (3, 6, 9, 12, 18 months). Design: Retrospective cohort. 3 periods: § § § Mid Oct 2011: After 3 months of food insecurity Mid Dec 2011: After 2 months of food security Mid Feb 2012: After 4 months of food security Sample size: 1036 children followed up Results (overall follow up): • Relapses: 4. 0% • Mortality: 0. 8% • 15. 5%: reached MUAC ≥ 125 mm at time of discharge • Mortality and relapse rate: no significant difference between children discharged with MUAC > 120 to those having a MUAC 120 -125 at discharge
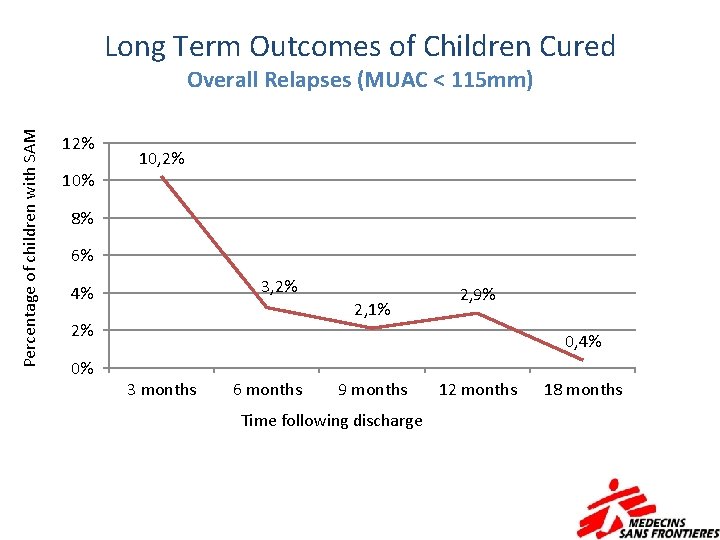
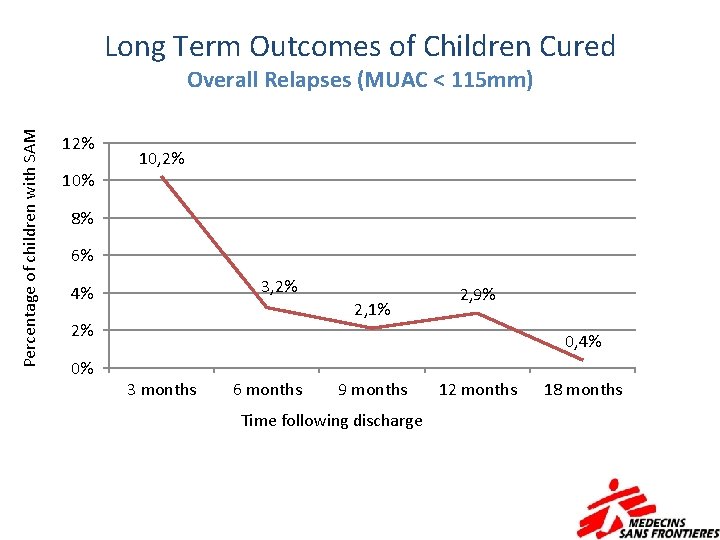
Long Term Outcomes of Children Cured Percentage of children with SAM Overall Relapses (MUAC < 115 mm) 12% 10, 2% 10% 8% 6% 3, 2% 4% 2, 1% 2% 0% 2, 9% 0, 4% 3 months 6 months 9 months Time following discharge 12 months 18 months
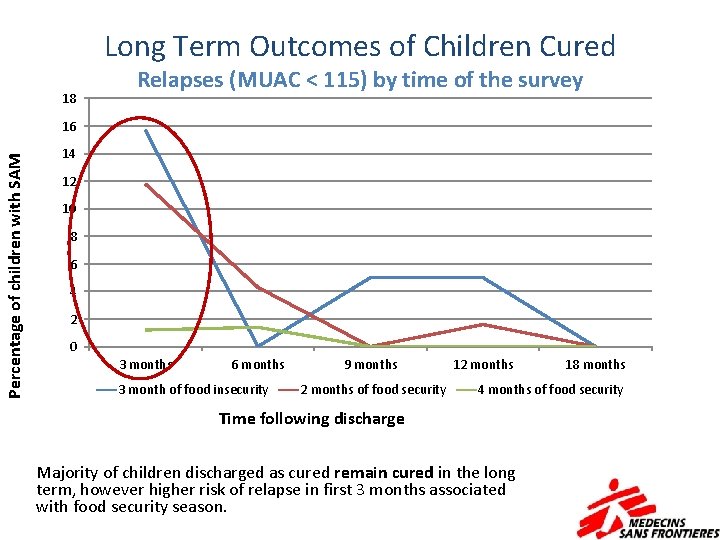
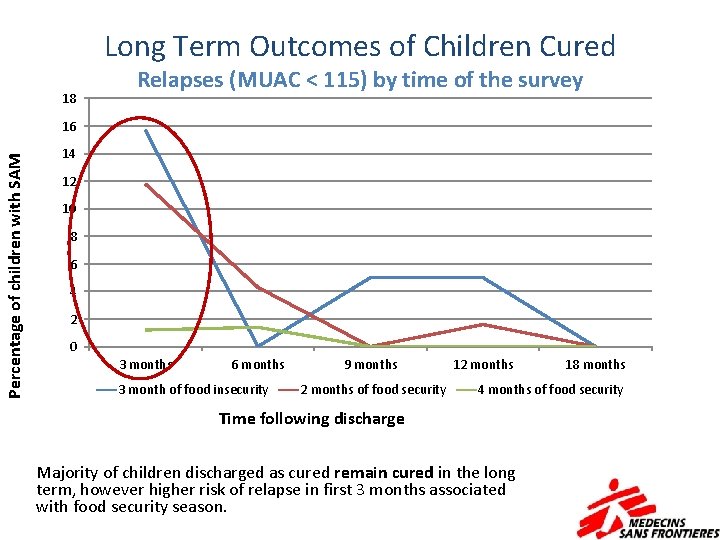
Long Term Outcomes of Children Cured 18 Relapses (MUAC < 115) by time of the survey Percentage of children with SAM 16 14 12 10 8 6 4 2 0 3 months 6 months 3 month of food insecurity 9 months 2 months of food security 12 months 18 months 4 months of food security Time following discharge Majority of children discharged as cured remain cured in the long term, however higher risk of relapse in first 3 months associated with food security season.
Risk factors for relapse and mortality in cured children For relapse: • W/H < -3 SD • Not using Anganwadi services • Low standard of living score • Longer LOS in programme • Season None associated with mortality
Conclusions • When analysing nutrition status at discharge, MUAC≥ 120 mm discharge demonstrated acceptable programme characteristics. • Relapse rates appeared significantly higher in children discharged with WHZ<-3 SD but absolute numbers were very small (2. 0%, 21/1036), not reflected in mortality (0%) and represented an older admission population. • When discharge is done during food insecurity period important follow up. • Current MUAC > 120 mm discharge criteria results in a long LOS for children with low MUAC and for children < 65 cm (> 6 months): self recovery perception-defaulting. Need to readjust criteria for children < 65 cm.