Mrs KFG 83 yo woman Lives alone Presents




- Slides: 15

Mrs. KFG, 83 yo woman • Lives alone • Presents with several weeks B/L LL oedema and redness • Background of: – Heart failure 2° to IHD and MR – Myelodysplastic syndrome – Asthma/COPD – CKD – Significant PVD with chronic LL ulcers – Multiple other comorbidities
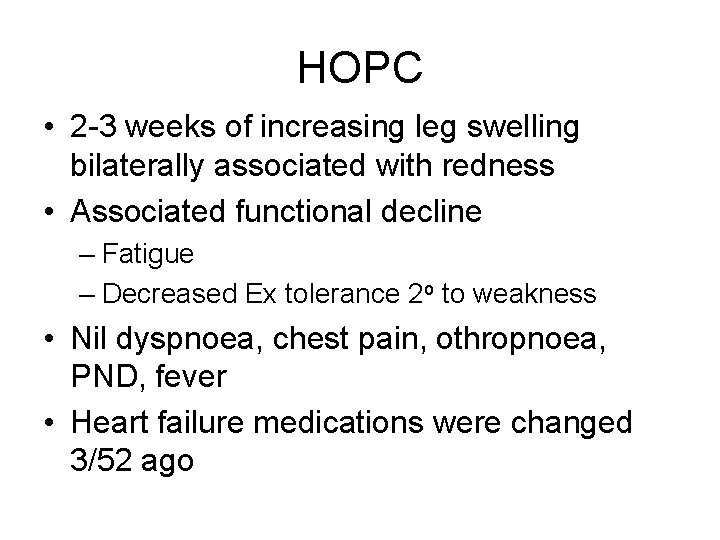
HOPC • 2 -3 weeks of increasing leg swelling bilaterally associated with redness • Associated functional decline – Fatigue – Decreased Ex tolerance 2 o to weakness • Nil dyspnoea, chest pain, othropnoea, PND, fever • Heart failure medications were changed 3/52 ago
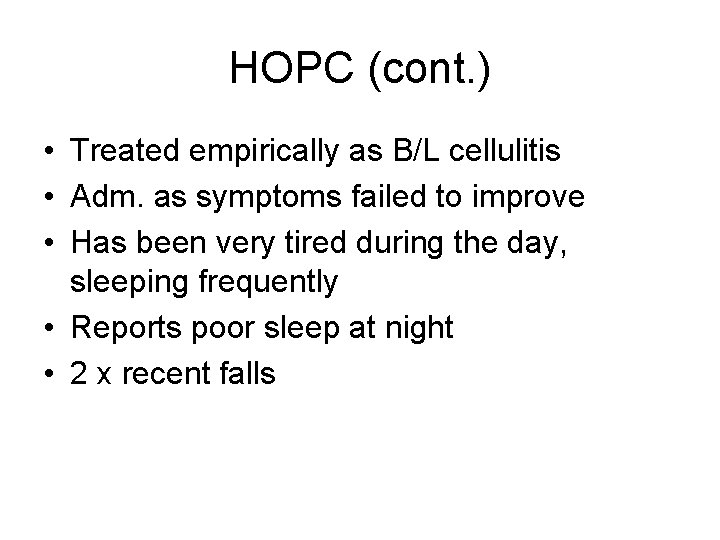
HOPC (cont. ) • Treated empirically as B/L cellulitis • Adm. as symptoms failed to improve • Has been very tired during the day, sleeping frequently • Reports poor sleep at night • 2 x recent falls
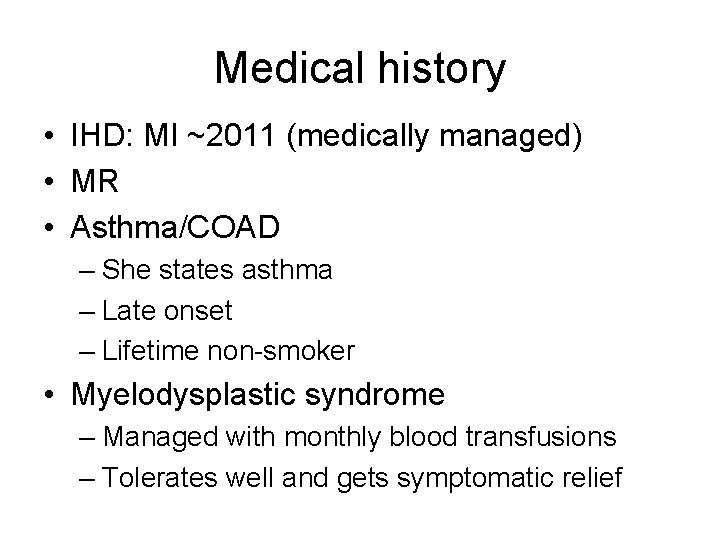
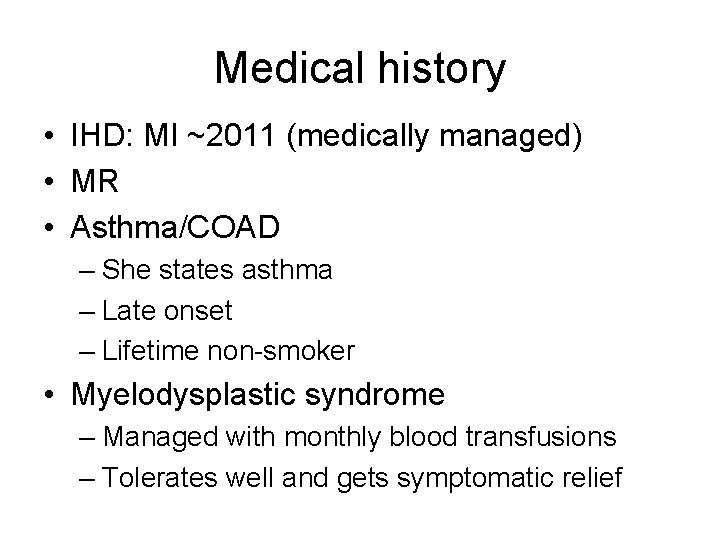
Medical history • IHD: MI ~2011 (medically managed) • MR • Asthma/COAD – She states asthma – Late onset – Lifetime non-smoker • Myelodysplastic syndrome – Managed with monthly blood transfusions – Tolerates well and gets symptomatic relief
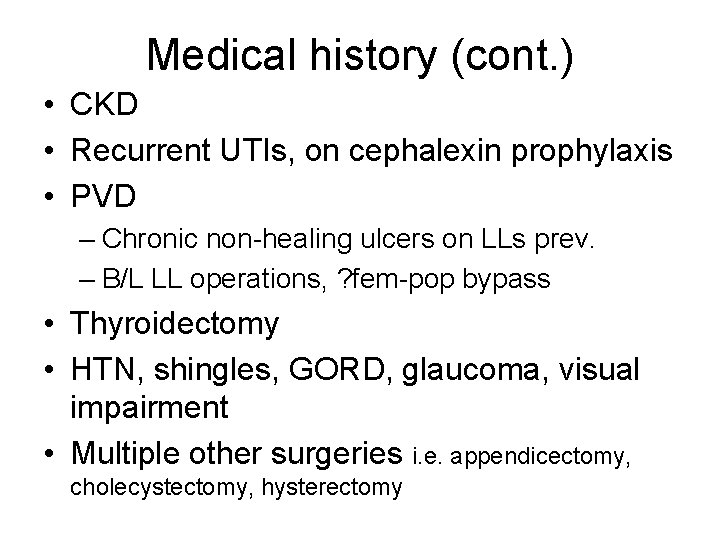
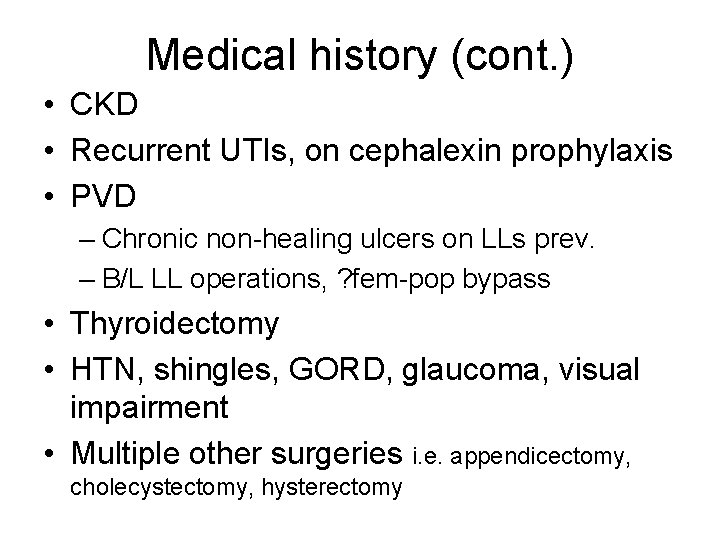
Medical history (cont. ) • CKD • Recurrent UTIs, on cephalexin prophylaxis • PVD – Chronic non-healing ulcers on LLs prev. – B/L LL operations, ? fem-pop bypass • Thyroidectomy • HTN, shingles, GORD, glaucoma, visual impairment • Multiple other surgeries i. e. appendicectomy, cholecystectomy, hysterectomy
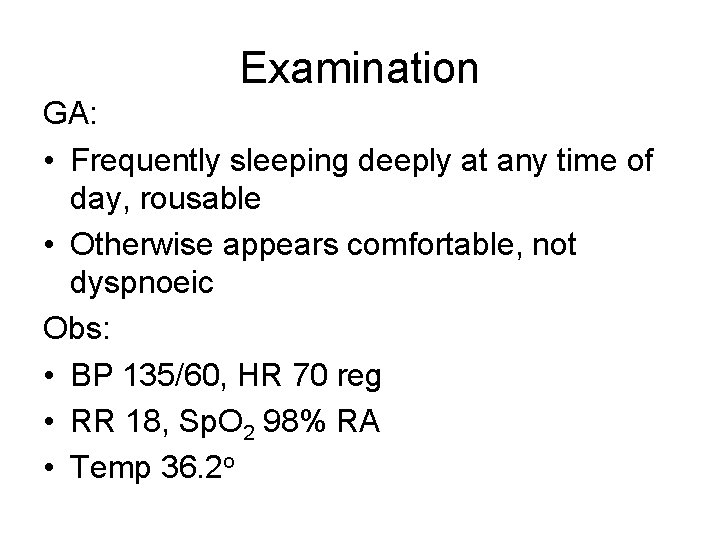
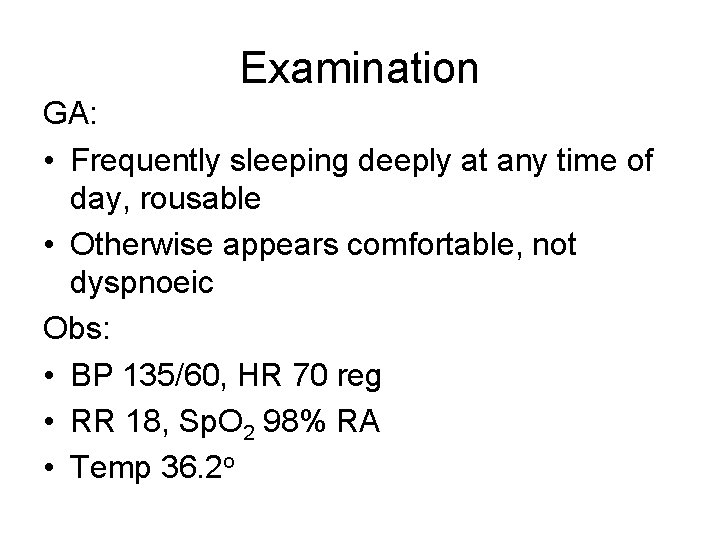
Examination GA: • Frequently sleeping deeply at any time of day, rousable • Otherwise appears comfortable, not dyspnoeic Obs: • BP 135/60, HR 70 reg • RR 18, Sp. O 2 98% RA • Temp 36. 2 o

Examination (cont. ) Cardio/resp: • JVP elevated 6 cm • Loud pansystolic murmur – Loudest at mitral region, radiating to axilla – Louder on expiration • Chest clear • Pitting oedema to knees B/L, with associated erythema • Dressing on L) leg
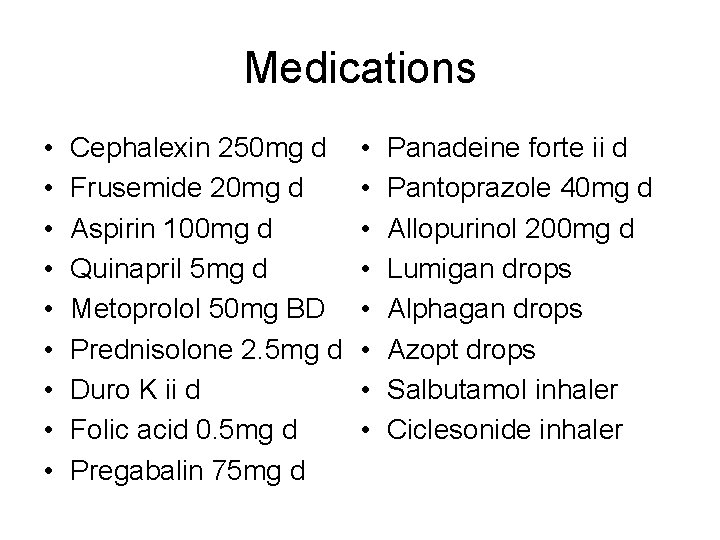
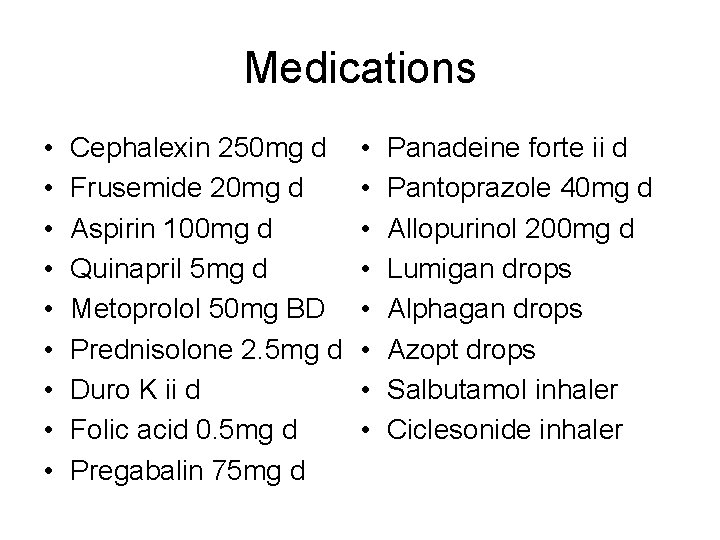
Medications • • • Cephalexin 250 mg d Frusemide 20 mg d Aspirin 100 mg d Quinapril 5 mg d Metoprolol 50 mg BD Prednisolone 2. 5 mg d Duro K ii d Folic acid 0. 5 mg d Pregabalin 75 mg d • • Panadeine forte ii d Pantoprazole 40 mg d Allopurinol 200 mg d Lumigan drops Alphagan drops Azopt drops Salbutamol inhaler Ciclesonide inhaler
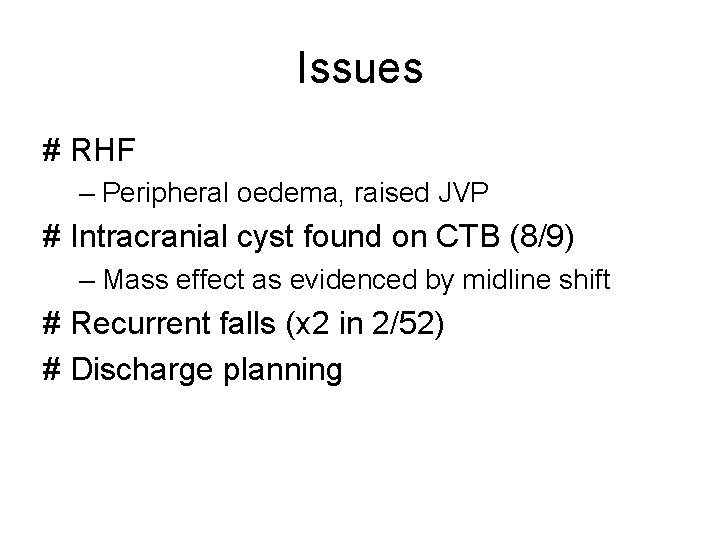
Issues # RHF – Peripheral oedema, raised JVP # Intracranial cyst found on CTB (8/9) – Mass effect as evidenced by midline shift # Recurrent falls (x 2 in 2/52) # Discharge planning

Social history • Lives alone, nearest family in Williamstown • Independent with personal care, shopping, cooking and most domestic chores • HH 1/14 to clean floors • Private services for gardening, maintenance • Goes out to lunch with friends at least once a week
Social history (cont. ) • Husband died 20 years ago (sudden cardiac death) • 2 daughters: – One in Williamstown who is very supportive, although has a young family – One in Byron Bay, their relationship is strained although they still talk • 2 living younger siblings live interstate • Does not drive • A lot of anxiety around new diagnosis of heart failure
Management • • • Diuresis and 1. 5 L fluid restriction Strict fluid balance and daily weighs Optimisation of heart failure medications Further Ix of intracranial cyst Physiotherapy, as below PMLOF Currently: – Assist x 1 to T/F – Supervision to ambulate with gait aid • Full allied health r/v, re: d/c needs
Myelodysplastic syndrome • Characterised by dyshaematopoesis – Dyserythropoesis Anaemia – Dysgranulocytopoesis Neutropenia – Dysmegakaryopoesis Thrombocytopenia • Classified broadly by the above + the percentage of blasts in peripheral film + bone marrow findings • >20% blasts = transformation to AML

Prognosis • Dependent on disease phenotype and patient’s age and comorbidities • May be as little as months, up to ten years or more • Manifestations of isolated anaemia with few blasts have the most favourable prognosis
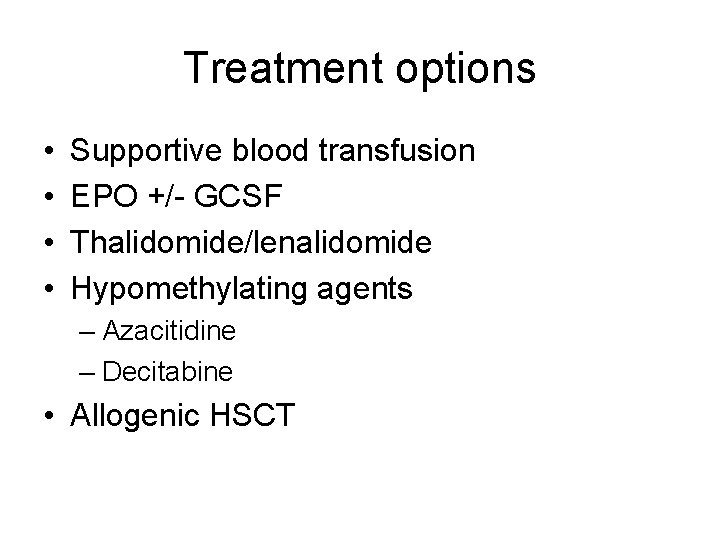
Treatment options • • Supportive blood transfusion EPO +/- GCSF Thalidomide/lenalidomide Hypomethylating agents – Azacitidine – Decitabine • Allogenic HSCT
 Building blocks in a sentence
Building blocks in a sentence Sensation vs perception
Sensation vs perception A woman travels in a lift. the mass of the woman is 50 kg
A woman travels in a lift. the mass of the woman is 50 kg The human ability to speedily recognize familiar objects
The human ability to speedily recognize familiar objects Once upon a time there lived a family
Once upon a time there lived a family They are mrs garcia and mrs castro
They are mrs garcia and mrs castro They are mrs garcia and mrs castro
They are mrs garcia and mrs castro Mrs. darling was ___________ of mrs. s.
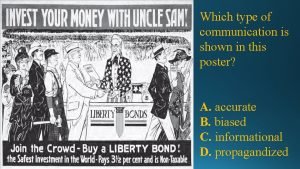
Mrs. darling was ___________ of mrs. s. Poster is a type of communication
Poster is a type of communication The text presents the house with
The text presents the house with Presents cause-effect relationship *
Presents cause-effect relationship * Where does “snowflake girl” help to deliver presents?
Where does “snowflake girl” help to deliver presents? 16 3 darwin presents his case answer key
16 3 darwin presents his case answer key This presents
This presents Prose writing that presents and explains ideas
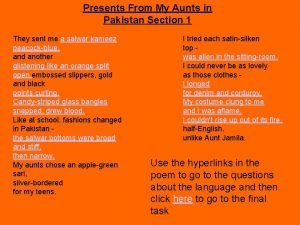
Prose writing that presents and explains ideas Presents from my aunts in pakistan poem
Presents from my aunts in pakistan poem