MRI in Breast Imaging Atiyah Yahya Ph D
MRI in Breast Imaging Atiyah Yahya, Ph. D. , FCCPM Department of Medical Physics, Cross Cancer Institute Department of Oncology, University of Alberta Edmonton, Canada
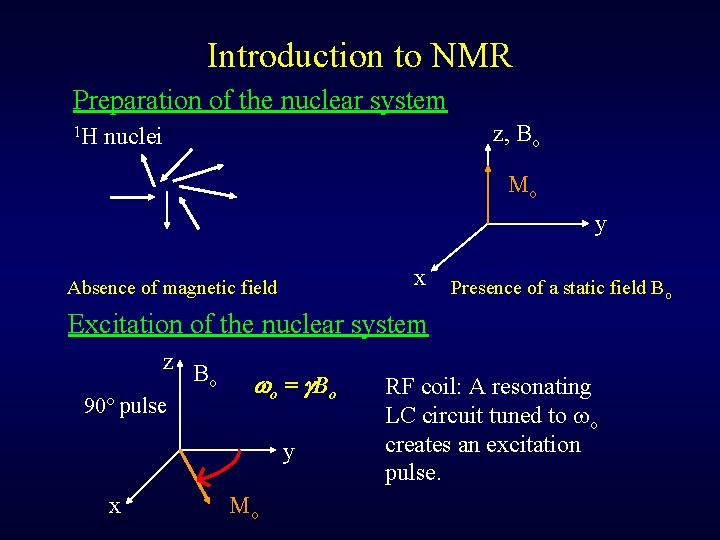
Introduction to NMR Preparation of the nuclear system 1 H z, Bo nuclei Mo y x Absence of magnetic field Presence of a static field Bo Excitation of the nuclear system z B o 90 pulse o = B o y x Mo RF coil: A resonating LC circuit tuned to o creates an excitation pulse.
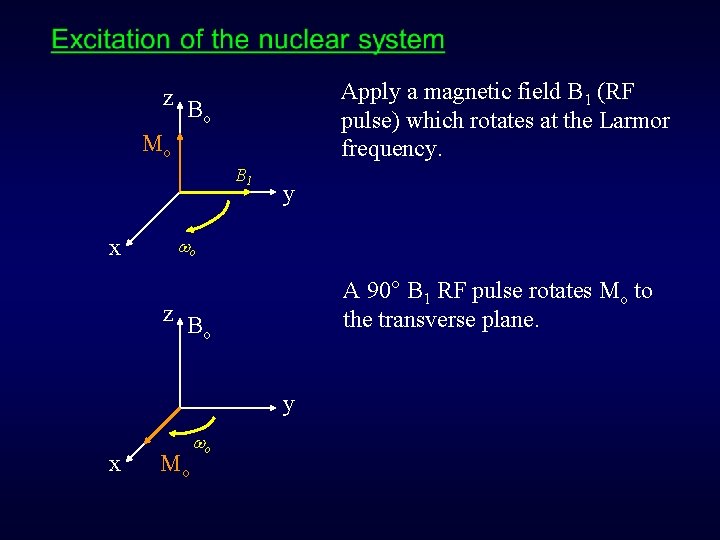
Apply a magnetic field B 1 (RF pulse) which rotates at the Larmor frequency. z B o Mo B 1 x y o A 90° B 1 RF pulse rotates Mo to the transverse plane. z B o y x Mo o
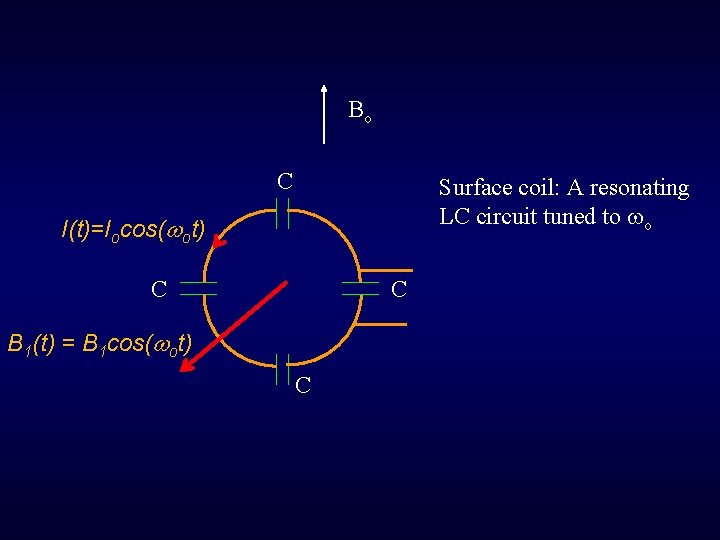
Bo C Surface coil: A resonating LC circuit tuned to o I(t)=Iocos( ot) C C B 1(t) = B 1 cos( ot) C
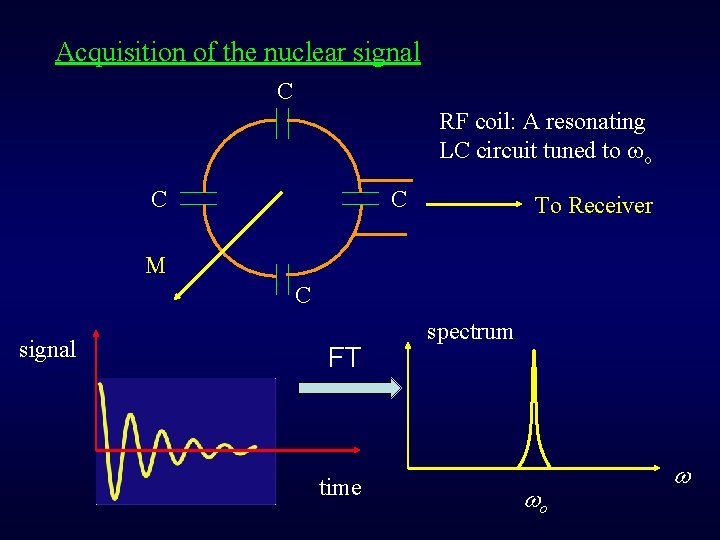
Acquisition of the nuclear signal C RF coil: A resonating LC circuit tuned to o C C To Receiver M C signal FT time spectrum o
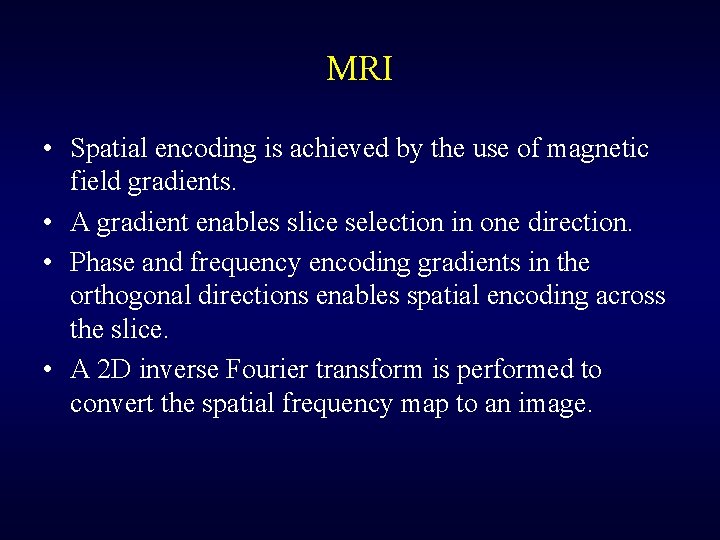
MRI • Spatial encoding is achieved by the use of magnetic field gradients. • A gradient enables slice selection in one direction. • Phase and frequency encoding gradients in the orthogonal directions enables spatial encoding across the slice. • A 2 D inverse Fourier transform is performed to convert the spatial frequency map to an image.

Three magnetic fields in MRI: • Main magnetic field, Bo (T) • Excitation RF field, B 1 ( T) • x, y, and z magnetic field gradients (m. T/m) Figure from: http: //image. slidesharecdn. com/mri 160403062142/95/mri-47638. jpg? cb=1459664619 Shim coils produce small currents that compensate for Bo inhomogeneities.
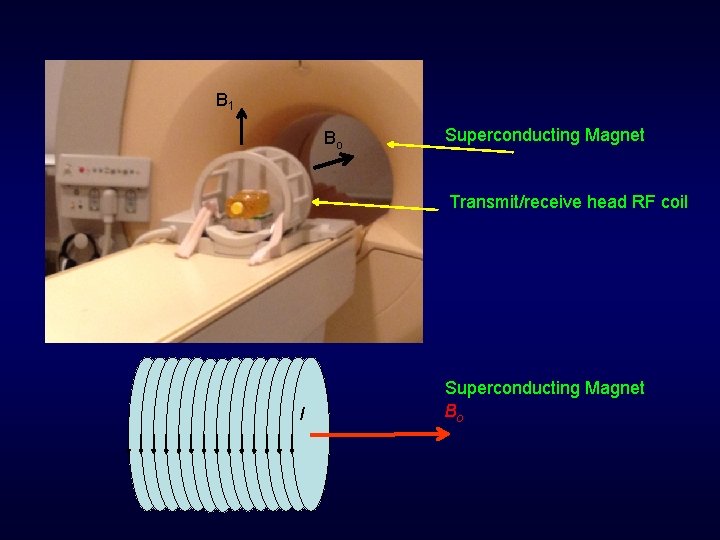
B 1 Bo Superconducting Magnet Transmit/receive head RF coil I Superconducting Magnet Bo
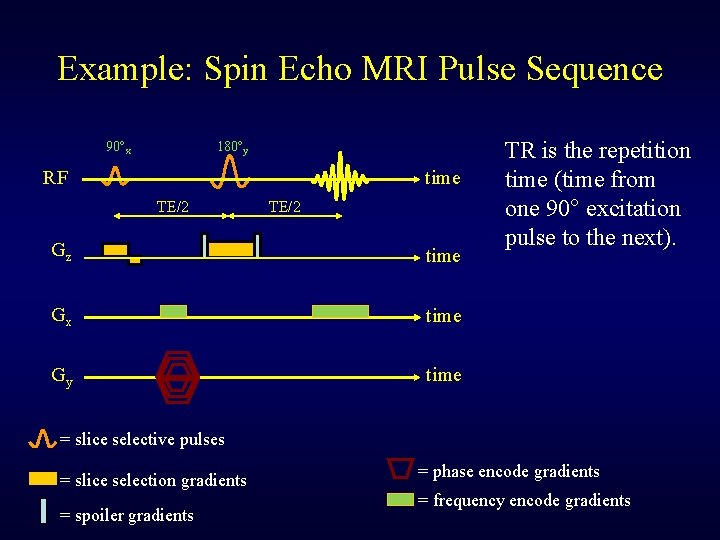
Example: Spin Echo MRI Pulse Sequence 90 x 180 y RF time TE/2 Gz time Gx time Gy time TR is the repetition time (time from one 90° excitation pulse to the next). = slice selective pulses = slice selection gradients = spoiler gradients = phase encode gradients = frequency encode gradients
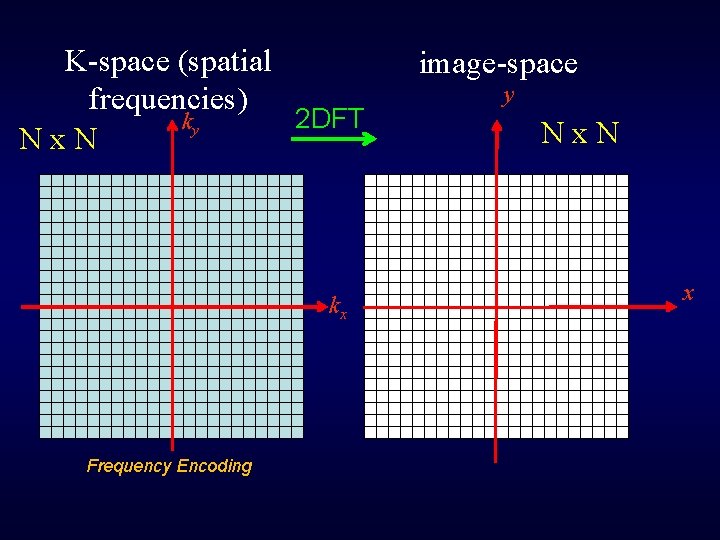
K-space (spatial frequencies) 2 DFT ky Nx. N kx kx Frequency Encoding image-space y Nx. N x
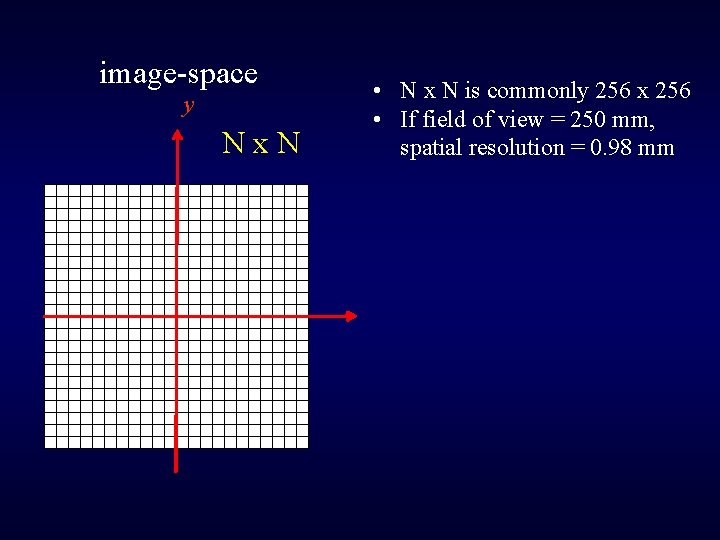
image-space y Nx. N kx • N x N is commonly 256 x 256 • If field of view = 250 mm, spatial resolution = 0. 98 mm
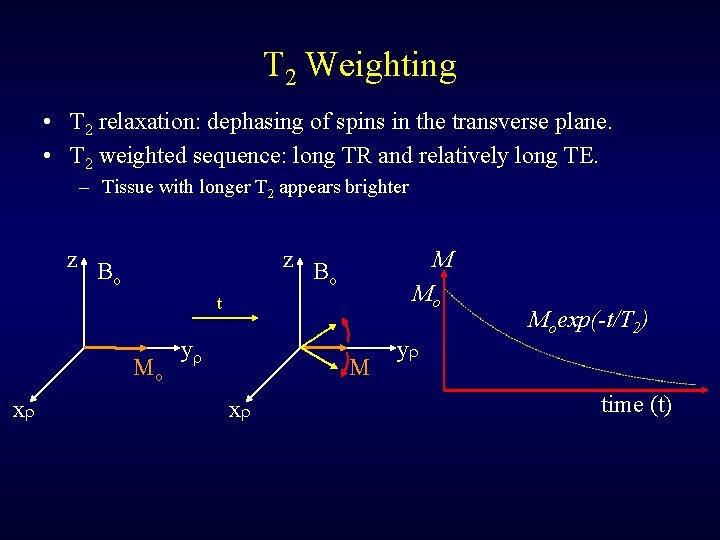
T 2 Weighting • T 2 relaxation: dephasing of spins in the transverse plane. • T 2 weighted sequence: long TR and relatively long TE. – Tissue with longer T 2 appears brighter z B o M Mo t Mo x y Moexp(-t/T 2) time (t)
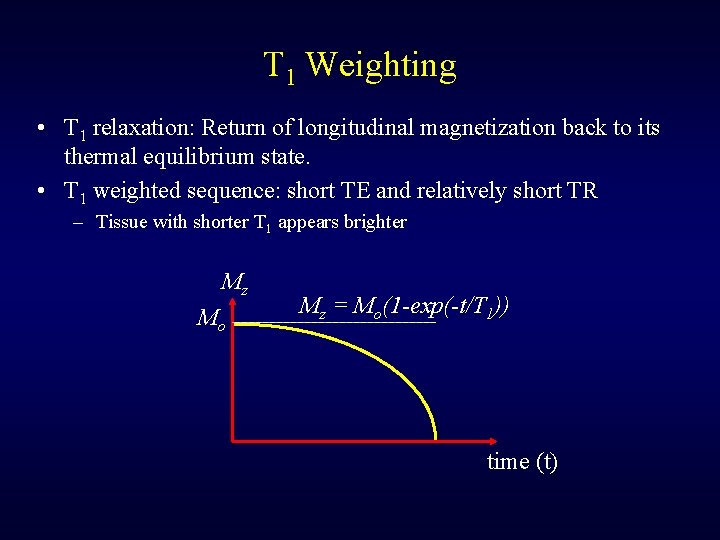
T 1 Weighting • T 1 relaxation: Return of longitudinal magnetization back to its thermal equilibrium state. • T 1 weighted sequence: short TE and relatively short TR – Tissue with shorter T 1 appears brighter Mz Mo Mz = Mo(1 -exp(-t/T 1)) time (t)
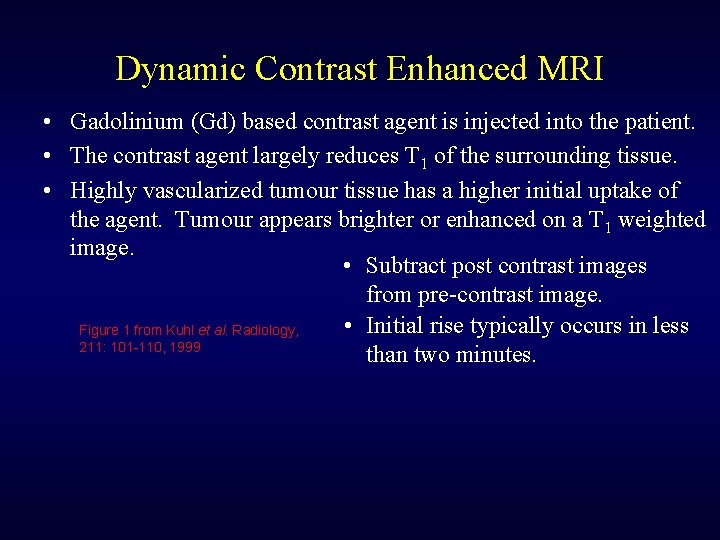
Dynamic Contrast Enhanced MRI • Gadolinium (Gd) based contrast agent is injected into the patient. • The contrast agent largely reduces T 1 of the surrounding tissue. • Highly vascularized tumour tissue has a higher initial uptake of the agent. Tumour appears brighter or enhanced on a T 1 weighted image. • Subtract post contrast images from pre-contrast image. • Initial rise typically occurs in less Figure 1 from Kuhl et al. Radiology, 211: 101 -110, 1999 than two minutes.
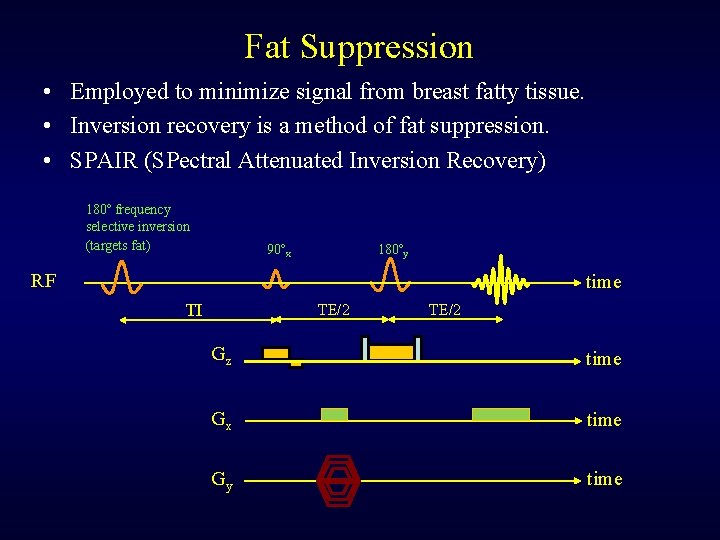
Fat Suppression • Employed to minimize signal from breast fatty tissue. • Inversion recovery is a method of fat suppression. • SPAIR (SPectral Attenuated Inversion Recovery) 180 frequency selective inversion (targets fat) 90 x 180 y RF time TI TE/2 Gz time Gx time Gy time
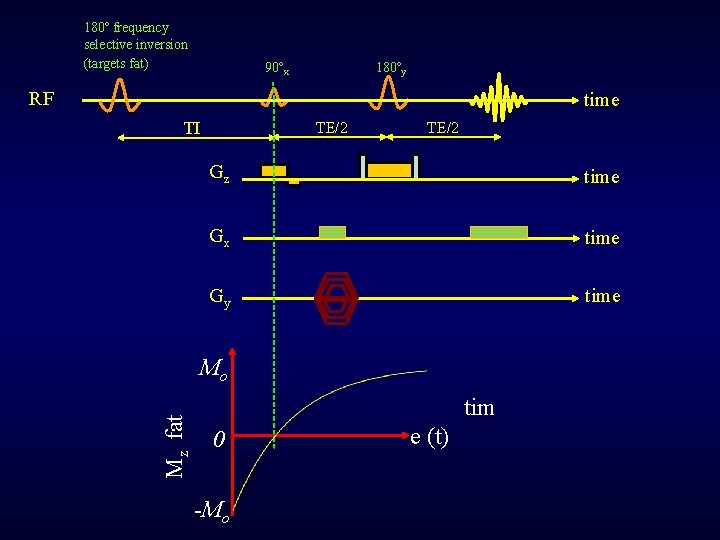
180 frequency selective inversion (targets fat) 90 x 180 y RF time TI TE/2 Gz time Gx time Gy time Mz fat Mo tim 0 -Mo e (t)

Invasive cancer T 2 weighted non-fat suppressed T 1 weighted, pre-contrast T 1 weighted, post-contrast fat suppressed Figure 1 from: http: //www. medscape. org/viewarticle/774824

T 2 weighted Figure 2 from: http: //www. medscape. org/viewarticle/774824 T 1 weighted, post-contrast
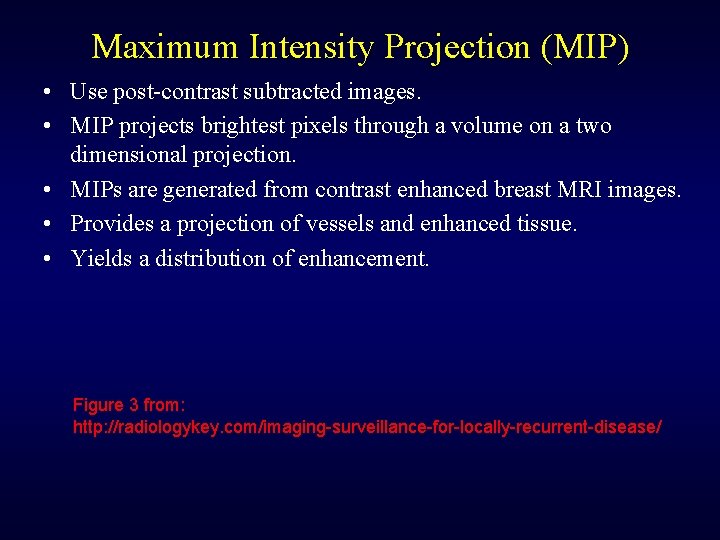
Maximum Intensity Projection (MIP) • Use post-contrast subtracted images. • MIP projects brightest pixels through a volume on a two dimensional projection. • MIPs are generated from contrast enhanced breast MRI images. • Provides a projection of vessels and enhanced tissue. • Yields a distribution of enhancement. Figure 3 from: http: //radiologykey. com/imaging-surveillance-for-locally-recurrent-disease/
MRI in Breast Screening • MRI is not recommended for general screening because it: – Results in more false positives (lower specificity) which leads to unnecessary biopsies. – Is expensive. – Is not able to detect cancers indicated by microcalcifications. – Scans during luteal phase of menstrual cycle are avoided due to background enhancement from higher levels of estrogen and progesterone 1. – Uses a contrast agent. – Longer acquisition times. 1. C. Klifa, J. Magn. Reson. Imaging, v. 33, p. 1229, 2011
• A number of guidelines 1 recommend MRI in addition to mammography annually for screening high risk women including those that: – Have an at least 20 – 25 % lifetime risk of developing breast cancer (e. g have a BRCA 1 and 2 gene mutation or family history). – Received chest radiation treatment between the ages of 10 -30 (for example to treat Hodgkin Lymphoma). Figure from: http: //breast-cancer. ca/images/mri-breast-highrisk-women-subtraction. jpg 1. A. Scaranelo, Canadian Medical Association Journal, v. 184, 2012
MRI in Diagnosis Extent of disease • MRI has shown to be useful for identifying – multicentric and multifocal breast cancer in some patients with invasive carcinoma and ductal carcinoma in situ (DCIS). – bilateral disease – the extent of invasive lobular carcinoma Lesion characterization • MRI may be used to characterize an indeterminate lesion (after assessing with mammography, ultrasound and physical inspection).
Metastatic disease with unknown primary • MRI may be able to identify a primary breast tumour when metastatic disease of unknown origin is present. MRI guided biopsy • MRI guided biopsy may be used when a lesion is only identifiable by MRI and can be used for fine needle aspiration, core needle, vacuum-assisted biopsy and pre-operative wire localization procedures.
Figures from: http: //www. soradtt. com/sub. php? content=news. Detail&id=146 http: //appliedradiology. com/articles/mr-guided-breast-interventionspearls-and-pitfalls-part-1
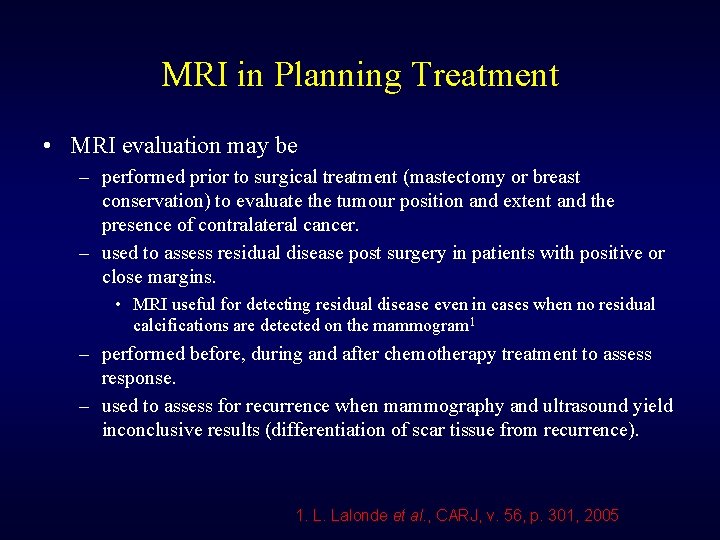
MRI in Planning Treatment • MRI evaluation may be – performed prior to surgical treatment (mastectomy or breast conservation) to evaluate the tumour position and extent and the presence of contralateral cancer. – used to assess residual disease post surgery in patients with positive or close margins. • MRI useful for detecting residual disease even in cases when no residual calcifications are detected on the mammogram 1 – performed before, during and after chemotherapy treatment to assess response. – used to assess for recurrence when mammography and ultrasound yield inconclusive results (differentiation of scar tissue from recurrence). 1. L. Lalonde et al. , CARJ, v. 56, p. 301, 2005
MRI for Assessing Breast Implant Ruptures • MRI provides high contrast between implants and soft tissue. • Can use T 2 weighted images or inversion recovery sequences where either the breast tissue or implant signal is saturated. Mz water Mo tim 0 -Mo e (t)
Left breast implant rupture Figure 2 from M. S. di Santolo et al. , Quantitative Imaging in Medicine and Surgery, v. 4, p. 462, 2014
Abbreviated MRI for Breast Screening 1 • Abbreviated protocol to reduce MRI acquisition time to improve the feasibility of MRI for breast screening. • Protocol includes one pre-contrast scan, one-post contrast scan and a MIP of the subtracted post-contrast images. • Acquisition time is approximately 3 minutes, the time for a radiologist to read the MIP is 3 seconds and the time to read the post contrast images is under 30 seconds. • Was found that the abbreviated protocol yielded results comparable to a full MRI screening protocol (about 40 minutes). 1. C. Kuhl et al. , Journal of Clinical Oncology, v. 32, p. 2304, 2014
Contraindications to Breast MRI • Implantable devices that are not MRI compatible (patients are screened) • Inability to lie prone • Severe obesity • Claustrophobia • Pregnancy (risk/benefit analysis) • Contraindications to gadolinium contrast agents
Contraindications to Gd Contrast Agents • Allergic reactions to Gd based contrast agents are rare ( 0. 15%)1 – Patients with a previous allergic reaction can be administered with a prophylaxis before another Gd contrast agent exposure. • Patients with advanced renal disease are at risk of developing nephrogenic systemic fibrosis (NSF) if administered with a Gd based contrast agent. – NSF is a fibrosis disease which causes skin thickening which can reduce mobility and joint motion. May affect internal organs. – Believed that slow clearance of Gd results in dissociation of Gd (toxic) from its chelate. – Some contrast agents (Omniscan, Magnevist and Opti. MARK) have been associated with more cases of NSF. 1 – Multi. Hance, Gadavist, Dotarem and Pro. Hance have been associated with fewer, if any, cases. 1 1. ACR Manual on Contrast Media, 2016
Screening for Renal Function Impairment • If a patient has a history of kidney disease, renal function should be assessed and a measure of the estimated glomerular filtration rate (e. GFR) should be obtained. • It is recommended to avoid administering Gd based contrast agents to patients with e. GFR < 30 m. L/min/1. 73 m 2. 1 1. ACR Manual on Contrast Media, 2016
Retention of Gd in the Brain • Retention of Gd in the brain has been found in patients with multiple (four or more) Gd contrast scans. 1, 2 • Not related to kidney function. 2 • Unknown if harmful. 2 • Found to occur with the use of linear chelate based Gd contrast agents. 3 1. Kanda et al. Radiology , v. 270, p. 834, 2014 2. http: //www. fda. gov/Safety/Med. Watch/Safety. Information/Safety. Alertsfor. Human. Medic al. Products/ucm 456012. htm 3. Kanda et al. Radiology, v. 275, p. 803, 2015

MRI Quality Control • ACR (American College of Radiology) has a breast MRI accreditation program with certain quality control requirements. • Standard ACR MRI tests. • Breast coil tests.
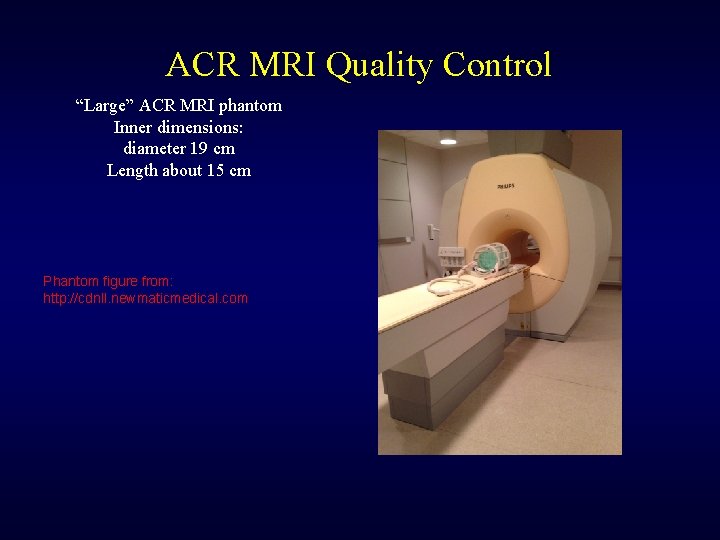
ACR MRI Quality Control “Large” ACR MRI phantom Inner dimensions: diameter 19 cm Length about 15 cm Phantom figure from: http: //cdnll. newmaticmedical. com
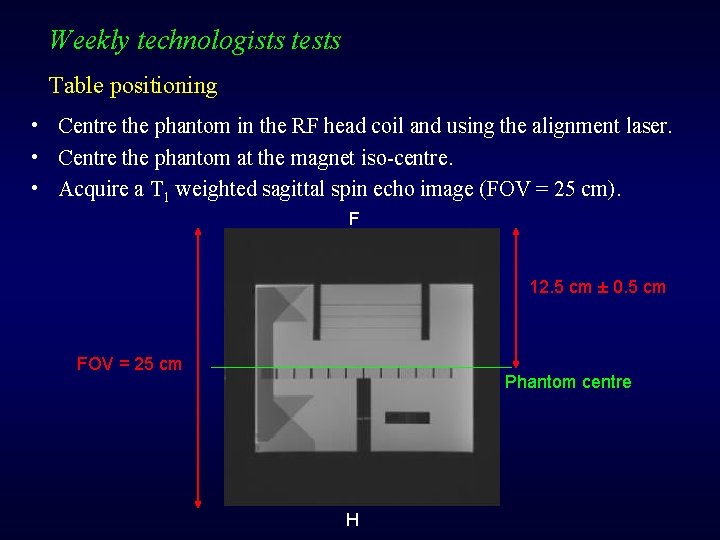
Weekly technologists tests Table positioning • Centre the phantom in the RF head coil and using the alignment laser. • Centre the phantom at the magnet iso-centre. • Acquire a T 1 weighted sagittal spin echo image (FOV = 25 cm). F 12. 5 cm ± 0. 5 cm FOV = 25 cm Phantom centre H
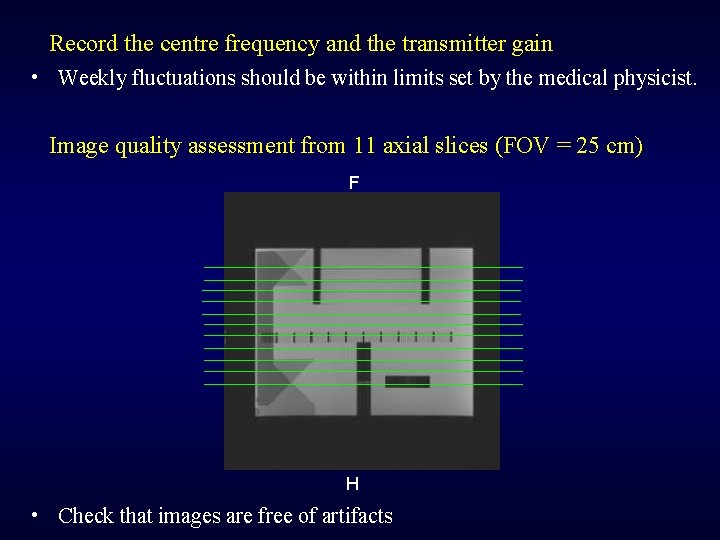
Record the centre frequency and the transmitter gain • Weekly fluctuations should be within limits set by the medical physicist. Image quality assessment from 11 axial slices (FOV = 25 cm) F H • Check that images are free of artifacts
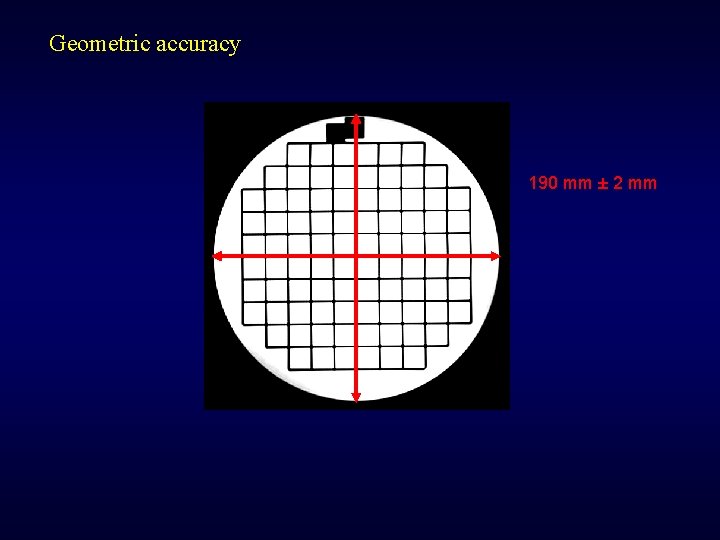
Geometric accuracy 190 mm ± 2 mm
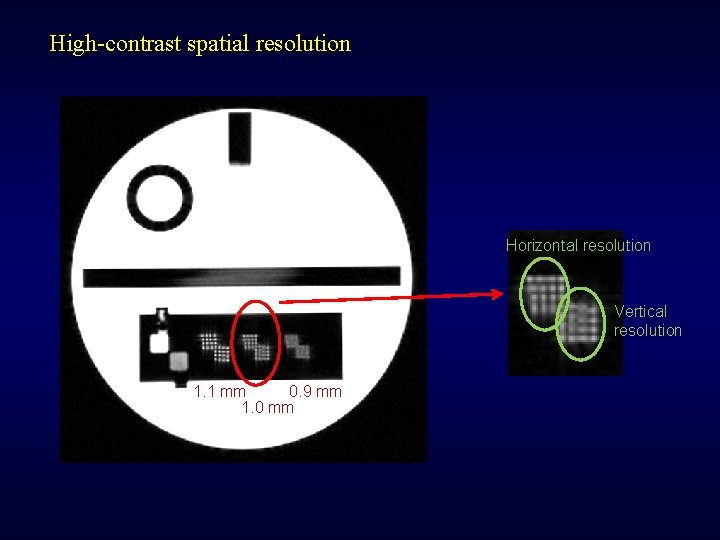
High-contrast spatial resolution Horizontal resolution Vertical resolution 1. 1 mm 0. 9 mm 1. 0 mm
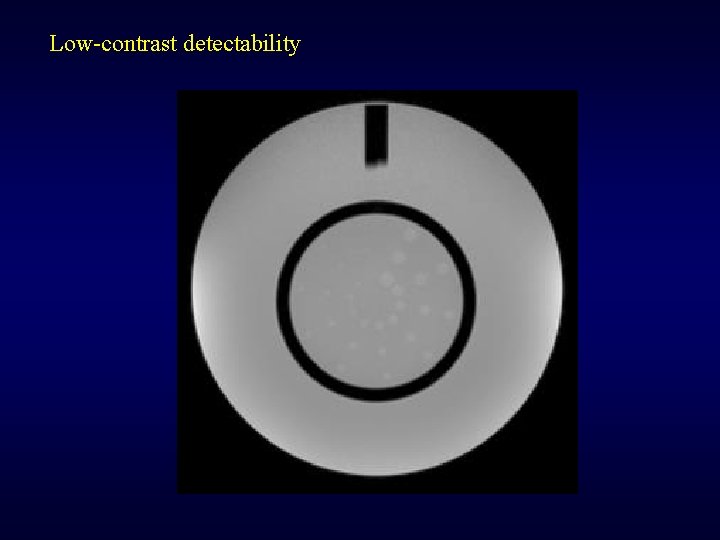
Low-contrast detectability
Visual checklist • Verify that the following are electrically and/or mechanically stable: – – – Patient bed Alignment laser Indicator lights RF room Signage monitors
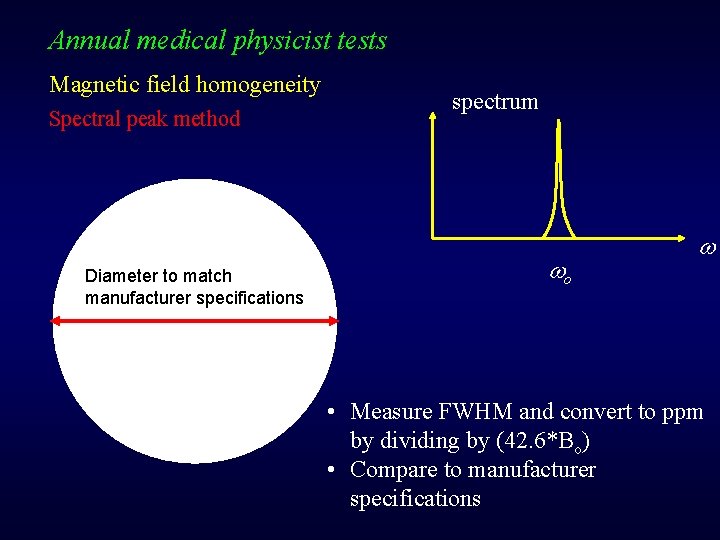
Annual medical physicist tests Magnetic field homogeneity Spectral peak method Diameter to match manufacturer specifications spectrum o • Measure FWHM and convert to ppm by dividing by (42. 6*Bo) • Compare to manufacturer specifications
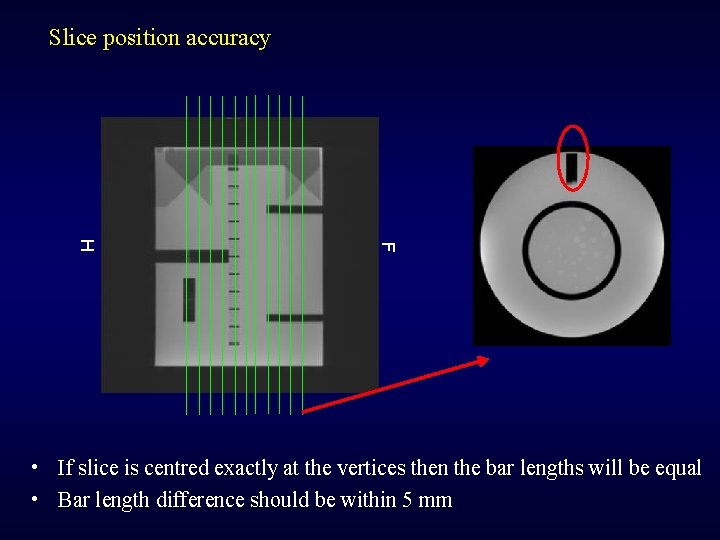
Slice position accuracy F H • If slice is centred exactly at the vertices then the bar lengths will be equal • Bar length difference should be within 5 mm
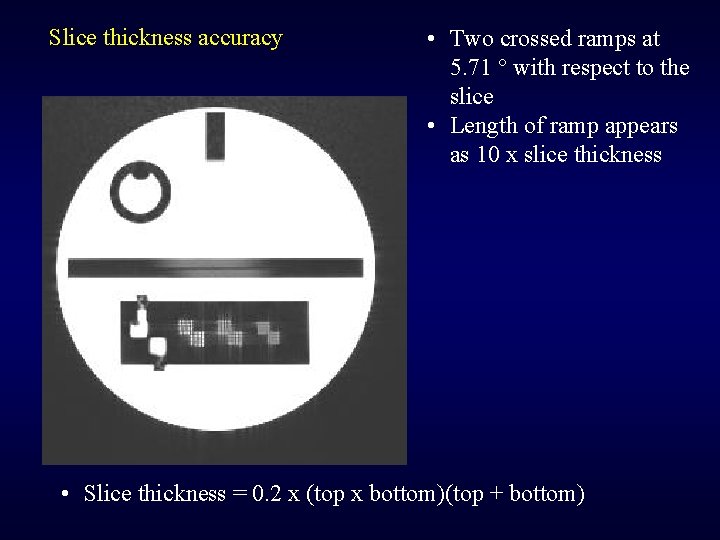
Slice thickness accuracy • Two crossed ramps at 5. 71 ° with respect to the slice • Length of ramp appears as 10 x slice thickness • Slice thickness = 0. 2 x (top x bottom)(top + bottom)
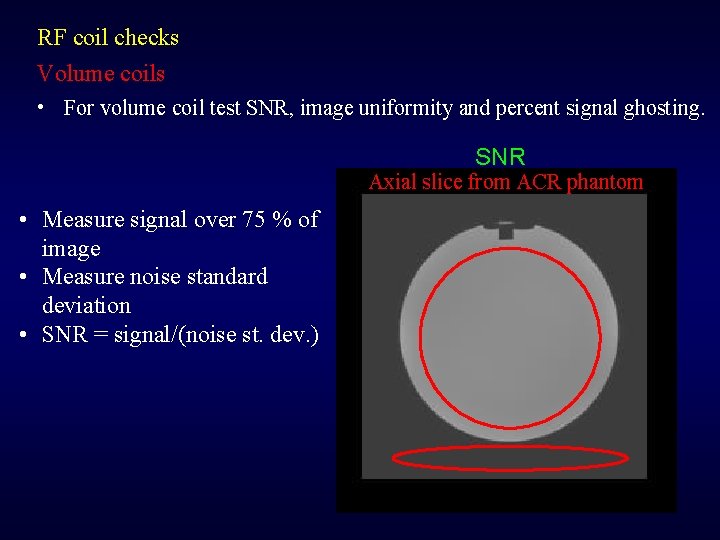
RF coil checks Volume coils • For volume coil test SNR, image uniformity and percent signal ghosting. SNR Axial slice from ACR phantom • Measure signal over 75 % of image • Measure noise standard deviation • SNR = signal/(noise st. dev. )
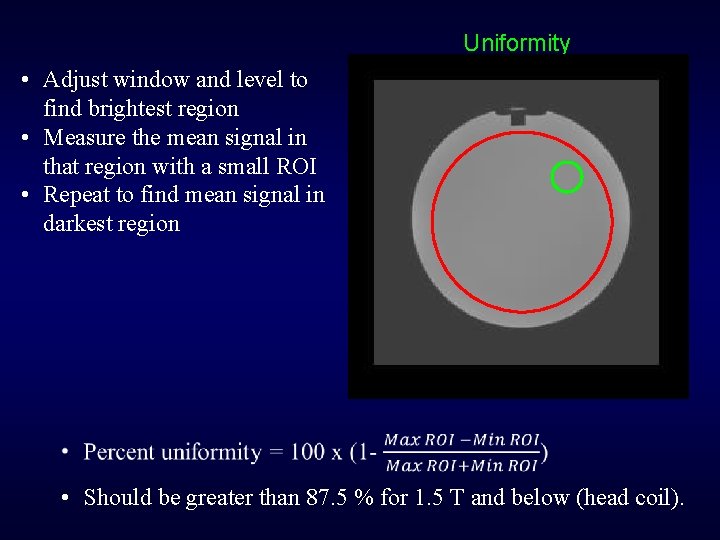
Uniformity • Adjust window and level to find brightest region • Measure the mean signal in that region with a small ROI • Repeat to find mean signal in darkest region • Should be greater than 87. 5 % for 1. 5 T and below (head coil).
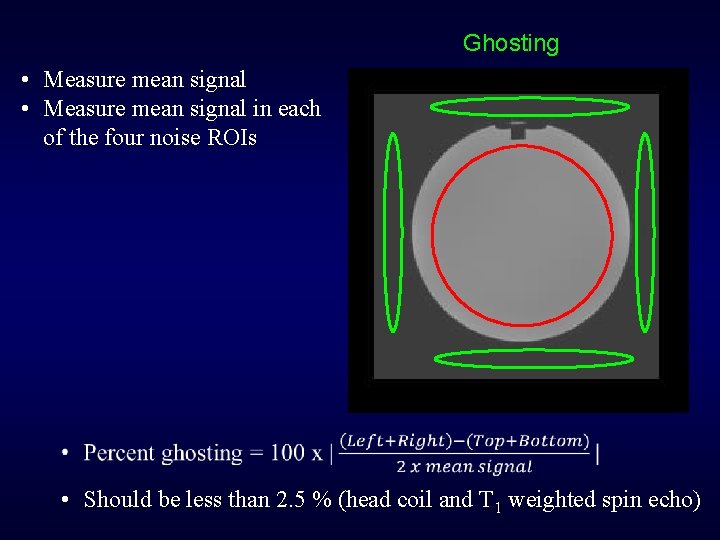
Ghosting • Measure mean signal in each of the four noise ROIs • Should be less than 2. 5 % (head coil and T 1 weighted spin echo)
Breast coil • Consist of multiple elements each with its own RF channel. • A 2 -L bottle filled with 10 m. M Cu. SO 4 can be inserted in each coil side. • “Small” ACR phantom can also be used.
• Breast coil testing should verify that all coil elements are functioning, that reasonable uniform images are obtained and that signal from the left and right breasts are comparable. - Measure SNR from all elements collectively and if possible from each individual element. http: //www. acraccreditation. org/Modalities/ Breast-MRI
Concluding Remarks • • • Overview of MRI Techniques used for breast MRI Role of MRI in breast screening, diagnosis and treatment Contraindications to MRI Safety concerns associated with gadolinium based contrast agents MRI quality control Questions?
- Slides: 49