MRCGP The Clinical Skills Assessment Purpose of the




- Slides: 36

MRCGP The Clinical Skills Assessment
Purpose of the CSA ‘An assessment of a doctor’s ability to integrate and apply appropriate clinical, professional, communication and practical skills in general practice’ The aim of the CSA is to test a doctor’s ability to gather information and apply learned understanding of disease processes and person-centred care appropriately in a standardised context, make evidence-based decisions, and communicate effectively with patients and colleagues. Being able to integrate these skills effectively is a key element of this assessment.
CSA: Marking Cases Each case has marking schedule consisting of 3 domains Data Gathering, Technical and Clinical Assessment skills Clinical Management skills Interpersonal skills Each domain carries equal marks
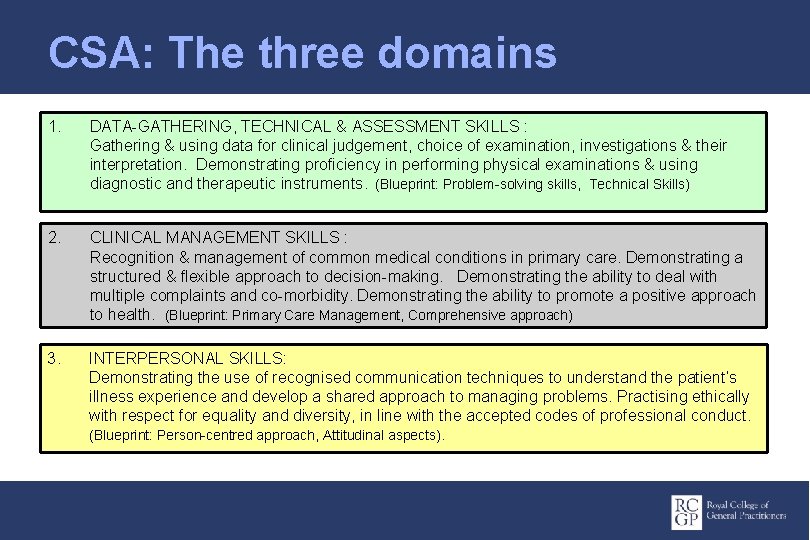
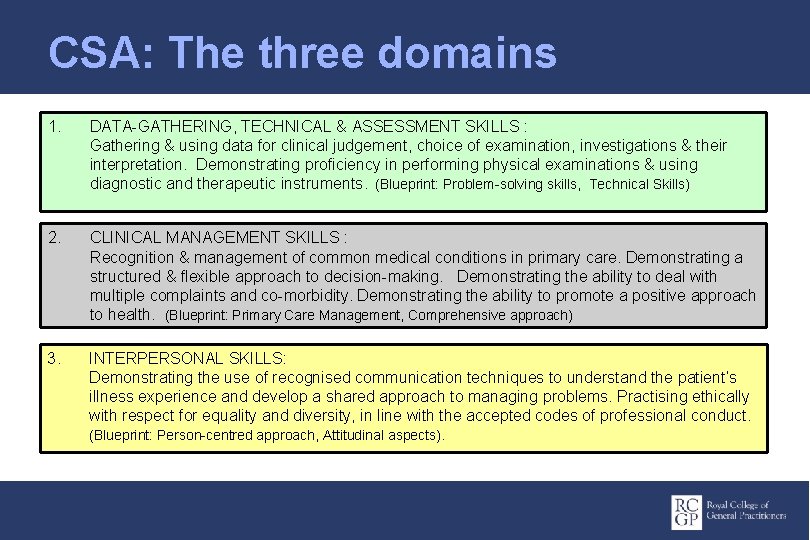
CSA: The three domains 1. DATA-GATHERING, TECHNICAL & ASSESSMENT SKILLS : Gathering & using data for clinical judgement, choice of examination, investigations & their interpretation. Demonstrating proficiency in performing physical examinations & using diagnostic and therapeutic instruments. (Blueprint: Problem-solving skills, Technical Skills) 2. CLINICAL MANAGEMENT SKILLS : Recognition & management of common medical conditions in primary care. Demonstrating a structured & flexible approach to decision-making. Demonstrating the ability to deal with multiple complaints and co-morbidity. Demonstrating the ability to promote a positive approach to health. (Blueprint: Primary Care Management, Comprehensive approach) 3. INTERPERSONAL SKILLS: Demonstrating the use of recognised communication techniques to understand the patient’s illness experience and develop a shared approach to managing problems. Practising ethically with respect for equality and diversity, in line with the accepted codes of professional conduct. (Blueprint: Person-centred approach, Attitudinal aspects).
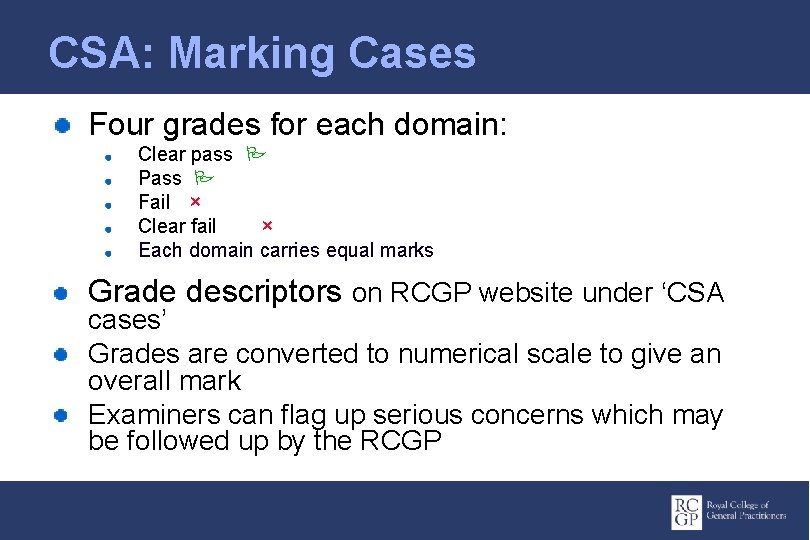
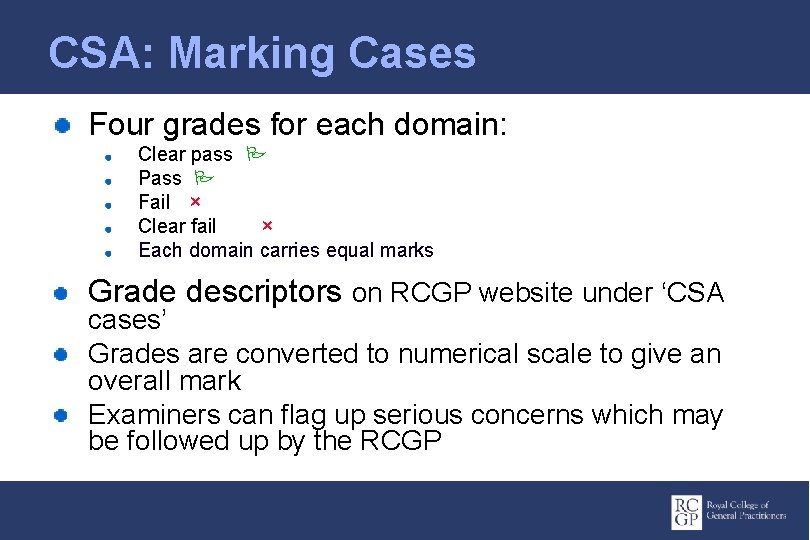
CSA: Marking Cases Four grades for each domain: Clear pass Pass Fail × Clear fail × Each domain carries equal marks Grade descriptors on RCGP website under ‘CSA cases’ Grades are converted to numerical scale to give an overall mark Examiners can flag up serious concerns which may be followed up by the RCGP
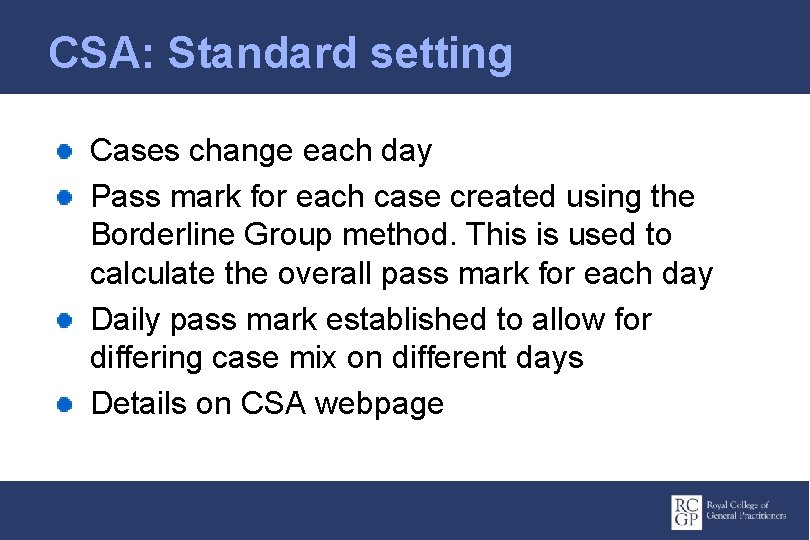
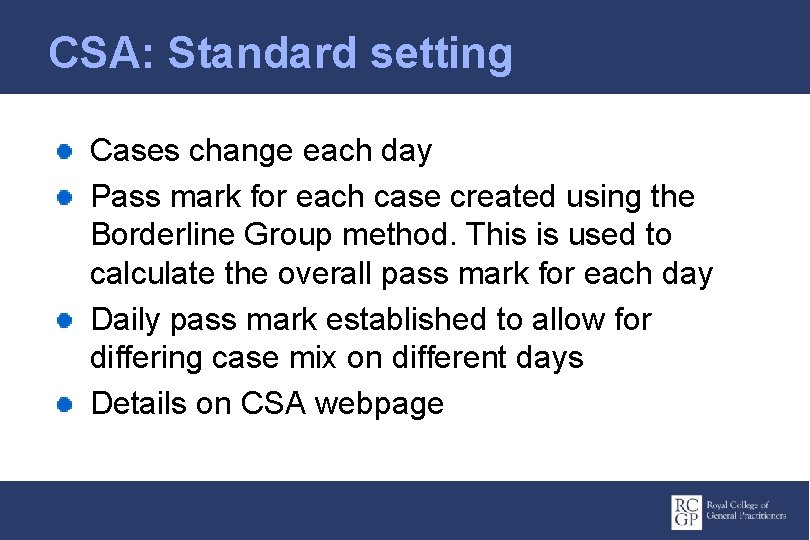
CSA: Standard setting Cases change each day Pass mark for each case created using the Borderline Group method. This is used to calculate the overall pass mark for each day Daily pass mark established to allow for differing case mix on different days Details on CSA webpage
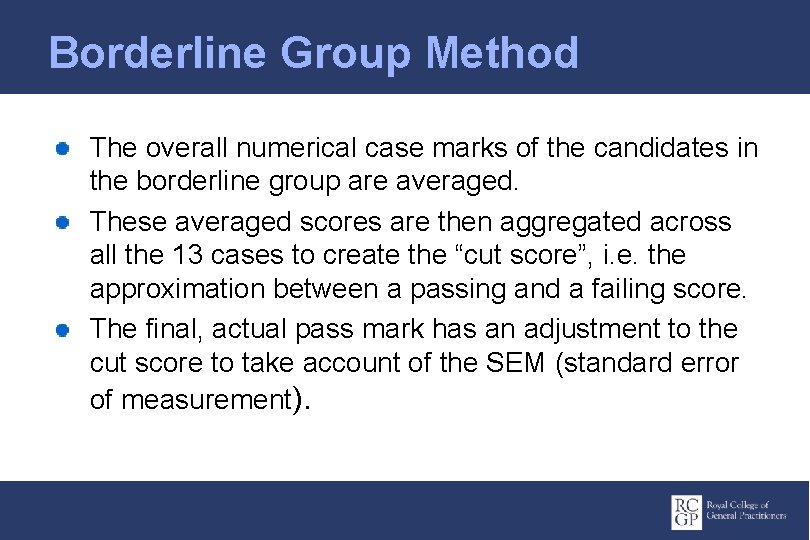
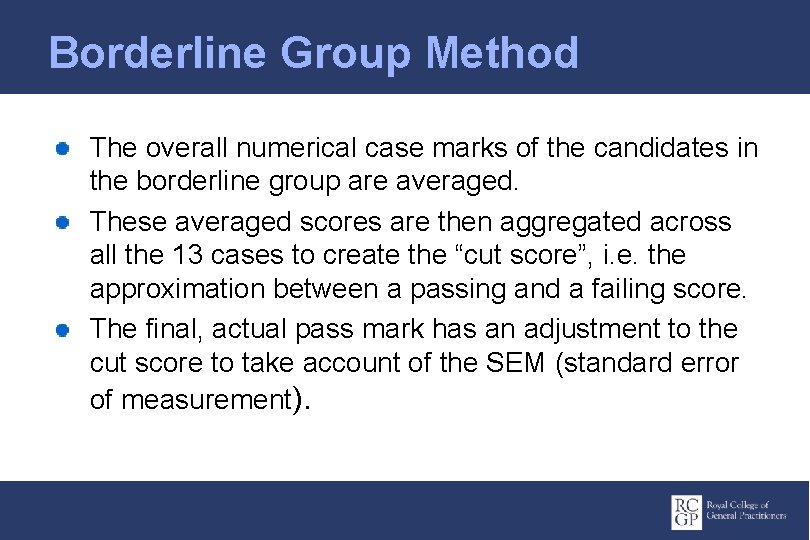
Borderline Group Method The overall numerical case marks of the candidates in the borderline group are averaged. These averaged scores are then aggregated across all the 13 cases to create the “cut score”, i. e. the approximation between a passing and a failing score. The final, actual pass mark has an adjustment to the cut score to take account of the SEM (standard error of measurement).
CSA: Failing Candidates A candidate who has failed will find the feedback helpful in preparing again for the CSA The CSA may be attempted a maximum of four times
CSA: Further Resources RCGP website CSA webpage ‘Information for Candidates’ Directions to the centre Timekeeping and conduct Format, timing, marking of the assessment Equipment to bring ‘Introduction to the cases’ document Feedback How to use the suggestions for improvement Preparation Courses at CSA Assessment Centre
AB notes 13 x 10 minute cases, same room 10 mins to settle in – look at the notes of first 7 patients on i. PAD 2 min reading time between cases Can call role player back in within 10 min time slot No penalty for “thinking time” if needed 15 minute break after 7 th case
AB notes Increasing prescribing content – may need to write a prescription (pad provided) Timer on wall – counts up to 10 mins No marks awarded after buzzer i. PAD used by examiners and candidates (no internet though!) Confidentiality agreement on i. PAD Patient records/letters/clinical findings on i. PAD
AB notes Examiners must have recent hands on experience training registrars Same case all day – role players and examiners rehearse case Mostly in hours surgery consultations but also tel triage, home visits, OOH Casebank >700 cases Re-sitting candidates should not get same case
AB notes Emergency, acute or chronic conditions Preventative medicine Physical, psychological or social problems Common conditions or serious Consultations with health professionals Ethical dilemmas Complexity and co-morbidity Most have paeds case (>8 y or proxy) & elderly
AB notes Different ethnicities Different social classes 4 nation compliant Disabled – deaf, blind Cases reflect real-life GP Standard is of GPR towards end training 4 -5 cases will require clinical examination

AB notes - pitfalls Jumping to Dx – think differential Mechanistic consulting Inadequate clinical examination skills Looking for non-existent hidden agendas Rigid Dr centred consulting Time management No QOF here – no irrelevant health promotion
AB notes Monthly sittings Nov to May Limited numbers for each session Results published following week directly into e. Portfolio Feedback statements ticked but no free text feedback – not formative 4 attempts – exceptional 5 th sitting
AB notes – how trainers help Exposure wide variety cases Observed surgeries best prep – not selected Move towards 10 mins as soon as possible but develop consultation skills first Joint consultations – different styles Role-plays for scenarios that trainee is not likely to see Real training not courses
AB notes Mainly single issue If 2 -3 problems the issue will be agenda setting and prioritising not full clinical Mx Immediate emerg treatment eg ectopic preg or PE or MI Emotionally challenging – breaking bad news or complaints Can be review of patient seen by partner
AB notes Proxy paeds case eg enuresis or stammer Can teach role player to have tennis elbow or frozen shoulder but not AF! May be given a model eg breast lump, pelvic model May be given card with examination findings At least 2 cases will have major prescribing safety elements eg calculate paeds dose
AB notes If blind pt – ask them if can take their arm before you grab them! If deaf patient may need to write everything down In these cases the medical aspects will be straightforward as emphasis on inter-personal Engage with patient and carer No longer any interpreter cases
AB notes Telephone cases – issue often confidentiality eg daughter phoning about elderly parent Avoid unnecessary or unexplained touch
AB notes Told to bring BNF/paeds BNF Would be expected to look up dose methotrexate but know dose amoxicillin No electronic BNF Generic marking scheme but Intended Learning Outcomes for station
AB notes – at risk groups IMG pass rate 31 – 53% Males pass rate 63% (Females 87%) Those who take it too early The highly anxious Those with lower exam/selection scores The inappropriately confident
AB notes Commonest reason to fail is not developing an adequate clinical management plan in line with current best practice or not making adequate arrangements for follow up and safety netting True for both IMGs and UK graduates Don’t recognise the challenge eg ethical Don’t make appropriate diagnosis Doesn’t develop shared management plan
AB notes Understand impact – show interest in pt Approx 5 mins data gathering and 5 mins management Look for non verbal cues Non genuine empathy is very clear Candidates need to listen and react Still need explanation even if give leaflets!
AB notes Welcome important – stand up, make eye contact, introduce themselves Positive body language “Tell me more” will get the response “what do you want to know” Target questions – “Tell me more about how this has changed over the last 2 months since it started”

AB notes Open questions – psychosocial and ICE (sensible and sensitive and in context) Closed Q – symptoms, red flags, excluding serious illness Rarely hidden agenda Listen properly, don’t interrupt Share ideas and decisions Examine unless told not to
AB notes Why have they come today? Are there other issues? Do I need to examine physically or mentally? What is my diagnosis and does pt agree? What is Mx plan including follow up Have I explained Mx plan and does patient agree?
AB notes – cultural issues Dr/patient relationship different Difficulties with empathy or admit uncertainty Heirarchy of team relationships Dr knows best – like clear solutions & rules Hear feedback defensively Used to being rewarded for spouting theory
AB notes – supporting IMGs Early needs assessment Use consultation models in teaching Discuss pt and Dr expectations Address managing uncertainty Handling emotion and confrontation Ethical issues and team heirarchy Joint surgeries ++++++ Allow them to flourish
AB notes Start work at ST 1 Allow enough time to take more than once in ST 3 – but not too early…. Encourage them not to work only with others who are struggling Don’t need to be perfect – not a checklist Don’t have to pass every station
AB notes Always 3 points for each of the 3 domains in every station Can still get 3 points for a clear pass in a domain without doing everything calibrated by the examiners for that case Not about gold standard – what is expected as a newly qualified independent GP

CSA 2015/16 all attempts All HENE candidates: 69. 8% pass rate (National 2014/15 75. 8%) UK Graduate HENE: 87. 2% Non UK Graduate HENE: 52. 3% 2014/15 nationally 76. 2% candidates were UK graduates but 62. 3% in our region
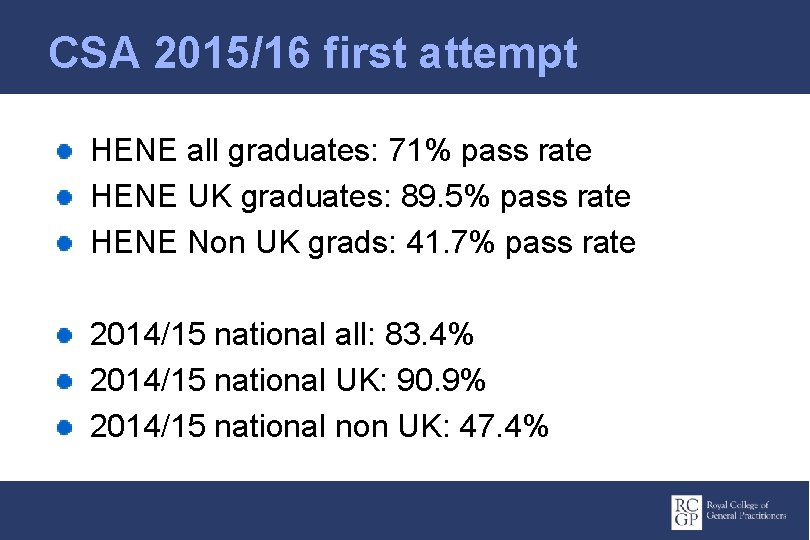
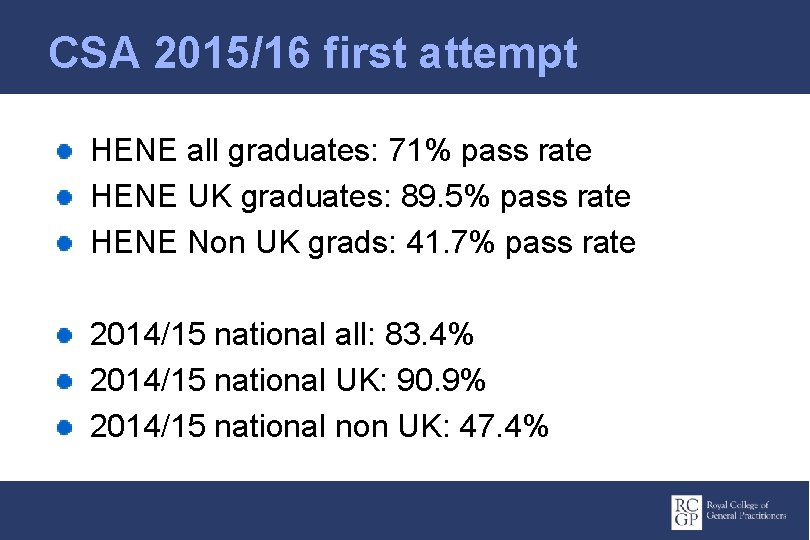
CSA 2015/16 first attempt HENE all graduates: 71% pass rate HENE UK graduates: 89. 5% pass rate HENE Non UK grads: 41. 7% pass rate 2014/15 national all: 83. 4% 2014/15 national UK: 90. 9% 2014/15 national non UK: 47. 4%
Cumulative pass rate Nationally after 3 attempts UK grad pass rate 98% IMG pass rate 68% 1 -5 trainees/yr will not complete training in our area at least partly due to exam failure so the vast majority pass even though we have a relatively high number in high risk groups
 Book akt exam
Book akt exam Akt exam review
Akt exam review Dr jeremy rogers
Dr jeremy rogers Clinical observation of motor and postural skills pdf
Clinical observation of motor and postural skills pdf Clinical skills definition
Clinical skills definition Clinical assessment
Clinical assessment Cas clinical assessment
Cas clinical assessment Direct methods of nutritional assessment
Direct methods of nutritional assessment Clinical assessment protocols
Clinical assessment protocols National clinical assessment service
National clinical assessment service Interpersonal skill adalah
Interpersonal skill adalah Skills are
Skills are Skills passport
Skills passport What is a sentence purpose
What is a sentence purpose General purpose specific purpose central idea
General purpose specific purpose central idea Autism encyclopedia curriculum
Autism encyclopedia curriculum Casey life skills curriculum
Casey life skills curriculum Casey life skills assessment scoring
Casey life skills assessment scoring Testing listening comprehension
Testing listening comprehension Alabama basic skills assessment
Alabama basic skills assessment Kindergarten foundational skills assessment
Kindergarten foundational skills assessment Physics math review
Physics math review Assessment skills
Assessment skills Purpose of health assessment
Purpose of health assessment Mood mse
Mood mse Assessment skills
Assessment skills Assessment skills
Assessment skills Assessment motor and process skills
Assessment motor and process skills Msa skills assessment
Msa skills assessment Scans competencies
Scans competencies Neurovascular assessment includes
Neurovascular assessment includes General principles of assessment
General principles of assessment Purpose of nursing assessment
Purpose of nursing assessment Purpose of skin assessment
Purpose of skin assessment What is summative evaluation
What is summative evaluation What is documentation portfolio
What is documentation portfolio Define dynamic assessment
Define dynamic assessment