mp MRI in Prostate cancer A Urologists Perspective


- Slides: 20
mp. MRI in Prostate cancer A Urologist’s Perspective Diagnosis Treatment Choice Surgical Planning Dr. Peter Heathcote, Adjunct Professor APCRC-Q QUT, Senior Urologist PAH and GPH
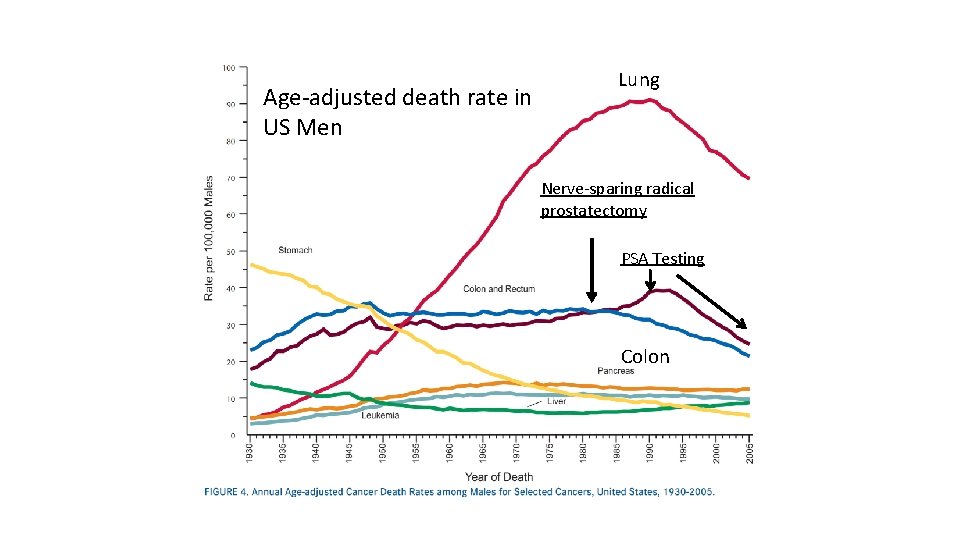
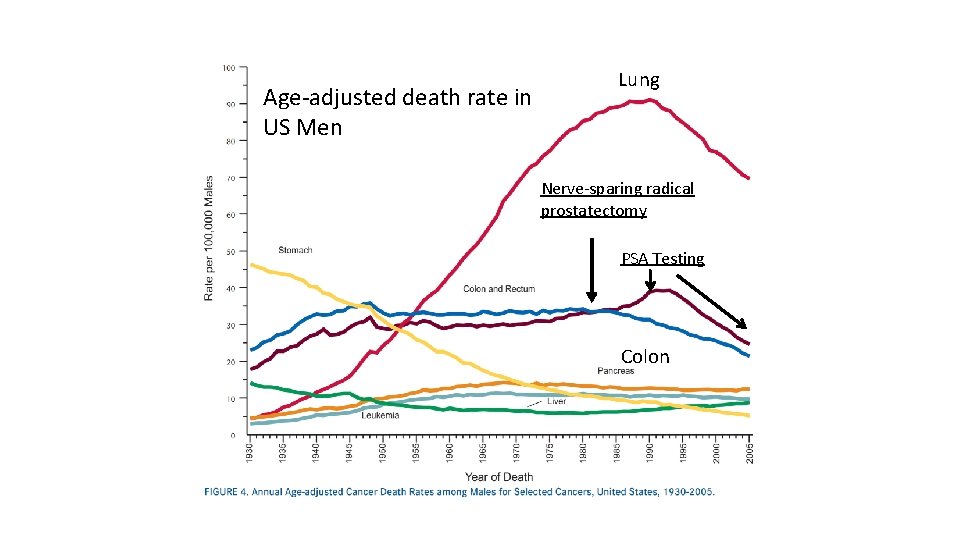
Age-adjusted death rate in US Men LL Lung Nerve-sparing radical prostatectomy PSA Testing Colon
Mortality results from the Göteborg randomised populationbased prostate-cancer screening trial Jonas Hugosson et al. Lancet Oncol 2010; 11: 725– 32 20, 000 patients randomised Median follow up 14 yrs ARR of death from Ca. P 0. 9% -> 0. 5% “This study shows that prostate cancer mortality was reduced almost by half over 14 years. However, the risk of overdiagnosis is substantial and the number needed to treat is at least as high as in breast-cancer screening programmes. ”
What is the problem? • Life time risk of being diagnosed with Ca. P is 17% • 10000 men/yr diagnosed in Australia • Life time risk of dying from prostate cancer is 3% • 3000 men /yr die in Australia SEER cancer statistics review 1975– 2004. Bethesda, MD: National Cancer Institute, 2007 (http: //seer. cancer. gov/csr/ 1975_2004).
This is the problem! The Goteberg study again* To prevent one prostate cancer death 293 men need to be screened 12 men need to be diagnosed 8 men need to be treated Over-diagnosis Over –treatment * Lancet Oncol 2010 11: 725 -32
What role mp. MRI? OVER-DIAGNOSIS ? Reduce number of biopsies. ? Reduce number of insignificant cancers diagnosed. BUT Is there a risk of missing significant cancers?
What role mp. MRI? • Over–treatment Can MRI facilitate greater use of Active Surveillance?
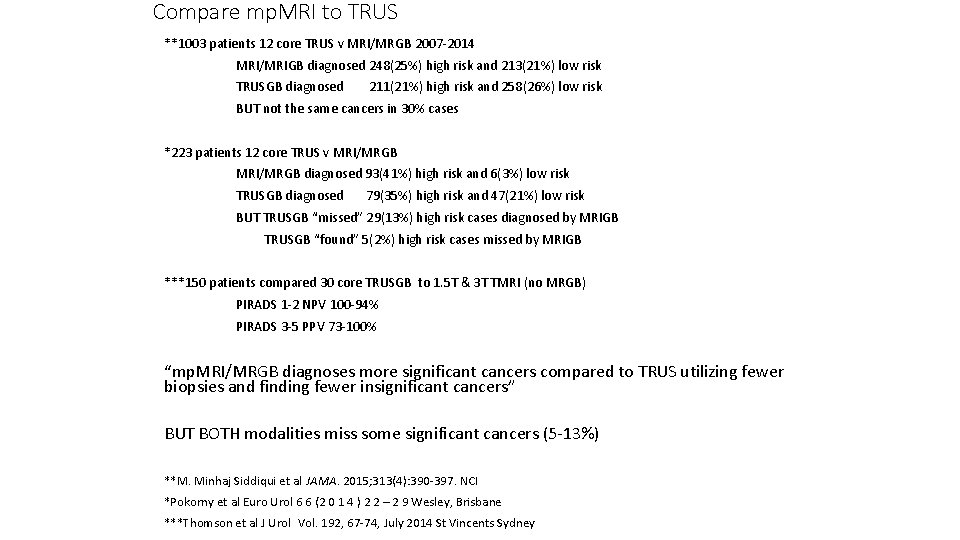
Compare mp. MRI to TRUS **1003 patients 12 core TRUS v MRI/MRGB 2007 -2014 MRI/MRIGB diagnosed 248(25%) high risk and 213(21%) low risk TRUSGB diagnosed 211(21%) high risk and 258(26%) low risk BUT not the same cancers in 30% cases *223 patients 12 core TRUS v MRI/MRGB diagnosed 93(41%) high risk and 6(3%) low risk TRUSGB diagnosed 79(35%) high risk and 47(21%) low risk BUT TRUSGB “missed” 29(13%) high risk cases diagnosed by MRIGB TRUSGB “found” 5(2%) high risk cases missed by MRIGB ***150 patients compared 30 core TRUSGB to 1. 5 T & 3 T TMRI (no MRGB) PIRADS 1 -2 NPV 100 -94% PIRADS 3 -5 PPV 73 -100% “mp. MRI/MRGB diagnoses more significant cancers compared to TRUS utilizing fewer biopsies and finding fewer insignificant cancers” BUT BOTH modalities miss some significant cancers (5 -13%) **M. Minhaj Siddiqui et al JAMA. 2015; 313(4): 390 -397. NCI *Pokorny et al Euro Urol 6 6 (2 0 1 4 ) 2 2 – 2 9 Wesley, Brisbane ***Thomson et al J Urol Vol. 192, 67 -74, July 2014 St Vincents Sydney
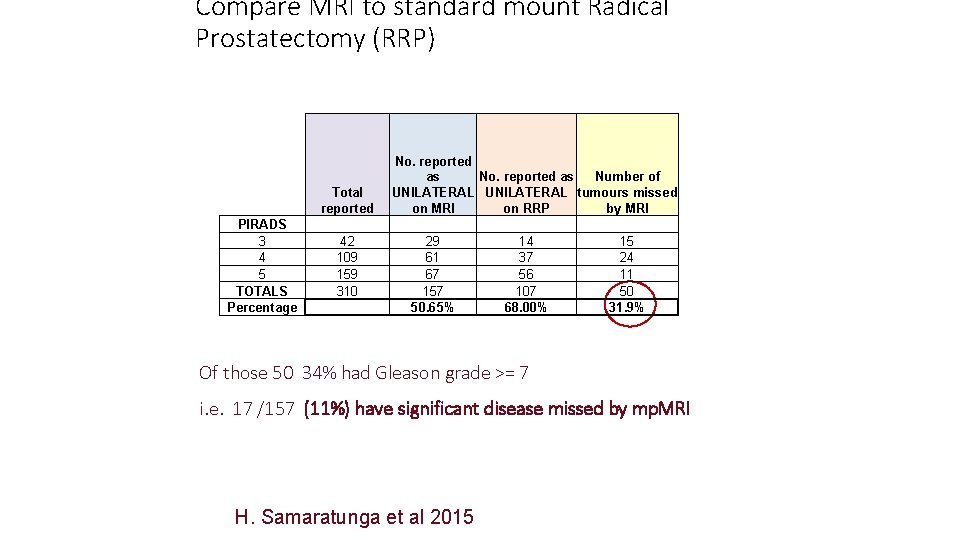
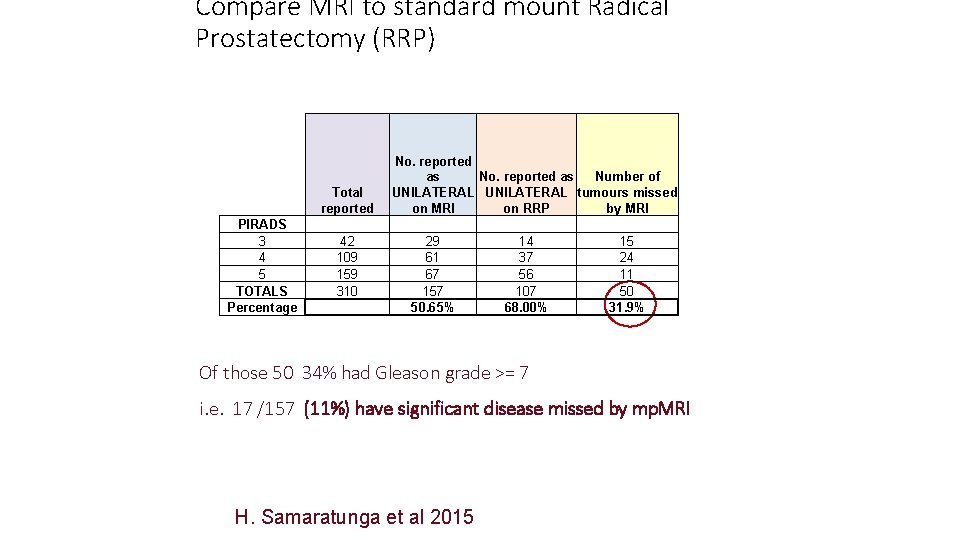
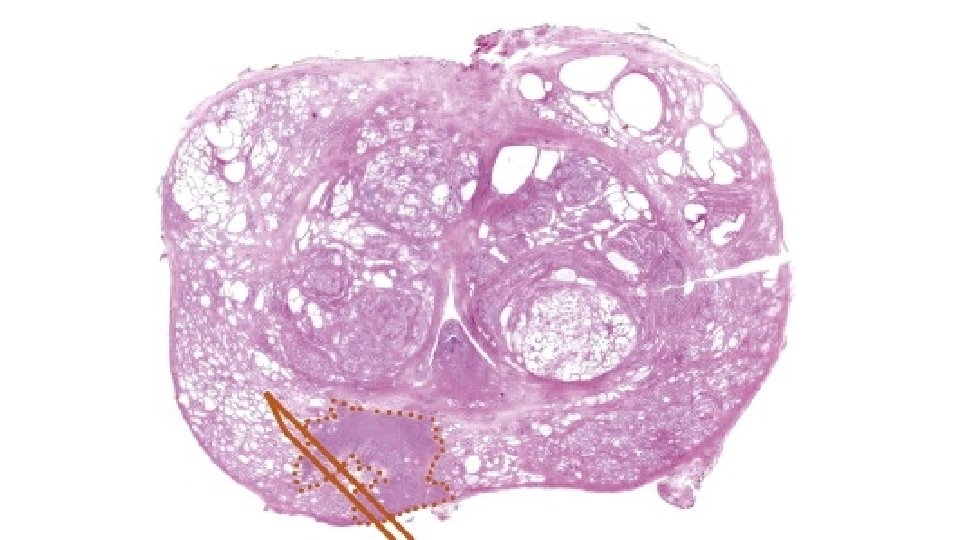
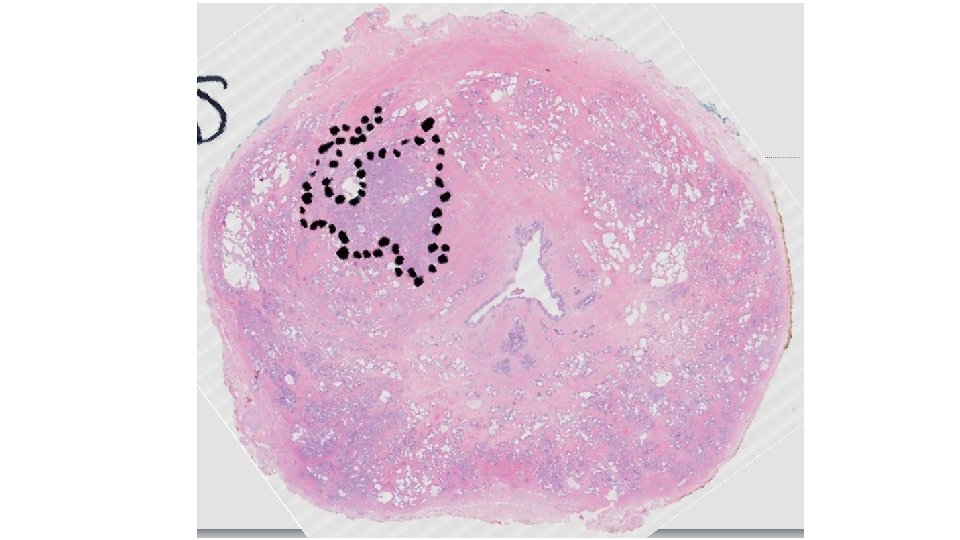
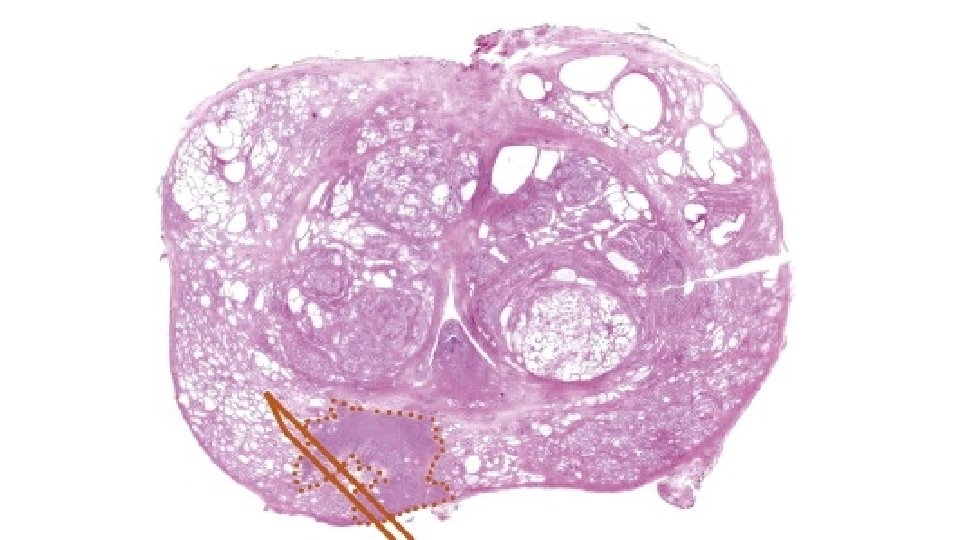
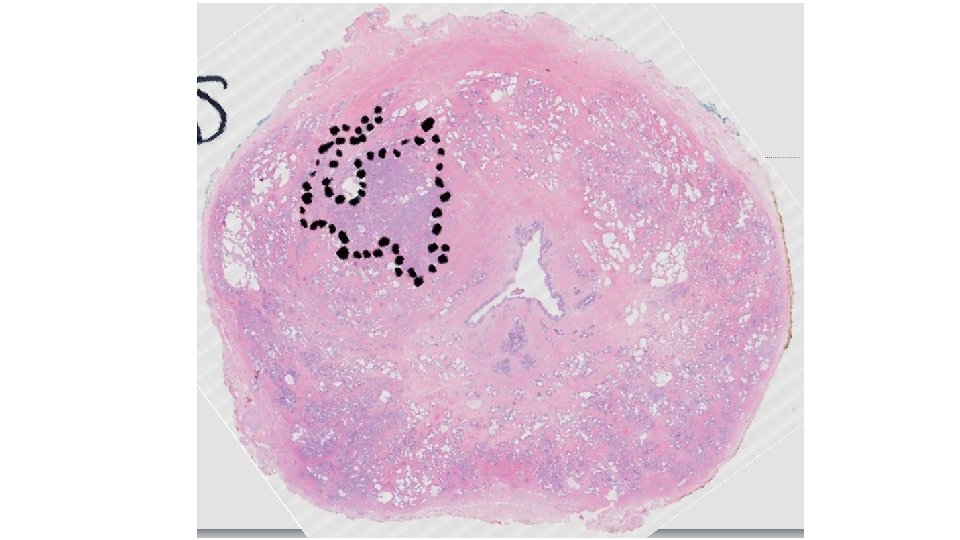
Compare MRI to standard mount Radical Prostatectomy (RRP) Total reported PIRADS 3 4 5 TOTALS Percentage 42 109 159 310 No. reported as Number of as UNILATERAL tumours missed on MRI on RRP by MRI 29 61 67 157 50. 65% 14 37 56 107 68. 00% 15 24 11 50 31. 9% Of those 50 34% had Gleason grade >= 7 i. e. 17 /157 (11%) have significant disease missed by mp. MRI H. Samaratunga et al 2015
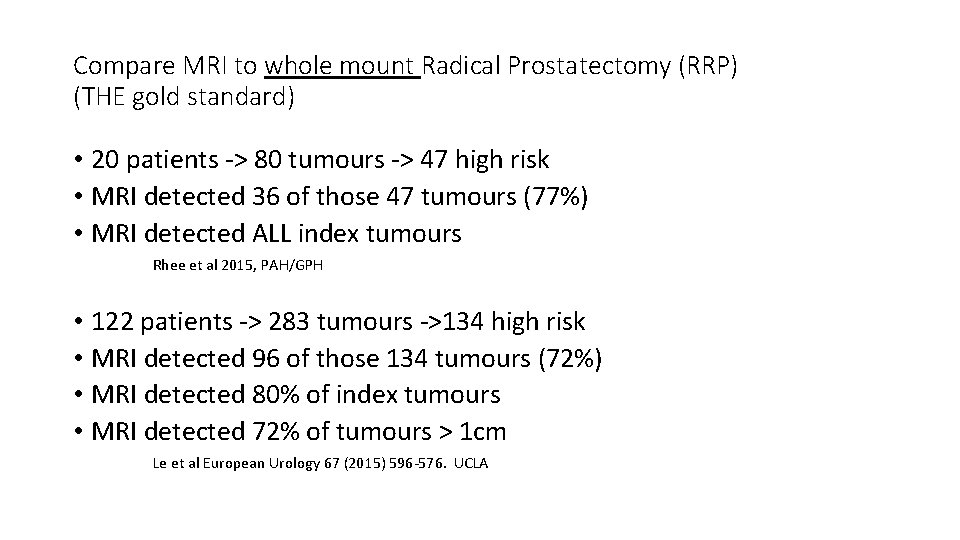
Compare MRI to whole mount Radical Prostatectomy (RRP) (THE gold standard) • 20 patients -> 80 tumours -> 47 high risk • MRI detected 36 of those 47 tumours (77%) • MRI detected ALL index tumours Rhee et al 2015, PAH/GPH • 122 patients -> 283 tumours ->134 high risk • MRI detected 96 of those 134 tumours (72%) • MRI detected 80% of index tumours • MRI detected 72% of tumours > 1 cm Le et al European Urology 67 (2015) 596 -576. UCLA

TAKE HOME MESSAGE • MRI finds more significant tumours than TRUS • MRI finds fewer insignificant tumours than TRUS BUT • TRUS finds some tumours missed by MRI • MRI misses up to 28% of significant tumours in radical prostatectomy specimens.
The solution to Overdiagnosis Improved diagnostic accuracy requires a multimodal cooperative approach between Urologists and radiologists MRI/MRIGB/TRUSGB DRE, PSAv, PSAD.
What role mp. MRI? OVER-TREATMENT Can mp. MRI facilitate selection of patients for Active Surveillance? Active surveillance with selective delayed intervention is the way to manage ‘good-risk’* prostate cancer Laurence Klotz University of Toronto** *Gleason score 6 or less PSA less than 10 ug/L Non palpable disease or small nodule Less than 1/3 cores positive Less than 50% involvement of any core **Nature Clinical Practice Urology March 2005 Vol 2 No 3
Active Surveillance Klotz et al 2010 J Clin Onc 28: 126 -131 N = 452 Median follow up 7 yrs Cancer specific survival 97% Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A, et al. Active surveillance for lowrisk prostate cancer worldwide: the PRIAS study. Eur Urol. 2013; 63: 597– 603. BUT!! Only 1 in 3 choose AS over active treatment** Only 2 in 3 stay on surveillance (Klotz et al) **Daubenmier et al 2006 J Urol 67: 125 -130
Active Surveillance • Why has take up of AS has been incomplete? • Only 1 in 3 opt for AS • Only 2 in 3 stay on AS • Literature not yet mature, short follow up • Risk of undergrading • Up to 33% of AS cases have higher Gleason Grade on repeat biopsy or subsequent radical prostatectomy. (Porten et al J Clin Oncol 2011; 29: 2795 -800)
Active Surveillance Improved diagnostic accuracy requires a multimodal cooperative approach between Urologists and radiologists MRI/MRIGB/TRUSGB DRE, PSAv, PSAD. • Guidelines starting to include MRI in AS protocols • TRUS biopsy numbers have fallen by 17% in the last 4 yrs* *MBS

MRI planning in Robotic Prostatectomy