Motivational Interviewing Encouraging Patients to Change Unhealthy Behavior
Motivational Interviewing: Encouraging Patients to Change Unhealthy Behavior CAPA 2015 Ian Jones, MPAS, CCPA, PA-C College of Medicine, University of Manitoba Adapted from Michael Vallis, Ph. D R Psych, 2013 and Ingrid Toews Ph. D
Changing Behaviors www. 2011 rrdc. com Fitafterfifty. com Image - Canadian Obesity Network.
Objectives: Teach the Teacher � Identify opportunities to integrate motivational interviewing in the practice setting � Identify patient cues for readiness to move towards change planning � Define empathetic counseling skills � Describe motivational interviewing as a style for meeting resistance
Predictors of. . . � What is the best predictor of future behavior? � Why is changing behavior difficult? � What is the best predictor of changed behavior?
Self-Efficacy � “A person’s confidence to perform a specific behavior in a specific context for a specific time period and in the face of specific barriers” Bandura, 1977
Motivational Interviewing Theory � Based on relevant theoretical models from psychology �A style is used to engage with patients, target their strengths and hopes, elicit their own reasons to change, and encourage autonomy in decision making. � Related to Patient-Centred Clinical Method – IFFE and Finding Common Ground Rollnick et al, 2010 Lussier et al. 2007
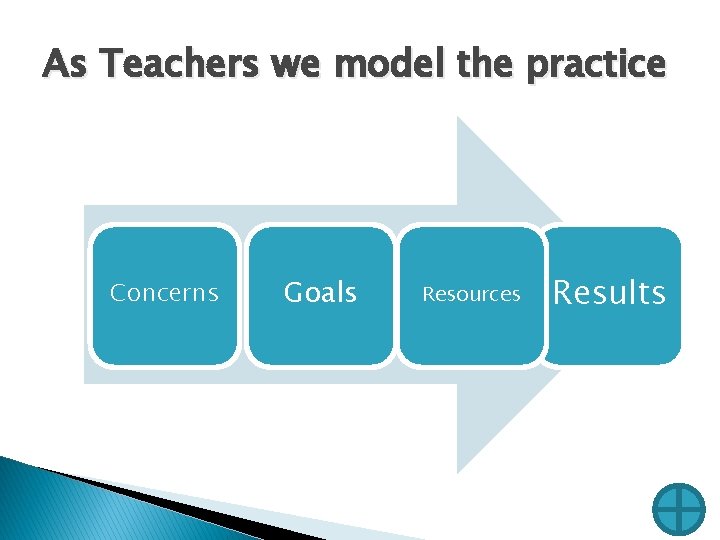
As Teachers we model the practice Concerns Goals Resources Results
Evidence � Meta-analysis by Burke, Arkowitz, & Dunn (2003) looked at 30 controlled clinical trials of motivational interviewing � Overall, motivational interviewing is effective with alcohol use, drug use, diet, exercise, and academics. � Apodace & Longabaugh (2009) found that the most consistent evidence of effectiveness was: client change talk and client experience of discrepancy Decisional balance had the strongest association with better outcomes.
Epidemiology � � � Smoking, poor diet, physical inactivity and alcohol misuse may account for 38% of annual US deaths (Woolf, 2008) Estimates that less than 5% of the population do not smoke, have a healthy weight, are physically active and eat 5 or more fruit/vegetables a day Lifestyle choices are integral to chronic disease occurrence. In 2005, the WHO estimated that Canada would lose US$500 million in national income from premature deaths due to heart disease, stroke, and diabetes yearly. As people die each year, losses accumulate; financial losses due to these premature deaths will skyrocket to an est. US$1. 5 billion by 2015, (http: //www. conferenceboard. ca/hcp/details/health. aspx)
Motivational Interviewing � How one interacts with patients appears to be as important as the approach � Empathy impacted 6 month drinking outcomes � Confrontational counselling has been associated with a higher drop out rate � Change talk and resistance has been found to be significantly influenced by counselling style � Rollick et al, 2010 What are the barriers to teaching or practicing – motivational interviewing?
Change-Based Relationship �Instead me” i. e. of: “I am the expert listen to �“Let me tell you what you need to do” �“Let me tell you what you need to know” To: “We both have a role to play” �“I understand that you will make your own decisions and I respect that. Can we have a conversation about your health? ” Vallis, 2013
Motivation for Health Behaviors � Positive reinforcement: ◦ Work an extra 60 min per day for 2 weeks and then I will give you $1000. 00 Negative reinforcement: Work an extra 60 min per day for 2 weeks At the end I will Not throw you down a flight of stairs. Long-term behavior change requires positive source of motivation in addition to negative reinforcement Vallis, 2013
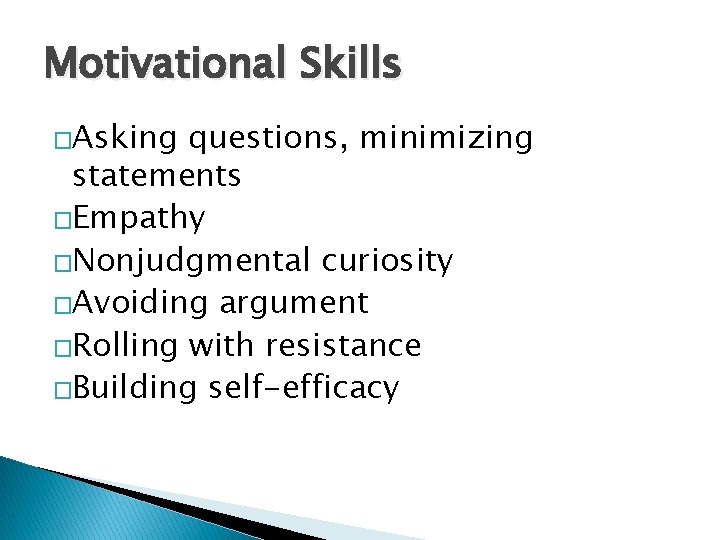
Motivational Skills �Asking questions, minimizing statements �Empathy �Nonjudgmental curiosity �Avoiding argument �Rolling with resistance �Building self-efficacy
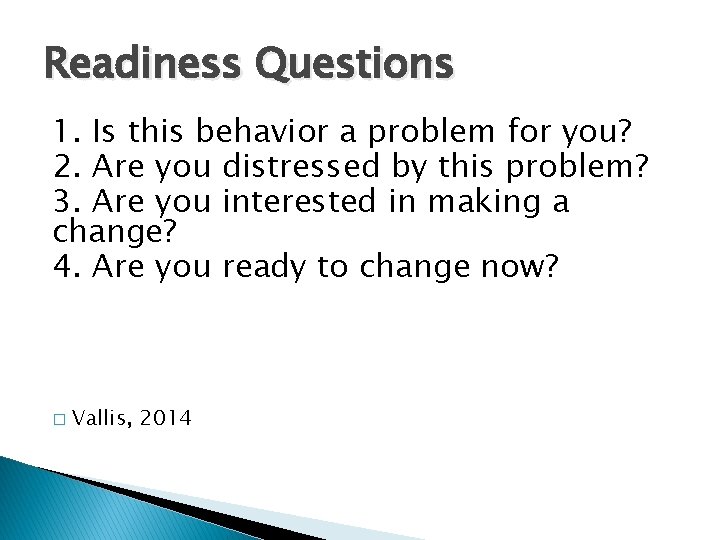
Readiness Questions 1. Is this behavior a problem for you? 2. Are you distressed by this problem? 3. Are you interested in making a change? 4. Are you ready to change now? � Vallis, 2014
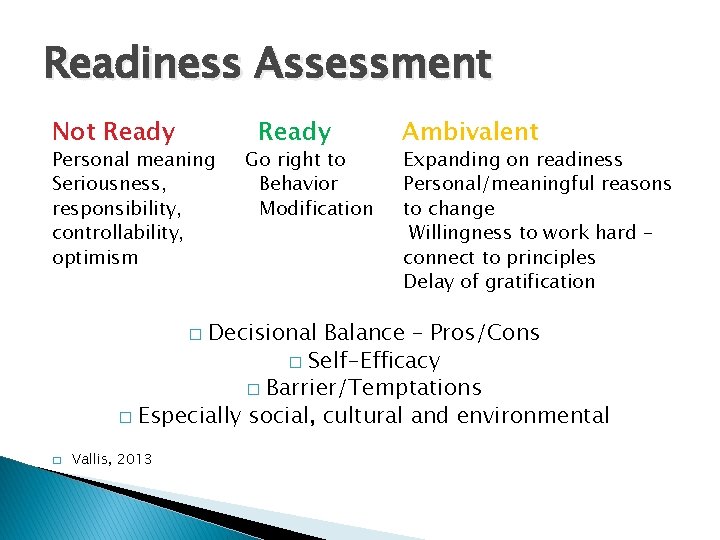
Readiness Assessment Not Ready Personal meaning Seriousness, responsibility, controllability, optimism Ready Go right to Behavior Modification Ambivalent Expanding on readiness Personal/meaningful reasons to change Willingness to work hard – connect to principles Delay of gratification Decisional Balance – Pros/Cons � Self-Efficacy � Barrier/Temptations � Especially social, cultural and environmental � � Vallis, 2013

5 A’s of Obesity Management https: //youtu. be/CDjn. YTOkja. Y
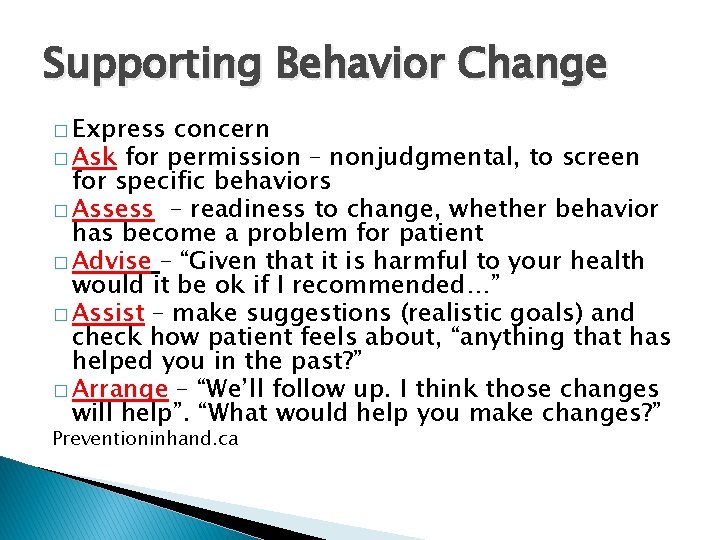
Supporting Behavior Change � Express concern � Ask for permission – nonjudgmental, to screen for specific behaviors � Assess – readiness to change, whether behavior has become a problem for patient � Advise – “Given that it is harmful to your health would it be ok if I recommended…” � Assist – make suggestions (realistic goals) and check how patient feels about, “anything that has helped you in the past? ” � Arrange – “We’ll follow up. I think those changes will help”. “What would help you make changes? ” Preventioninhand. ca
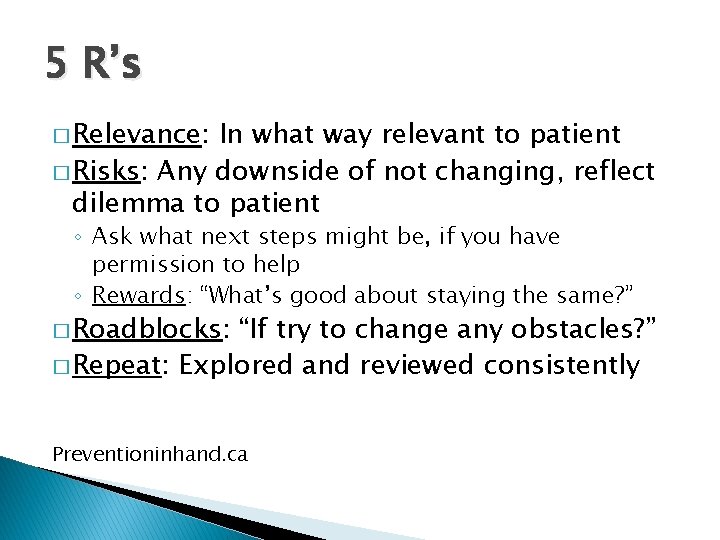
5 R’s � Relevance: In what way relevant to patient � Risks: Any downside of not changing, reflect dilemma to patient ◦ Ask what next steps might be, if you have permission to help ◦ Rewards: “What’s good about staying the same? ” � Roadblocks: “If try to change any obstacles? ” � Repeat: Explored and reviewed consistently Preventioninhand. ca
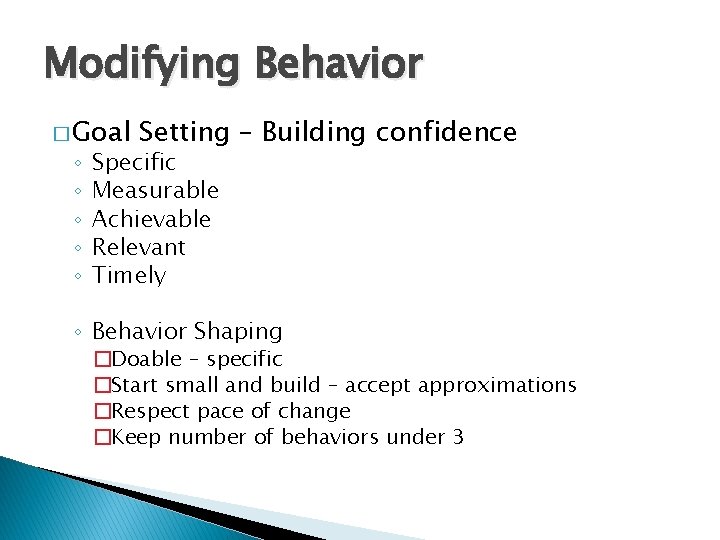
Modifying Behavior � Goal ◦ ◦ ◦ Setting – Building confidence Specific Measurable Achievable Relevant Timely ◦ Behavior Shaping �Doable – specific �Start small and build – accept approximations �Respect pace of change �Keep number of behaviors under 3
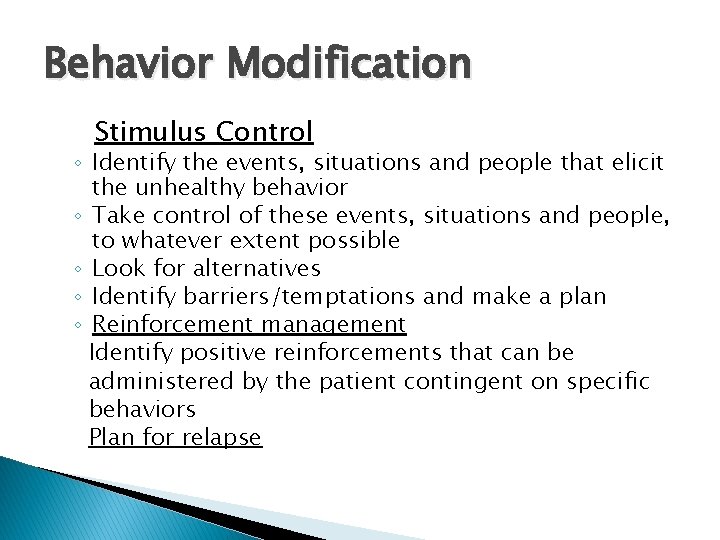
Behavior Modification Stimulus Control ◦ Identify the events, situations and people that elicit the unhealthy behavior ◦ Take control of these events, situations and people, to whatever extent possible ◦ Look for alternatives ◦ Identify barriers/temptations and make a plan ◦ Reinforcement management Identify positive reinforcements that can be administered by the patient contingent on specific behaviors Plan for relapse
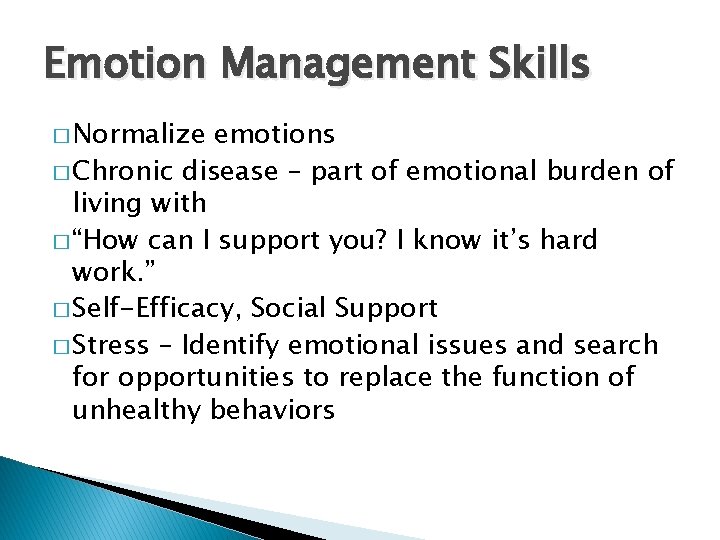
Emotion Management Skills � Normalize emotions � Chronic disease – part of emotional burden of living with � “How can I support you? I know it’s hard work. ” � Self-Efficacy, Social Support � Stress – Identify emotional issues and search for opportunities to replace the function of unhealthy behaviors
� Patient may need to try several or many times, the best chance of success is in making continued efforts (not giving up). � Physician continues to support the patients’ efforts to change and provides continuing encouragement. � Ambivalence can resurface Lussier & Richard, 2007
Exercises � http: //im 4 us. org/Behavior+Change+Teachin g+Materials � We use SP – Standardized Patient exercises ◦ Or Provide students with case then role play ◦ Video tape and then review
Summary - Change Skills � Relationship skills � Motivational skills – asking questions, minimizing statements, empathy, nonjudgmental curiosity, avoiding argument, rolling with resistance and building self-efficacy � Behavior change skills - goal-setting, behavior shaping, stimulus control, reinforcement management � Emotion management skills – identifying function served by unhealthy behaviors, stress management

Objectives � Identify opportunities to integrate motivational interviewing in the practice setting � Identify patient cues for readiness to move towards change planning � Define empathetic counseling skills � Describe motivational interviewing as a style for meeting resistance � Michael Vallis www. behaviourchangeinstitute. ca

Resources � http: //www. obesitynetwork. ca/ � http: //rethinkingdrinking. niaaa. nih. gov/ � http: //www. exerciseismedicine. ca/ � http: //www. hc-sc. gc. ca/hc-ps/tobac- tabac/quit-cesser/index-eng. php
References � � � � � Apodaca, T. R. & Longabaugh, R. (2209) Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence, Addiction, 104 (5): p. 705 -715. Bandura, A. (1977). Self-Efficacy: Toward a unifying theory of behavior change. Psychological Review, 84, 191 -215. Burke, B. L. , Arkowitz, H. , & Dunn, C. (2003). The efficacy of motivational interviewing: A metaanalysis of controlled clinical trials. Journal of Consulting and Clinical Psychology, 71, 843861. Lussier, M. & Richard, C. (2007). The Motivational Interview, Canadian Family Physician, 53, p. 2117 – 2118. Lussier, M. & Richard, C. (2007). The Motivational Interview, Canadian Family Physician, 53, p. 1895 -1896. Prevention in Hand, College of Family Physicians of Canada and the Public Health Agency of Canada. Preventioninhand. ca Reeves, MJ, Rafferty AP. Health lifestyle characteristics among adults in the United States, 2000. Arch Intern Med 2005; 165: 854 -7. Rollick S. et al. (2010). Motivational Interviewing, BMJ 2010; 340: c 1900. Tamakoshi A, Tamakoshi K, Lin Y, et al. Healthy lifestyle and preventable death: Findings from the Japan Collaborative Cohort (JACC) Study. Prev Med 2009; 48: 486 -92. Vallis, M. V. 2009 Appreciating the Challenge: Motivation and Change. Association of Faculties of Pharmacy of Canada 66 th Annual Meeting and Conference.
References (cont’d) � � � Vallis, M. Workshop for the Manitoba Psychological Society, October, 2013, Winnipeg, MB Vallis, M. Behavior Change Counselling-How Do I Know If I Am Doing It Well? The Development of the Behavior Change Counselling Scale (BCCS), Canadian Journal of Diabetes, 37, 18 -26. Woolf, S. H. (2008). The power of prevention and what it requires. JAMA, 299: 2437 -9.
- Slides: 28