Motivational Change Model in Healthcare An Intrinsic Motivational


- Slides: 16
Motivational Change Model in Healthcare
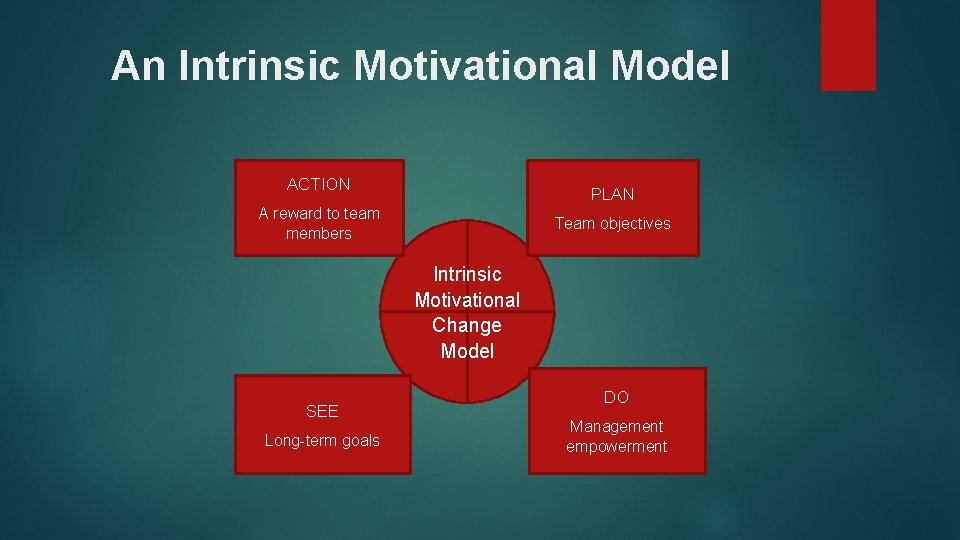
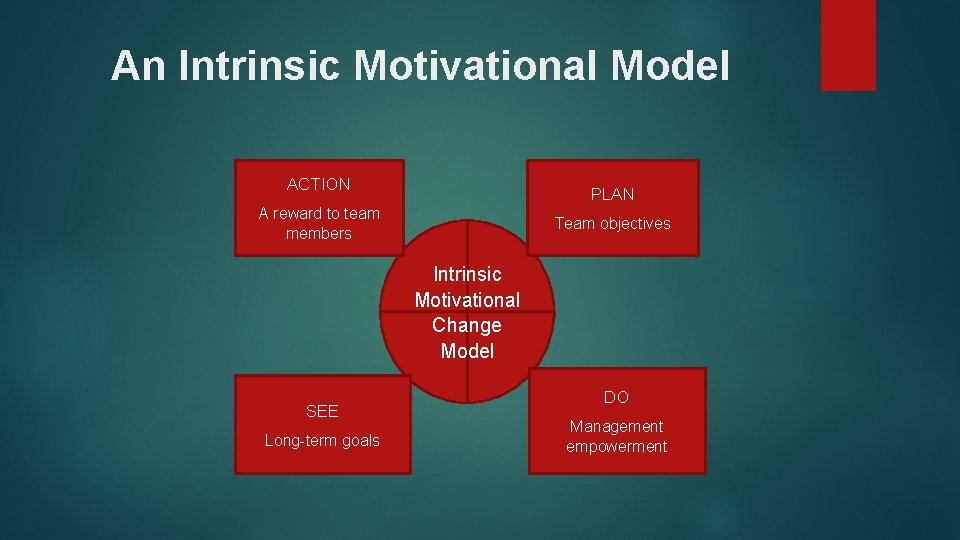
An Intrinsic Motivational Model ACTION PLAN A reward to team members Team objectives Intrinsic Motivational Change Model SEE Long-term goals DO Management empowerment
Methods of Evaluating the need for Change Healthcare needs keep increasing with time hence the practitioners need to have motivational means to help them work well. According to the study, healthcare practitioners must be motivated through action, plan, vision (see) and management empowerment. Through the evaluation of the models for change, the motivational means that can help healthcare practitioners in working and delivering to their level best should be incentives from employers (Asimakopoulos, & Spillers, 2017, March). The modes of evaluating change in the healthcare system must have a clear purpose that can solve social implications through originality methods. Previously failed tactics should not be used.

Need for Change
Approach and Criteria The determination of change must be executed in a manner that cannot hinder normal operations from taking place. For example, making a change in shift should not disregard scheduled patient checkups and other treatment appointments. Therefore, the criteria must be selected in ways that fit smoothly into the system (Pinzone, Guerci, Lettieri, & Redman, 2016). To effectively engage into a proper setup of the model of change, the operations within the proposed change must be aligned to ensure everyone within the nursing department has received a motivation through salary increment, overtime pay, and other forms of compensating extra work.
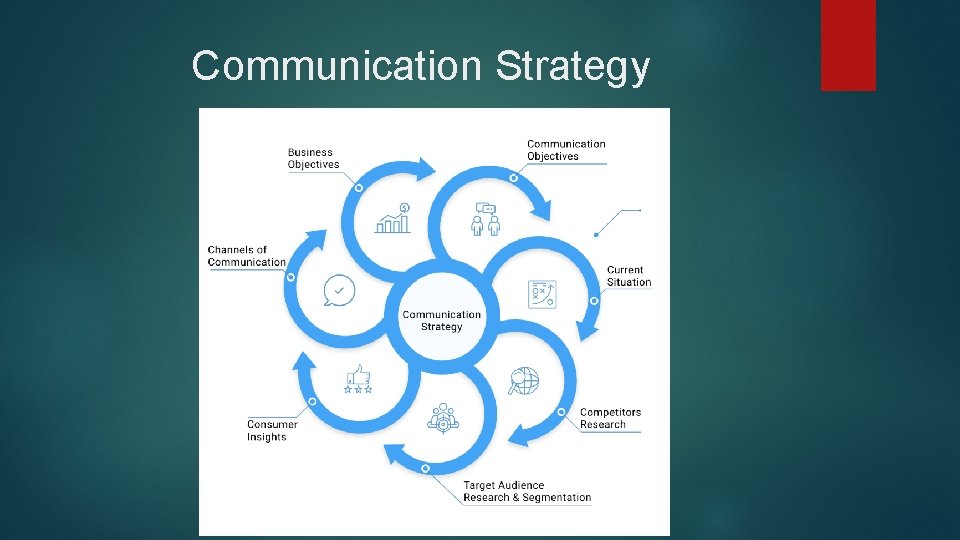
Communication Strategy Before the implementation of change, the management must be informed of the proposed change. The reason for communicating before effecting the change is to make those involved in the motivational change model aware of the planned changes within the institution. Setting out of the effectiveness of the plan must be structured out for communication channel to work out properly (Naidu, Nunn, & Irwin, 2015). Since the goal for the change of model is to ensure long-term satisfaction of healthcare practitioners, a consideration of the passage of information from current to future recruits into the system must be communicated well to help pass information regarding motivational standards.
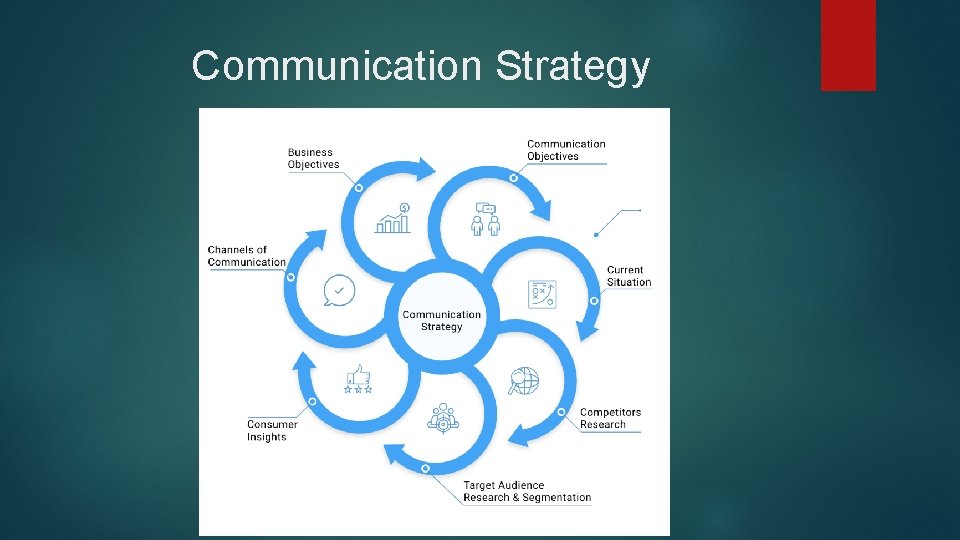
Communication Strategy
Stakeholder Support Apart from setting strategies of implementing a change model to healthcare practitioners, the stakeholder support must be involved to help determine the amount of extra finances to set aside for the motivational plan (Fu, Roth, Battaglia, Nelson, Farmer, Do, & Zillich, 2015). However, it is not guaranteed to receive monetary value support from stakeholders, but certain nonmonetary help can be issued such as employing more practitioners or hiring part-time staff (Silver, Mc. Quillan, Harel, Weizman, Thomas, Nesrallah, & Chertow, 2016).
Overcoming Resistance is a possible expectation from any management when extra cost is proposed to the system. during the resistance from stakeholders and other top managers on the acceptance of motivating staff, the presentation of the outcome to the healthcare institution should be informed to help accept the proposal (Barker, Atkins, & Lusignan, 2016). For example, such a system will increase efficiency and reduce long queues that are caused by slow workers due to low wages. However, when employees are remunerated well, the motivation to work increases hence become more productive.
Overcoming Resistance
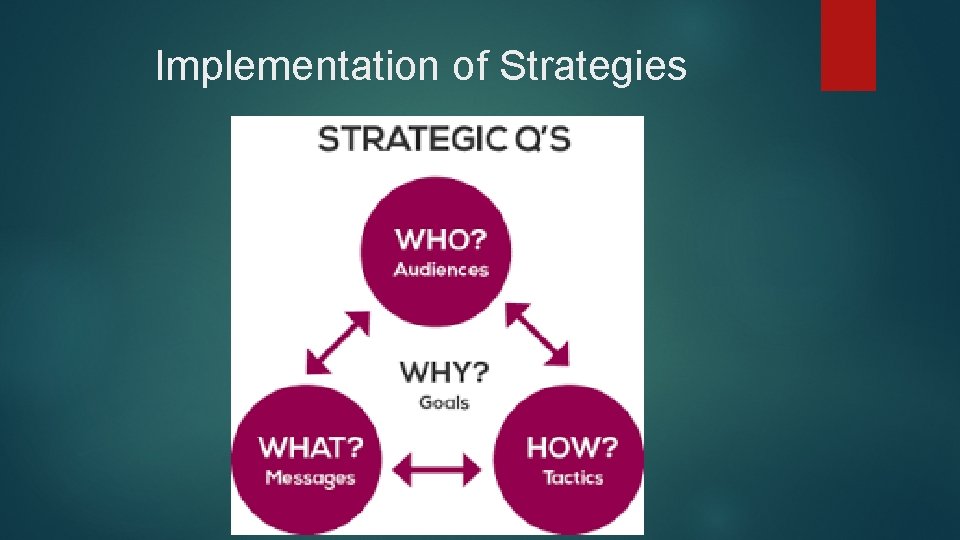
Implementation of Strategies While developing the change of model strategy, the success of the model highly depends on the critical success factors such as when, who, where, and how the desired objectives and goals must be achieved. The people, resources, and place of strategy implementation must be ascertained to ensure consistency of workflow. Provided the required staff and equipment, offering motivation in other means like time and monetary value can offer healthcare practitioners the morale of working hard and meeting deadlines (Copeland, Mc. Namara, Kelson, & Simpson, 2015). In cases of emergencies and extra time, serving patients will be easier due to set compensation plans.
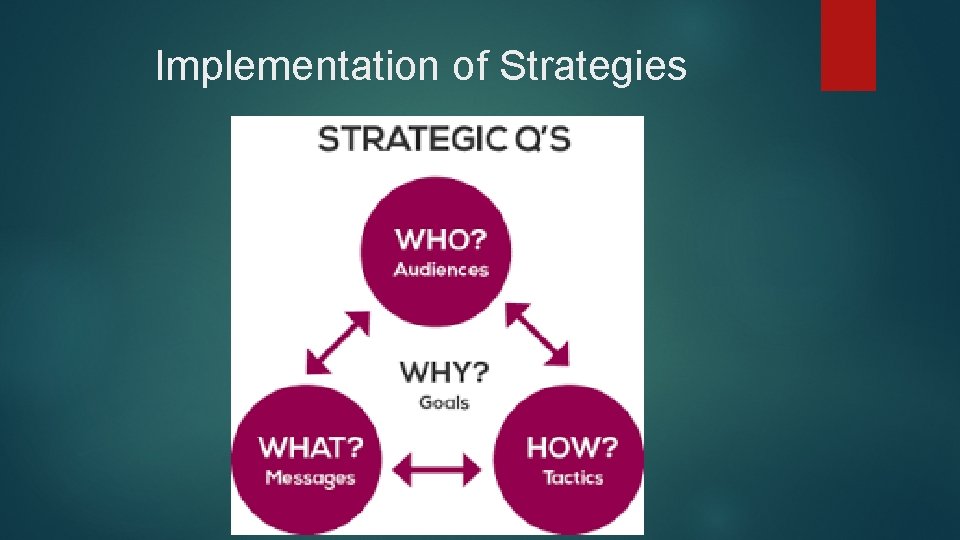
Implementation of Strategies
Sustainability Strategies The sustainability of the set model will be made possible through environmental neutrality and other sustainability goals like improved operations and advanced supply chain. The supply chain will ensure medicine and other facilities are available as needed to prevent running out of tools (Deschamps, Rinfret, Lagacé, & Privé, 2016). The ability of maintaining set strategies of making changes in the mode of motivating healthcare providers will make the program a success.

Sustainability Strategies
Conclusion The change model is believed to offer the intended solution to healthcare motivation. Nurses and doctors that are underpaid will receive recognition both from the employer and the public who will help in collaborating. Motivation can be done in various wasy apart from monetary value. Therefore, the proposed change for motivation in the healthcare system will revive healthcare institutions. Recognition and appreciation can make great improvements.
References Asimakopoulos, S. , Asimakopoulos, G. , & Spillers, F. (2017, March). Motivation and user engagement in fitness tracking: Heuristics for mobile healthcare wearables. In Informatics (Vol. 4, No. 1, p. 5). Multidisciplinary Digital Publishing Institute. Barker, F. , Atkins, L. , & de Lusignan, S. (2016). Applying the COM-B behaviour model and behaviour change wheel to develop an intervention to improve hearing-aid use in adult auditory rehabilitation. International journal of audiology, 55(sup 3), S 90 -S 98. Copeland, L. , Mc. Namara, R. , Kelson, M. , & Simpson, S. (2015). Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: a systematic review. Patient education and counseling, 98(4), 401 -411. Deschamps, C. , Rinfret, N. , Lagacé, M. C. , & Privé, C. (2016). Transformational leadership and change: How leaders influence their followers’ motivation through organizational justice. Journal of Healthcare Management, 61(3), 194 -213. Fu, S. S. , Roth, C. , Battaglia, C. T. , Nelson, D. B. , Farmer, M. M. , Do, T. , . . . & Zillich, A. J. (2015). Training primary care clinicians in motivational interviewing: a comparison of two models. Patient education and counseling, 98(1), 61 -68. Naidu, R. , Nunn, J. , & Irwin, J. D. (2015). The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: an exploratory cluster randomised controlled study. BMC Oral Health, 15(1), 101. Pinzone, M. , Guerci, M. , Lettieri, E. , & Redman, T. (2016). Progressing in the change journey towards sustainability in healthcare: the role of ‘Green’HRM. Journal of Cleaner Production, 122, 201 -211. Silver, S. A. , Mc. Quillan, R. , Harel, Z. , Weizman, A. V. , Thomas, A. , Nesrallah, G. , . . . & Chertow, G. M. (2016). How to sustain change and support continuous quality improvement. Clinical Journal of the American Society of Nephrology, 11(5), 916 -924.