MORTALITY Respir dis Cancer Injury poisoning Gastroint dis







- Slides: 34
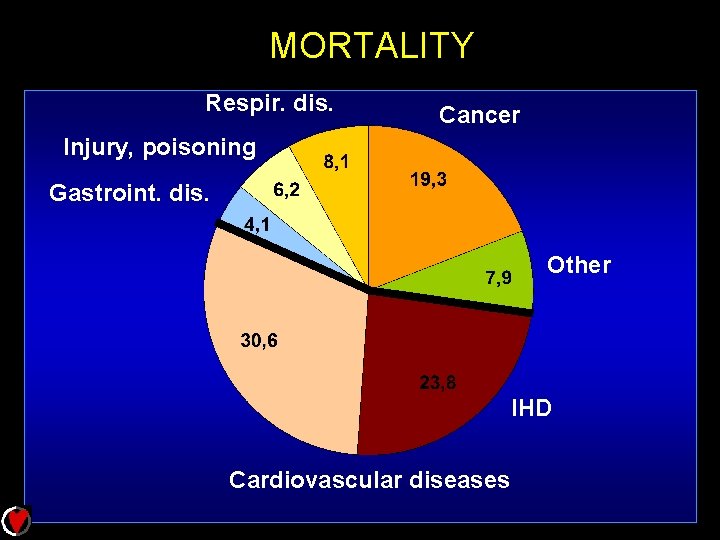
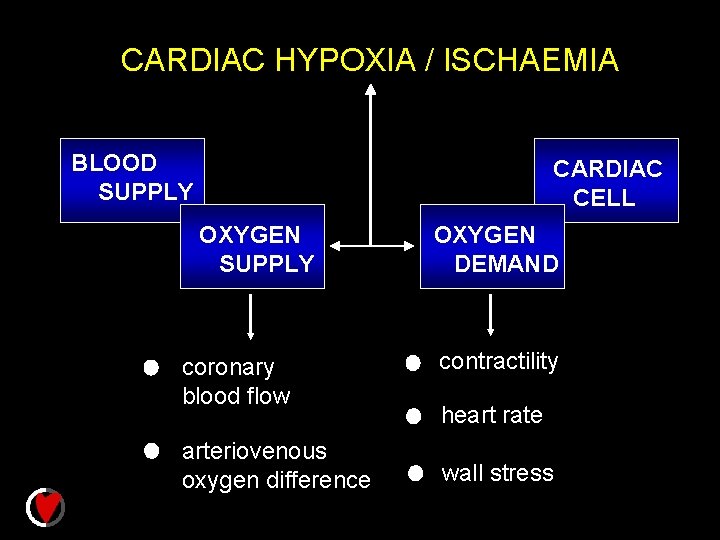
MORTALITY Respir. dis. Cancer Injury, poisoning Gastroint. dis. Other IHD Cardiovascular diseases
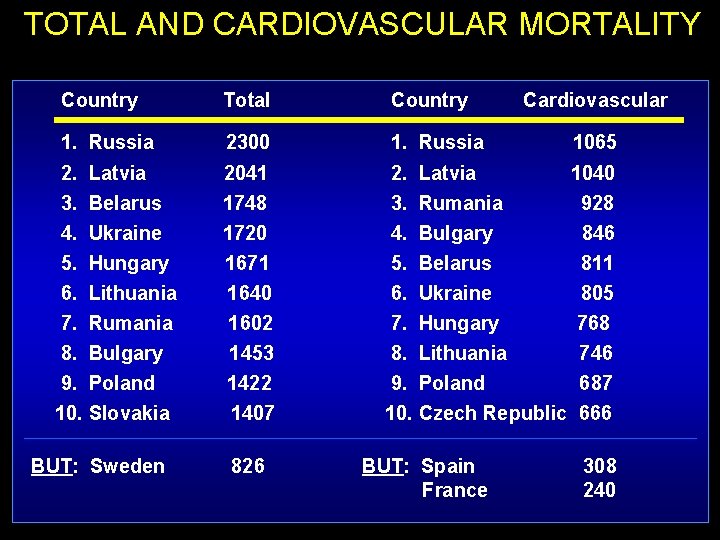
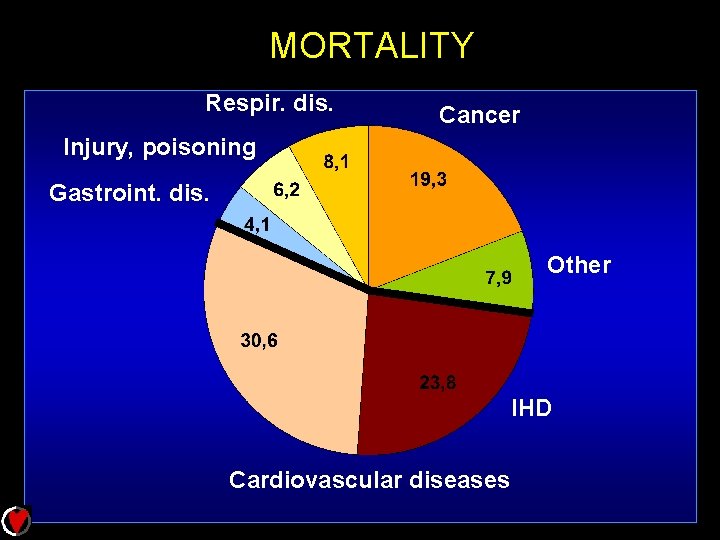
TOTAL AND CARDIOVASCULAR MORTALITY Country Total Country 1. Russia 2300 1. Russia 2. Latvia 3. Belarus 4. Ukraine 5. Hungary 6. Lithuania 7. Rumania 8. Bulgary 9. Poland 10. Slovakia 2041 1748 1720 1671 1640 1602 1453 1422 1407 2. Latvia 1040 3. Rumania 928 4. Bulgary 846 5. Belarus 811 6. Ukraine 805 7. Hungary 768 8. Lithuania 746 9. Poland 687 10. Czech Republic 666 BUT: Sweden 826 BUT: Spain France Cardiovascular 1065 308 240
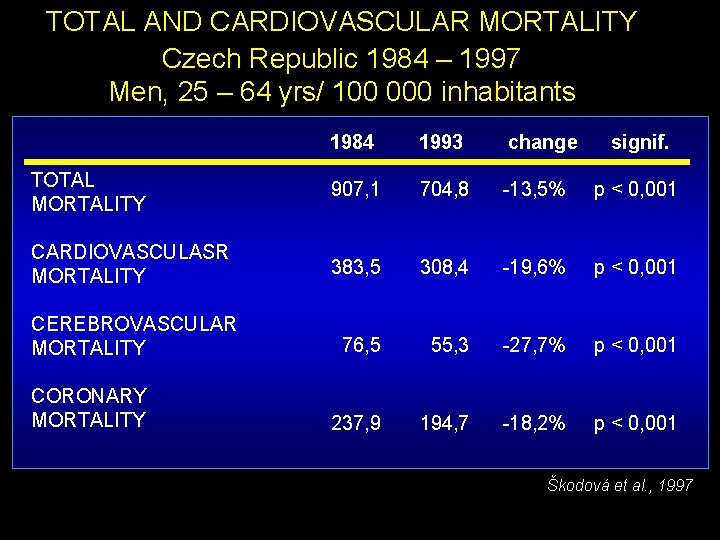
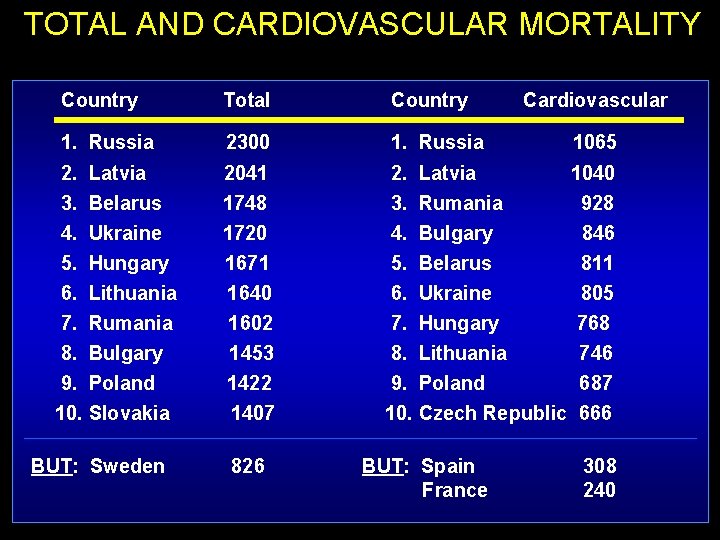
TOTAL AND CARDIOVASCULAR MORTALITY Czech Republic 1984 – 1997 Men, 25 – 64 yrs/ 100 000 inhabitants 1984 1993 change TOTAL MORTALITY 907, 1 704, 8 -13, 5% p < 0, 001 CARDIOVASCULASR MORTALITY 383, 5 308, 4 -19, 6% p < 0, 001 CEREBROVASCULAR MORTALITY 76, 5 55, 3 -27, 7% p < 0, 001 237, 9 194, 7 -18, 2% p < 0, 001 CORONARY MORTALITY signif. Škodová et al. , 1997
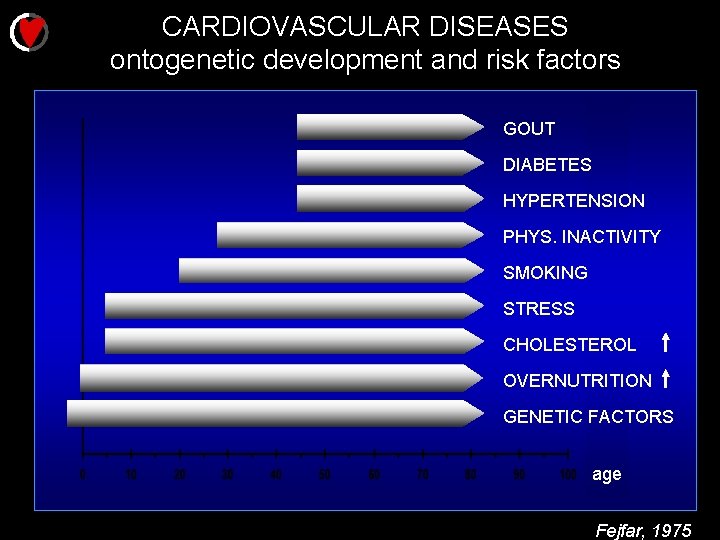
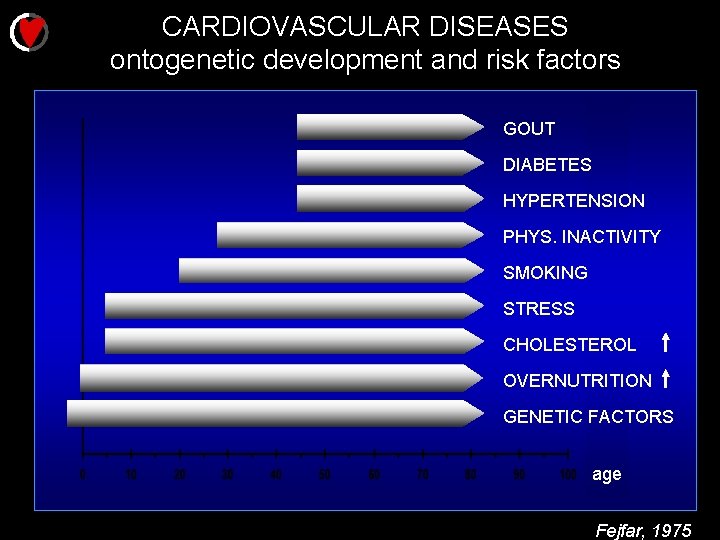
CARDIOVASCULAR DISEASES ontogenetic development and risk factors GOUT DIABETES HYPERTENSION PHYS. INACTIVITY SMOKING STRESS CHOLESTEROL OVERNUTRITION GENETIC FACTORS age Fejfar, 1975
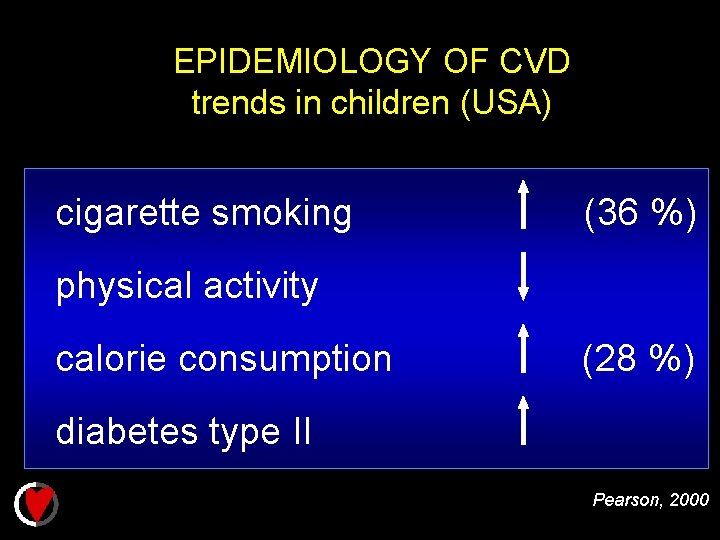
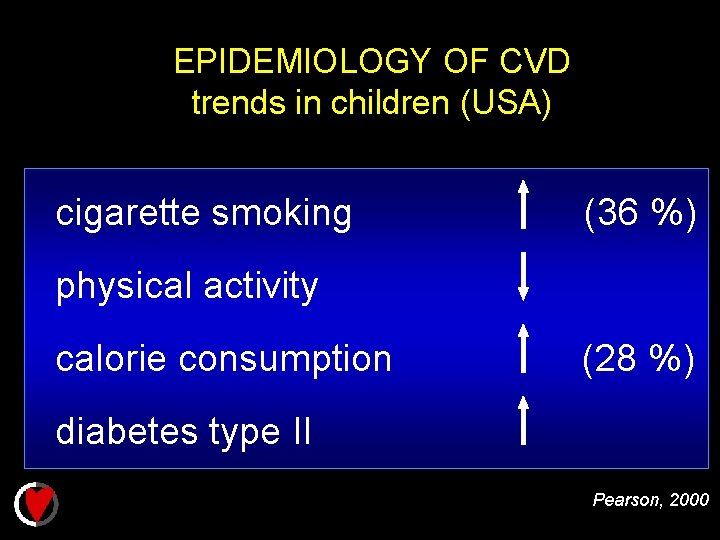
EPIDEMIOLOGY OF CVD trends in children (USA) cigarette smoking (36 %) physical activity calorie consumption (28 %) diabetes type II Pearson, 2000

CARDIAC ISCHEMIA vascular resistance heart rate coronary flow O 2 SUPPLY transporting capacity of blood for O 2 CONSUMP. contractility wall stress

DEVELOPMENT OF ISCHEMIC INJURY MINUTES SECONDS ONSET OF SEVERE HYPOXIA Reduced oxygen availability Acute contractile failure Reduction of mitochondrial oxidative metabolism Disturbances of transmembrane ionic balance Reduced ATP production Reduction of creatine phosphate stores Reduction of amplitude and duration of action potential Leakage of potassium ST-segment changes Accumulation of sodium and chloride ions Catecholamine release Stimulation of glycogenolysis Increase in glycolytic flux Development of intracellular acidosis Inhibition of fatty acid oxidation Utilization of glycogen Slowing of glycolytic flux Increasing depletion of energy stores Cell swelling Increase in cytosolic calcium ions Possible exhaustion of glycogen reserves Inhibition of glycolysis Severe depletion of ATP and creatine phosphate Ultrastructural changes, eg. mitochondrial swelling Possible onset of contracture HOURS ONSET OF IRREVERSIBLE DAMAGE? Lysosomal changes and activation of hydrolases Increasing cellular edema Loss of mitochondrial respiratory control Nonspecific electrocardiographic changes Major ultrastructural changes Complete depletion of energy reserves Loss of mitochondrial components Membrane injury and cellular disruption Cellular autolysis CELL DEATH AND TISSUE NECROSIS Hearse, 1979
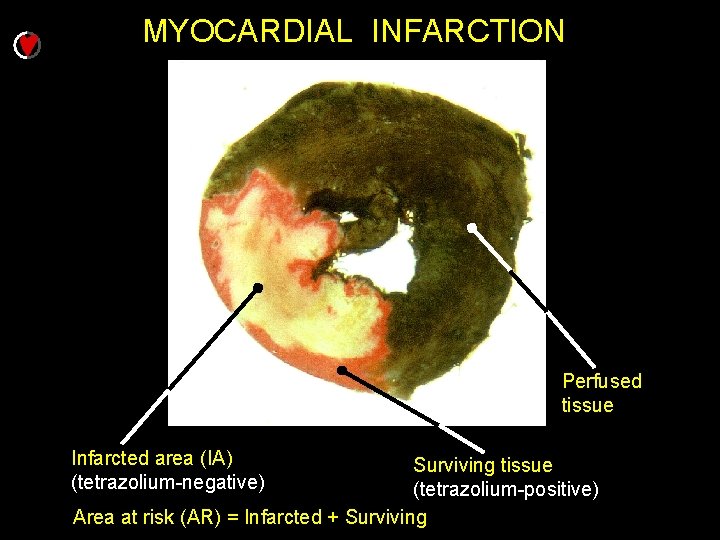
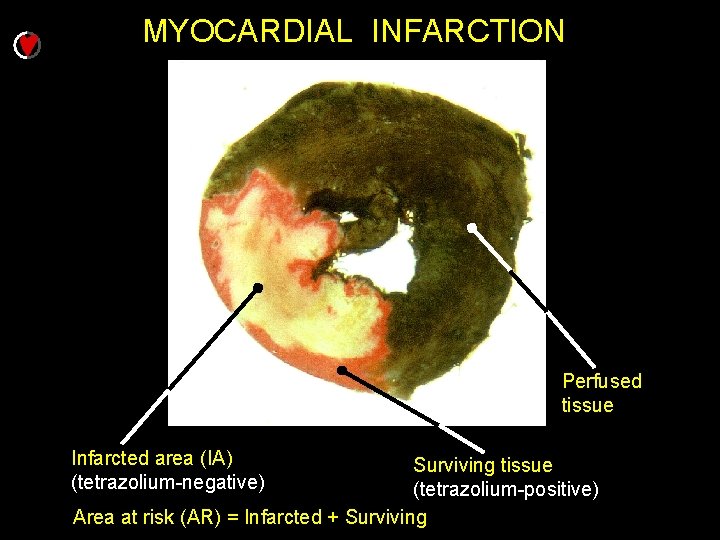
MYOCARDIAL INFARCTION Perfused tissue Infarcted area (IA) (tetrazolium-negative) Surviving tissue (tetrazolium-positive) Area at risk (AR) = Infarcted + Surviving
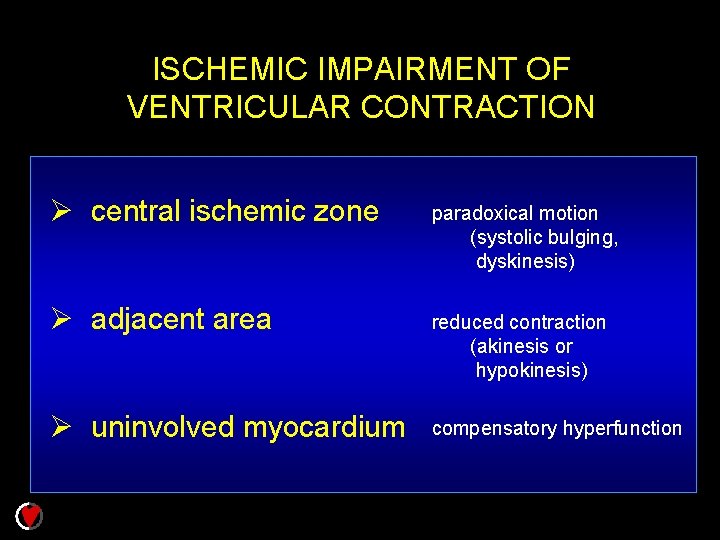
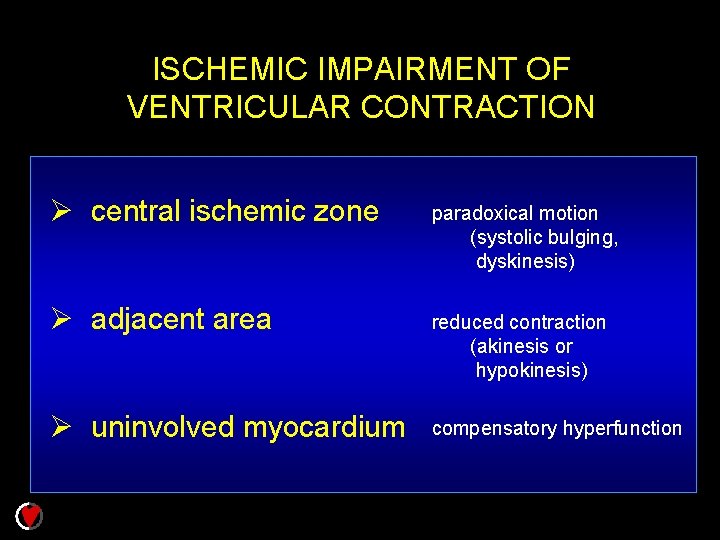
ISCHEMIC IMPAIRMENT OF VENTRICULAR CONTRACTION Ø central ischemic zone paradoxical motion (systolic bulging, dyskinesis) Ø adjacent area reduced contraction (akinesis or hypokinesis) Ø uninvolved myocardium compensatory hyperfunction
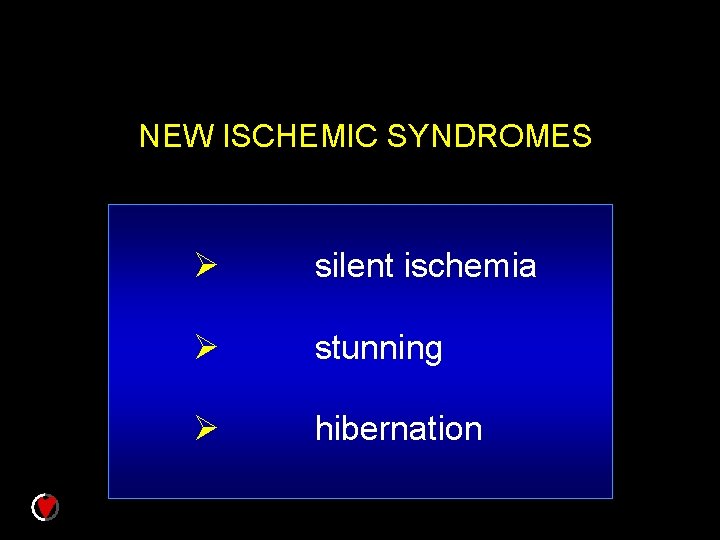
NEW ISCHEMIC SYNDROMES Ø silent ischemia Ø stunning Ø hibernation
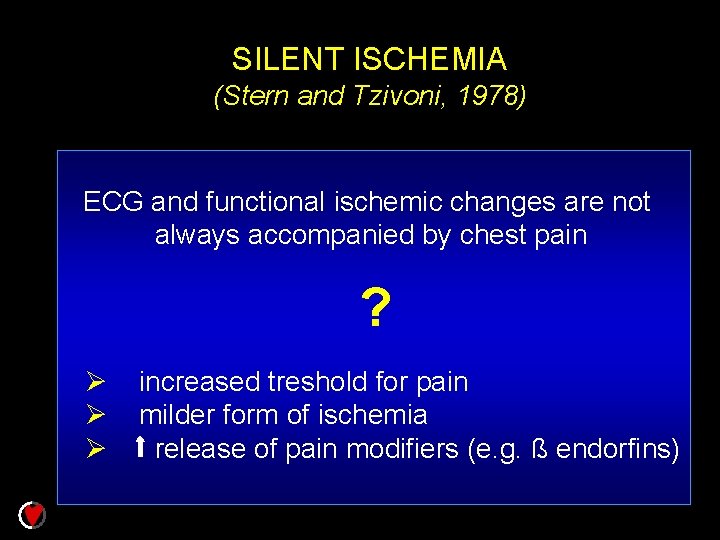
SILENT ISCHEMIA (Stern and Tzivoni, 1978) ECG and functional ischemic changes are not always accompanied by chest pain ? Ø Ø Ø increased treshold for pain milder form of ischemia release of pain modifiers (e. g. ß endorfins)

STUNNING (Heyndrickx et al. , 1975 Braunwald and Kloner, 1982) „Mechanical dysfunction that persists after reperfusion despite Ø absence of irreversible damage Ø restoration of normal or near-normal coronary flow“ Bolli, 1990
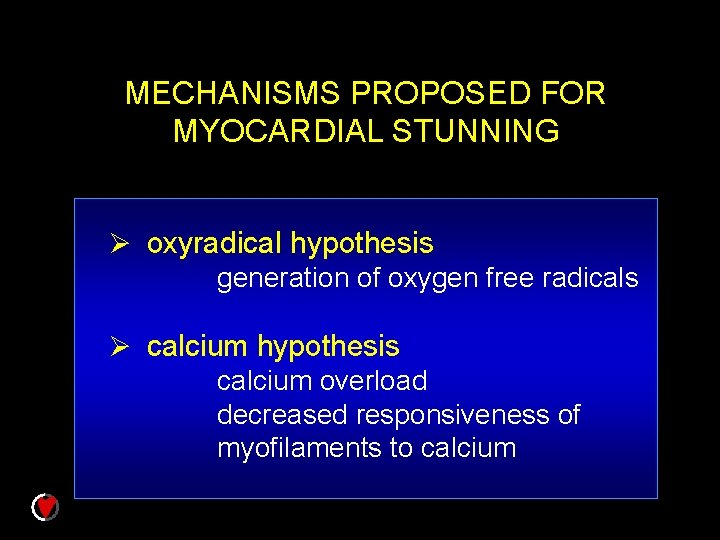
MECHANISMS PROPOSED FOR MYOCARDIAL STUNNING Ø oxyradical hypothesis generation of oxygen free radicals Ø calcium hypothesis calcium overload decreased responsiveness of myofilaments to calcium
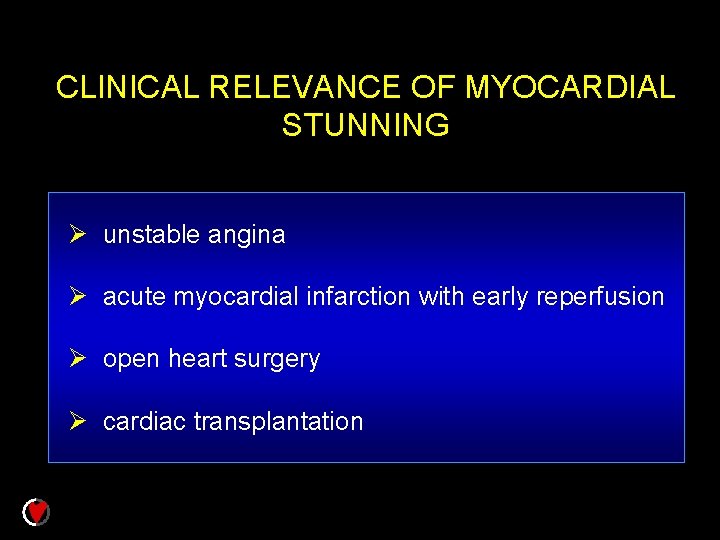
CLINICAL RELEVANCE OF MYOCARDIAL STUNNING Ø unstable angina Ø acute myocardial infarction with early reperfusion Ø open heart surgery Ø cardiac transplantation

HIBERNATION „…a persistent contractile dysfunction that is associated with reduced coronary flow but preserved myocardial viability. “ Bolli, 1992 ONCE CORONARY FLOW IS RESTORED, THE DYSFUNCTION IS COMPLETELY REVERSED
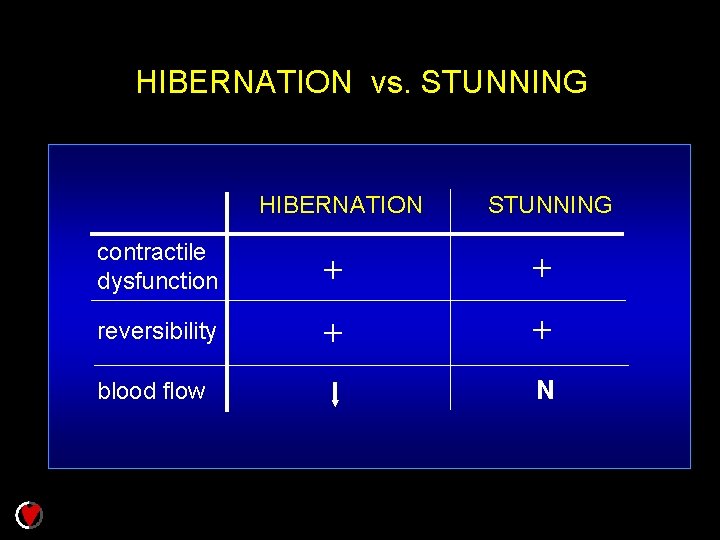
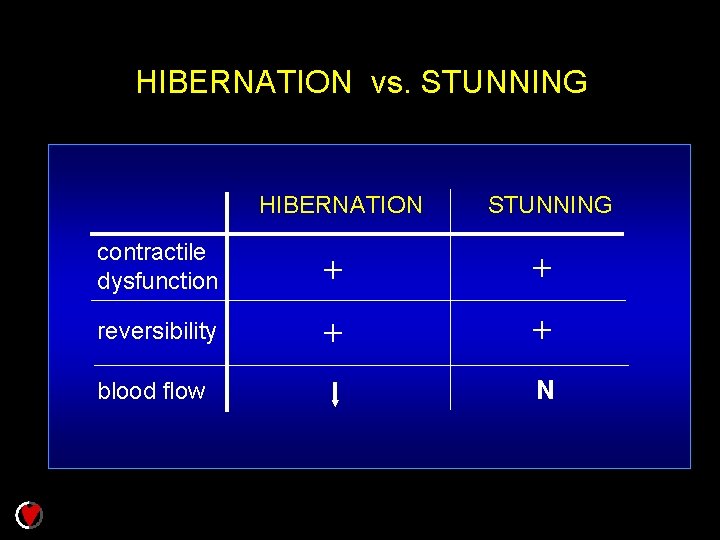
HIBERNATION vs. STUNNING HIBERNATION STUNNING contractile dysfunction + + reversibility + + blood flow N
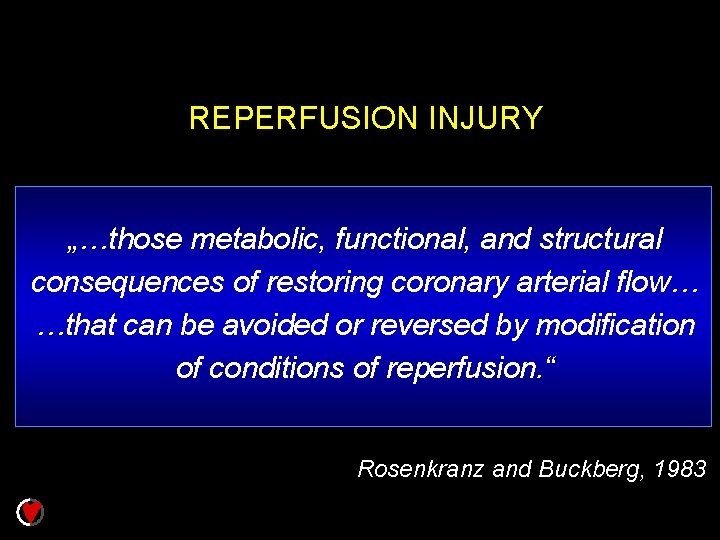
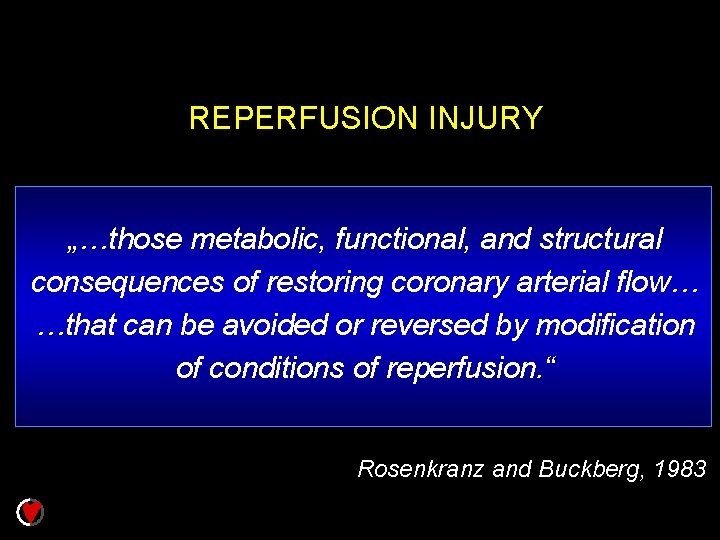
REPERFUSION INJURY „…those metabolic, functional, and structural consequences of restoring coronary arterial flow… …that can be avoided or reversed by modification of conditions of reperfusion. “ Rosenkranz and Buckberg, 1983
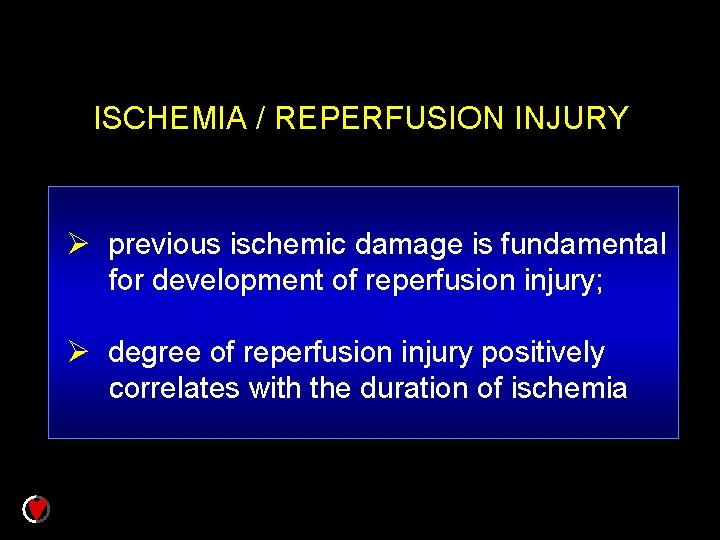
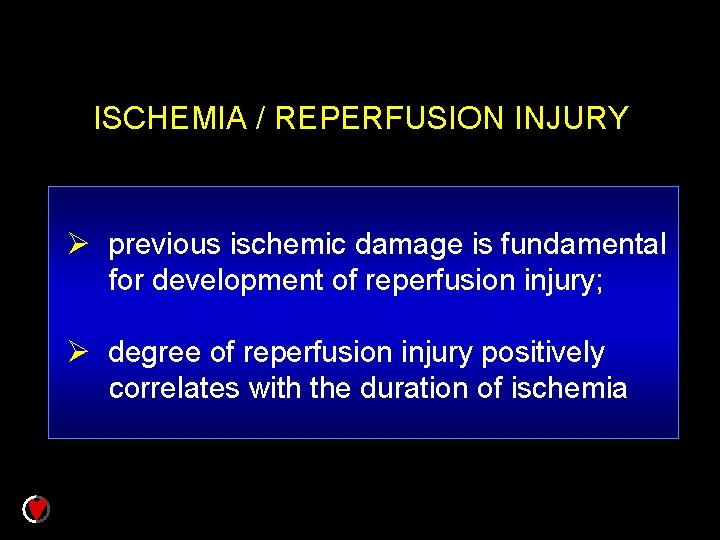
ISCHEMIA / REPERFUSION INJURY Ø previous ischemic damage is fundamental for development of reperfusion injury; Ø degree of reperfusion injury positively correlates with the duration of ischemia

MECHANISMS OF REPERFUSION INJURY Ø FACTORS USEFUL OR ESSENTIAL FOR NORMAL CELLS - re-energization - p. H normalization Ø FACTORS HARMFUL IF DECREASED SELF-DEFENSE SYSTEM - oxygen radicals - proteases Ø FACTORS ACTIVATED BY ISCHEMIA-INDUCED CHANGES - neutrophils - complement system - other factors of inflammatory reaction Ø „NO-REFLOW“ PHENOMENON
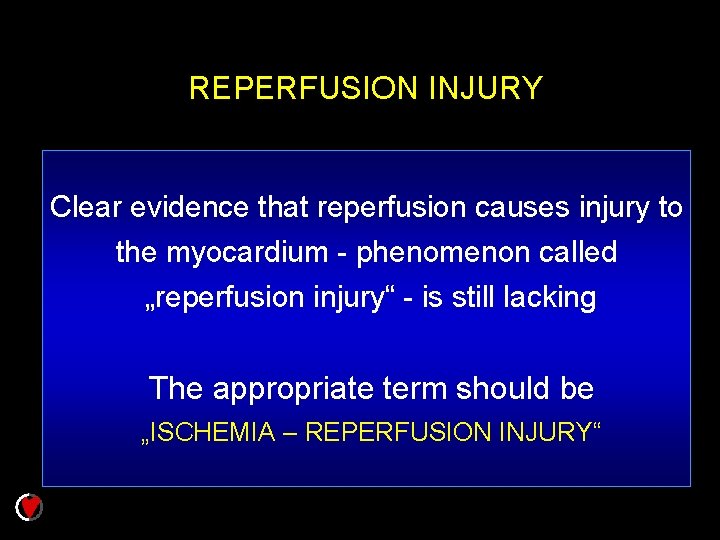
REPERFUSION INJURY Clear evidence that reperfusion causes injury to the myocardium - phenomenon called „reperfusion injury“ - is still lacking The appropriate term should be „ISCHEMIA – REPERFUSION INJURY“
CARDIAC TOLERANCE TO OXYGEN DEPRIVATION depends on: w AGE w SEX
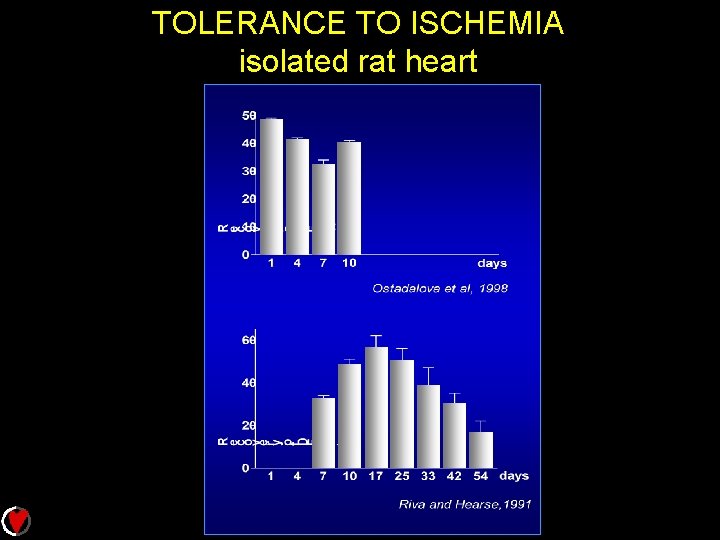
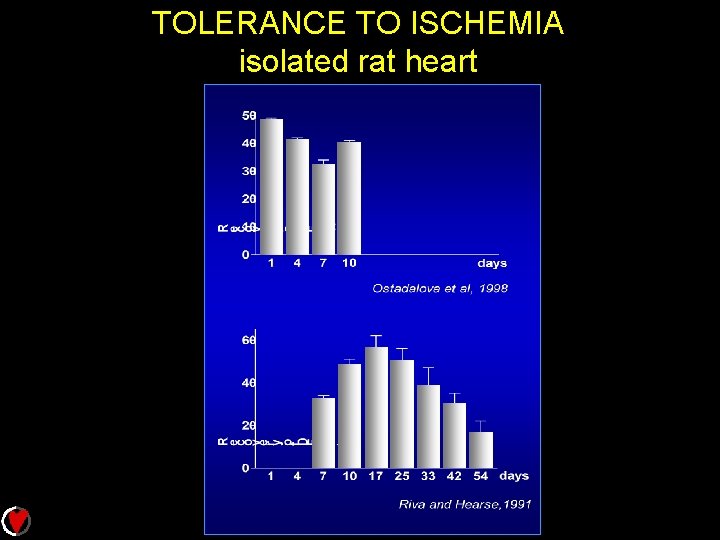
TOLERANCE TO ISCHEMIA isolated rat heart
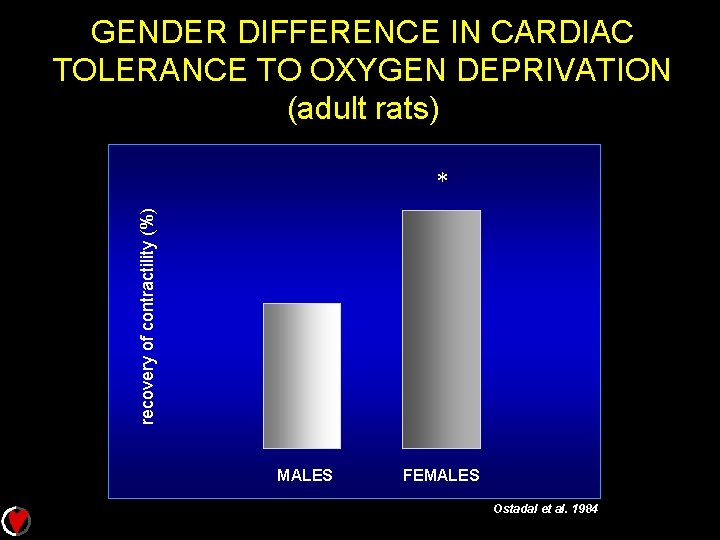
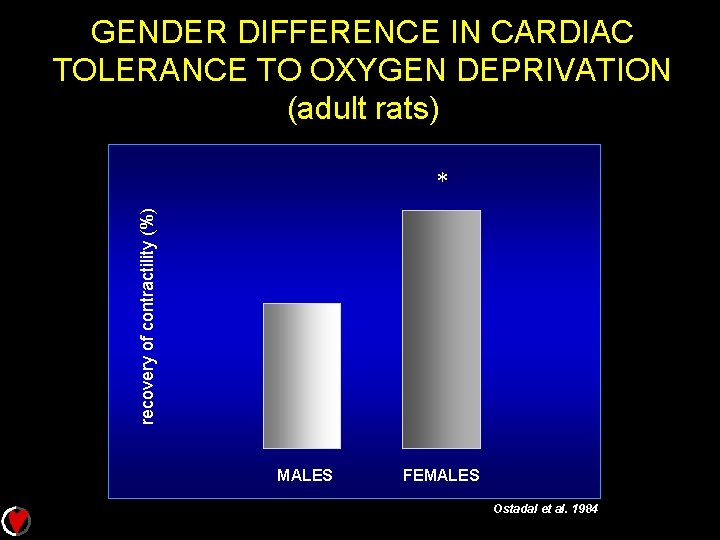
GENDER DIFFERENCE IN CARDIAC TOLERANCE TO OXYGEN DEPRIVATION (adult rats) recovery of contractility (%) * MALES FEMALES Ostadal et al. 1984
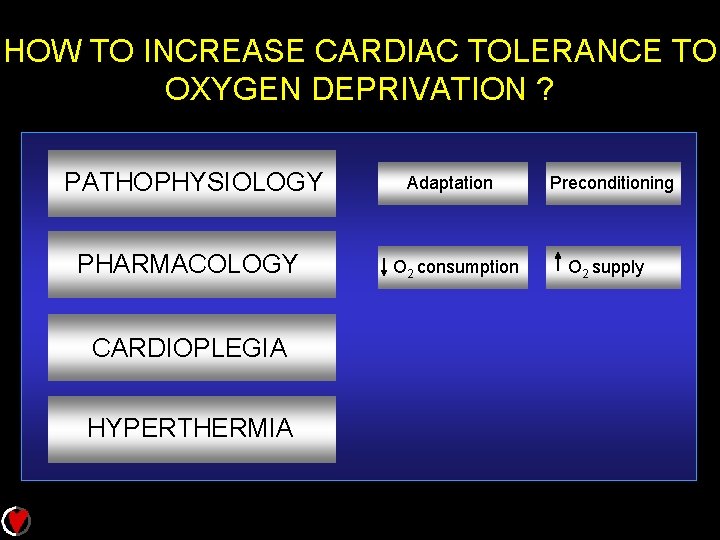
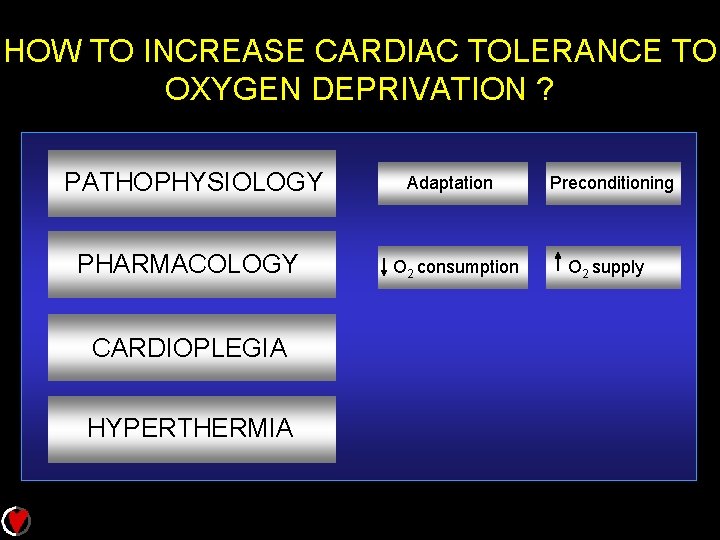
HOW TO INCREASE CARDIAC TOLERANCE TO OXYGEN DEPRIVATION ? PATHOPHYSIOLOGY PHARMACOLOGY CARDIOPLEGIA HYPERTHERMIA Adaptation O 2 consumption Preconditioning O 2 supply
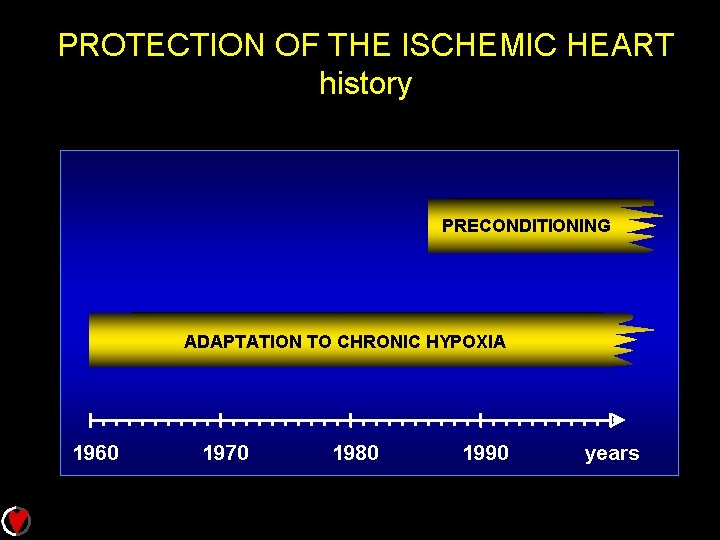
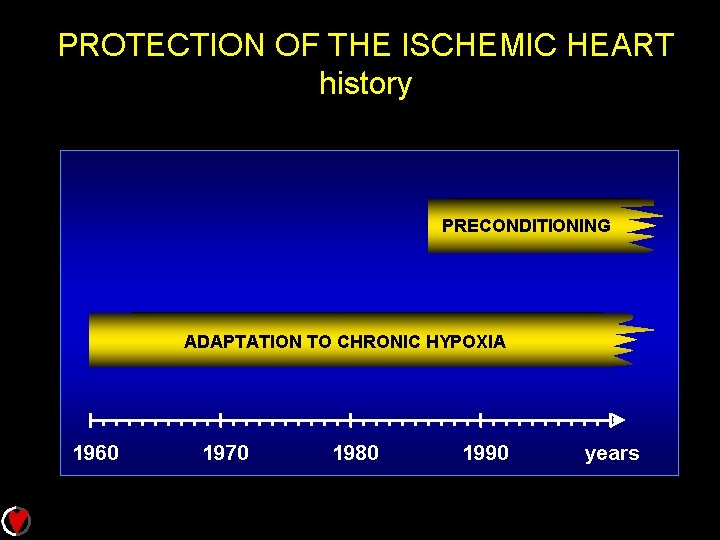
PROTECTION OF THE ISCHEMIC HEART history PRECONDITIONING ADAPTATION TO CHRONIC HYPOXIA 1960 1970 1980 1990 years
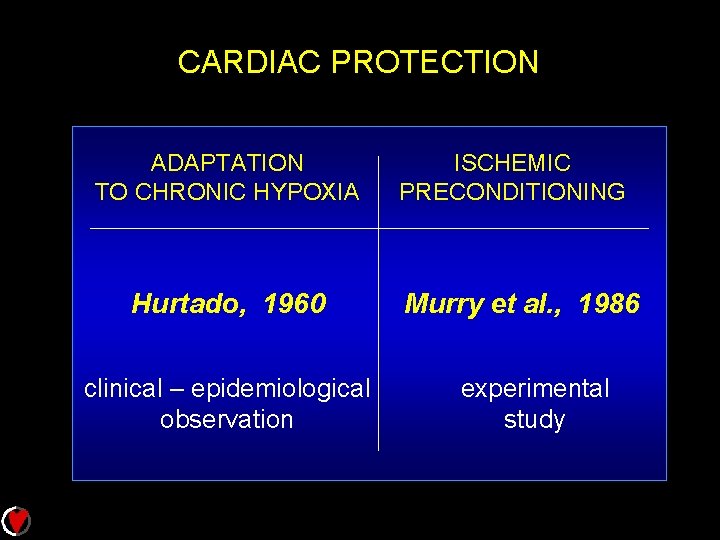
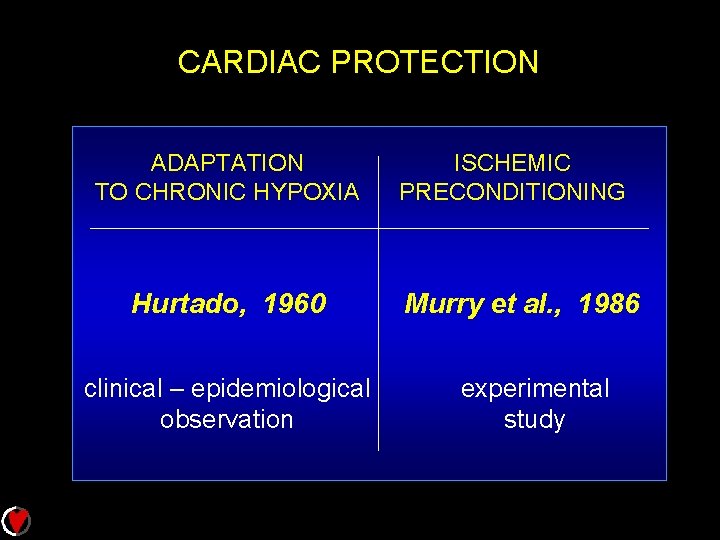
CARDIAC PROTECTION ADAPTATION TO CHRONIC HYPOXIA Hurtado, 1960 clinical – epidemiological observation ISCHEMIC PRECONDITIONING Murry et al. , 1986 experimental study

TYPICAL PRECONDITIONING PROTOCOL Sustained test occlusion Pr ec o st ndi im tio ul ni us ng ea s in ure pe fa rfu rc me t s nt si on ize of Re Re pe rfu si on M
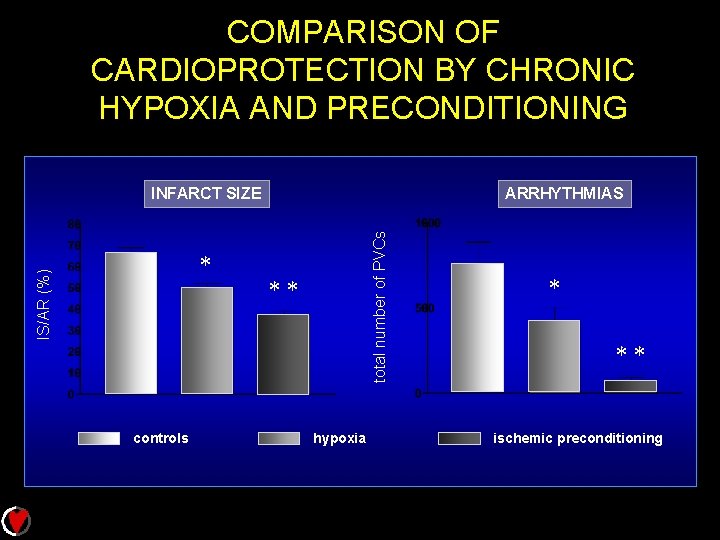
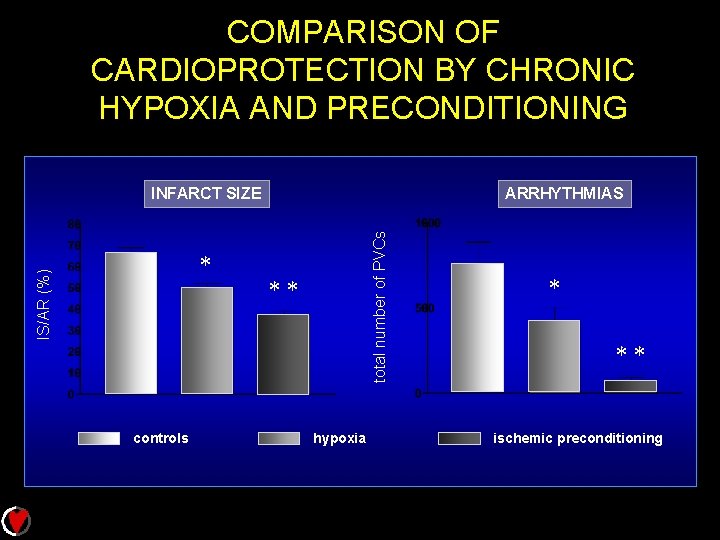
COMPARISON OF CARDIOPROTECTION BY CHRONIC HYPOXIA AND PRECONDITIONING IS/AR (%) * controls ARRHYTHMIAS total number of PVCs INFARCT SIZE ** hypoxia * ** ischemic preconditioning
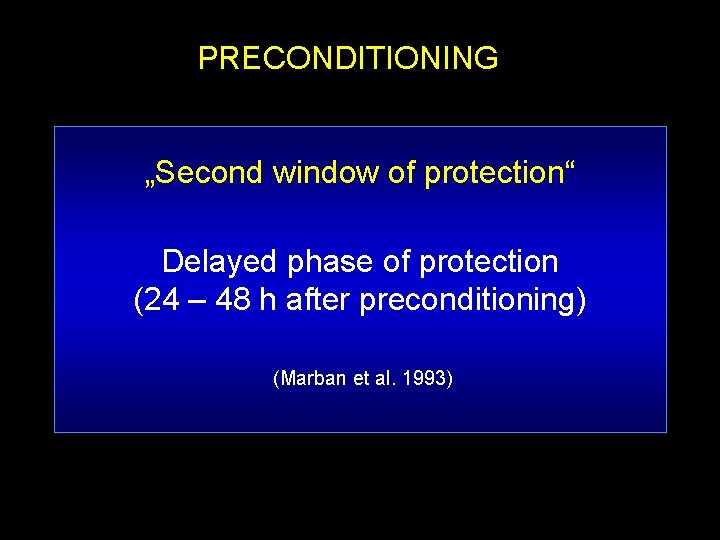
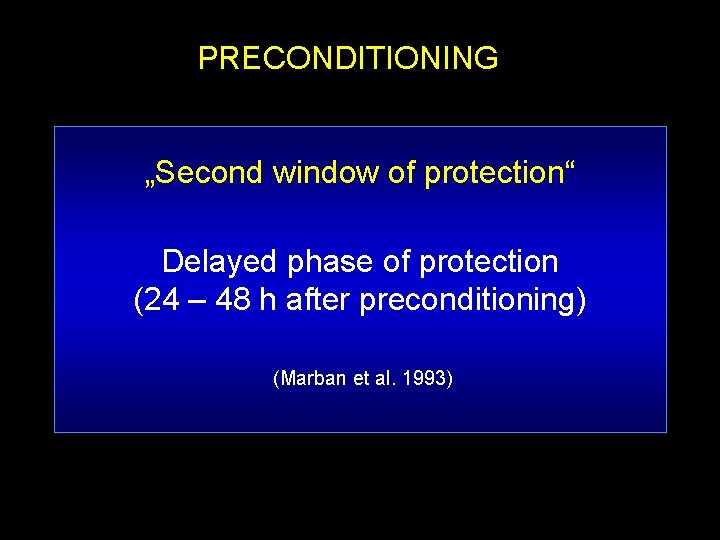
PRECONDITIONING „Second window of protection“ Delayed phase of protection (24 – 48 h after preconditioning) (Marban et al. 1993)

ADAPTATION TO CHRONIC HYPOXIA Protective effects: infarct size recovery of contractile function arrhythmias hypertension Adverse effects: pulmonary hypertension RV hypertrophy
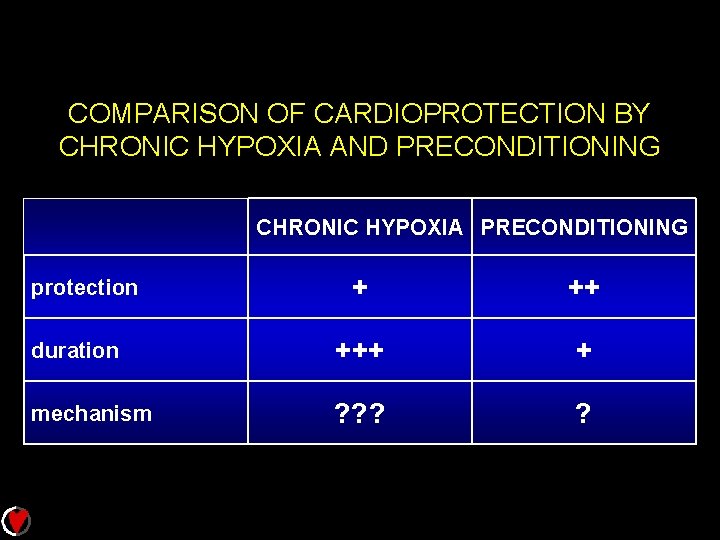
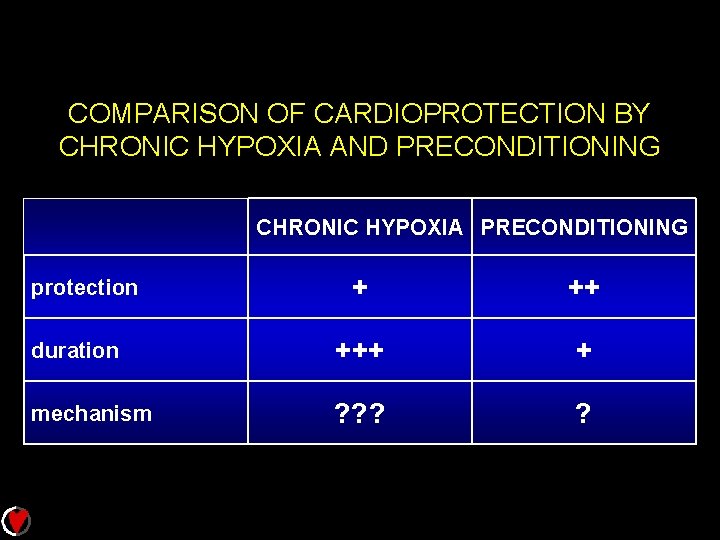
COMPARISON OF CARDIOPROTECTION BY CHRONIC HYPOXIA AND PRECONDITIONING CHRONIC HYPOXIA PRECONDITIONING + ++ duration +++ + mechanism ? ? ? ? protection
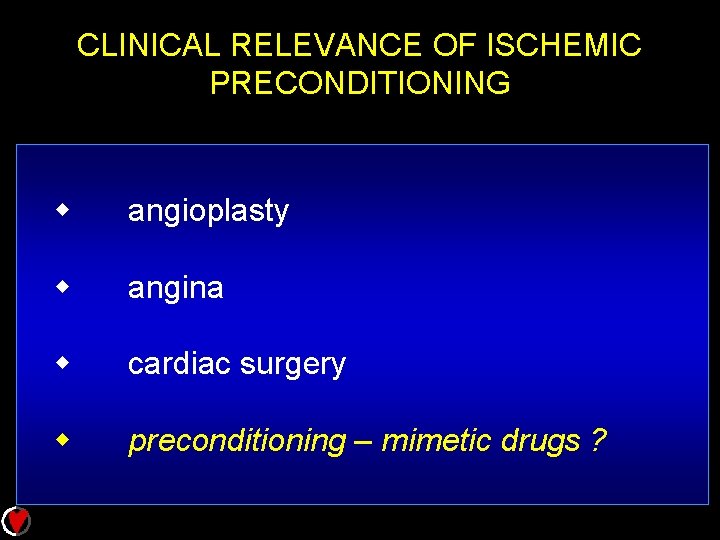
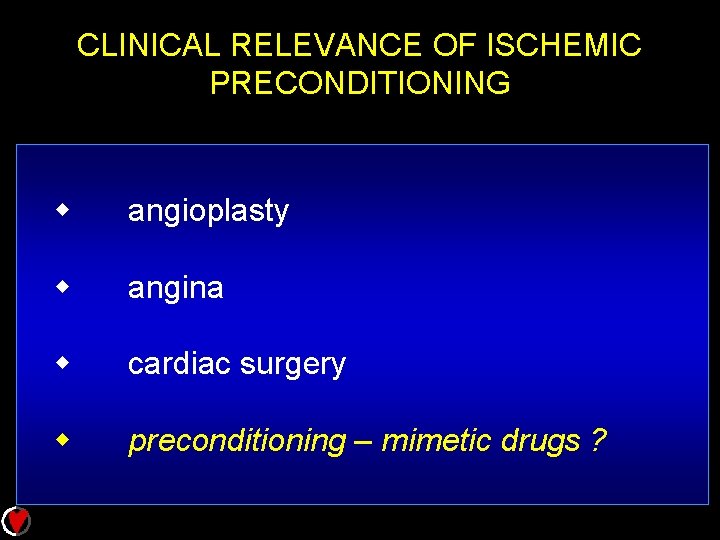
CLINICAL RELEVANCE OF ISCHEMIC PRECONDITIONING w angioplasty w angina w cardiac surgery w preconditioning – mimetic drugs ?
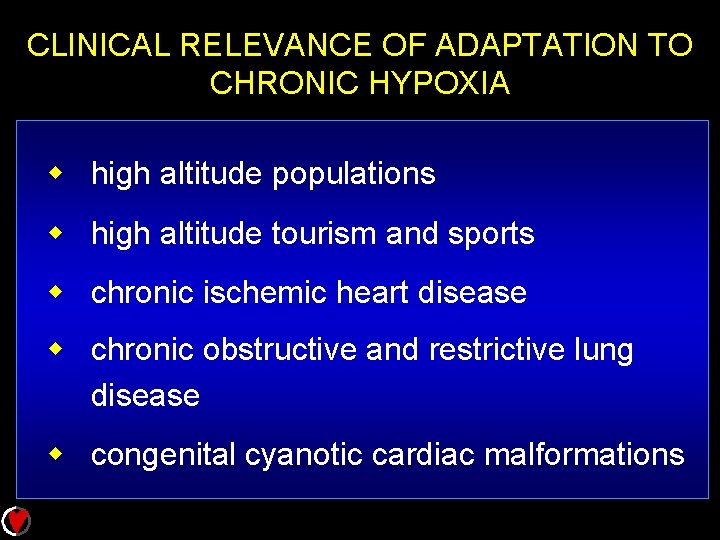
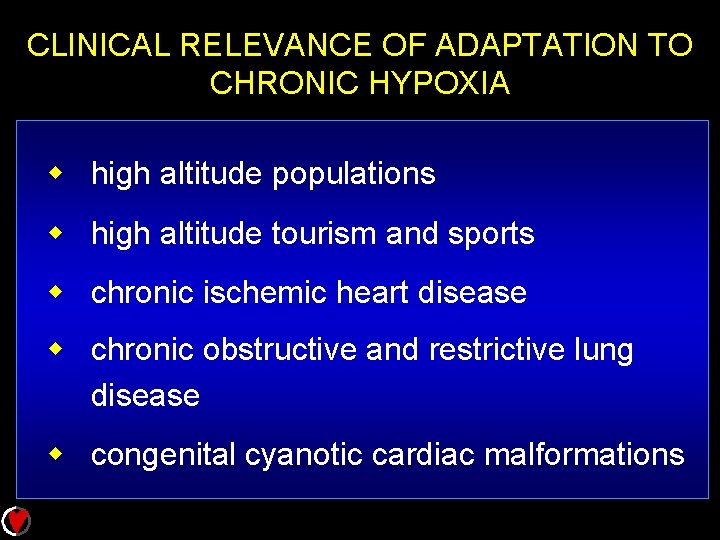
CLINICAL RELEVANCE OF ADAPTATION TO CHRONIC HYPOXIA w high altitude populations w high altitude tourism and sports w chronic ischemic heart disease w chronic obstructive and restrictive lung disease w congenital cyanotic cardiac malformations
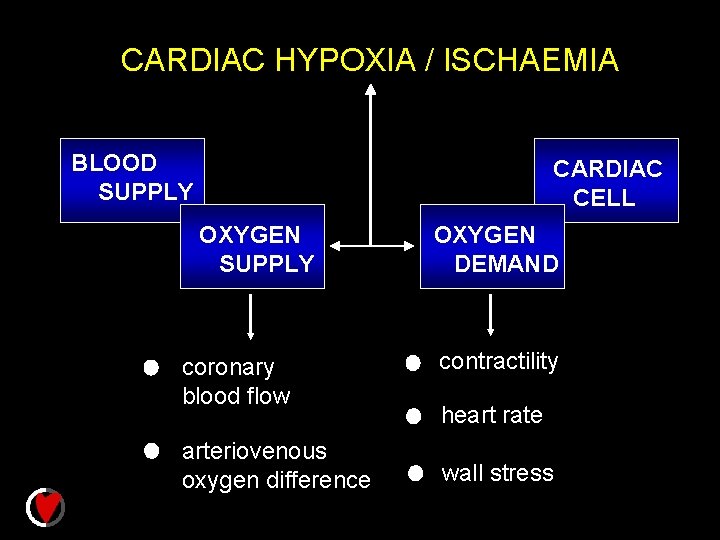
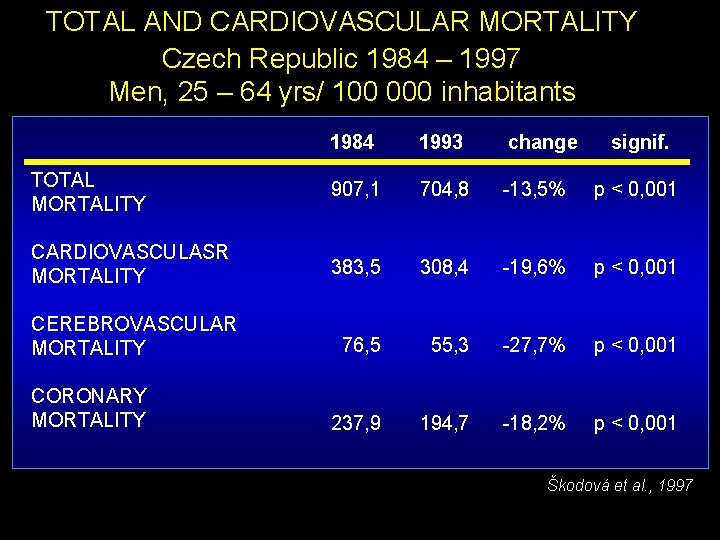
CARDIAC HYPOXIA / ISCHAEMIA BLOOD SUPPLY CARDIAC CELL OXYGEN SUPPLY coronary blood flow arteriovenous oxygen difference OXYGEN DEMAND contractility heart rate wall stress
 Intentional and unintentional injury
Intentional and unintentional injury Cdsl tpin
Cdsl tpin Attributable mortality
Attributable mortality Nir ap human geography
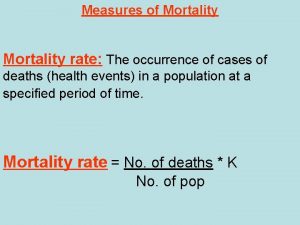
Nir ap human geography Disease specific mortality rate formula
Disease specific mortality rate formula Miracle plays characteristics
Miracle plays characteristics Death rate formula
Death rate formula Neonatal mortality rate formula
Neonatal mortality rate formula Prevalence rate formula
Prevalence rate formula Imr formula
Imr formula Infant mortality rate formula
Infant mortality rate formula Indirect age adjustment
Indirect age adjustment Flacker score
Flacker score Mortality vs morbidity
Mortality vs morbidity Continuous mortality investigation
Continuous mortality investigation Perinatal mortality rate
Perinatal mortality rate Crude death rate adalah
Crude death rate adalah Age adjusted mortality rate definition
Age adjusted mortality rate definition Health continuum pdhpe
Health continuum pdhpe Theme of mortality
Theme of mortality Infant mortality rate formula
Infant mortality rate formula Rumus case fatality rate
Rumus case fatality rate Infant mortality rate formula
Infant mortality rate formula An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Prinso poisoning
Prinso poisoning Methanol poisoning
Methanol poisoning Dh-mo-1
Dh-mo-1 Dimethoate poisoning
Dimethoate poisoning Infectious mononucleosis
Infectious mononucleosis Foodafactoflife
Foodafactoflife Lahari paladugu
Lahari paladugu Poisoning the well
Poisoning the well What is oxygen poisoning
What is oxygen poisoning Seo poisoning wikipedia
Seo poisoning wikipedia Nero lead poisoning
Nero lead poisoning