Morphology The functional unit of the thyroid gland

- Slides: 12

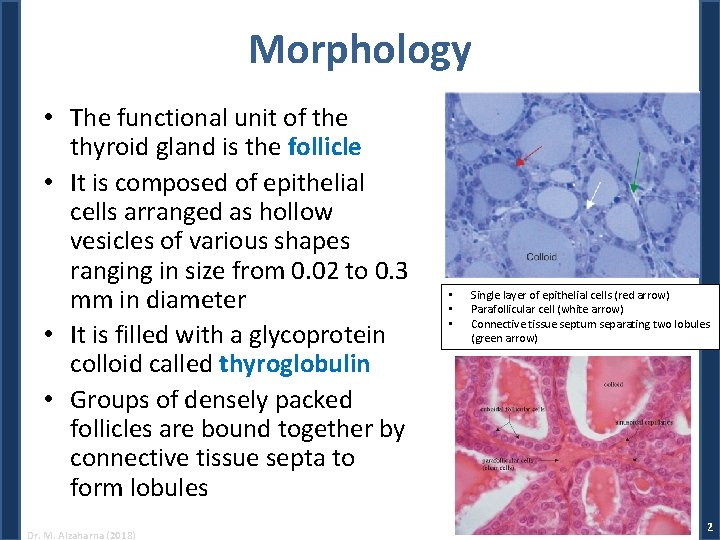
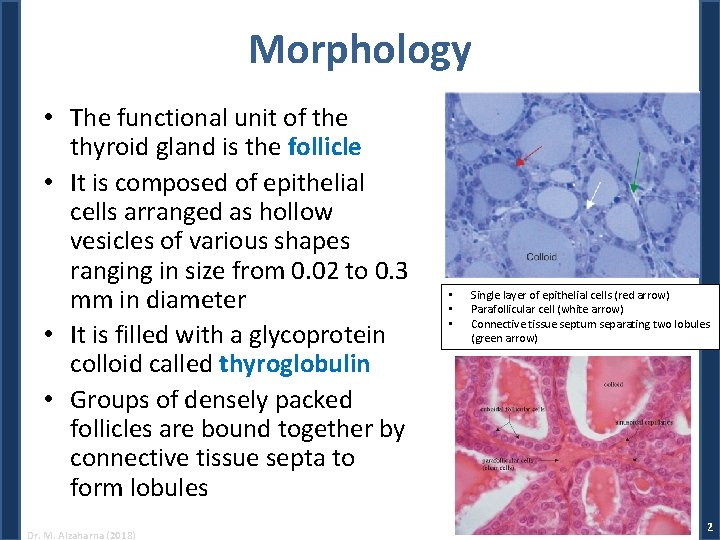
Morphology • The functional unit of the thyroid gland is the follicle • It is composed of epithelial cells arranged as hollow vesicles of various shapes ranging in size from 0. 02 to 0. 3 mm in diameter • It is filled with a glycoprotein colloid called thyroglobulin • Groups of densely packed follicles are bound together by connective tissue septa to form lobules Dr. M. Alzaharna (2018) • • • Single layer of epithelial cells (red arrow) Parafollicular cell (white arrow) Connective tissue septum separating two lobules (green arrow) 2
• Secretory cells of the thyroid gland are of two types: – Follicular cells, which produce the classical thyroid hormones, thyroxine and triiodothyronine – Parafollicular, or C cells, are located between the follicles and produce the polypeptide hormone calcitonin Dr. M. Alzaharna (2018) 3
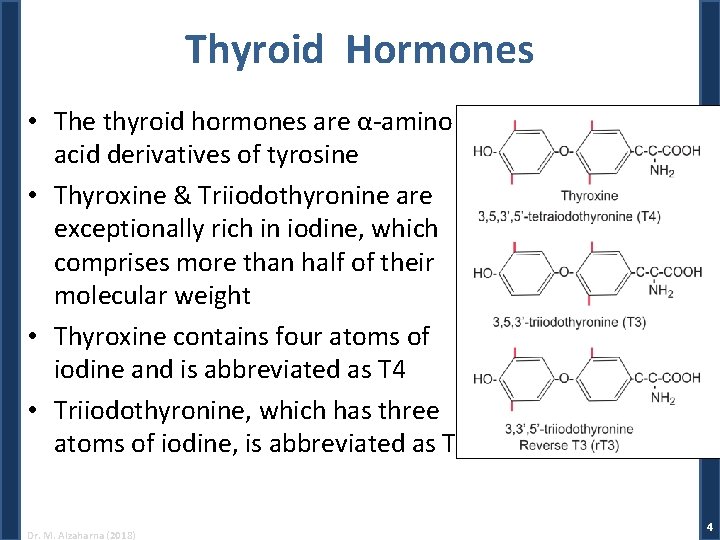
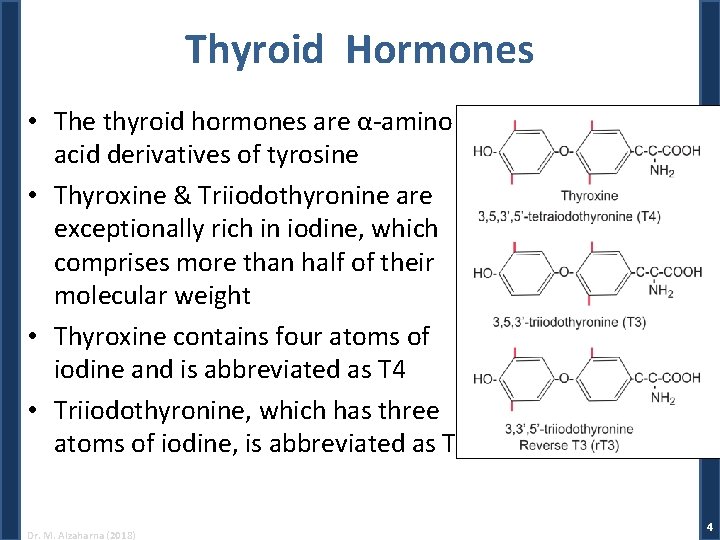
Thyroid Hormones • The thyroid hormones are α-amino acid derivatives of tyrosine • Thyroxine & Triiodothyronine are exceptionally rich in iodine, which comprises more than half of their molecular weight • Thyroxine contains four atoms of iodine and is abbreviated as T 4 • Triiodothyronine, which has three atoms of iodine, is abbreviated as T 3 Dr. M. Alzaharna (2018) 4
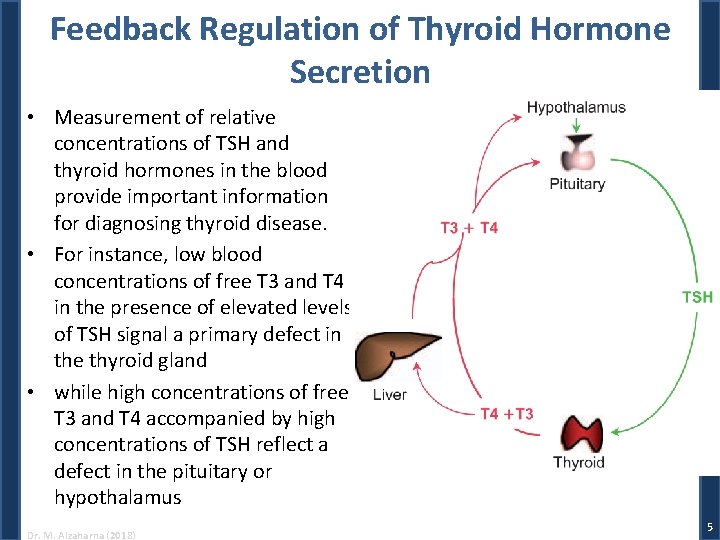
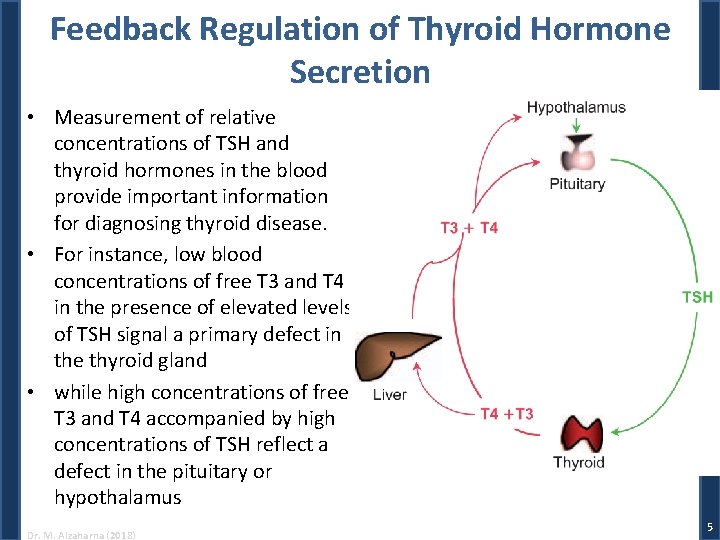
Feedback Regulation of Thyroid Hormone Secretion • Measurement of relative concentrations of TSH and thyroid hormones in the blood provide important information for diagnosing thyroid disease. • For instance, low blood concentrations of free T 3 and T 4 in the presence of elevated levels of TSH signal a primary defect in the thyroid gland • while high concentrations of free T 3 and T 4 accompanied by high concentrations of TSH reflect a defect in the pituitary or hypothalamus Dr. M. Alzaharna (2018) 5
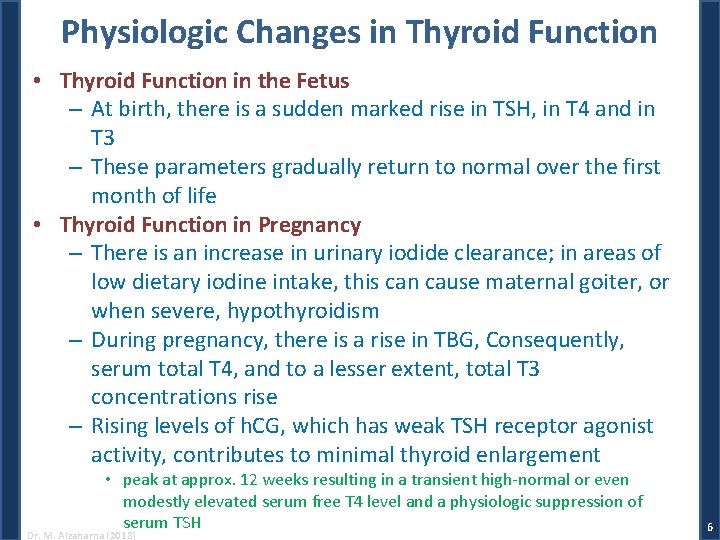
Physiologic Changes in Thyroid Function • Thyroid Function in the Fetus – At birth, there is a sudden marked rise in TSH, in T 4 and in T 3 – These parameters gradually return to normal over the first month of life • Thyroid Function in Pregnancy – There is an increase in urinary iodide clearance; in areas of low dietary iodine intake, this can cause maternal goiter, or when severe, hypothyroidism – During pregnancy, there is a rise in TBG, Consequently, serum total T 4, and to a lesser extent, total T 3 concentrations rise – Rising levels of h. CG, which has weak TSH receptor agonist activity, contributes to minimal thyroid enlargement • peak at approx. 12 weeks resulting in a transient high-normal or even modestly elevated serum free T 4 level and a physiologic suppression of serum TSH Dr. M. Alzaharna (2018) 6
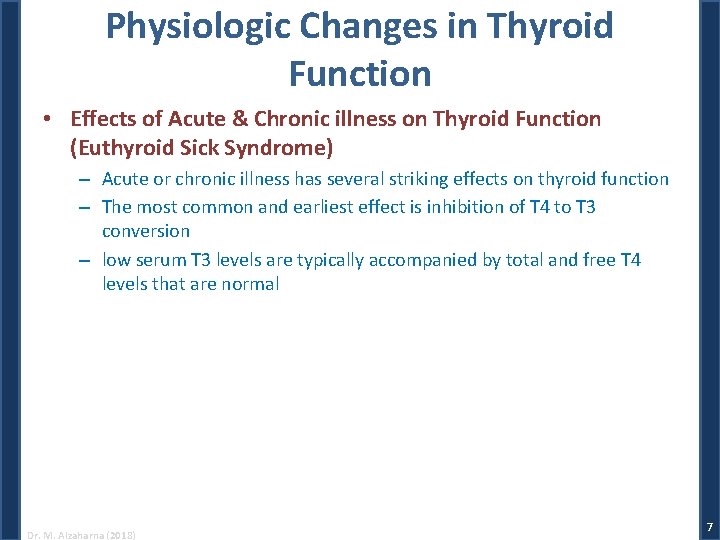
Physiologic Changes in Thyroid Function • Effects of Acute & Chronic illness on Thyroid Function (Euthyroid Sick Syndrome) – Acute or chronic illness has several striking effects on thyroid function – The most common and earliest effect is inhibition of T 4 to T 3 conversion – low serum T 3 levels are typically accompanied by total and free T 4 levels that are normal Dr. M. Alzaharna (2018) 7
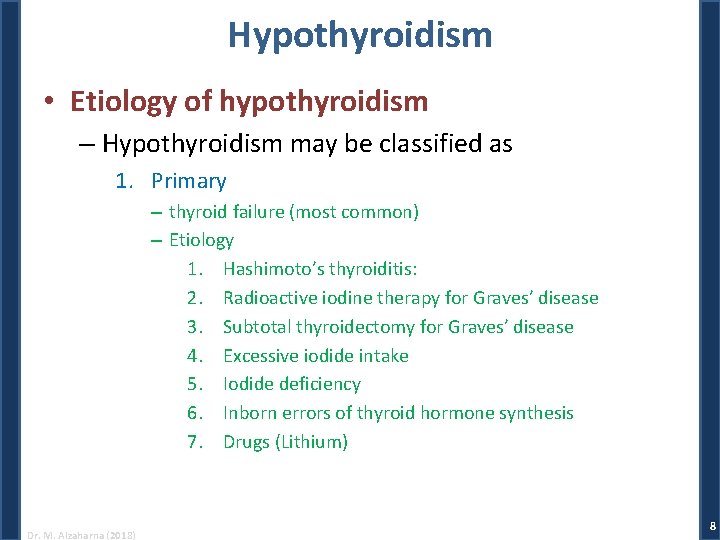
Hypothyroidism • Etiology of hypothyroidism – Hypothyroidism may be classified as 1. Primary – thyroid failure (most common) – Etiology 1. Hashimoto’s thyroiditis: 2. Radioactive iodine therapy for Graves’ disease 3. Subtotal thyroidectomy for Graves’ disease 4. Excessive iodide intake 5. Iodide deficiency 6. Inborn errors of thyroid hormone synthesis 7. Drugs (Lithium) Dr. M. Alzaharna (2018) 8
2. Secondary – due to pituitary TSH deficiency 3. Tertiary – due to hypothalamic deficiency of TRH 4. Peripheral resistance to the action of thyroid hormones Dr. M. Alzaharna (2018) 9
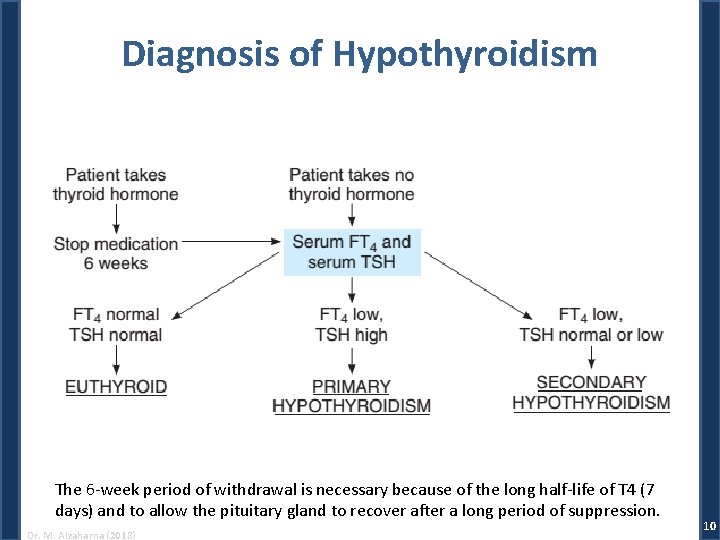
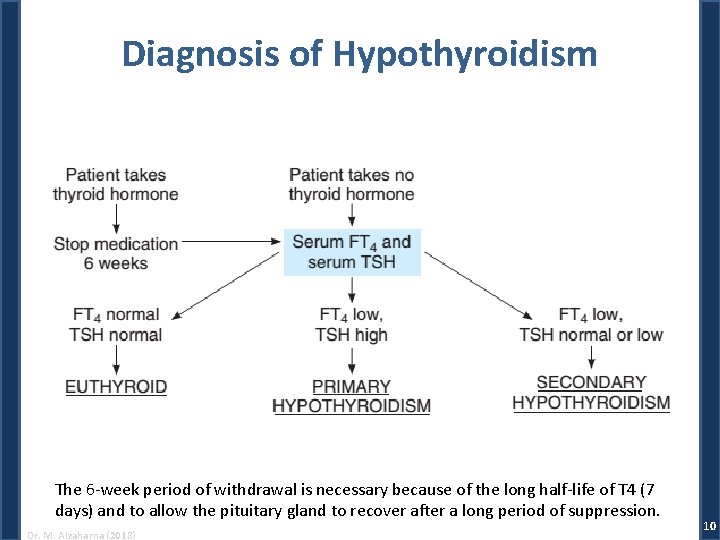
Diagnosis of Hypothyroidism The 6 -week period of withdrawal is necessary because of the long half-life of T 4 (7 days) and to allow the pituitary gland to recover after a long period of suppression. Dr. M. Alzaharna (2018) 10
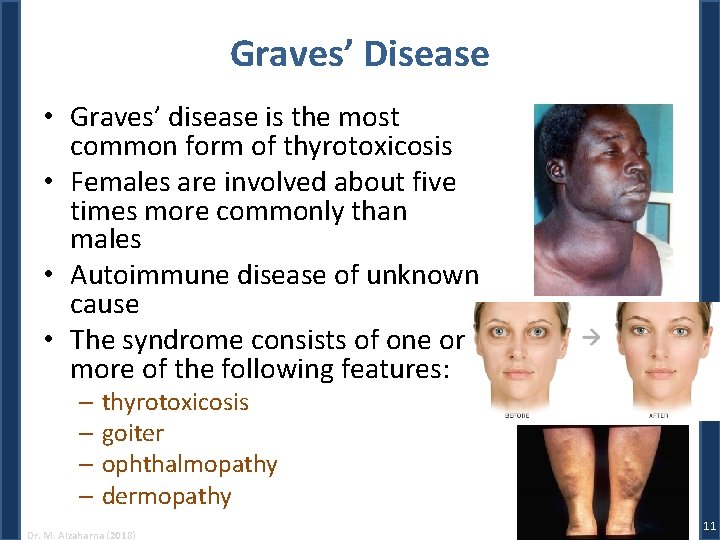
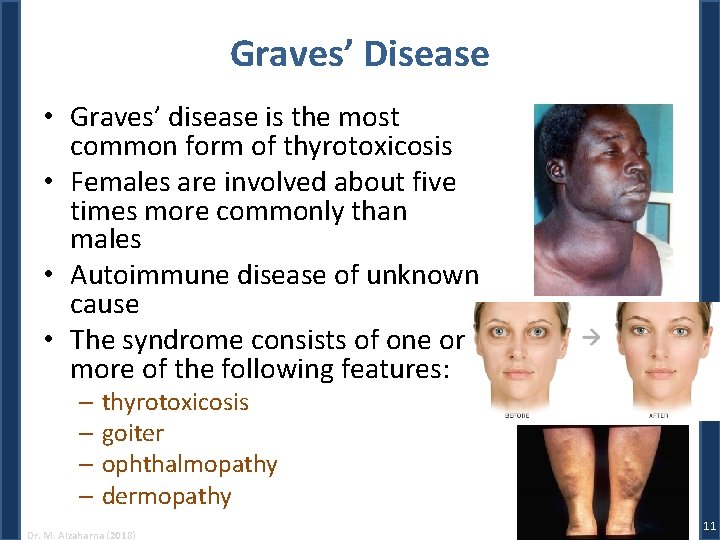
Graves’ Disease • Graves’ disease is the most common form of thyrotoxicosis • Females are involved about five times more commonly than males • Autoimmune disease of unknown cause • The syndrome consists of one or more of the following features: – thyrotoxicosis – goiter – ophthalmopathy – dermopathy Dr. M. Alzaharna (2018) 11
Treatment of Graves’ Disease • Although autoimmune mechanisms are responsible for the syndrome of Graves’ disease, management has been largely directed toward controlling the hyperthyroidism • Three good methods are available: – Antithyroid Drug therapy • inhibiting TPO-mediated iodination of thyroglobulin – Surgery • Partial or total thyroidectomy – and radioactive iodine therapy (131 I) • destroys thyroid cells Dr. M. Alzaharna (2018) 12