Mood Disorders Mental Health vs Mental Illness Maslow














- Slides: 66

Mood Disorders Mental Health vs Mental Illness
Maslow • Identified self actualization as being “psychologically healthy, fully human, highly evolved, and fully mature. ” • Appropriate perception of reality • Ability to accept oneself and others • Ability to focus (concentrate) and problem solve • Ability to have satisfactory interpersonal relationships
• Creativeness • Desire for a certain amount of privacy and ability to detach if needed • Sense of ethics • Creativity • A degree of conformance
Jahoda • Positive attitude • Growth, development, and the Ability to Achieve Self-Actualization • Integration • Autonomy • Perception of reality • Environmental mastery
Locus of Control • External • Internal

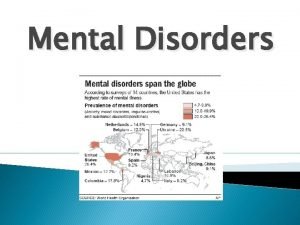
Mental Health Viewed as the successful adaptation to stressors from the internal or external environment, evidenced by thoughts, feelings, and behaviors that are age-appropriate and congruent with local and cultural norms.

Mental Illness • Universal concept is difficult because of the influence of cultural factors. • Maladaptive responses to stressors from the internal or external environment, evidenced by :
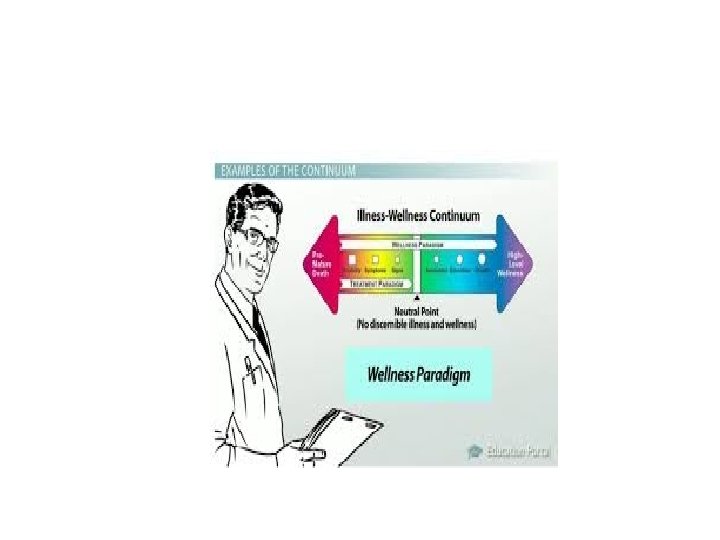
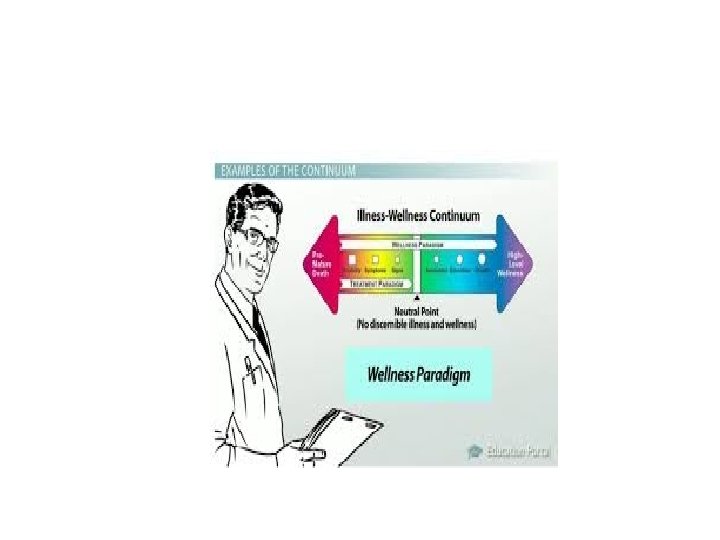
Anxiety and Grief • Two major primary responses to stress • Continuum of health to illness Mild anxiety or feelings of sadness or life’s everyday disappointments-use coping mechanisms such as smoking, talking it out
Moderate anxiety-add in defense mechanisms (such as denial) and/or psychophysiological responses (such as headaches, ulcers). Also see Neurotic responses, dysthymia (non psychotic depression) Severe anxiety to panic- add in psychoneurotic responses such as obsessions, amnesia. Can even become delusional (psychotic)
Depression
Non psychotic mood disorders • An occasional bout with the blues Short lived, normal, utilized learned coping skills. Transient depression –life’s everyday disappointments Seasonal depression
• Grief Normal response to losses perceived as important to the individual. What might cause grief in one person cause little or no sadness in another.
• Cyclothymia

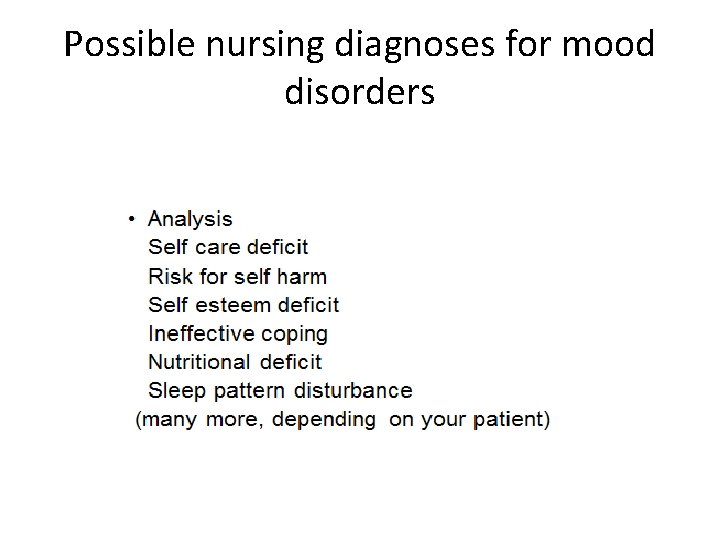
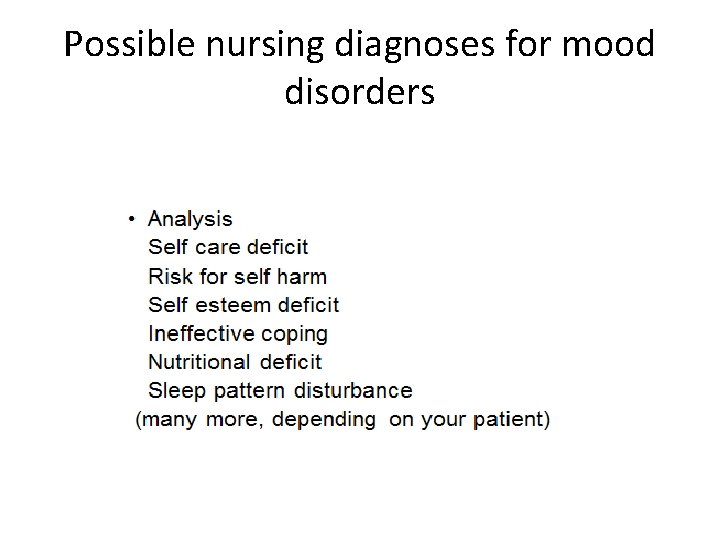
Possible nursing diagnoses for mood disorders

• Mild depression May experience anorexia or overeating, insomnia or hypersomnia, headaches, backaches, chest pain, tearfulness, blaming others, guilt, anger

• Moderate depression Signs and Symptoms:
• Severe Depression • Major Depression • Will learn more about this in Soph II but we will have a brief description
Affect: Blunted: significantly reduced intensity of emotional expression Flat: absent or nearly absent affective expression Inappropriate: expression does not reflect the content of speech or ideation Labile: varied, rapid, abrupt shifts in affective expression
Bipolar disorder • Theory -Etiology is unclear. Most believe that biological and psychosocial factors come into play.
• Affect-
• May or may not have delusions/hallucinations. • Delusions-many times grandiosity or paranoia Grandiosity is an exaggerated sense of self importance, power, or status. Employed to reduce feelings of insecurity and increases feeling of power. • Hallucinations
Interventions • Accurate assessment of s/sx • Develop a trusting relationship, encourage client to express feelings openly • Encourage them to express anger (do not become defensive) • Participation in large motor activities just as physical exercises, volleyball, punching bag help discharge pent-up anger

Assist in problem solving Encourage support groups Intake and output Teach effective communication (I message, etc) • Provide helpful measures to promote sleep • •
• Watch for suicidal gestures or ideation • Suicide watch if nurse feels it is warranted (usually 1: 1 to closely monitor patient) Remember that when in deepest depression, patients aren’t as likely to commit suicide because of decreased energy. It’s when they start to feel more energy that they are more likely to harm self. But be aware IT CAN HAPPEN ANYTIME.
• Clients are usually very withdrawn when depressed with little energy. We don’t want to overtax, but we want them to participate as soon as possible. Maybe have to walk them to their activity. • Newly admitted depressed patients do better with one on one interaction, then progressed to socialization with others/groups.
Therapies • Cognitive therapy-individual is taught about thought distortions (individual and/or group) • Group therapy-used once acute phase of depression passed. Peer support provides feeling of security. Yalom’s curative factors • Family therapy- aimed at restoring family functioning
• Behavioral therapy • Light therapy • ECT • Psychopharmacology
Medications for depression Antidepressants • • Tricyclics Monoamine Oxidase Inhibitors Selective Serotonin Reuptake Inhibitors Others

Antidepressants may cause sedation at first. But over time, the patient’s body gets used to the medication, and the patient is not sleepy from taking it. Many antidepressant will lower the seizure threshold. Many cause anticholinergic side effects.

• Tricyclic antidepressants Blocks the absorption (reuptake) of the neurotransmitters serotonin and norepinephrine, making more of these chemicals available in the brains. Helps brain cells send and receive messages, which in turn, boosts mood. There is also a drug that is a tetracyclic that you may see (Maprotiline)
• Side effects of tricyclics: Anticholinergic effects (dry mouth, urinary retention) Increased appetite Drop in blood pressure when moving to a standing position. Increased sweating Other side effects
• Interactions Taking a tricyclic with other drugs can cause many drug interactions. Always note this when you look up and read about an antidepressant. For example: when used with phenothiazines (antipsychotic drugs) risk for seizure increases. .
• Decreased or increased effects of other drugs can occur. • Example-increased anticoagulation effects may occur with dicumarol. (So patient could have bleeding)
• Some names you might see Amitriptyline-Elavil Amoxapine Imipramine-(Tofranil) Nortriptyline-Pamelor Tricyclic antidepressants are ordered per their generic name at this time.
• Monoamine Oxidase Inhibitors Major problem-Interaction with tyramine-rich foods and certain medication that can result in hypertensive crisis. Names: Isoboxazid (Marplan), Tranylcypromine (Parnate), and Phenelzine (Nardil)
• Tyramine Rich Foods: • Sympathomimetics
• SSRI’s Citalopram (Celexa) Escitalopram (Lexapro) Fluoxetine (Prozac) Paroxetine (Paxil) Sertraline (Zoloft)
• SSRI’s Action: Decreased serotonergic neurotransmission has been proposed to play a key role in depression. Prozac was the first of a class of drugs that acted “selectively” on serotonin. All SSRIs inhibit the reuptake of serotonin by blocking its transport into the presynaptic neuron, which in turn increases the concentration of synaptic serotonin.
• Side effects of SSRIs Headache, anxiety, insomnia, transient nausea and vomiting, diarrhea. Sedation may occur. See chapter 11 for other side effects.

• Norepinephrine Dopamine Reuptake Inhibitors Bupropion (Wellbutrin) inhibits reuptake of norepinephrine, serotonin, and dopamine. Some have experienced anxiety, insomnia, appetite suppression. A few have experienced hallucinations and delusions. Lowers seizure threshold. (So not good to give to head injury pt)
Lithium • Once dosage adjusted, don’t change salt intake. • Lithium levels • Drink plenty of fluids • Lithium is prescribed as a mood stabilizer for the treatment of bipolar disorder. It acts to help control the associated mania, hypomania, depression and psychosis.

• Lithium is formally approved to treat manic episodes of bipolar disorder when symptoms such as grandiosity, racing thoughts, hypersexuality, delusions, hallucinations, and decreased need for sleep appear. • However, it has also been shown to help with depressive symptoms • Some research has shown that lithium can be effective in treating unipolar depression when added to one or more other depression medications, so it is sometimes prescribed for this use.

• • Warnings About Lithium There are several important warnings for people taking lithium. These include: • Serum blood level must be monitored regularly. Lithium can be toxic if this gets too high. Symptoms of lithium toxicity include diarrhea, vomiting, tremor, mild problems walking, drowsiness, or muscular weakness. Report such symptoms to a doctor immediately. • There is a danger of a condition called lithium nephrogenic diabetes insipidus (NDI). If you notice that you are excessively thirsty and are urinating too often, check with a doctor at once. Precautions When Taking Lithium • Make sure you maintain normal fluid and salt intake when taking lithium. Dehydration or low levels of sodium in the blood may have serious consequences. • Prolonged sweating, diarrhea, or a high fever can cause your tolerance to lithium to decrease and may require medical treatment. Check with your doctor if any of these conditions occurs. • Lithium can cause increased thyroid and parathyroid activity. Your doctor should check blood calcium levels periodically, as these are connected to the workings of the parathyroid gland, as well as for overactive thyroid. Be extremely careful when used with diuretic.
• Serum blood level describes the amount of a given medication present in your blood at the time of testing. Blood serum is the liquid part of the blood that contains no clotting factors or blood cells. • Some medications used to treat bipolar disorder require serum blood level testing. People taking lithium in particular must be tested regularly, as there is a narrow "therapeutic window" for lithium. That means that the difference between a therapeutic level and toxic level can be small in some individuals. . 5 -1. 5 m. Eq/L • Above 1. 5 is considered critical • Other medications that require serum blood level testing include Tegretol (carbamazepine) and Depakote / Depakene (sodium valproate, valproic acid). (These are anti seizure meds but are also used for mood disorders)
Anticonvulsants: ( also used for mood stabilizers) Need blood levels Tegretol (Carbamazepine)-watch for hematologic and hepatic toxicity. Also may have neurotoxic side effects and EKG changes. Sedation is common. Decreases blood levels of doxycycline, theophylline, coumadin, and birth control pills. May aggravate CV disease, so no smoking when on drug. Depakote (divalproex sodium) -Fewer drug interactions than carbamazepine. Neurotin (gabapentin)- Side effect of gait instability. Trileptal-(Oxcarbazepine) -Watch for adverse neurologic events such as speech problems, gait disturbance, fatigue, somnolence, abnormal cooridation.
ECT • Electroconvulsive Therapy • Meds used: Short acting anesthetic Succinylcholine- Muscle relaxant Airway applied Shock applied-seizure must be 25 sec Ventilation Airway removed Confusion when awakes-protect and reorient
Suicide

Risk for suicide Ask the client directly, “Have you thought about killing/harming yourself today”? If yes, do they have a plan. If so, risk is higher that it happens soon. Create a safe environment. No sharps, etc. Short term verbal or written contract with the client that he /she won’t harm self during a specific time period. Have them commit to
Notifying staff if the thought enters their mind. Maintain close observation. Encourage verbalization of honest feelings. Identify community resources/support people, etc. Orient as needed. Spend time with the client. Conveys the message “You are important”.
Signs of possible suicide ideation
Signs/symptoms of suicidal thoughts • • Talking about suicide Obtaining the means to do it Withdrawal Mood swings Preoccupied with death Feeling trapped or hopeless Increased use of drugs or alcohol

• Giving away belongings or getting affairs in order • Changing normal routine, including eating or sleeping patterns • Doing risky or self destructive things • Saying goodbye to people • Personality changes or being severely agitated
• What do you do when a client is suicidal? • If a patient says he’s thinking of harming himself, ask him if he has a plan. Find out what the plan is/lethality • No suicide contract • 1: 1 • No sharps, eating utensils, strings, ropes, cords, etc.
High risk for suicide • Elderly men (especially if wife dead) • Adolescents taking antidepressants-not as high risk typically as elderly men • Others
Aging Adult • Cognitive Changes: Depression NOT a normal part of aging Contributing factor to social/physical limitations Complicates/interferes with medical tx Decrease in overall happiness-Isolates Increases risk for suicide Often caused by transitions in life and loss
During retirement • Causes of stressors are often: economic, relationships, loss to death of loved ones and friends, changes in routine • Affects spouse, children, grandchildren • Early planning for retirement smooths transition
Psychosocial changes • Correlation with extent of isolation and age • Attitudes/problems that may be seen: “My family no longer needs me” Inability to provide adequate self care May exhibit odd/off putting behaviors If no longer able to drive self or institutionalized, may suffer from not seeing loved ones
Children and Adolescents • Two week period of change of behavior-may indicate an underlying depressive disorder
 Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Stress management jeopardy
Stress management jeopardy Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Mental health disorders
Mental health disorders Mood disorders
Mood disorders Historical views of mental illness psychology ocr
Historical views of mental illness psychology ocr Fair housing act mental illness
Fair housing act mental illness Mental illness in ancient times
Mental illness in ancient times Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Mark rothko mental illness
Mark rothko mental illness Catherine earnshaw mental illness
Catherine earnshaw mental illness Americanization of mental illness
Americanization of mental illness Classification of mental illness
Classification of mental illness Ksi depression
Ksi depression Illness and wellness continuum
Illness and wellness continuum Health illness continuum
Health illness continuum Continuum of health
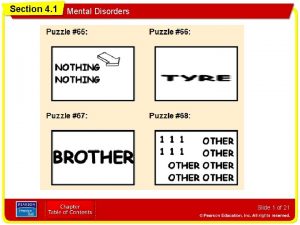
Continuum of health Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Chapter 5 lesson 4 mental and emotional problems
Chapter 5 lesson 4 mental and emotional problems Chapter 5 lesson 2 mental disorders
Chapter 5 lesson 2 mental disorders Health and social care unit 14
Health and social care unit 14 Flinders model of chronic care self-management limitations
Flinders model of chronic care self-management limitations Physical disorders and health psychology
Physical disorders and health psychology Topgunauditschool.com
Topgunauditschool.com Food borne illness poster
Food borne illness poster Na groups and medication
Na groups and medication Foodborne illness vocabulary
Foodborne illness vocabulary Foodborne illness
Foodborne illness Stages of heat illness
Stages of heat illness Chapter 17:12 applying dressings and bandages
Chapter 17:12 applying dressings and bandages 4 examples of sudden illness
4 examples of sudden illness Providing first aid for sudden illness
Providing first aid for sudden illness Chief complaint of patient
Chief complaint of patient Mike mazzalongo illness
Mike mazzalongo illness Trustmark critical illness
Trustmark critical illness Craig jackson psychologist
Craig jackson psychologist Ilness script
Ilness script Illness and wellness continuum
Illness and wellness continuum Accidents/illness of family members
Accidents/illness of family members Thanatos illness artinya
Thanatos illness artinya Hypotyreos typ 2
Hypotyreos typ 2 National minor illness centre
National minor illness centre David mechanic illness behaviour
David mechanic illness behaviour Minor illness definition
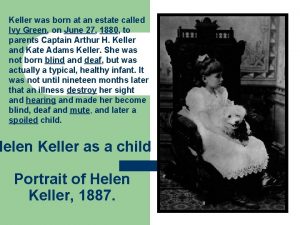
Minor illness definition Helen keller illness
Helen keller illness Illness prevention definition
Illness prevention definition Filipino theories of illness
Filipino theories of illness Ning li cause of death
Ning li cause of death Foodborne illness
Foodborne illness Chief complaint present illness
Chief complaint present illness Eye illness
Eye illness Illness script
Illness script Foodborne illness definition servsafe
Foodborne illness definition servsafe Dextrum genus
Dextrum genus Illness management and recovery worksheet
Illness management and recovery worksheet History of present illness example
History of present illness example Illness script
Illness script Enzo calzaghe illness
Enzo calzaghe illness Improving chronic illness care model
Improving chronic illness care model What does fattom mean
What does fattom mean Frankston ccu
Frankston ccu Lenawee county cmh
Lenawee county cmh Van buren community mental health
Van buren community mental health The intentional use of unfriendly or offensive behavior
The intentional use of unfriendly or offensive behavior Together for mental health
Together for mental health The mental health act 2007 summary
The mental health act 2007 summary