Monitors and Records TSBDE Rules and Regulations 110
Monitors and Records TSBDE Rules and Regulations 110. 3 (f) Clinical Requirements

Patient Evaluation Healthy or medically stable patient (ASA I, II) – Review of history, PE, medications Significant health disability (ASA III, IV) – Documentation of medical consult regarding potential procedure risks

Pre-Procedure Preparation: Informed Consent The patient and/or guardian must be advised of the procedure associated with the delivery of the enteral conscious sedation

(h) Monitoring and Documentation Pre-procedure: patients who have been administered enteral conscious sedation must be monitored during waiting periods prior to operative procedures – Alertness – Responsiveness – Breathing – Skin color

Monitoring: During the Procedure Direct Supervision Oxygenation – Color of mucosa, skin or blood must be continuously evaluated. O 2 saturation must be continuously evaluated by pulse oximetry Ventilation – Chest excursions – Precordial stethoscope

Monitoring: During the Procedure Circulation – Initial blood pressure and pulse – There after as appropriate (10 minutes) Time oriented anesthetic record – – – Vital signs Individual administering drugs Assistants in the room Name of drug Dosage administered Time of administration

Pulse Oximetry Ventilation vs. Oxygenation Arterial vs. venous – Sp. O 2—arterial oxygen saturation Hb. O 2 vs. Hb; absorption of infra-red and red light – Ratio of oxygenated hemoglobin to total hemoglobin (%) Use of supplemental O 2 Limits and alarms

Recovery and Discharge Positive pressure O 2 and suction immediately available Direct continuous supervision until O 2 and circulation stable and patient appropriately responsive for DC Document O 2 circulation, activity, skin color, and level of consciousness appropriate and stable for DC

Written Postoperative Instructions: DC criteria CV function satisfactory Airway patency Patient easily arousable Protective reflexes intact Hydration adequate Patient can talk if applicable Patient can sit unaided if applicable
Written Postoperative Instructions: DC criteria Patient can ambulate if applicable Very young and disabled—return to presedation baseline Responsible individual available Any unusual reactions documented and assisted Dentist must determine that the patient is appropriate for DC

OFFICE EMERGENCIES

Medical Emergencies… Goal is to recognize and treat minor emergencies to prevent a major lifethreatening emergency, and initiate treatment of the life-threatening emergencies awaiting transport to an acute care facility

Prevention… Patient’s baseline – Vital signs – Psychological baseline Important to get vital signs at each appointment to establish a solid baseline Any variations in baseline before sedation need to be evaluated This established baseline gives an accurate record to base any intra-operative changes

Prevention/Warning Signs… Physical Signs – Bradycardia – Tachycardia – Irregular pulse rate – Irregular respiratory rate – Abnormal temperature

Prevention… Mentation Signs – Inappropriate alterations in cognitive function Sensation Signs – Inappropriate Psychological Signs – – – Acute changes Apprehension Agitation

Emergency Equipment… Oxygen Suction – Back-up suction Airway management equipment Drugs AED ?

Office Emergency Drug Kit… Commercial vs. “Home Made” Kits Primary or critical drugs – Vasopressor—Epinephrine – Histamine blocker—Benadryl – Bronchodilator—Albuterol – Carbohydrate—Cake frosting – Antiplatelet—ASA
Office Emergency Drug Kit: Primary or Critical Drugs Anticonvulsant—Benzodiazepine Opioid antagonist—Naloxone Benzodiazepine antagonist—Flumazenil Ammonia capsules ? ?
Complications/Emergencies Recognition and Management
Syncope: Transient Cerebral Hypoxia Signs and Symptoms: – Clammy-sweaty, pale appearance – C/O nausea/vomiting – Rapid pulse – Nervousness – Loss of consciousness – Dilated pupils
Syncope: Management Supine position with feet elevated ABC’s Spirits of Ammonia? Cold compresses to neck and face Monitor vital signs: BP, HR, Sp. O 2

Syncope: Outcome Signs and symptoms resolved Return of normal state of consciousness Return of vital signs to near baseline levels

Orthostatic Hypotension… Cause: syncopal episode secondary to supine vertical position change Management: same as syncope, reposition pt slowly after stable Outcome: signs and symptoms resolve, pt returns to normal state of consciousness and return to baseline vitals

Allergic Reactions… History, History Slow / delayed reactions (mild) Immediate / rapid onset(Anaphylaxis)
Slow / Delayed Reaction… Signs and Symptoms: one hour or days after offending drug allergen administered – Urticaria – Pruritus

Slow / Delayed Allergic Rxn Management… Identify and eliminate the cause Document vital signs (BP, HR, Resp) Treatment of skin lesions: – Systemic: diphenhydramine (Benadryl) 50 mg IV, IM initially. If lesions persist may need po 5 -7 days of Benadryl 25 -50 mg q 68 o
Slow / Delayed Allergic Rxn Management… Treatment of skin lesions – Topical: corticosteroid preparations (Lidex, Kenalog Synalar) Medical consultation with physician or allergist prior to any further treatment

Immediate Rxn (Anaphylaxis) Identification of offending agent and management of signs and symptoms. Signs and symptoms – – – Urticaria, Pruritis, rhinitis Erythema Hypotension and bronchoconstriction Swelling of lips, eyelids, cheeks Constriction of pharynx or larynx with stridor/hoarseness

Anaphylaxis Management… Head down position ABC’s with supplemental O 2 Triad of Drugs: – Epinephrine-IV 1: 1, 000 Adults 0. 3 ml; Child, 0. 01 mg/kg – Antihistamine—diphenhydramine 50 mg IM – Corticosteroid--Solu-Medrol 125 mg IV or Decadron 8 mg IV

Anaphylaxis Management… Activate the EMS Must have stable vital signs for 1 hour prior to DC from acute care facility or office. Medical consultation recommended Rx diphenhydramine 50 mg q 6 -8

Severe Hypoglycemia (Insulin Shock) Normal B. S. : 80 -120 mg/dl – Acute hypoglycemia B. S. < 50 mg/dl Signs and Symptoms – Adrenergic symptoms: sweating, nervousness, tremulousness, faintness, palpitations – CNS manifestations: Visual disturbances, stupor, coma, Sz

Severe Hypoglycemia Management If possible, sugar by mouth If oral route not possible: – IV dextrose 50%(500 mg/cc); 50 cc infused over 2 -3 minutes Activate EMS
Seizures… The most dramatic finding in medicine Belief that trained assistance is necessary Partial seizures – Simple partial Sz—”spells” – Complex partial Grand Mal – Generalized tonic-clonic (90%)
Seizures… Petit Mal – Brief lapse of consciousness 5 -10 seconds No tonic clonic movement Cyclic blinking Seizure prevention – Therapeutic blood levels

Seizures… Management – Prevention of injury – Maintenance of adequate ventilation – Usually self limiting and not requiring intervention – ABC’s

Cerebrovascular Accident… “Brain Attack” Causes – Hemorrhagic – Occlusive Signs and symptoms – Variable—violent to HA, dizziness, vertigo, loss of consciousness Management – ABC’s – Transport to hospital
Chest Pain… Angina Pectoris – History, History – Location of pain Substernal radiating pain Treatment – – – Termination of procedure Position—upright ABC’s Vasodilators and oxygen EMS

Acute Myocardial Infarct… Mangement – ABC’s vs. ABCD – Activate EMS – Oxygen – Nitroglycerin – ASA

AED Automatic External Defibrillation
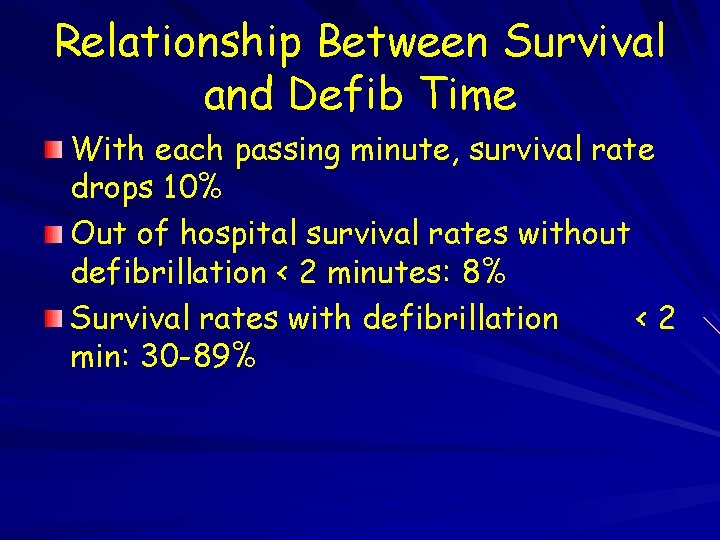
Relationship Between Survival and Defib Time With each passing minute, survival rate drops 10% Out of hospital survival rates without defibrillation < 2 minutes: 8% Survival rates with defibrillation <2 min: 30 -89%
FEATURES OF AED’s Monophasic defibrillators deliver 200 -360 Joules in ONE direction Biphasic defibrillators deliver 150 Joules of energy in TWO directions (Double pass through the heart) Biphasic defibrillators are smaller, lighter, less expensive, and less demanding of batteries, with fewer maintenance requirements
FEATURES OF AED’S Biphasic waveform shocks combined with impedance adjustment or compensation provides equivalent defibrillation success at lower energy levels than those of monophasic shocks Laboratory studies have verified and clinical human studies are supporting
RESTRICTIONS CONTRAINDICATION Not recommended in children under 8 years and/or 90 pounds Not used unless adult patient has NO pulse Not to be used in moving vehicle

AED’s ON THE MARKET Heartstream Forerunner (Agilent Technologies) Physiolcontrol 500 (Medtronics) Surviva. Link Quickstart (Surviva. Link) Laerdal Heart. Start 911 (Laerdal)

Respiratory Distress… Apnea—absence of respiratory movement Hyperventilation – Tachypnea – Treatment Hypoventilation—Pa. CO 2 > 45 torr Hypoxia—deficiency of O 2

Airway Obstruction… Partial vs. complete obstruction – Partial—coughing, wheezing—should allow the coughing to continue – Partial with weak cough reflex—crowing sound, prolonged inspiration In the conscious patient there is a good chance that the object well be swallowed or coughed up
Asthmatic… Mangaement – Termination of procedure – Position—upright – Calming of the patient – ABC’s – Definitive care—administration of bronchodilator
Management of Airway Position—supine Head tilt-chin lift Jaw-thrust maneuver Artificial ventilation

Airway Obstruction Most common cause: tongue and/or epiglottis

Opening the Airway Jaw thrust Head tilt–chin lift
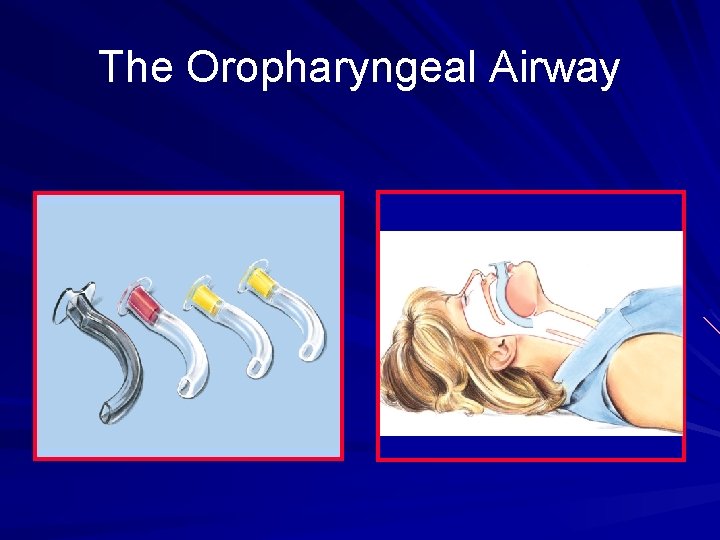
The Oropharyngeal Airway

Malposition of Oropharyngeal Airway Too short
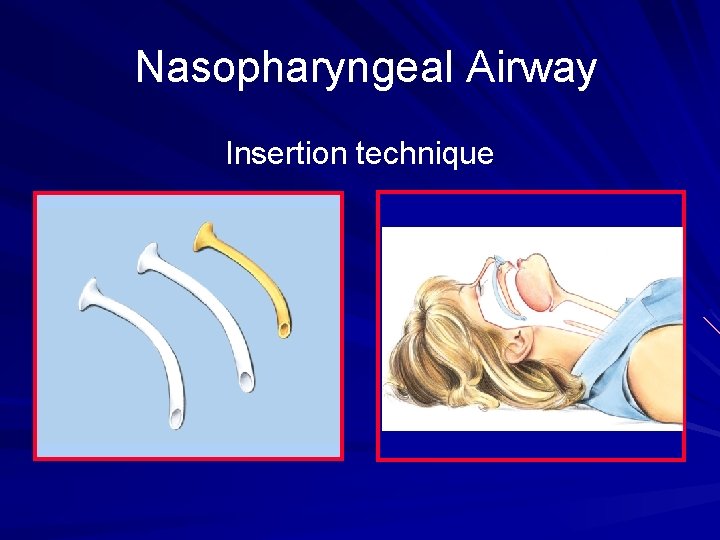
Nasopharyngeal Airway Insertion technique

Bag-Mask Ventilation Key—ventilation volume: “enough to produce obvious chest rise” 1 -Person: difficult, less effective 2 -Person: easier, more effective

Cricoid Pressure Thyroid Cartilage Cricoid

Equipment for Intubation Laryngoscope with several blades Tracheal tubes Malleable stylet 10 -m. L syringe Magill forceps Water-soluble lubricant Suction unit, catheters, and tubing

Aligning Axes of Upper Airway A Mouth A B B Pharynx C C Trachea Extend-the-head-on-neck (“look up”): aligns axis A relative to B Flex-the-neck-on-shoulders (“look down”): aligns axis B relative to C
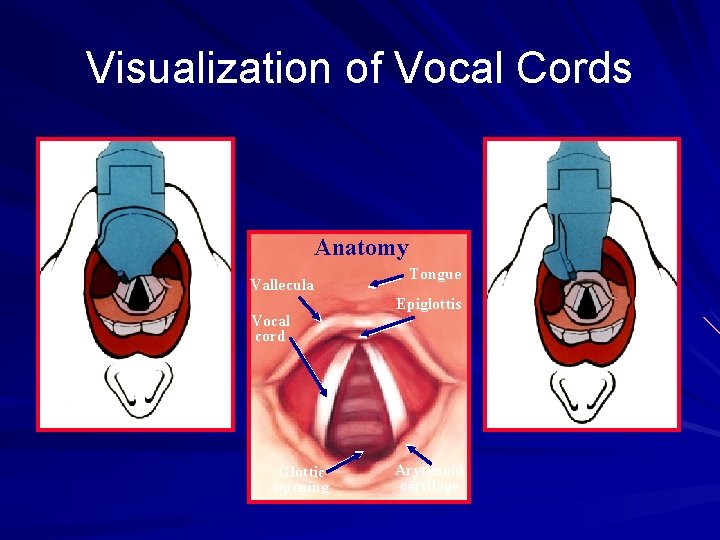
Visualization of Vocal Cords Anatomy Vallecula Vocal cord Glottic opening Tongue Epiglottis Arytenoid cartilage

Esophageal-Tracheal Combitube A = esophageal obturator; ventilation into trachea through side openings = B E C = tracheal tube; ventilation through open end if proximal end inserted in trachea Distal End D = pharyngeal cuff; inflated through catheter = E F = esophageal cuff; inflated through catheter = G H = teeth marker; blindly insert Combitube until marker is at level of teeth A C H Proximal End D B F G
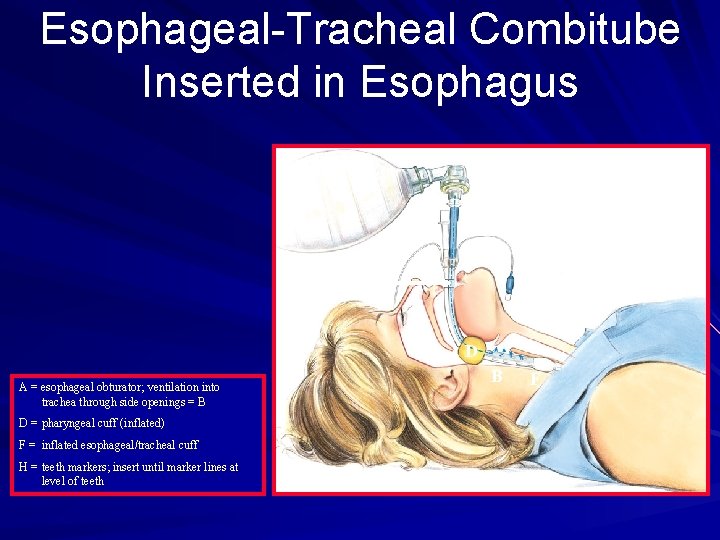
Esophageal-Tracheal Combitube Inserted in Esophagus A H D A = esophageal obturator; ventilation into trachea through side openings = B D = pharyngeal cuff (inflated) F = inflated esophageal/tracheal cuff H = teeth markers; insert until marker lines at level of teeth D B F

Laryngeal Mask Airway (LMA) The LMA is an adjunctive airway that consists of a tube with a cuffed mask-like projection at distal end.

LMA Introduced Through Mouth Into Pharynx
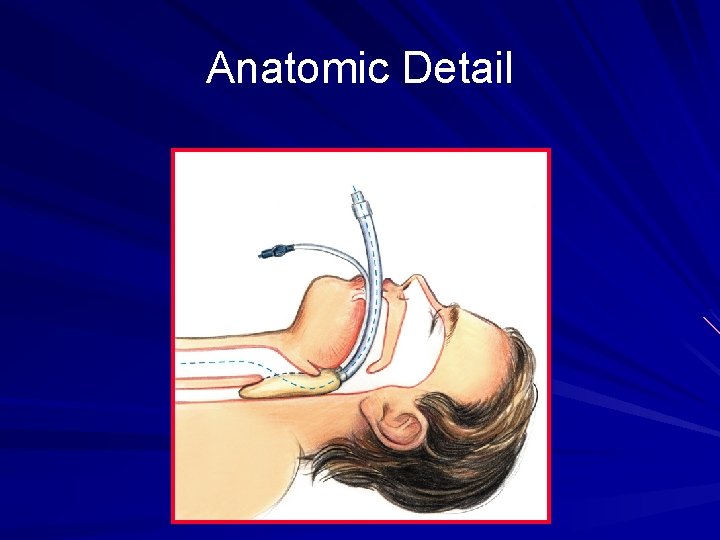
Anatomic Detail
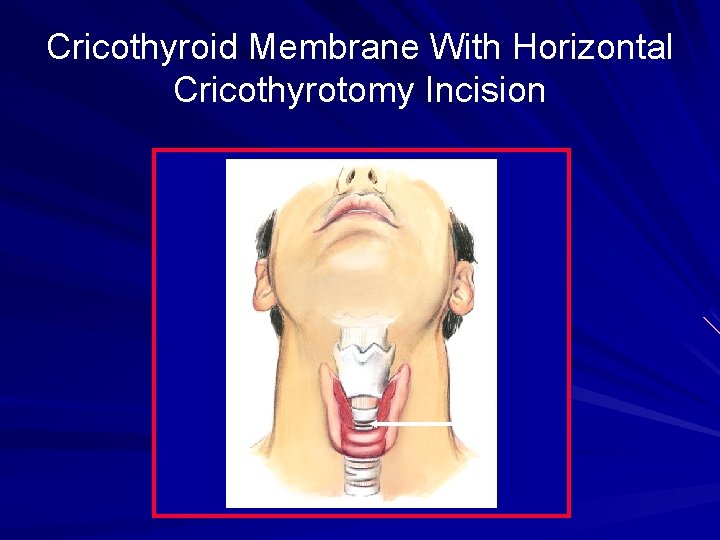
Cricothyroid Membrane With Horizontal Cricothyrotomy Incision
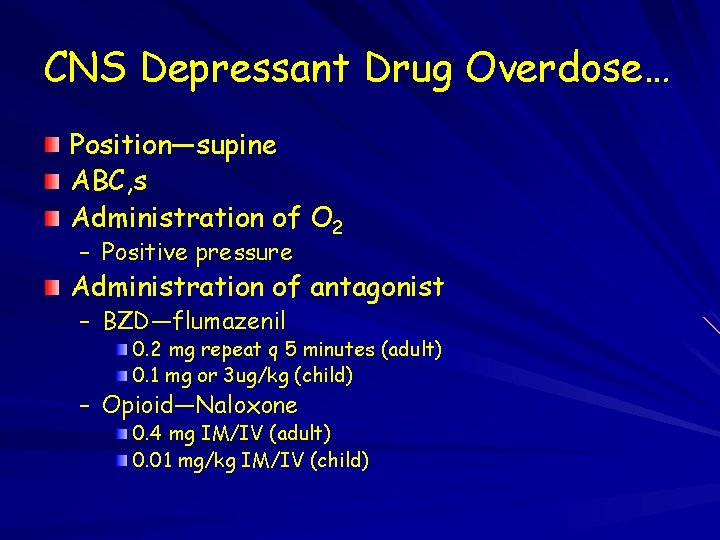
CNS Depressant Drug Overdose… Position—supine ABC, s Administration of O 2 – Positive pressure Administration of antagonist – BZD—flumazenil 0. 2 mg repeat q 5 minutes (adult) 0. 1 mg or 3 ug/kg (child) – Opioid—Naloxone 0. 4 mg IM/IV (adult) 0. 01 mg/kg IM/IV (child)
- Slides: 66