Monitoring in Labour Objectives Discuss fetal heart rate

Monitoring in Labour
Objectives • Discuss fetal heart rate patterns using Continuous Electronic Fetal Monitoring (CEFM) tracings. • Compare the evidence between EFM and structured intermittent auscultation (SIA) • Discuss relevant physiology in fetal monitoring • Describe systematic approaches in fetal monitoring using Dr C Bravado • Outline guidelines for fetal heart rate monitoring using SIA
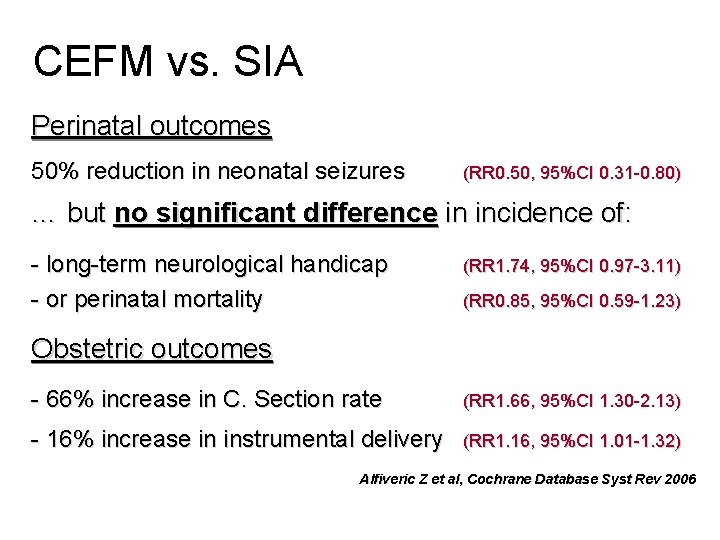
CEFM vs. SIA Perinatal outcomes 50% reduction in neonatal seizures (RR 0. 50, 95%CI 0. 31 -0. 80) … but no significant difference in incidence of: - long-term neurological handicap - or perinatal mortality (RR 1. 74, 95%CI 0. 97 -3. 11) (RR 0. 85, 95%CI 0. 59 -1. 23) Obstetric outcomes - 66% increase in C. Section rate (RR 1. 66, 95%CI 1. 30 -2. 13) - 16% increase in instrumental delivery (RR 1. 16, 95%CI 1. 01 -1. 32) Alfiveric Z et al, Cochrane Database Syst Rev 2006
Pathophysiology of FH rate changes • Changes in FH rate patterns occur in response to changes in O 2, CO 2, hydrogen ions and arterial pressure • These changes are mediated via the vagus nerve, chemoreceptors & carotid body baroreceptors • It is difficult to measure fetal oxygenation and p. H continuously • FH rate patterns only allow indirect assessment of fetal acid-base balance. Fetal scalp sampling is required to confirm whether the fetus is hypoxic… Hinshaw K & Ullal A. Anaes Int Care Med (Aug 2007)
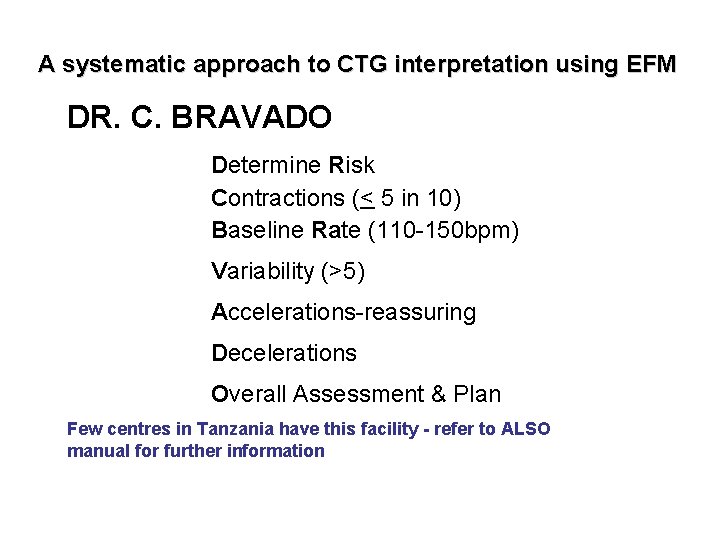
A systematic approach to CTG interpretation using EFM DR. C. BRAVADO Determine Risk Contractions (< 5 in 10) Baseline Rate (110 -150 bpm) Variability (>5) Accelerations-reassuring Decelerations Overall Assessment & Plan Few centres in Tanzania have this facility - refer to ALSO manual for further information
“ DR C BRAVADO” A systematic approach to CTG interpretation Determine Risk Assess degree of “clinical risk” in relation to clinical outcome • High Comparable to TRAFFIC LIGHTS • Low
Risk Factors Maternal: • Previous Caesarean section • Pre-eclampsia • Pregnancy >42 weeks • Prolonged ROM >24 hours • Diabetes • Antepartum haemorrhage • Significant medical condition – eg cardiac
Risk Factors Fetal: • Intrauterine growth restriction • Oligohydramnios • Preterm labour • Multiple pregnancy • Breech presentation
Risk Factors Intrapartum • Significant meconium-stained liquor • Abnormal FHR on auscultation Ø baseline <110 or >160 bpm Ø any decelerations after a contraction • • • Maternal pyrexia Fresh bleeding in labour Oxytocin augmentation
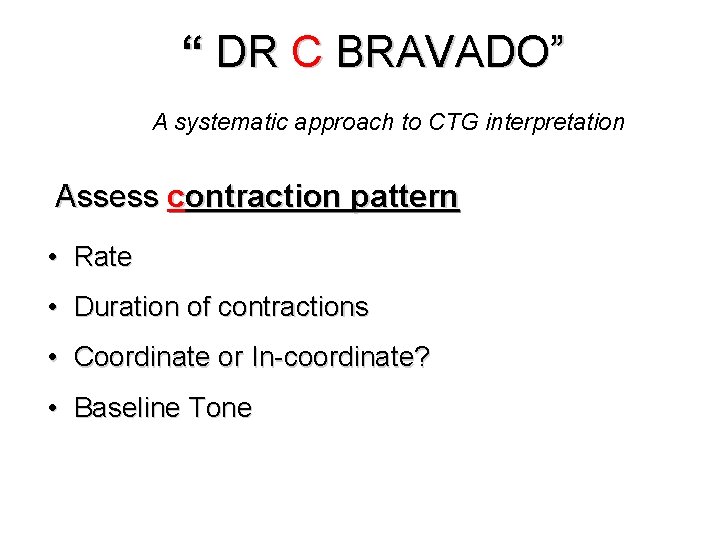
“ DR C BRAVADO” A systematic approach to CTG interpretation Assess contraction pattern • Rate • Duration of contractions • Coordinate or In-coordinate? • Baseline Tone
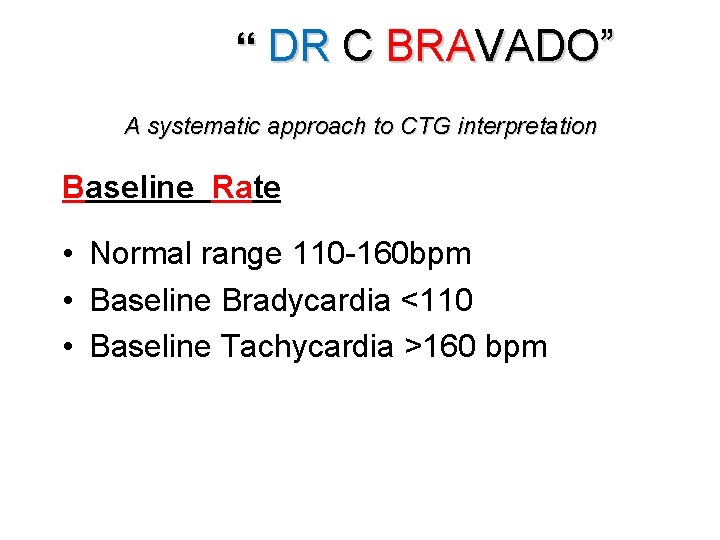
“ DR C BRAVADO” A systematic approach to CTG interpretation Baseline Rate • Normal range 110 -160 bpm • Baseline Bradycardia <110 • Baseline Tachycardia >160 bpm
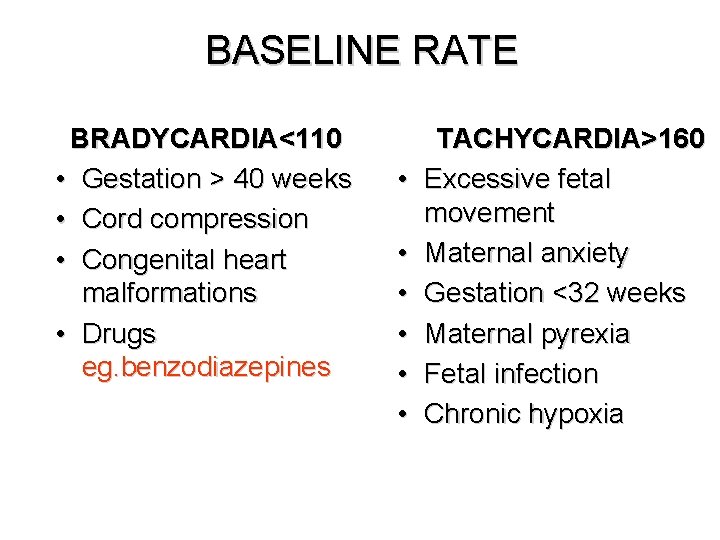
BASELINE RATE BRADYCARDIA<110 • Gestation > 40 weeks • Cord compression • Congenital heart malformations • Drugs eg. benzodiazepines • • • TACHYCARDIA>160 Excessive fetal movement Maternal anxiety Gestation <32 weeks Maternal pyrexia Fetal infection Chronic hypoxia
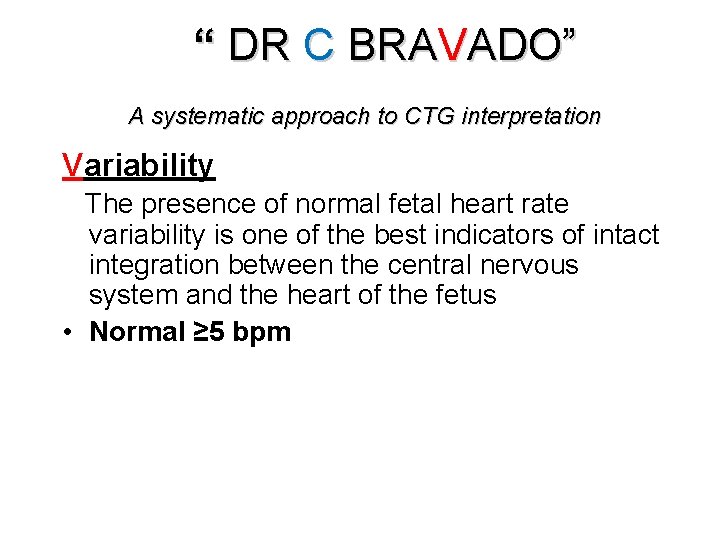
“ DR C BRAVADO” A systematic approach to CTG interpretation Variability The presence of normal fetal heart rate variability is one of the best indicators of intact integration between the central nervous system and the heart of the fetus • Normal ≥ 5 bpm
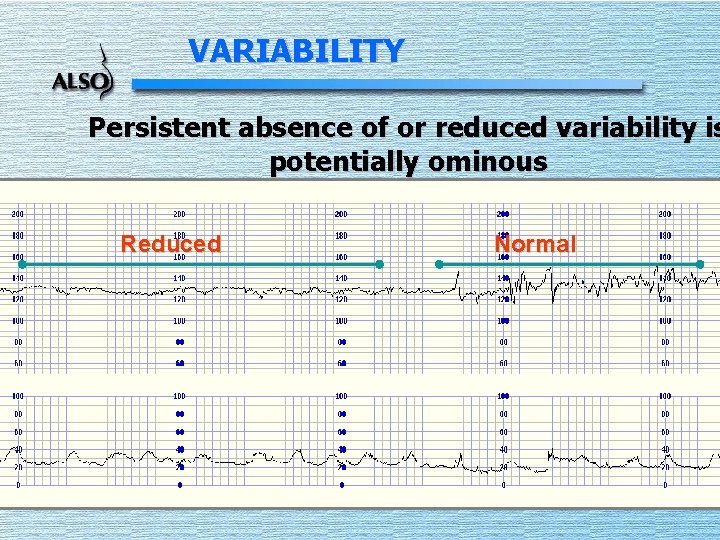
VARIABILITY Persistent absence of or reduced variability is potentially ominous Reduced Normal
“ DR C BRAVADO” A systematic approach to CTG interpretation Accelerations • Increase of at least 15 bpm above the baseline for at least 15 seconds • Associated with movement or stimulation • Presence is the single best indicator of fetal well-being • An antenatal CTG should always contain accelerati to be considered normal.
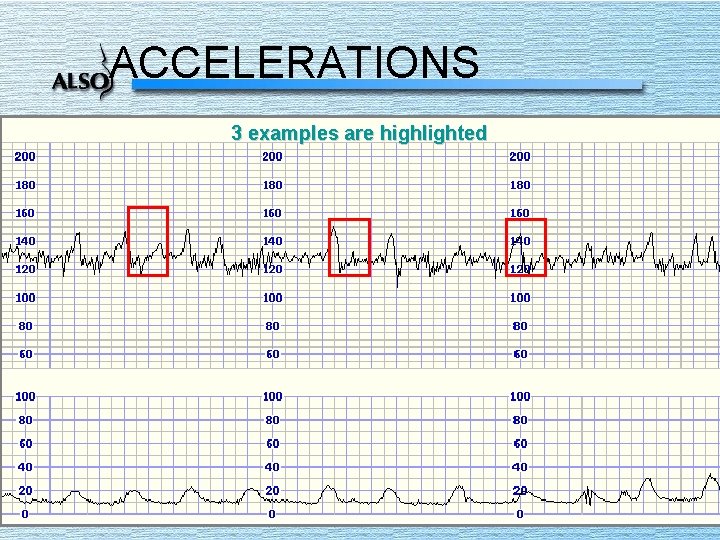
ACCELERATIONS 3 examples are highlighted
“ DR C BRAVADO” A systematic approach to CTG interpretatio • Early Decelerations mirror contractions • Fall of <60 beats from baseline associated (almost exclusively) with excellent fetal outcome • True early uniform decelerations ar rare and benign and therefore not significant
“ DR C BRAVADO” A systematic approach to CTG interpretation Variable Decelerations • Most decelerations in labour are variable • Can reflect cord compression • ‘Variable’ in shape, depth and/or onset • Usually benign but …. if late or deep may imply cord prolapse or hypoxia • ‘Need to assess the frequency and duration
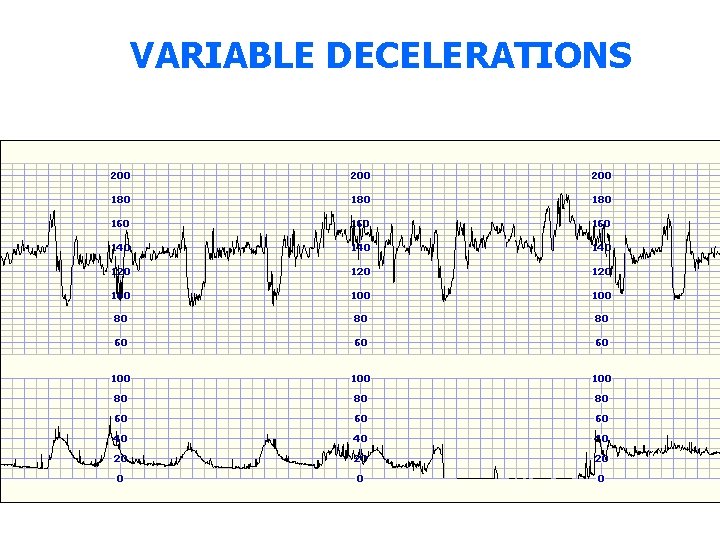
VARIABLE DECELERATIONS
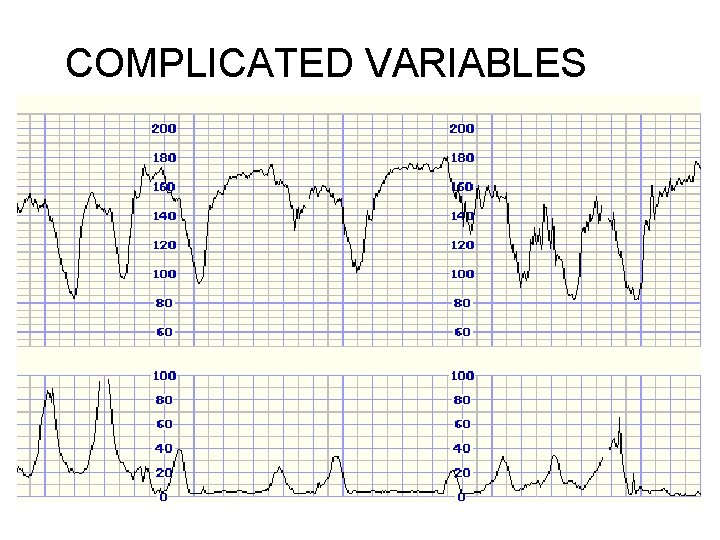
COMPLICATED VARIABLES
“ DR C BRAVADO” A systematic approach to CTG interpretation Late Decelerations • Associated with fetal compromise (hypoxia) but only in 50 -60% of cases • Ominous if associated with: - fresh particulate meconium - ‘high-risk’ clinical situation • Ominous if: - ‘lag-time’ (peak to trough) - deceleration is slow to recover
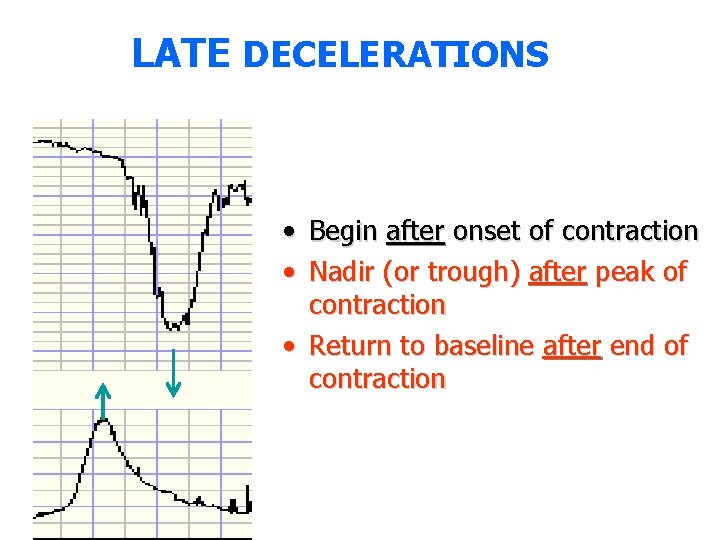
LATE DECELERATIONS • Begin after onset of contraction • Nadir (or trough) after peak of contraction • Return to baseline after end of contraction
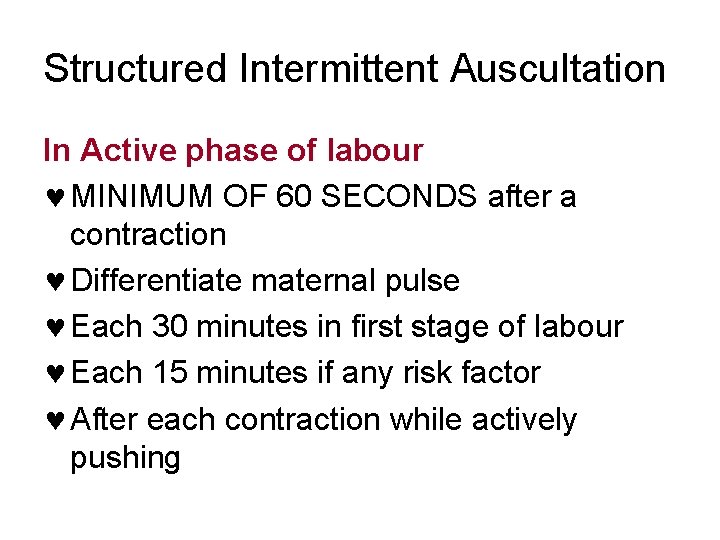
Structured Intermittent Auscultation In Active phase of labour © MINIMUM OF 60 SECONDS after a contraction © Differentiate maternal pulse © Each 30 minutes in first stage of labour © Each 15 minutes if any risk factor © After each contraction while actively pushing
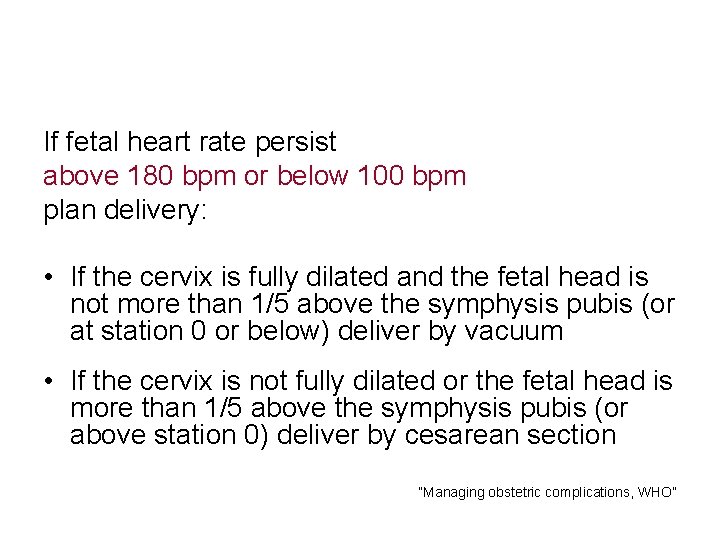
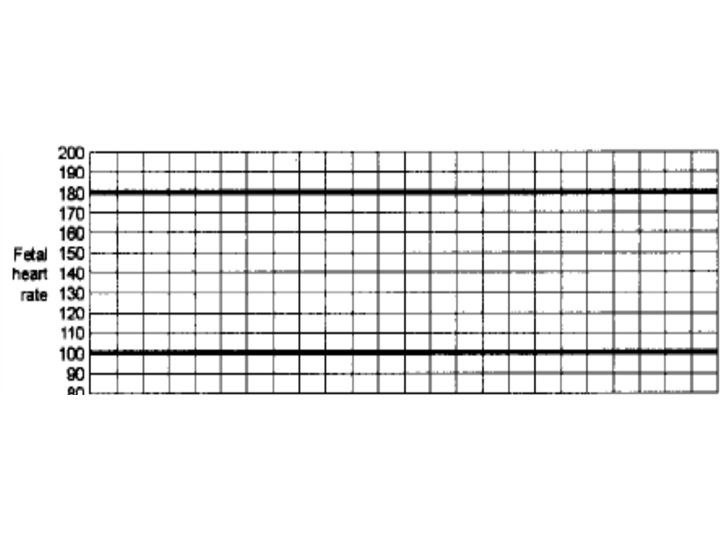
If fetal heart rate persist above 180 bpm or below 100 bpm plan delivery: • If the cervix is fully dilated and the fetal head is not more than 1/5 above the symphysis pubis (or at station 0 or below) deliver by vacuum • If the cervix is not fully dilated or the fetal head is more than 1/5 above the symphysis pubis (or above station 0) deliver by cesarean section ”Managing obstetric complications, WHO”
- Slides: 25