Monitoring in Anesthesia Medical Student Lecture Series Introductory






- Slides: 16

Monitoring in Anesthesia Medical Student Lecture Series Introductory Anesthesiology Clerkship Canvas Department of Anesthesiology University of Minnesota

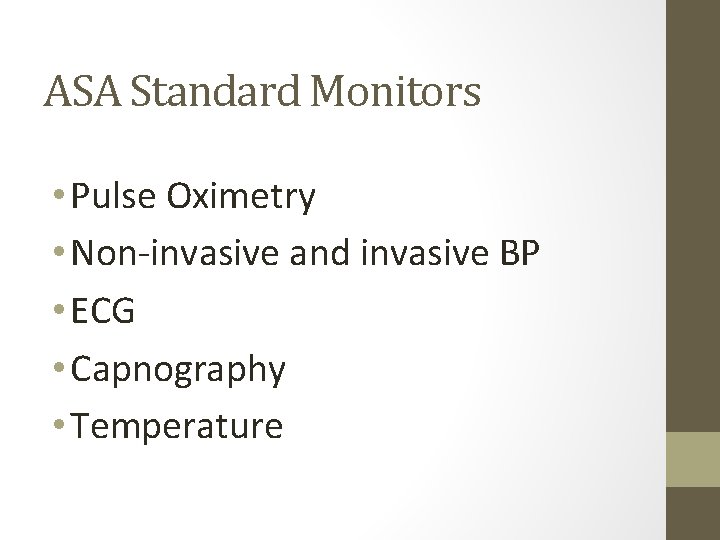
Objectives • Understand the American Society of Anesthesiology Standard Monitors • Understand what organ systems/ functions need to be monitored • Gain a basic appreciation of what information monitors provide and how this information is obtained
ASA Standard Monitors • Pulse Oximetry • Non-invasive and invasive BP • ECG • Capnography • Temperature
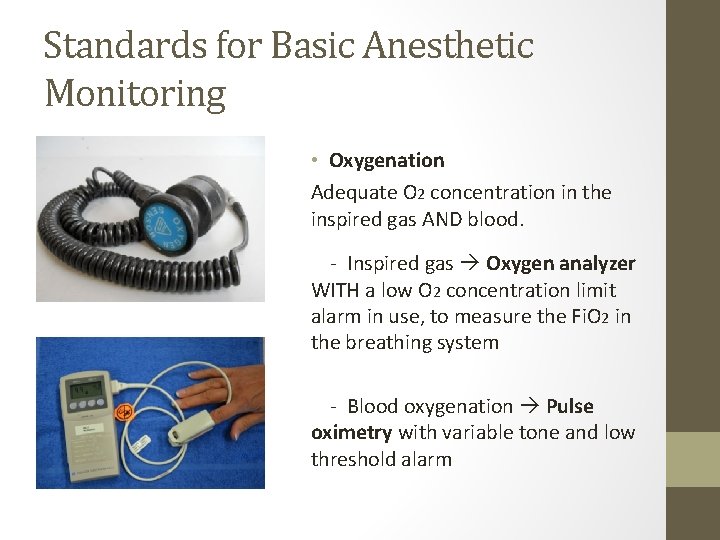
Standards for Basic Anesthetic Monitoring • Oxygenation Adequate O 2 concentration in the inspired gas AND blood. - Inspired gas Oxygen analyzer WITH a low O 2 concentration limit alarm in use, to measure the Fi. O 2 in the breathing system - Blood oxygenation Pulse oximetry with variable tone and low threshold alarm
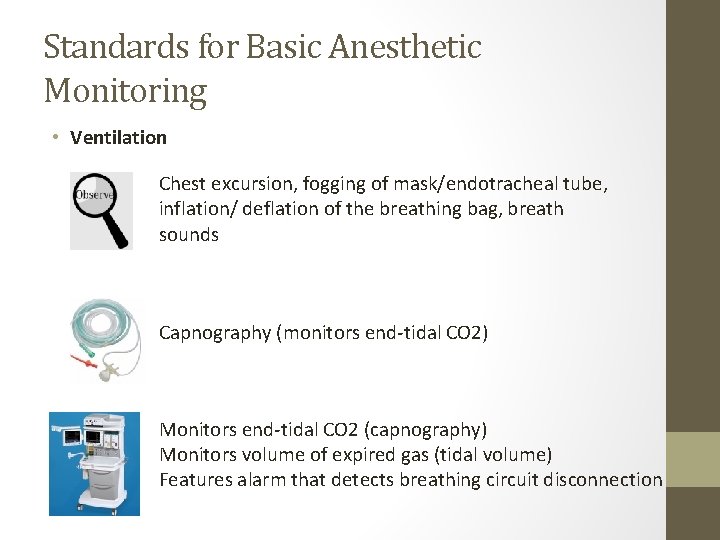
Standards for Basic Anesthetic Monitoring • Ventilation Chest excursion, fogging of mask/endotracheal tube, inflation/ deflation of the breathing bag, breath sounds Capnography (monitors end-tidal CO 2) Monitors end-tidal CO 2 (capnography) Monitors volume of expired gas (tidal volume) Features alarm that detects breathing circuit disconnection
Standards for Basic Anesthetic Monitoring • Circulation Continuous ECG Arterial blood pressure and Heart rate determined and evaluated at least every 5 minutes • Body Temperature Assessment of circulatory function: palpation of a pulse, auscultation of heart sounds, monitoring of invasive or non-invasive blood pressure, ultrasound of a peripheral pulse or pulse oximetry or plethysmography
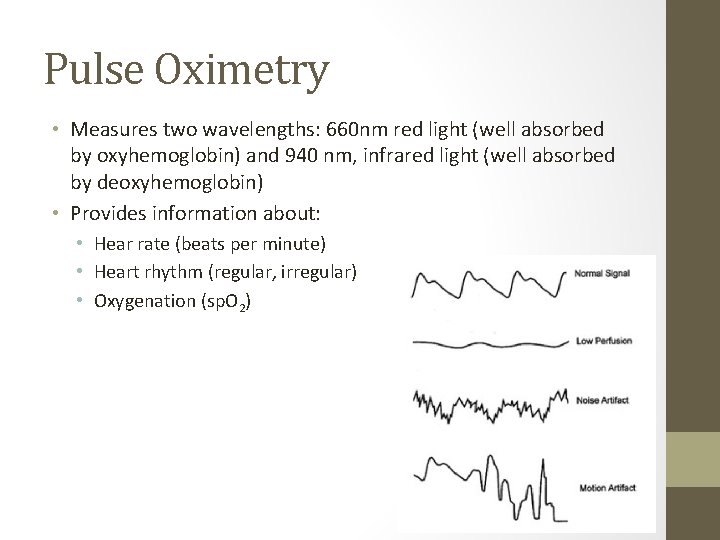
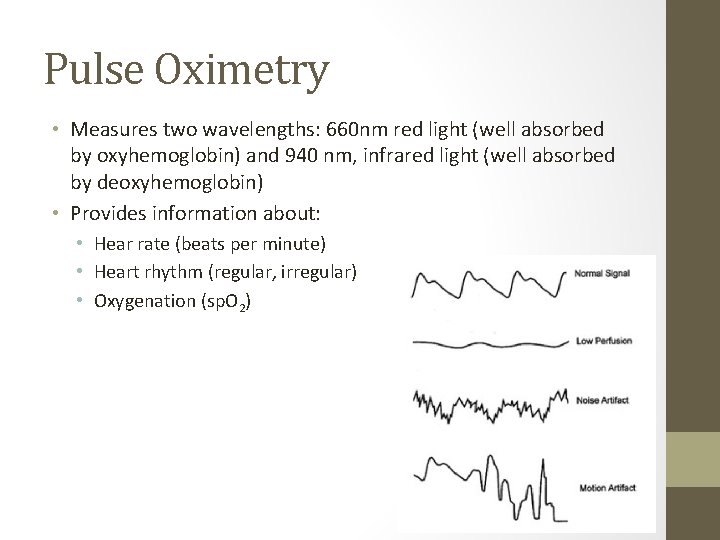
Pulse Oximetry • Measures two wavelengths: 660 nm red light (well absorbed by oxyhemoglobin) and 940 nm, infrared light (well absorbed by deoxyhemoglobin) • Provides information about: • Hear rate (beats per minute) • Heart rhythm (regular, irregular) • Oxygenation (sp. O 2)
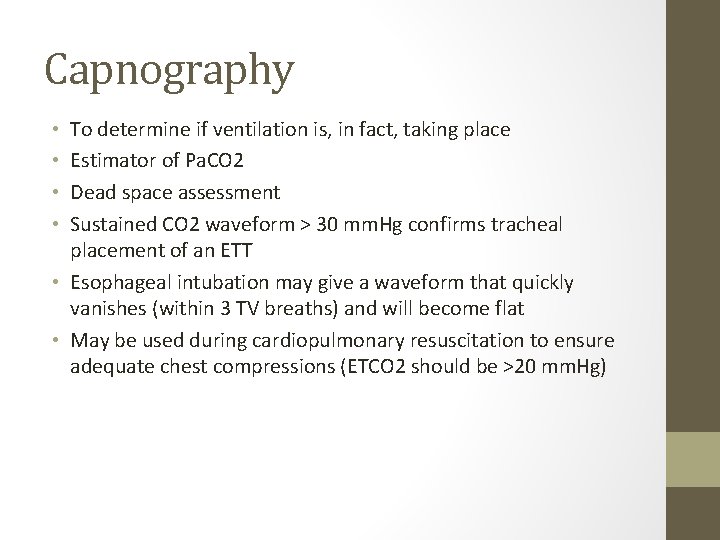
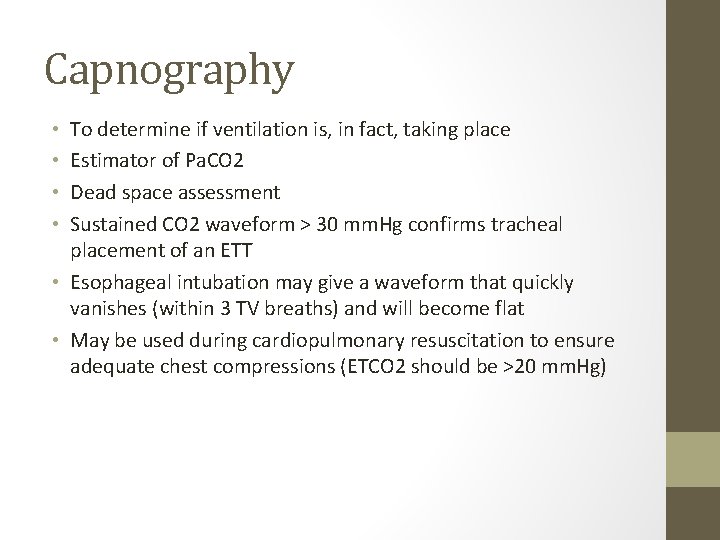
Capnography To determine if ventilation is, in fact, taking place Estimator of Pa. CO 2 Dead space assessment Sustained CO 2 waveform > 30 mm. Hg confirms tracheal placement of an ETT • Esophageal intubation may give a waveform that quickly vanishes (within 3 TV breaths) and will become flat • May be used during cardiopulmonary resuscitation to ensure adequate chest compressions (ETCO 2 should be >20 mm. Hg) • •

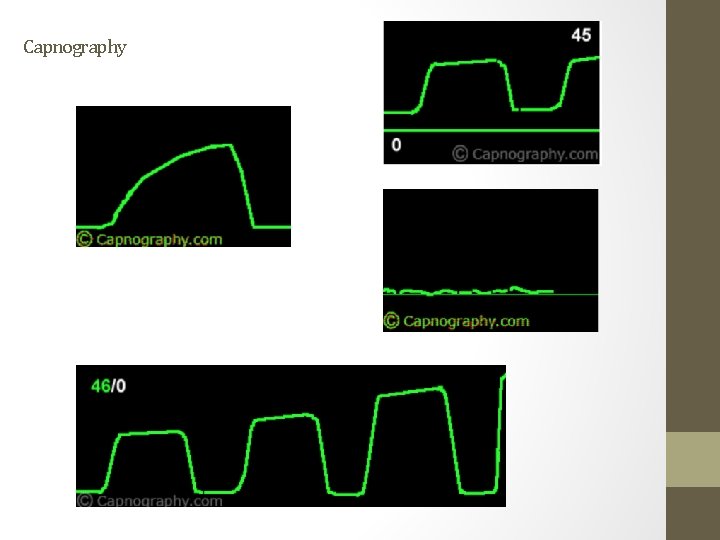
Capnography Four distinct phases of the capnogram waveform: - A-B: Dead space exhalation, devoid of CO 2 - B-C: Sharp upstroke, evenness of ventilation and alveolar emptying; slow rate of rise in conditions with lower airway obstruction - C-D: Alveolar gas exhalation with D point being the ETCO 2 - D-E: Inspiration downstroke, back to baseline or zero, unless rebreathing CO 2
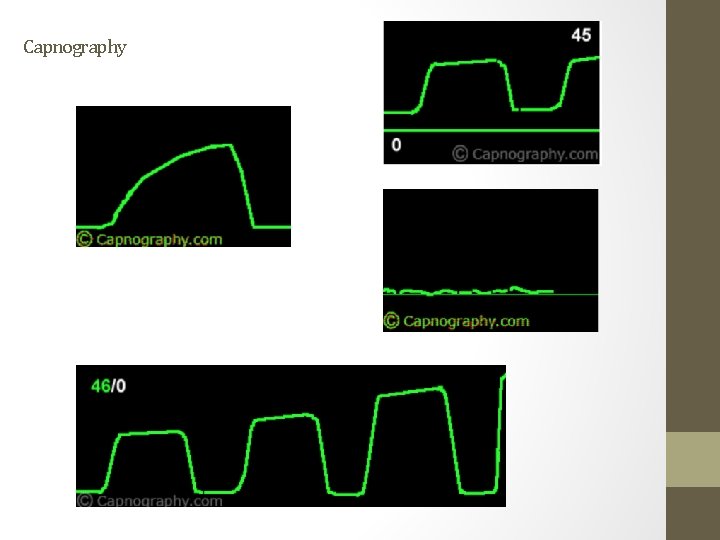
Capnography
NIBP • In the past, frequently performed manually using a stethoscope • In perioperative period, automatic non-invasive blood pressure cuffs are used (oscillometric method) • Blood pressure cuff size is important • Width should be 40% of arm circumference • If too small: measured BP is too high • If too large: measured BP is too low

Direct Arterial Pressure Monitoring • Direct BP monitoring: Invasive measurement by placing a catheter in a peripheral artery which is connected to a transducer system and display. • Indications: CPB, wide swings in BP are expected, when rigorous control of BP is required, need of frequent analysis of ABG’s • Possible cannulation sites: - Radial, Ulnar, Axillary, Brachial, Femoral, Dorsalis Pedis, Posterior Tibial
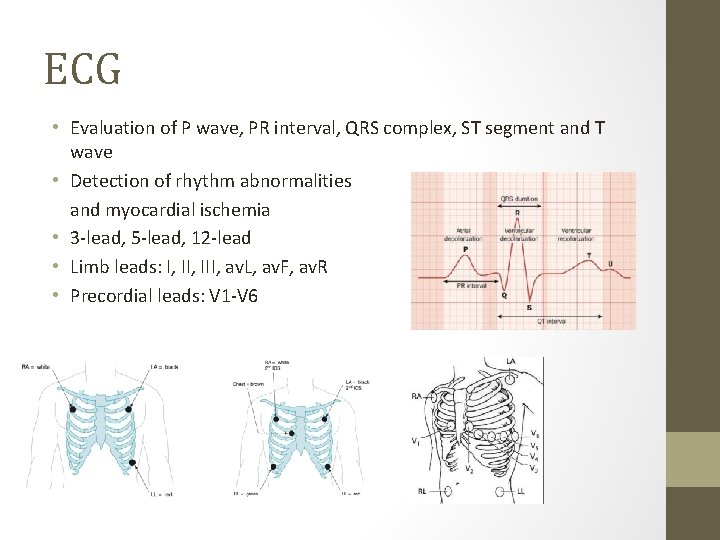
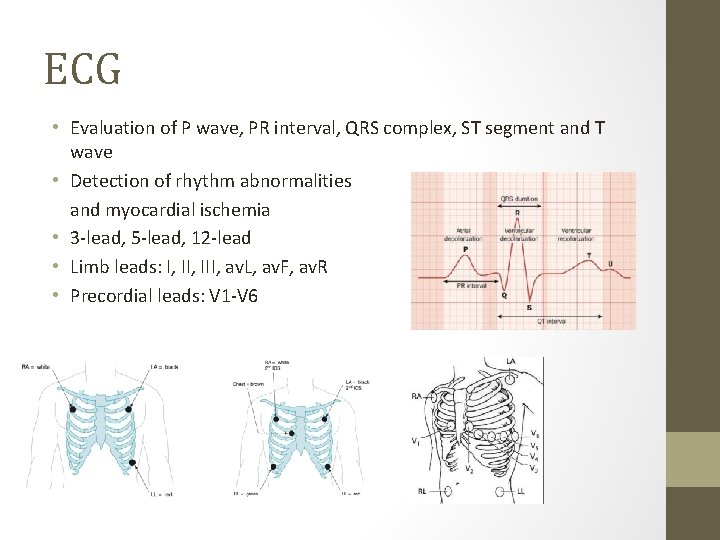
ECG • Evaluation of P wave, PR interval, QRS complex, ST segment and T wave • Detection of rhythm abnormalities and myocardial ischemia • 3 -lead, 5 -lead, 12 -lead • Limb leads: I, III, av. L, av. F, av. R • Precordial leads: V 1 -V 6

Temperature monitoring • Decreases in body temperature are frequent during surgical procedures related to • • Radiation Conduction Convection Evaporation • Effects of hypothermia: delayed recovery from anesthesia; shivering, increases O 2 consumption, dysrhythmias, impairment of coagulation and wound healing • Possible monitoring sites: esophageal, nasopharyngeal, tympanic, oral, bladder, rectal, skin
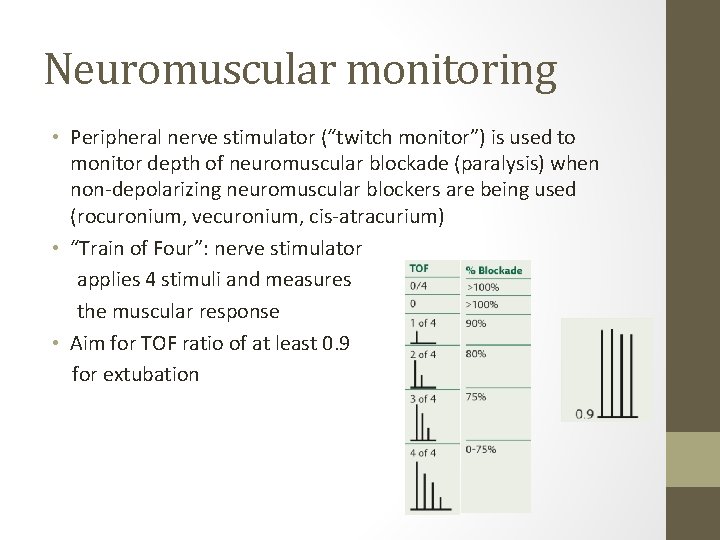
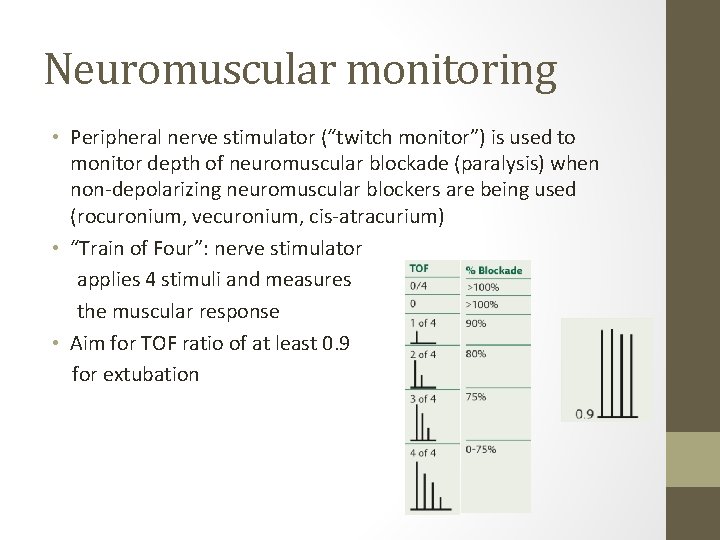
Neuromuscular monitoring • Peripheral nerve stimulator (“twitch monitor”) is used to monitor depth of neuromuscular blockade (paralysis) when non-depolarizing neuromuscular blockers are being used (rocuronium, vecuronium, cis-atracurium) • “Train of Four”: nerve stimulator applies 4 stimuli and measures the muscular response • Aim for TOF ratio of at least 0. 9 for extubation

Other monitors that may be used • Central Venous Catheter • Pulmonary artery catheter • Echocardiography (TEE) • Evoked Potentials (SSEP, MEP, visual and auditory) • Brain Electrical Activity Monitoring (BIS) • Cardiac Output Monitoring • Intracranial Pressure Monitoring • Cerebral Oximetry
 Anesthesia machine lecture
Anesthesia machine lecture Anesthesia monitoring
Anesthesia monitoring Ga medical abbreviation anesthesia
Ga medical abbreviation anesthesia Medical direction
Medical direction 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Geology lecture series
Geology lecture series Dcac lecture series
Dcac lecture series Genetic counseling definition
Genetic counseling definition Medical ethics lecture
Medical ethics lecture Quadrant streak
Quadrant streak Medical statistics lecture
Medical statistics lecture Aim of health psychology
Aim of health psychology Maclaurin series vs taylor series
Maclaurin series vs taylor series Balmer series lyman series
Balmer series lyman series Maclaurin series vs taylor series
Maclaurin series vs taylor series Taylor frederick
Taylor frederick P series server
P series server