Molecular Classification of Endometrial Cancer Improving the approach

- Slides: 50
Molecular Classification of Endometrial Cancer: Improving the approach to research and clinical care -Jessica N Mc. Alpine-
Learning Objectives • Understand the limitations of the current system of endometrial cancer classification and risk categorization. • Be familiar with new molecular tools for the classification of endometrial cancers. • Learn how these advances are being brought to the clinic and how molecular classification can be used to improve management for women with this disease. Jessica N Mc. Alpine, MD Associate Professor-University of British Columbia Dpt of Gynecology and Obstetrics, Div of Gynecologic Oncology OVCARE Tumor Bank Director. BC Cancer Agency
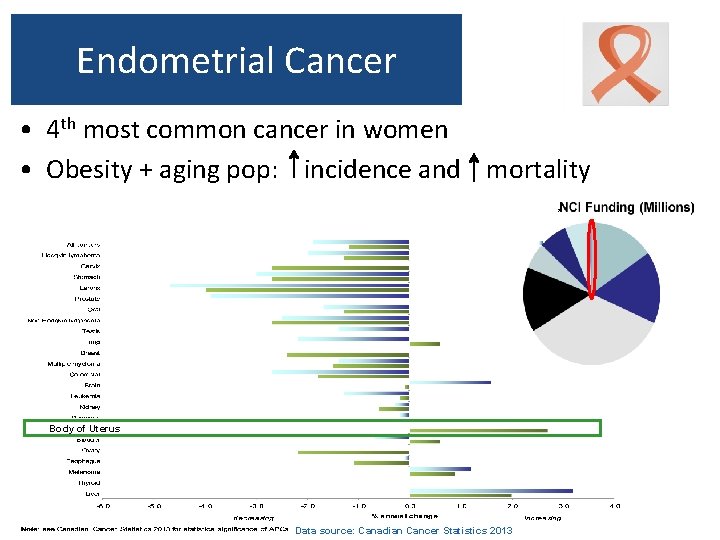
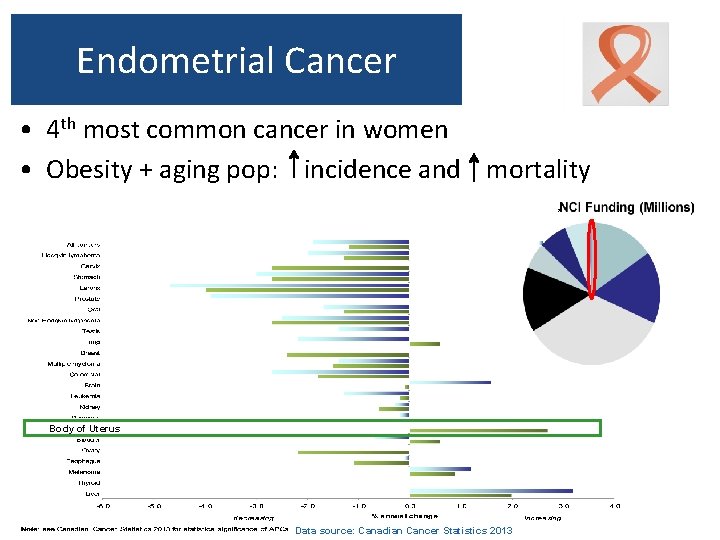
Endometrial Cancer • 4 th most common cancer in women • Obesity + aging pop: incidence and mortality Body of Uterus Data source: Canadian Cancer Statistics 2013
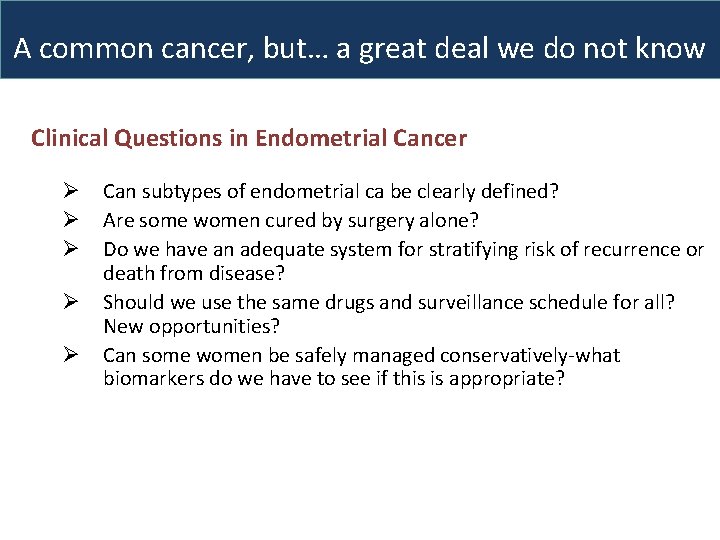
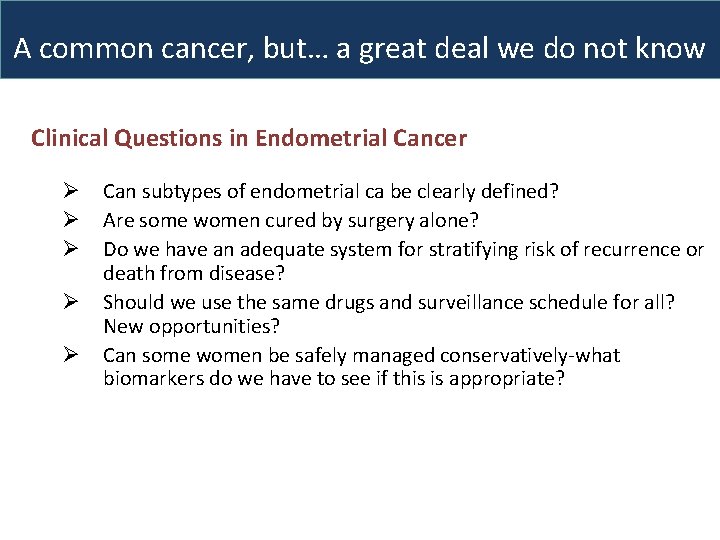
A common cancer, but… a great deal we do not know Clinical Questions in Endometrial Cancer Ø Ø Ø Can subtypes of endometrial ca be clearly defined? Are some women cured by surgery alone? Do we have an adequate system for stratifying risk of recurrence or death from disease? Should we use the same drugs and surveillance schedule for all? New opportunities? Can some women be safely managed conservatively-what biomarkers do we have to see if this is appropriate?
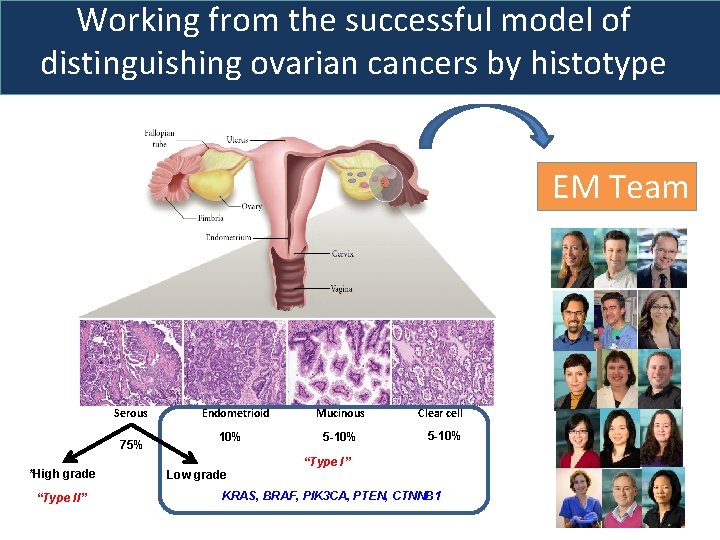
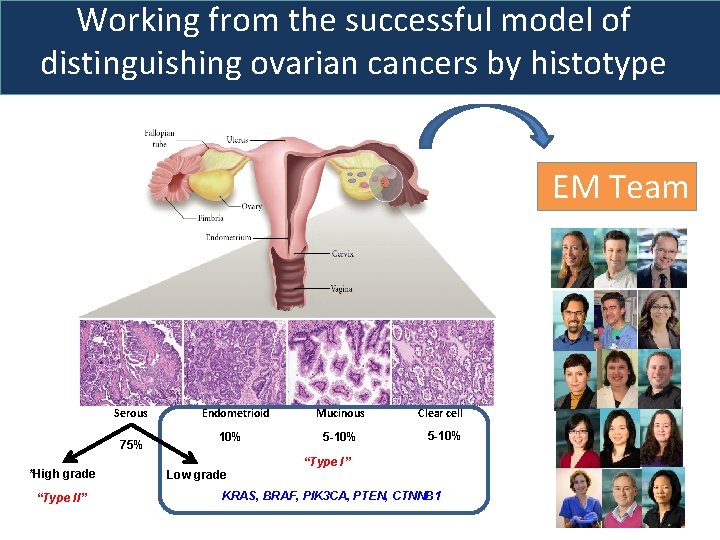
Working from the successful model of distinguishing ovarian cancers by histotype EM Team Serous 75% *High grade “Type II” Endometrioid 10% Low grade Mucinous 5 -10% Clear cell 5 -10% “Type I” KRAS, BRAF, PIK 3 CA, PTEN, CTNNB 1
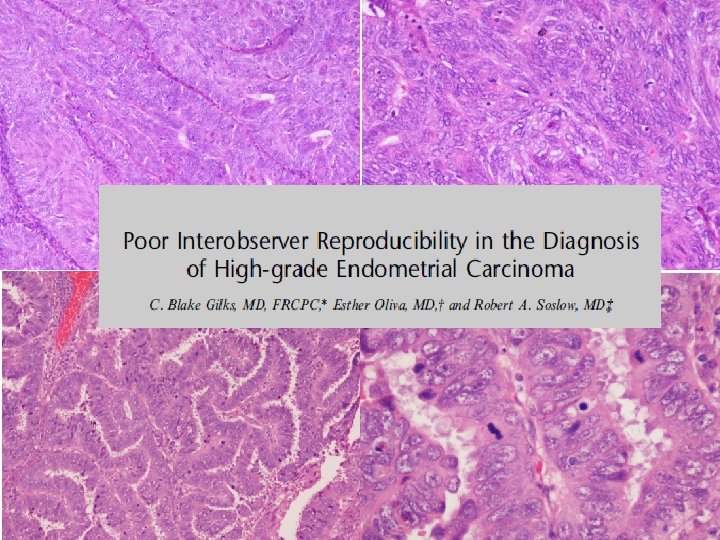
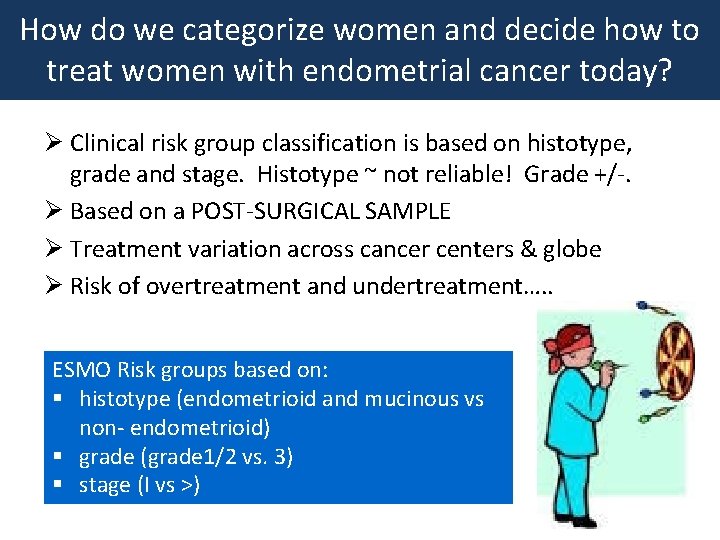
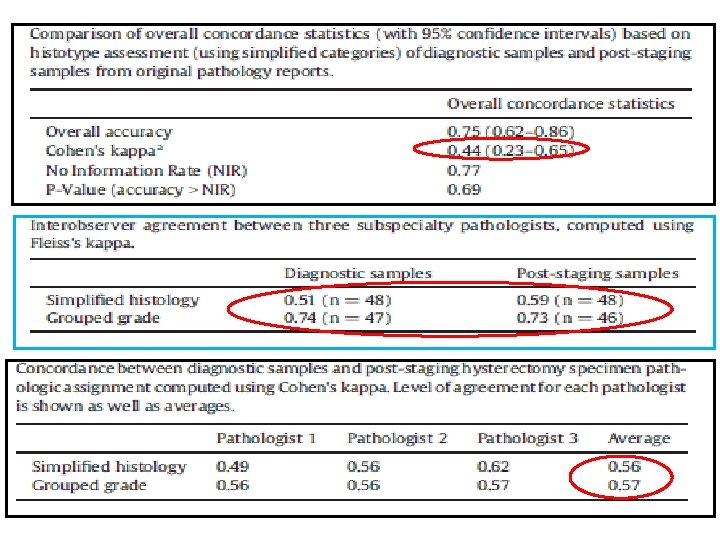
How do we categorize women and decide how to treat women with endometrial cancer today? Ø Clinical risk group classification is based on histotype, grade and stage. Histotype ~ not reliable! Grade +/-. Ø Based on a POST-SURGICAL SAMPLE Ø Treatment variation across cancer centers & globe Ø Risk of overtreatment and undertreatment…. . ESMO Risk groups based on: § histotype (endometrioid and mucinous vs non- endometrioid) § grade (grade 1/2 vs. 3) § stage (I vs >)
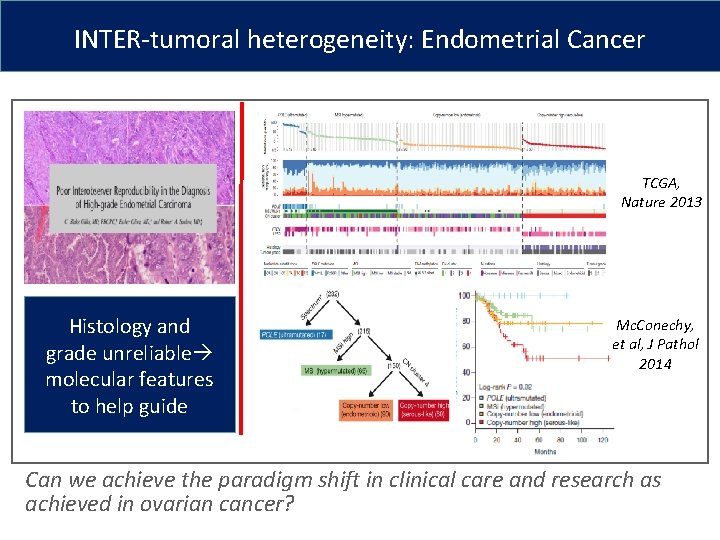
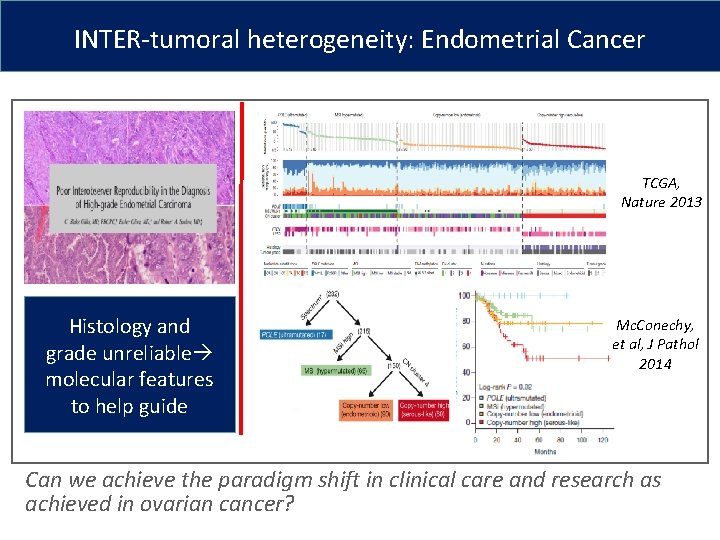
INTER-tumoral heterogeneity: Endometrial Cancer TCGA, Nature 2013 Histology and grade unreliable molecular features to help guide Mc. Conechy, et al, J Pathol 2014 Can we achieve the paradigm shift in clinical care and research as achieved in ovarian cancer?
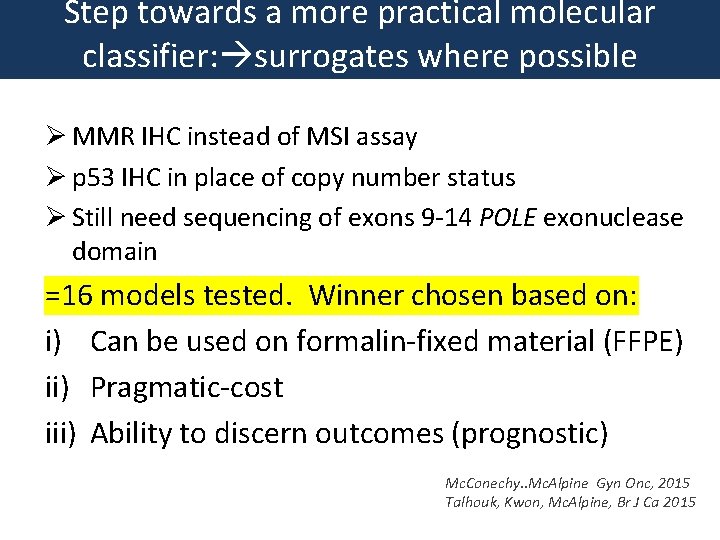
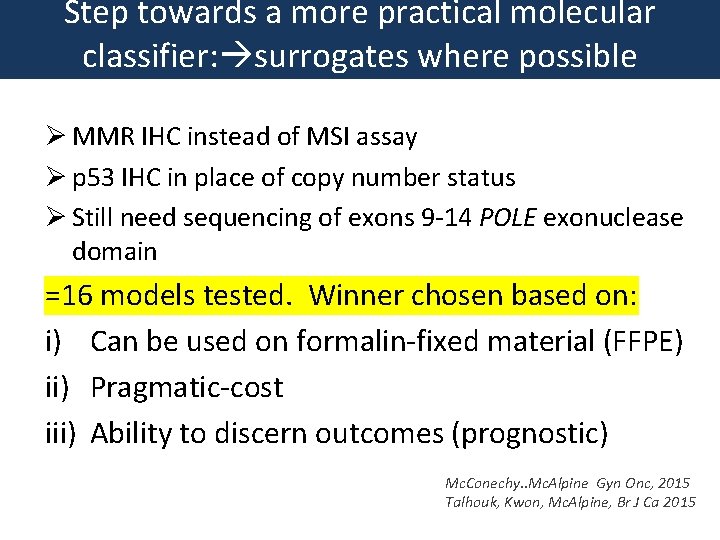
Step towards a more practical molecular classifier: surrogates where possible Ø MMR IHC instead of MSI assay Ø p 53 IHC in place of copy number status Ø Still need sequencing of exons 9 -14 POLE exonuclease domain =16 models tested. Winner chosen based on: i) Can be used on formalin-fixed material (FFPE) ii) Pragmatic-cost iii) Ability to discern outcomes (prognostic) Mc. Conechy. . Mc. Alpine Gyn Onc, 2015 Talhouk, Kwon, Mc. Alpine, Br J Ca 2015
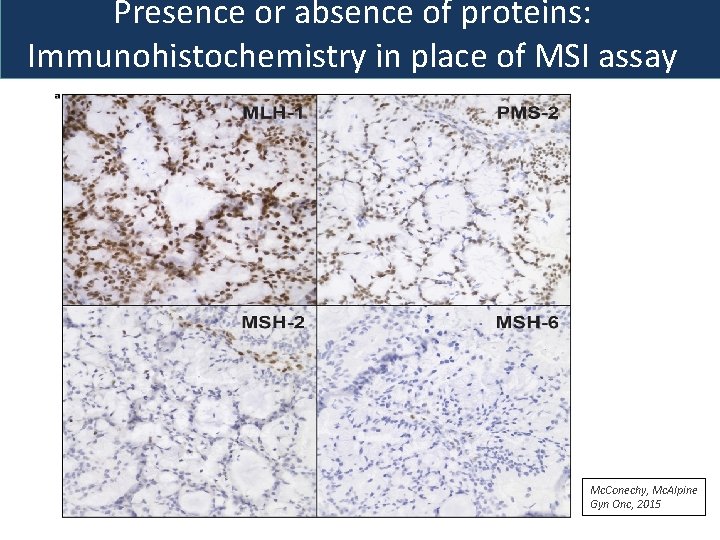
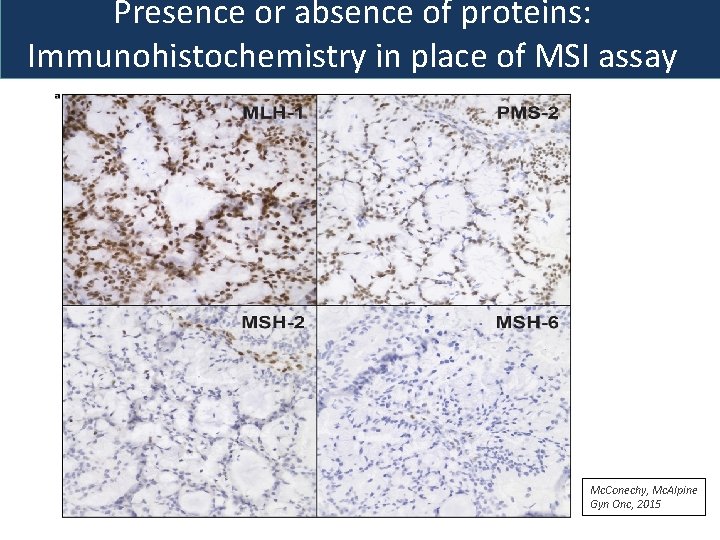
Presence or absence of proteins: Immunohistochemistry in place of MSI assay Mc. Conechy, Mc. Alpine Gyn Onc, 2015
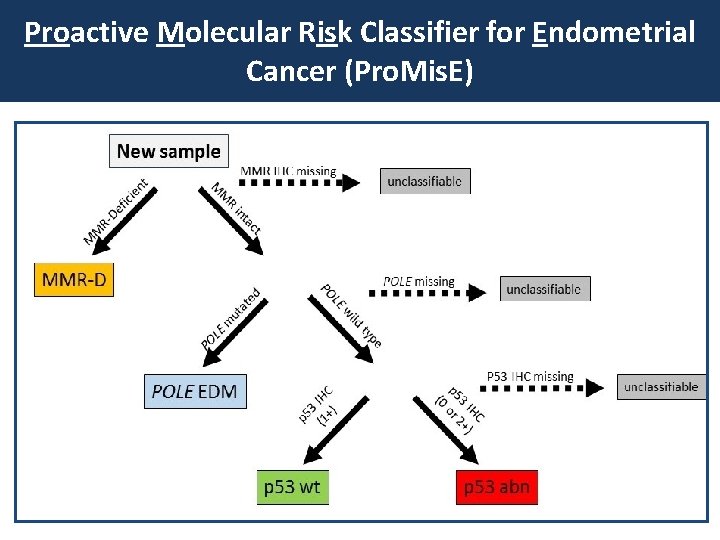
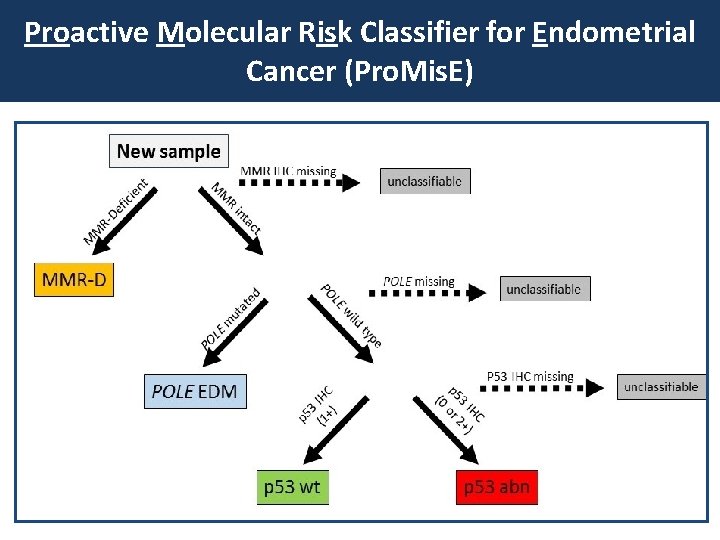
Proactive Molecular Risk Classifier for Endometrial Cancer (Pro. Mis. E)
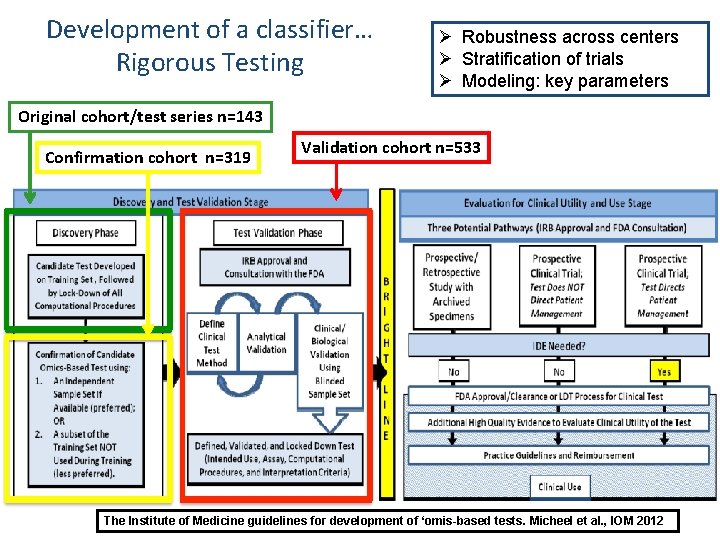
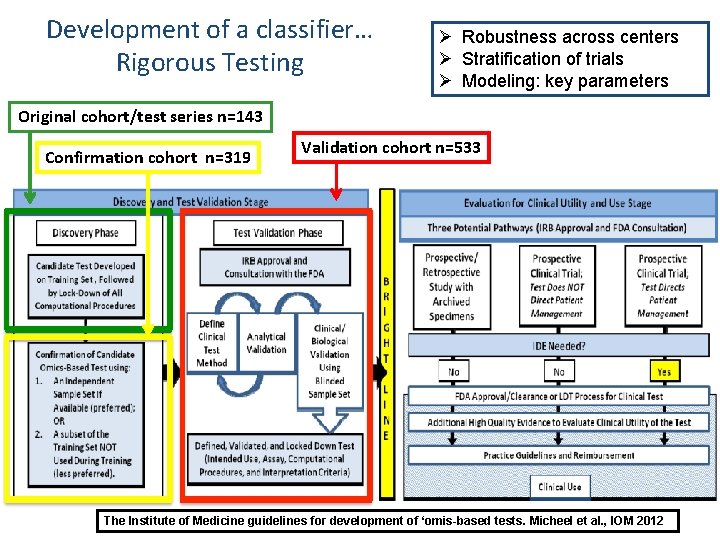
Development of a classifier… Rigorous Testing Ø Robustness across centers Ø Stratification of trials Ø Modeling: key parameters Original cohort/test series n=143 Confirmation cohort n=319 Validation cohort n=533 IOM Guidelines for the development of prognostic and diagnostic assays The Institute of Medicine guidelines for development of ‘omis-based tests. Micheel et al. , IOM 2012
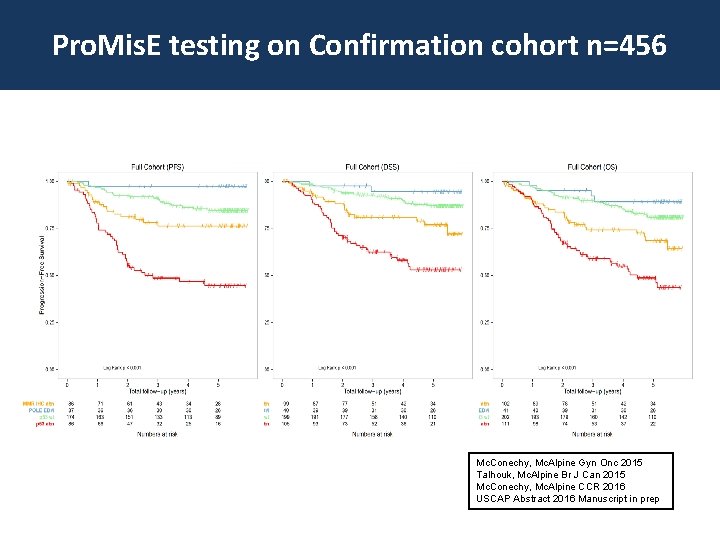
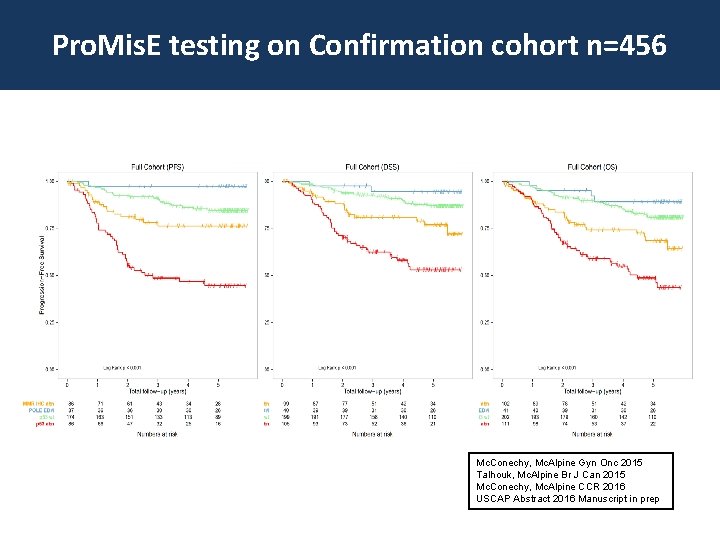
Pro. Mis. E testing on Confirmation cohort n=456 Mc. Conechy, Mc. Alpine Gyn Onc 2015 Talhouk, Mc. Alpine Br J Can 2015 Mc. Conechy, Mc. Alpine CCR 2016 USCAP Abstract 2016 Manuscript in prep
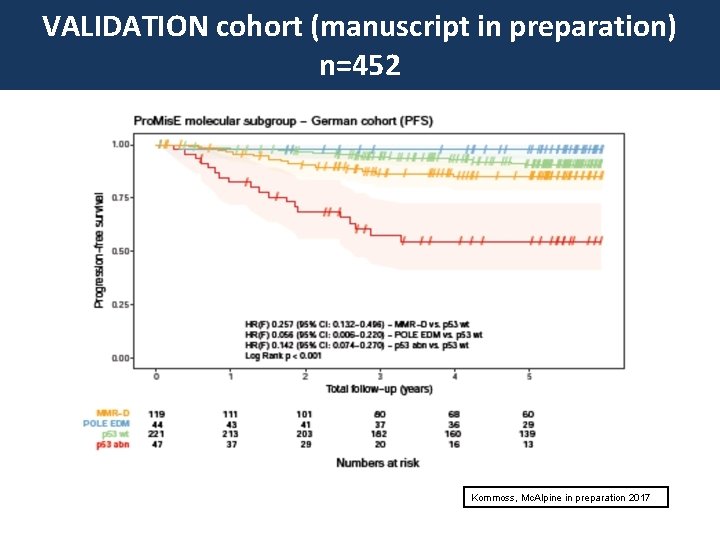
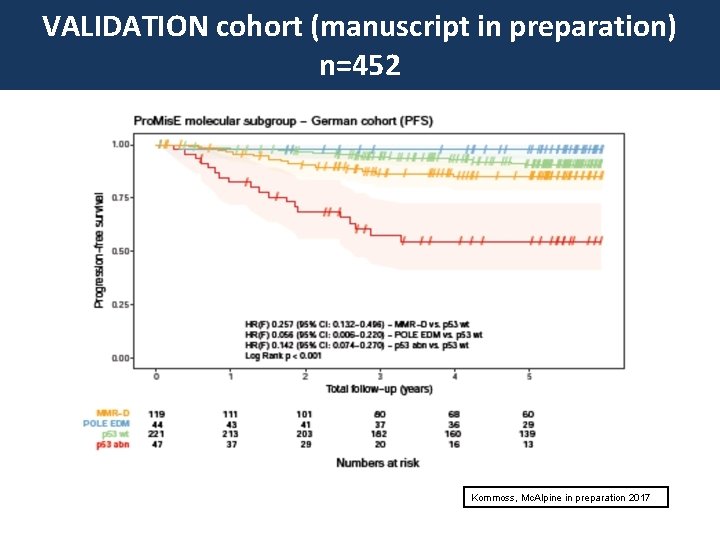
VALIDATION cohort (manuscript in preparation) n=452 Kommoss, Mc. Alpine in preparation 2017
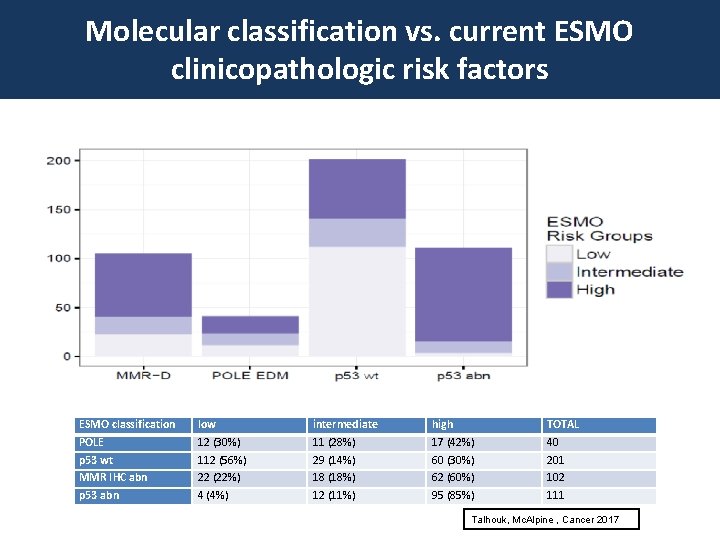
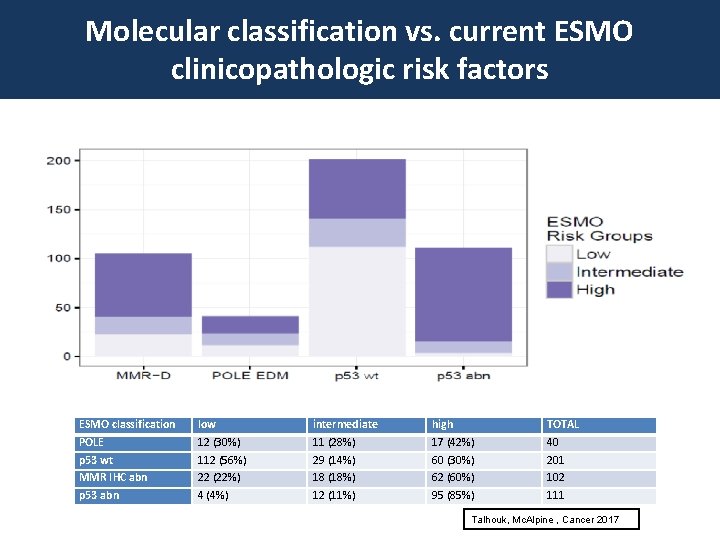
Molecular classification vs. current ESMO clinicopathologic risk factors ESMO classification POLE p 53 wt MMR IHC abn p 53 abn low 12 (30%) 112 (56%) 22 (22%) 4 (4%) intermediate 11 (28%) 29 (14%) 18 (18%) 12 (11%) high 17 (42%) 60 (30%) 62 (60%) 95 (85%) TOTAL 40 201 102 111 Talhouk, Mc. Alpine , Cancer 2017
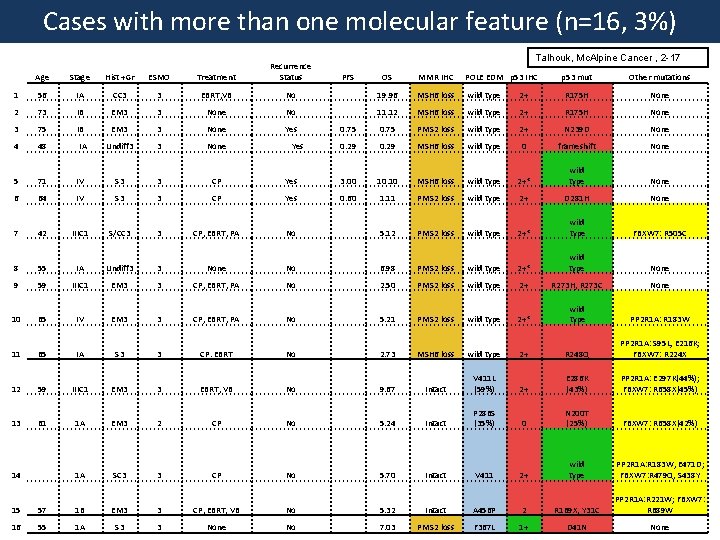
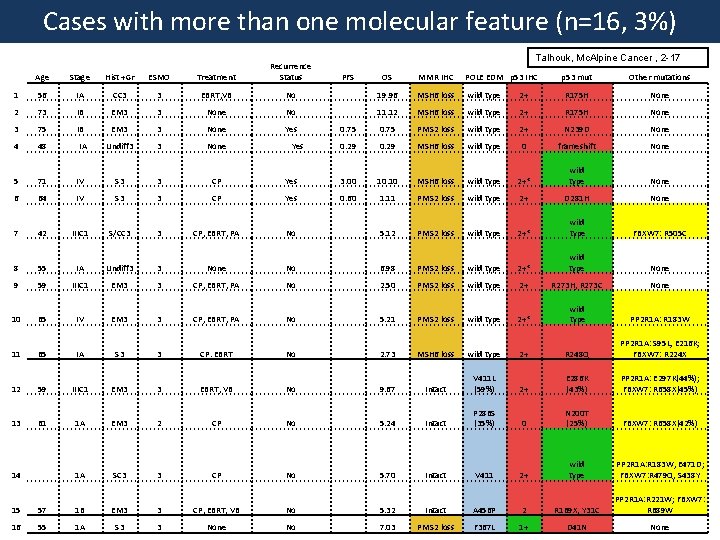
Cases with more than one molecular feature (n=16, 3%) Talhouk, Mc. Alpine Cancer , 2 -17 Age Stage Hist +Gr ESMO Treatment Recurrence Status 1 56 IA CC 3 3 EBRT, VB No 19. 96 MSH 6 loss wild type 2 73 IB EM 3 3 None No 11. 12 MSH 6 loss 3 75 IB EM 3 3 None Yes 0. 75 4 48 Undiff 3 3 None 0. 29 5 71 IV S 3 3 CP Yes 6 64 IV S 3 3 CP 7 42 IIIC 1 S/CC 3 3 8 55 IA Undiff 3 9 59 IIIC 1 10 65 11 p 53 mut Other mutations 2+ R 175 H None wild type 2+ R 175 H None PMS 2 loss wild type 2+ N 239 D None 0. 29 MSH 6 loss wild type 0 frameshift None 3. 00 10. 10 MSH 6 loss wild type 2+* wild type None Yes 0. 60 1. 11 PMS 2 loss wild type 2+ D 281 H None CP, EBRT, PA No 5. 12 PMS 2 loss wild type 2+* wild type FBXW 7: R 505 C 3 None No 6. 98 PMS 2 loss wild type 2+* wild type None EM 3 3 CP, EBRT, PA No 2. 50 PMS 2 loss wild type 2+ R 273 H, R 273 C None IV EM 3 3 CP, EBRT, PA No 5. 21 PMS 2 loss wild type 2+* wild type PP 2 R 1 A: R 183 W 65 IA S 3 3 CP. EBRT No 2. 73 MSH 6 loss wild type 2+ R 248 Q PP 2 R 1 A: S 95 L, E 216 K; FBXW 7: R 224 X 12 59 IIIC 1 EM 3 3 EBRT, VB No 9. 67 Intact V 411 L (59%) 2+ E 286 K (43%) PP 2 R 1 A: E 297 K(44%); FBXW 7: R 658 X(45%) 13 61 1 A EM 3 2 CP No 5. 24 Intact P 286 S (35%) 0 N 200 T (25%) FBXW 7: R 658 X(42%) 14 1 A SC 3 3 CP No 5. 70 Intact V 411 2+ wild type PP 2 R 1 A: R 183 W, E 471 D; FBXW 7: R 479 Q, S 438 Y 15 57 1 B EM 3 3 CP, EBRT, VB No 5. 32 Intact A 456 P 2 R 169 X, Y 31 C PP 2 R 1 A: R 221 W; FBXW 7: R 689 W 16 55 1 A S 3 3 None No 7. 03 PMS 2 loss F 367 L 1+ D 41 N None IA Yes PFS OS MMR IHC POLE EDM p 53 IHC
No disclosures
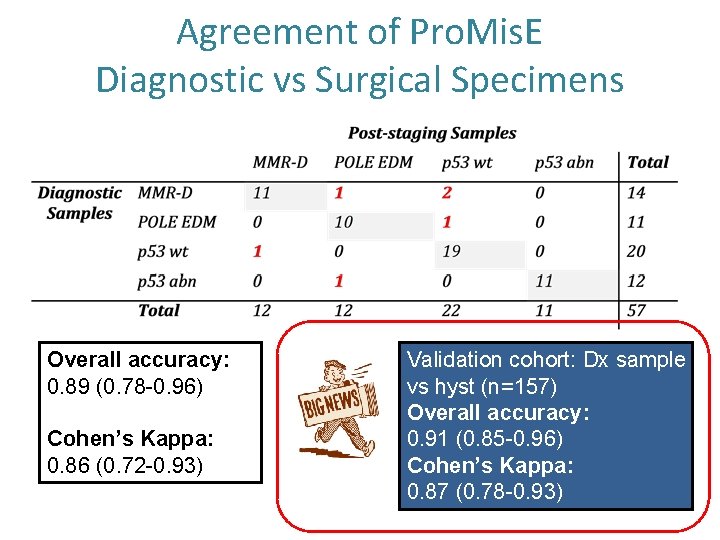
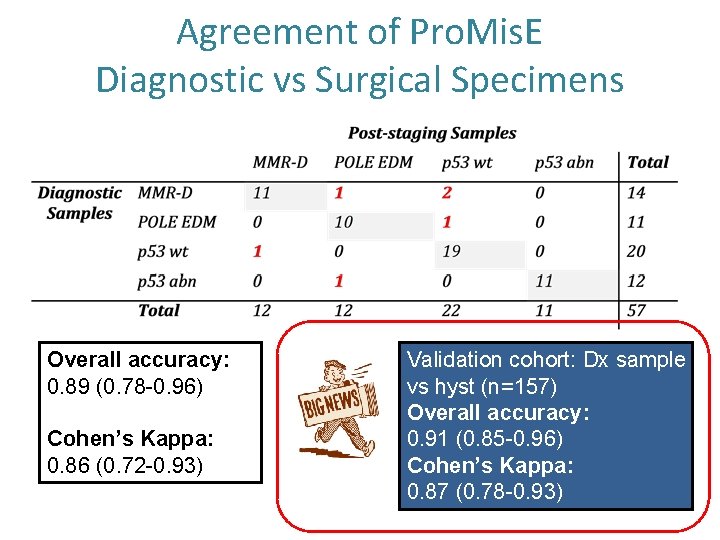
Agreement of Pro. Mis. E Diagnostic vs Surgical Specimens Overall accuracy: 0. 89 (0. 78 -0. 96) Cohen’s Kappa: 0. 86 (0. 72 -0. 93) Validation cohort: Dx sample vs hyst (n=157) Overall accuracy: 0. 91 (0. 85 -0. 96) Cohen’s Kappa: 0. 87 (0. 78 -0. 93)
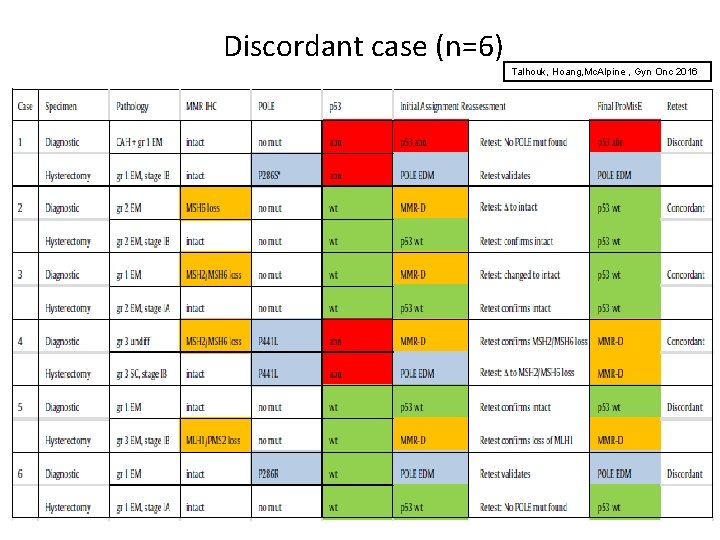
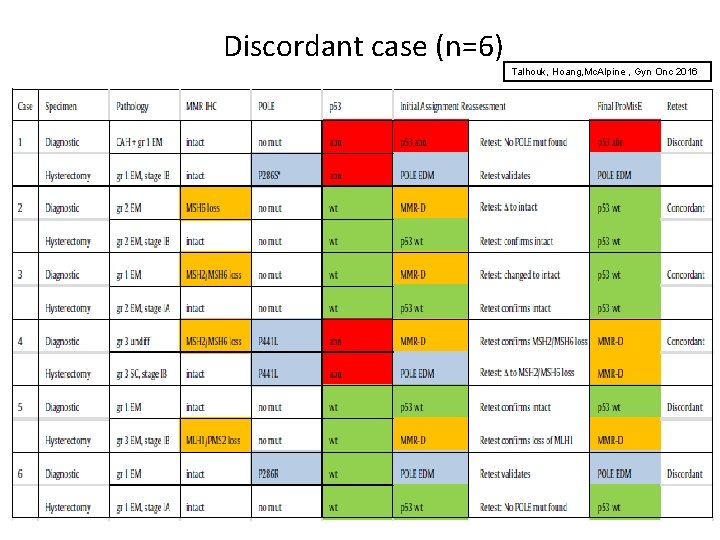
Discordant case (n=6) Talhouk, Hoang, Mc. Alpine , Gyn Onc 2016
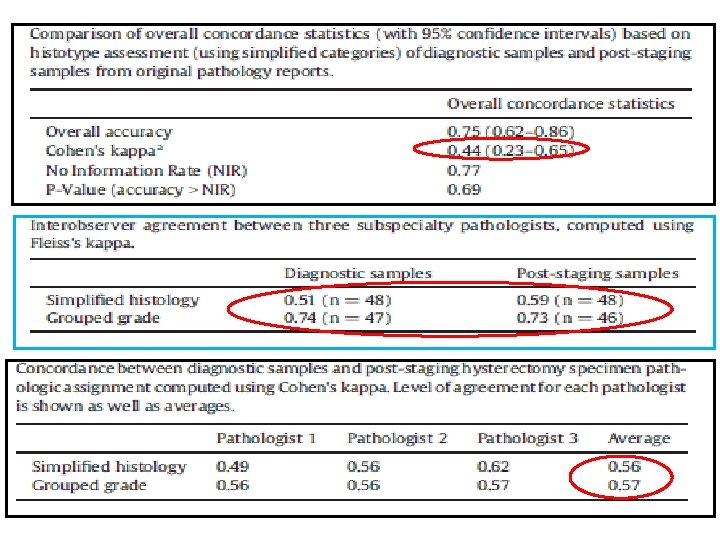
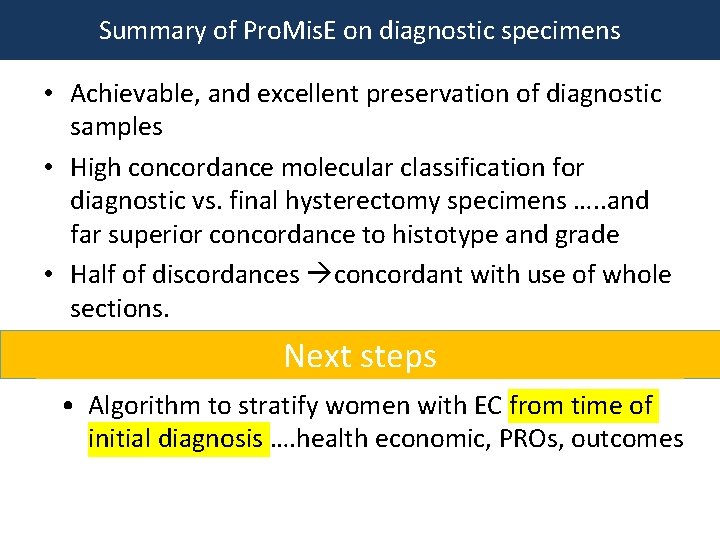
Summary of Pro. Mis. E on diagnostic specimens • Achievable, and excellent preservation of diagnostic samples • High concordance molecular classification for diagnostic vs. final hysterectomy specimens …. . and far superior concordance to histotype and grade • Half of discordances concordant with use of whole sections. Next steps • Algorithm to stratify women with EC from time of initial diagnosis …. health economic, PROs, outcomes
What is the role for additional prognostic markers in the framework of molecular classification in endometrial cancers?
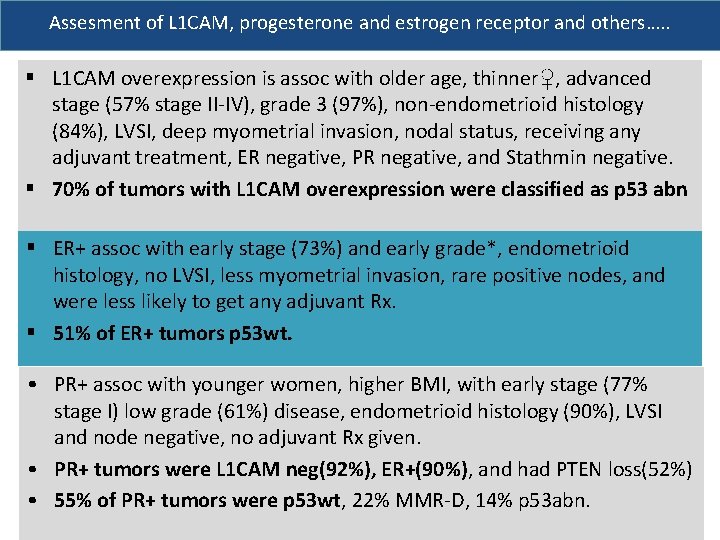
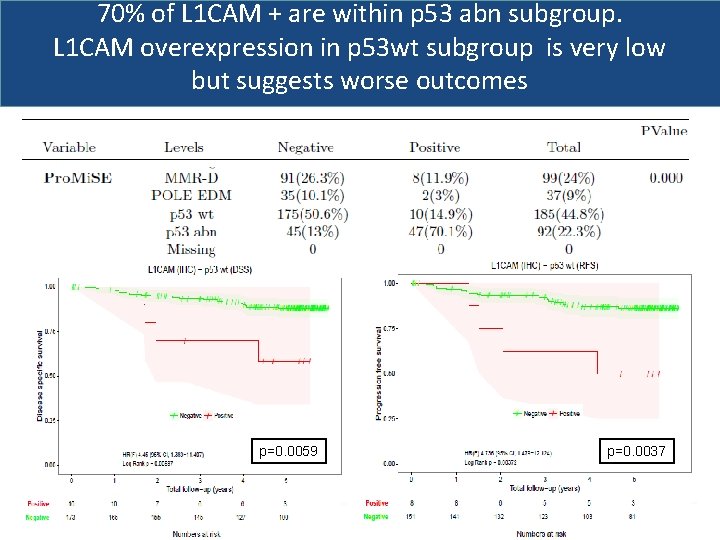
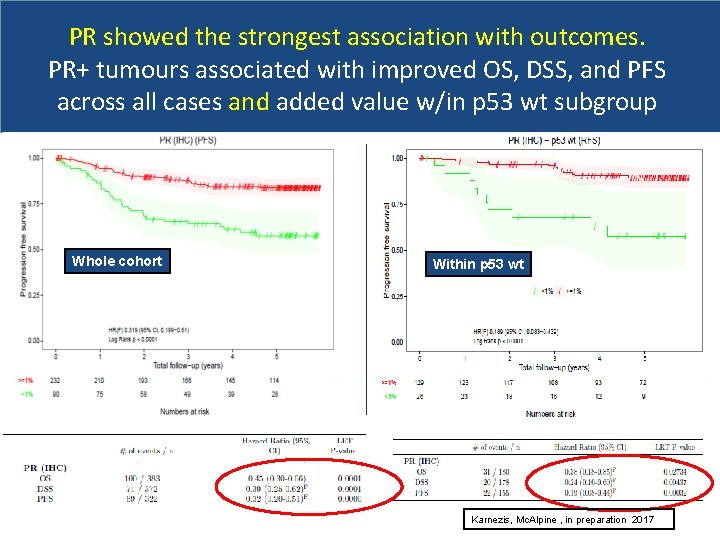
Assesment of L 1 CAM, progesterone and estrogen receptor and others…. . § L 1 CAM overexpression is assoc with older age, thinner♀, advanced stage (57% stage II-IV), grade 3 (97%), non-endometrioid histology (84%), LVSI, deep myometrial invasion, nodal status, receiving any adjuvant treatment, ER negative, PR negative, and Stathmin negative. § 70% of tumors with L 1 CAM overexpression were classified as p 53 abn § ER+ assoc with early stage (73%) and early grade*, endometrioid histology, no LVSI, less myometrial invasion, rare positive nodes, and were less likely to get any adjuvant Rx. § 51% of ER+ tumors p 53 wt. • PR+ assoc with younger women, higher BMI, with early stage (77% stage I) low grade (61%) disease, endometrioid histology (90%), LVSI and node negative, no adjuvant Rx given. • PR+ tumors were L 1 CAM neg(92%), ER+(90%), and had PTEN loss(52%) • 55% of PR+ tumors were p 53 wt, 22% MMR-D, 14% p 53 abn.
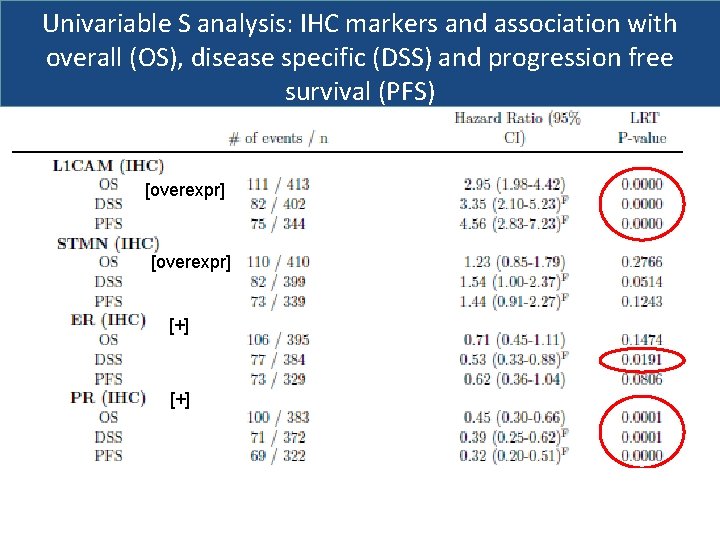
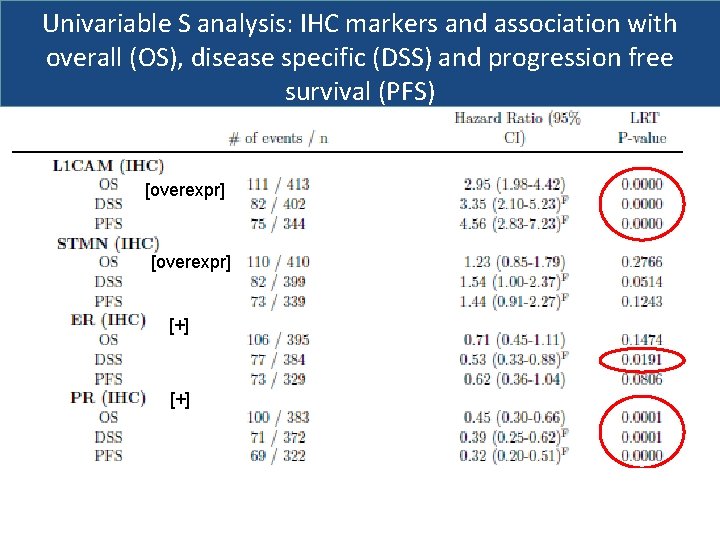
Univariable S analysis: IHC markers and association with overall (OS), disease specific (DSS) and progression free survival (PFS) [overexpr] [+]
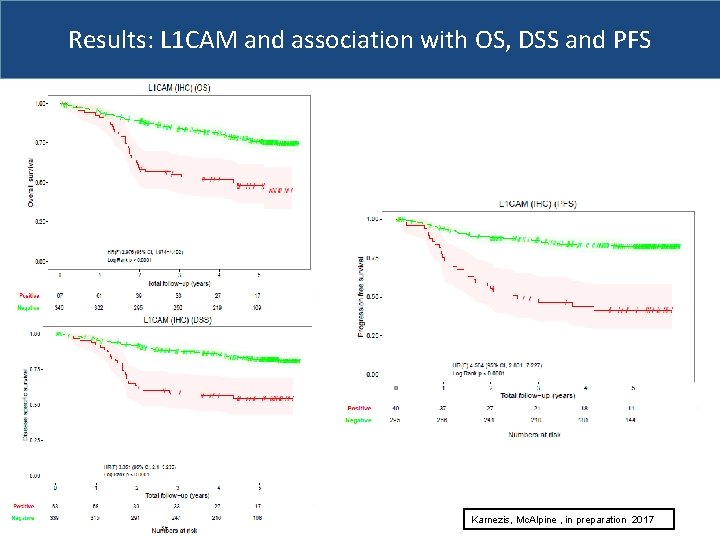
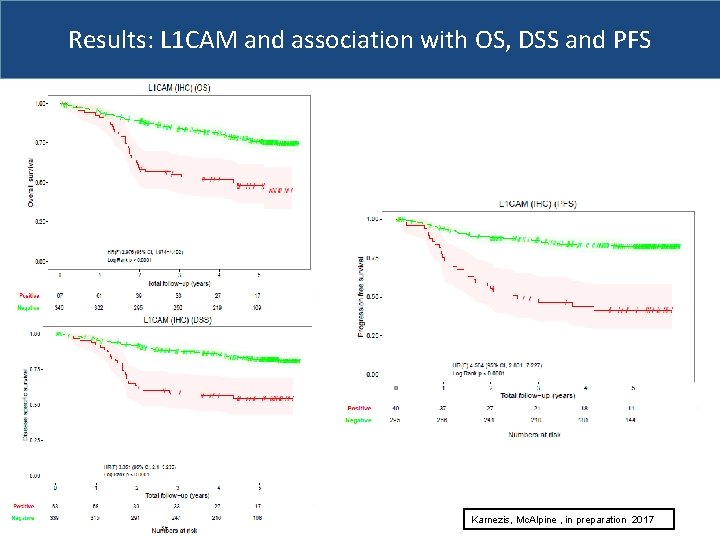
Results: L 1 CAM and association with OS, DSS and PFS Karnezis, Mc. Alpine , in preparation 2017
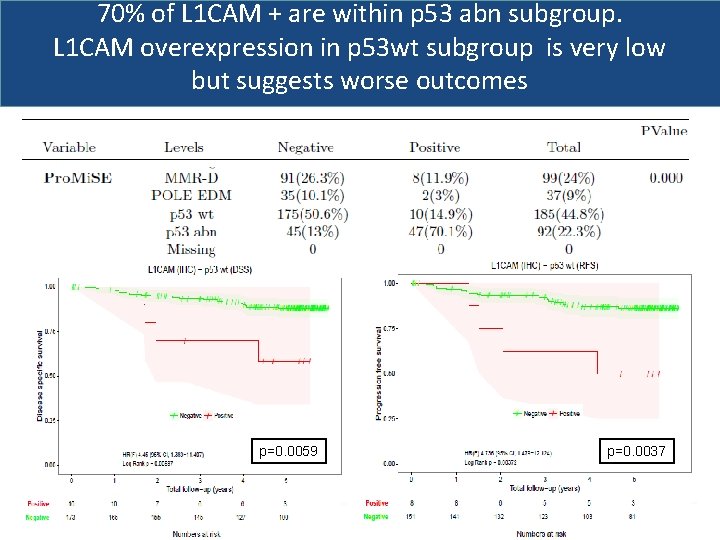
70% of L 1 CAM + are within p 53 abn subgroup. L 1 CAM overexpression in p 53 wt subgroup is very low but suggests worse outcomes p=0. 0059 p=0. 0037
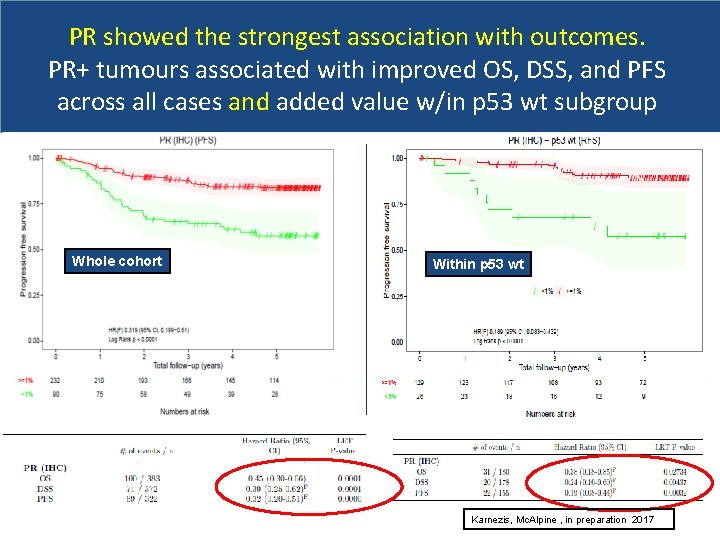
PR showed the strongest association with outcomes. PR+ tumours associated with improved OS, DSS, and PFS across all cases and added value w/in p 53 wt subgroup Whole cohort Within p 53 wt Karnezis, Mc. Alpine , in preparation 2017
Results-Multivariable analysis § Only Pro. Mis. E molecular classifier maintained prognostic significance for OS, DSS, and PFS when correcting for clinicopathologic factors and any IHC marker(s)* * Considered age, BMI, histotype, grade, any Rx, Pro. Mis. E (stage, LVSI, nodes) Next steps § Modeling what factors most important and can be used from time of first diagnosis? i. e. , IHC markers +phenotype (e. g. , age, BMI), + immunophenotype
Defining the immune landscape in endometrial cancers in the era of molecular classification
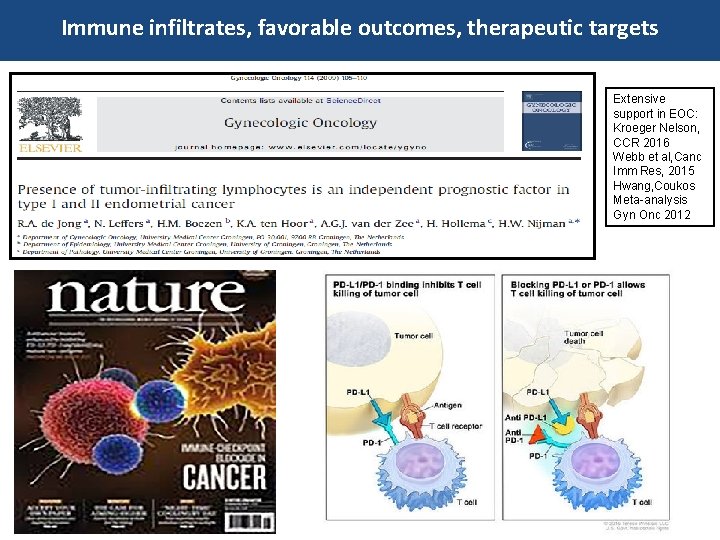
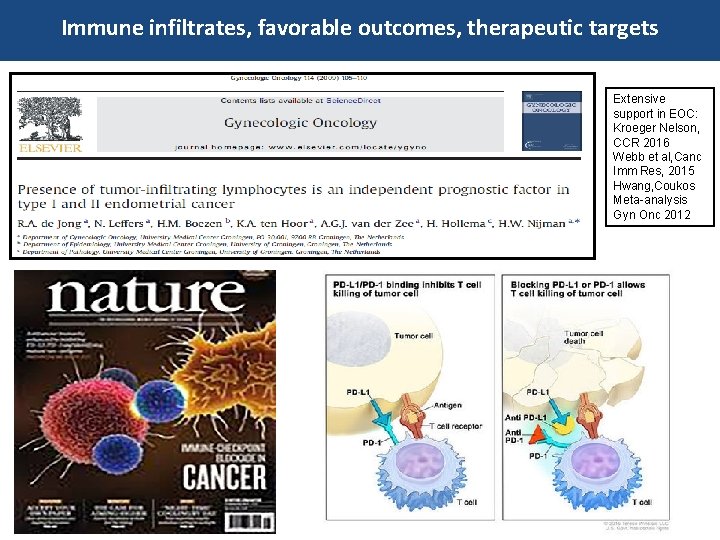
Immune infiltrates, favorable outcomes, therapeutic targets Extensive support in EOC: Kroeger Nelson, CCR 2016 Webb et al, Canc Imm Res, 2015 Hwang, Coukos Meta-analysis Gyn Onc 2012
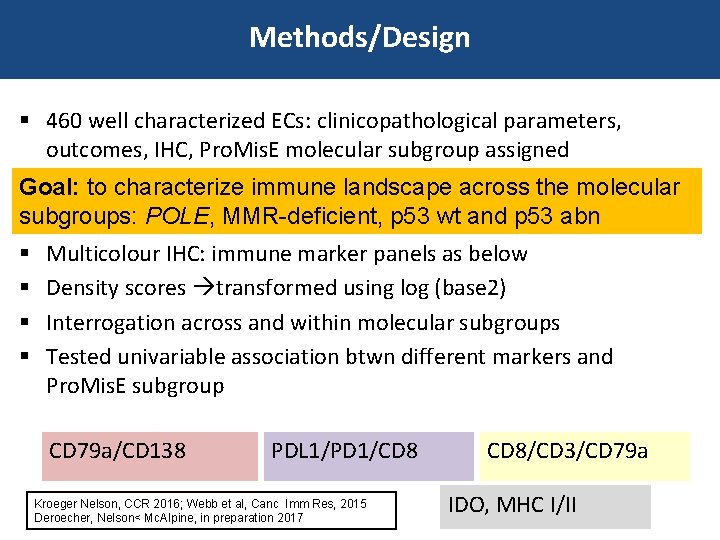
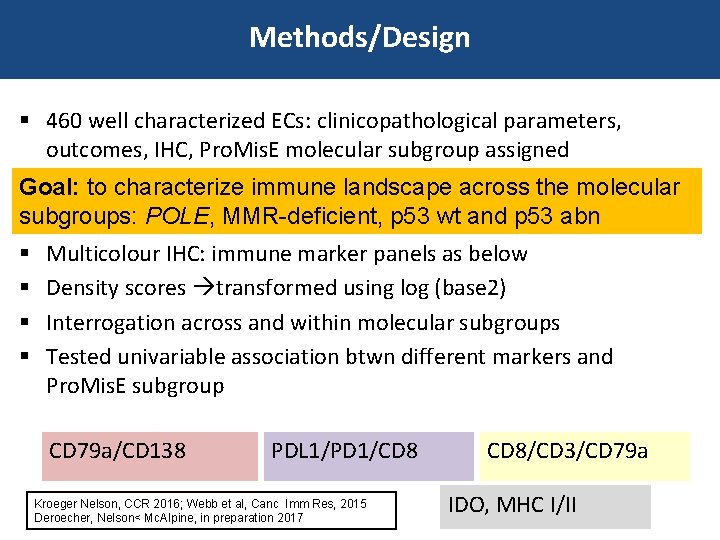
Methods/Design § 460 well characterized ECs: clinicopathological parameters, outcomes, IHC, Pro. Mis. E molecular subgroup assigned Goal: to characterize immune landscape across the molecular subgroups: POLE, MMR-deficient, p 53 wt and p 53 abn § § Multicolour IHC: immune marker panels as below Density scores transformed using log (base 2) Interrogation across and within molecular subgroups Tested univariable association btwn different markers and Pro. Mis. E subgroup CD 79 a/CD 138 PDL 1/PD 1/CD 8 Kroeger Nelson, CCR 2016; Webb et al, Canc Imm Res, 2015 Deroecher, Nelson< Mc. Alpine, in preparation 2017 CD 8/CD 3/CD 79 a IDO, MHC I/II
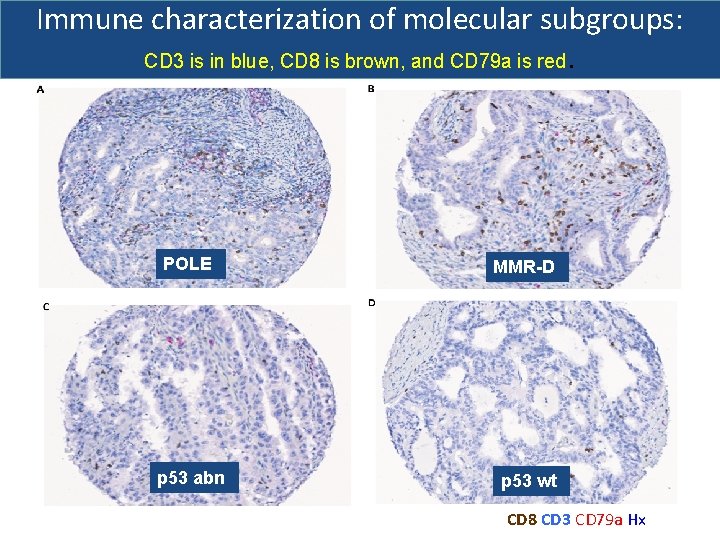
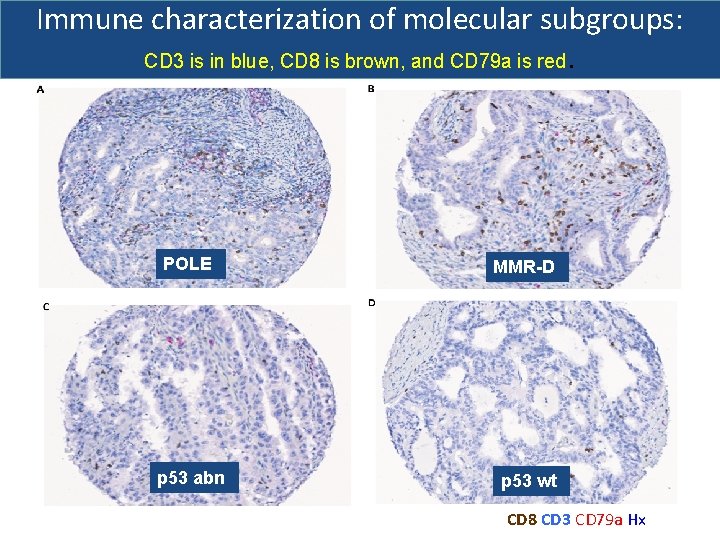
Immune characterization of molecular subgroups: CD 3 is in blue, CD 8 is brown, and CD 79 a is red. POLE MMR-D p 53 abn p 53 wt CD 8 CD 3 CD 79 a Hx
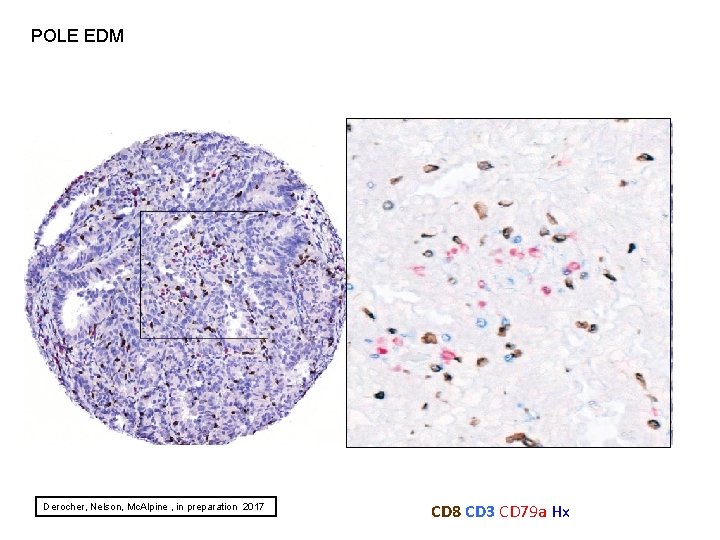
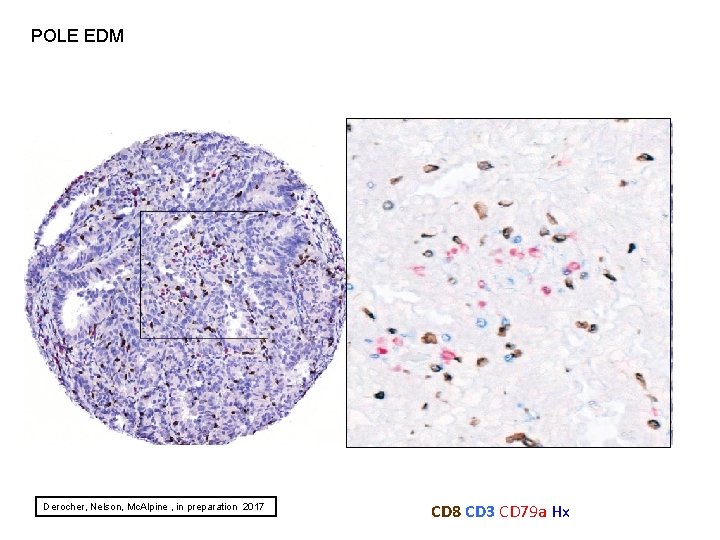
POLE EDM Derocher, Nelson, Mc. Alpine , in preparation 2017 CD 8 CD 3 CD 79 a Hx
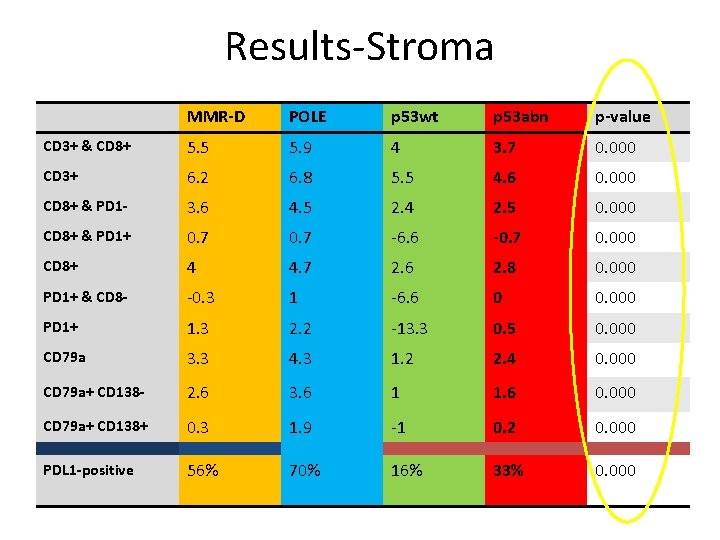
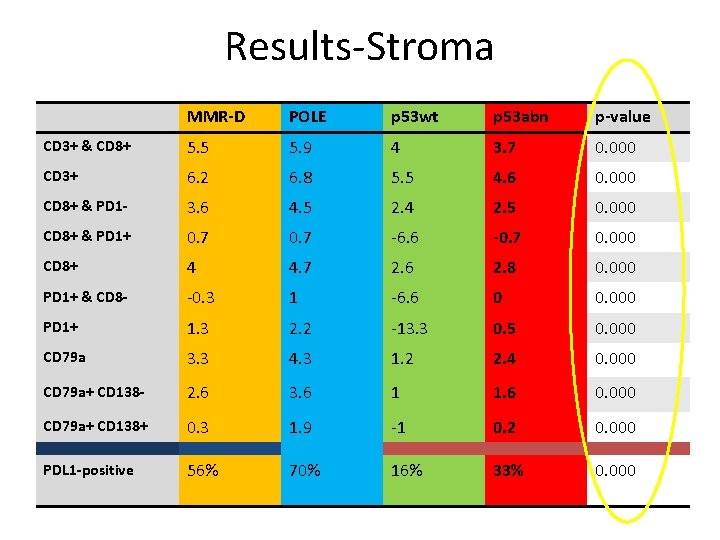
Results-Stroma MMR-D POLE p 53 wt p 53 abn p-value CD 3+ & CD 8+ 5. 5 5. 9 4 3. 7 0. 000 CD 3+ 6. 2 6. 8 5. 5 4. 6 0. 000 CD 8+ & PD 1 - 3. 6 4. 5 2. 4 2. 5 0. 000 CD 8+ & PD 1+ 0. 7 -6. 6 -0. 7 0. 000 CD 8+ 4 4. 7 2. 6 2. 8 0. 000 PD 1+ & CD 8 - -0. 3 1 -6. 6 0 0. 000 PD 1+ 1. 3 2. 2 -13. 3 0. 5 0. 000 CD 79 a 3. 3 4. 3 1. 2 2. 4 0. 000 CD 79 a+ CD 138 - 2. 6 3. 6 1 1. 6 0. 000 CD 79 a+ CD 138+ 0. 3 1. 9 -1 0. 2 0. 000 PDL 1 -positive 56% 70% 16% 33% 0. 000
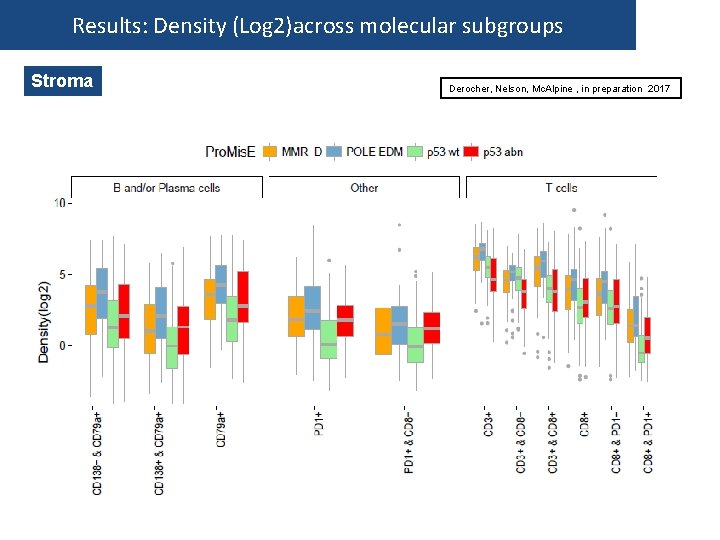
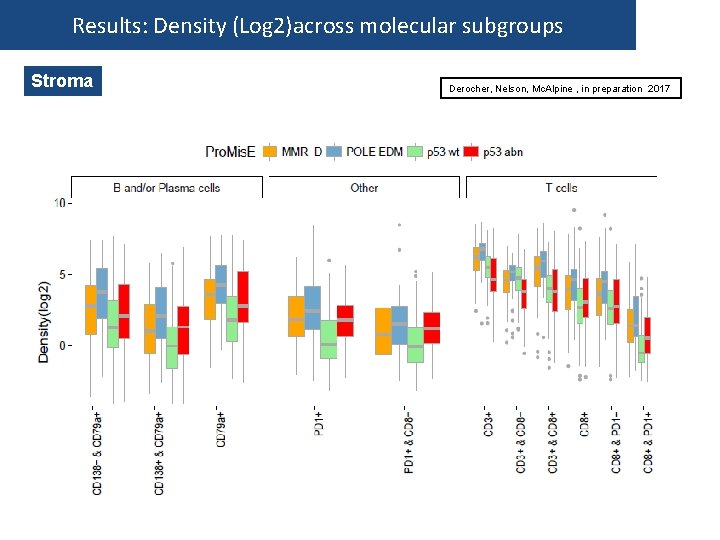
Results: Density (Log 2)across molecular subgroups Stroma Derocher, Nelson, Mc. Alpine , in preparation 2017
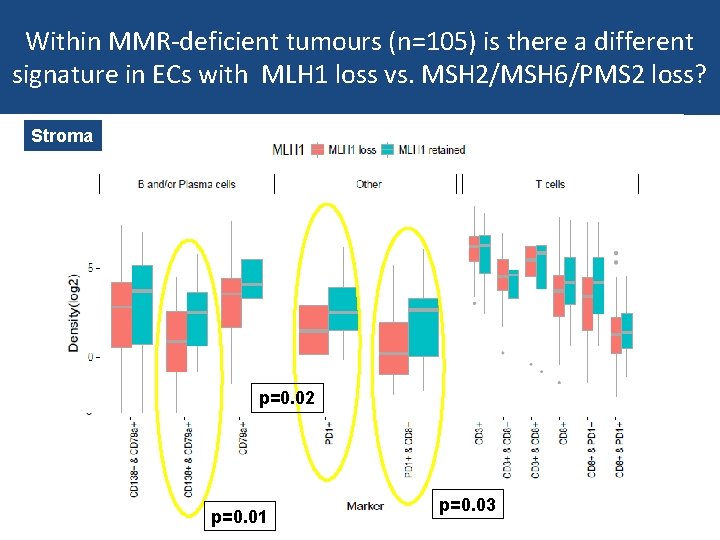
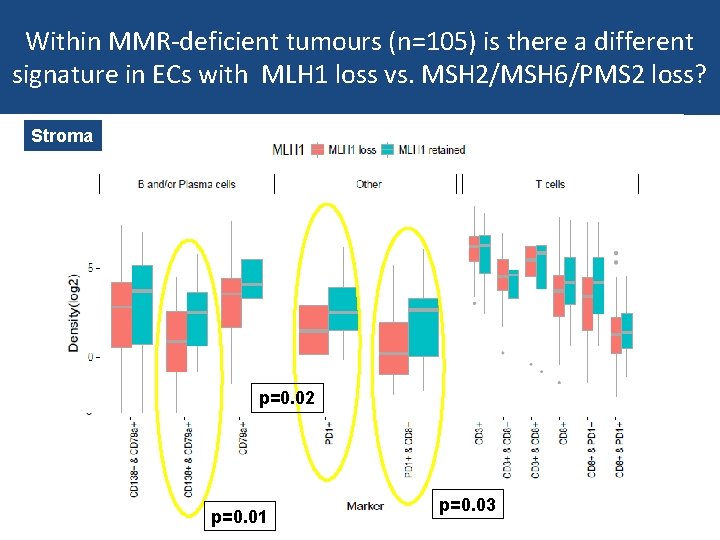
Within MMR-deficient tumours (n=105) is there a different signature in ECs with MLH 1 loss vs. MSH 2/MSH 6/PMS 2 loss? Stroma p=0. 02 p=0. 01 p=0. 03
Grade 3 endometrioid endometrial cancer project Tjalling Bosse 37 Insert > Header & footer 21 -Feb-21
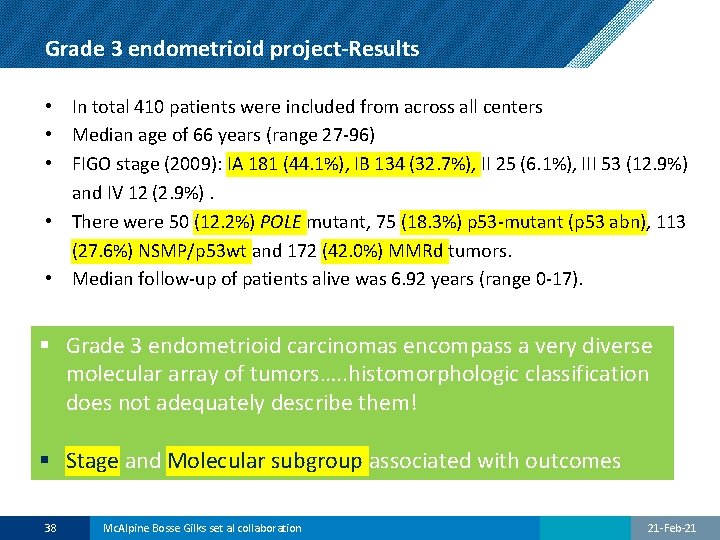
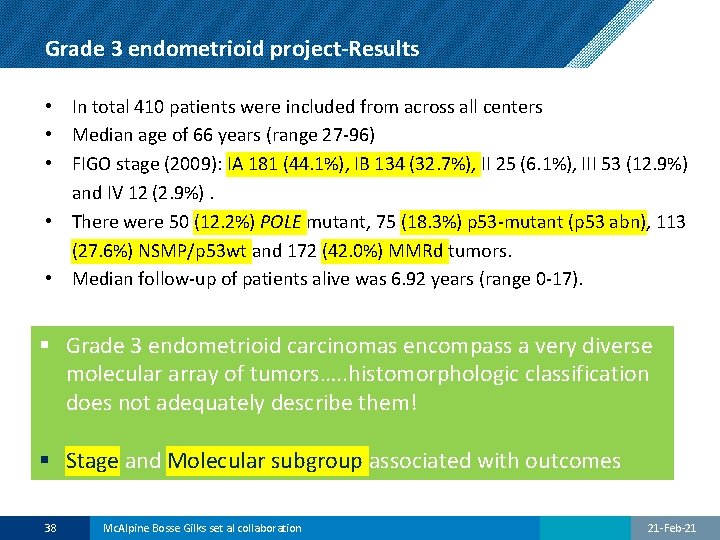
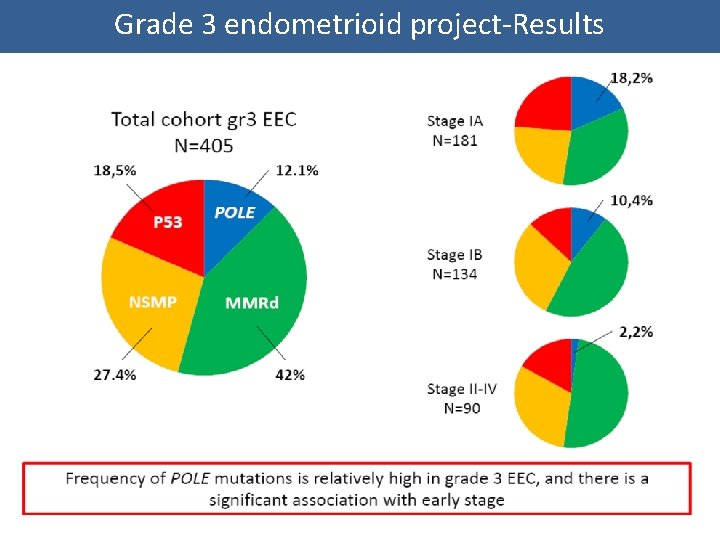
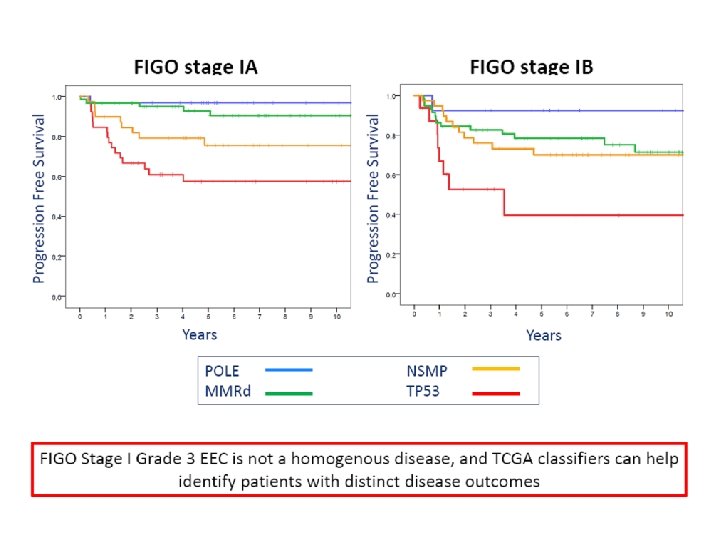
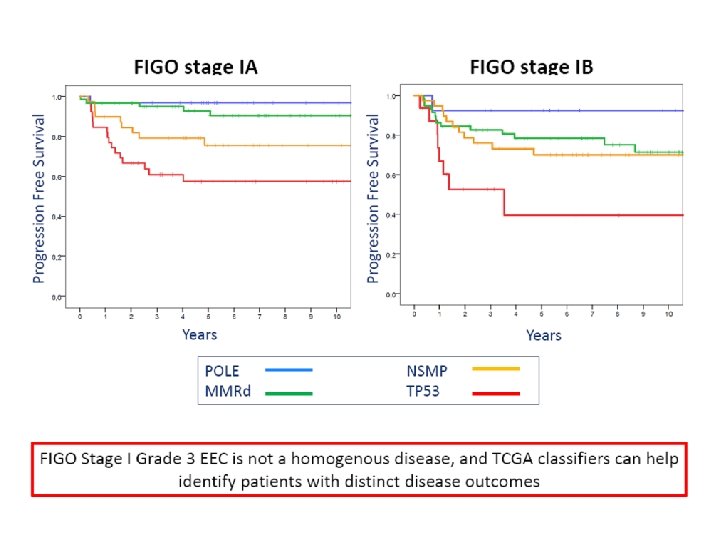
Grade 3 endometrioid project-Results • In total 410 patients were included from across all centers • Median age of 66 years (range 27 -96) • FIGO stage (2009): IA 181 (44. 1%), IB 134 (32. 7%), II 25 (6. 1%), III 53 (12. 9%) and IV 12 (2. 9%). • There were 50 (12. 2%) POLE mutant, 75 (18. 3%) p 53 -mutant (p 53 abn), 113 (27. 6%) NSMP/p 53 wt and 172 (42. 0%) MMRd tumors. • Median follow-up of patients alive was 6. 92 years (range 0 -17). § Grade 3 endometrioid carcinomas encompass a very diverse molecular array of tumors…. . histomorphologic classification does not adequately describe them! § Stage and Molecular subgroup associated with outcomes 38 Mc. Alpine Bosse Gilks set al collaboration 21 -Feb-21
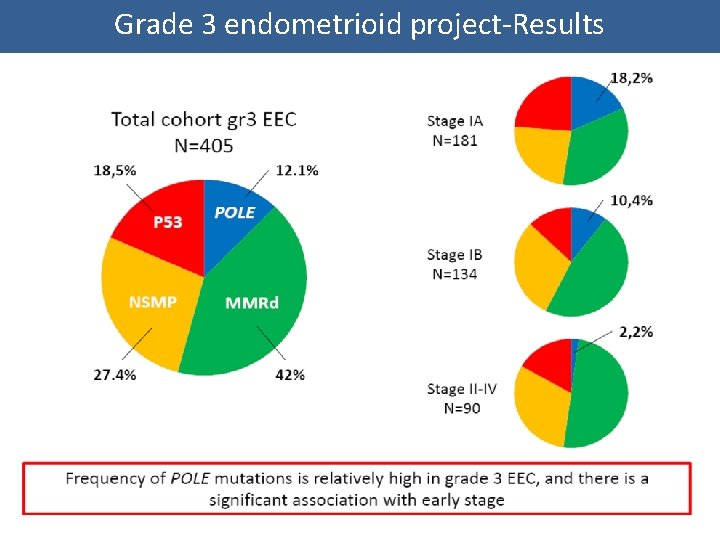
Grade 3 endometrioid project-Results
Endometrial cancer: Other challenges Intratumoral heterogeneity, management of young women, synchronous tumours
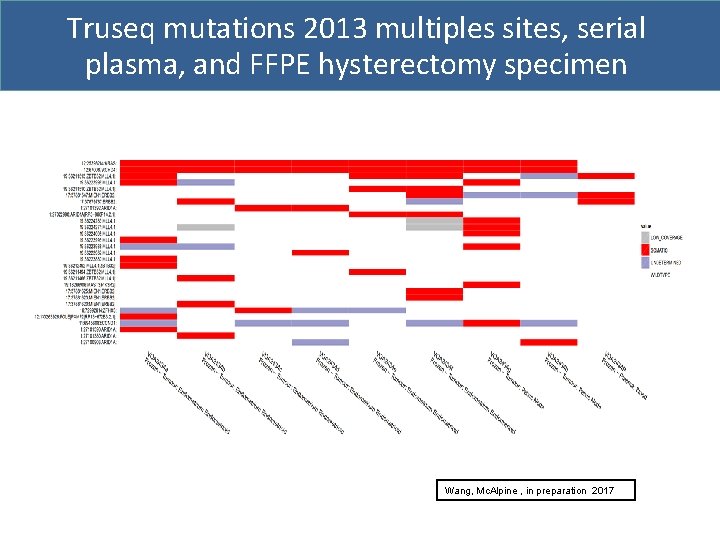
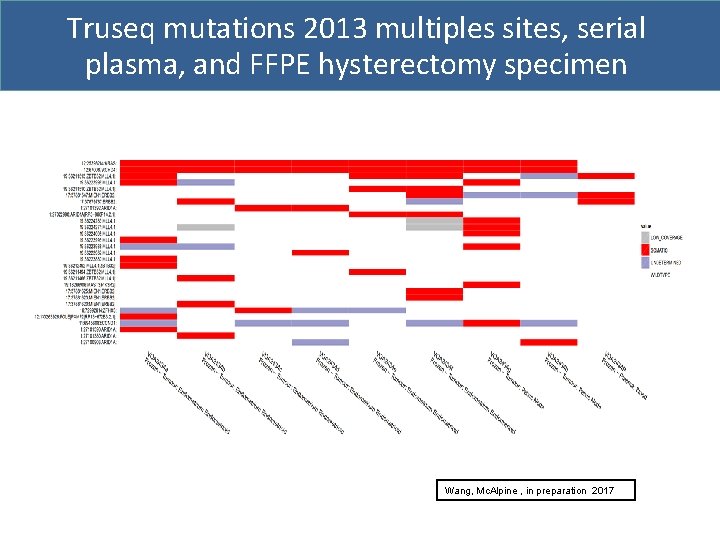
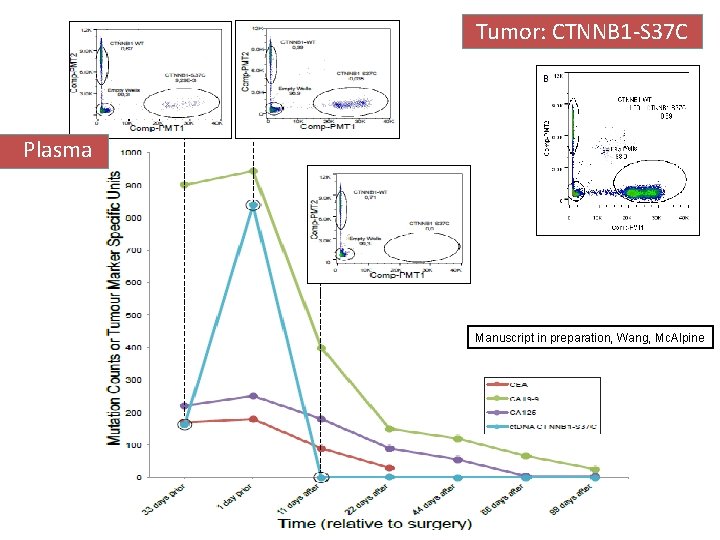
Truseq mutations 2013 multiples sites, serial plasma, and FFPE hysterectomy specimen Wang, Mc. Alpine , in preparation 2017
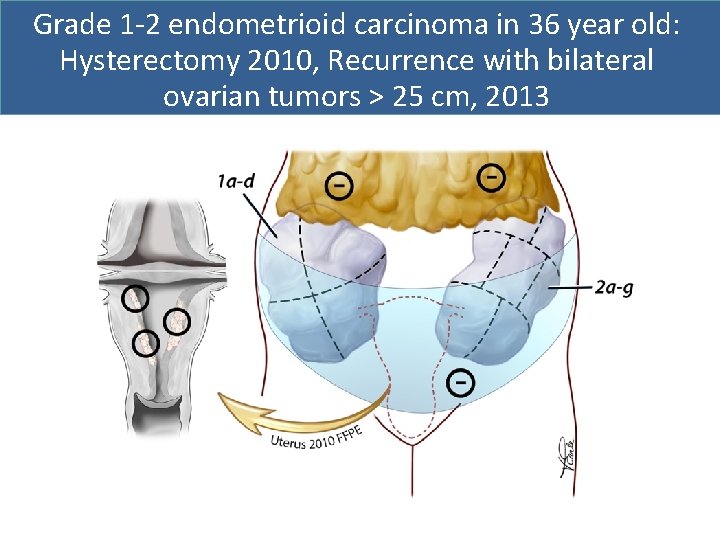
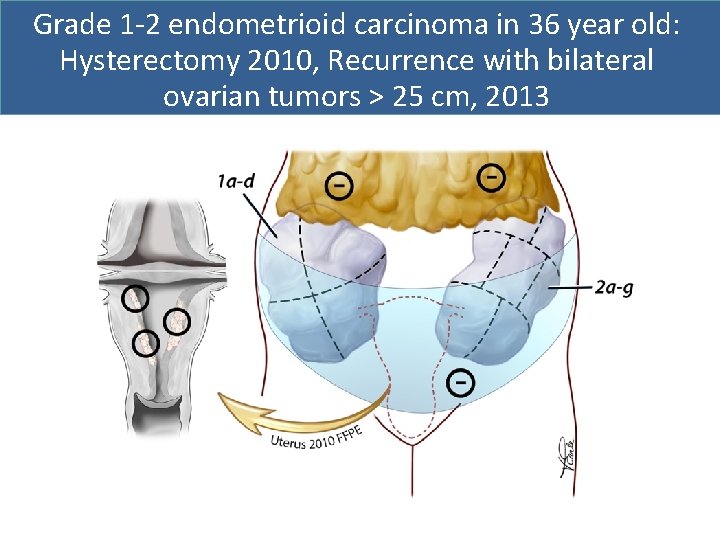
Grade 1 -2 endometrioid carcinoma in 36 year old: Hysterectomy 2010, Recurrence with bilateral ovarian tumors > 25 cm, 2013
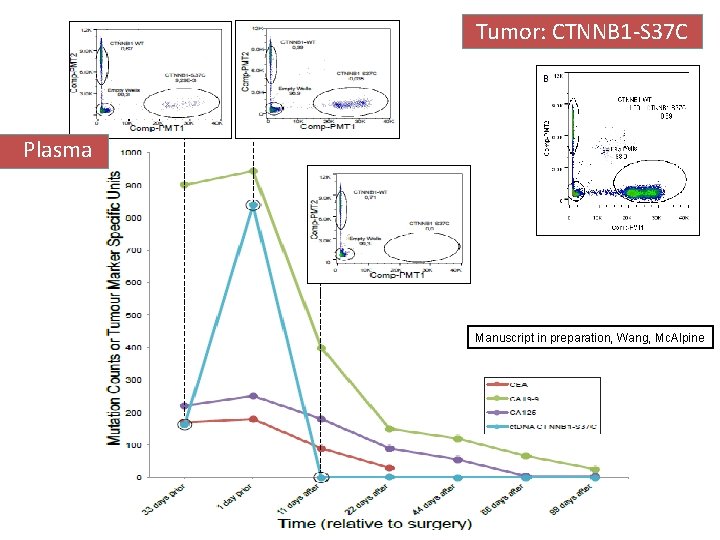
Tumor: CTNNB 1 -S 37 C Plasma Manuscript in preparation, Wang, Mc. Alpine
Summary: What will molecular classification yield? ØReproducible classification ØRisk stratification-biologically informative stratification of trials ØEarly referral to hereditary cancer program/Lynch ØEarlier information to help decisions ØFuture: guide management ØSurgery-how aggressive? Who performs? ØImmune modulator/targeted therapy-best candidates ØInformed surveillance-based on prognosis
Next/in progress 1. Testing across centers/pathology laboratories 2. Modeling-what key parameters add value to Pro. Mis. E 3. POLE subgroups-are good outcomes independent of treatment? 4. Apply classifier to specific subgroups i. e. young♀ 5. Health economic analysis 6. Stratify care-clinical trial

Acknowledgements BCCRC DG Huntsman M Mc. Conechy N Boyd A Lum W Yang Y Ng S Padilla J Magrill UBC & BCCA Clinical Dianne Miller Janice Kwon Judith Pike Sarah Finlayson Gavin Stuart Mark Carey Mark Heywood Marette Lee Paul Hoskins Anna Tinker Susan Ellard Trevor Cohen Mona Mazgani Pathology C Blake Gilks L Hoang CH Lee MSKCC- Pathology R Soslow Deeley Cancer Center B Nelson H Derocher K Milne U of Calgary- Pathology M Kobel Presented by: Jessica Mc. Alpine Statistics/modeling A Talhouk S Leung Health economics Gillian Hanley Janice Kwon
EXTRA SLIDES
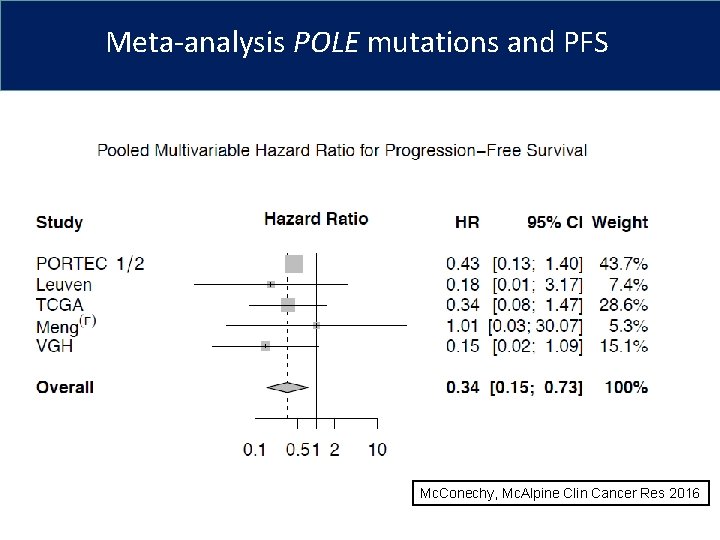
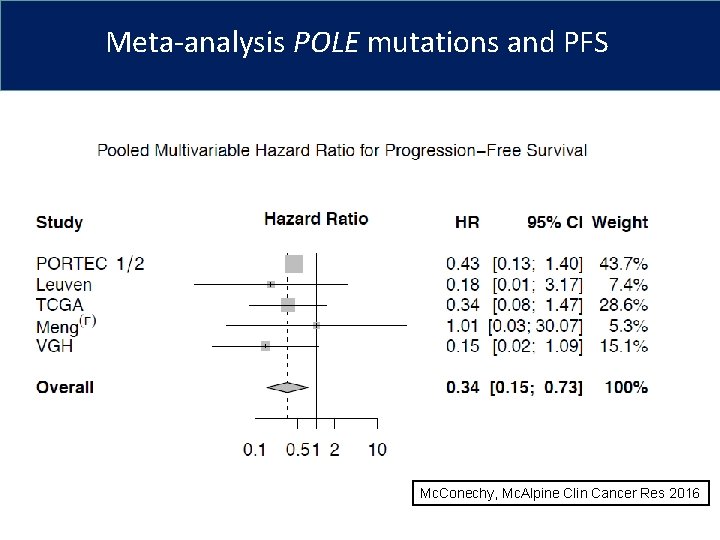
Meta-analysis POLE mutations and PFS Mc. Conechy, Mc. Alpine Clin Cancer Res 2016