Module Health Psychology Lecture Chronic illness and somatisation



- Slides: 27
Module: Health Psychology Lecture: Chronic illness and somatisation Date: 16 March 2009 Chris Bridle, Ph. D, CPsychol Associate Professor (Reader) Warwick Medical School University of Warwick Tel: +44(24) 761 50222 Email: C. Bridle@warwick. ac. uk www. warwick. ac. uk/go/hpsych
Aims and Objectives n n Aim: To provide an overview of the psychological aspects of chronic illness and somatisation Objectives: You should be able to describe … n common somatoform symptoms; n characteristics of somatoform disorders; n cause, course and consequence of somatoform disorders; n n principles of assessment, treatment and management of somatoform disorders; ways to distinguish between normal and abnormal somatisation.
Greek Origin n Σωμα n Soma = 'the body' n Σωματικóς n Somatic = 'of the body' n ψυχή n Psyche = 'of the mind' n ψυχοσωματικός n Psychosomatic = 'influence of the mind on the body'

Terminology § § § Somatic symptoms: physical symptoms (assumption: with physiological cause) Somatoform symptoms: physical symptoms without (identifiable) physiological cause Psychosomatic symptoms: physical symptoms with psychological cause Somatopsychic symptoms: psychological symptoms with physiological cause Somatisation: expression of emotional problems in somatic symptoms Somatic fixation: bias towards (automatic) medicalisation of symptoms
Somatisation 'Somatisation is a ubiquitous and diverse process in medicine, linking the physiology of distress and the psychology of symptom perception' Joseph Ransohoff (1915 - 2001) '. . . the history of medicine has written the prehistory of psychosomatics' William Osler (1849 - 1919) 'Representation of the bodily processing of emotion' Leonardo da Vinci (1452 - 1519)
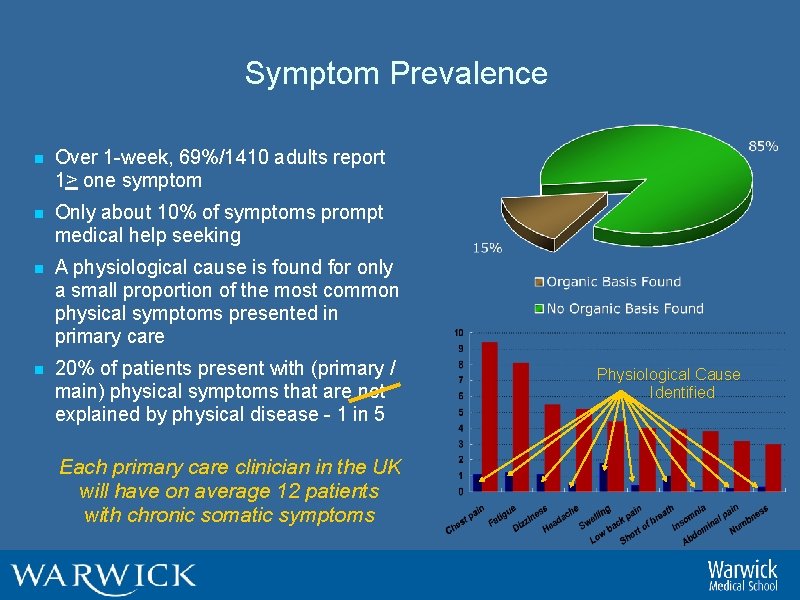
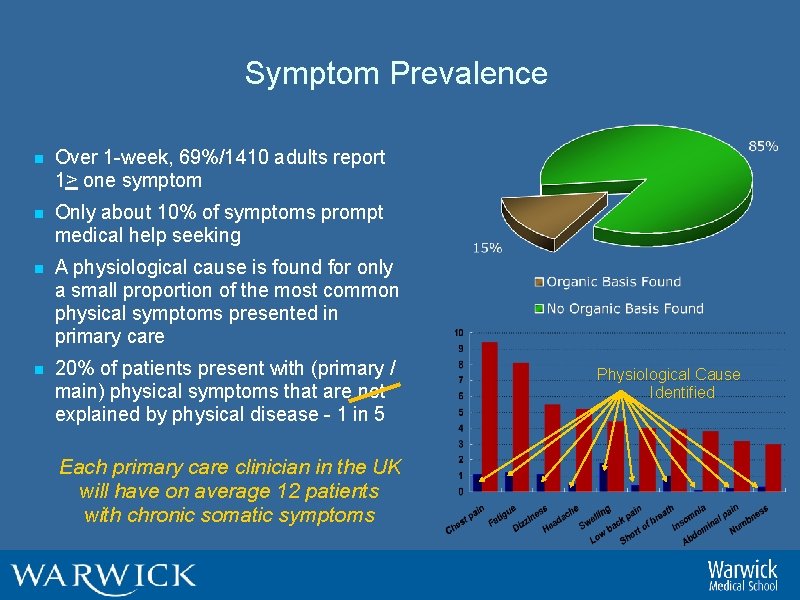
Symptom Prevalence n Over 1 -week, 69%/1410 adults report 1> one symptom n Only about 10% of symptoms prompt medical help seeking n A physiological cause is found for only a small proportion of the most common physical symptoms presented in primary care n 20% of patients present with (primary / main) physical symptoms that are not explained by physical disease - 1 in 5 Each primary care clinician in the UK will have on average 12 patients with chronic somatic symptoms Physiological Cause Identified
Symptom Presentation n Of all the symptoms for which an identifiable physiological cause can not be found, the most common are: n Pain: related to different sites (e. g. head, abdomen, back) or bodily functions (e. g. menstruation, intercourse, urination) n Gastrointestinal: nausea, bloating, vomiting (not during pregnancy), diarrhoea, intolerance of several foods n Sexual: indifference to sex, difficulties with erection or ejaculation, irregular menses, excessive menstrual bleeding n Pseudoneurological: voice loss, impaired vision, hearing and balance/coordination, paralysis, hallucination, seizure, amnesia
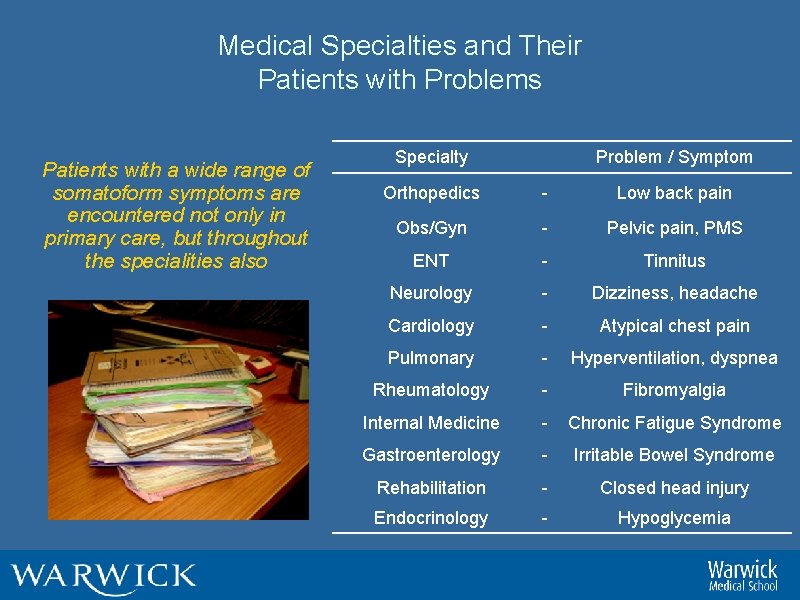
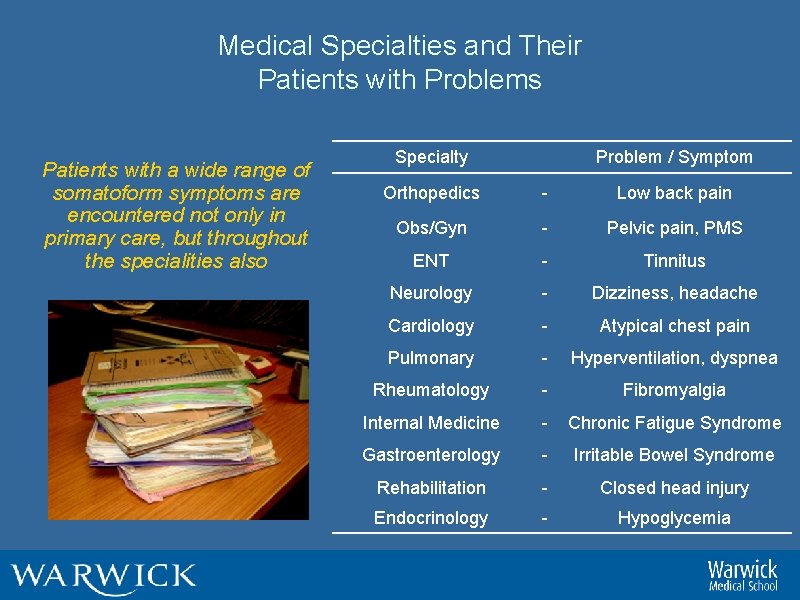
Medical Specialties and Their Patients with Problems Patients with a wide range of somatoform symptoms are encountered not only in primary care, but throughout the specialities also Specialty Problem / Symptom Orthopedics - Low back pain Obs/Gyn - Pelvic pain, PMS ENT - Tinnitus Neurology - Dizziness, headache Cardiology - Atypical chest pain Pulmonary - Hyperventilation, dyspnea Rheumatology - Fibromyalgia Internal Medicine - Chronic Fatigue Syndrome Gastroenterology - Irritable Bowel Syndrome Rehabilitation - Closed head injury Endocrinology - Hypoglycemia

Characteristics of Somatoform Disorders n A class of disorder defined by n n presence of physical symptoms that are not fully explained by the presence of a medical condition; symptoms cause clinically significant distress and impairment; psychological factors judged important in symptom onset, severity, and/or maintenance; symptoms are chronic, independent of one another and not intentionally produced.
Somatoform Disorders n Somatisation disorder (Briquet's syndrome): A history of many physical complaints beginning before age 30 years that occur over a period of several years and result in treatment being sought n Conversion disorder (conversion hysteria): Symptoms or deficits affecting voluntary motor or sensory function n Hypochondriacal disorder (hypochondriasis): Preoccupation with fears of developing or having a serious disease, based on (mis)interpretation of bodily symptoms, which persist despite medical reassurance n Somatoform pain disorder (psychogenic pain): Disabling pain of sufficient severity to cause treatment being sought n Body dysmorphic disorder (dysmorphophobia): Preoccupation with an imagined defect in appearance, or if real / present, concern is markedly excessive
Somatisation Disorder n Description: A history of many physical complaints beginning before age 30 years that occur over a period of several years and results in treatment being sought or significant impairment in social, occupational or other areas of functioning n Epidemiology: 10 X> females, familial pattern for 10 -20% of 1 st degree female relatives; n Course: Chronic, fluctuating and rarely remits. Diagnostic criteria usually met before age 25 yrs. n Cues: Symptom onset / progression following loss; symptom amplification with stress n Other features: Complicated medical history; numerous (12+) somatic complaints; Dr shopping
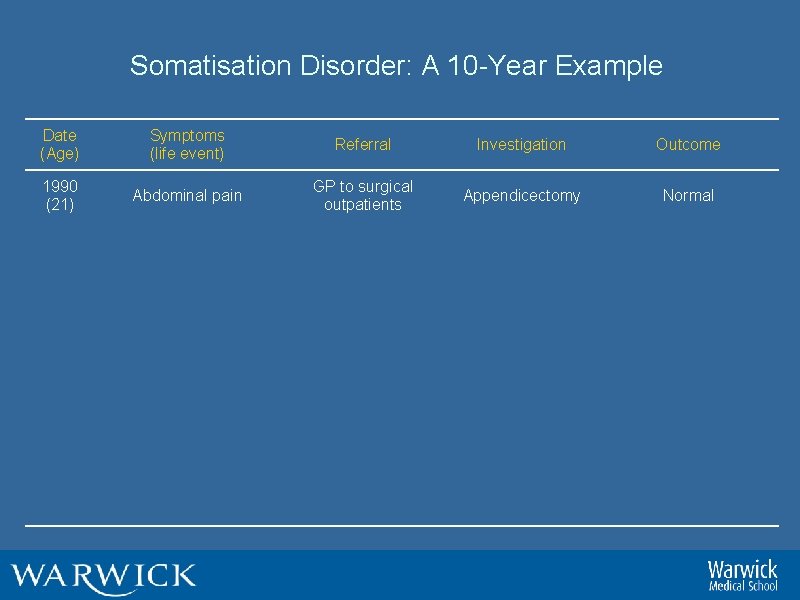
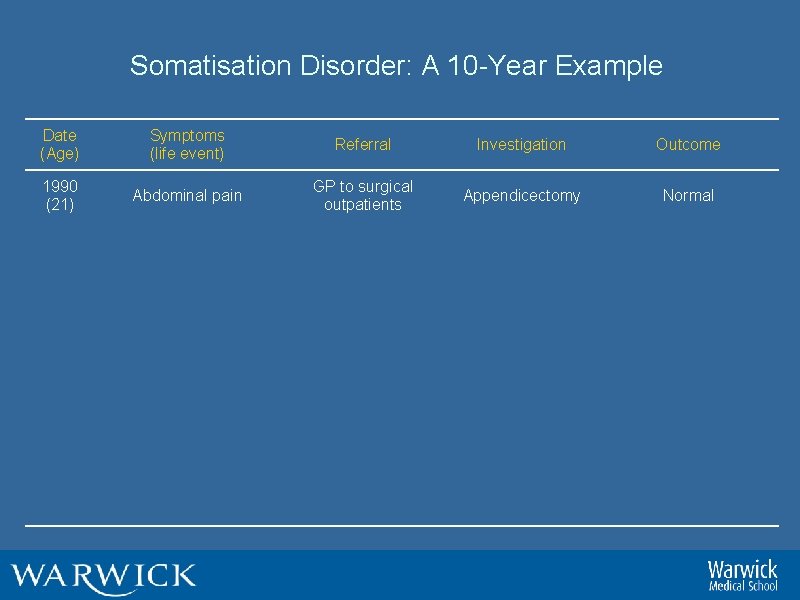
Somatisation Disorder: A 10 -Year Example Date (Age) Symptoms (life event) Referral Investigation Outcome 1990 (21) Abdominal pain GP to surgical outpatients Appendicectomy Normal 1992 (23) Nausea (boyfriend in prison) GP to Obs/Gyn outpatient Pregnant Termination of pregnancy 1994 (25) Bloating, abdominal pain, (divorce) GP to gastro outpatient All tests normal IBS diagnosis; treat with Fybogel 1995 (26) Pelvic pain (wants sterilisation) GP to O&G outpatient Sterilised Pelvic pain for 2 yrs post-surgery 1997 (28) Fatigue (dissatisfied at work) GP to infectious disease clinic All tests normal Self-diagnosed ME, joins self-help group 1998 (29) Aching, painful muscles GP to rheumatology clinic Mild cervical spondylosis Tryptizol 50 mg, pain clinic referral 1999 (30) Chest pain (lost job) A&E to chest clinic Normal; probable hyperventilation Refer to psychiatric services
Conversion Disorder n Description: Symptoms or deficits affecting voluntary motor or sensory function n Epidemiology: Rare condition; acute onset in adolescence or early adulthood; twice as prevalent in females; more common in rural populations and lower SES n Course: Recurrent symptoms with short duration n Cues: Traumatic events; stress; Samuel Pepys recorded inability to cope conversion disorder after the n Other features: high suggestibility; prone to seizures and convulsions; unaware of retained functions Great Fire of London in 1666
Hypochondriacal Disorder n Description: Preoccupation with fears of developing or having a serious disease based on (mis)interpretation of bodily symptoms, which persists despite medical reassurance n Epidemiology: About 3% and 5% prevalence among general population and primary care outpatients, respectively n Course: Onset at any age, but typically early adulthood; familial deaths and illness; media n Cues: Heightened awareness of physical self; symptom amplification when stressed n Other features: Dr Shopping; background expertise

Somatoform Pain Disorder n Description: Pain of sufficient severity to cause clinically significant distress or impairment and treatment being sought n Epidemiology: Precise prevalence unknown but likely to be fairly common; small female bias possible; variable onset age n Course: Chronic, fluctuating and rarely remits n Cues: Often develops from illness or accidental injury; symptom amplification when exposed to illness, accident cues and stress n Other features: Dr shopping (often precipitated by maximum dose); risk for multiple registrations; pharmacologically informed; initiated and discontinued various CAM formulations
Body Dysmorphic Disorder (BDD) n Description: Preoccupation with an imagined defect in appearance, or if present, concern is markedly excessive n Epidemiology: Prevalence unknown in general population; 1030% in mental health settings n Course: Onset early adulthood; increasingly distressing; potential for suicidal ideation n Cues: Unclear; possible sensitivity / bias to facial feature priming n Other features: Typically remain single; examined potential for plastic surgery BDD?
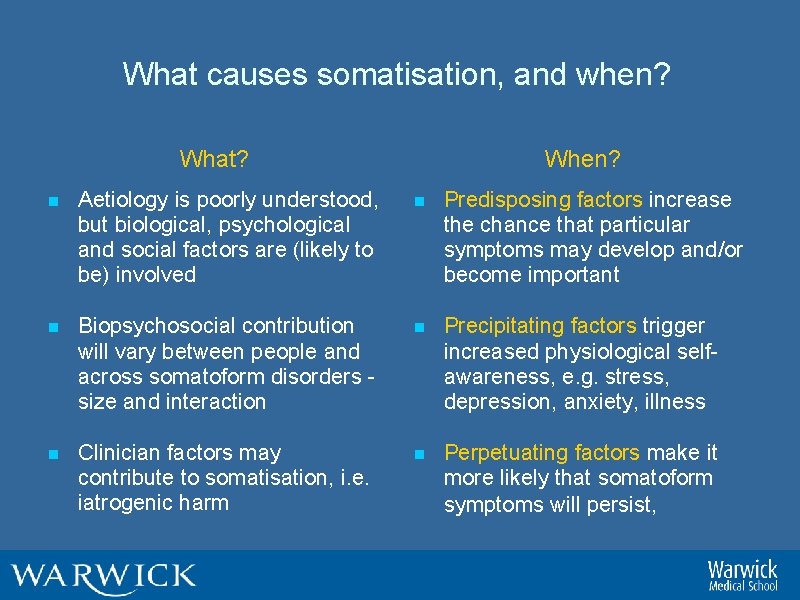
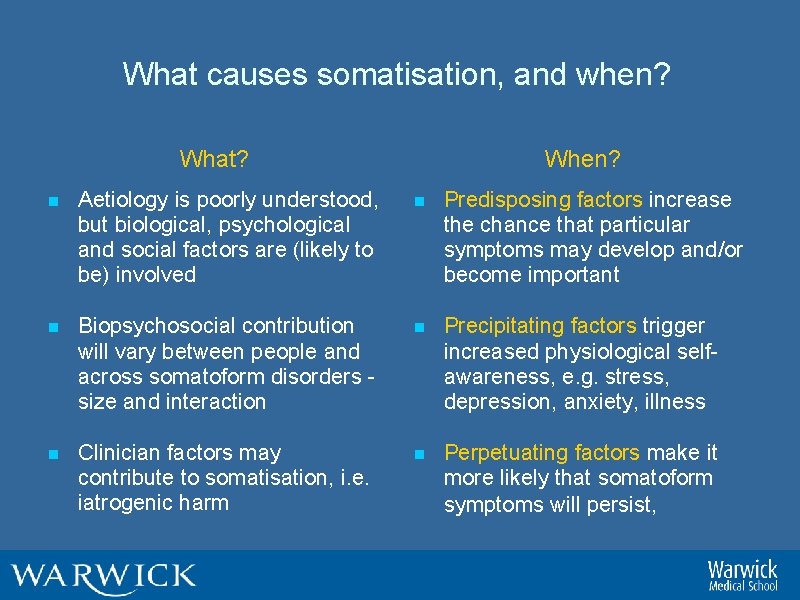
What causes somatisation, and when? What? When? n Aetiology is poorly understood, but biological, psychological and social factors are (likely to be) involved n Predisposing factors increase the chance that particular symptoms may develop and/or become important n Biopsychosocial contribution will vary between people and across somatoform disorders - size and interaction n Precipitating factors trigger increased physiological selfawareness, e. g. stress, depression, anxiety, illness n Clinician factors may contribute to somatisation, i. e. iatrogenic harm n Perpetuating factors make it more likely that somatoform symptoms will persist,
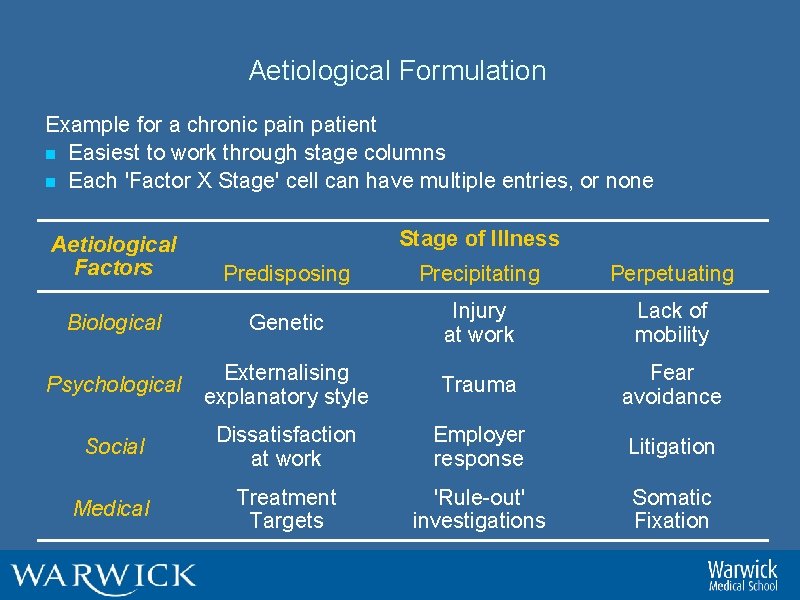
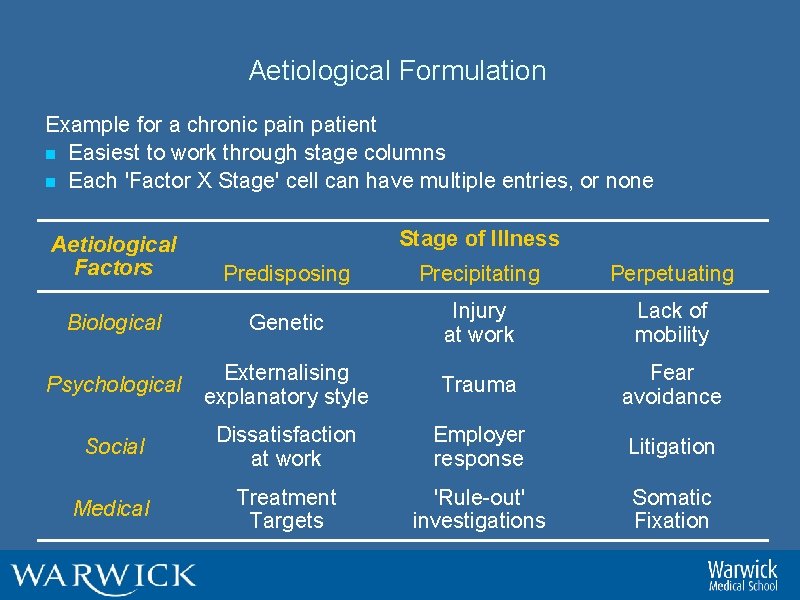
Aetiological Formulation Example for a chronic pain patient n Easiest to work through stage columns n Each 'Factor X Stage' cell can have multiple entries, or none Stage of Illness Aetiological Factors Predisposing Precipitating Perpetuating Biological Genetic Injury at work Lack of mobility Psychological Externalising explanatory style Trauma Fear avoidance Social Dissatisfaction at work Employer response Litigation Medical Treatment Targets 'Rule-out' investigations Somatic Fixation
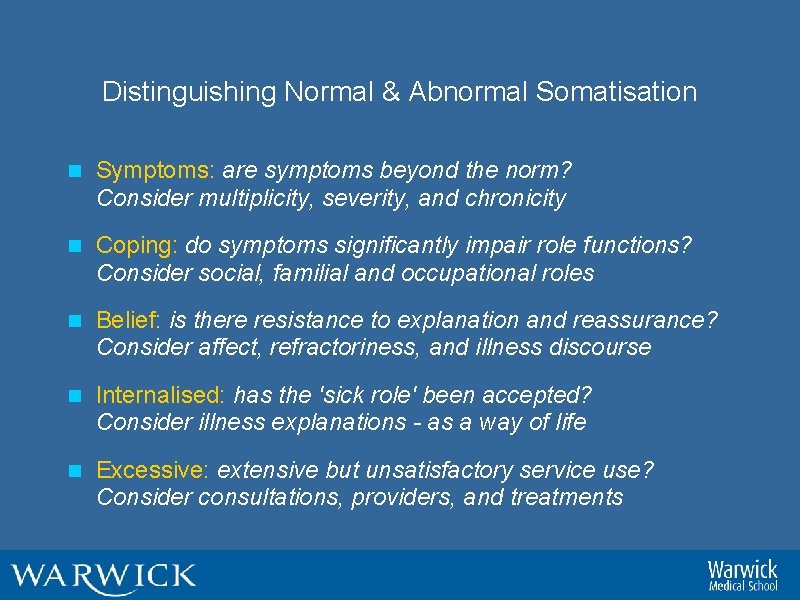
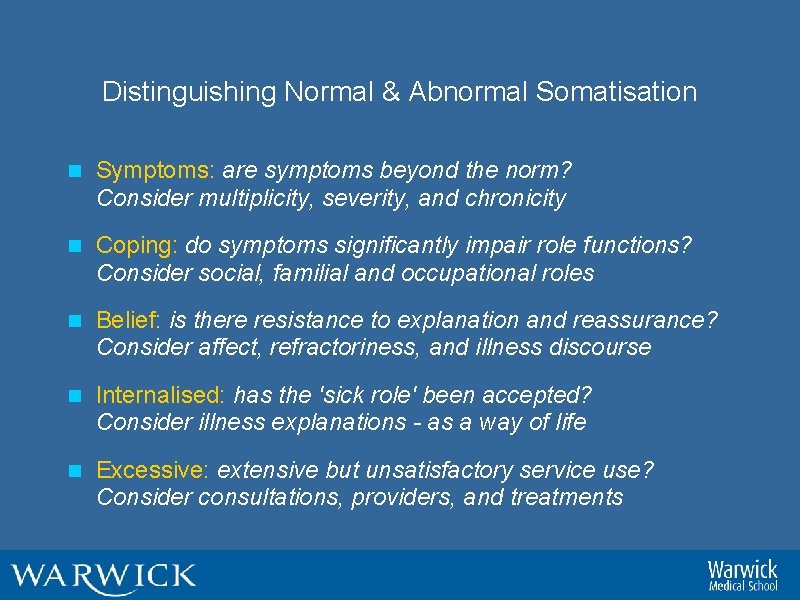
Distinguishing Normal & Abnormal Somatisation n Symptoms: are symptoms beyond the norm? Consider multiplicity, severity, and chronicity n Coping: do symptoms significantly impair role functions? Consider social, familial and occupational roles n Belief: is there resistance to explanation and reassurance? Consider affect, refractoriness, and illness discourse n Internalised: has the 'sick role' been accepted? Consider illness explanations - as a way of life n Excessive: extensive but unsatisfactory service use? Consider consultations, providers, and treatments
Principles of Assessment n Be vigilant to iatrogenic harm, e. g. be a part of the solution and not the problem n Identify patients' concerns and beliefs, e. g. illness representation n Contextualise patients' health-related experiences, e. g. previous illness, symptoms, contact with medical services, etc. n Review recent history of current symptoms, paying particular attention to possible life events, i. e. stressors n Ask questions about patients' reaction to and coping with symptoms, e. g. habitual patterns of poor coping n Use screening questions for psychiatric morbidity
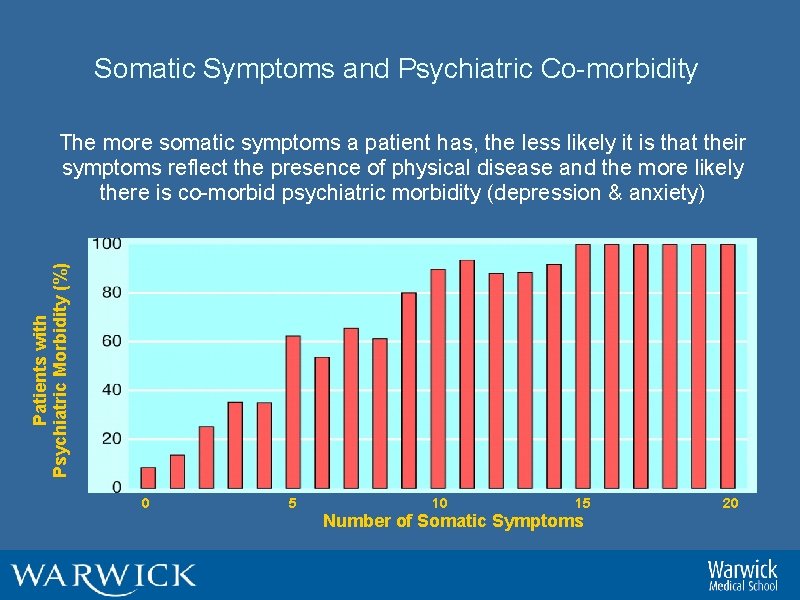
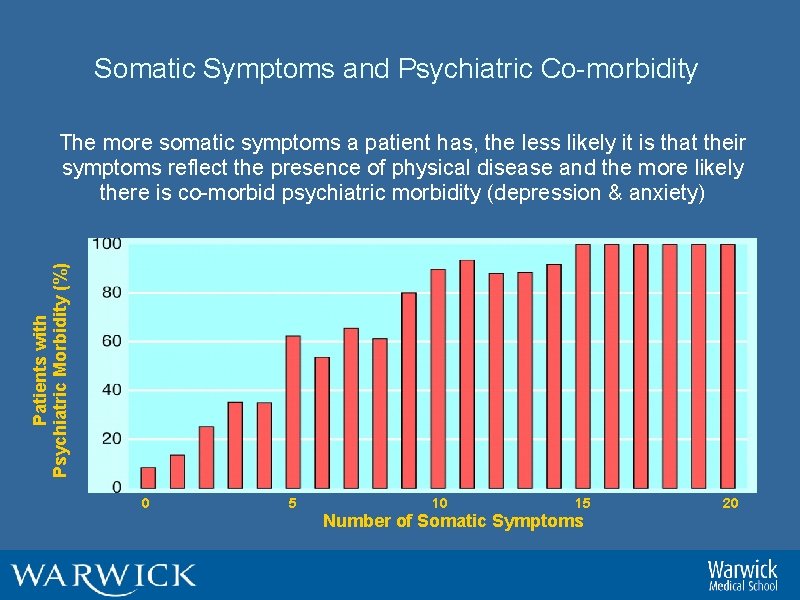
Somatic Symptoms and Psychiatric Co-morbidity Patients with Psychiatric Morbidity (%) The more somatic symptoms a patient has, the less likely it is that their symptoms reflect the presence of physical disease and the more likely there is co-morbid psychiatric morbidity (depression & anxiety) 0 5 10 15 Number of Somatic Symptoms 20
Principles of Treatment n Validate patient experience, e. g. explain that the symptoms are real and familiar to doctor n Provide a framework, e. g. describe how psychological factors (ABC) may exacerbate somatic symptoms n Offer opportunity for discussion of patient's worries at the earliest opportunity n Give practical advice on coping with symptoms and encourage return to normal activity as soon as possible n Discuss and agree a treatment plan that includes a planned follow up and review n Encourage specific tasks before next meeting, e. g. identify three situations that worsen symptoms
Treatment Aims n Treatment focus should be on coping with symptoms and impairment rather than on symptomatic cure n Target perpetuating factors n Depression, anxiety, or panic disorder n Chronic marital or family discord n Dependent or avoidant personality traits n Occupational stress n Abnormal illness beliefs n Iatrogenic factors n Pending medico-legal claim
Management Strategy n Proactive not reactive: arrange to see patients at regular, fixed intervals n Broaden agenda: establish a problem list and allow patients to discuss relevant problems n Minimise providers: only one or two providers to reduce iatrogenic harm n Co-opt a relative: a therapeutic ally to help implement and monitor the management plan n Cope not cure: cure is an unrealistic expectation, instead aim for containment and damage limitation, and remind patient at each consultation
Conclusions n Common: Somatoform symptoms are common and occur in all medical specialities n Harm: Somatisation is chronic, disabling, distressing and destructive n Cause: Multiple biological, psychological and social factors predispose, precipitate and perpetuate somatisation n Treatment: Focus on coping with symptoms and impairment, and removing perpetuating factors n Management: Somatisation can be managed effectively in primary care
Summary n This session would have helped you to understand … n common somatoform symptoms; n characteristics of somatoform disorders; n cause, course and consequence of somatoform disorders; n n principles of assessment, treatment and management of somatoform disorders; ways to distinguish between normal and abnormal somatisation.
Any questions? n What now? n Obtain / download one of the recommended readings n Consider today’s lecture in relation to your tutorial tasks : a) integrated template b) ESA question Tutorial begins at 3. 15 Completed templates (supported topics) available after today’s session on module webpage – tutor’s page
 Improving chronic illness care model
Improving chronic illness care model Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Historical views of mental illness psychology ocr
Historical views of mental illness psychology ocr Health psychology definition ap psychology
Health psychology definition ap psychology Conclusion of mental hygiene
Conclusion of mental hygiene Define health illness continuum
Define health illness continuum Mental health jeopardy game
Mental health jeopardy game Health illness continuum
Health illness continuum 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Flinders model of care
Flinders model of care C device module module 1
C device module module 1 Ap psychology module 2 review
Ap psychology module 2 review Module 7 research design and ethics in psychology
Module 7 research design and ethics in psychology Social psychology lecture
Social psychology lecture Forensic psychology lecture
Forensic psychology lecture Introduction to psychology lecture
Introduction to psychology lecture Definition of health psychology
Definition of health psychology Module 43 stress and health
Module 43 stress and health Healthmis.ng
Healthmis.ng Health economics lecture notes
Health economics lecture notes Module 9 gestalt psychology
Module 9 gestalt psychology Module 79 ap psychology
Module 79 ap psychology Module 62 ap psychology
Module 62 ap psychology Module 26 ap psychology
Module 26 ap psychology Fundamental attribution error
Fundamental attribution error _____ is the unselfish regard for the welfare of others.
_____ is the unselfish regard for the welfare of others. Ap psychology module 23
Ap psychology module 23 Module 16 ap psychology
Module 16 ap psychology