Module AE 0001 Introduction to Anesthesiology D John


- Slides: 51

Module AE 0001 Introduction to Anesthesiology D. John Doyle MD Ph. D FRCPC doylej@ccf. org 51 slides Rev 1. 0
ABOUT ANESTHESIOLOGY • • Goals of Anesthesia General Anesthesia Regional Anesthesia Perioperative Problems
Anesthesiology Involves. . . – Drugs and fluids – Lines and catheters – Monitors and equipment – Clinical knowledge and judgment – Technical and psychomotor skills – Team building and interpersonal relations – Crisis management and problem prevention – Dealing with patients and their fears
Anesthesia Techniques for Surgery • General Anesthesia - Spontaneous Breathing - Machine Ventilation - Cardiopulmonary Bypass • Regional Anesthesia - Epidural Spinal Plexus Block Nerve Block
Anesthesia Techniques for Surgery • Local Anesthesia (Infiltration) • Other Methods • Acupuncture • Hypnosis • Cold
What is General Anesthesia? • • Unconsciousness (no awareness) Airway Management Amnesia (no recall) Analgesia (no pain) Blunting of Reflexes Physiological Homeostasis (stability) Muscle Paralysis (sometimes)
General Anesthesia • • • Assessment Planning I: Monitors Planning II: Drugs Planning III: Fluids Planning IV: Airway Management • • Induction Maintenance Emergence Postoperative
Goals and Issues in General Anesthesia • • • Unconsciousness Amnesia Analgesia Oxygenation Ventilation Homeostasis Airway Management Reflex Management Muscle Relaxation Monitoring
Airway Management Choices • Intubation vs. LMA vs. “nothing special” • Positive pressure ventilation vs. spontaneous breathing • Intubation awake vs. asleep • Conservative vs. surgical airway • Muscle relaxant vs. none
Airway Equipment • Single Lumen Tracheal Tubes – – • • • Regular RAE Armored Nasal Double Lumen Tubes Laryngeal Mask Airway Oropharyngeal Airways Fiberoptic Intubation Cart Difficult Intubation Kit Surgical Airway Kit
Amnesia • Generally sought, but not always desirable • Lorazepam (Ativan) 2 -4 mg sublingually 60 - 90 min preop • Midazolam (Versed) 1 mg IV increments • Scopolamine (old but still effective)

Analgesia • Analgesia = no pain • Anesthesiologists generally accept the notion of “unconscious pain” • Pain manifests under general anaesthesia as increased sympathetic tone with tachycardia, hypertension, diaphoresis etc. • Pain Rx: fentanyl, morphine, epidural analgesia
Reflexes • Gag reflex • Oculocardiac reflex NOTE: Epidural or spinal anaesthesia sympathectomy effects may blunt the tachycardia reflex response to hypovolemia
Homeostasis • Fluid and electrolyte balance • Adequate – – – blood pressure blood volume hemoglobin concentration urine output temperature
Muscle Relaxation • For intubation • Where inadvertent patient movement might be disastrous • For abdominal muscle relaxation • To facilitate positive pressure ventilation • Special purposes – ECT therapy – tetanus / lock jaw
Muscle Relaxants • Succinylcholine (very short effect; no reversal; occasional nasty side-effects) • Nondepolarizing Drugs (require reversal eg, neostigmine+atropine) – – Curare Pancuronuim Vecuronium Rocuronium etc.
Preoperative Assessment • • ASA Physical Status Allergies Medications Identify Anaesthetic Considerations Review Need for Consultations Estimate Potential for Blood Loss Postop Ventilation? Need for ICU bed?
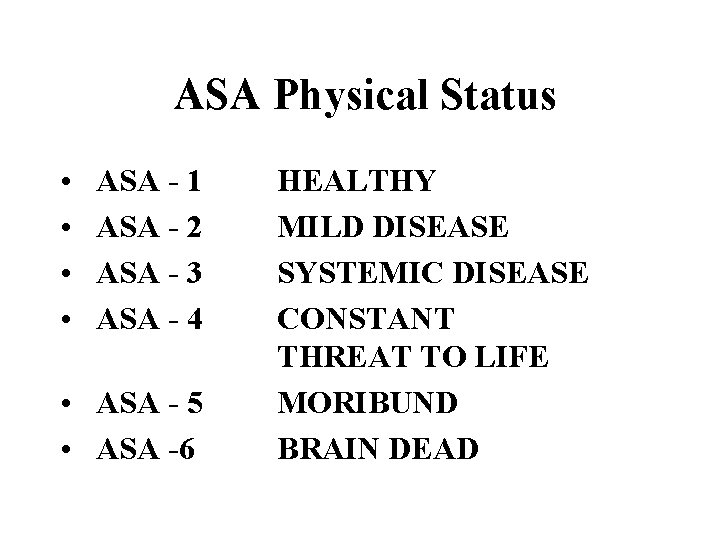
ASA Physical Status • • ASA - 1 ASA - 2 ASA - 3 ASA - 4 • ASA - 5 • ASA -6 HEALTHY MILD DISEASE SYSTEMIC DISEASE CONSTANT THREAT TO LIFE MORIBUND BRAIN DEAD
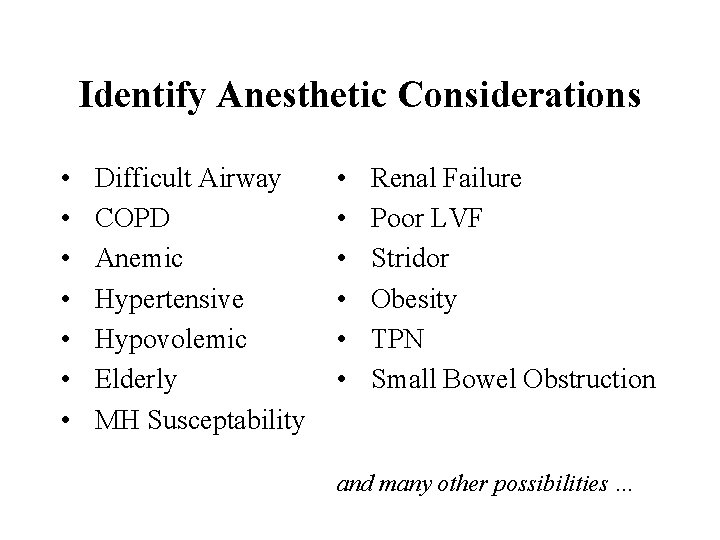
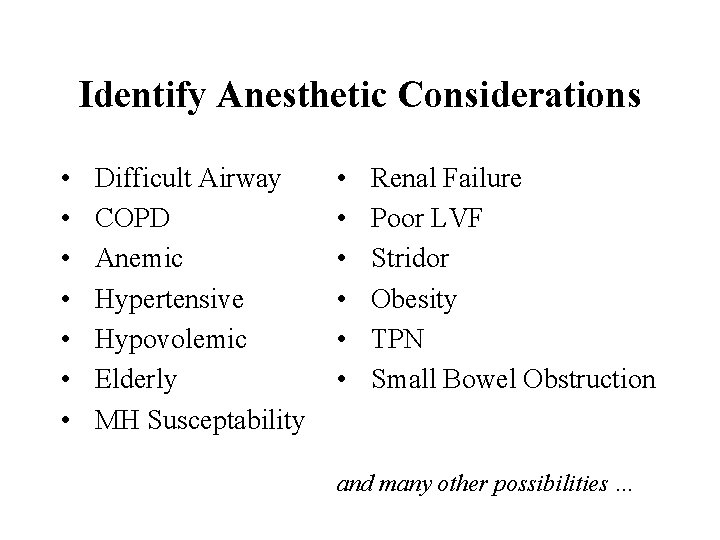
Identify Anesthetic Considerations • • Difficult Airway COPD Anemic Hypertensive Hypovolemic Elderly MH Susceptability • • • Renal Failure Poor LVF Stridor Obesity TPN Small Bowel Obstruction and many other possibilities …
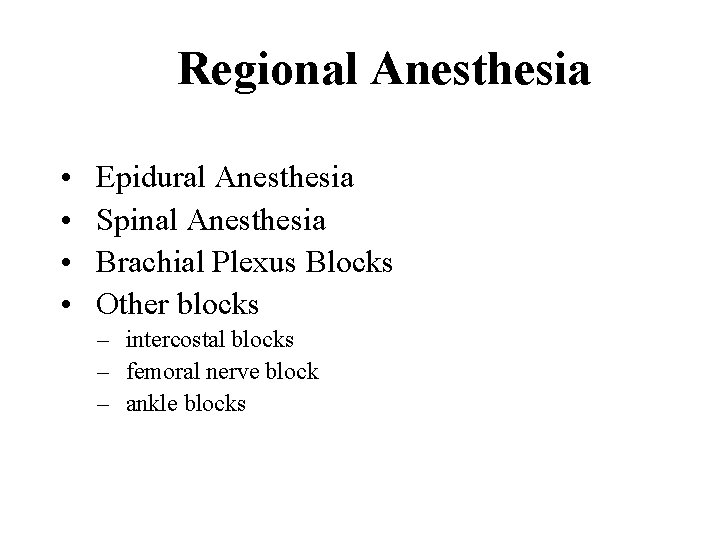
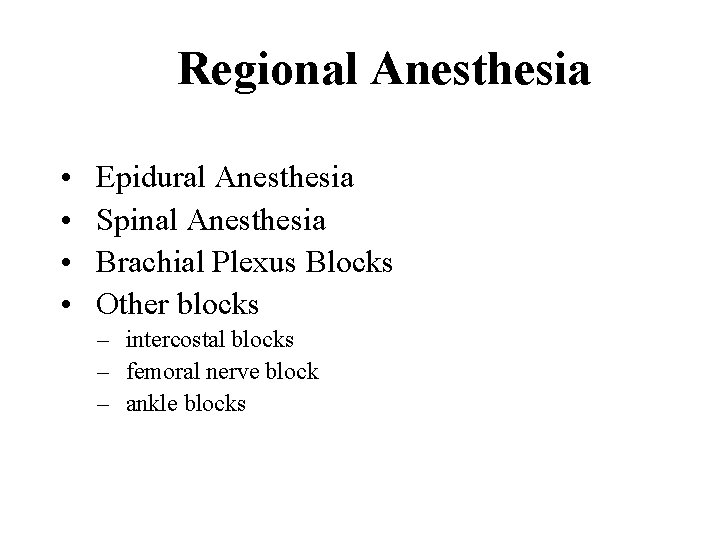
Regional Anesthesia • • Epidural Anesthesia Spinal Anesthesia Brachial Plexus Blocks Other blocks – intercostal blocks – femoral nerve block – ankle blocks
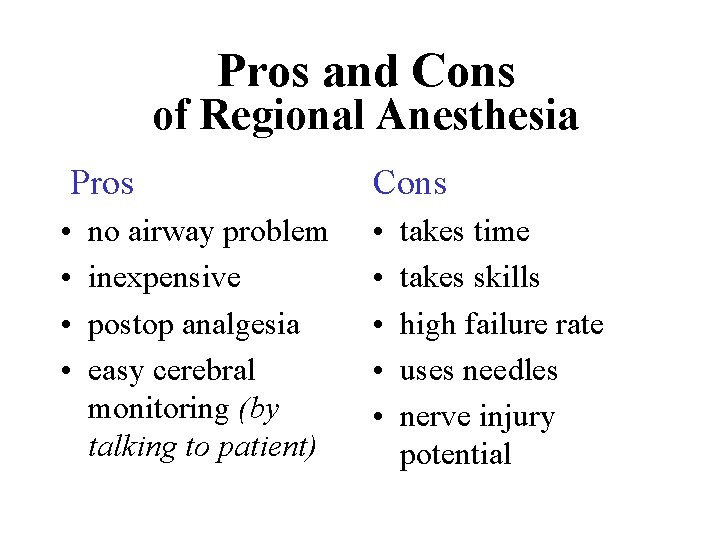
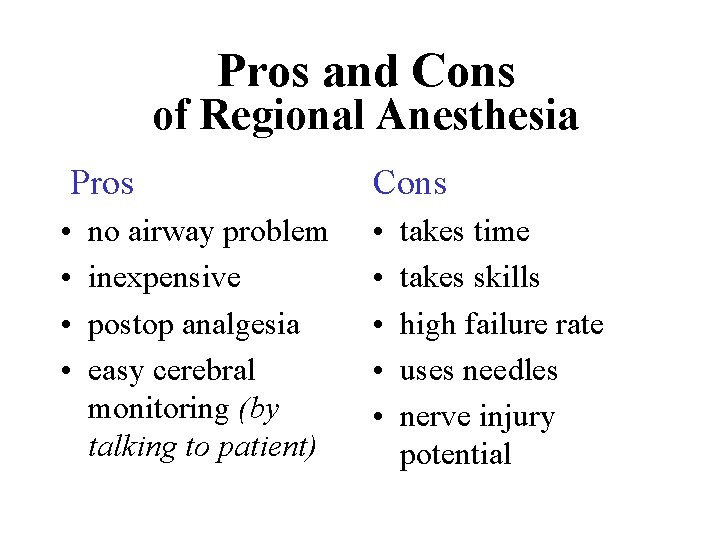
Pros and Cons of Regional Anesthesia Pros Cons • • • no airway problem inexpensive postop analgesia easy cerebral monitoring (by talking to patient) takes time takes skills high failure rate uses needles nerve injury potential
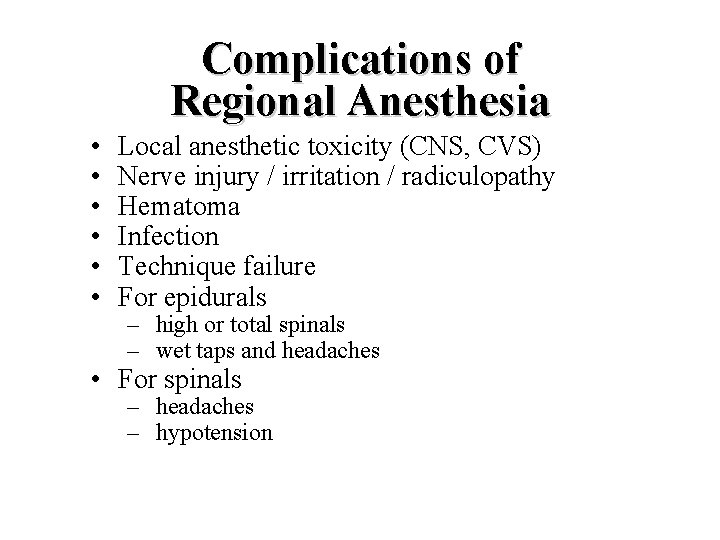
Complications of Regional Anesthesia • • • Local anesthetic toxicity (CNS, CVS) Nerve injury / irritation / radiculopathy Hematoma Infection Technique failure For epidurals – high or total spinals – wet taps and headaches • For spinals – headaches – hypotension
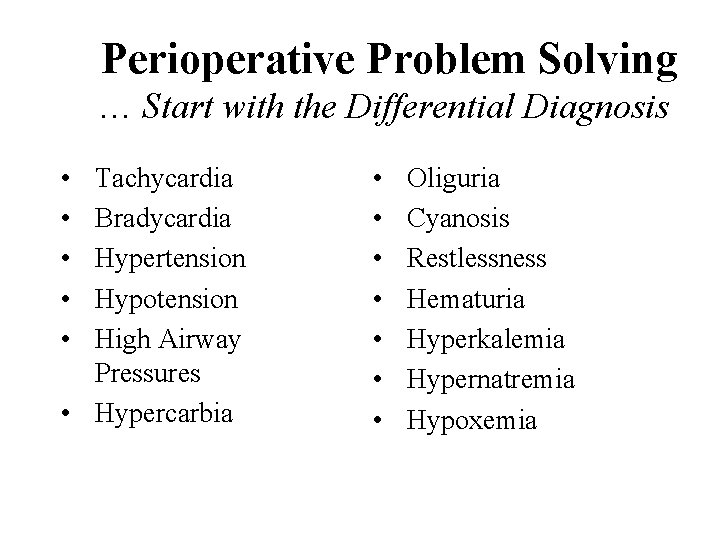
Perioperative Problem Solving … Start with the Differential Diagnosis • • • Tachycardia Bradycardia Hypertension Hypotension High Airway Pressures • Hypercarbia • • Oliguria Cyanosis Restlessness Hematuria Hyperkalemia Hypernatremia Hypoxemia
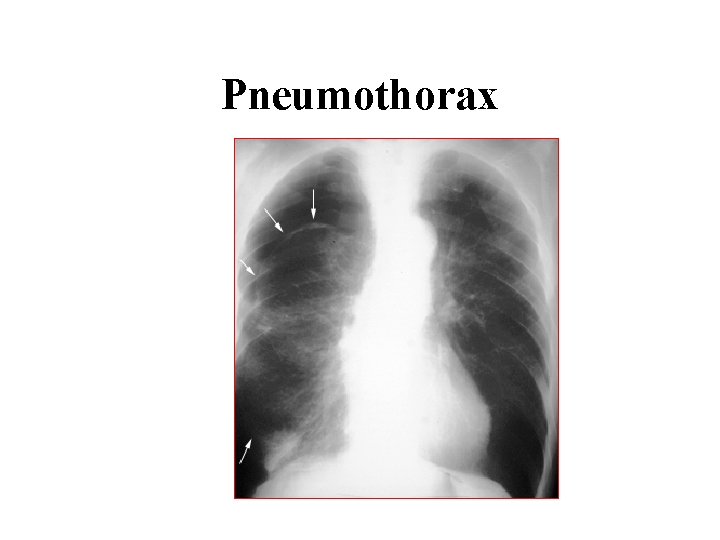
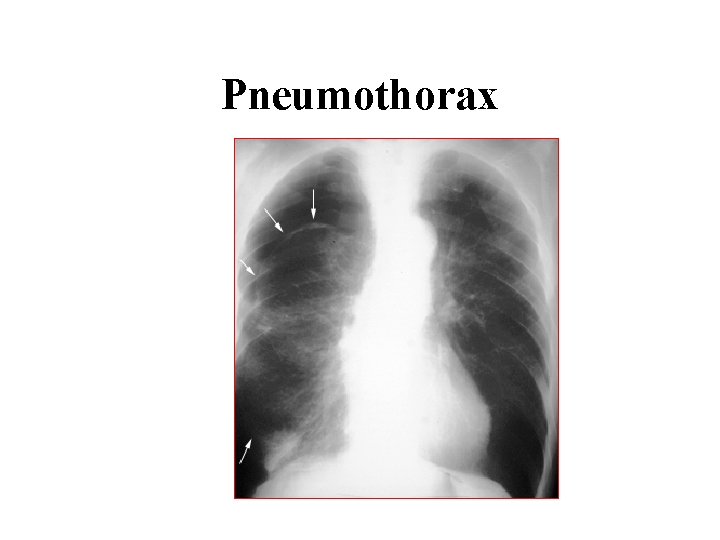
Pneumothorax
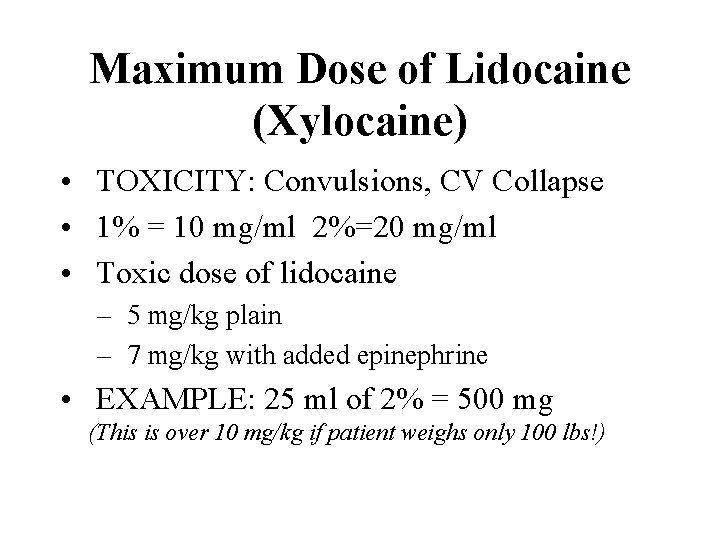
Maximum Dose of Lidocaine (Xylocaine) • TOXICITY: Convulsions, CV Collapse • 1% = 10 mg/ml 2%=20 mg/ml • Toxic dose of lidocaine – 5 mg/kg plain – 7 mg/kg with added epinephrine • EXAMPLE: 25 ml of 2% = 500 mg (This is over 10 mg/kg if patient weighs only 100 lbs!)
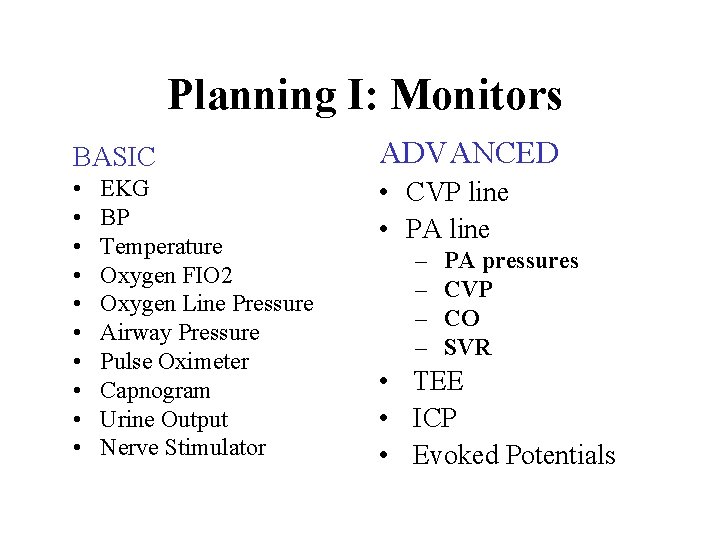
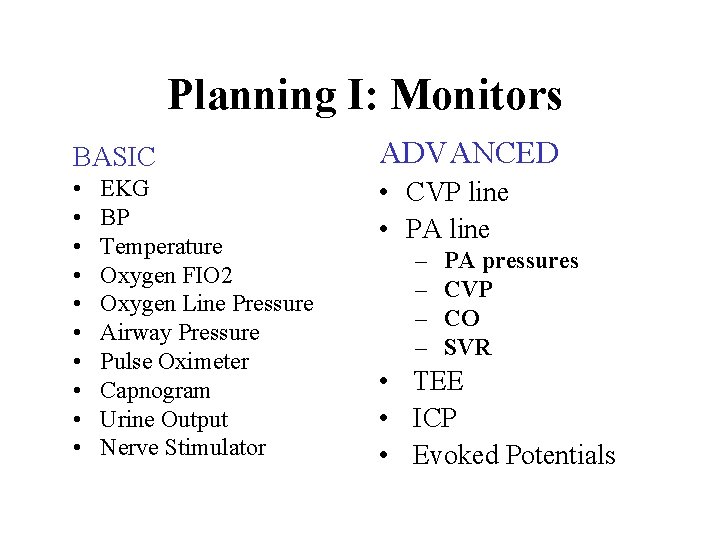
Planning I: Monitors BASIC ADVANCED • • • CVP line • PA line EKG BP Temperature Oxygen FIO 2 Oxygen Line Pressure Airway Pressure Pulse Oximeter Capnogram Urine Output Nerve Stimulator – – PA pressures CVP CO SVR • TEE • ICP • Evoked Potentials
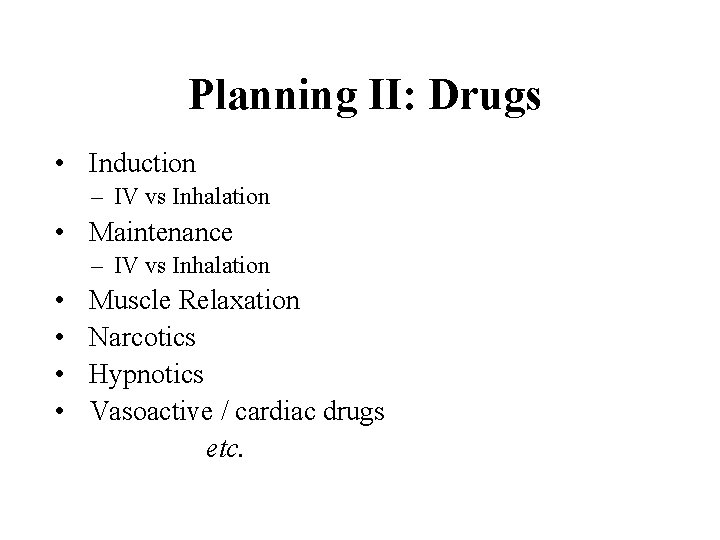
Planning II: Drugs • Induction – IV vs Inhalation • Maintenance – IV vs Inhalation • • Muscle Relaxation Narcotics Hypnotics Vasoactive / cardiac drugs etc.
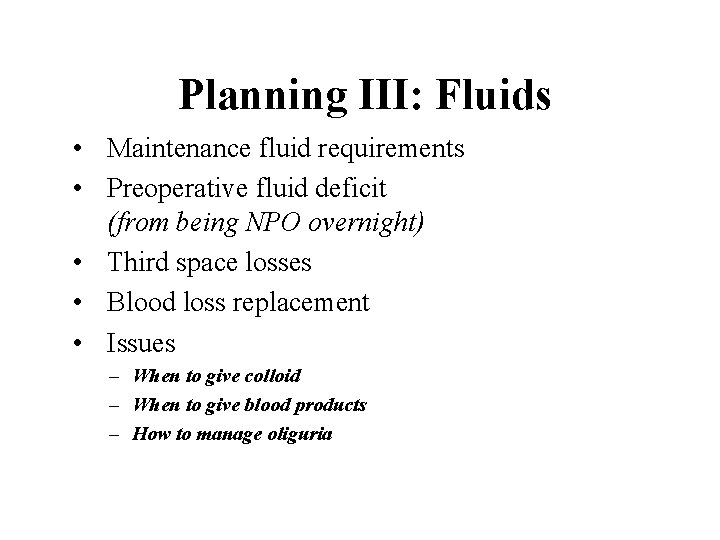
Planning III: Fluids • Maintenance fluid requirements • Preoperative fluid deficit (from being NPO overnight) • Third space losses • Blood loss replacement • Issues – When to give colloid – When to give blood products – How to manage oliguria
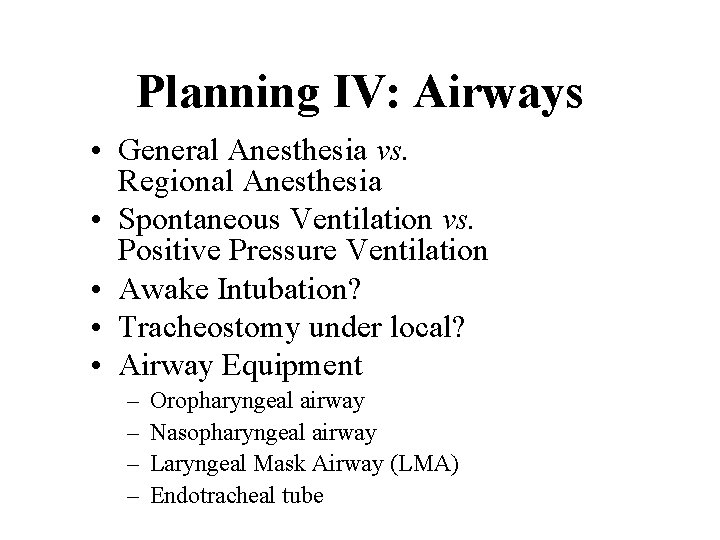
Planning IV: Airways • General Anesthesia vs. Regional Anesthesia • Spontaneous Ventilation vs. Positive Pressure Ventilation • Awake Intubation? • Tracheostomy under local? • Airway Equipment – – Oropharyngeal airway Nasopharyngeal airway Laryngeal Mask Airway (LMA) Endotracheal tube
Planning V: Postoperative Analgesia • • • IM morphine e. g. 10 mg IM q 3 h prn IV morphine e. g. 2 -4 mg IV q 10 min prn PCA Epidural Analgesia Oral Analgesics
IV Induction Agents • • • Thiopental Propofol (Diprivan) Etomidate Ketamine High-dose fentanyl (or other opiate) High-dose midazolam
Potent Inhaled Anesthetics • • • Ether (flammable) Halothane (20% metabolized) Enflurane (2% metabolized) Isoflurane (0. 2% metabolized) Sevoflurane (newer, expensive, good for inhalation inductions) • Desflurane (newer, expensive, not good for inhalation inductions) • Even Xenon makes a passable agent!
Opiates in the OR • • Fentanyl (Sublimaze) Sufentanil Alfentanil Remifentanil Morphine Meperidine (Demerol) Hydromorphone (Dilaudid)
Anesthesiology Operating Room Technology Issues • • Anesthesia Machines Airway Gas Monitors Physiological Monitoring Equipment IV and Inhalational Drug Delivery Technology • Medical Ergonomics • Safety Standards
About Anesthesiology • MD degree, then 4 -5 years more training • Written and oral board exams • Work in OR, ICU, pain service, even palliative care • Experts in resuscitation / reanimation • Bring patients “to the brink of death” several times a day • Among most technically inclined MDs
Clinical Tools in Anesthesiology Drugs • • intravenous inhalational epidural / spinal oral / sublingual
Clinical Tools in Anesthesiology Airway Management Tools • • Endotracheal tubes Laryngoscopes Oral and nasopharyngeal airways Fiberoptic broncoscopes
Clinical Tools in Anesthesiology Monitors • Clinical observation • Noninvasive techniques • Invasive techniques
Anesthesia Machines • Delivery of measured flows of gases: oxygen, nitrous oxide, anesthetic gas • Percent oxygen adjustable 25 to 100% • Ventilator with adjustable rate and volume • Lots of dials and gauges • Lots of safety features • Can be expensive and requires maintenance
Anaesthesia Machines: Oxygen Safety Systems • Electronic oxygen controller forbids oxygen concentrations under 25% • Pulse oximeter provides good clinical oxygenation data (usually) • Airway Gas Monitor warns about hypoxic gas mixtures or about rebreathing of CO 2 • Gauges display tank pressure, oxygen flow, percent oxygen being delivered • Oxygen tanks are green in US (white elsewhere) and hook to yoke via PIN INDEX system
Anaesthesia Machines: Ventilator Operations ANESTHESIA VENTILATOR PARAMETERS • • • Respiratory Rate (frequency) Volume of each breath (tidal volume) Ratio of expiration to inspiration (eg, 2 to 1) Baseline lung distension (PEEP) Percent (fraction) oxygen (FIO 2)
Respiratory Monitoring l Clinical: wheezing, crackles, equal air entry, color, respiratory, pattern (rate, rhythm, depth) l Airway pressure l Spirometry (measured tidal volume) l Capnography (CO 2 concentration vs. time) l Oxygraphy (O 2 concentration vs. time) l Pulse oximetry l OTHER : ETT cuff pressure, NIF, VC
BREATHING • Spontaneous Breathing – Specify percent (fraction) oxygen (FIO 2) – Clinically monitor airway, breathing characteristics, and respiration rate • Machine Ventilation – Respiratory Rate (frequency) – Volume of each breath (tidal volume) – Baseline lung distension (PEEP) – Percent (fraction) oxygen (FIO 2)
Respiratory Assessment Clinical Assessment of Breathing – Visual inspection: breathing pattern, rate, depth, signs of airway obstruction – Trend charting of respiratory rate (increases in respiratory rate may herald pulmonary edema; decreases in respiratory rate may herald apnea)
Respiratory Assessment Lab Respiratory Monitoring Methods • • Pulse Oximeter (art oxygen saturation ) Capnograph (expired CO 2 conc signal) Oxygram (expired O 2 concentration sig) Arterial Blood Gas Analysis – arterial oxygen tension – arterial carbon dioxide tension – arterial p. H
What is Monitoring? • • • Keeping an “eye on the patient” Patient defense strategy / algorithm High-tech electronics Old fashioned viligence Preparing for future events Keeping “quality” in the system, including monitoring care providers
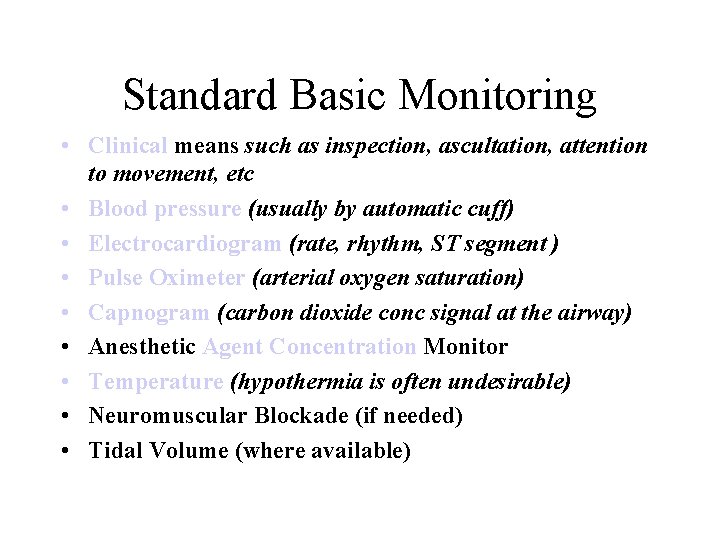
Standard Basic Monitoring • Clinical means such as inspection, ascultation, attention to movement, etc • Blood pressure (usually by automatic cuff) • Electrocardiogram (rate, rhythm, ST segment ) • Pulse Oximeter (arterial oxygen saturation) • Capnogram (carbon dioxide conc signal at the airway) • Anesthetic Agent Concentration Monitor • Temperature (hypothermia is often undesirable) • Neuromuscular Blockade (if needed) • Tidal Volume (where available)
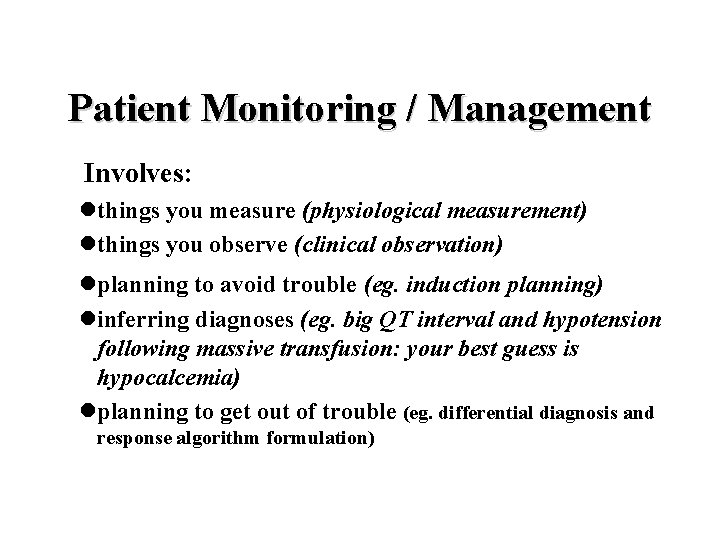
Patient Monitoring / Management Involves: lthings you measure (physiological measurement) lthings you observe (clinical observation) lplanning to avoid trouble (eg. induction planning) linferring diagnoses (eg. big QT interval and hypotension following massive transfusion: your best guess is hypocalcemia) lplanning to get out of trouble (eg. differential diagnosis and response algorithm formulation)
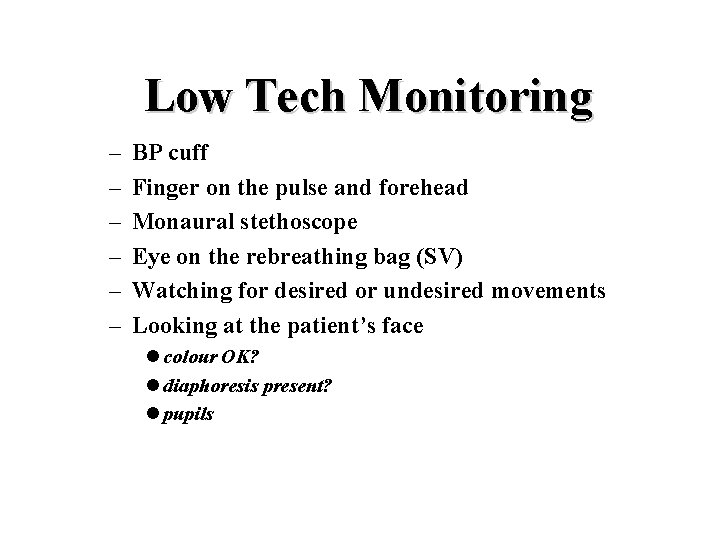
Low Tech Monitoring – – – BP cuff Finger on the pulse and forehead Monaural stethoscope Eye on the rebreathing bag (SV) Watching for desired or undesired movements Looking at the patient’s face l colour OK? l diaphoresis present? l pupils
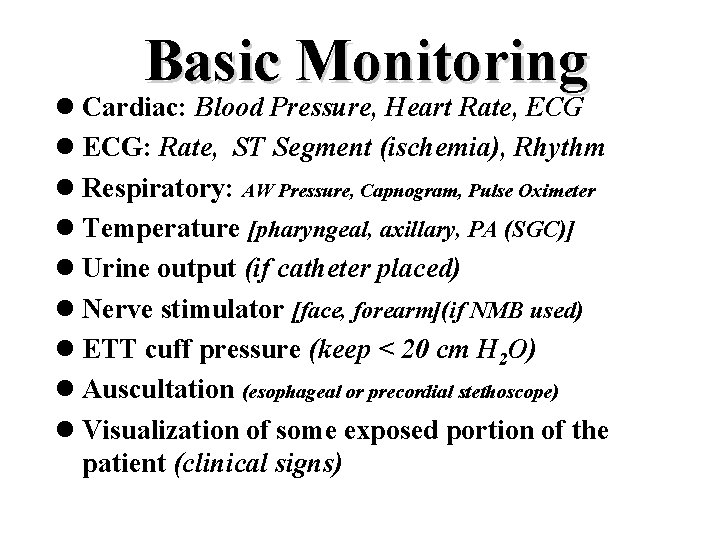
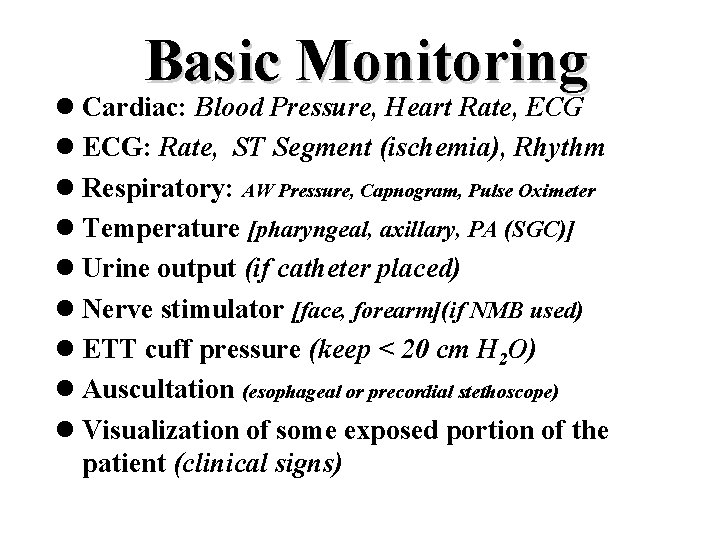
Basic Monitoring l Cardiac: Blood Pressure, Heart Rate, ECG l ECG: Rate, ST Segment (ischemia), Rhythm l Respiratory: AW Pressure, Capnogram, Pulse Oximeter l Temperature [pharyngeal, axillary, PA (SGC)] l Urine output (if catheter placed) l Nerve stimulator [face, forearm](if NMB used) l ETT cuff pressure (keep < 20 cm H 2 O) l Auscultation (esophageal or precordial stethoscope) l Visualization of some exposed portion of the patient (clinical signs)
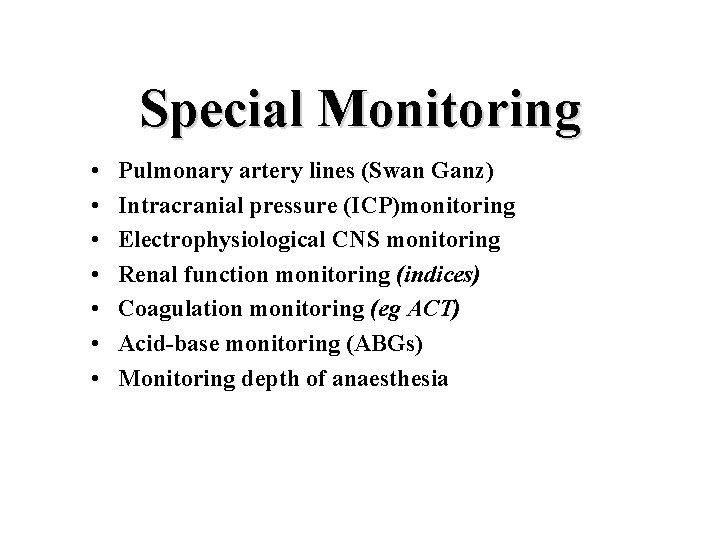
Special Monitoring • • Pulmonary artery lines (Swan Ganz) Intracranial pressure (ICP)monitoring Electrophysiological CNS monitoring Renal function monitoring (indices) Coagulation monitoring (eg ACT) Acid-base monitoring (ABGs) Monitoring depth of anaesthesia