Module 3 Testosterone therapy Approval Number G MKT
Module 3 Testosterone therapy Approval Number: G. MKT. GM. MH. 04. 2018. 0513

Testosterone: use and misuse in men • The main indication for testosterone use in men is male hypogonadism • Other known uses and misuses include: Use Condition Licensed clinical applications • Male hypogonadism – Primary, secondary or adult-onset • Delayed puberty • Aplastic and renal anemia Off-label and experimental applications • Excessive growth • Male contraception Obsolete application • Idiopathic infertility Misuse/abuse • Sports performance enhancement, bodybuilding Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 2
Aim of testosterone therapy in men • To restore testosterone levels to the physiological range in men with consistently low levels of serum testosterone and associated symptoms of androgen deficiency 1 – To improve Qo. L, sense of well-being, sexual function, muscle strength and bone mineral density 1 • Qualities of the ‘ideal’ testosterone therapy: 2 – Achieve and maintain a physiological level of testosterone – Ensure a favorable safety profile – Convenient dosing schedule and administration – Reasonable cost to the patient Qo. L, quality of life 1. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 2. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 3

Testosterone therapy in men: main indications Main indications • Delayed puberty (constitutional or congenital forms: hypogonadotrophic hypogonadism, Kallmann syndrome) • Klinefelter syndrome with hypogonadism • Sexual dysfunction and low testosterone, not responding to PDE-5 inhibitors • Low bone mass in hypogonadism • Adult men with low testosterone PLUS consistent and preferably multiple signs and symptoms of hypogonadism following unsuccessful treatment of obesity and comorbidities • Hypopituitarism PDE-5, phosphodiesterase type 5 Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 4
Testosterone therapy in men: main contraindications Main contraindications • Locally advanced or metastatic prostate cancer • Male breast cancer • Men with an active desire to have children • Hematocrit >0/54% • Severe chronic cardiac failure (New York Heart Association Class IV) Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 5
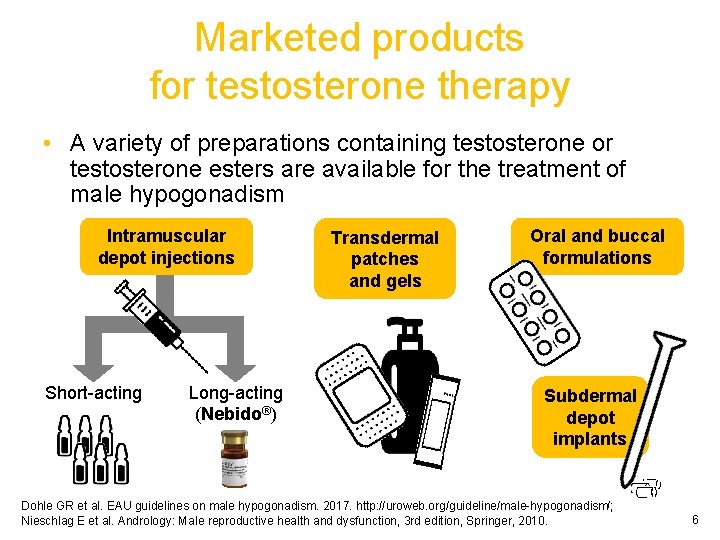
Marketed products for testosterone therapy • A variety of preparations containing testosterone or testosterone esters are available for the treatment of male hypogonadism Intramuscular depot injections Short-acting Long-acting (Nebido®) Transdermal patches and gels Oral and buccal formulations Subdermal depot implants Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/; Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 6

Available testosterone therapies: long-acting intramuscular preparation Administration route Formulation Advantages Disadvantages Long-acting intramuscular injection 1000 mg 1 Every 10– 14 weeks 1– 3 Testosterone undecanoate (Nebido®) • Maintains steady state physiological serum testosterone levels without fluctuation 3 • Long-acting preparation: requires less frequent administration, 1 and allows for greater convenience 2 • Better adherence versus other testosterone therapies 4 • Well-tolerated in long-term use 1, 2 • Long-acting preparation: does not allow rapid withdrawal in case of poor tolerability/ adverse events 3 • Relatively high cost 2, 5 1. Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 2. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 3. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 4. Isidori AM et al. Eur Urol. 2014; 65(1): 99– 112. 5. Seftel A. Int J Impot Res. 2007; 19(1): 2– 24. 7
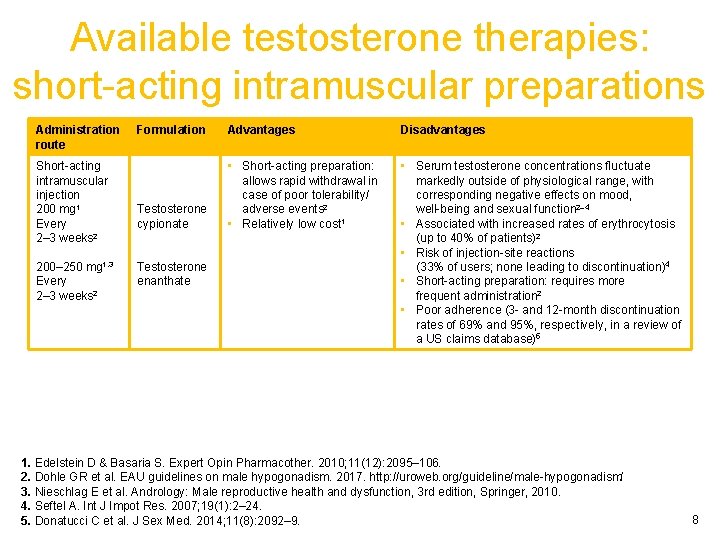
Available testosterone therapies: short-acting intramuscular preparations Administration route Short-acting intramuscular injection 200 mg 1 Every 2– 3 weeks 2 200– 250 mg 1, 3 Every 2– 3 weeks 2 Formulation Advantages Disadvantages Testosterone cypionate • Short-acting preparation: allows rapid withdrawal in case of poor tolerability/ adverse events 2 • Relatively low cost 1 • Serum testosterone concentrations fluctuate markedly outside of physiological range, with corresponding negative effects on mood, well-being and sexual function 2– 4 • Associated with increased rates of erythrocytosis (up to 40% of patients)2 • Risk of injection-site reactions (33% of users; none leading to discontinuation)4 • Short-acting preparation: requires more frequent administration 2 • Poor adherence (3 - and 12 -month discontinuation rates of 69% and 95%, respectively, in a review of a US claims database)5 Testosterone enanthate 1. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 2. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 3. Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 4. Seftel A. Int J Impot Res. 2007; 19(1): 2– 24. 5. Donatucci C et al. J Sex Med. 2014; 11(8): 2092– 9. 8
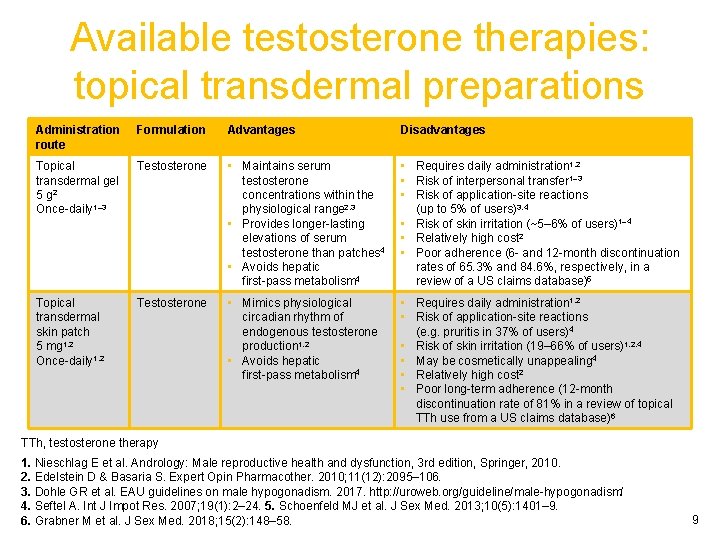
Available testosterone therapies: topical transdermal preparations Administration route Formulation Advantages Disadvantages Topical transdermal gel 5 g 2 Once-daily 1– 3 Testosterone • Maintains serum testosterone concentrations within the physiological range 2, 3 • Provides longer-lasting elevations of serum testosterone than patches 4 • Avoids hepatic first-pass metabolism 4 • Requires daily administration 1, 2 • Risk of interpersonal transfer 1– 3 • Risk of application-site reactions (up to 5% of users)3, 4 • Risk of skin irritation (~5– 6% of users)1– 4 • Relatively high cost 2 • Poor adherence (6 - and 12 -month discontinuation rates of 65. 3% and 84. 6%, respectively, in a review of a US claims database)5 Topical transdermal skin patch 5 mg 1, 2 Once-daily 1, 2 Testosterone • Mimics physiological circadian rhythm of endogenous testosterone production 1, 2 • Avoids hepatic first-pass metabolism 4 • Requires daily administration 1, 2 • Risk of application-site reactions (e. g. pruritis in 37% of users)4 • Risk of skin irritation (19– 66% of users)1, 2, 4 • May be cosmetically unappealing 4 • Relatively high cost 2 • Poor long-term adherence (12 -month discontinuation rate of 81% in a review of topical TTh use from a US claims database)6 TTh, testosterone therapy 1. Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 2. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 3. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 4. Seftel A. Int J Impot Res. 2007; 19(1): 2– 24. 5. Schoenfeld MJ et al. J Sex Med. 2013; 10(5): 1401– 9. 6. Grabner M et al. J Sex Med. 2018; 15(2): 148– 58. 9
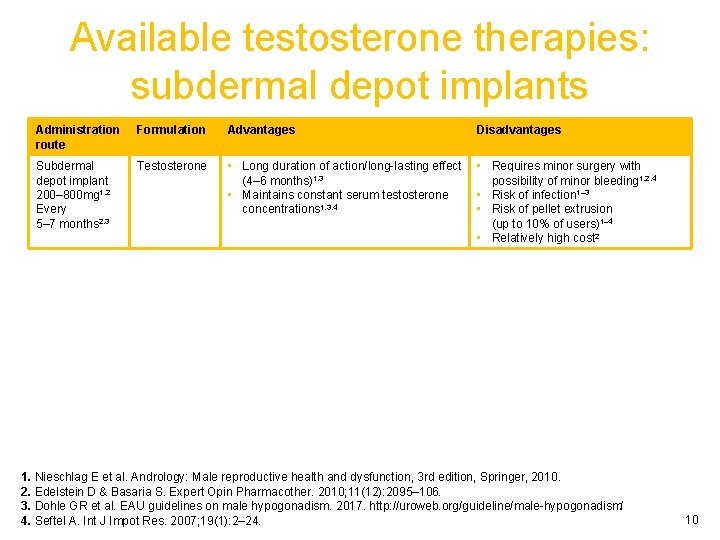
Available testosterone therapies: subdermal depot implants Administration route Formulation Advantages Disadvantages Subdermal depot implant 200– 800 mg 1, 2 Every 5– 7 months 2, 3 Testosterone • Long duration of action/long-lasting effect (4– 6 months)1, 3 • Maintains constant serum testosterone concentrations 1, 3, 4 • Requires minor surgery with possibility of minor bleeding 1, 2, 4 • Risk of infection 1– 3 • Risk of pellet extrusion (up to 10% of users)1– 4 • Relatively high cost 2 1. Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 2. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 3. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 4. Seftel A. Int J Impot Res. 2007; 19(1): 2– 24. 10
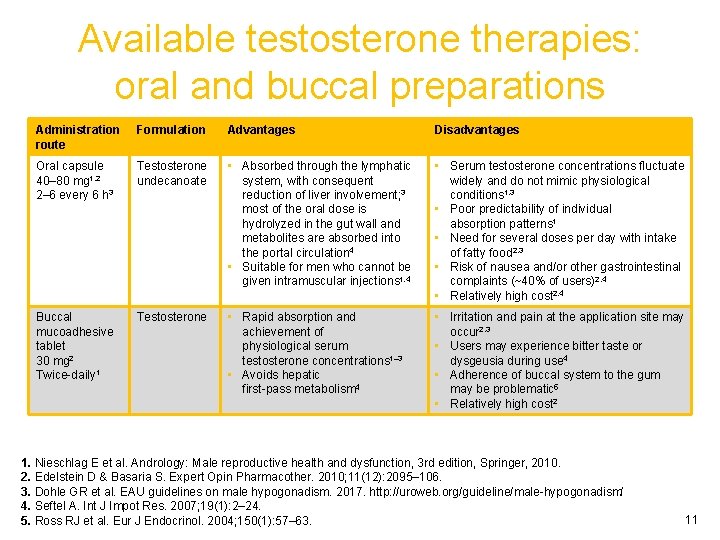
Available testosterone therapies: oral and buccal preparations Administration route Formulation Advantages Disadvantages Oral capsule 40– 80 mg 1, 2 2– 6 every 6 h 3 Testosterone undecanoate • Absorbed through the lymphatic system, with consequent reduction of liver involvement; 3 most of the oral dose is hydrolyzed in the gut wall and metabolites are absorbed into the portal circulation 4 • Suitable for men who cannot be given intramuscular injections 1, 4 • Serum testosterone concentrations fluctuate widely and do not mimic physiological conditions 1, 3 • Poor predictability of individual absorption patterns 1 • Need for several doses per day with intake of fatty food 2, 3 • Risk of nausea and/or other gastrointestinal complaints (~40% of users)2, 4 • Relatively high cost 2, 4 Buccal mucoadhesive tablet 30 mg 2 Twice-daily 1 Testosterone • Rapid absorption and achievement of physiological serum testosterone concentrations 1– 3 • Avoids hepatic first-pass metabolism 4 • Irritation and pain at the application site may occur 2, 3 • Users may experience bitter taste or dysgeusia during use 4 • Adherence of buccal system to the gum may be problematic 5 • Relatively high cost 2 1. Nieschlag E et al. Andrology: Male reproductive health and dysfunction, 3 rd edition, Springer, 2010. 2. Edelstein D & Basaria S. Expert Opin Pharmacother. 2010; 11(12): 2095– 106. 3. Dohle GR et al. EAU guidelines on male hypogonadism. 2017. http: //uroweb. org/guideline/male-hypogonadism/ 4. Seftel A. Int J Impot Res. 2007; 19(1): 2– 24. 5. Ross RJ et al. Eur J Endocrinol. 2004; 150(1): 57– 63. 11
Module 3: Testosterone therapy Pharmacokinetic profiles of the various preparations 12
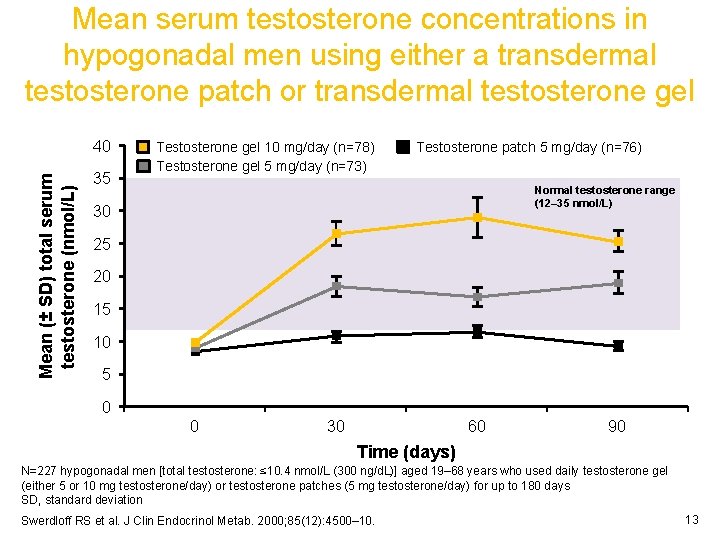
Mean serum testosterone concentrations in hypogonadal men using either a transdermal testosterone patch or transdermal testosterone gel Mean (± SD) total serum testosterone (nmol/L) 40 35 Testosterone gel 10 mg/day (n=78) Testosterone gel 5 mg/day (n=73) Testosterone patch 5 mg/day (n=76) Normal testosterone range (12– 35 nmol/L) 30 25 20 15 10 5 0 0 30 60 90 Time (days) N=227 hypogonadal men [total testosterone: ≤ 10. 4 nmol/L (300 ng/d. L)] aged 19– 68 years who used daily testosterone gel (either 5 or 10 mg testosterone/day) or testosterone patches (5 mg testosterone/day) for up to 180 days SD, standard deviation Swerdloff RS et al. J Clin Endocrinol Metab. 2000; 85(12): 4500– 10. 13
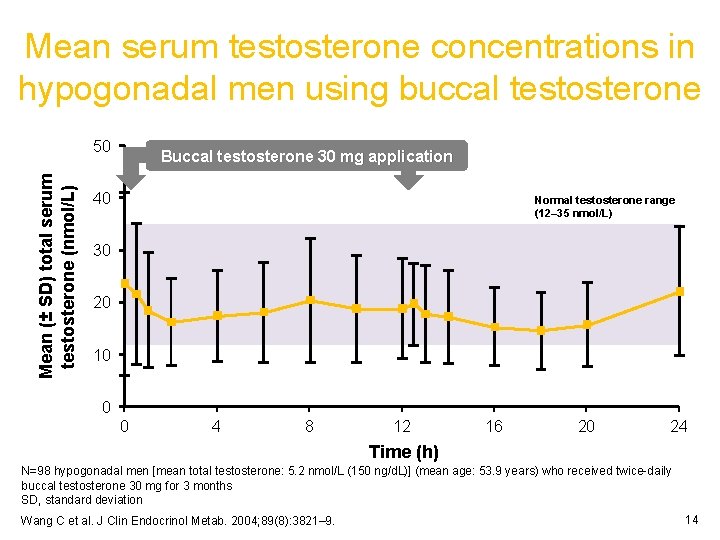
Mean serum testosterone concentrations in hypogonadal men using buccal testosterone Mean (± SD) total serum testosterone (nmol/L) 50 Buccal testosterone 30 mg application 40 Normal testosterone range (12– 35 nmol/L) 30 20 10 0 0 4 8 12 16 20 24 Time (h) N=98 hypogonadal men [mean total testosterone: 5. 2 nmol/L (150 ng/d. L)] (mean age: 53. 9 years) who received twice-daily buccal testosterone 30 mg for 3 months SD, standard deviation Wang C et al. J Clin Endocrinol Metab. 2004; 89(8): 3821– 9. 14

Mean serum testosterone concentrations in hypogonadal men using subdermal depot implants Mean (± SEM) total serum testosterone (nmol/L) 50 30 Normal testosterone range (12– 35 nmol/L) 20 10 7 5 3 2 0 0 2 1 50 100 150 200 250 300 Time (days) N=14 hypogonadal men [mean total testosterone: 1. 17 nmol/L (34 ng/d. L)] (mean age: 32. 77 years) who were implanted with six subdermal depot testosterone 200 mg implants (1200 mg total dose) and followed for 300 days SEM, standard error of the mean Jockenhövel F et al. Clin Endocrinol (Oxf). 1996; 45(1): 61– 71. 15
Summary • Appropriate use of testosterone therapy is effective for the management of hypogonadal symptoms • Available testosterone preparations include: – Intramuscular depot injections – Transdermal patches and gels – Oral and buccal formulations – Subdermal depot implants • These differ in their pharmacokinetic profiles, and have specific advantages and disadvantages, which can influence the hypogonadal patient’s decision to use a particular formulation 16
- Slides: 16