Module 3 How to Use the Adult Flipchart






































- Slides: 42

Module 3: How to Use the Adult Flipchart

Learning Objectives • Using the Viral Load Monitoring and Enhanced Adherence Counseling Flipchart as a guide, participants will be able to: – Interpret and explain the meaning of a viral load result <1, 000 copies/ml – Interpret and explain the meaning of a viral load >1, 000 copies/ml – Assess adherence among those with viral load >1, 000 copies/ml using the VL flipchart – Develop targeted interventions to improve adherence counseling and support – Manage next steps based on repeat viral load results

Outline • Orientation to the Viral Load Monitoring and Enhanced Adherence Counseling Flipchart • Viral load results, interpretation, and explaining meaning to patient • Assessing adherence for those with elevated viral load • Developing individualized adherence intervention plan • Repeat viral load testing and follow up on results

Orientation to the Flipchart

About the Flipchart • Purpose: – Provide information about viral load and promote adherence for those starting and already receiving ARVs. – Explain the meaning of viral load results and improve adherence assessment counseling for those with elevated viral load. • Intended Users: Health care workers (adherence counselors, doctors, nurses, community health workers, lay counselors, expert clients).

How to Use the Flipchart • Place the flipchart on the table so the patient has a good view of the pictures while you use the side with notes. • Key messages to convey to the patients are on the patient picture side and on the left part of the provider side. PATIENT’S VIEW Key Messages
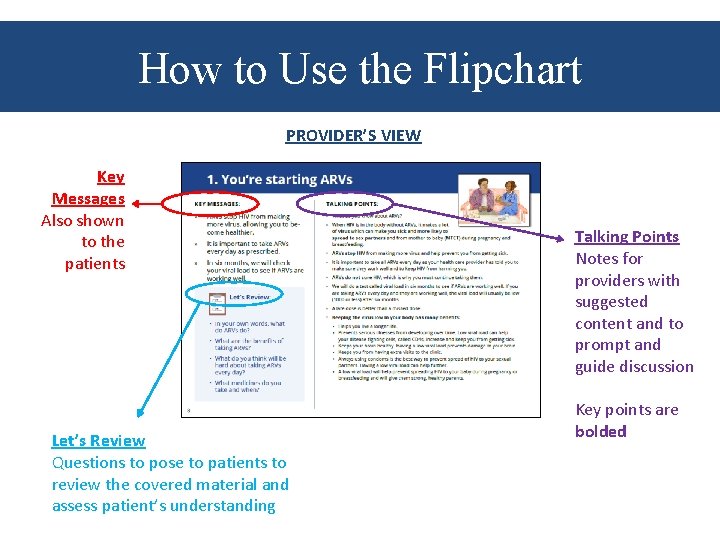
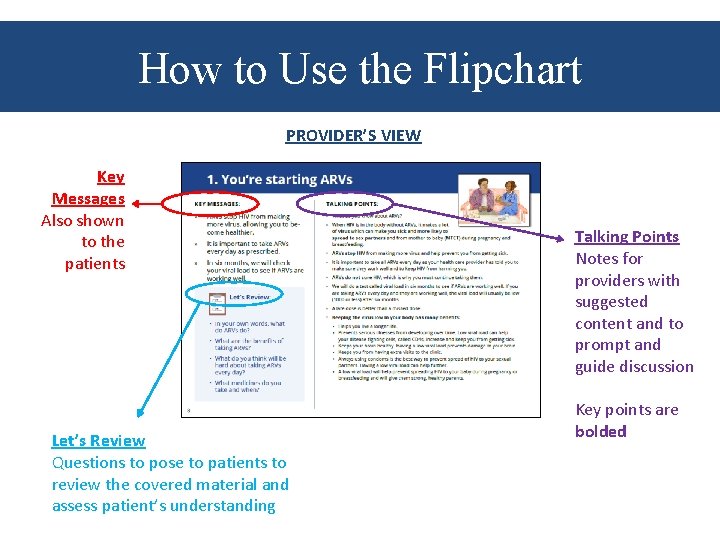
How to Use the Flipchart PROVIDER’S VIEW Key Messages Also shown to the patients Let’s Review Questions to pose to patients to review the covered material and assess patient’s understanding Talking Points Notes for providers with suggested content and to prompt and guide discussion Key points are bolded
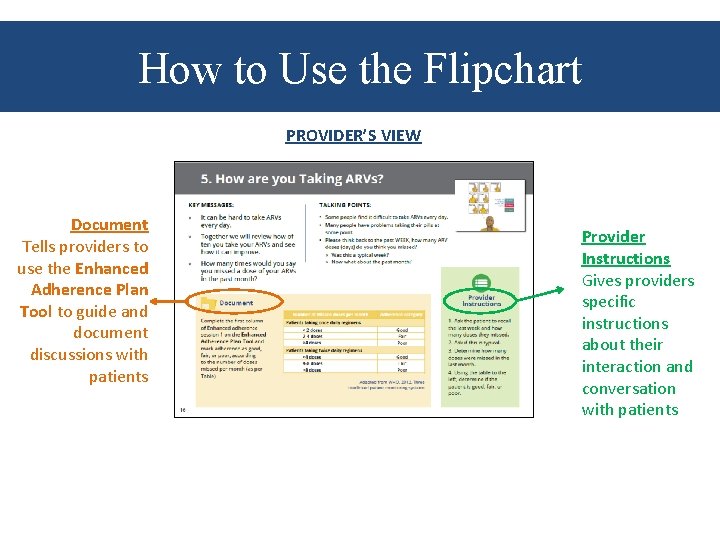
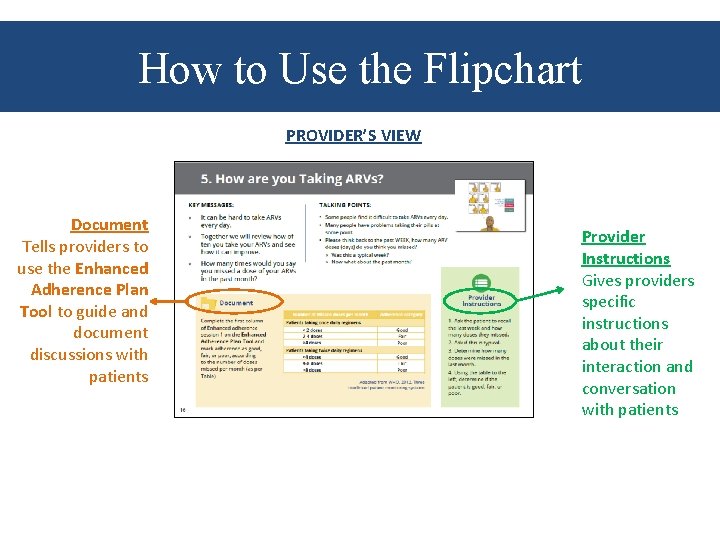
How to Use the Flipchart PROVIDER’S VIEW Document Tells providers to use the Enhanced Adherence Plan Tool to guide and document discussions with patients Provider Instructions Gives providers specific instructions about their interaction and conversation with patients
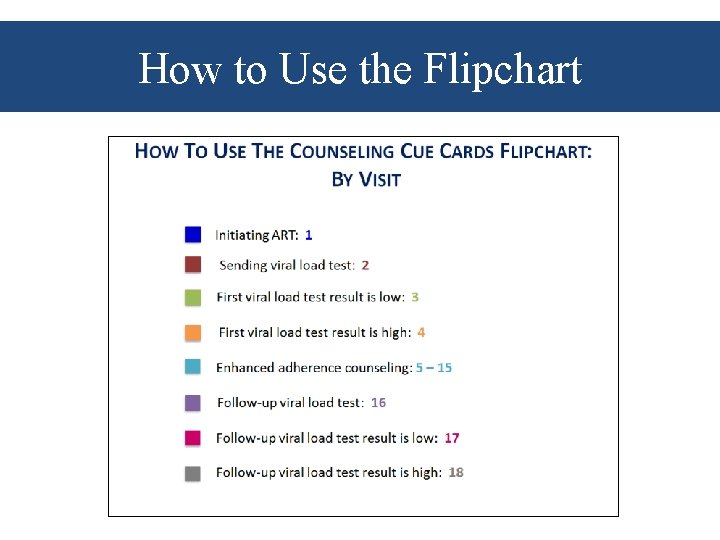
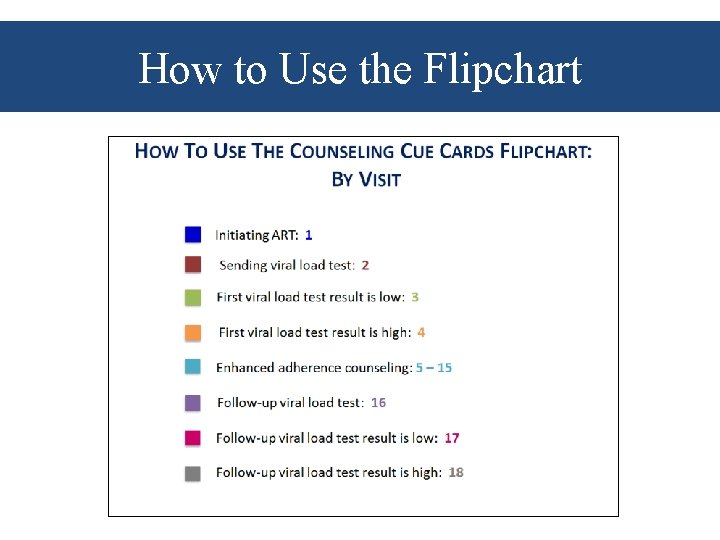
How to Use the Flipchart

How to Use the Flipchart Each card, or set of cards, focuses on a specific topic important to the care, treatment, and support of patients on ARVs who will have a viral load test done or who already have a viral load result.

Counseling and Communication Skills

Enhanced Adherence Plan Tool • Providers should use this tool along with the flipchart during sessions with the patient. • Many cards on the flipchart will prompt providers to fill this sheet out at the same time. • This sheet is intended to be part of the patient file/medical record.

Enhanced Adherence Plan Tool • During each session, the provider should indicate: – The patient’s adherence level (good, fair, poor)* – Whether they missed any pharmacy drug pick-ups

Enhanced Adherence Plan Tool • As providers speak with the patient, they will check off the barriers to taking ARVs that are cited by patients.

Enhanced Adherence Plan Tool • Then, the provider should mark which interventions they have discussed as solutions to these barriers. • The tool is designed to capture information at all repeat adherence sessions, in many countries this will

Enhanced Adherence Plan Tool

Enhanced Adherence Plan Tool • The provider should complete the Repeat Viral Load section after results reviewed and interpreted: – Date – VL result – Plan • Providers should write down specifics of next steps in the comments section.

ART Initiation

Explaining Viral Load

Interpretation of Viral Load Results: <1, 000 copies/ml

Explanation of Viral Load Results: >1, 000 copies/ml

Adherence Assessment and Counseling • Patients with VL >1, 000 copies/ml should undergo adherence assessment using the Viral Load Monitoring Flipchart • Based on identified barriers, an Enhanced Adherence Treatment Plan with specific, targeted interventions should be developed • Use cards 5 -18 in the Adult flipchart to assist you in conducting the Enhanced Adherence Assessment • After the first enhanced adherence counseling session, begin the session with card 16 and repeat 5 -15 as needed

Assessing Adherence

Assessing Adherence Number of Missed Doses per Month Adherence Category Patients taking once daily regimens <2 doses Good 2 -4 doses Fair >4 doses Poor Patients taking twice daily regimens <4 doses Good 4 -8 doses Fair >8 doses Poor

Assessing Adherence • Use Talking Points and Provider Instructions to explore any challenges the patient may be facing when taking ARVs. • Remember to use Open-Ended Questions rather than questions that are answered as Yes/No. – “Please feel comfortable telling me about challenges you are facing; I am asking because I want to try to find ways to make it more successful. ” – “Can you recall and describe the circumstances around the last missed dose? ”

Individual Barriers BARRIERS QUESTIONS TO ASSESS BARRIERS INDIVIDUAL Knowledge Deficit - Can you tell me the names of your ARVs? - What is your understanding of how you are supposed to take (e. g. what time of day, how much [if liquid], how many [if pills]? ) - What is your understanding of the purpose of the ARVs? Side Effects - Have the ARVs affected the way you feel? - Do you think the ARVs have made you/your child feel ill in any way? - If yes, please describe what problems they cause, i. e. nausea, diarrhea, sleep disturbance Forgot - Have you ever forgotten or do you often forget to take your ARVs? - Do you take/give them at a set time of days(s)? - What is your method of remembering/reminding yourself to take ARVs? Feeling Better - Do you take ARVs even when you are feeling well? Physical Illness - Have you had illnesses that have prevented you from taking ARVS? Alcohol or Drug Use - Do you use alcohol? - Do you use drugs? - Do you feel this affects your ability to take your ARVs? Depression - How is your mood in general? - Have you been feeling sad or confused? - If yes, has this affected your ability to take your ARVs?
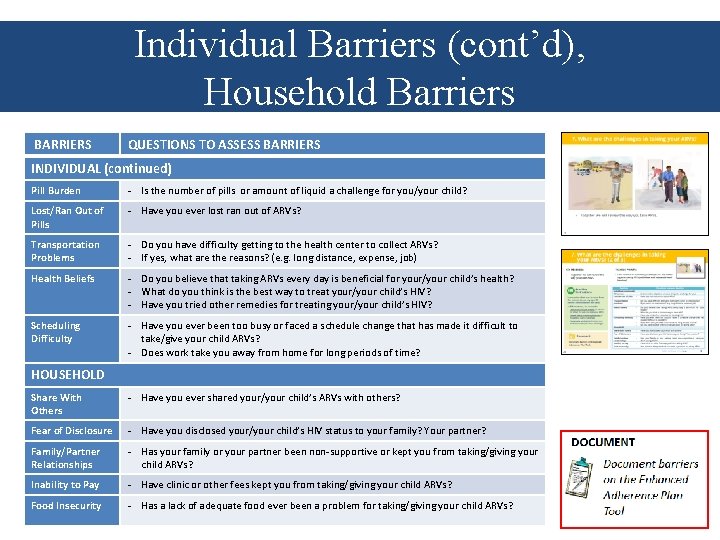
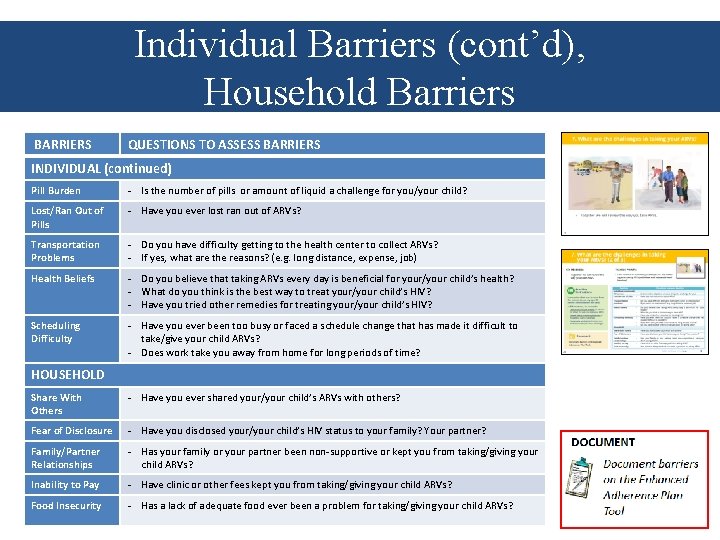
Individual Barriers (cont’d), Household Barriers BARRIERS QUESTIONS TO ASSESS BARRIERS INDIVIDUAL (continued) Pill Burden - Is the number of pills or amount of liquid a challenge for you/your child? Lost/Ran Out of Pills - Have you ever lost ran out of ARVs? Transportation Problems - Do you have difficulty getting to the health center to collect ARVs? - If yes, what are the reasons? (e. g. long distance, expense, job) Health Beliefs - Do you believe that taking ARVs every day is beneficial for your/your child’s health? - What do you think is the best way to treat your/your child’s HIV? - Have you tried other remedies for treating your/your child’s HIV? Scheduling Difficulty - Have you ever been too busy or faced a schedule change that has made it difficult to take/give your child ARVs? - Does work take you away from home for long periods of time? HOUSEHOLD Share With Others - Have you ever shared your/your child’s ARVs with others? Fear of Disclosure - Have you disclosed your/your child’s HIV status to your family? Your partner? Family/Partner Relationships - Has your family or your partner been non-supportive or kept you from taking/giving your child ARVs? Inability to Pay - Have clinic or other fees kept you from taking/giving your child ARVs? Food Insecurity - Has a lack of adequate food ever been a problem for taking/giving your child ARVs?

Institutional/Community Barriers BARRIERS QUESTIONS TO ASSESS BARRIERS INSTITUTIONAL/COMMUNITY Drug Stock Out - Have you ever come to the health facility and found that there were no ARVs available? - Have you ever come to the health facility and been given only a small supply of ARVs? Long Wait Times - Have you ever left the health facility before receiving your/your child’s ARVs because of long wait times? Stigma and Discrimination - Are you fearful that people in the community will find out about your/your child’s HIV? - Does that prevent you from coming to clinic or taking/giving ARVs? Political Crisis/ War/ Natural Disaster - Is it ever unsafe for you to pick up ARVs from the health facility?

Improving Adherence

Individual Interventions BARRIERS INTERVENTIONS TO ADDRESS BARRIERS AND IMPROVE ADHERENCE INDIVIDUAL Knowledge Deficit q Individual counseling for basic HIV/ARV education q Group counseling/peer support group q Written instructions Side Effects q q q Nausea take with food, anti-emetic Diarrhea anti-diarrheal once infections are ruled out, hydration Anxiety/depression take before bed Headache paracetamol, evaluate for meningitis Fatigue check Hgb, consider substitution if on AZT Forgot q q q Medication organizer (e. g. pillbox) Visual medication schedule (e. g. calendar, journal/log) Reminder devices (e. g. phone calls, SMS, watch alarm) Treatment buddy or supporter Directly Observed Therapy (DOTS) Announced pill count at next session Feeling Better q Basic HIV/ARV education Physical Illness q Clinical care to address comorbidities q Directly Observed Therapy q Treatment buddy Alcohol or Drug Use q q Opioid substitution therapy Directly Observed Therapy Peer support group Individual counseling Depression q q Screening for and management of depression Individual counseling Peer support group Treatment buddy

Individual Interventions (cont’d), Household Interventions BARRIERS INTERVENTIONS TO ADDRESS BARRIERS AND IMPROVE ADHERENCE INDIVIDUAL (continued) Pill burden q Change to fixed-dose combination or once-daily dosing if possible Lost or Ran Out of Pills q Extra supply of pills q Drug pick-up group q Educate patient to alert facility if it occurs Transportation Problems q Drug pick-up group q Three month supply when feasible q ART group Health Beliefs q Individual counseling for basic HIV/ARV education q Group counseling q Peer support group Scheduling Difficulty q q q Education (e. g. combine with daily routine such as bedtime or brushing teeth) Reminder devices (e. g. phone calls, SMS, watch alarm) Treatment buddy Three month supply when feasible ART group HOUSEHOLD Share with Others q Individual counseling for basic HIV/ARV education q Group counseling q Facilitate enrollment into care/Pr. EP for family members Fear of Disclosure q q Family/Partner Relationships q Group counseling Inability to Pay q Refer to social worker, peer worker, or NGO Food Insecurity q Refer to social worker, peer worker, or NGO Individual counseling Group counseling Peer support group Treatment buddy q Unmarked pill bottle q ART group q Couples counseling and testing

Institutional/Community Interventions BARRIERS INTERVENTIONS TO ADDRESS BARRIERS AND IMPROVE ADHERENCE INSTITUTIONAL/COMMUNITY Long Wait Times q Nurse-led or community-based care q Three month supply where feasible q ART group Stigma and Discrimination q Individual counseling q Group counseling q Peer support group q ART group Political Crisis/War/ Natural Disaster q Individual counseling q Case management

Additional Help to Take ARVs Cards 12 -15 provide further adherence counseling support. Identify common barriers to taking ARVs. Forgets Knowledge Side Effects Physical Illness Disclosure

Remembering to Take ARVs

Understanding Your ARVs

Managing Privacy and Getting Support

Subsequent Adherence Sessions • Use Talking Points on Card 16 to review the plan you discussed at the last session. – “Last time we met, we planned _____ (fill in with interventions decided upon at first stepped-up adherence session) to help you take ARVs. ” – “How has that been going? Are there any new challenges taking ARVs? ” – “Do you have any new ideas how to make it easier to take ARVs? ”

Subsequent Adherence Sessions • Measure adherence again based on the table. • Cards 5 -15 can be reviewed as needed to identify new barriers and interventions. • Be sure to document new barriers and interventions on the Enhanced Adherence Plan Tool!

Repeat Viral Load <1, 000 copies/ml

Repeat Viral Load ≥ 1, 000 copies/ml

Facilitator Demonstration • Using the flipchart, facilitators will do a demonstration of conducting adherence assessment and counseling

Questions?