Module 2 Understanding Advance Care Planning documents commonly


- Slides: 17

Module 2: Understanding Advance Care Planning documents commonly used in Queensland
Objective • The aim on this module is to enable you to understand the advance care planning (ACP) documents commonly used in Queensland. • After completing this module you should be able to: ü Explain why it is important to understand the differences between the Queensland documents ü Identify the sources of law in Australia and relevant Queensland legislation for ACP ü List the Queensland hierarchy of who can make decisions and provide consent for health care for a person who has lost decision-making capacity. ü List the suite of commonly used documents that are available in Queensland for ACP and indicate if they are legally-binding or have legal effect.
Relevance of ACP documents • Every competent adult has the right to accept or to refuse medical treatment. This right, based on the principle of autonomy, is the fundamental basis of ACP. • People may choose to document their advance care plans in various ways. In Queensland, the three most commonly used documents are: • Advance Health Directive • Enduring Power of Attorney • Statement of Choices. • These documents serve different purposes and vary in legal standing. • An understanding of these documents will help you to practise according to your duty of care as defined by your profession and your workplace. This includes advocating on behalf of the people in your care for end-of-life care according to their wishes, as expressed in ACP documents.
Sources of law in Australia In Australia, there are two sources of law: • Common law refers to decisions made by the courts. This law evolves with new case decisions made by judges in courts. • Statute law refers to laws passed by Parliament. In Australia there are laws passed by the federal and the state/territory governments; not all states/territories have the same laws.
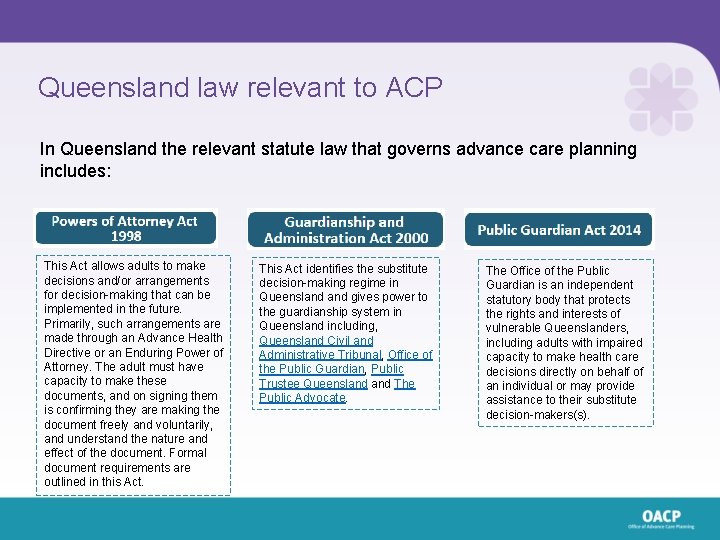
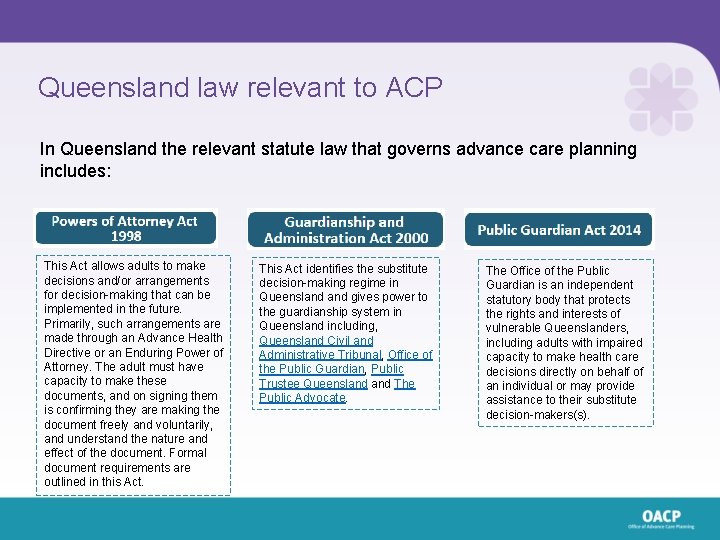
Queensland law relevant to ACP In Queensland the relevant statute law that governs advance care planning includes: This Act allows adults to make decisions and/or arrangements for decision-making that can be implemented in the future. Primarily, such arrangements are made through an Advance Health Directive or an Enduring Power of Attorney. The adult must have capacity to make these documents, and on signing them is confirming they are making the document freely and voluntarily, and understand the nature and effect of the document. Formal document requirements are outlined in this Act. This Act identifies the substitute decision-making regime in Queensland gives power to the guardianship system in Queensland including, Queensland Civil and Administrative Tribunal, Office of the Public Guardian, Public Trustee Queensland The Public Advocate. The Office of the Public Guardian is an independent statutory body that protects the rights and interests of vulnerable Queenslanders, including adults with impaired capacity to make health care decisions directly on behalf of an individual or may provide assistance to their substitute decision-makers(s).
Capacity and advance care planning Capacity refers to a person’s ability to make a specific decision in a particular area of their life. A person has capacity for health care decisions when they can understand the information provided by a doctor about their health and treatment options and are able to freely make and communicate decisions regarding their care. • The law assumes that every adult has capacity, unless it has been proven otherwise, to make their own decisions. • Health care decisions must also be made of the person’s free will. • Impaired capacity does not mean that a person cannot make some decisions. The law states that people with impaired capacity have a right to adequate and appropriate support in decision-making. • If you have any doubts about a person’s capacity to complete an advance care plan or make decisions about their health care, you should follow your relevant workplace policies and procedures. • The Queensland Capacity Assessment Guidelines 2020 (capacity guidelines) are available to help understand capacity, capacity assessment and the legal tests of capacity under Queensland’s guardianship legislation.
Consent to withdraw or withhold treatment • In Queensland, by law, consent is required to withhold or withdraw life-sustaining measures except in cases of medical emergency. • The GAA 2000 outlines, without limiting, each of the following is a life-sustaining measure; a) Cardiopulmonary resuscitation b) Assisted ventilation; c) Artificial nutrition and hydration • If a person has capacity then they provide their own consent for treatments – they may accept or refuse any treatments according to their wishes. Health care clinicians must respect those decisions to refuse treatment, and, if directed to do so by the person with capacity, doctors can legally withhold or withdraw life-sustaining treatment, even if this might result in the patient’s death. • It can also be lawful for a substitute decision-maker to ask that life-sustaining treatment be withheld or withdrawn from someone who no longer can decide on treatment for themselves. • The people in your care, their families and substitute decision-makers may demand treatment which doctors do not consider to be good medical practice, however doctors are not compelled to provide such treatments.
The substitute decision-maker In Queensland, for adults with capacity: • A substitute decision-maker can legally be appointed as an attorney in an Enduring Power of Attorney or Advance Health Directive For adults without capacity: • A substitute decision-maker can be appointed by the Queensland Civil and Administrative Tribunal. This may be a private guardian (family/friend) or Public Guardian. Anyone who acts as an attorney, including the Public Guardian, must apply the General principles and health care principles under Queensland’s guardianship framework.
The Public Guardian • A person with capacity who doesn’t have anyone suitable to appoint as their attorney for personal and health matters, can apply to appoint the Public Guardian. • Note: the Office of the Public Guardian does not manage a person’s money - this is the role of the Public Trustee Queensland. • If a person wishes to appoint the Public Guardian as their attorney for personal and health matters, they should contact the Office of the Public Guardian for further information at: Phone: 1300 653 187 Email: publicguardian@publicguardian. qld. gov. au Website: www. publicguardian. qld. gov. au
A Statutory Health Attorney (SHA) • If an attorney or guardian has not been appointed, a SHA can make decisions. This is someone with authority under law to make health care decisions for a person if they become unable to make them because of illness or incapacity. The SHA regime in Queensland comes under the Powers of Attorney Act 1998. • A person does not appoint a SHA; this is an informal arrangement determined by their relationship with the adult. A person’s SHA is the first available adult, who is culturally appropriate and has a close and continuing relationship with the person, This is a: • spouse or de facto partner • person who is responsible for their primary care, but not a paid carer • close friend or relative over the age of 18 • If no-one listed above is readily available and culturally appropriate to exercise power for a matter, the public guardian is the adult’s statutory health attorney for the matter. Note: Paid staff in any health care setting cannot act as a SHA.
Hierarchy of decision making for a person who has lost capacity In Queensland, when consent is required for health care, including withholding or withdrawing life-sustaining treatments for a person without capacity, the following hierarchy or priority for gaining consent should be followed: 1. The person’s valid Advance Health Directive expressing their consent, or refusal, for specific treatments in specific circumstances 2. A Queensland Civil and Administrative Tribunal appointed guardian 3. The person’s attorney, legally-appointed in the valid Enduring Power of Attorney or Advance Health Directive 4. The person’s Statutory Health Attorney 5. The Public Guardian, Statutory Health Attorney of last resort.

Commonly used ACP documents • As already mentioned, there is a suite of ACP documents commonly used in Queensland: • Enduring Power of Attorney (EPOA) • Advance Health Directive (AHD) • Statement of Choices (So. C). • A documented advance care plan normally consists of one or more of these documents. • A person does not need to complete all three documents. • A person can choose to complete any of the documents they think suits their needs and personal values.
Enduring Power of Attorney (EPOA) • An EPOA is a legally-binding document used by a person with decision-making capacity to appoint an attorney for personal (including health care) and/or financial matters. • An EPOA allows for the person to nominate one or more attorneys, and outlines when and how their power would function. • The EPOA has two versions: • EPOA Short Form: used to appoint the same attorney(s) for personal (including health care) matters and/or financial matters • EPOA Long Form: used to appoint different attorney(s) for personal (including health care) matters and/or financial matters • If a person wishes to revoke their EPOA this may be done on the approved Revocation of Enduring Power of Attorney form while the individual has capacity.
Advance Health Directive (AHD) (1) • The Advance Health Directive is a legally-binding document that can only be completed by an adult with decision-making capacity. It allows a person to give directions about his or health care in the future, including refusing lifesustaining treatment. The AHD can also be used to appoint an attorney for health matters. • It only comes into effect when a person has impaired capacity (i. e. is unable to make their own decisions) for the matter covered by the direction. • By law, decisions within the AHD must be followed. There are, however, some circumstances where the AHD may be overruled or not relevant. For instance: • If the AHD does not contain instructions reflecting the medical scenario that actually occurs, then it cannot be used to direct medical treatment. • If the treatment directed by the person is considered inconsistent with good medical practice.
Advance Health Directive (2) • Individuals are encouraged to read the AHD and explanatory guide • talk about their choices with their substitute decision-makers • talk with their Doctor about questions related to completion of their AHD • A doctor will need to complete Section 5 of the AHD form • Is completed in consultation with a doctor and witnessed by an eligible witness (a Justice of the Peace, Commissioner for Declarations, Notary Public or lawyer) • If an interpreter/translator interprets or translates an AHD for a non-English speaking person, a completed and signed Interpreter's/Translator's statement should be attached to the document • If a person wishes to revoke an AHD this must be done in writing while the individual has capacity.
Statement of Choices (So. C) The Statement of Choices is a values-based document to guide decision making about future health care if a person becomes unable to participate in decisionmaking. The Statement of Choices form: • Records and focuses on the person’s views, wishes and preferences for future health care • Records contact details of the person’s substitute decision-makers • It is not legally-binding but as it records the person’s objections to withholding or withdrawing treatments, it can have legal effect providing information about the person’s interest, values and beliefs that health professionals must take into account • These views, wishes and preferences can be taken into account at the time a decision is required.
Summary In this module you have learnt about: • Why it is important to understand the differences between the Queensland documents • The sources of law in Australia and relevant Queensland legislation for ACP • The Queensland hierarchy of who can make decisions and provide consent for health care for a person who has lost decision-making capacity • The suite of commonly used documents that are available in Queensland for ACP and whether they are legally-binding or have legal effect.