MODULE 12 Integrated Care Model 1 OBJECTIVES 1

MODULE 12 Integrated Care Model 1
OBJECTIVES 1) Define integrated care – the combination of behavioral and primary health care 2) Learn about three different integrated care models 3) Understand the role CHWs play in the integrated care models 2
DEFINING INTEGRATED CARE Behavior al Health Primary Care 3
DEFINITION The Substance Abuse and Mental Health Services Administration (SAMHSA) defines integrated care as “the systematic coordination of general and behavioral health. Integrating mental health, substance abuse and primary care services produces the best outcomes and proves the most effective approach to caring for people with multiple healthcare needs. ” 4

HEALTHCARE INTEGRATION WATCH VIDEO 5
WHY INTEGRATED CARE? People with mental and substance abuse disorders may die decades earlier than the average person mostly from untreated and preventable chronic illnesses like: • • hypertension diabetes obesity cardiovascular disease 6
GATEWAY TO BEHAVIORAL HEALTH Primary care settings have become the gateway to the behavioral health system, and primary care providers need support and resources to screen and treat individuals with behavioral and general healthcare needs. 7
PREVALENCE OF CO-OCCURRING CONDITIONS AND THE IMPORTANCE OF INTEGRATION • Efforts to improve population health and reduce costs must adequately address behavioral health. • Primary care providers have experienced challenges with regards to treating chronic illness among individuals with mental health/substance abuse disorders. • Neuropsychiatric disorders are now the number one cause of disability. • Depression and other Mental 8 Health/Substance Use Disorder are associated
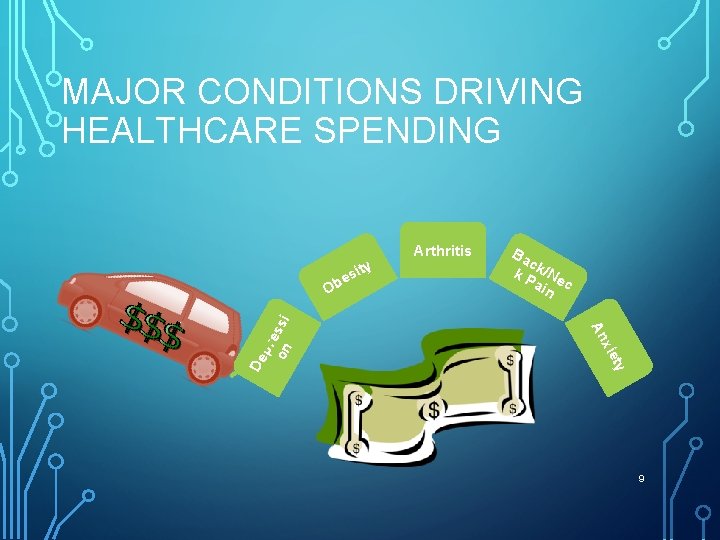
MAJOR CONDITIONS DRIVING HEALTHCARE SPENDING s Arthritis Ba c k P k/Ne ain c y t xie An De pre on ssi e Ob ity 9
CO-OCCURRING CONDITIONS • Physical and behavioral health conditions have high rates of cooccurrence, with unmet behavioral health needs frequently complicating treatment for medical practitioners. • One out of five patients with coronary heart disease and one out of three patients with congestive heart failure also experience depression but are not diagnosed or treated. • The interaction between a person’s psychiatric status and health is dramatic: one in three patients who go to the emergency room with chest pains is actually experiencing panic disorder or depression. 10

INTEGRATED MODEL BENEFITS • Purchasers are creating incentives. • Health plans and MBHOs are developing systems of care. • Accountable Care Organizations (ACOs) and Community Care Organizations (CCOs) are creating provider networks. • Providers are affiliating across primary and behavioral healthcare. 11
THREE INTEGRATED CARE MODELS Primary Care Settings Behavioral Health Settings Medical Health Home 12
PRIMARY CARE SETTINGS • Medical Hospital • Physician Offices • Community Based Outpatient Clinics • Critical Access Hospital • Immediate Care Center • Health Clinics 13
PRIMARY CARE SETTINGS Why seek MH care in PC settings? • Uninsured or underinsured • Cultural beliefs and attitudes • Limited access to public MH services • Stigma of seeking Mental Health Services • Availability of MH services, especially in rural areas *PC = Primary Care *MH = Mental Health 14
PRIMARY CARE SETTINGS Mild to moderate BH issues are common in PC settings: • Anxiety, depression, substance use in adults • Anxiety, ADHD, behavioral problems in children Prevention and early intervention opportunity • People with common medical disorders have high rates of BH issues: i. e. diabetes, heart disease, & asthma + depression 15 Worse outcomes & higher costs if both problems aren’t addressed
BEHAVIORAL HEALTH SETTINGS • Psychiatric Hospital • Psychiatric Unit of a Medical Hospital • Psychiatrist, Psychologist or Therapist Office • Outpatient Clinics • Addiction Treatment Center • Domestic Violence Shelter • Residential Treatment Center 16
BEHAVIORAL HEALTH SETTINGS • People with serious mental illness (SMI) are dying 25 years earlier than the general population. • 2/3 of premature deaths are due to preventable/treatable medical conditions such as cardiovascular, pulmonary, and infectious diseases. • Studies suggest that depression increases the risk of developing Type 2 Diabetes by more than 20% in young adults. 17
BH CONSUMERS WHO SEEK CARE IN PC SETTINGS • Are less likely to receive effective medical care, including preventive services, • Report difficulties establishing relationships with PC Physicians, • Express dissatisfaction in time limitations with PC staff, and • Feel the stigma of having a MH diagnosis. 18
METHODS FOR CLINICALLY ALIGNING PC AND BH • Training for primary care practitioners on identification and treatment of behavioral health conditions • Screening for behavioral health conditions in primary care settings • Screening for medical conditions in behavioral health organizations 19
METHODS FOR CLINICALLY ALIGNING PC AND BH (CONT. ) • Providing consultation services to primary care practitioners • Creating strategies for increasing patients’ health literacy and activation • Co-locating behavioral health and primary care services • Delivering integrated team-based behavioral health and primary care 20
WHOLE HEALTH ACTION MANAGEMENT Promising Practice: The Whole Health Action Management Program (WHAM) was developed by the SAMHSA-HRSA Center for Integrated Health Solutions and is a peer-led, research-informed program that includes: • Person-Centered Goals • Weekly Action Plan • Daily/Weekly Personal Log • One-to-One Peer Support • Weekly Peer Support Group 21
MEDICAL HEALTH HOME MODELS • Person-Centered Healthcare Home • Healthcare home may be a PC or BH setting depending on a person’s preference • Ongoing relationship with a PCP • Team with collective responsibility for ongoing care • “Whole person” orientation • PCMHs need MH and SU capacity – i. e. , MH and SU services need to be integrated into the medical home 22
UNDERSTANDING THE ROLE CHWS PLAY IN THE INTEGRATED CARE MODELS 23
24 CHWS PRIMARY ROLE • Care Coordination • Patient Engagement • Health Education • Treatment Compliance Overarching Goal: Deliver better patient care for the healthcare systems and reduce costs.
FIVE MODELS IN WHICH CHWS PROVIDE CARE 1. Member of health care team 2. Navigator of the health care system 3. Screening and health education provider 4. Outreach-enrolling-informing agent 5. Organizer 25
• 1. Measuring and monitoring blood CHW ROLE IN A “MULTIDISCIPLINARY pressure, blood glucose TEAM” • Providing social support and helping them solve problems • Creating community-clinical linkages • Assessing and supporting selfmanagement patient plans • Increasing the team’s cultural competence • Supporting individualized goal- 26
2. HELPING PATIENTS NAVIGATE HEALTH CARE SYSTEMS • Insurance Enrollment • Appointments • Referrals • Transportation • Child Care Arrangements • Bilingual Providers or Translators 27
3. SCREENING AND HEALTH EDUCATION PROVIDER Educating patients/families on: • Lifestyle Changes • Adherence to Treatments • Medications Compliance 28
4. OUTREACH-ENROLLING-INFORMING AGENT • Providing social support by listening to the concerns of patients and their family members and helping them solve problems • Creating community-clinical linkages to help create a team based approach through supporting and enhancing the work of healthcare team • Assessing how well a self-management plan is helping patients to meet their goals 29
5. ORGANIZER Playing a role in selfmanagement program administration by leading or supporting self-management programs 30
ASSIST WITH ACA IDENTIFIED ESSENTIAL HEALTH SERVICES • • • Ambulatory patient services Emergency services Hospitalization Maternity and newborn care Mental health and substance abuse disorder services Prescription drugs Rehabilitative and habilitative services Laboratory services Preventative and wellness services and chronic disease management 31 Pediatric services
ACA FREE PREVENTATIVE SCREENING Educate the consumer in the ACA mandated free preventative screening services that include: • • • Cancer Chronic conditions Immunization health promotion Pregnancy related Reproductive health 32
CHWS IMPACT THE BOTTOM LINE Using their unique position, skills, and an expanded knowledge base, CHWs can help reduce system costs for health care by linking patients to community resources and helping patients avoid unnecessary hospitalizations and other forms of more expensive care as they help improve outcomes for community members. 33
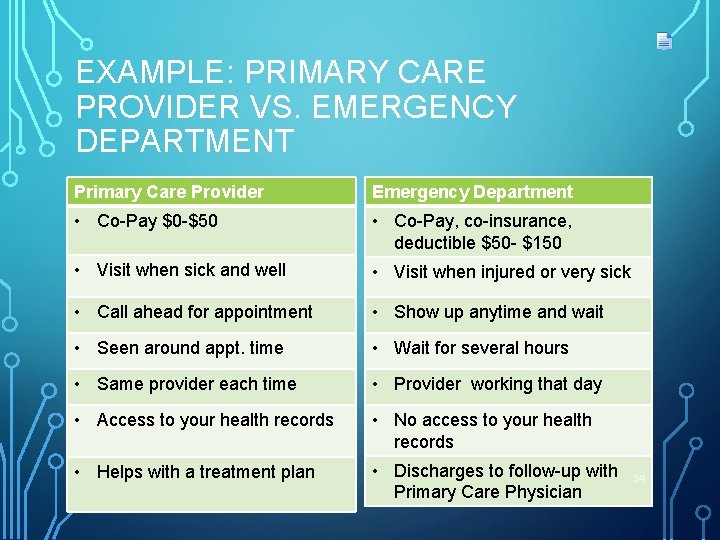
EXAMPLE: PRIMARY CARE PROVIDER VS. EMERGENCY DEPARTMENT Primary Care Provider Emergency Department • Co-Pay $0 -$50 • Co-Pay, co-insurance, deductible $50 - $150 • Visit when sick and well • Visit when injured or very sick • Call ahead for appointment • Show up anytime and wait • Seen around appt. time • Wait for several hours • Same provider each time • Provider working that day • Access to your health records • No access to your health records • Helps with a treatment plan • Discharges to follow-up with Primary Care Physician 34
CONCLUSION In this module we: • Defined integrated care - behavioral health combined with primary health care • Learned about three different integrated care models • Covered the role CHWs play in the integrated care models 35
EVALUATION Please complete the module evaluation. 36
SOURCES • http: //www. integration. samhsa. gov/integrated-caremodels/Healthcare_Integration_In_the_Era_of_ACA. pdf HEALTHCARE INTEGRATION IN THE ERA OF THE AFFORDABLE CARE ACT Colette Croze, MSW; Croze Consulting for the Association for Behavioral Health and Wellness July 2015 • • • http: //www. cdc. gov/dhdsp/docs/chw_brief. pdf www. integration. samhsa. gov store. samhsa. gov/product/Services-Integration/SMA 07 -4294 http: //www. integration. samhsa. gov/research http: //nashp. org/wp-content/uploads/2016/01/Peer-Supports. pdf www. thenationalcouncil. org for more info on the person-centered healthcare home and the role of MH/SU in medical homes. • www. pcpcc. net site for more about medical homes. 37
- Slides: 37