Module 1 Reinforcing and Enhancing Concussion Knowledge Version




- Slides: 29
Module 1: Reinforcing and Enhancing Concussion Knowledge Version used for Training Peer Concussion Educators Presented by: William Ernst, Psy. D. , Neuropsychologist and Associate Professor of Psychology Brendan Connell, M. S, LAT, ATC, Assistant Athletic Trainer For: Brianna Ferrell, Meghan Guagenti, Andrew Hildebrand Matt Pedrick Peer Concussion Educators Chestnut Hill College Peer Concussion Education Program
• Presentation Overview: • Part 1: Review and Discuss Concussion Education Materials Required by Chestnut Hill College (CHC) Department of Athletics for all student-athletes • Part 2: Provide more in-depth information on concussion – Pathophysiology of concussion – Symptoms of concussion – Recovery from concussion – Return to Play Protocol at CHC – Rationale for the Return to Play Protocol at CHC – Concussion prevention
Part 1: Review and Discuss Concussion Education Materials Required by CHC Department of Athletics for all student-athletes – These materials are located in appendices A-C and include: • Concussion: A Fact Sheet for Student-Athletes [developed by the NCAA and CDC (see Appendix A)] • Chestnut Hill College Student-Athlete Concussion Statement (see Appendix B) • The Chestnut Hill College Athletics Concussion Policy (see Appendix C)
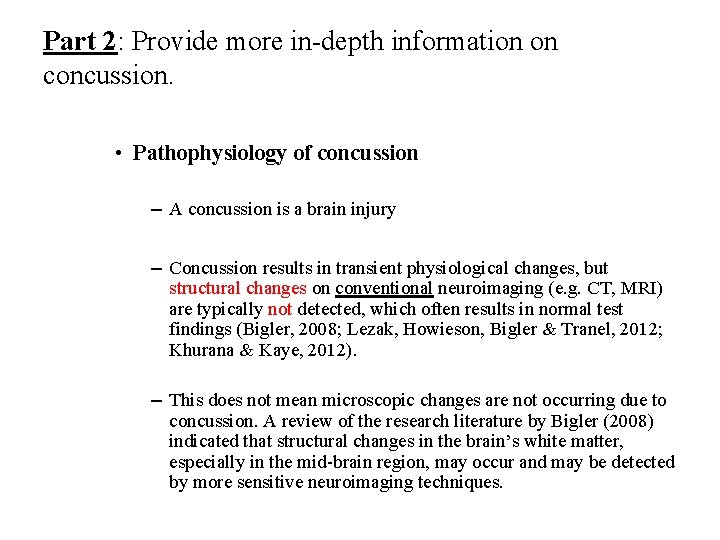
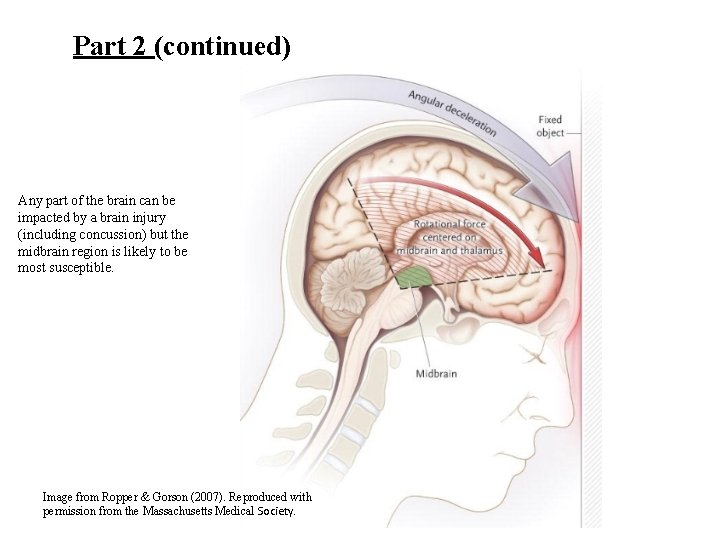
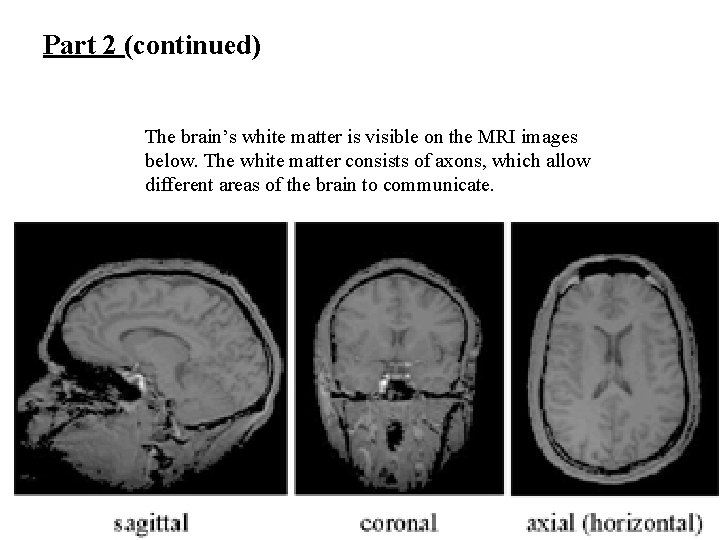
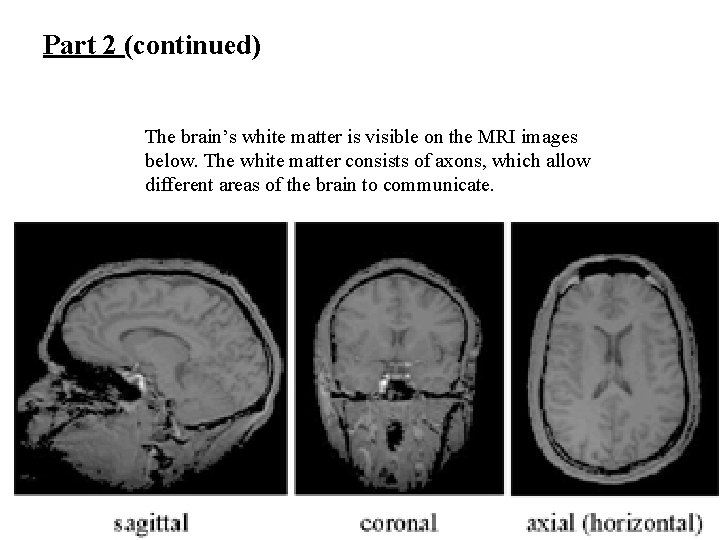
Part 2: Provide more in-depth information on concussion. • Pathophysiology of concussion – A concussion is a brain injury – Concussion results in transient physiological changes, but structural changes on conventional neuroimaging (e. g. CT, MRI) are typically not detected, which often results in normal test findings (Bigler, 2008; Lezak, Howieson, Bigler & Tranel, 2012; Khurana & Kaye, 2012). – This does not mean microscopic changes are not occurring due to concussion. A review of the research literature by Bigler (2008) indicated that structural changes in the brain’s white matter, especially in the mid-brain region, may occur and may be detected by more sensitive neuroimaging techniques.
Part 2 (continued) Any part of the brain can be impacted by a brain injury (including concussion) but the midbrain region is likely to be most susceptible. Image from Ropper & Gorson (2007). Reproduced with permission from the Massachusetts Medical Society.
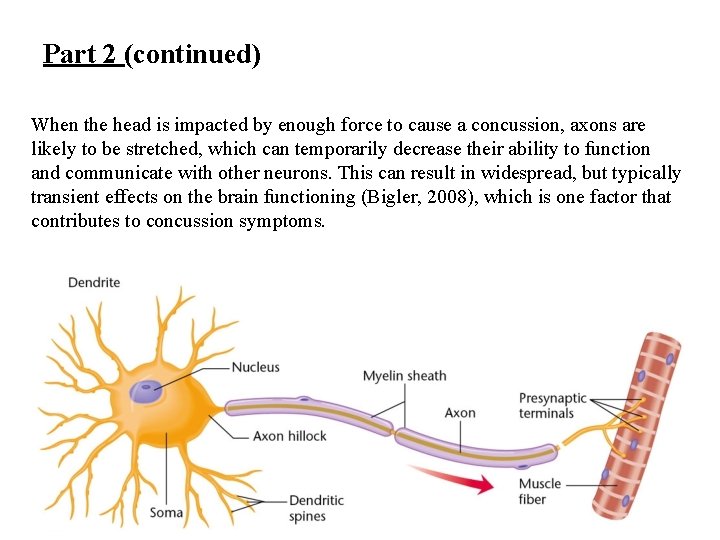
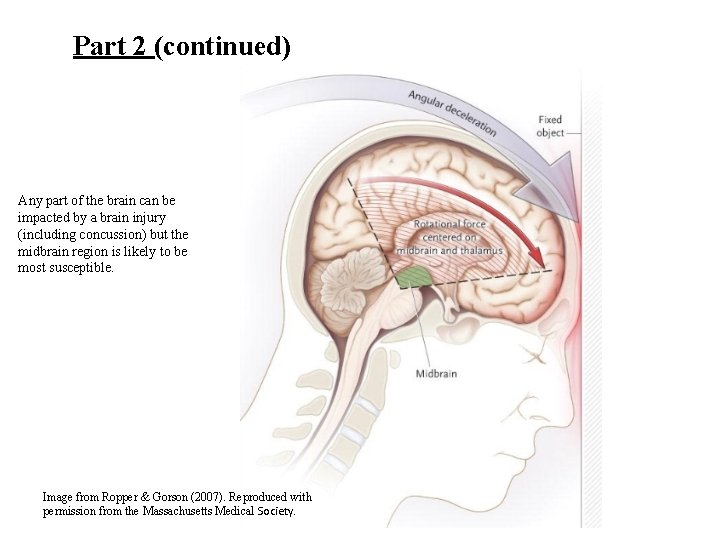
Part 2 (continued) When the head is impacted by enough force to cause a concussion, axons are likely to be stretched, which can temporarily decrease their ability to function and communicate with other neurons. This can result in widespread, but typically transient effects on the brain functioning (Bigler, 2008), which is one factor that contributes to concussion symptoms.
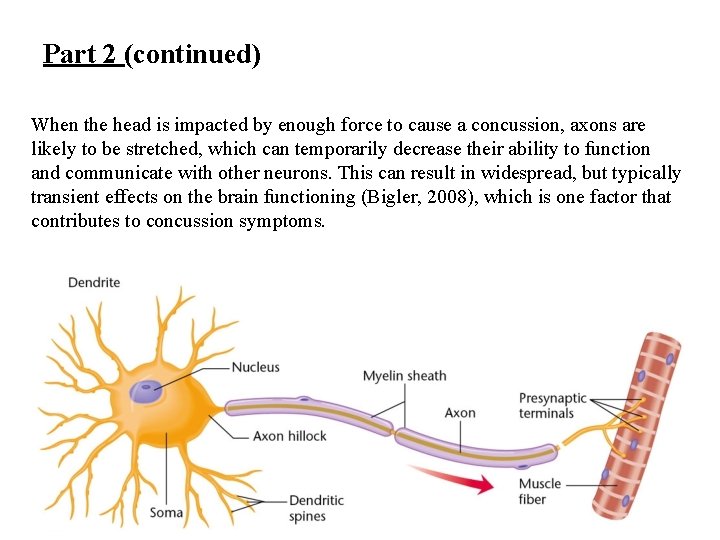
Part 2 (continued) The brain’s white matter is visible on the MRI images below. The white matter consists of axons, which allow different areas of the brain to communicate.
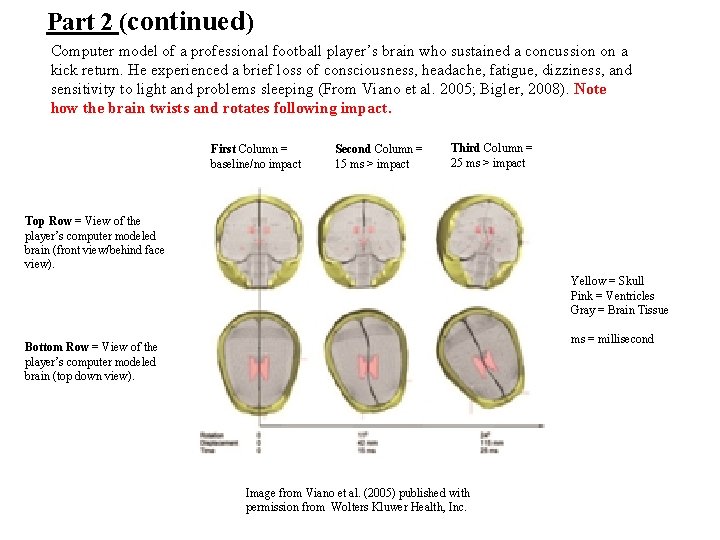
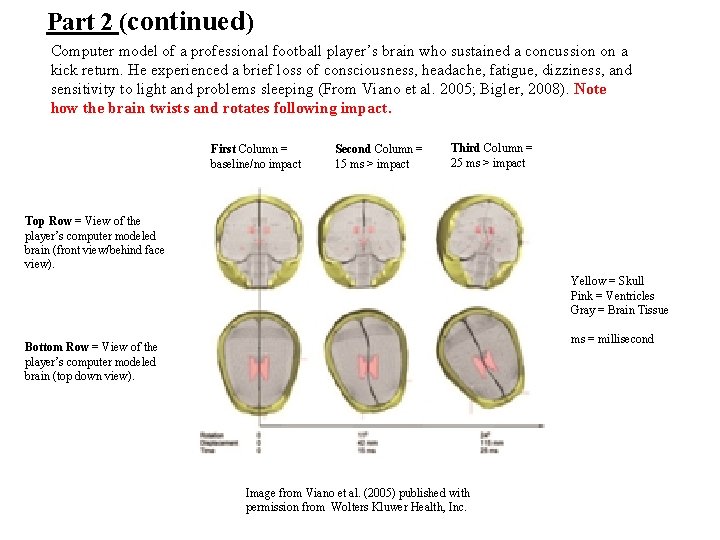
Part 2 (continued) Computer model of a professional football player’s brain who sustained a concussion on a kick return. He experienced a brief loss of consciousness, headache, fatigue, dizziness, and sensitivity to light and problems sleeping (From Viano et al. 2005; Bigler, 2008). Note how the brain twists and rotates following impact. First Column = baseline/no impact Second Column = 15 ms > impact Third Column = 25 ms > impact Top Row = View of the player’s computer modeled brain (front view/behind face view). Yellow = Skull Pink = Ventricles Gray = Brain Tissue ms = millisecond Bottom Row = View of the player’s computer modeled brain (top down view). Image from Viano et al. (2005) published with permission from Wolters Kluwer Health, Inc.
Part 2 (continued) – Following concussion/MTBI, significant increases in acetylcholine and excitatory neurotransmitters such as glutamate may occur. This causes neuronal depolarization which is likely to cause cognitive difficulties and other concussion symptoms (Lucas & Addeo, 2006). – Therefore, a significant blow to the head results in rotational forces that act on the brain, which stretches axons. When the axons are stretched, their ability to regulate neurotransmitters, especially excitatory ones like glutamate, is decreased. The resulting neurochemical dysregulation cause widespread abnormalities in brain functioning, which in turn contributes to concussion symptoms including loss of consciousness, confusion, amnesia and persisting cognitive deficits (Khurana & Kaye, 2012).

Part 2 (continued) • Brief video from the NCAA indicating what happens in the brain during and following concussion. • The video can be viewed via You. Tube by clicking on the link below or by advancing to the next slide. – https: //www. youtube. com/watch? v=-6 HB 8 HSl. C-k

Part 2 (continued) • Symptoms of Concussion – Cognitive Symptoms » Attention/Concentration Problems (e. g. difficulty remaining focused; easily distracted) » Memory difficulties (e. g. forgetting day of week, current location, game-related information including score and plays as well as learning new information) » Slowed reaction time (e. g. trouble responding to questions quickly and keeping up with conversations)
Part 2 (continued) – Cognitive Symptoms (continued) » Difficulty reasoning (e. g. poor problem solving that is a decline from pre-concussion status). » Taking longer to figure things out » Difficulty with planning and organization, which is a decline from pre-concussion status) » Confusion
Part 2 (continued) – Physiological and sensory symptoms » » » » Loss of consciousness Headache Balance problems Dizziness Double or blurry vision Sensitivity to light and noise Ringing in ears
Part 2 (continued) – Physiological and sensory symptoms (continued) » Sleep Difficulties including difficulty falling asleep, as well as sleeping more or less than usual (Cournoyer & Tripp, 2014). » Drowsiness » Nausea (e. g. feeling like you might vomit) » Fatigue (e. g. feeling tired often or getting tired more easily when working on the computer, reading or engaging in physical activity. » Feeling groggy or like your mind is in a fog. • Note: Symptoms in red are less likely to be associated with concussion by various groups according to research studies (e. g. , Cournoyer & Tripp, 2014; Kelley, Ernst, Kneavel & Manfredi, 2015).
Part 2 (continued) – Emotional and Behavioral Symptoms » Irritability (Cournoyer & Tripp, 2014) » Anxiety/nervousness especially more than is typical (Cournoyer & Tripp, 2014; Kelley, Ernst, Kneavel & Manfredi, 2015) » Feeling depressed or sad (Kelley, Ernst, Kneavel & Manfredi, 2015) » More emotional (Cournoyer & Tripp, 2014; Kelley, Ernst, Kneavel & Manfredi, 2015) » Change in personality (Cournoyer & Tripp, 2014) Note: Symptoms presented were adapted from the NCAA and CDC Concussion: A fact sheet for Student-Athletes and the National Athletic Trainers’ Association Position Statement: Management of Sport Concussion. The symptoms reported do not represent an exhaustive list. Note: Research conducted by Kroshus & Baugh (2015) found that studentathletes would like symptoms of concussion covered in concussion education programs.
Part 2 (continued) • Recovery from Concussion – Recovery is associated with the axonal, neurochemical and metabolic changes in the brain returning to normal and may take days or weeks for most people. The following are likely to help the recovery process. – Rest and Limit Activity » Physical exertion, including exercise, can worsen concussion symptoms or cause them to reappear. » Activities that require considerable mental activity including texting, studying, working on the computer, videogames and anything else that requires a lot of concentration can also worsen symptoms or cause them to reappear (Broglio et al. , 2014).

Part 2 (continued) – Avoid alcohol » Alcohol can slow the brain’s recovery process from concussion. » Alcohol can impair your judgement, motor skills, and balance, which can increase your risk for additional injury including brain injury. – Avoid Driving » Driving while experiencing symptoms of concussion including confusion, dizziness, poor attention is dangerous to yourself and others. Recommendations for recovering from concussion were adapted from the NCAA and CDC Concussion: A fact sheet for Student-Athletes and the National Athletic Trainers’ Association Position Statement: Management of Sport Concussion. The symptoms reported do not represent an exhaustive list.
Part 2 (continued) • Summary of the Concussion Return to Play Protocol at CHC • Im. PACT Testing for Student-Athletes • Completed before the first practice at CHC to establish a baseline of cognitive functioning for all student athletes. – Tests reaction time, verbal and visual memory, visual motor skills, impulse control, and also records symptoms. Computer administered. • If an athlete presents with concussion like symptoms, they are evaluated by a certified athletic trainer. If a concussion is suspected, then the student athlete is removed from activity. • Post-Concussion Im. PACT testing is administered to compare the studentathletes functioning following concussion with their baseline functioning as needed. • Impact testing is one of many tools used by healthcare professionals in order to assess, monitor, treat, and determine when an athlete can return to sport safely.
Part 2 (continued) • Sideline Evaluation – SCAT 3 • Conducted by a certified athletic trainer – Used during practices or competitions • • • Mechanism of Injury Symptoms Balance & coordination Cognitive function Symptoms with Exertion
Part 2 (continued) Stepwise Return to Play Process • • Stage 1: Complete Rest. Once asymptomatic of concussive symptoms, proceed to next stage. Stage 2: 30 -40% of max exertion. Done in a quiet area, limited head movement. – Light aerobic work or treadmill walking. 10 -15 minutes. – Static stretching. – Balance exercises eyes open/closed. • Stage 3: 60 -80% maximal exertion. – – – • Active stretching. Dynamic warmup. Aerobic activity. 25 -30 minutes. Strength training. Functional squat, pushups, Balance and proprioception. Bosu ball balance and catch, Bird dips, Skaters, Agility drills. Box drill, T-drill, Ladders, Stage 4: 80% max exertion non-contact. – Sports specific training. – Interval training – Plyometric activities. Box jumps, Burpees, double and single leg bounding. • Stage 5: Full exertion with contact. – Aggressive strength and conditioning. – Practice and game intensity speed.
Part 2 (continued) • Rationale for the Concussion Return to Play Protocol at CHC – Assess whether the student-athlete has recovered from her/his concussion (e. g. no longer has symptoms and feels back to normal) to determine whether she/he is safe to return to play. – Determining whether a student-athlete is safe to resume participation in athletics is crucial as retuning to play prematurely (e. g. while still experiencing symptoms) is likely to delay the typical recovery period from concussion resulting in symptoms including but not limited to those below taking longer to resolve. » » Headache Dizziness and balance problems Fatigue Personality change
Part 2 (continued) » Problems with attention and memory, which are likely to impact academic functioning and the ability to carry out daily tasks (e. g. managing finances) and can persist especially if appropriate steps are not taken regarding recovery from concussion and return to play. » You are much more likely to have a repeat concussion if you return to play before your symptoms resolve. » In rare cases, second impact syndrome can occur, which results when a second concussion is sustained while the student-athlete is still symptomatic. The neurochemical and metabolic changes occurring in the brain from the initial concussion increase dramatically resulting in diffuse brain swelling, which may result in death.
Part 2 (continued) » Increased risk for sustaining another concussion in the future. » Student-athletes that sustain multiple concussions are likely to take longer to recover following each successive concussion and are at an increased risk of experiencing persistent, long-term consequences like those discussed previously. • Research conducted by Kroshus & Baugh (2015) found that student-athletes would like information on the long-term consequences of concussion, impact on academic functioning and the importance of reporting concussion symptoms to be covered in concussion education programs.
Part 2 (continued) » In summary, the Rationale for the Concussion Return to Play Protocol at CHC is to ensure that concussion is safely managed in order to: • Avoid dangerous medical complications • Avoid medical complications that can negatively impact your health and wellbeing (e. g. chronic headaches) • Avoid persisting cognitive impairments that can impact daily activities and academic functioning. • Get you back to the field of play when you are safe to do so and when you are ready to perform your best.
Part 2 (continued) • Concussion Prevention – Do not initiate contact with head or helmet – Play hard but safe. Avoid playing recklessly. Try to avoid head to head, elbow to head or stick to head contact. – Practice and perfect appropriate skills of the sport. » From Concussion: A Fact Sheet for Student-Athletes by the NCAA and CDC.
References Bigler, E. D. (2008). Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. Journal of the International Neuropsychological Society, 14(01), 1 -22. Broglio, S. P. , Cantu, R. C. , Gioia, G. A. , Guskiewicz, K. M. , Kutcher, J. , Palm, M. , & Mc. Leod, T. C. V. (2014). National Athletic Trainers' Association position statement: Management of sport concussion. Journal of athletic training, 49(2), 245. Cournoyer, J. , & Tripp, B. L. (2014). Concussion knowledge in high school football players. Journal of Athletic Training, 49(5), 654 -658. Guskiewicz, K. M. , Bruce, S. L. , Cantu, R. C. , Ferrara, M. S. , Kelly, J. P. , Mc. Crea, M. , . . . & Mc. Leod, T. C. V. (2004). National Athletic Trainers' Association position statement: Management of sport-related concussion. Journal of Athletic Training, 39(3), 280. Kelley S. M. , Ernst, W. J, Kneavel, M. & Manfredi, R. (2015). Youth Football Coaches’ Understanding of Concussion Identification and Management. (Unpublished doctoral dissertation). Khurana, V. G. , & Kaye, A. H. (2012). An overview of concussion in sport. Journal of Clinical Neuroscience, 19(1), 1 -11. Kroshus, E. , & Baugh, C. M. (2015). Concussion Education in US Collegiate Sport: What is happening and what do athletes want? . Health Education & Behavior, doi: 1090198115599380.

References (continued) Lezak, Howieson, Bigler, & Tranel, 2012 Lezak, M. D. , Howieson, D. B. , & Bigler, E. D. , Tranel, D. (2012). Neuropsychological Assessment (5 th ed. ). New York: Oxford University Press. Lucas, J. A. , & Addeo, R. (2006). Traumatic brain injury and post-concussion syndrome. Clinical Neuropsychology, 2, 351 -380. National Collegiate Athletic Association & Center for Disease Control (2013). Concussion: A fact sheet for student-athletes. Retrieved from http: //fs. ncaa. org/Docs/health_safety/Con. Fact. Sheetsa. pdf Ropper, A. H. & Gorson, K. C. (2007). Clinical practice. Concussion. New England Journal of Medicine, 356, 166– 172. Viano, D. C. , Casson, I. R. , Pellman, E. J. , Zhang, L. , King, A. I. , & Yang, K. H. (2005). Concussion in professional football: Brain responses by finite element analysis: Part 9. Neurosurgery, 57(5), 891 -916.
Appendices Please visit the Materials and Videos site for all appendices. • Appendix A: Concussion: A Fact Sheet for Student-Athletes • Appendix B: Chestnut Hill College Student-Athlete Concussion Statement • Appendix C: The Chestnut Hill College Athletics Concussion Policy