Module 1 OT Health Promotion Health Behavior and
Module 1: OT Health Promotion, Health Behavior, and Public Health Barry University MSOT Program OTR 675: Models of Service Delivery Fall Semester
• Topics • 1. OT Theory and Conceptual Models for Health Promotion • 2. Health Behavior Frameworks for Health Promotion • 3. Public Health and Health Promotion
1. OT Theory and Conceptual Models for Health Promotion • Conceptual Models, based in theory, provide the foundational contexts for program design, implementation, and evaluation • When utilized, these models can enhance the design and evaluation of health promotion programming. • These models have the ability to capture data in promoting evidence-based practice
OT Conceptual Models • Ecology of Human Performance Framework (EHP) • Model of Human Occupation (MOHO) • Occupational Adaptation Model (OA) • Person-Environment-Occupation Model (PEO) • Person-Environment-Occupation-Performance Model (PEOP) • KAWA Model
Ecology of Human Performance (EHP) • Interventions are intended to assist individuals in recognizing their health needs, acting, and gaining competence in the performance of these behaviors. • An Ecology of Human Performance Health Promotion example is the case of Cindy, pp. 28 -29, Scaffa, Reitz, & Pizzi (2010).
Model of Human Occupation (MOHO) PRINCIPLES: • Humans have an innate need for occupation, and the ability to fulfill this need promotes health and wellbeing. • Health and well-being depend on a constant inter -play between the person and the environment.
Occupational Adaptation (OA) ASSUMPTIONS: • Competence in occupation is a lifelong process of adaptation to internal and external demands to perform. • Demands to perform occur naturally as part of the person’s occupational roles and the context • Dysfunction occurs because the person’s ability to adapt has been challenged to the point that the demands for performance are not satisfactorily met.
(OA Assumptions, cont’d) • At any stage of life, the person’s adaptive capacity can be overwhelmed by impairment, physical or emotional disability, and stressful life events. • The greater the level of dysfunction, the greater the demand for changes in the person’s adaptive response. • Success in occupational performance is a direct result of the person’s ability to adapt with sufficient mastery to satisfy the self and others
Person-Environment. Occupation (PEO) • Individuals are viewed holistically with their unique combination of physical, cognitive, and affective characteristics and their life experiences. • Main constructs of PEO Model: • Person • Environment • Occupation • Primary Assumption of PEO Model: the person is intrinsically motivated and continually developing. • “The Person” in this model refers to an individual, group, or organization
Person-Environment-Occupation-Performance (PEOP) • This model views health as an enabler, not as an outcome. • When people are healthy, they can optimally participate in daily occupations that promote life satisfaction and enhance quality of life. • This model illustrates the interrelationships between the primary constructs of person, environment, occupation, and performance and the desired outcomes of occupational performance and participation, wellbeing, and quality of life.
Kawa Model • Model constructs include: • Environmental factors • Life circumstances and problems • Personal assets and liabilities • Life flow and health • Can be useful for developing community based health promotion programs through identifying assets and liabilities.
2. Health Behavior Frameworks for Health Promotion • Health behavior theories are relevant and can be useful tools in occupational therapy health promotion • Explanatory Theory • Change Theory
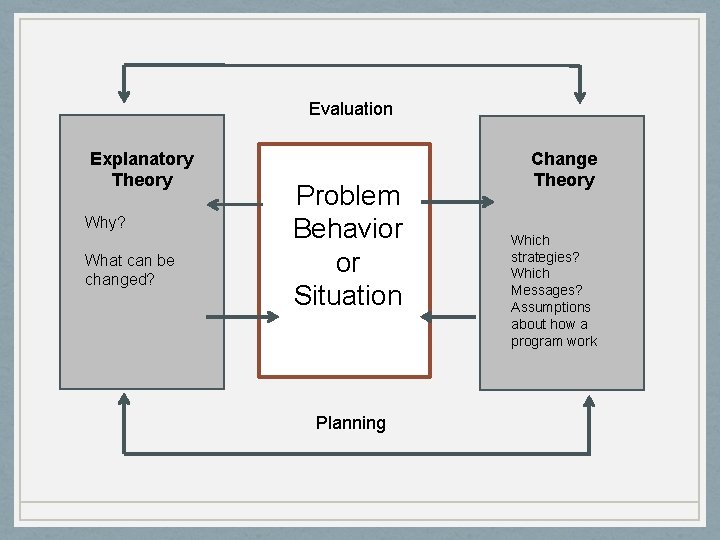
Evaluation Explanatory Theory Why? What can be changed? Problem Behavior or Situation Planning Change Theory Which strategies? Which Messages? Assumptions about how a program work
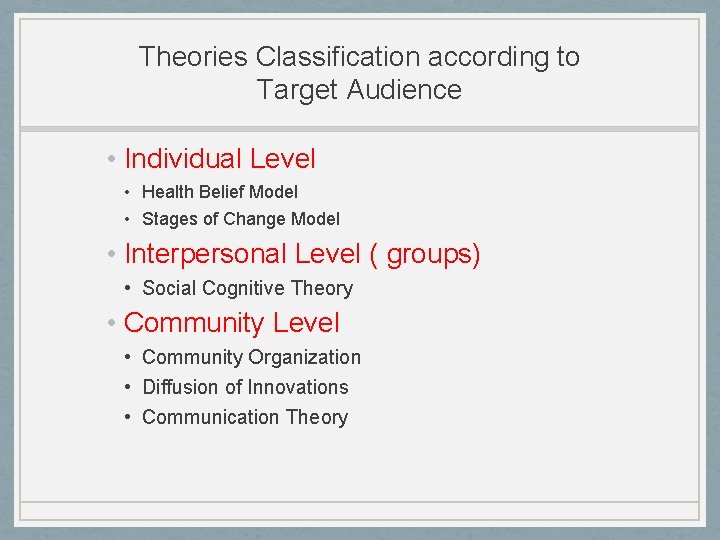
Theories Classification according to Target Audience • Individual Level • Health Belief Model • Stages of Change Model • Interpersonal Level ( groups) • Social Cognitive Theory • Community Level • Community Organization • Diffusion of Innovations • Communication Theory
Health Belief Model • The individual’s perceptions of self and the environment determine health behavior, not the environment. • Describes the relationships between person’s beliefs about health and his/her health specific behaviors.

Beliefs that Mediate Health Behavior Perceived Susceptibility Individual impression of their risk of contracting a disease or illness Once health condition exists perceived susceptibility includes re-susceptibility Perceived Severity Conviction Re: the degree of seriousness of a given health problem Perceived Benefits Person’s beliefs RE: availability and effectiveness of a variety of possible actions in reducing the threat of illness Perceived Barriers Costs of negative aspects associated with engaging n specific health behaviors: Fear of pain, inconvenience of seeking care expense.
Diffusion of Innovations Theory • Idea, practice, or object that is perceived as new by an individual or other unit of adoption. • The perception of newness characterizes innovation. • Model helpful when developing health promotion strategies and programs
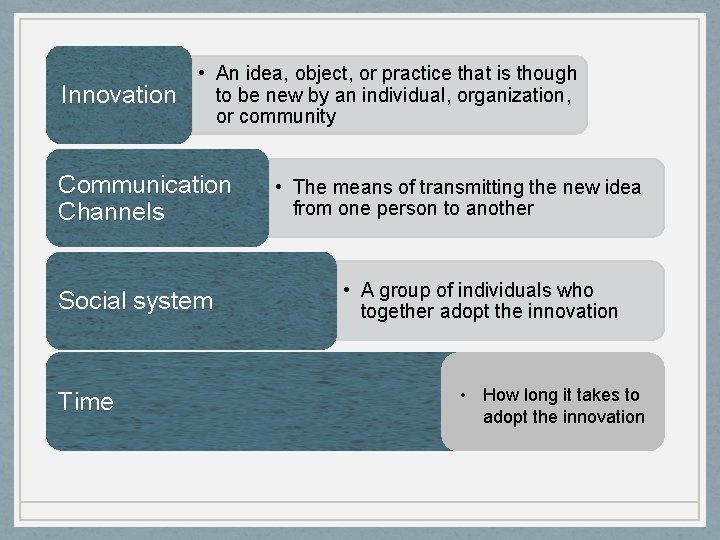
Innovation • An idea, object, or practice that is though to be new by an individual, organization, or community Communication Channels Social system Time • The means of transmitting the new idea from one person to another • A group of individuals who together adopt the innovation • How long it takes to adopt the innovation
PRECEDE-PROCEED MODEL • Intended to provide structure and organization to health education program planning and evaluation. May be used as a planning model, not theory to guide research. • May assist OT in addressing a community health concern. • Elements of Model p. 59, Scaffa, Reitz, & Pizzi (2010).
Social Ecological Model of Health • Proposes that human behavior is influenced by intrapersonal physical environment and sociocultural factors • Model focuses on environmental causes of behavior and environmental interventions for health promotion at different levels Health Promotive Environments • Enhance the physical, mental, emotional and social wellbeing of individuals, families and communities • Environmental influences on health behavior can occur on small or large scale across life domains and life situation
How do Physical and Social Environments Impact Health? • The Environment can: • Transmit disease • Be a stressor (noise, economic climate, isolation) • Be a source of danger: violence, pollution natural disaster, crime • Be an enabler of health behavior: Cultural practices that promote health, health education • Provide health resources: clean water, clean air, sanitation, health insurance.
Social Ecological Model of Health and Occupational Therapy • Obesity prevention • Physical activity • Violence Prevention • Substance Abuse • Stress Reduction
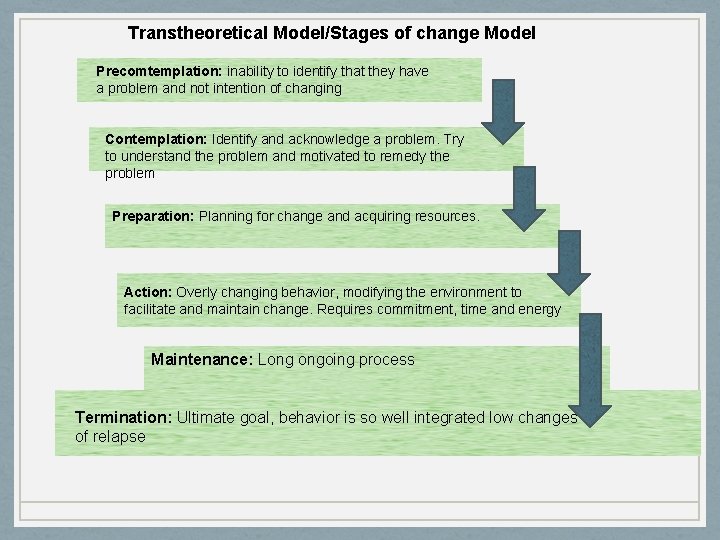
Transtheoretical Model/Stages of change Model Precomtemplation: inability to identify that they have a problem and not intention of changing Contemplation: Identify and acknowledge a problem. Try to understand the problem and motivated to remedy the problem Preparation: Planning for change and acquiring resources. Action: Overly changing behavior, modifying the environment to facilitate and maintain change. Requires commitment, time and energy Maintenance: Long ongoing process Termination: Ultimate goal, behavior is so well integrated low changes of relapse
Healthy People (DHHS) Health Promotion and Disease Prevention Objectives • Increase the quality, as well as the number of years of healthy life. • Emphasize health status (full range of functional capacities across the life span). • Satisfying relationships and the ability to work and play. • To eliminate health disparities. Everyone is treated fairly and have the same opportunities to participate in societal activities. • AOTA Handout: OT in the promotion of health and the prevention of disease and disability.
3. Public Health and Health Promotion • Traditional Public Health focused on the health state of populations and communities, where as traditional medicine and allied health professions focused on the individual or family. • The US Public Health system has also been the representative of the US in the World Health Organization (WHO).
Early Public Health • Focus was on identification of causes of disease, elimination of disease, sanitation and hygiene, and mental health treatment on group, population, and community scales. • With the incorporation of research methods, tracking data, and development of medications, Public Health services experienced a lot of success in the war against illness and disease.
New Public Health • Starting in the 20 th century, the focus has shifted to • • Health Education Maternal & Child Health Previously undetected impairments Prevention strategies to promote health and wellbeing of individuals and communities. • Advocate for access to healthcare • Established the Centers for Disease Control (CDC)
General Goals of Public Health in the 21 st Century • Prevent epidemics and minimize the spread of disease • Protect against environmental hazards • Prevent injuries • Promote health behaviors • Respond to disasters and assist communities in recovery • Assure access to health services • Enhance quality of life
The Relationship of Public Health to Occupational Therapy • Health Promotion • Wellness • Language of OTPF aligns with WHO’s International Classification of Functioning, Disability, and Health (ICF) • Community Health • Prevention
(cont’d) • Public Health has produced much information on health promotion, including program development, data and statistics, and community resources that are beneficial to the practice of occupational therapy. • Leading Health Indicators/Determinants of Health • Levels of Prevention • Follows on next slides • Evidence based practice • Preliminary information to support funding requests • Interdisciplinary findings
Three Levels of Prevention • Primary • Secondary • Tertiary
Primary Prevention • Identify and reduce risk factors. • Educates or health promotion strategies designed to help people to avoid the onset and reduce the incidence of unhealthy conditions, disease or injury. • Examples: • Musculoskeletal injury prevention and management programs • Anger management and conflict resolution training for youth, parents and teachers • Parenting skills for adolescent mothers • Fall prevention for community dwelling seniors.
Secondary Prevention • Early detection and intervention after disease has occurred. • Designed to prevent or disrupt disabling process. • Examples: • Education and training on eating, habits, activity levels. • Education and Training on stress management and coping skills • Osteoporosis management classes.
Tertiary Prevention • Treatment and services designed to arrest the progression of condition & prevent further disability • Independent living skills training for people who have mental illness, cognitive impairments • Groups for elders with dementia to improve quality life • Stroke support groups
The End
- Slides: 35