Module 1 LEPROSY The Disease WHAT IS LEPROSY









- Slides: 66
Module 1: LEPROSY: The Disease
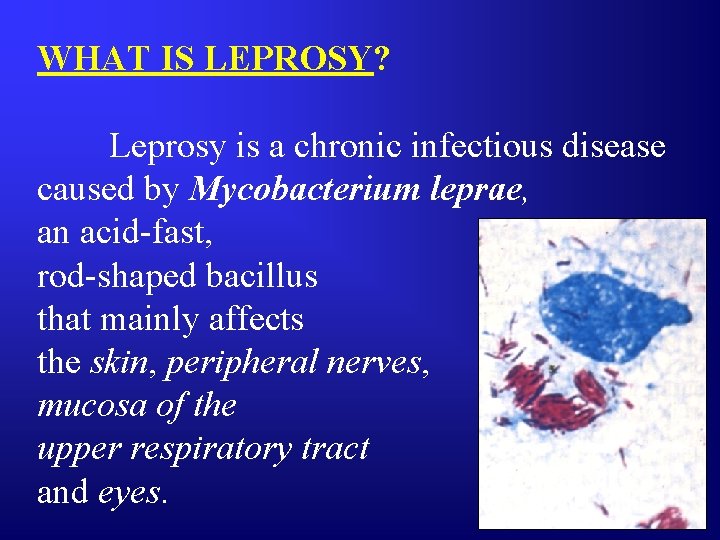
WHAT IS LEPROSY? Leprosy is a chronic infectious disease caused by Mycobacterium leprae, an acid-fast, rod-shaped bacillus that mainly affects the skin, peripheral nerves, mucosa of the upper respiratory tract and eyes.

It has a very long incubation period or latency which ranges from 3 to 15 years.
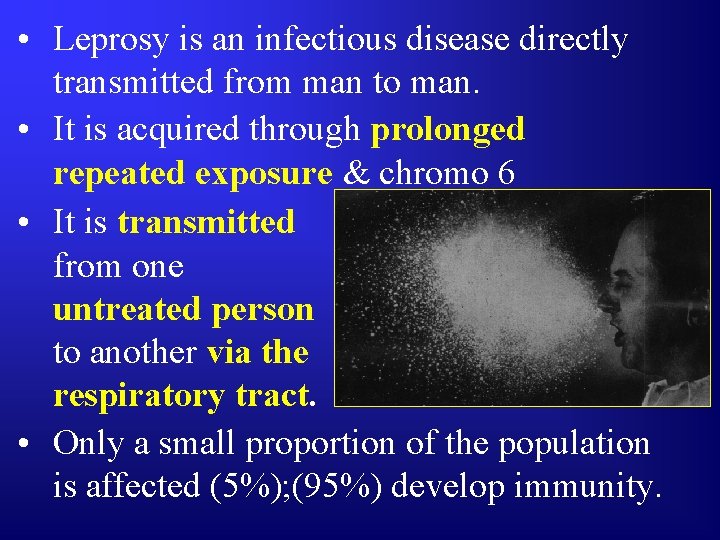
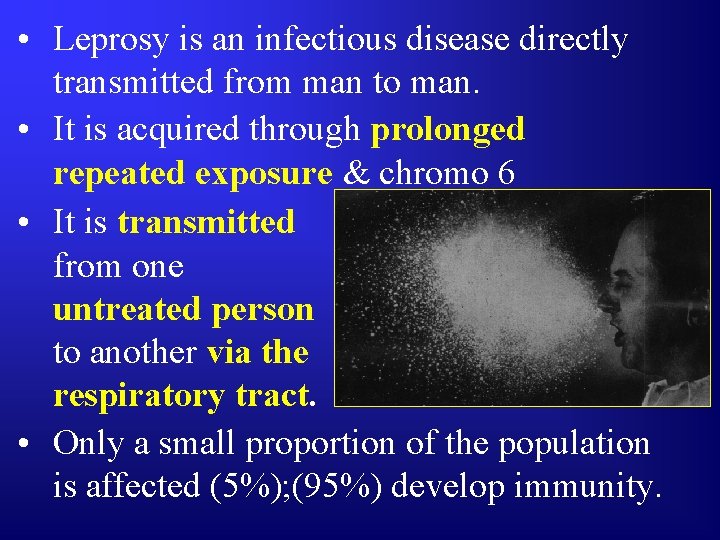
• Leprosy is an infectious disease directly transmitted from man to man. • It is acquired through prolonged repeated exposure & chromo 6 • It is transmitted from one untreated person to another via the respiratory tract. • Only a small proportion of the population is affected (5%); (95%) develop immunity.
DIAGNOSIS OF LEPROSY: Diagnosis of leprosy is mainly based on clinical signs and symptoms. Only in rare instances is there a need to use laboratory and other investigations to confirm a diagnosis of leprosy.
An individual should be regarded as having leprosy if he exhibits the following cardinal signs: q Hypo-pigmented or reddish skin lesion(s) with definite sensory loss; q Peripheral nerve damage, as demonstrated by loss of sensation and muscle weakness in the hands, feet and/ or face; q Positive skin smear.
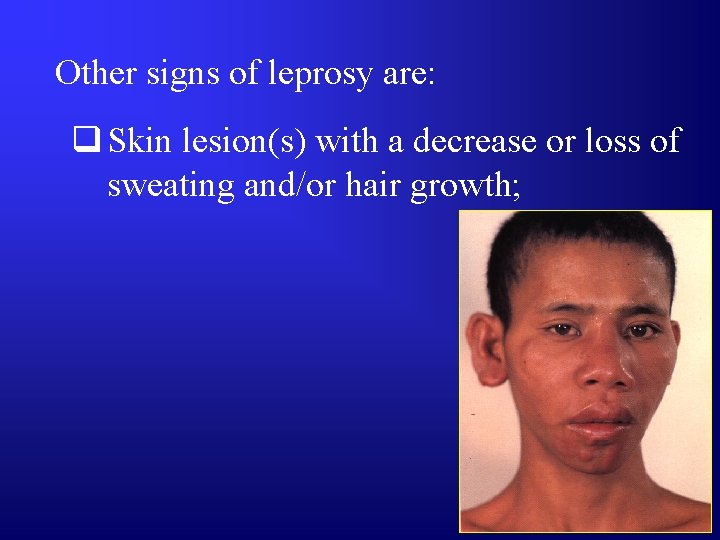
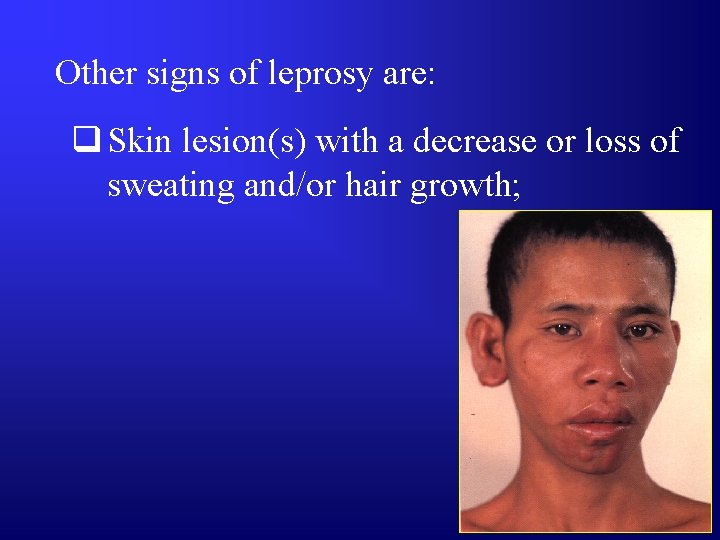
Other signs of leprosy are: q Skin lesion(s) with a decrease or loss of sweating and/or hair growth;
Other signs of leprosy are: q Skin lesion(s) with a decrease or loss of sweating and/or hair growth; q Constant redness in the eyes from irritation and dryness;
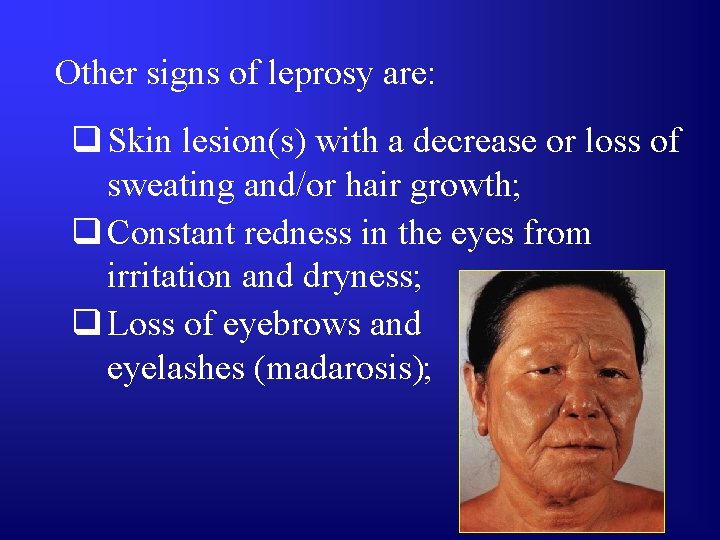
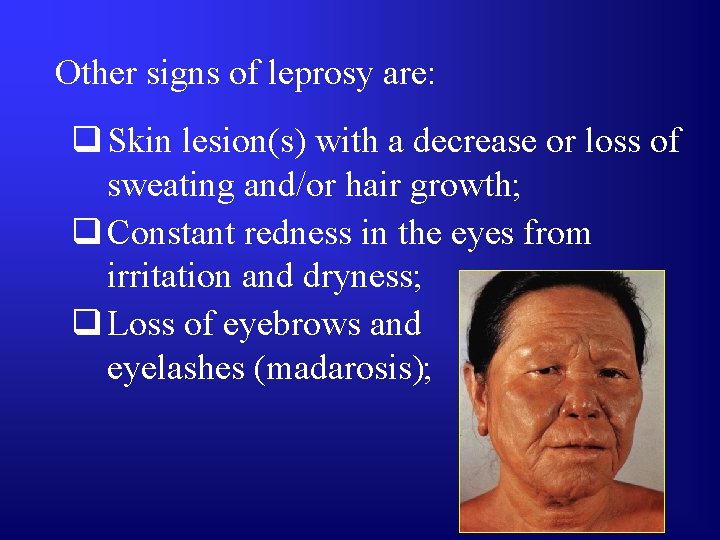
Other signs of leprosy are: q Skin lesion(s) with a decrease or loss of sweating and/or hair growth; q Constant redness in the eyes from irritation and dryness; q Loss of eyebrows and eyelashes (madarosis);
Other signs of leprosy are: q Skin lesion(s) with a decrease or loss of sweating and/or hair growth; q Constant redness in the eyes from irritation and dryness; q Loss of eyebrows and eyelashes (madarosis);
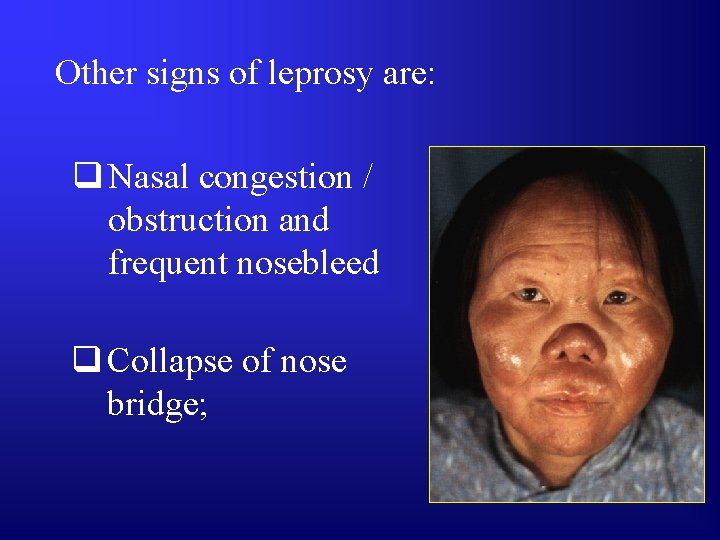
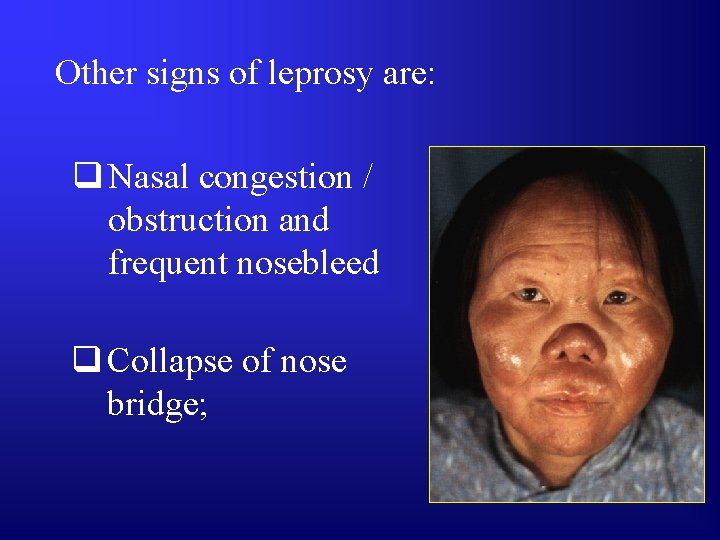
Other signs of leprosy are: q Nasal congestion / obstruction and frequent nosebleed q Collapse of nose bridge;
Other signs of leprosy are: q Enlargement of the breast in males (gynecomastia);
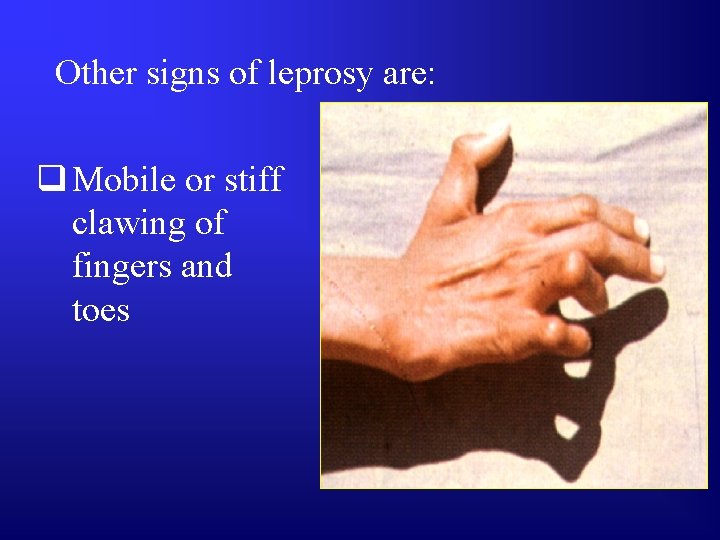
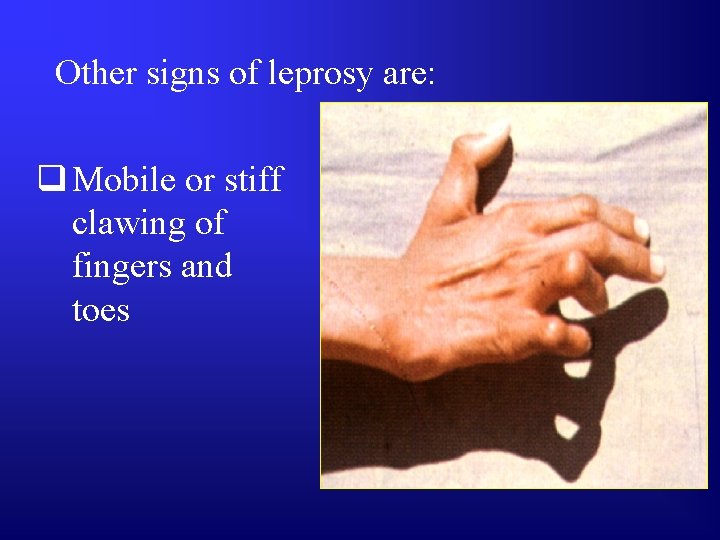
Other signs of leprosy are: q Mobile or stiff clawing of fingers and toes

Other signs of leprosy are: q Chronic ulcers, usually in the sole of the foot, palm of the hands and fingers.
Diagnosis of leprosy is mainly based on clinical signs and symptoms. i

The development of complications can be effectively prevented through early detection, correct diagnosis and effective treatment. i
PATIENT’S HISTORY: The leprosy case history should have the following information: 1. The nature of the first lesion or symptom and its progress. This is because the skin lesion usually develops slowly over several months and is not troublesome.
Ask: • When did the patient first notice the lesion? • What was its appearance? • How did it feel? Was it painful? Itchy? ?
PATIENT’S HISTORY: 2. Past Treatment. ? Ask: • What did the patient do when he first noticed the lesion? • Did he apply any drug(s)? • What was the effect of this/these drug(s)?
PATIENT’S HISTORY: 3. Other Illnesses. Pay attention to contra-indications to MDT drugs; or any other illness requiring special attention and/or referral.
Ask: • Does the patient have a history of liver disease? • Allergy to drugs? • If yes, what drugs? ?
PATIENT’S HISTORY: 4. Contact with Persons With Leprosy (PWLs) This information will help determine the patient’s susceptibility to the disease.
Ask: • Does/did anyone in the family have leprosy? • Does he have a friend or acquaintance who has/had leprosy? ?
CLASSIFICATION: Leprosy can be classified on the basis of clinical manifestations and skin smear results. The Ridley-Jopling classification has seven (7) types of leprosy:
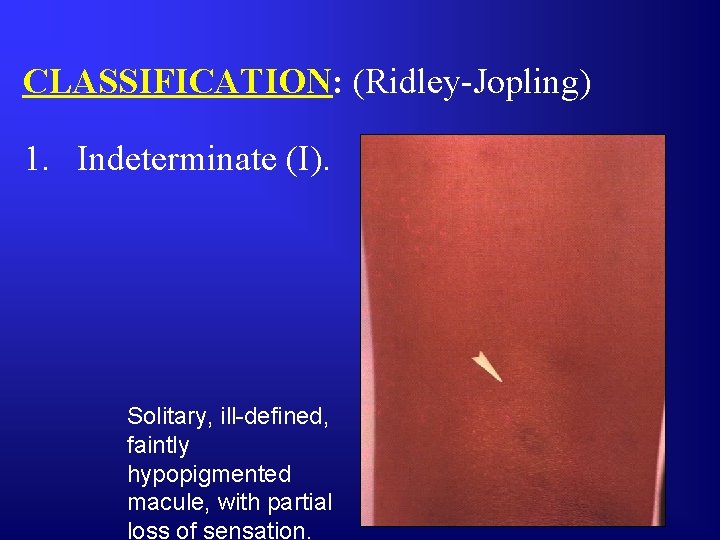
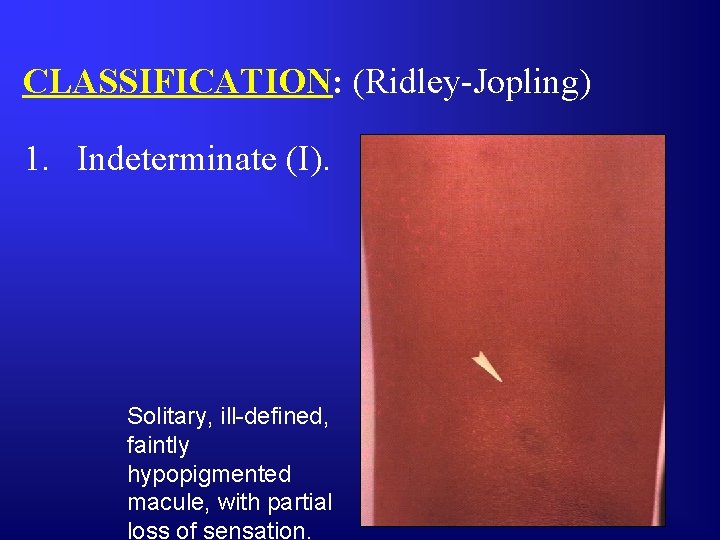
CLASSIFICATION: (Ridley-Jopling) 1. Indeterminate (I). Solitary, ill-defined, faintly hypopigmented macule, with partial loss of sensation.
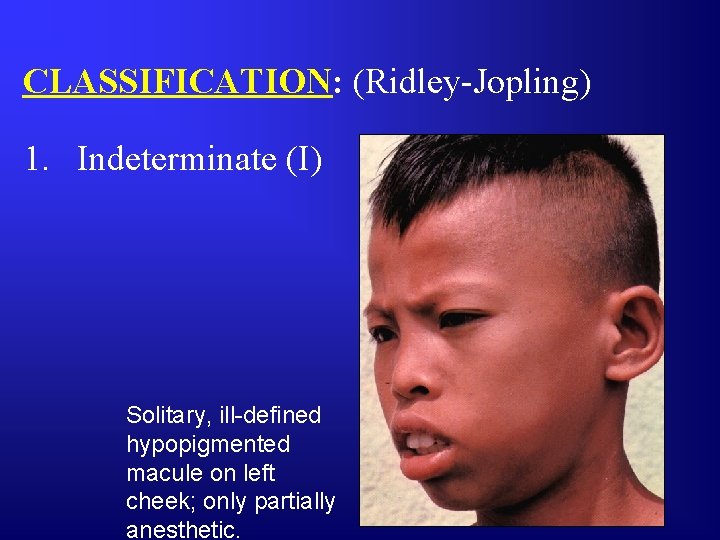
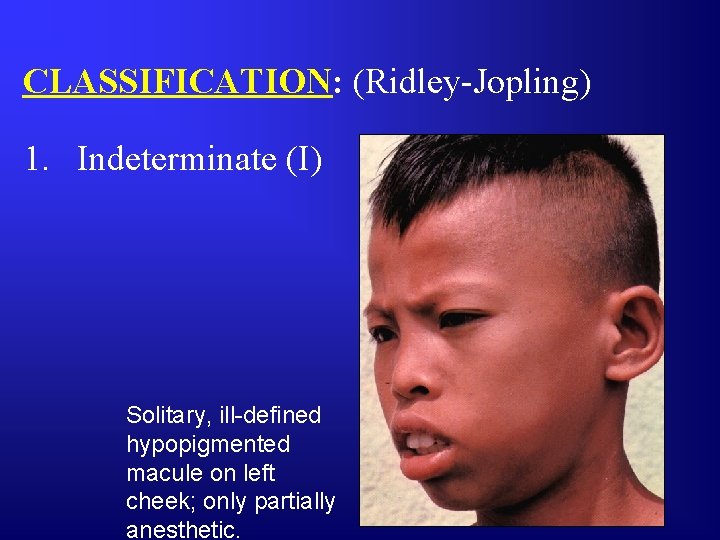
CLASSIFICATION: (Ridley-Jopling) 1. Indeterminate (I) Solitary, ill-defined hypopigmented macule on left cheek; only partially anesthetic.
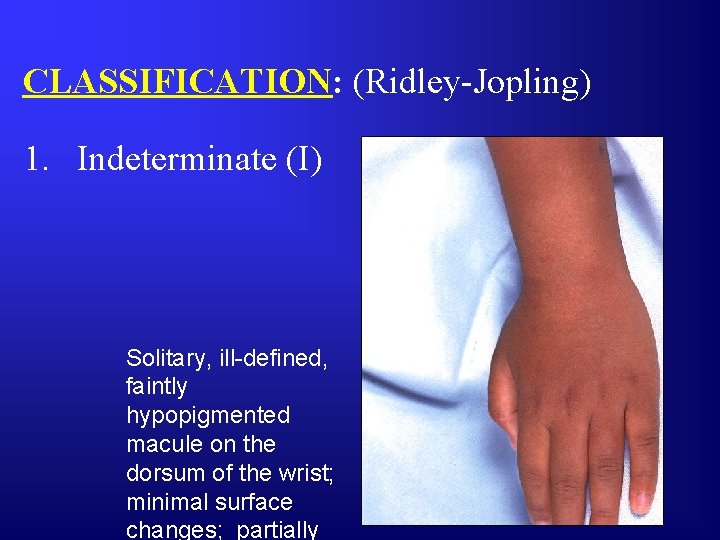
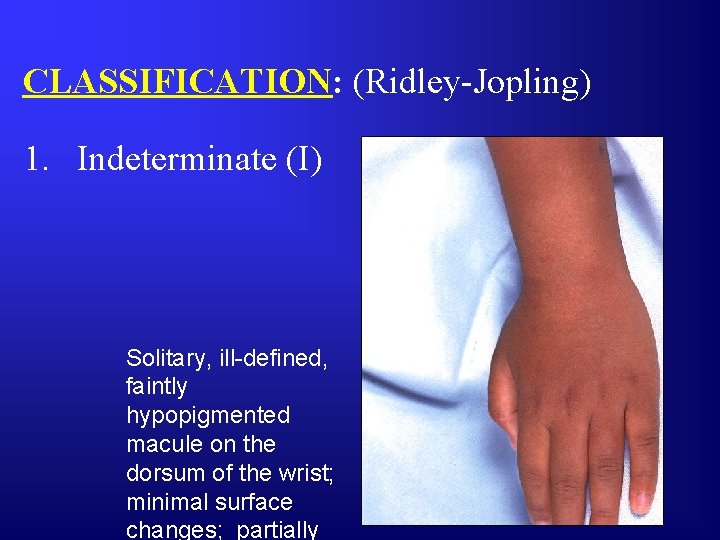
CLASSIFICATION: (Ridley-Jopling) 1. Indeterminate (I) Solitary, ill-defined, faintly hypopigmented macule on the dorsum of the wrist; minimal surface changes; partially
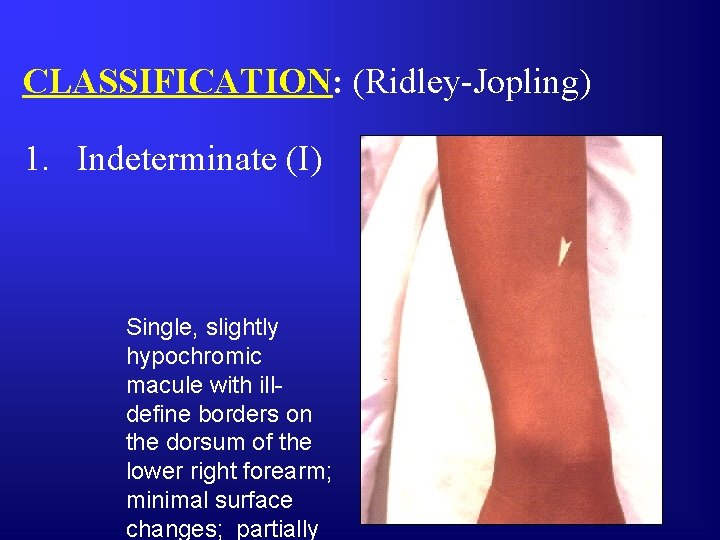
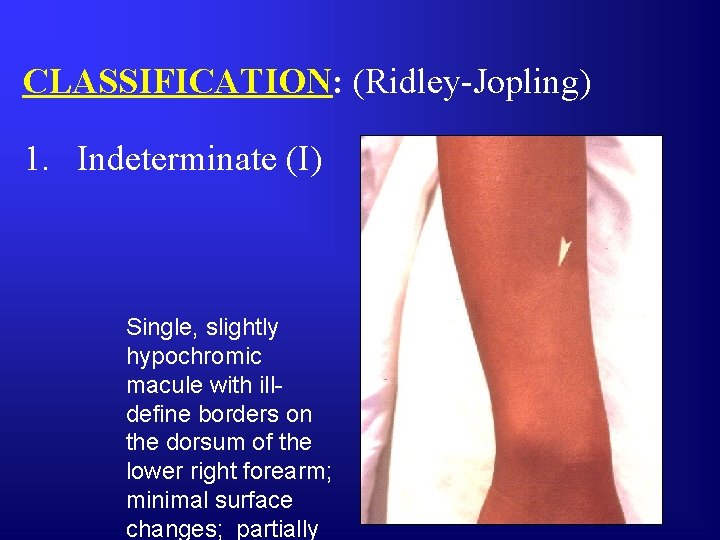
CLASSIFICATION: (Ridley-Jopling) 1. Indeterminate (I) Single, slightly hypochromic macule with illdefine borders on the dorsum of the lower right forearm; minimal surface changes; partially
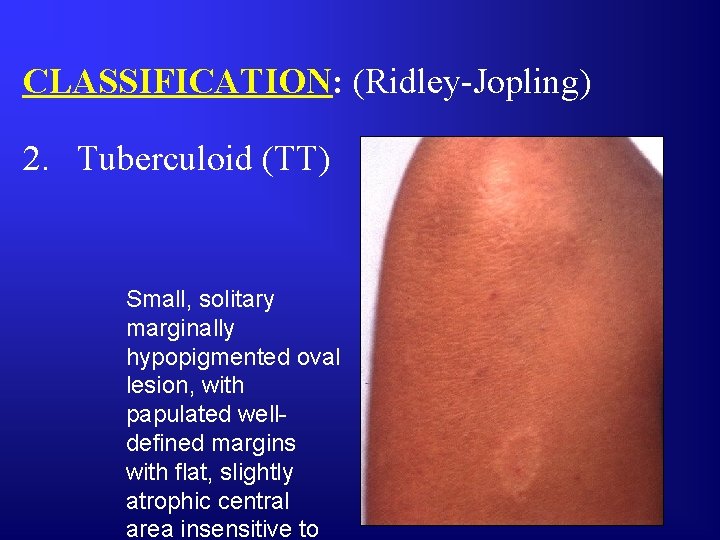
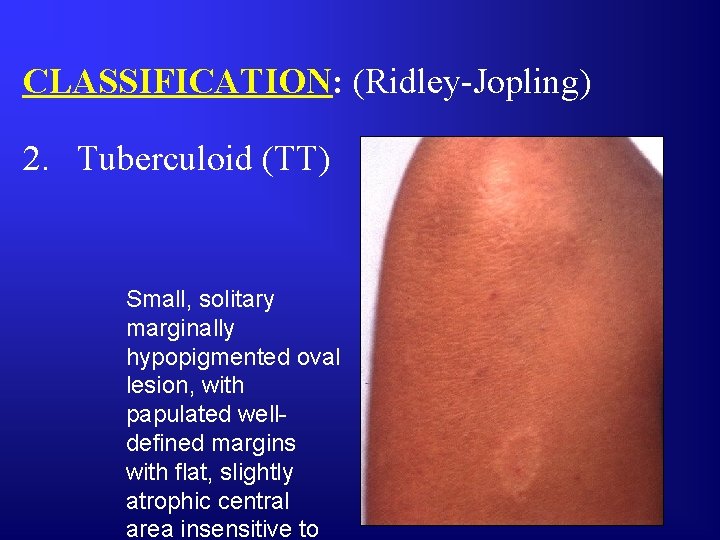
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Small, solitary marginally hypopigmented oval lesion, with papulated welldefined margins with flat, slightly atrophic central area insensitive to
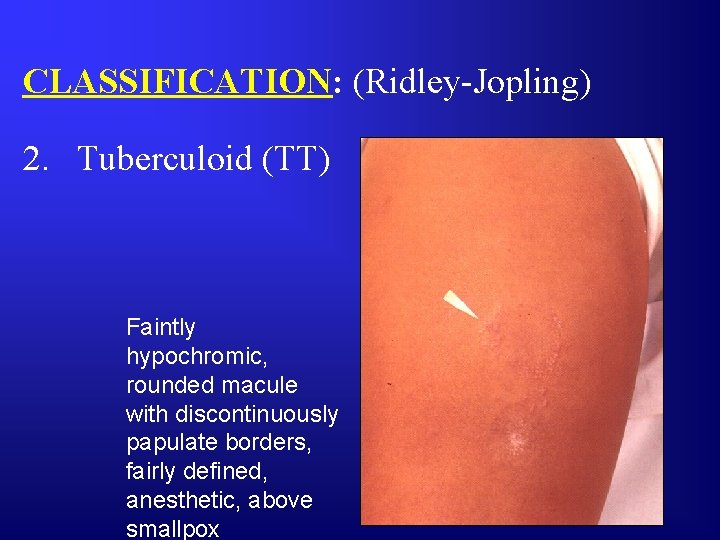
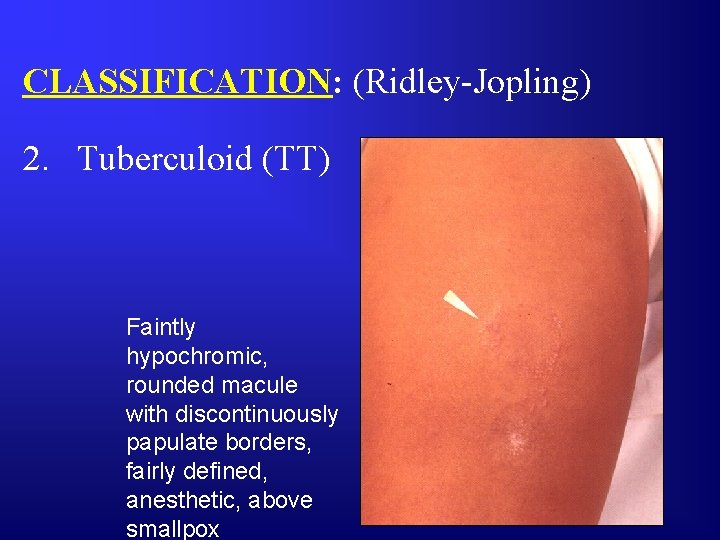
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Faintly hypochromic, rounded macule with discontinuously papulate borders, fairly defined, anesthetic, above smallpox
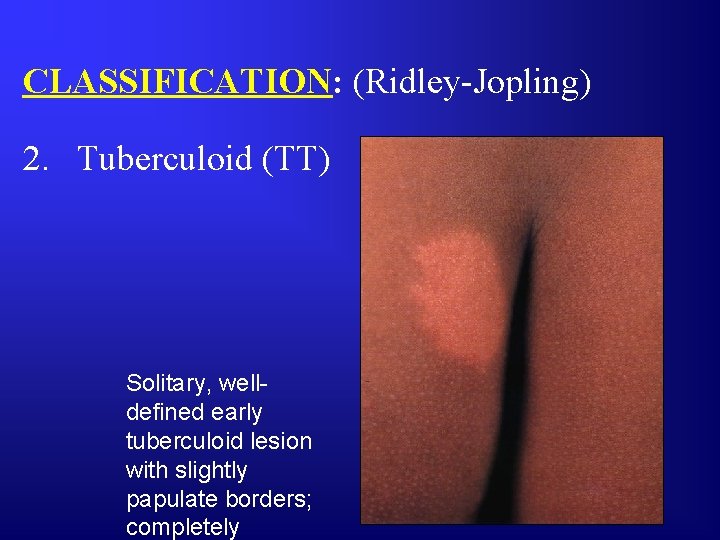
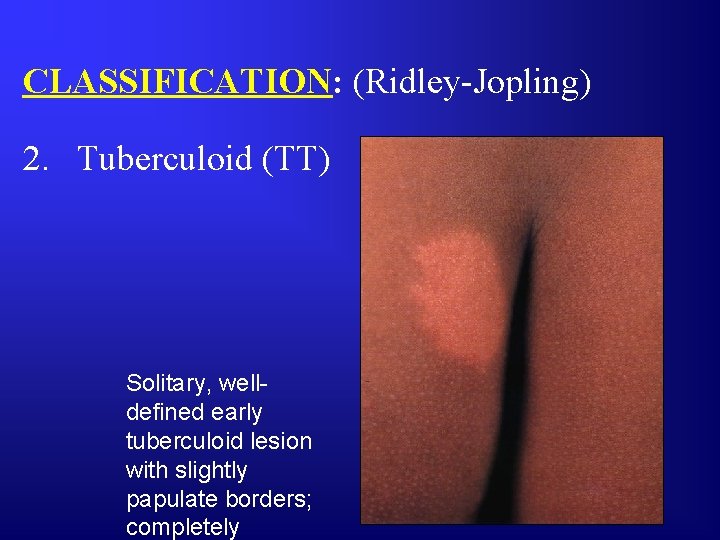
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Solitary, welldefined early tuberculoid lesion with slightly papulate borders; completely
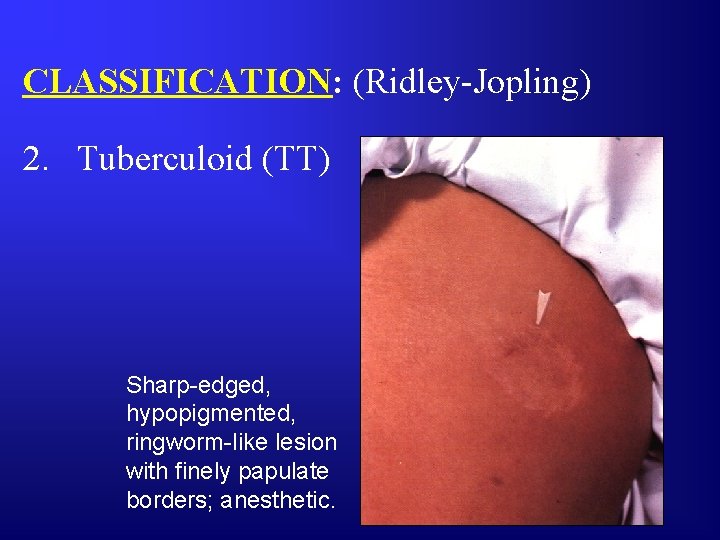
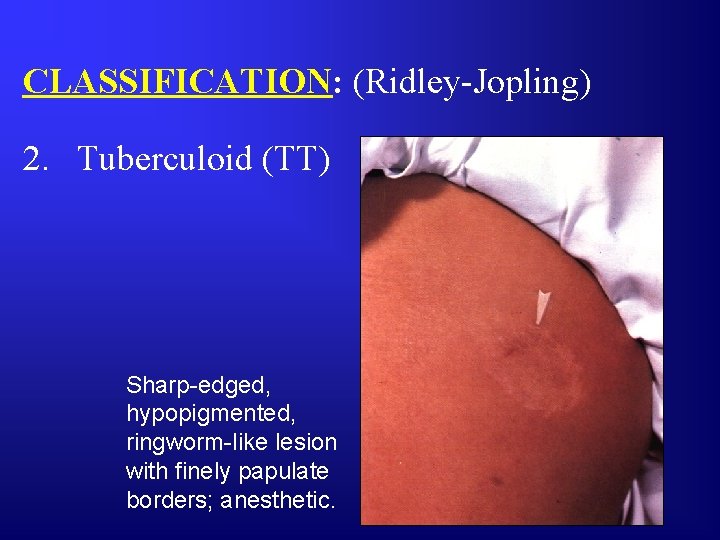
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Sharp-edged, hypopigmented, ringworm-like lesion with finely papulate borders; anesthetic.
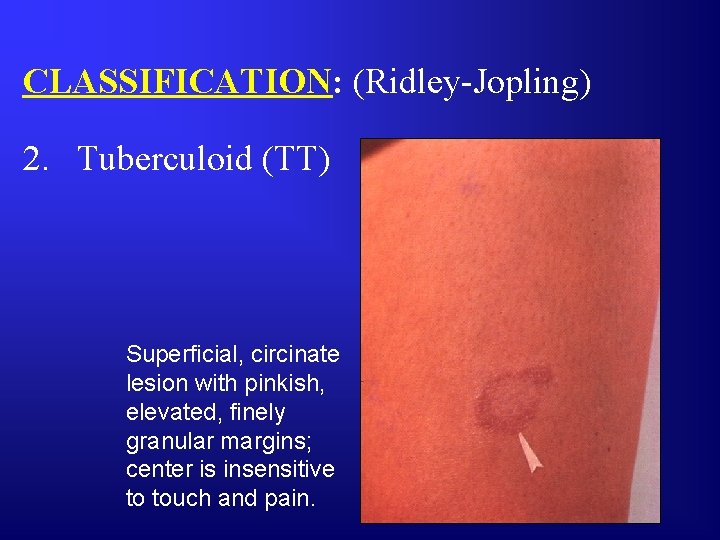
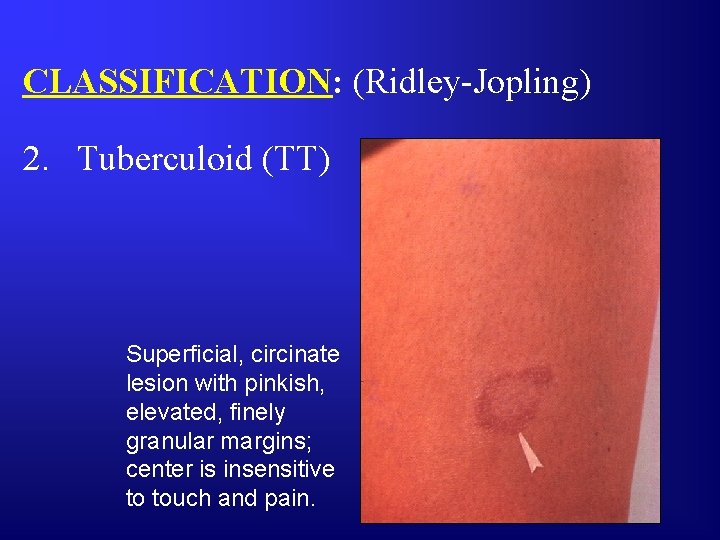
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Superficial, circinate lesion with pinkish, elevated, finely granular margins; center is insensitive to touch and pain.
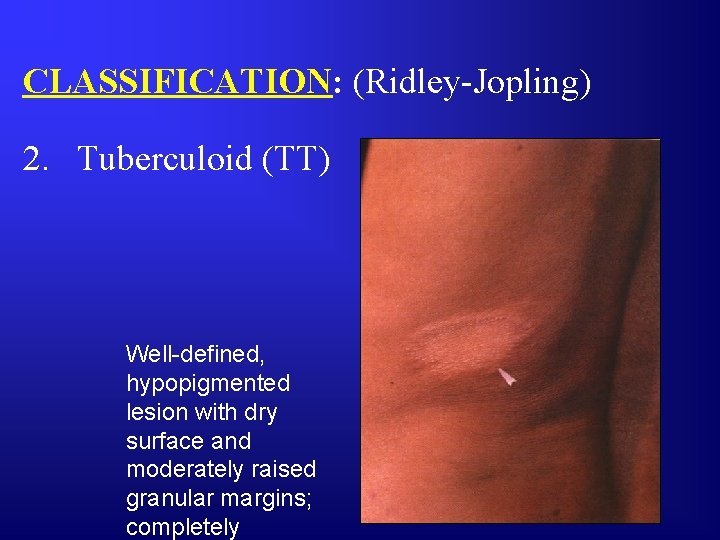
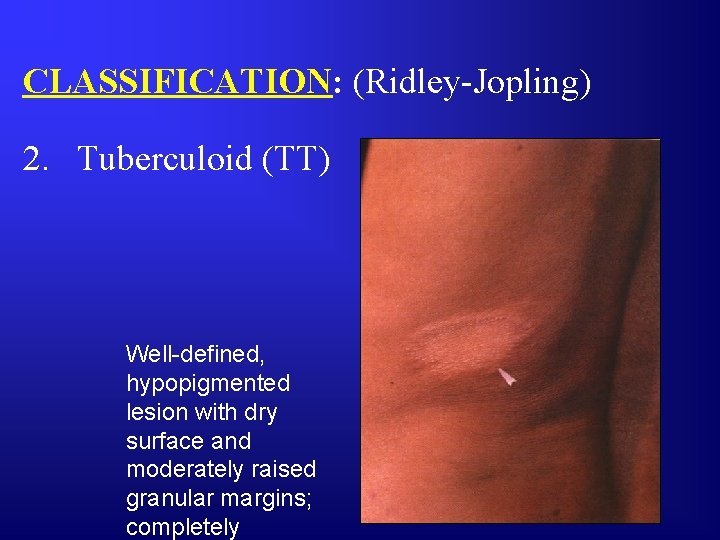
CLASSIFICATION: (Ridley-Jopling) 2. Tuberculoid (TT) Well-defined, hypopigmented lesion with dry surface and moderately raised granular margins; completely
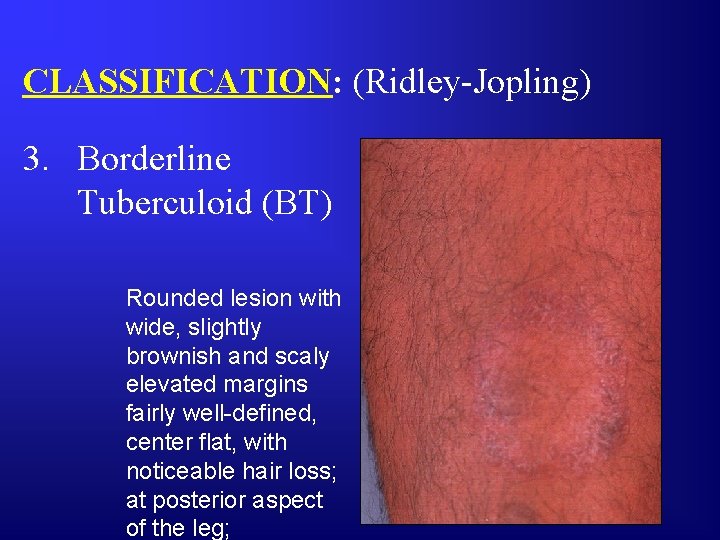
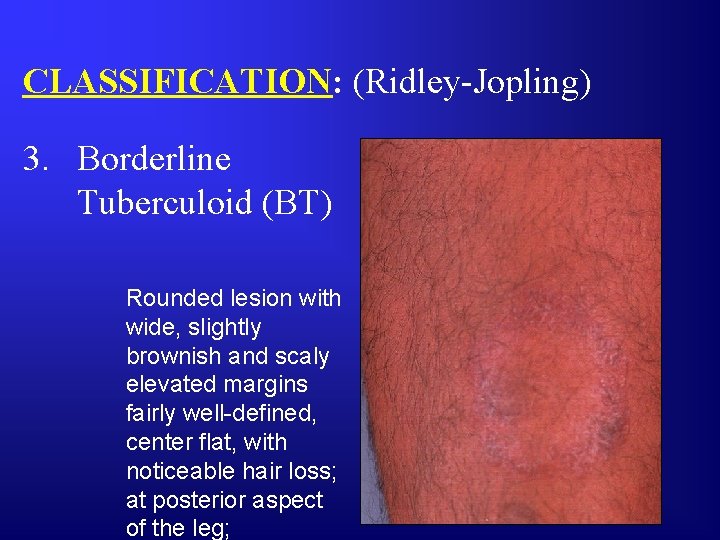
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Rounded lesion with wide, slightly brownish and scaly elevated margins fairly well-defined, center flat, with noticeable hair loss; at posterior aspect of the leg;

CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) One of several sharp-edged, erythematous patches on the patient, with fairly thick granular margins and small satellite lesions;
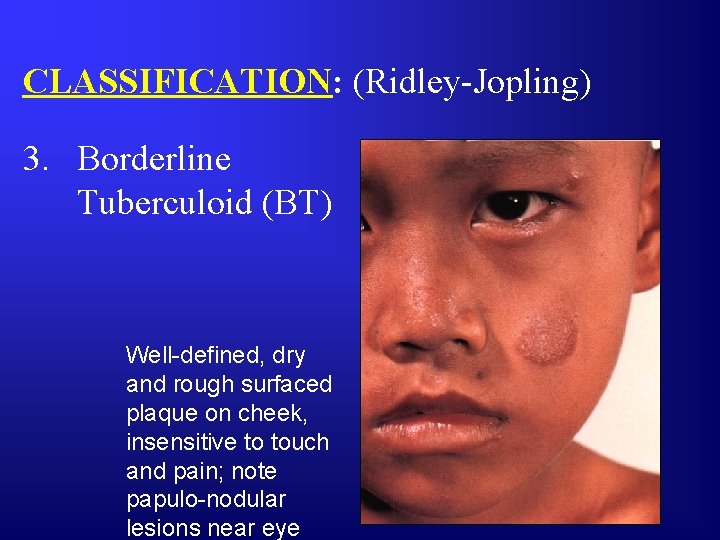
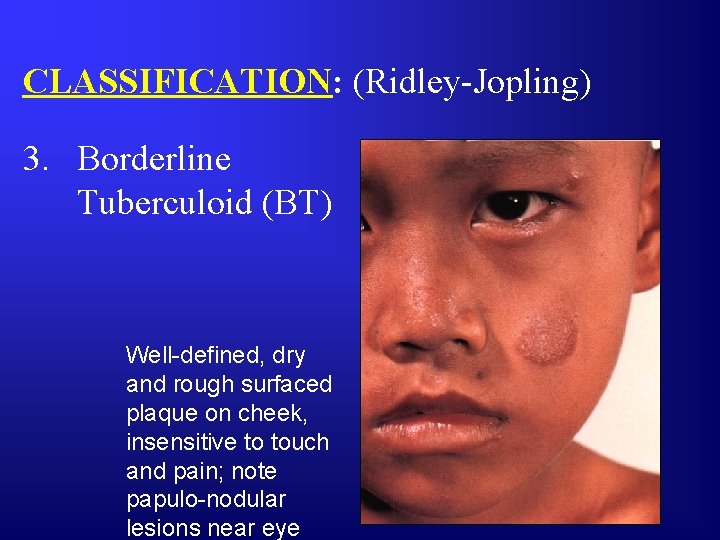
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Well-defined, dry and rough surfaced plaque on cheek, insensitive to touch and pain; note papulo-nodular lesions near eye
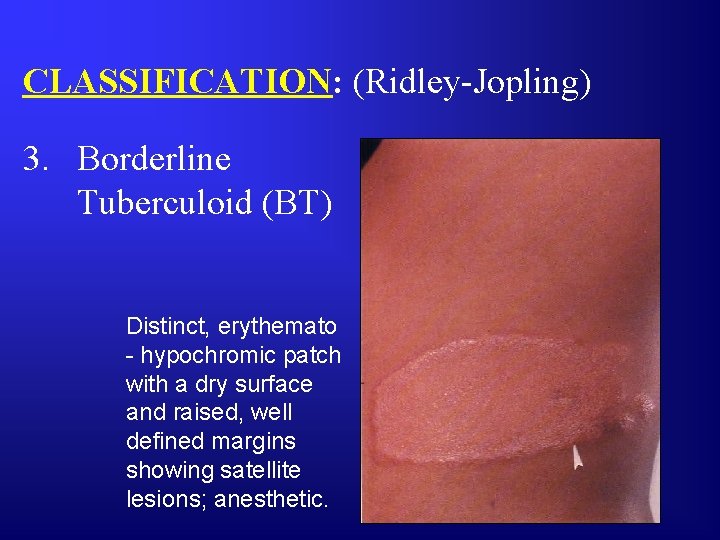
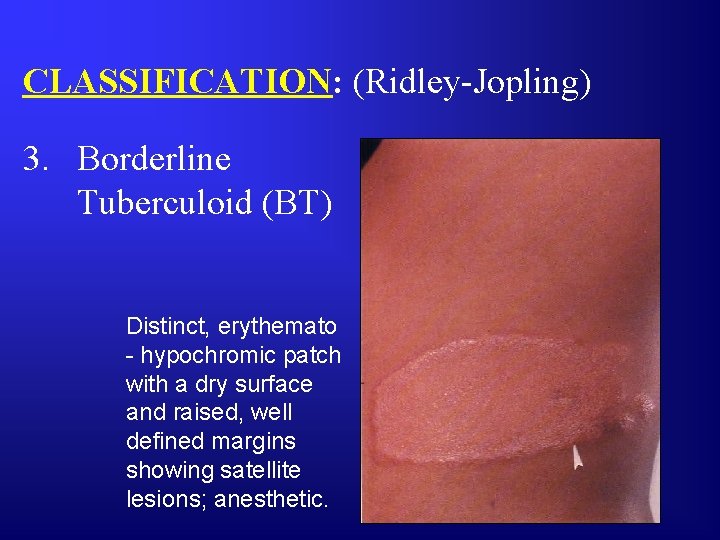
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Distinct, erythemato - hypochromic patch with a dry surface and raised, well defined margins showing satellite lesions; anesthetic.
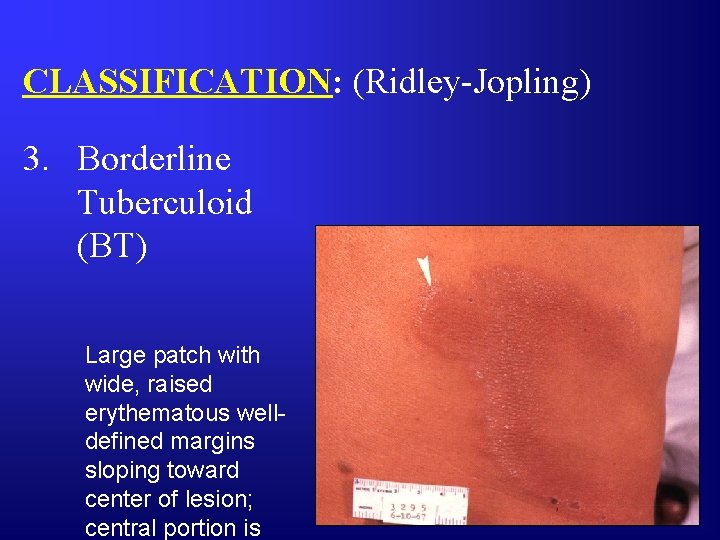
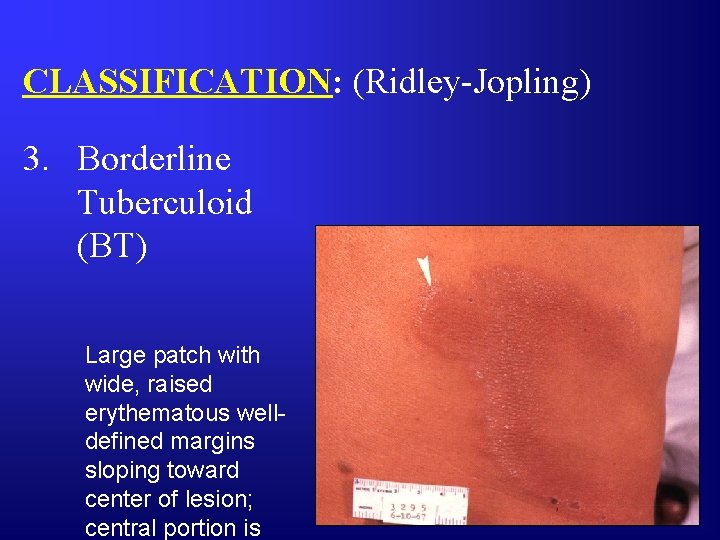
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Large patch with wide, raised erythematous welldefined margins sloping toward center of lesion; central portion is
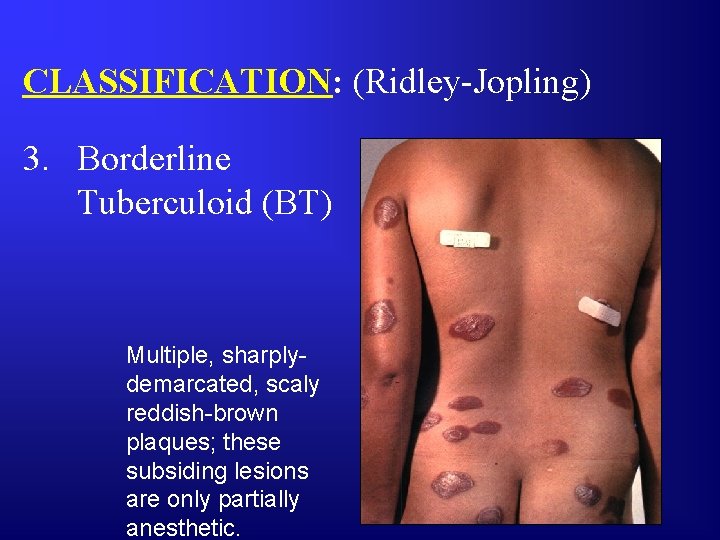
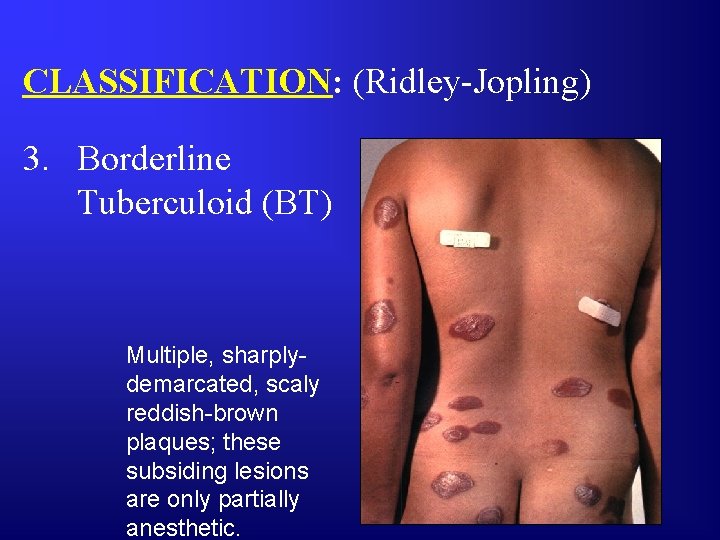
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Multiple, sharplydemarcated, scaly reddish-brown plaques; these subsiding lesions are only partially anesthetic.
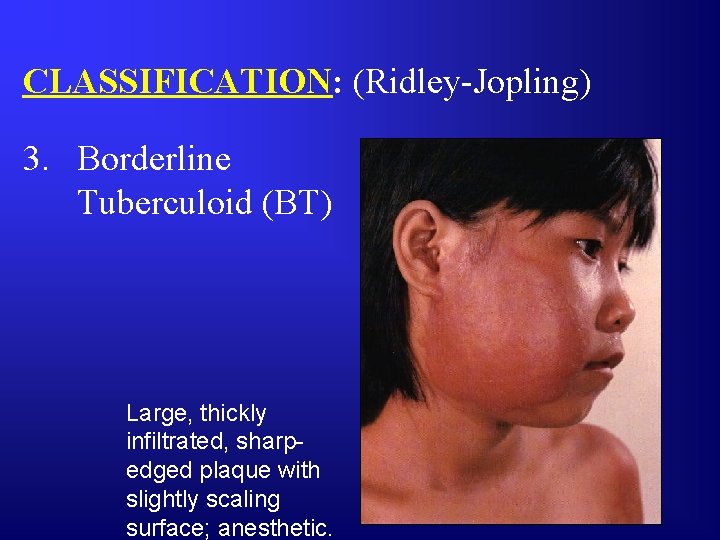
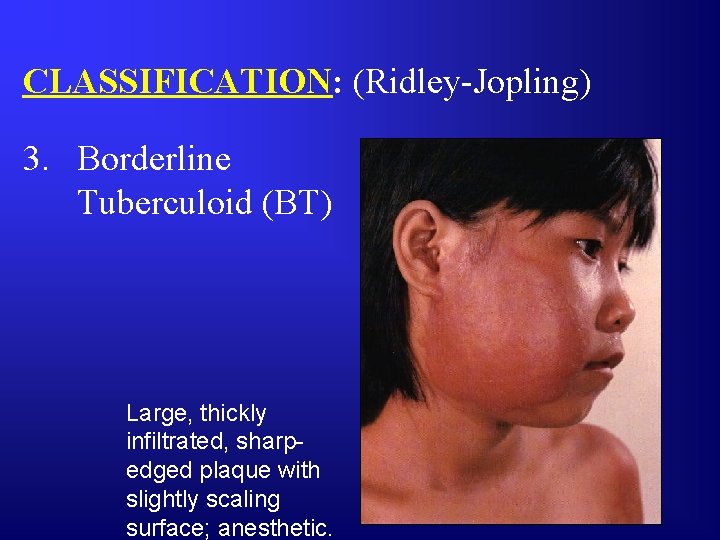
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Large, thickly infiltrated, sharpedged plaque with slightly scaling surface; anesthetic.
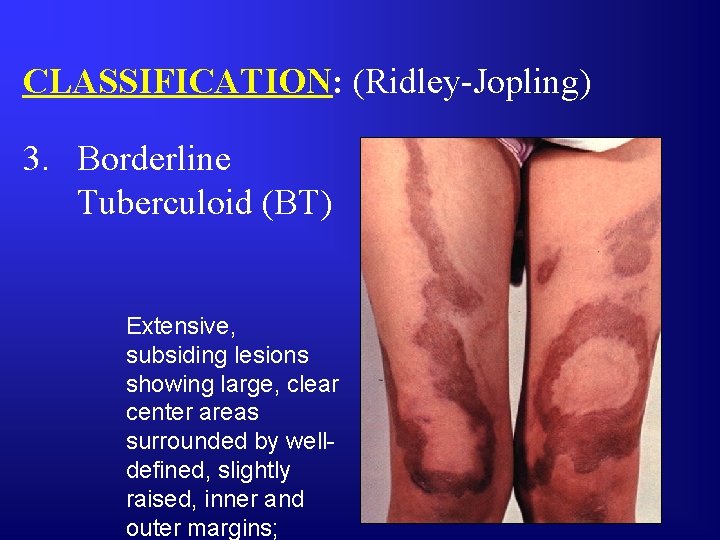
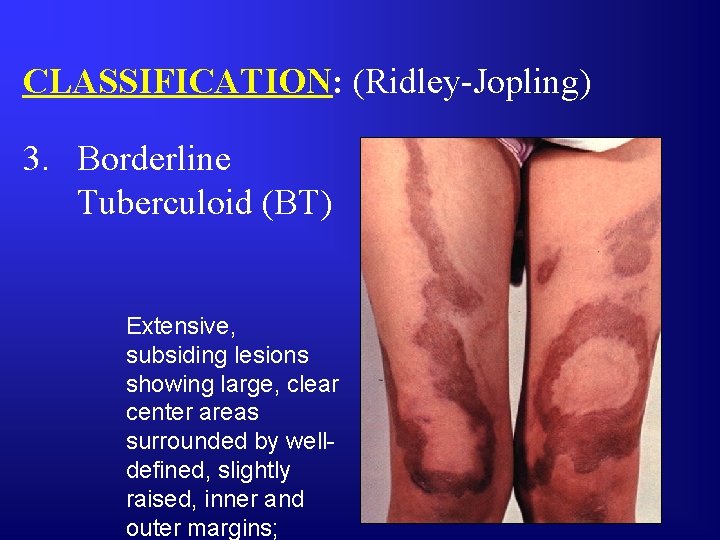
CLASSIFICATION: (Ridley-Jopling) 3. Borderline Tuberculoid (BT) Extensive, subsiding lesions showing large, clear center areas surrounded by welldefined, slightly raised, inner and outer margins;
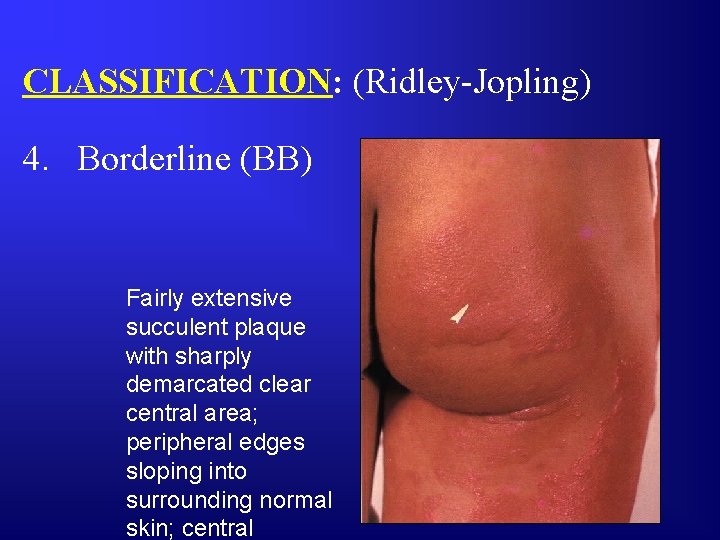
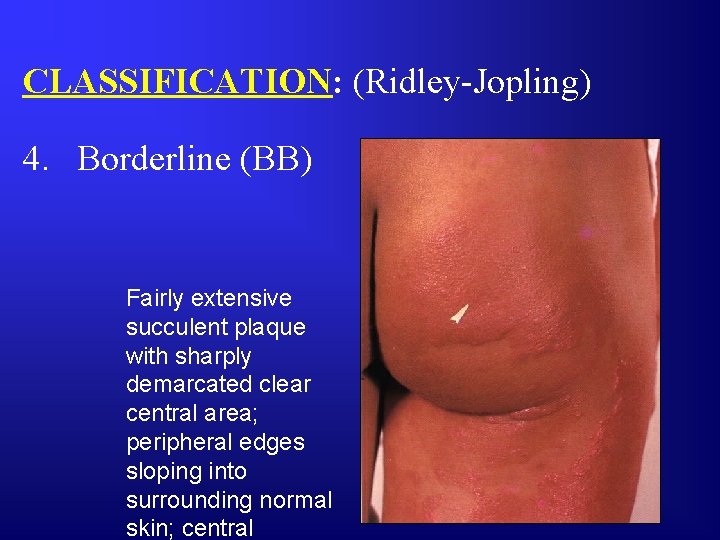
CLASSIFICATION: (Ridley-Jopling) 4. Borderline (BB) Fairly extensive succulent plaque with sharply demarcated clear central area; peripheral edges sloping into surrounding normal skin; central
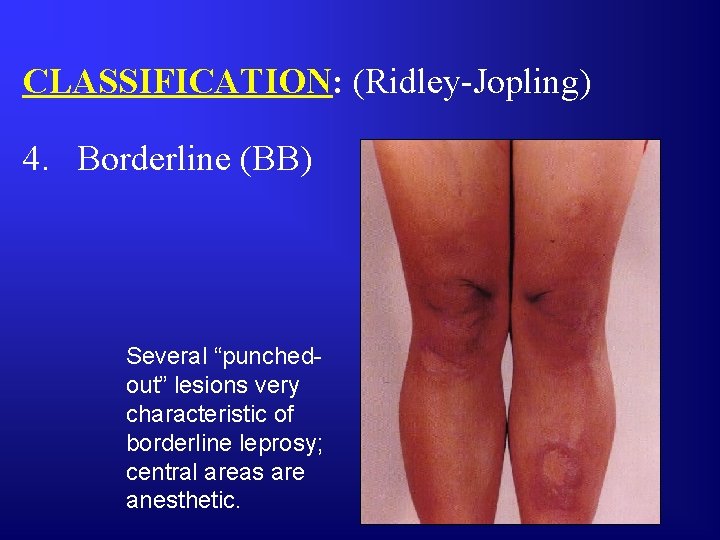
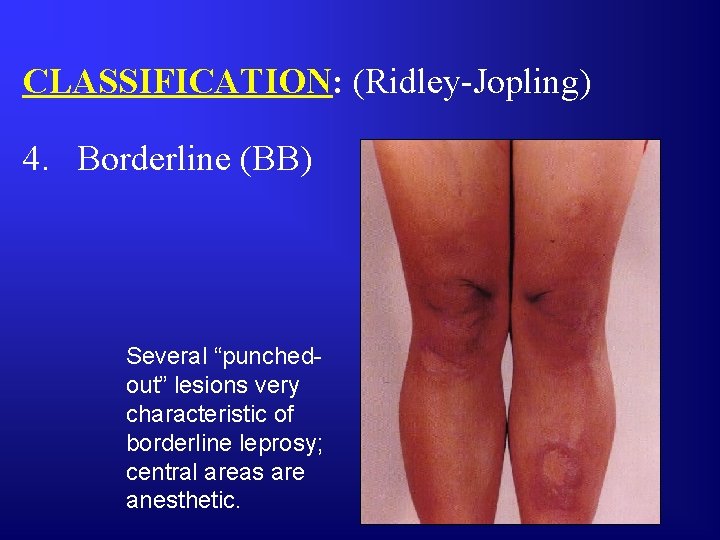
CLASSIFICATION: (Ridley-Jopling) 4. Borderline (BB) Several “punchedout” lesions very characteristic of borderline leprosy; central areas are anesthetic.
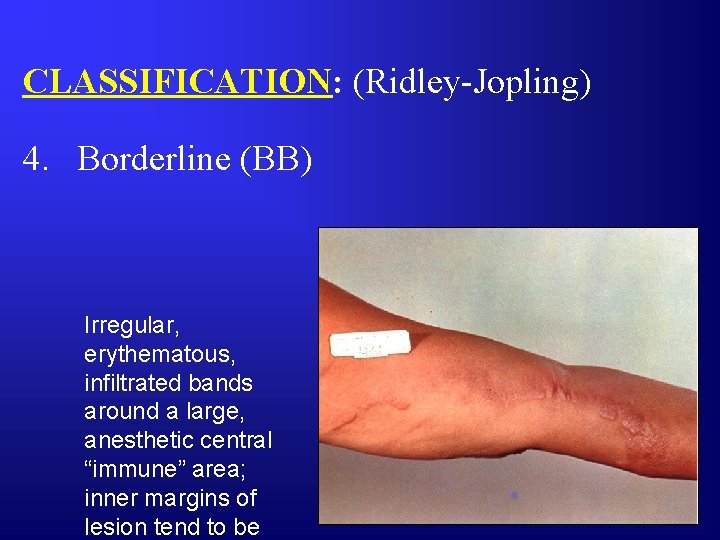
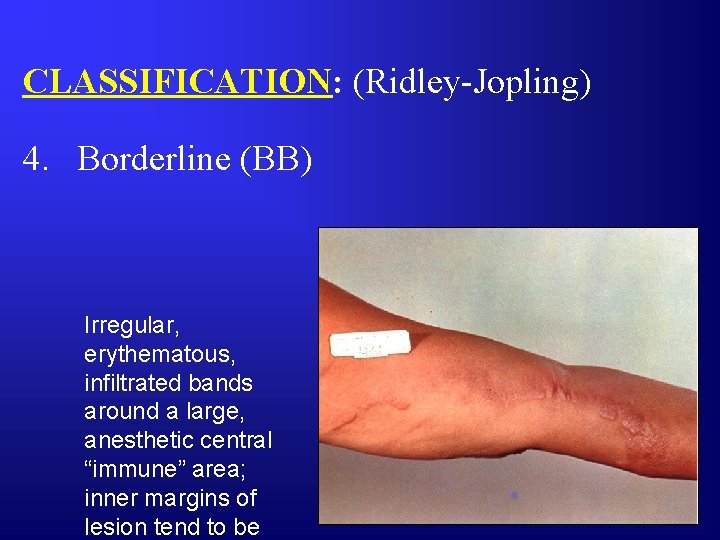
CLASSIFICATION: (Ridley-Jopling) 4. Borderline (BB) Irregular, erythematous, infiltrated bands around a large, anesthetic central “immune” area; inner margins of lesion tend to be
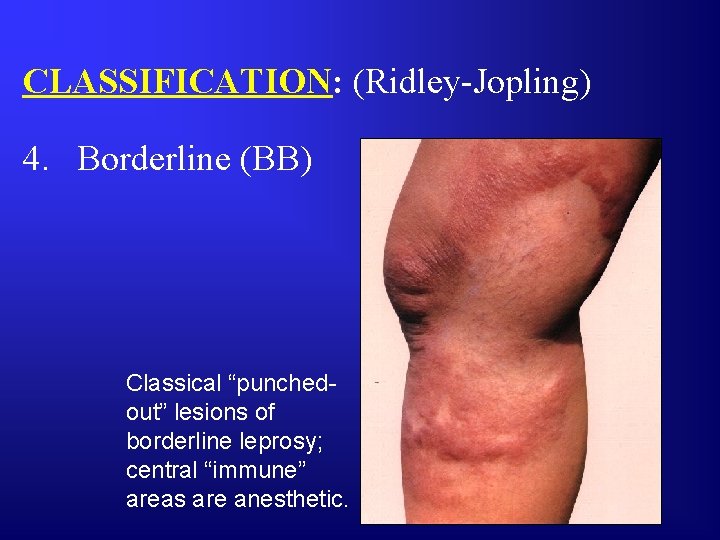
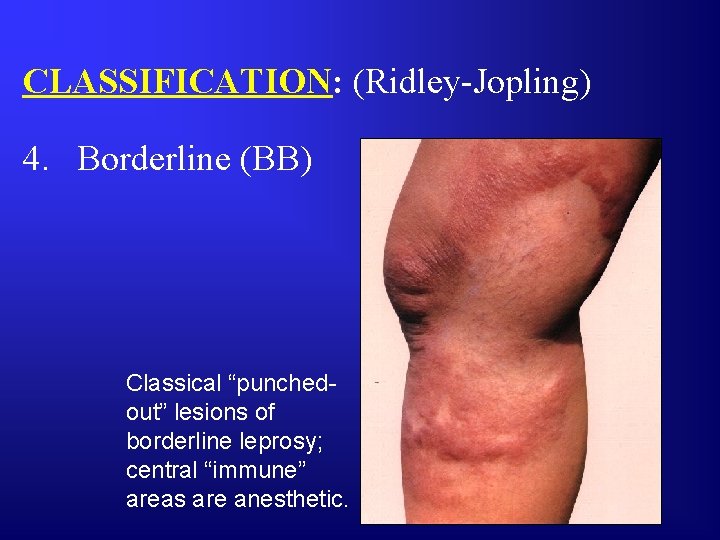
CLASSIFICATION: (Ridley-Jopling) 4. Borderline (BB) Classical “punchedout” lesions of borderline leprosy; central “immune” areas are anesthetic.
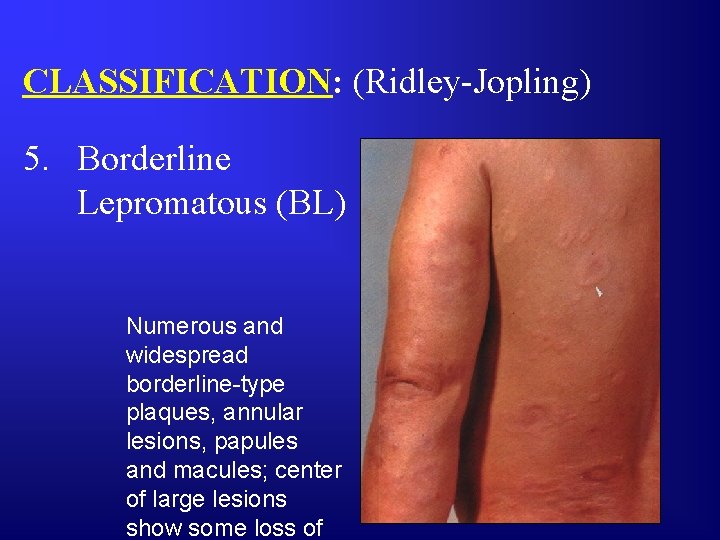
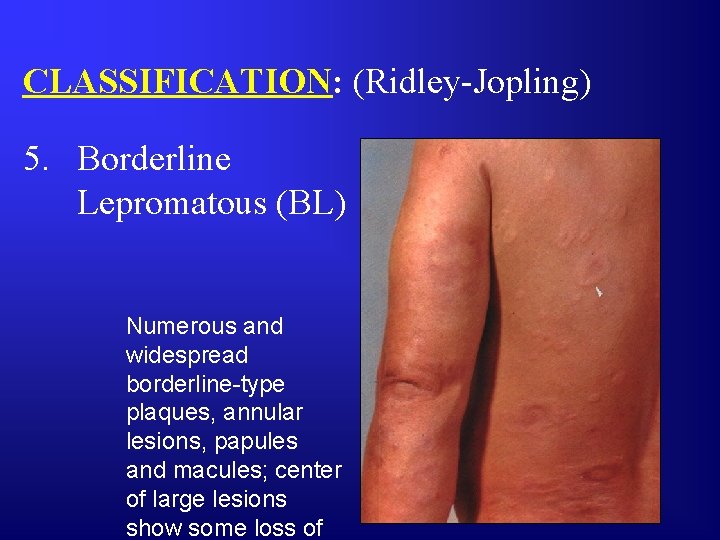
CLASSIFICATION: (Ridley-Jopling) 5. Borderline Lepromatous (BL) Numerous and widespread borderline-type plaques, annular lesions, papules and macules; center of large lesions show some loss of
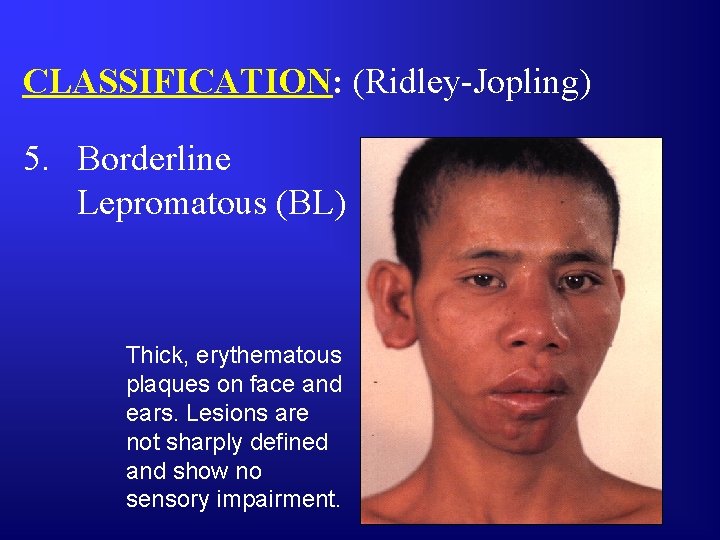
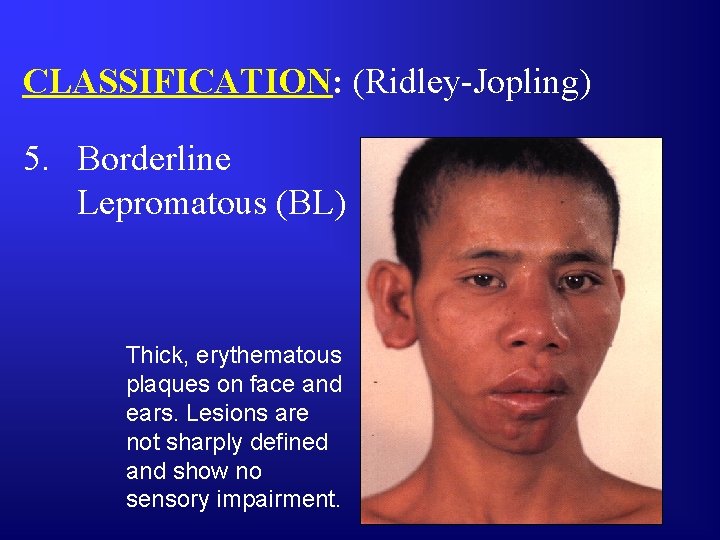
CLASSIFICATION: (Ridley-Jopling) 5. Borderline Lepromatous (BL) Thick, erythematous plaques on face and ears. Lesions are not sharply defined and show no sensory impairment.
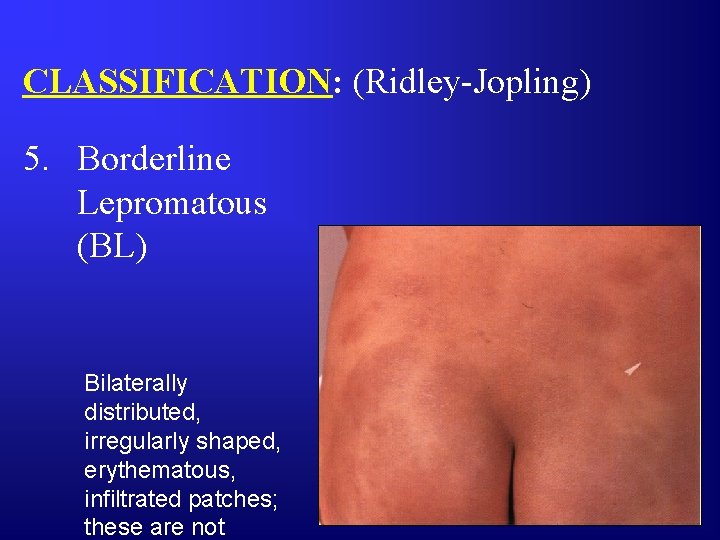
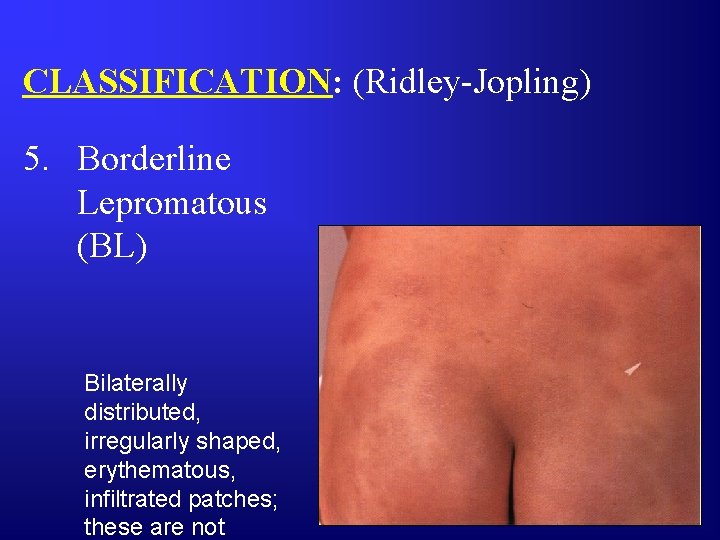
CLASSIFICATION: (Ridley-Jopling) 5. Borderline Lepromatous (BL) Bilaterally distributed, irregularly shaped, erythematous, infiltrated patches; these are not

CLASSIFICATION: (Ridley-Jopling) 5. Borderline Lepromatous (BL) Fairly uniform symmetrically distributed, infiltrated, maculopapular lesions, none of which show sensory impairment.
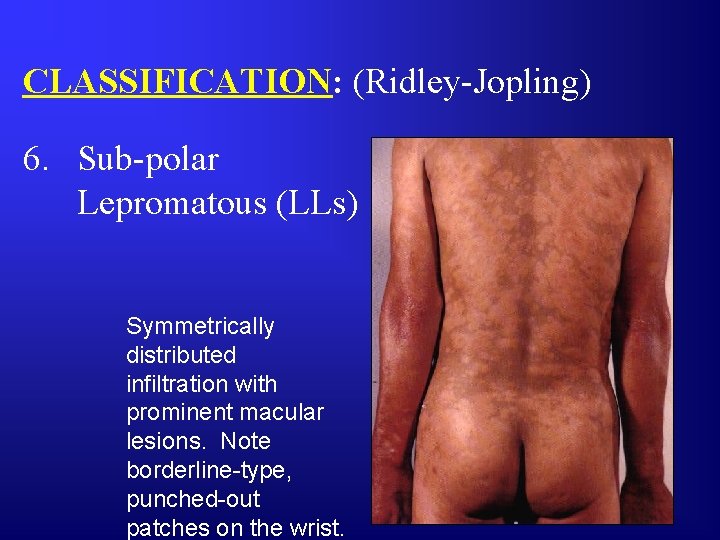
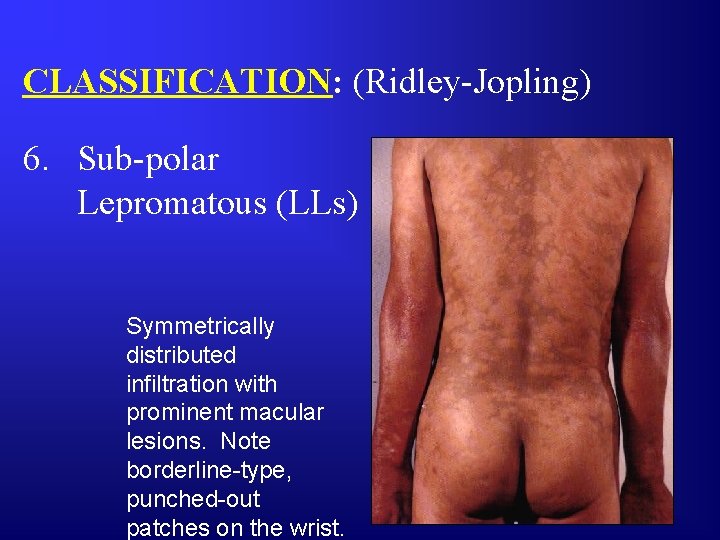
CLASSIFICATION: (Ridley-Jopling) 6. Sub-polar Lepromatous (LLs) Symmetrically distributed infiltration with prominent macular lesions. Note borderline-type, punched-out patches on the wrist.
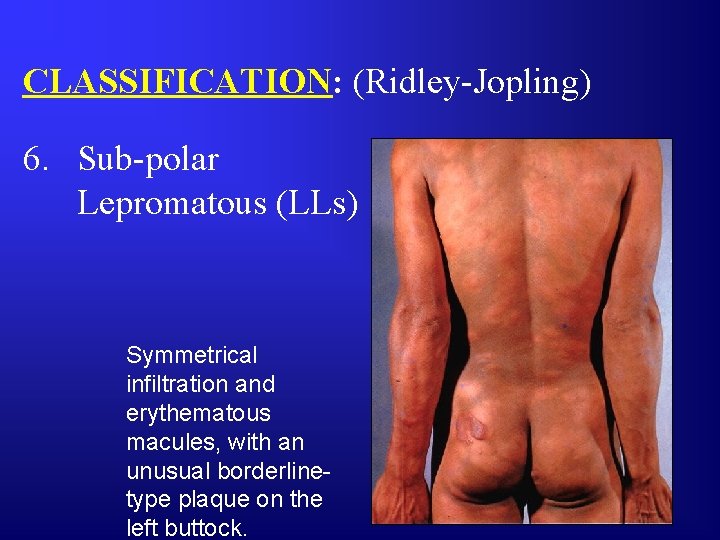
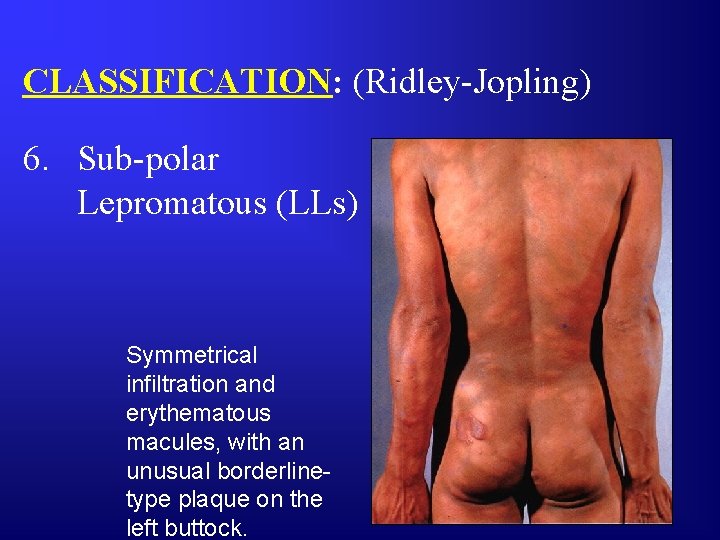
CLASSIFICATION: (Ridley-Jopling) 6. Sub-polar Lepromatous (LLs) Symmetrical infiltration and erythematous macules, with an unusual borderlinetype plaque on the left buttock.

CLASSIFICATION: (Ridley-Jopling) 6. Sub-polar Lepromatous (LLs) Extensive, symmetrically distributed infiltration with almost coalescent macules and plaques. These lesions are not anesthetic. Note small rounded borderline-type plaque on the left lumbar
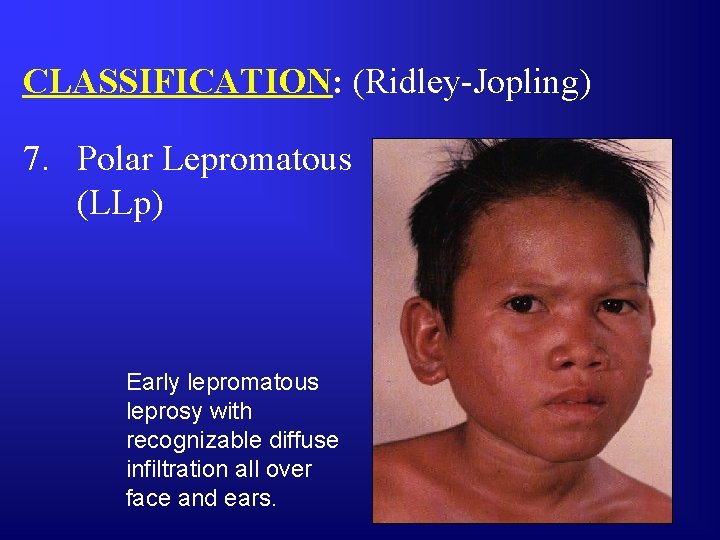
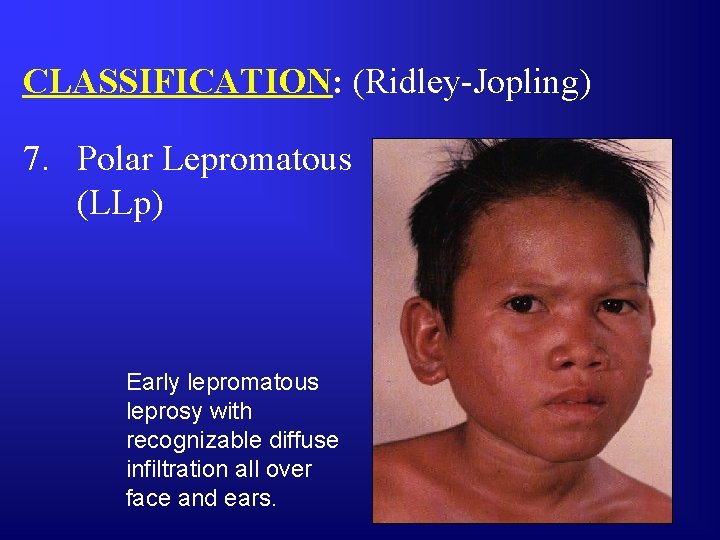
CLASSIFICATION: (Ridley-Jopling) 7. Polar Lepromatous (LLp) Early lepromatous leprosy with recognizable diffuse infiltration all over face and ears.
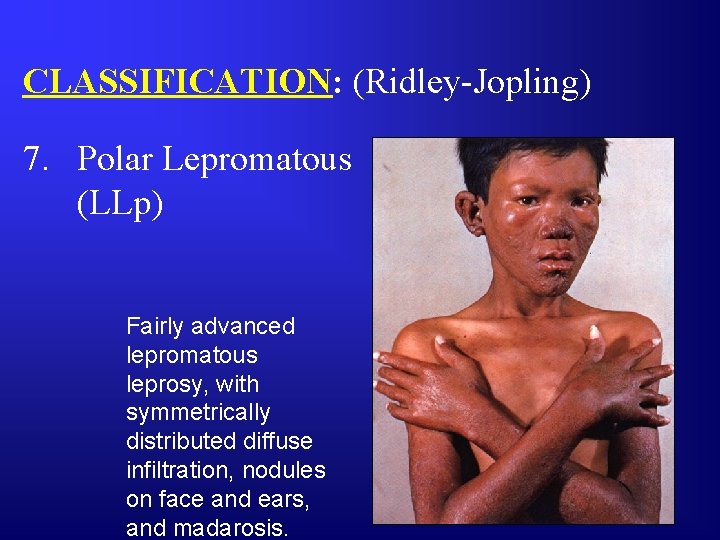
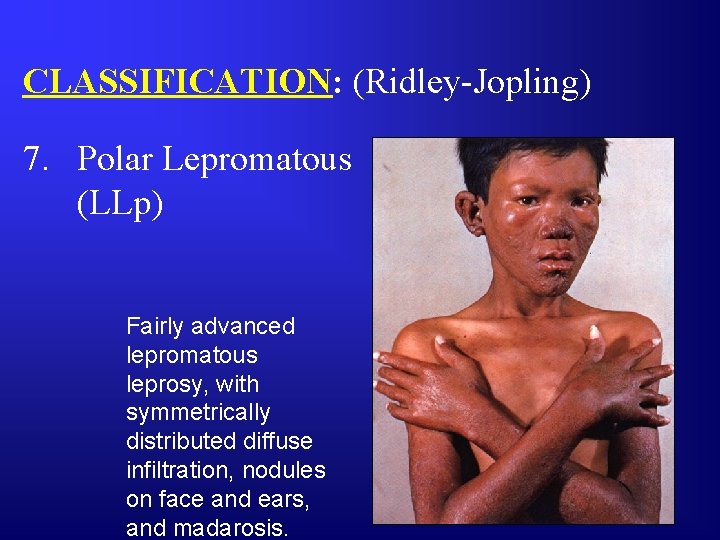
CLASSIFICATION: (Ridley-Jopling) 7. Polar Lepromatous (LLp) Fairly advanced lepromatous leprosy, with symmetrically distributed diffuse infiltration, nodules on face and ears, and madarosis.
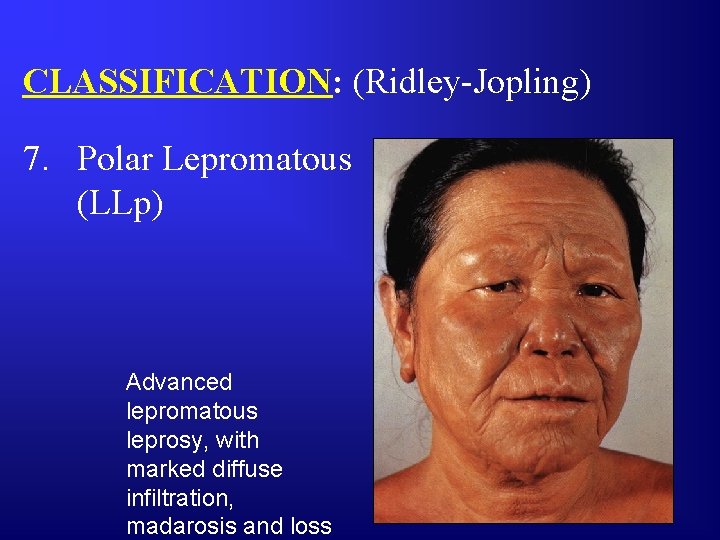
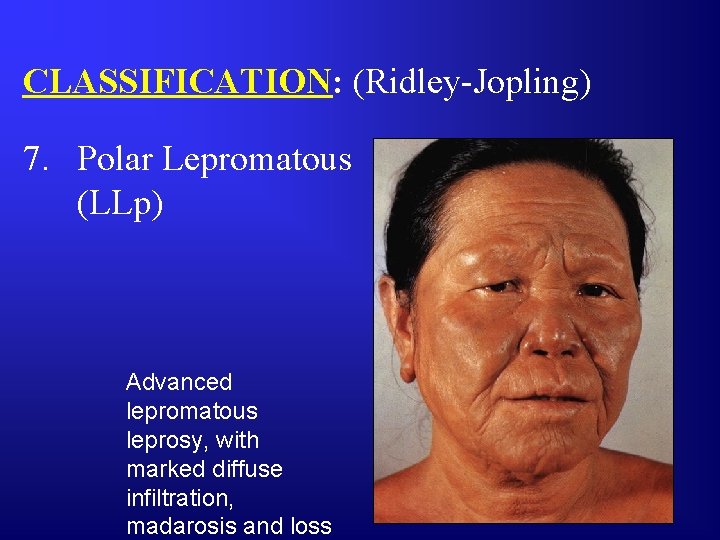
CLASSIFICATION: (Ridley-Jopling) 7. Polar Lepromatous (LLp) Advanced lepromatous leprosy, with marked diffuse infiltration, madarosis and loss
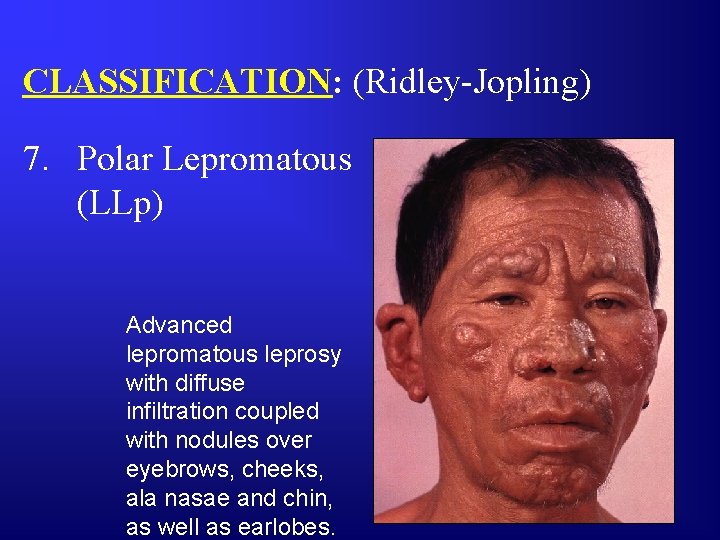
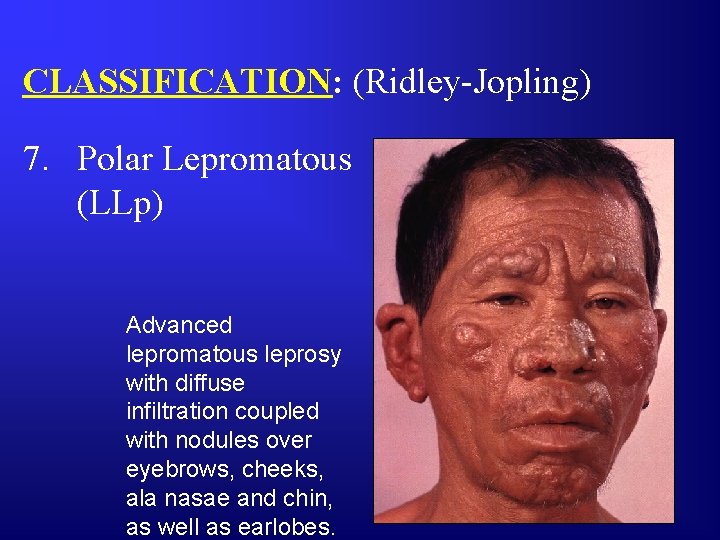
CLASSIFICATION: (Ridley-Jopling) 7. Polar Lepromatous (LLp) Advanced lepromatous leprosy with diffuse infiltration coupled with nodules over eyebrows, cheeks, ala nasae and chin, as well as earlobes.

CLASSIFICATION: (Ridley-Jopling) 7. Polar Lepromatous (LLp) Advanced lepromatous leprosy with diffuse infiltration and nodular lesions.
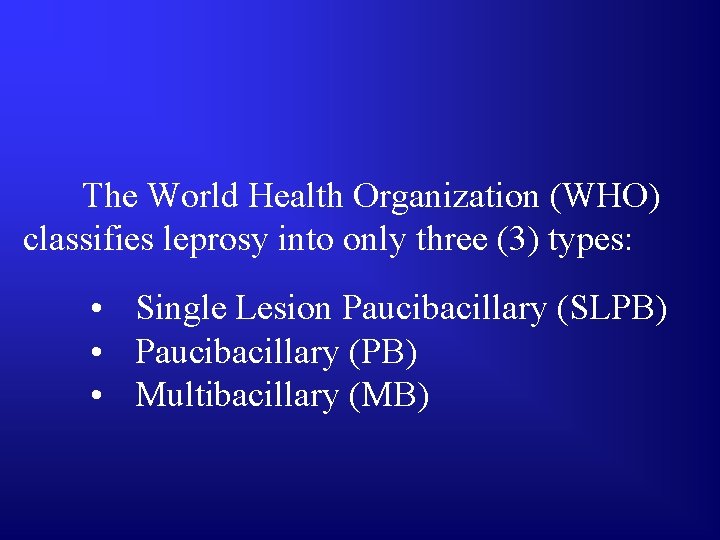
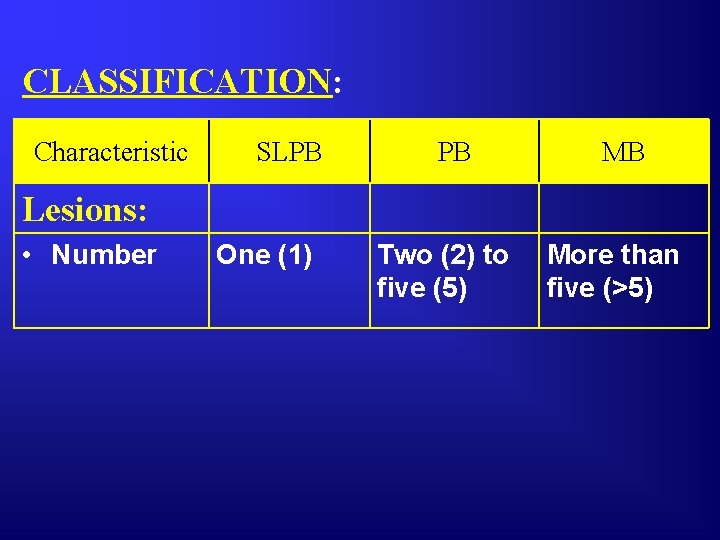
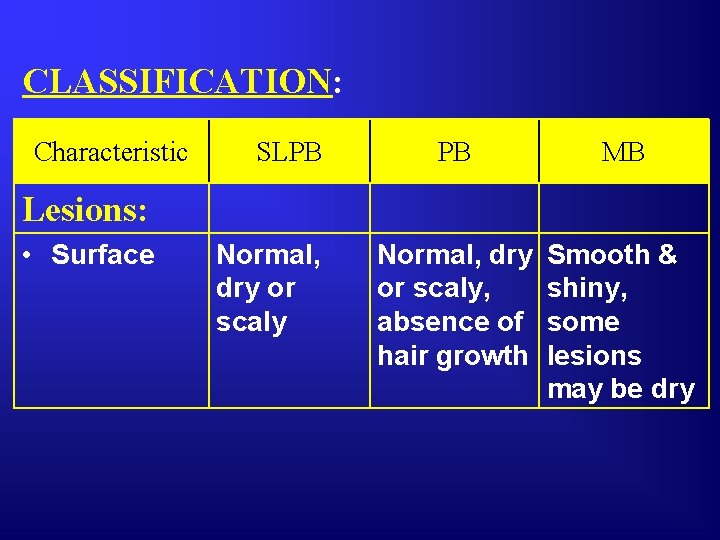
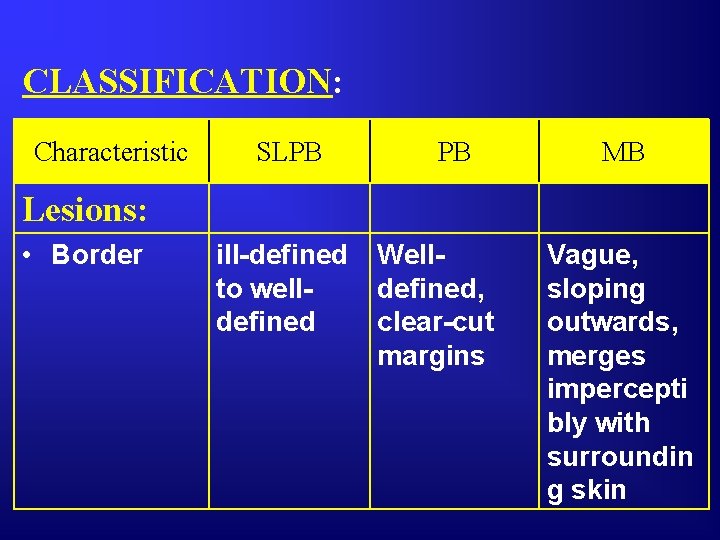
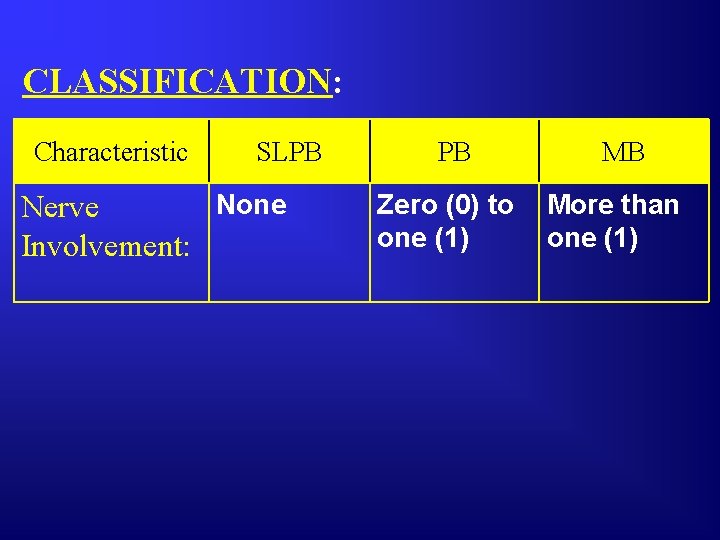
The World Health Organization (WHO) classifies leprosy into only three (3) types: • Single Lesion Paucibacillary (SLPB) • Paucibacillary (PB) • Multibacillary (MB)

CLASSIFICATION: Characteristic SLPB PB MB Lesions: • Type Macule Infiltrated patches Macules, plaques, papules & infiltration
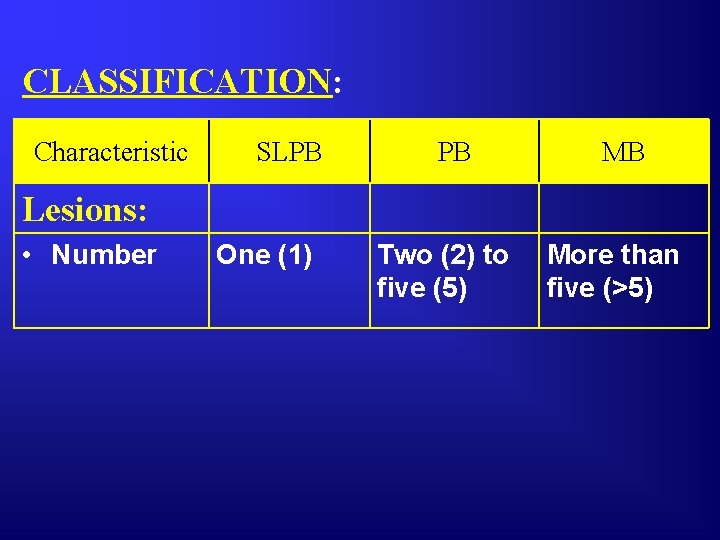
CLASSIFICATION: Characteristic SLPB PB MB Lesions: • Number One (1) Two (2) to five (5) More than five (>5)
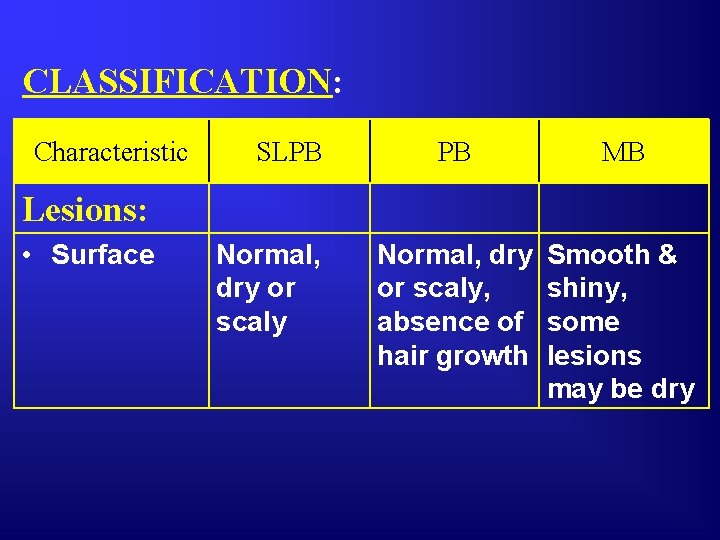
CLASSIFICATION: Characteristic SLPB PB MB Normal, dry or scaly, absence of hair growth Smooth & shiny, some lesions may be dry Lesions: • Surface Normal, dry or scaly
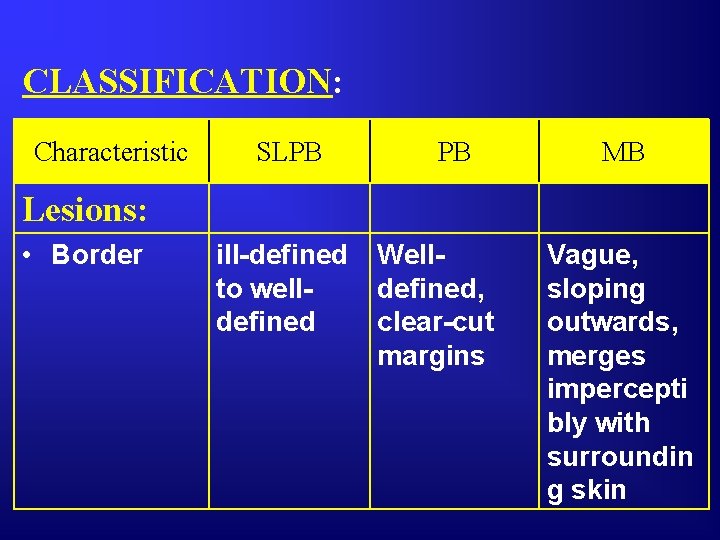
CLASSIFICATION: Characteristic SLPB PB MB Lesions: • Border ill-defined to welldefined Welldefined, clear-cut margins Vague, sloping outwards, merges impercepti bly with surroundin g skin
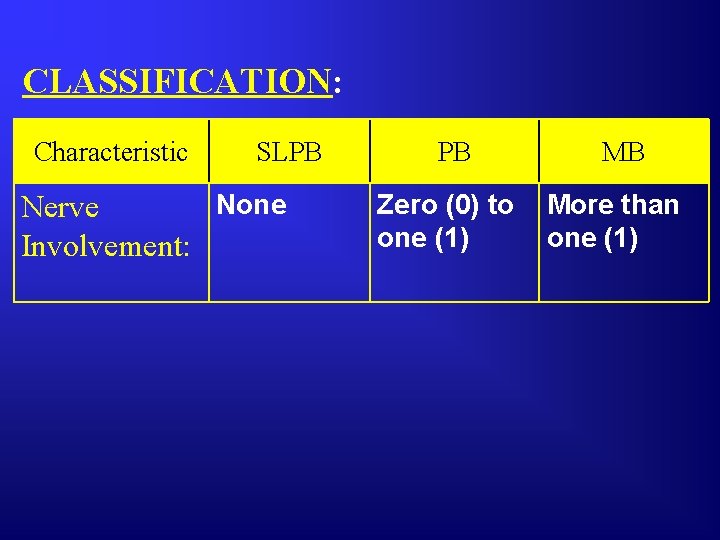
CLASSIFICATION: Characteristic SLPB None Nerve Involvement: PB Zero (0) to one (1) MB More than one (1)
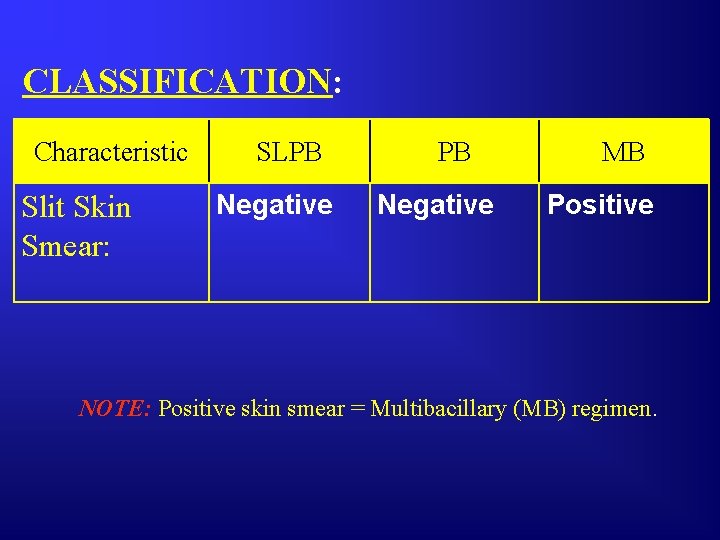
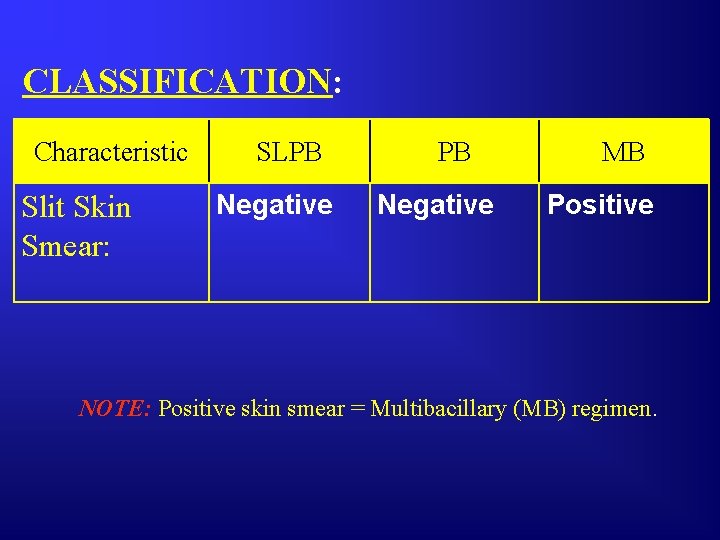
CLASSIFICATION: Characteristic Slit Skin Smear: SLPB Negative MB Positive NOTE: Positive skin smear = Multibacillary (MB) regimen.
