Modern Medicine Health Care Revolution 1 Previous session



- Slides: 46
Modern Medicine , Health Care Revolution 1
Previous session • Introduction to Community Medicine • Evolution of Public Health • Medicine in Antiquity • Origin of Indian System of Medicine • Birth of Preventive Medicine • Rise of Public Health 2
MODERN MEDICINE • Dichotomy of medicine into two major branches namely curative medicine, and public health/preventive medicine was evident by 19 th Century. • After 1900, medicine moved faster towards specialization, and a rational, scientific approach to disease. • Pattern of disease began to change. • With the control of acute infectious diseases, the socalled modern diseases such as cancer, diabetes, cardiovascular disease, mental illness and accidents came into prominence and have become the leading cause of death in industrialized countries.
Curative Medicine • Realization began to dawn that there are other factors or causes in the aetiology of diseases, namely social, economic, genetic, environmental and psychological factors which are equally important. • Germ theory of disease gave place to a newer concept of disease - “multifactorial causation” • In fact, it was Pettenkofer of Munich (1819 -1901) who first mooted the concept of multifactorial causation of disease but his ideas were lost in the bacteriological era. • Concept of multifactorial causation was revived by epidemiologists who have contributed significantly to our present-day understanding of multifactorial causation of disease and “risk factors” in the aetiology of disease.
Curative medicine • Some specialties have emerged, based on clearly defined skills such as surgery, radiology, and anesthesia; • Some based on parts of the body such as ENT, ophthalmology, cardiology, gynecology; • Some based on particular age or sex groups such as pediatrics, geriatrics and obstetrics. • Again, within each specialty, there has been a growth of sub-specialities, as for example, neonatology, perinatology, pediatric cardiology, paediatric neurology and pediatric surgery — all in paediatrics.
Curative medicine • Specialization has no doubt raised the standards of medical care, but it has escalated the cost of medical care and placed specialist medical care beyond the means of an average citizen, without outside aid or charity. • Specialization has also contributed to the decline of general practice and the isolation of medical practitioners at the periphery of the medical care system.
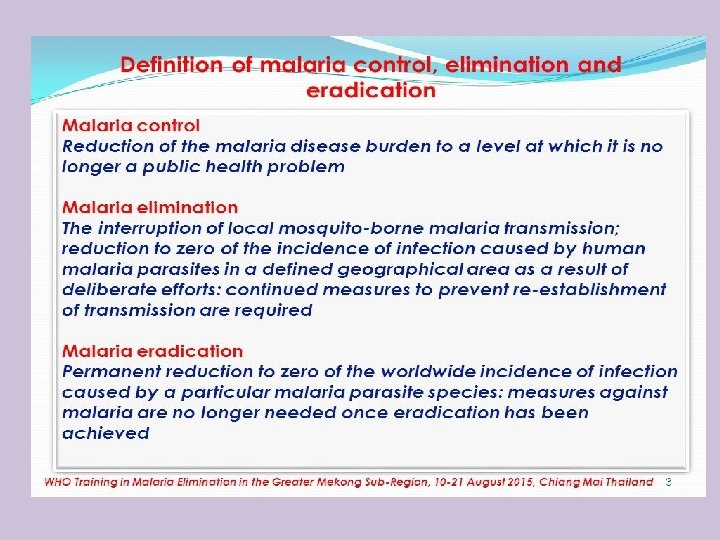
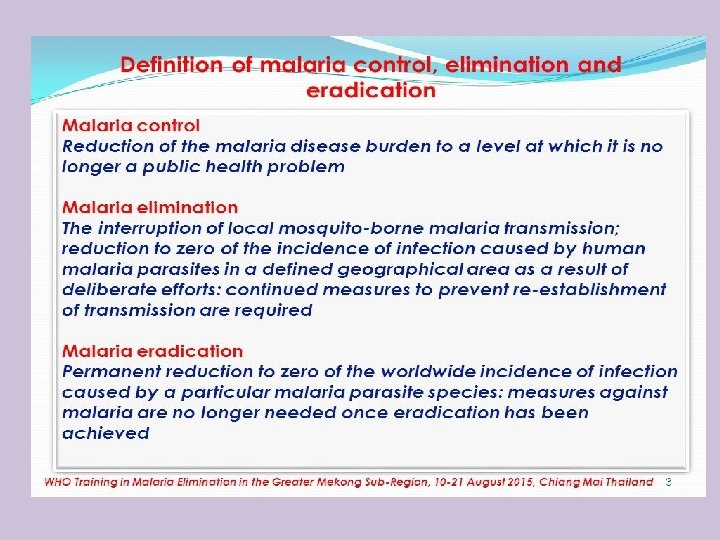
Preventive medicine • A new concept - concept of disease eradication began to take shape. • Between control and eradication, an intermediate goal has been described, called “regional elimination”. • Term “elimination” is used to describe interruption of transmission of disease, as for example, elimination of measles, polio and diphtheria from large geographic regions or areas.
§Eradication literally means to “tear out by roots’. §Eradication of disease implies termination of all transmission of infection by extermination of the infectious agent. §Word eradication is reserved to cessation of infection and disease from the whole world. 8
Preventive medicine • Consequently, research in human fertility and contraceptive technology has gained momentum. • Genetic counseling is another aspect of the population problem that is receiving attention. • Preventive medicine has become a growing point in medicine. • Preventive measures are already being applied not only to the chronic degenerative and hereditary diseases but also to the special problems of old age. • In fact, as medical science advances, it will become more and more preventive medical practice in nature. • Emergence of preventive paediatrics, geriatrics and preventive cardiology reflect newer trends in the scope of preventive medicine.
Preventive medicine • Three levels of prevention are now recognized: • Primary, intended to prevent disease among healthy people; • Secondary , directed towards those in whom the disease has already developed; and • Tertiary, to reduce the prevalence of chronic disability consequent to disease. • Besides communicable diseases, it is concerned with the environmental, social, economic and more general aspects of prevention. • Modern preventive medicine has been defined as “The art and science of health promotion, disease prevention, disability limitation and rehabilitation”.
SOCIAL MEDICINE 12
Social medicine • In 1911, the concept of social medicine was revived by Alfred Grotjahn (1869 -1931) of Berlin who stressed the importance of social factors in the aietology of disease, which he called “social pathology”. • In 1912 Rene Sand had founded the Belgian Social Medicine Association. • Developments in the field of social sciences (e. g. , sociology, psychology, anthropology) rediscovered that man is not only a biological animal but also a social being, and disease has social causes, social consequences and social therapy • Ideas of social medicine spread to other countries. • Promoted the concept of social medicine in England. • A Chair of social medicine was setup at Oxford in 1942 followed by similar others in other Universities in England.
Social medicine • By derivation social medicine is the “Study of man as a social being in his total environment”. • In short, social medicine is not a new branch of medicine but rather a new orientation of medicine to the changing needs of man and society. • Emphasizes the strong relationship between medicine and social sciences. • Entered into a productive relationship with social sciences and statistics to be able to elucidate the role of social factors in disease aetiology.
Changing concepts of Public Health • In the history of public health, four distinct phases may be demarcated: I. Disease control phase(1880 -1920) II. Health promotional phase(1920 -1960) III. Social engineering phase(1960 -1980) IV. Health for all phase(1980 -2000)
a. Disease control phase (1880 -1920) • Public health during the 19 th century was largely a matter of sanitary legislation and sanitary reforms aimed at the control of man’s physical environment, e. g. , water supply, sewage disposal, etc. • Clearly these measures were not aimed at the control of any specific disease, for want of the needed technical knowledge. • However, these measures vastly improved the health of the people due to disease and control of deaths.
b. Health promotional phase (1920 -1960): • At the beginning of the 20 th century, a new concept, the concept of “health promotion” began to take shape. • Consequently, in addition to disease control activities, one more goal was added to public health, that is, health promotion of individuals. It was initiated as personal health services such as o. Mother and child health services, o. School health- services, o. Industrial health services, o. Mental health and o. Rehabilitation services.
b. Health promotional phase (1920 -1960): • Public health nursing was a direct offshoot of this concept. • Public health departments began expanding their programmes towards health promotional activities. • C. E. A. Winslow, one of the leading figures in the history of public health, in 1920, defined public health as • “The science and art of preventing disease, prolonging life and promoting health and efficiency through organized community effort”. • This definition summarises the philosophy of public health which remains largely true even today.
b. Health promotional phase (1920 -1960): • Two great movements were initiated for human development during the first half of the present century namely • a) Provision of “basic health services” through the medium of primary health centres and sub-centres for rural and urban areas. • Evolution of health centres is an important development in the history of public health. • Bhore Committee (1946) in India had also recommended the establishment of health centers for providing integrated curative and preventive medicine.
b. Health promotional phase (1920 -1960): • (b) Second great movement was the community development programme to promote village development through the active participation of the whole community and on the initiative of the community. • This programme tried to do too much quickly with inadequate resources. • It was a great opportunity lost because it failed to survive. • However the establishment of primary health centers and sub-centers provided the much needed infrastructure of health services, especially in the rural areas.
c. Social engineering phase (1960 -1980) • With the advances in preventive medicine and practice of public health, the pattern of disease began to change in the developed world. • Many of the acute illness problems have been brought under control. • However, as old problems were solved, new health problems in the form of chronic diseases began to emerge, e. g. , cancer, diabetes, cardiovascular diseases, alcoholism and drug addiction etc.
c. Social engineering phase (1960 -1980): • A new concept, the concept of “risk factors” as determinants of these diseases came into existence. • Consequences of these diseases, unlike the swift death brought by the acute infectious diseases, was to place a chronic burden on the society that created them. • Public health entered a new phase in the 1960 s, described as the “social engineering” phase.
d. Health for all phase (1981 -2000 AD): • Most people in the developed countries, and the elite of the developing countries, enjoy all the determinants of good health - adequate income, nutrition, education, sanitation, safe drinking water and comprehensive health care. • In contrast, only 10 to 20 per cent of the population in developing countries enjoy ready access to health services of any kind. • Death claims 60 -250 of every 1000 live births within the first year of life, and the life expectancy is 30 per cent lower than in the developed countries.
d. Health for all phase (1981 -2000 AD): • John Bryant focused on challenge of inequalities in health by saying: “Large numbers of the world’s people, perhaps more than half, have no access to health care at all, and for many of the rest the care they receive does not answer the problems they have”. • Global conscience was stirred leading to a new awakening that the health gap between rich and poor within countries and between countries should be narrowed and ultimately eliminated.
d. Health for all phase (1981 -2000 AD) • Against this background, in 1981, the members of the WHO pledged themselves to an ambitious target to provide Health for All by the year 2000, that is attainment of a level of health that will permit all peoples “to lead a socially and economically productive life”. • Currently public health, along with other medical sciences and other health-related sectors is engaged in this broad field of effort.
MEDICAL REVOLUTION
Failure of medicine • Some critics have even described modern medicine as a threat to health. • Their argument have been based on certain facts such as: • With increased medical costs has not come increased benefits in terms of health (a) Despite spectacular advances in medicine, the threat posed by certain major diseases such as malaria, schistosomiasis, leprosy, filaria, trypanosomiasis and leishmaniasis either has not lessened or has actually increased. (b) The expectation of life has remained low and infant and child mortality rates high in many developing countries, despite advances in medicine (c) There is no equity in the distribution of health services, resulting in limited access to health care for large segments of the world’s population.
Family and community medicine • Emergence of Family and Community Medicine represents a counterforce to the direction which medical science has taken during the past 20 years or so. • Called for a rapid return of the general physician (family physician) who would give comprehensive and personalized care. • Field of specialization of family and community medicine is neither an organ system nor a disease syndrome, but rather in both instances, a designation of social categories namely family and community. • Family and community medicine overlap and strengthen each other.
Family Medicine • Emergence of family medicine has been hailed as a rediscovery of the human, social and cultural aspects of health and disease and of the recognition of family as a focal point of health care and the right place for integrating preventive, promotive and curative services. • Family medicine has been defined as “a field of specialization in medicine which is neither disease nor organ oriented”. • It is family oriented medicine or health care centred on the family as the unit - from first contact to the ongoing care of chronic problems (from prevention to rehabilitation). • When family medicine is applied to the care of patients and their families, it becomes the speciality of family practice. • Speciality of family practice is specially designed to deliver “primary care”.
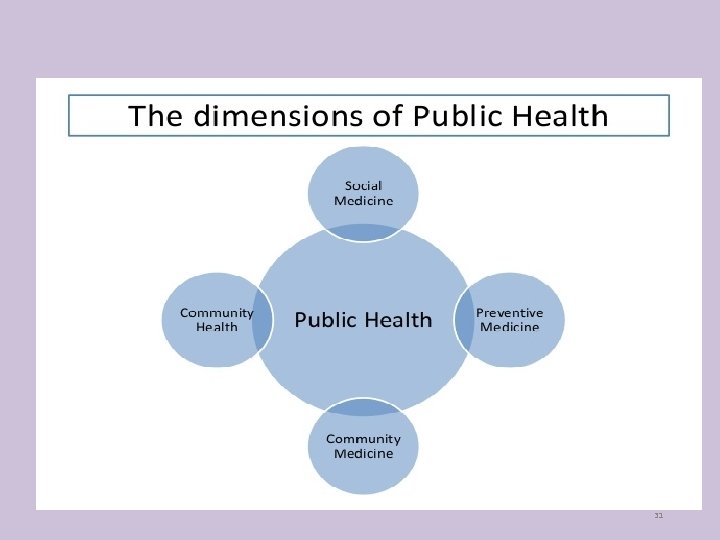
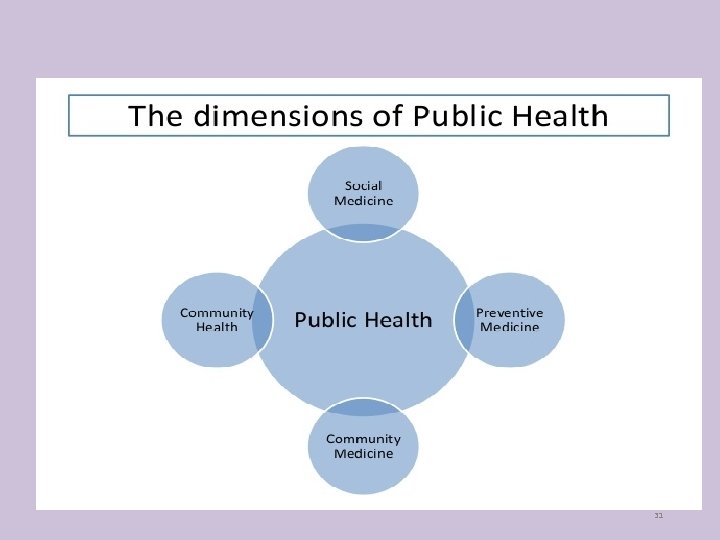
Community Medicine: • Like family medicine, community medicine is a-newcomer. • It is the successor of what was previously known as public health, community health, preventive and social medicine. • All these share common ground, i. e. , prevention of disease and promotion of health. • Faculty of Community Medicine of the Royal College of Physicians has defined community medicine as “That specialty which deals with populations and comprises those doctors who try to measure the needs of the population, both sick and well, who plan and administer services to meet those needs, and those who are engaged in research and teaching in the field”. • To make matters worse, a WHO study group stated that since health problems vary from country to country, each country should formulate its own definition of community medicine in the light of its traditions, geography and resources.
31
HEALTH CARE REVOLUTION
Background • In both developed and developing countries, the standard of health services the public expected was not being provided. • Services do not cover the whole population. • A very high proportion of the population in many developing countries, and especially in rural areas does not have ready access to health services. • Health services favoured only the privileged few and urban dwellers. • Although there was the recognition that health is a fundamental human right, there is a denial of this right to millions of people who are caught in the vicious circle of poverty and ill health. • There are marked differences in health status between people in different countries as well as between different groups in the same country; the cost of health care is rising without much improvement in their quality.
Health for All • Against the above background the 30 th World Health Assembly resolved in May 1977, that “The main social target of governments and WHO in the coming decades should be the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life”. • Culminated in the international objective of HEALTH FOR ALL by the year 2000 as the social goal of all governments.
Health for All • Goal of Health for All has two perspectives. • Long-term context, it simply means the realization of the WHO’s objective of “Attainment by all peoples of the highest possible level of health”. • But, what is of immediate relevance is the meaning that, as a minimum, all people in all countries should have at least such a level of health that they are capable of working productively and of participating actively in the social life of the community in which they live.

Primary health care • With increasing recognition of the failure of existing health services to provide health care, alternative ideas and methods to provide health care have been considered and tried. • Discussing these issues at the Joint WHO-UNICEF international conference in 1978 at Alma-Ata (USSR), the governments 134 countries and many voluntary agencies called for a revolutionary approach to health care. • Declaring that “The existing gross inequality in the health status of people particularly between developed and developing countries as well as within countries is politically, socially and economically unacceptable” • Alma-Ata conference called for acceptance of the WHO goal of Health For All by 2000 AD and proclaimed primary health care as way to achieving Health for All.

Primary health care • Primary health care is a new approach to health care, which integrates at the community level all the factors required for improving the health status of the population. • Primary health care is available to all people at the first level of health care. • It is based on principles of equity, wider coverage, individual and community involvement and intersectoral coordination. • While it integrates promotive, preventive and curative services, it is also conceived as an integral part of the country’s plan for socio-economic development.
Primary health care • Alma-Ata Declaration called on all governments to formulate national policies, strategies and plans of action to launch and sustain primary health care as part of a national health system. • It is left to each country to innovate, according to its own circumstances to provide primary health care. • This was followed by the formulation and adoption of the Global strategy for Health for All by the 34 th World Health Assembly in 1981. • Primary health care got off to a good start in many countries with theme “Health for All by 2000 AD”.
Deprofessionalization of medicine • Practice of primary health care involves a good deal of “Deprofessionalization” of medicine. • While the physician still holds his unique position in the field of health care in general, the participation of a new cadre of health workers (e. g. , community health workers, anganwadi workers, multipurpose workers, practitioners of indigenous medicine, social workers) with relatively little training and support have been considered and fried to provide health care. They now comprise part of the “health teams”. • Medical man can no longer restrict himself to his traditional role as diagnoser of ailments, prescriber of pills and potions, and exciser of lumps. • He has acquired new roles - being an educator, case-finder, preventer, counsellor and an agent of social change.
The Millennium Development Goals • In September 2000, representatives from 189 countries met at the Millennium Summit in New York to adopt the United Nations Millennium Declaration. • Road Map established goals and targets to be reached by year 2015 in each of seven areas. • Goals in the area of development and poverty eradication are now widely referred to as “Millennium Development Goals”.
The Millennium Development Goals • Millennium Development Goals place health at the heart of development and represent commitments by governments throughout the world to do more to poverty and hunger, and to tackle ill-health, gender inequality, lack of education, access to clean water and environmental degradation. • Thus three of the eight goals are directly health related and all of other goals have important indirect effects on health; 8 of the 18 targets are required to achieve these goals, and 18 of the 48 indicators of the progress are health related.
MCQs The term Social Medicine was introduced by a) Jules Guerin b) Crew c) John Ryle d) Alfred Grotjahn Who is regarded as father of Public Health a) Louis Pasteur b) Cholera c) John Snow d) James Lind
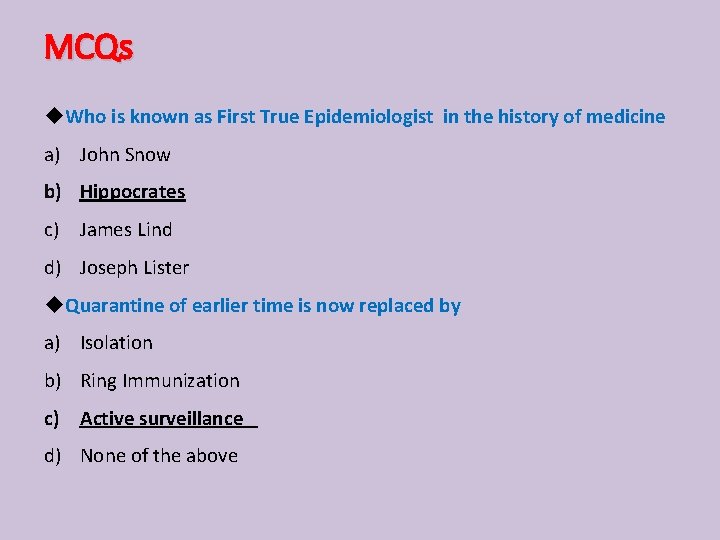
MCQs Who is known as First True Epidemiologist in the history of medicine a) John Snow b) Hippocrates c) James Lind d) Joseph Lister Quarantine of earlier time is now replaced by a) Isolation b) Ring Immunization c) Active surveillance d) None of the above
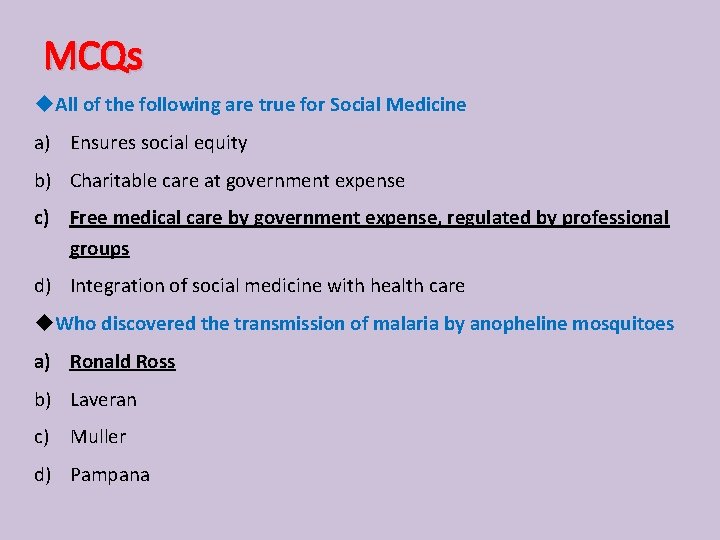
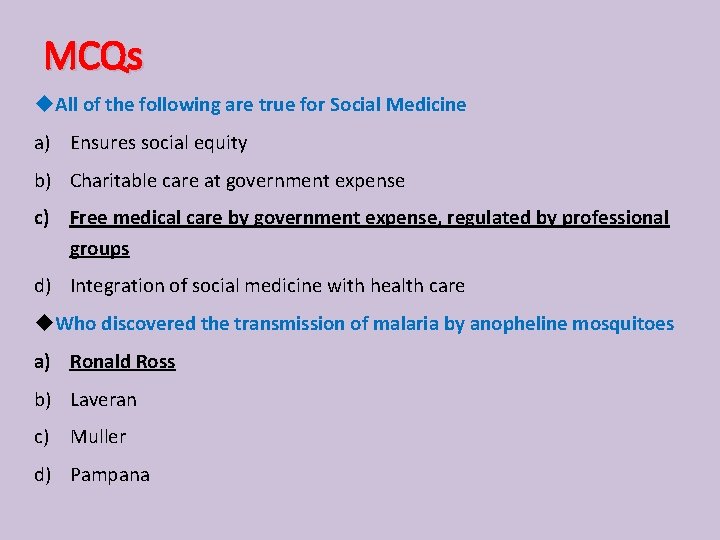
MCQs All of the following are true for Social Medicine a) Ensures social equity b) Charitable care at government expense c) Free medical care by government expense, regulated by professional groups d) Integration of social medicine with health care Who discovered the transmission of malaria by anopheline mosquitoes a) Ronald Ross b) Laveran c) Muller d) Pampana
References • Parks text book of Community Medicine: 24 th Edition. • Epidemiology by Leon Gordis: 6 th Edition • Suryakantha: A text of “Community medicine with Recent Advances”: 4 th Edition. • www. who. int

THANKS 46