MODELING HEALTHY BEHAVIOR VALIDATING THE SOCIAL WORK LEADERSHIP
MODELING HEALTHY BEHAVIOR: VALIDATING THE SOCIAL WORK LEADERSHIP ROLE IN A GROWING PALLIATIVE CARE WORLD DANA RIBEIRO MILLER M. DIV. , LMSW, ACHP-SW PALLIATIVE SOCIAL WORKER NYU WINTHROP PALLIATIVE MEDICINE & BIOETHICS REBECCA FREEMAN, LMSW, ACHP-SW HOSPICE LIAISON SUPERVISOR HOSPICE OF NEW YORK
OBJECTIVES • Reinforce the role of palliative social work as the behavioral health expert on the Palliative Care Team • Reinforce foundational social work learning that validates our ability to take a leadership role in team function and strategy • • Discuss strategies for recognizing and correcting team dysfunction Explore strategies for facilitating ongoing team success
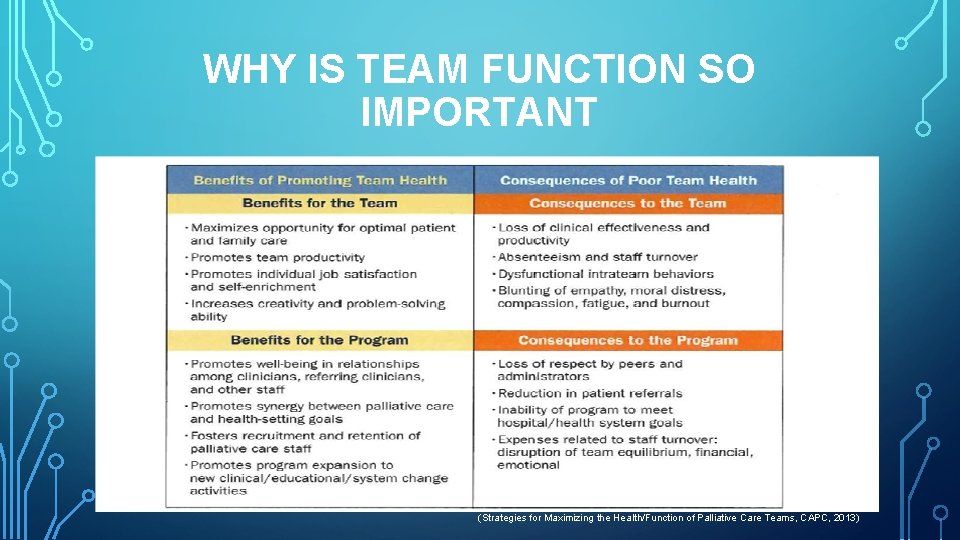
WHY IS TEAM FUNCTION SO IMPORTANT (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
ATTRIBUTES OF HEALTHY TEAMS • Well defined program, mission, vision and goals • Clearly delineated roles for each clinician/discipline • • Recognizing expertise while acknowledging shared work Recognition that each discipline has its own unique code of ethics and relational responsibility • Shared team values that are consistently articulated • Established lines of accountability, reporting, and supervision (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013

ATTRIBUTES OF HEALTHY TEAMS • Demonstrated respect and appreciation for • • Individual team members Team as a whole • Open communication striving to • • Resolve conflicts Promote trust Work towards common goals Strong leadership skills visible from program directors/leaders (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013
WHY PALL SW DOMAIN • While palliative colleagues have many shared attributes, social workers are specifically trained in: • • Verbal and non verbal communication Role modeling • • • Shared decision making Joint learning Group Therapy Facilitation Relational Dynamics Family Systems Therapy – teams are “families”
WHAT WE DO – COLLEAGUES • Colleague Distress • We don’t just work for patients and families, but our colleagues as well • If a case is particularly distressing we are always available to discuss • Medical Clinicians are people too, its normal to have emotions related to • our patients Not every patient/family will trigger “nice” feelings • Curbside • • We, like other colleagues can be curbsides for brief opinions or insights Often “unofficial team confidant”
UNOFFICIAL ROLE CAN BE DANGEROUS • Find ourselves powerless to act on information • Trapped in cycle of anonymity • Potentially dangerous information may be told to us in a collegial manner • • Raises ethical questions Raises moral questions • Feeling forced to share “unofficial” “confidential” information may lead to a disruption of team trust
IDENTIFYING OURSELVES AS TEAM EXPERT • Sets clear boundary for information that is shared with us • If dangerous, will be discussed further • If damaging, may be addressed • Latitude to use clinical judgement • Gives us autonomy within which to act accordingly • Unburdens us as “Secret Keeper” with no place to rest our own distress
FOUNDATIONAL SOCIAL WORK SKILLS • Unique skills that validate our ability to take a leadership role in team function and strategy: • Clinical training in: • • Therapeutic models Communication styles/patterns • Possess awareness of systems of power and culture • • Larger system culture Individual team interactions

WARNING SIGNS OF TEAM DISTRESS (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
INTERNAL RISKY BEHAVIORS • Absence of trust among team members • Fear of conflict within team • Lack of commitment to the team/program • Avoidance of staff accountability • Inattention to desired team outcomes/results (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
INTERNAL RISKY BEHAVIORS • Wanting team based results without constructing a team based structure • • • Focus on tasks vs. process/relationship Neglecting talent pool of team Discouraging collaboration and cooperation • Insufficient training • Team or individual attitudes of clinical or moral superiority that inhibit appropriate communication on patient care (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
HIGH RISK EVENTS • • • Young teams developing quickly • Personal crisis of a team member • Deaths, seriously ill family members, etc. Change in team membership Clinicians new to the field Disruptive behavior Vicarious trauma due to critical clinical incident: • Team member feeling they contributed to a death • Death of a young patient (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
POTENTIAL EXTERNAL DISTRESS CREATORS • Lack of well defined program mission within hospital culture • Lack of administrative/institutional support • Various assumptions, perspectives, legal responsibilities, and values that may not be articulated and/or respected • Clinical workload/financial pressures • Lack of clarity regarding the populations that can be served given existing resources (Strategies for Maximizing the Health/Function of Palliative Care Teams, CAPC, 2013)
PALLIATIVE SOCIAL WORKERS • Team Development • Palliative Social Workers are trained to facilitate healthy interdisciplinary teams • Create curriculums and programs that support this goal • Model collaborative skills • Model communication skills with primary teams
PALLIATIVE SW & TEAM FUNCTION • Maintain a pulse on the teams general health • Highlight when there is a need to refocus • Initiate inter-team conversations: • Role Clarity • Conflict • Nuances of Team Functions • Initiate time out to debrief/grieve/rejuvenate
A TEAM APPROACH TO DISTRESS • Team success is a joint effort, however we can take a leadership role by modeling healthy behaviors such as: • Boundaries • See Something Say Something • Create a space to be heard • Feedback as a tool to mitigate further conflict • A constant and evolving conversation vs. one big blowup over many slights • Being honest with colleagues about external pressures that might be affecting your function
CREATING TEAM SUCCESS • Respect for collective and individual wisdom • Team activities outside of patient care • • Social activities Celebrating life events Retreats Trainings/Conferences/Presentations • Intentional commitment to creating an environment of safety • Blending our work and personal selves highest indicator of team success (Project Aristotle, Google, 2016)
REFERENCES • Abramson, J. S. and Mizrahi, T. 1996. When social workers and physicians collaborate: Positive and negative interdisciplinary experiences. Social Work, 41: 270– 281. • Back, A. 2000. Communication between professions: Doctors are from Mars, social workers are from Venus. Journal of Palliative Medicine, 3(2): 221– 222. • Connor, S. R. , Egan, K. A. , Kwilosz, D. M. , Larson, D. G. and Reese, D. J. 2002. Interdisciplinary approaches to assisting with end-of-life care and decision making. American Behavioral Scientist, 46: 340– 356. Stark, D. Teamwork in Palliative Care: An Integrative Approach. Oxford Textbook of Palliative Social Work. NY, 2011. Pg. 415 -424
REFERENCES • Duhigg, C. , What Google Learned From Its Quest to Build the Perfect Team, The New York Times, August 2016 • Altilio, Et. Al. , Strategies for Maximizing the Health/Function of Palliative Care Teams: A Resource Monograph , CAPC, 2013 • • https: //www. socialworkers. org • http: //www. socialworklicensure. org/articles/clinical-vs-direct-servicessocial-work. html http: //www. bls. gov/ooh/community-and-social-service/mobile/socialworkers. htm
CONTACT INFORMATION Dana Ribeiro Miller M. Div. , LMSW, ACHP-SW: dmribeiro@nyuwinthrop. org Rebecca Freeman LMSW, ACHP-SW: Rebecca. freeman. @hospiceny. com
- Slides: 22