MLO 130 Hematology I Iron Metabolism and Hypochromic
MLO 130: Hematology I Iron Metabolism and Hypochromic Anemias
Factors Affecting Iron Levels • Amount ingested – Dietary intake • Amount absorbed – Non-reduced is converted to reduced by stomach acid – Reduced is converted to transferrin (transport) • Amount recycled – Heme returned to bone marrow
Factors Affecting Iron Levels • Iron stores – Ferritin – Hemosiderin • Iron loss – Blood loss

Iron Metabolism • Function – bind oxygen for transport • Where is it found? – 65% in RBCs – 25% stored in macrophages and hepatocytes (ferritin) – 10% in muscles, plasma, cytochromes of cells, enzymes

Iron balance

Iron Studies • • • Serum Iron TIBC: total iron binding capacity Percent saturation Prussian blue staining of tissues Serum ferritin

Serum Iron • Iron: 50 -160 ug/d. L with 95% bound to transferrin • Diurnal variation • Little value on its own
Total Iron Binding Capacity • amount of Fe transferrin carry 250 -450 ug/d. L • Indirect indicator of transferrin – total number of sites for Fe binding
Percent Transferrin Saturation • Calculation – (Serum Iron/TIBC) x 100 = % transferrin saturation • 20 -55% = normal •

Prussian Blue Staining • Reacts with ferric iron in tissue = microscopic blue dots – Also reacts with hemosiderin • Gold standard to assess amount of iron • Typically performed on bone marrow and liver biopsies

Ferritin • Detects amount of storage iron • Disadvantage: acute phase reactant – Increased during inflammation • Low ferritin levels correlate with iron deficiency anemia • Normal: 40 -400 ng/m. L
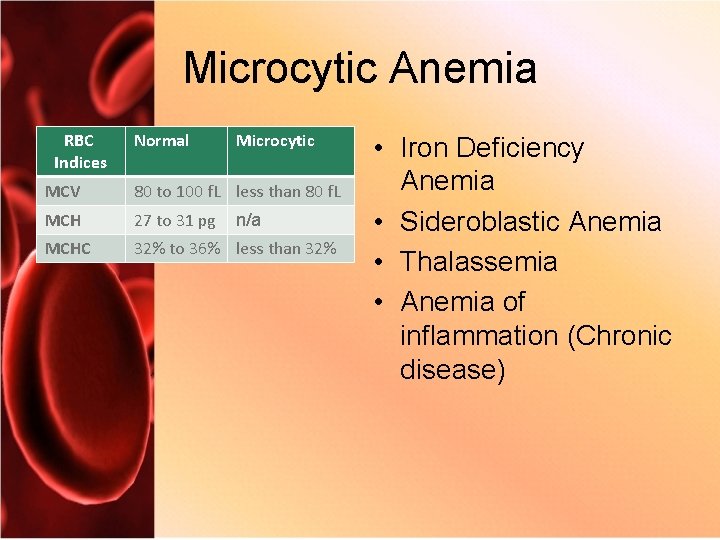
Microcytic Anemia RBC Indices Normal Microcytic MCV 80 to 100 f. L less than 80 f. L MCH 27 to 31 pg MCHC 32% to 36% less than 32% n/a • Iron Deficiency Anemia • Sideroblastic Anemia • Thalassemia • Anemia of inflammation (Chronic disease)
Causes of IDA • Dietary deficiency – Need to replace 1 mg of iron lost each day for balance • Blood loss • Increased need – Infancy, childhood, adolescence, pregnancy • Malabsorption – Celiac disease, decreased stomach acidity
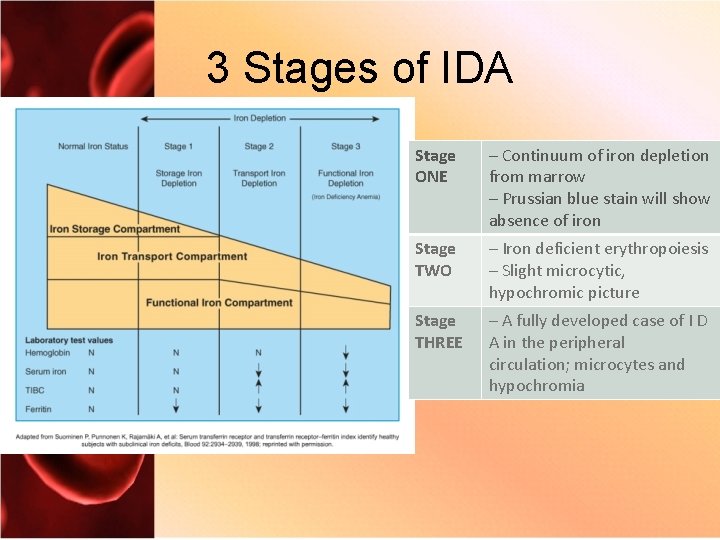
3 Stages of IDA Stage ONE – Continuum of iron depletion from marrow – Prussian blue stain will show absence of iron Stage TWO – Iron deficient erythropoiesis – Slight microcytic, hypochromic picture Stage THREE – A fully developed case of I D A in the peripheral circulation; microcytes and hypochromia
Clinical Features of IDA • • • Fatigue Pallor Vertigo Dyspnea Cold intolerance • • Lethargy Pica Cheilitis Koilonychia
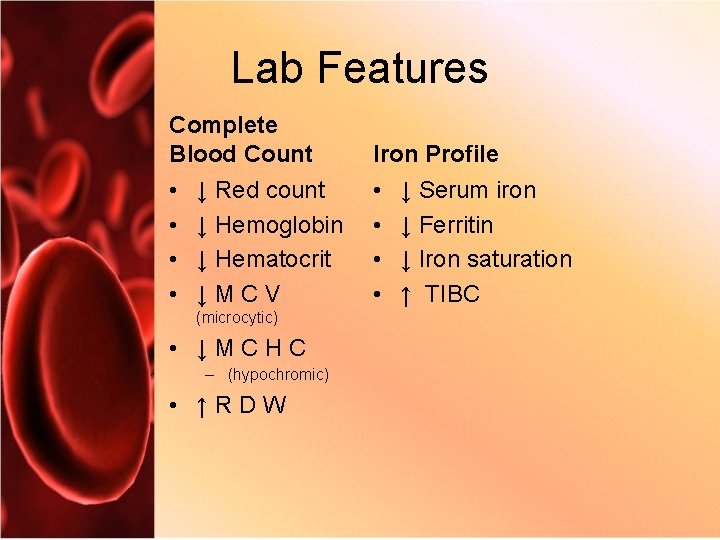
Lab Features Complete Blood Count Iron Profile • • ↓ Red count ↓ Hemoglobin ↓ Hematocrit ↓ M C V (microcytic) • ↓ M C H C – (hypochromic) • ↑ R D W ↓ Serum iron ↓ Ferritin ↓ Iron saturation ↑ TIBC
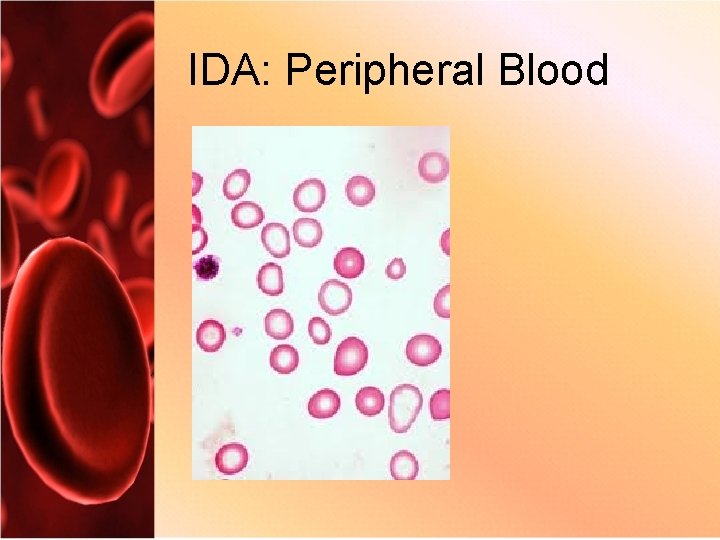
IDA: Peripheral Blood
Treatment • Oral – Ferrous sulfate – Ferrous gluconate – Ferrous fumarate • Infusion – Dosage, preparations, and time frame are dependent on age, conditions, and patient compliance
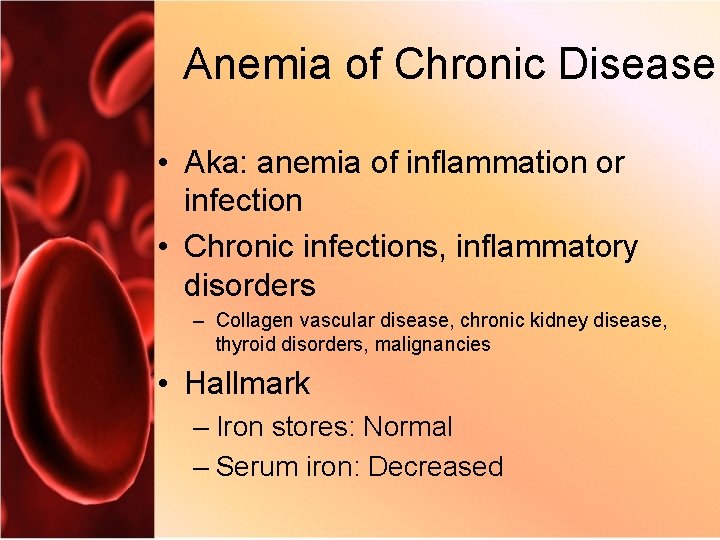
Anemia of Chronic Disease • Aka: anemia of inflammation or infection • Chronic infections, inflammatory disorders – Collagen vascular disease, chronic kidney disease, thyroid disorders, malignancies • Hallmark – Iron stores: Normal – Serum iron: Decreased
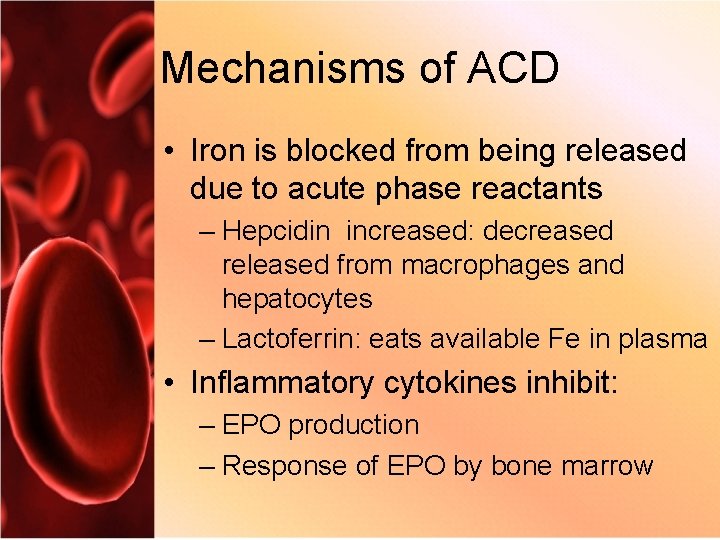
Mechanisms of ACD • Iron is blocked from being released due to acute phase reactants – Hepcidin increased: decreased released from macrophages and hepatocytes – Lactoferrin: eats available Fe in plasma • Inflammatory cytokines inhibit: – EPO production – Response of EPO by bone marrow
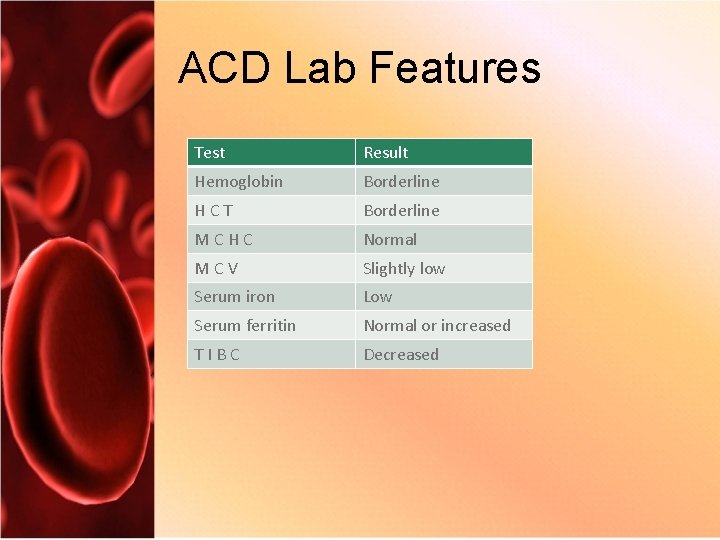
ACD Lab Features Test Result Hemoglobin Borderline H C T Borderline M C H C Normal M C V Slightly low Serum iron Low Serum ferritin Normal or increased T I B C Decreased
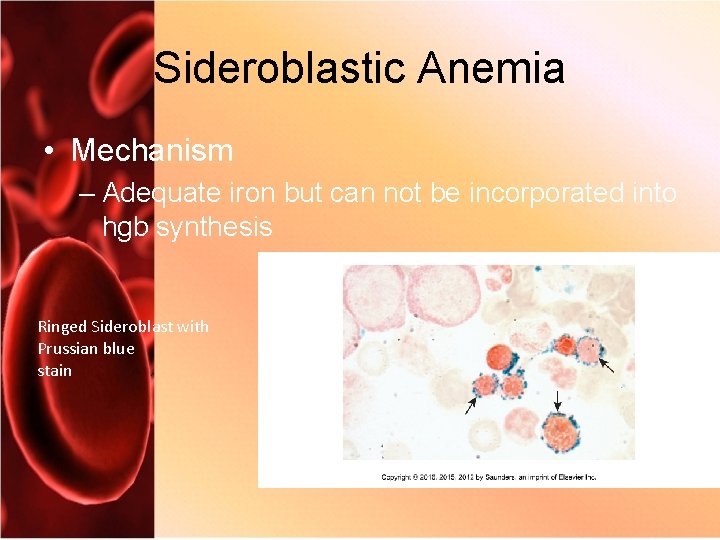
Sideroblastic Anemia • Mechanism – Adequate iron but can not be incorporated into hgb synthesis Ringed Sideroblast with Prussian blue stain
Classification of Sideroblastic Anemia • Hereditary – Sex-linked; abnormal ALA production = ineffective erythropoiesis • Acquried – Refractory anemia with ringed sideroblasts – Caused by drugs and bone marrow toxins
Sideroblastic Anemia Laboratory Diagnosis • Microcytic, hypochromic anemia – Dimorphism – Pappenheimer bodies • • Splenomegaly Increased serum ferritin Increased protoporphyrin Increased serum iron
Hemochromatosis • Inheritied iron overloading – Increased iron absorption • Unbalanced iron absorption and storage – Deposits in organs • Liver, spleen, pancreas; can lead to fibrosis • Acquired (increased transfusions) or hereditary (HFE mutation) • Hyperpigmented skin • Therapy: – Therapeutic phlebotomy – Chelation
HH Symptions • Chronic fatigue and weakness • Cirrhosis of the liver • Hyperpigmentation • Diabetes • Impotence • Sterility • Cardiac arrhythmias • Tender, swollen joints • Hair loss • Abdominal symptoms
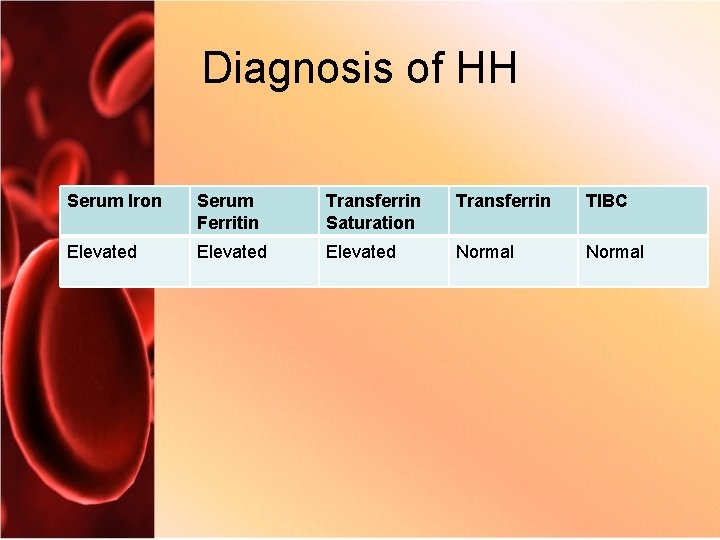
Diagnosis of HH Serum Iron Serum Ferritin Transferrin Saturation Transferrin TIBC Elevated Normal
Lead Poisoning • Interferes with porphyrin synthesis – ALA to porphobilingogen; ALA accumulates – Incorporating Fe into protoporphyrin ring; Fe and protoporphyrin accumulate • Basophilic stippling
Porpyrias • Impaired production of porphryin component of heme • Increased to excessive production of porphyrins – Leak out of cell and can accumulate in tissues (photosensitivity) or are excreted through urine/feces
- Slides: 29