Mitral Stenosis Cath Lab in the echo era
Mitral Stenosis Cath Lab – in the echo era André C. Lapeyre, III, M. D. Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Transthoracic echo is primary diagnostic modality • Transesophageal echo supplementary to TTE • Diagnostic catheterization – ACC/AHA* In those few patient with non-diagnostic studies or whose clinical and echocardiographic findings conflict, it is essential to further characterize MS with hemodynamics and catheterization as the next best approach. Catheterization is also the only method available to measure absolute pressures inside the heart, which may be important in clinical decision making. *Nishimura et al, JACC 2014 Vol 63(22); e 57 -e 185 Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Ideal – simultaneous left ventricle and left atrial pressures via transseptal catheterization. • Properly performed pulmonary wedge pressure may be acceptable substitute • Large bore, stiff catheter (or pressure wire) – end hole wedge • Confirmed full wedge with oxygen saturation • Properly corrected “phase delay” • Using PCWP will overestimate true transmitral gradient due to phase and pressure transmission delays. Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Properly corrected PCWP phase delay • Difficult to do properly • Always an approximation • Proximal wedge pressure using balloon catheter exaggerates the problems and errors • Correction should move the peak of the V wave in the PCWP to a point where the downstroke of the LV pressure decline bisects the V wave of the PCWP tracing. Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Ideally – Rhythm should be regular (if irregular or atrial fibrillation consider pacing to regularize rhythm – if rhythm can not be regularized then average gradient and filling period over at least 5 to 7 beats) – Cardiac output should be normal (if low output, consider ionotropic challenge) – Mean gradient should be 5 mm. Hg or more to reduce errors in the calculation of the valve area (if low gradient, especially with symptom mismatch, consider exercise or other maneuver to determine if the gradient increases) Andre Lapeyre, MD © Mayo Clinic
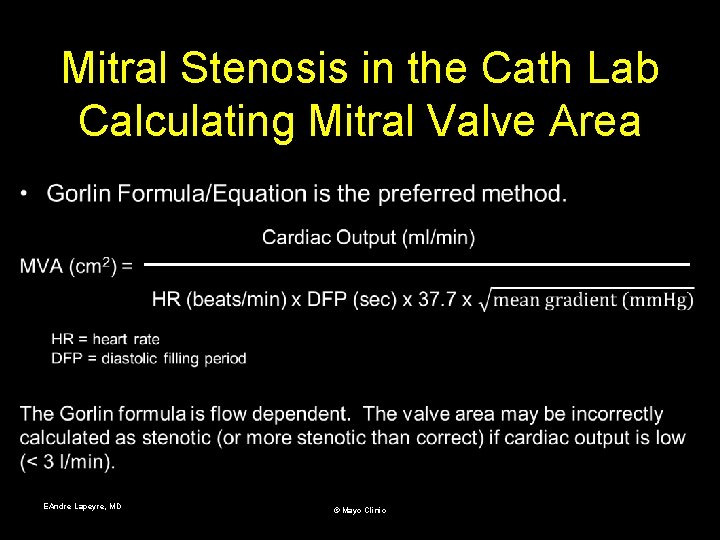
Mitral Stenosis in the Cath Lab Calculating Mitral Valve Area • EAndre Lapeyre, MD © Mayo Clinic
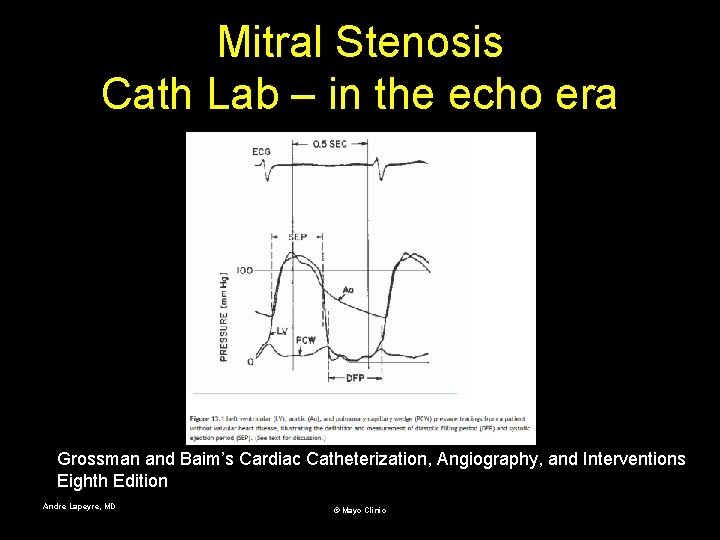
Mitral Stenosis Cath Lab – in the echo era Grossman and Baim’s Cardiac Catheterization, Angiography, and Interventions Eighth Edition Andre Lapeyre, MD © Mayo Clinic
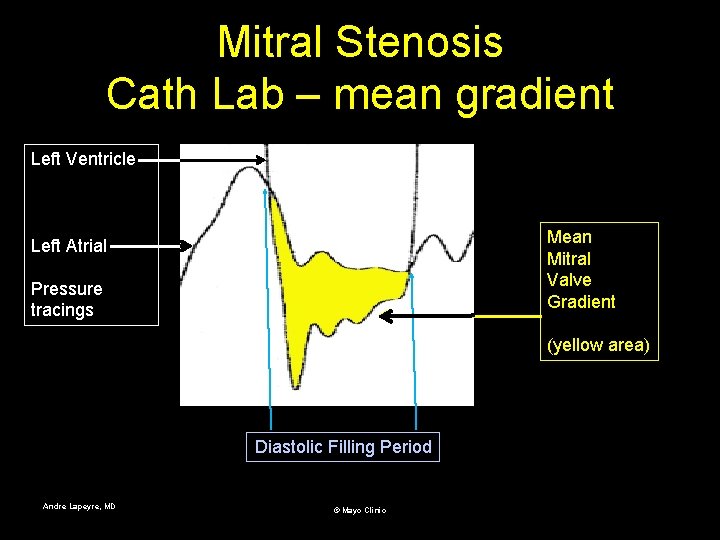
Mitral Stenosis Cath Lab – mean gradient Left Ventricle Mean Mitral Valve Gradient Left Atrial Pressure tracings (yellow area) Diastolic Filling Period Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Normal mitral valve – Area – 4 to 5 cm 2 – Mean gradient ≤ 1 mm. Hg Andre Lapeyre, MD © Mayo Clinic
Mitral Stenosis Cath Lab – in the echo era • Technical problems/errors • Using PCWP or poorly phase corrected PCWP (especially balloon wedge) • Partial wedge pressure (not properly confirmed with O 2 sat) • Catheters not properly equalized at zero pressure • Inaccuracies in determining cardiac output • Inaccuracies in measuring diastolic filling period (see Grossman text discussion “early diastasis”) • Severe aortic insufficiency reducing the measured diastolic gradient (also pigtail catheter with some side holes above the aortic valve leaflets or inducing aortic regurgitation) • Severe mitral regurgitation increasing the measured diastolic gradient Andre Lapeyre, MD © Mayo Clinic
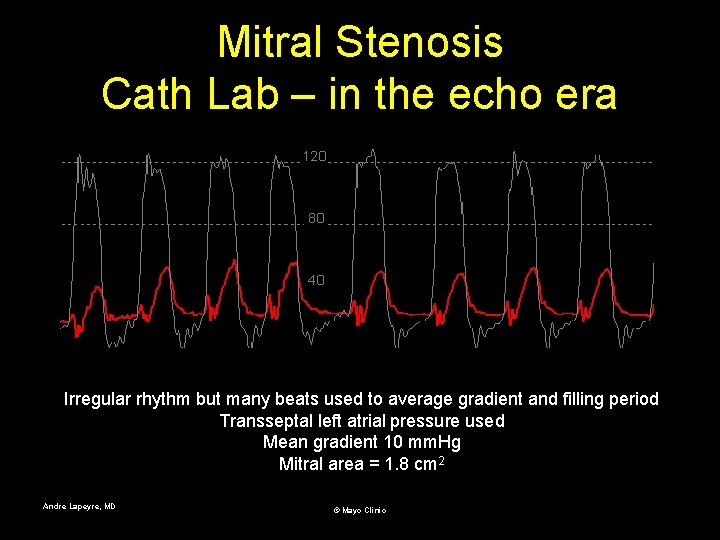
Mitral Stenosis Cath Lab – in the echo era Irregular rhythm but many beats used to average gradient and filling period Transseptal left atrial pressure used Mean gradient 10 mm. Hg Mitral area = 1. 8 cm 2 Andre Lapeyre, MD © Mayo Clinic
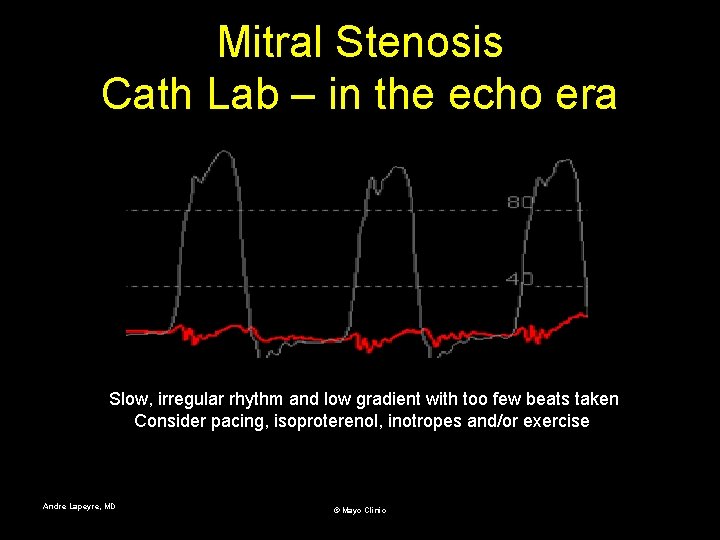
Mitral Stenosis Cath Lab – in the echo era Slow, irregular rhythm and low gradient with too few beats taken Consider pacing, isoproterenol, inotropes and/or exercise Andre Lapeyre, MD © Mayo Clinic
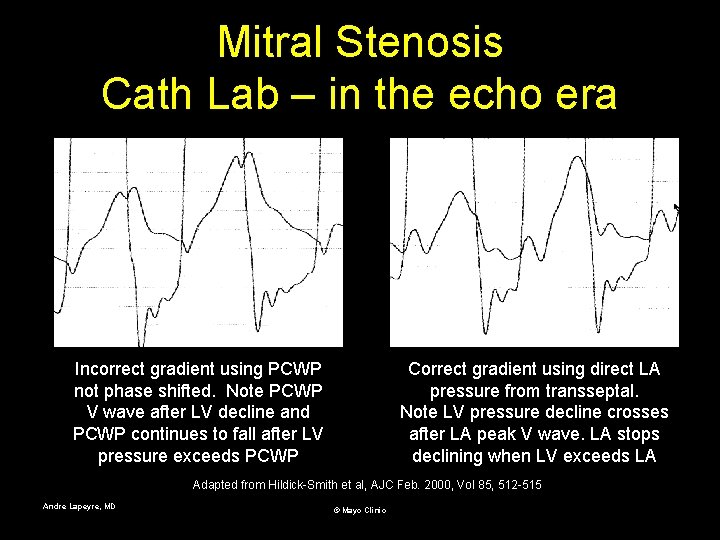
Mitral Stenosis Cath Lab – in the echo era Incorrect gradient using PCWP not phase shifted. Note PCWP V wave after LV decline and PCWP continues to fall after LV pressure exceeds PCWP Correct gradient using direct LA pressure from transseptal. Note LV pressure decline crosses after LA peak V wave. LA stops declining when LV exceeds LA Adapted from Hildick-Smith et al, AJC Feb. 2000, Vol 85, 512 -515 Andre Lapeyre, MD © Mayo Clinic
- End of this slide set - Andre Lapeyre, MD © Mayo Clinic
- Slides: 14