Miscellaneous Endocrine Addisons Addisons disease Adrenal hypofunction or






- Slides: 23
Miscellaneous Endocrine Addisons
Addison’s disease Adrenal hypofunction or adrenal insufficiency Two forms Primary Secondary Can progress to adrenal crisis Produce Aldosterone and Cortisol
Primary Addison’s Cause is in the adrenal glands themselves Usually symptoms are noted when 90% of gland is destroyed Autoimmune process Other causes of primary: TB Bilateral adrenalectomy Hemorrhage into the adrenal glands Neoplasms Infections
Secondary Addison’s Cause lies outside the adrenal glands Pituitary gland malfunction Decreased secretion of ACTH Abrupt steroid withdrawal Removal of a corticotropin-secreting tumor
Adrenal Crisis Gradual or sudden decrease in the amount of circulating aldosterone and cortisol

Risk Factors Pt who don’t respond to hormone replacement therapy Undergo extreme stress without adequate glucocorticoid replacement Abruptly stop hormone therapy Undergo trauma Undergo bilateral adrenalectomy Develop adrenal gland thrombosis after a severe infection
What Happens Destruction of the adrenal cortex leads to a rapid decline in the steroid hormones cortisol and aldosterone This directly affects the liver, stomach, and kidney
Absent or very low aldosterone Kidneys Sodium and water loss with potassium retention Heart Arrhythmias and decreased cardiac output Problems in one or both of these systems can lead to Hypovolemia and hypotension Shock Coma and death
Absent or very low Cortisol Stomach Decrease in digestive enzymes Vomiting, cramps, diarrhea Leads you down the hypovolemia/shock/coma pathway Liver Decrease in hepatic glucose output Hypoglycemia Profound hypoglycemia leading to coma and brain death Brain is the only organ that absolutely need glucose for metabolism
Addison’s crisis-signs and symptoms Profound hypotension Dehydration Profound weakness and fatigue Nausea & vomiting Hypoglycemia Neurologic changes Hyperkalemia Hyponatremia Hypercalcemia Tachycardia
Diagnostics Plasma cortisol is decreased Serum sodium and fasting blood glucose levels are decreased Corticotropin is increased Serum potassium level is increased Serum BUN level is increased Radiologic tests can identify adrenal gland size and level of calcification
Treatment Prompt IV Bolus of 100 mg of hydrocortisone Hydrocortisone diluted with normal saline with added electrolytes given as an IV infusion until the patient’s condition stabilizes
Further treatment may include Aggressive fluid replacement with up to 5 liters of saline with electrolyte replacement such as sodium and potassium Vasopressors such as epinephrine or norepinephrine Blood glucose management with IV dextrose solution Maintenance corticosteroid replacement the patient’s condition is stable

Myxedema coma Life-threatening disorder that progresses from hypothyroidism

What causes it Can result from either primary or secondary hypothyroidism Usually progresses slowly and gradually Can develop abruptly if stress aggravates severe or prolonged hypothyroidism Usually precipitated by infection, exposure to cold, or central nervous system depressants or anesthetics Cellular metabolism decreases to a fatal level if the patient with myxedema coma is left untreated
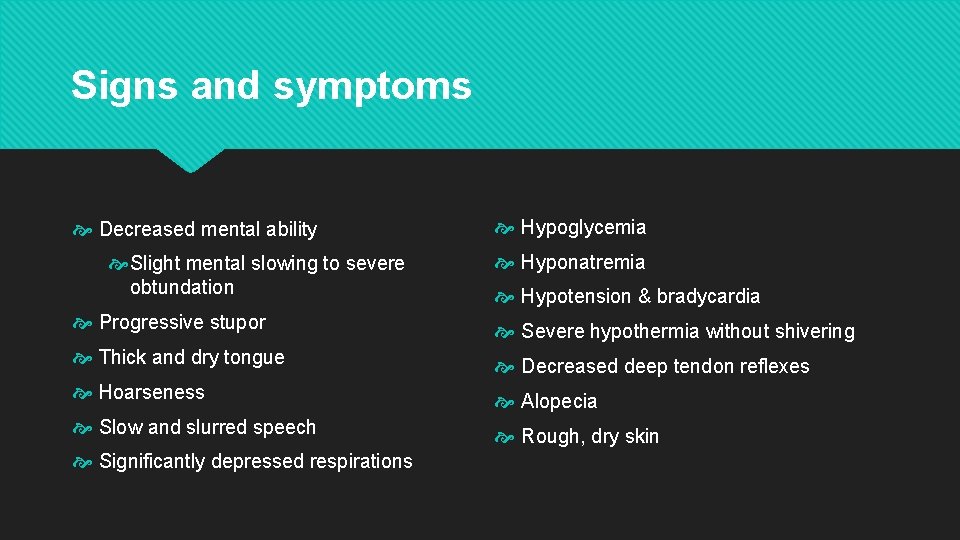
Signs and symptoms Decreased mental ability Slight mental slowing to severe obtundation Hypoglycemia Hyponatremia Hypotension & bradycardia Progressive stupor Severe hypothermia without shivering Thick and dry tongue Decreased deep tendon reflexes Hoarseness Alopecia Slow and slurred speech Rough, dry skin Significantly depressed respirations

Diagnostics T 3 and T 4 levels are decreased Serum levels of TSH are increased Radioactive iodine testing reveals low serum levels of thyroid hormones Radioisotope scanning of thyroid tissue is used to identify ectopic thyroid tissue CT, MRI, or skull X-ray may disclose an underlying cause such as pituitary or hypothalamic lesions Chest X-ray may show pleural effusion

Treatment Administration of IV hydrocortisone and IV levothyroxine Possible ventilatory support IV fluid replacement Warming devices
Thyroid Storm Life-threatening emergency in a patient with hyperthyroidism
What causes it The onset is almost always abrupt and evoked by a stressful event such as trauma, surgery, or infection Not-so-common causes Metastatic carcinoma of the thyroid Pituitary tumor secreting TSH DKA Poor compliance with anti-thyroid therapy
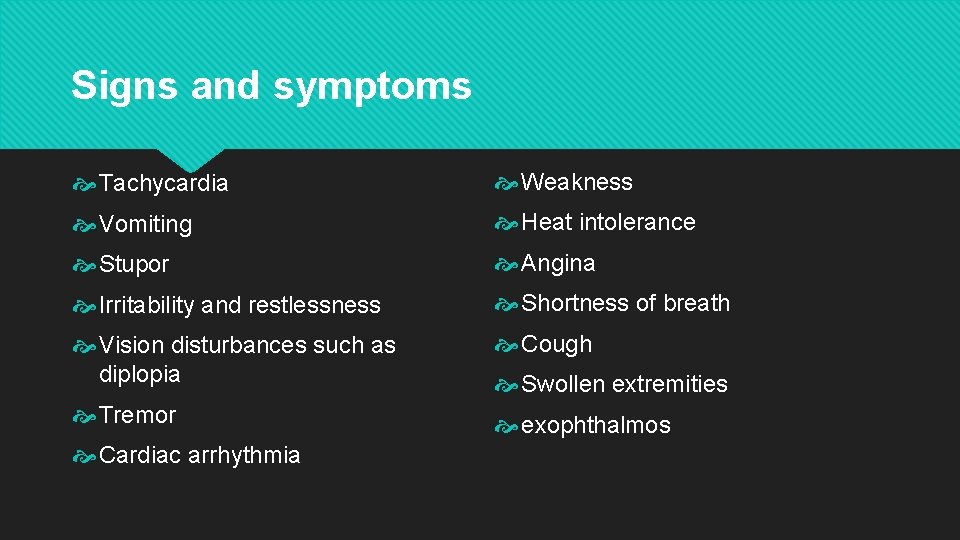
Signs and symptoms Tachycardia Weakness Vomiting Heat intolerance Stupor Angina Irritability and restlessness Shortness of breath Vision disturbances such as diplopia Cough Tremor exophthalmos Cardiac arrhythmia Swollen extremities
Diagnostics Serum T 3 and T 4 levels are elevated TSH level is decreased Radioisotope scanning shows increased uptake CT scan or MRI may disclose an underlying cause such as pituitary lesion 12 lead ECG may show supraventricular tachycardia and premature atrial and ventricular contractions

Treatment-immediate treatment is necessary to prevent death Beta blockers to block adrenergic effects Propylthiouracil and methimazole to block thyroid hormone synthesis Possible corticosteroid administration to block conversion of T 3 & T 4 Cooling measures such as use of a hyperthermia-hypothermia blanket