Mini Case Study Samantha Walters Sodexo MidAtlantic Dietetic

- Slides: 21
Mini Case Study Samantha Walters Sodexo Mid-Atlantic Dietetic Intern
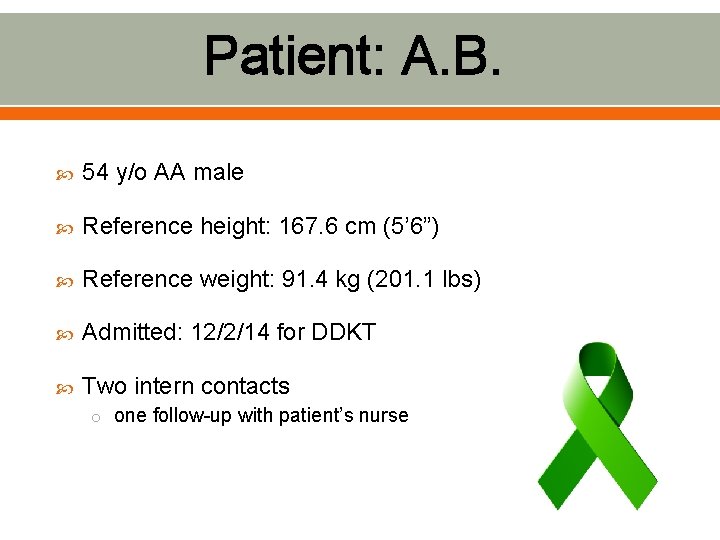
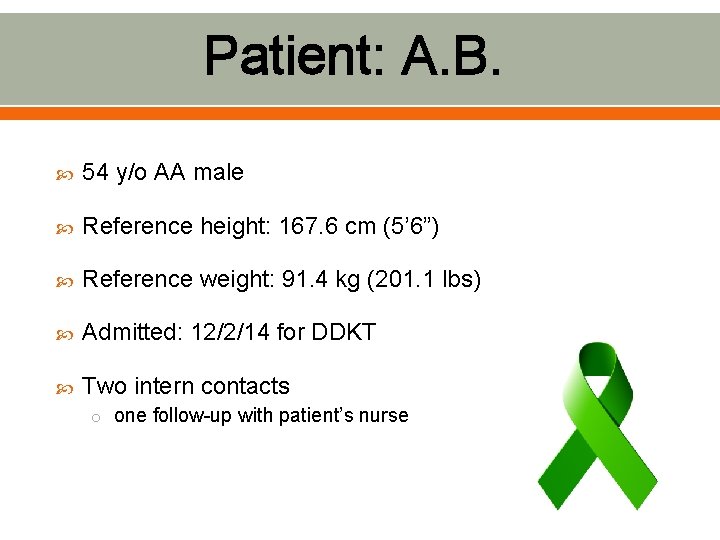
Patient: A. B. 54 y/o AA male Reference height: 167. 6 cm (5’ 6”) Reference weight: 91. 4 kg (201. 1 lbs) Admitted: 12/2/14 for DDKT Two intern contacts o one follow-up with patient’s nurse
Family/Social Hx Patient is single and lives with his brother On disability, no longer working as a landscaper (left in 2008) Denies tobacco, Et. OH, and illicit drug use Family hx includes: • • older brother who was dx with Alport syndrome HTN CAD CA
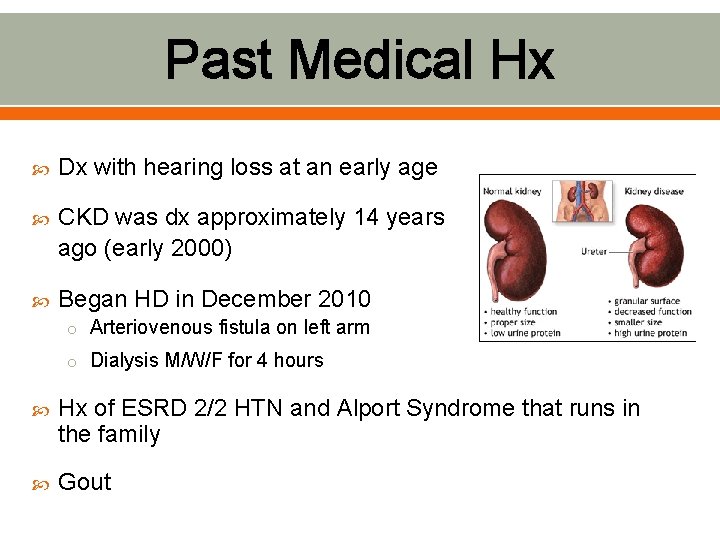
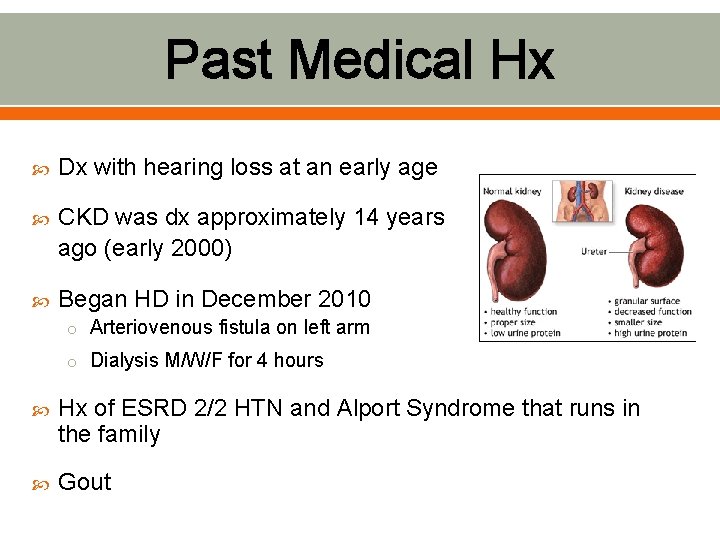
Past Medical Hx Dx with hearing loss at an early age CKD was dx approximately 14 years ago (early 2000) Began HD in December 2010 o Arteriovenous fistula on left arm o Dialysis M/W/F for 4 hours Hx of ESRD 2/2 HTN and Alport Syndrome that runs in the family Gout
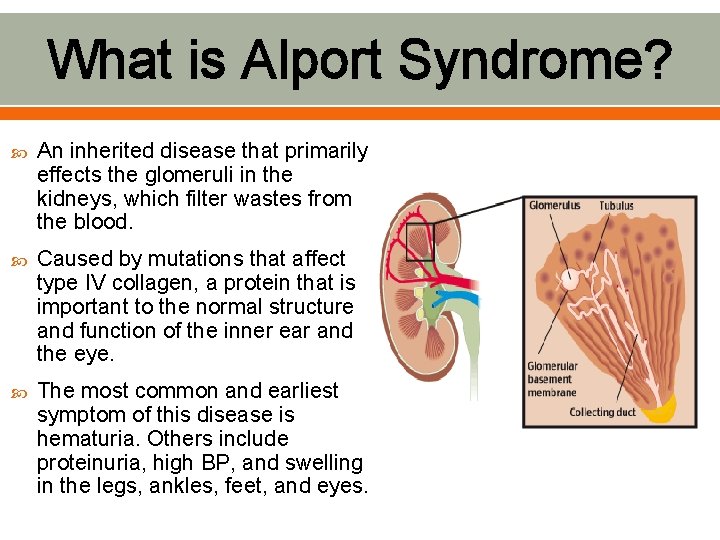
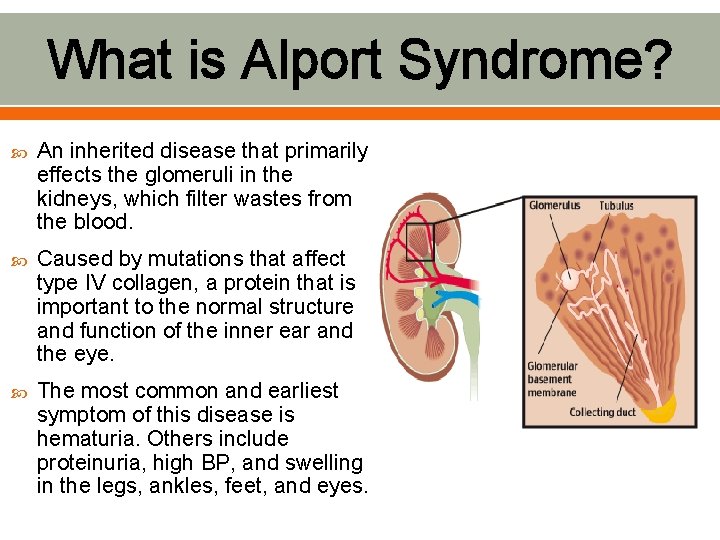
What is Alport Syndrome? An inherited disease that primarily effects the glomeruli in the kidneys, which filter wastes from the blood. Caused by mutations that affect type IV collagen, a protein that is important to the normal structure and function of the inner ear and the eye. The most common and earliest symptom of this disease is hematuria. Others include proteinuria, high BP, and swelling in the legs, ankles, feet, and eyes.
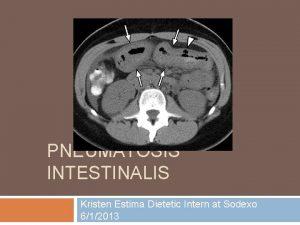
Hospital Course Operative Day: Admitted December 2 for deceased donor kidney transplant o Transplanted to right side o 22 y/o DCD with cause of death 2/2 MVA o High term Cr donor o 23 hours Cold Ischemia Time o Campath Induction
Hospital Course POD 1: Pt transferred from PACU to ZAYED 9 W Delayed Graft Function 2/2 minimal urine output (0 m. L) and K 6. 5 Received HD at beside Clinical Nutrition consult received for assessment and education Visited patient POD 1, and he was NPO. Observed HD and had nurse walk me through the process.
Delayed Graft Function Caused by issues between the donor or recipient Fairly common, occurring in about 30% of deceaseddonor kidneys and 5% of living-related kidneys Transplanted kidney is called a graft Occurs right after surgery and can take some time for the kidney to heal after transplant. Can take from weeks, even months for kidney to resume its normal functions Often times requires short-term HD in order to get it functioning properly
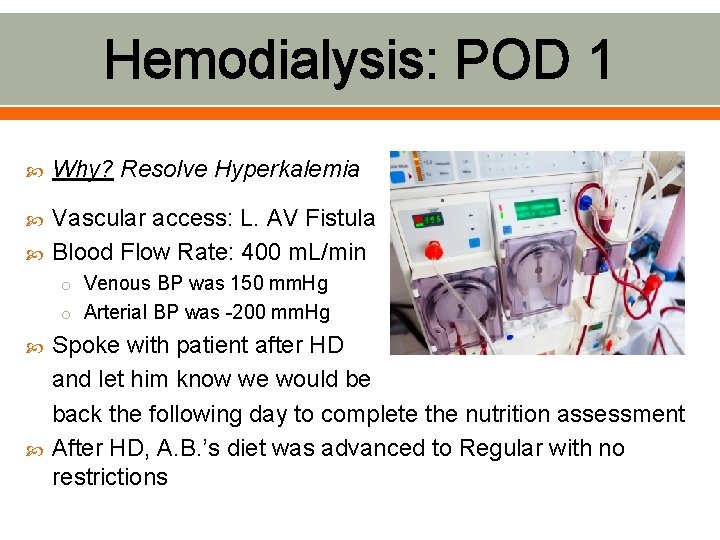
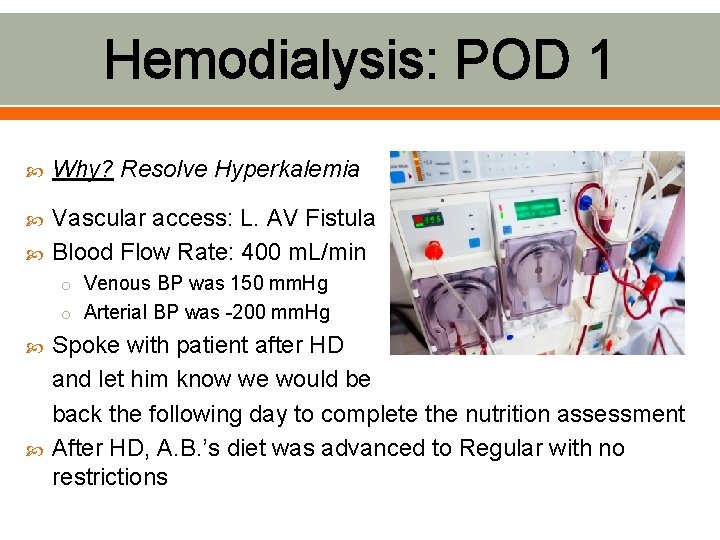
Hemodialysis: POD 1 Why? Resolve Hyperkalemia Vascular access: L. AV Fistula Blood Flow Rate: 400 m. L/min o Venous BP was 150 mm. Hg o Arterial BP was -200 mm. Hg Spoke with patient after HD and let him know we would be back the following day to complete the nutrition assessment After HD, A. B. ’s diet was advanced to Regular with no restrictions
Hospital Course POD 2: Patient still with minimal urine output (25 m. L over 24 hrs) Hyperkalemia resolved Patient seen for nutrition assessment and education s/p DDKT Significant Labs: • • • BUN: 42 (H) Cr: 10. 2 (H) Ca: 8. 1 (L) Phos: 5. 4 (H) DEXIS: 12/4— 161, 124 12/3— 124, 109. 99, 120, 131, 105
Noteworthy Medications Bisacodyl (Constipation) Docusate (stool softener) Pantoprazole (reflux common after transplant d/t meds— Prednisone especially) Senna (stool softener) Pravastatin (statin) MVI Insulin Sliding Scale
Immunosuppressants Cell. Cept (Mycophenolate Mofetil) o Inhibits enzyme needed for growth of T and B cells Prednisolone o Block the T cell activation/expression cascade WAS on Thymoglobulin POD 1 o Used immediately after transplant o Uses antibodies directed against T cell antigens, making T cells non-responsive Prograf (Tacrolimus) o Reduces interleukin 2 production by T cells o IL 2 responsible for regulation of WBCs
Nutrition Assessment Pt reports good appetite; no N/V/D/C or chewing/swallowing difficulties Generalized Edema States he still has little urine output and last BM was prior to transplant Recent estimated dry weight was 92. 8 kg CBW: 91. 4 kg UBW: 95. 5 kg (98. 5%) DBW: 64. 5 kg (142%)
Nutrition Assessment Estimated Needs: All needs based on DBW of 64. 5 kg: (KDIGO/KDOQI) -Kcal: 1950 -2300 kcal/day (30 -35 kcal/kg) -Protein: 85 -95 gm/day (1. 3 -1. 5 gm/kg) -Fluid: No restriction, per team
Nutrition Diagnosis Increased nutrient needs (NI 5. 1) (calories, protein) related to wound healing as evidenced by s/p kidney transplant and catabolic effect of steroids Food and nutrition-related knowledge deficit (NB 1. 1) related to limited post-transplant diet education as evidenced by s/t DDKT on 12/2/2014
Nutrition Education Provided NCM: Post-Transplant Nutrition Therapy Handout Post Kidney Transplant Diet Recommendations: o Heart-Healthy diet o Avoid concentrated sweets/moderate CHO diet o Food Safety • • • Check expiration dates Thaw foods properly Cook/Chill foods thoroughly Wash all fruits/vegetables Heat cold cuts, hot dogs, deli meats, and sausages to steaming before eating • Avoid grapefruit, raw meats, unpasteurized dairy/juice/cider, fresh sprouts, moldy foods, and alcohol
Recommendations Continue Regular Diet with no restrictions as tolerated Continue vitamin/mineral supplement QD Suggest checking Vitamin D and supplement if low Continue to monitor renal labs and checking DEXIS to monitor BG response to steroids Pt encouraged to contact RD with questions/concerns regarding diet – Provided with RD contact information Will f/u per standards of care
Follow-up POD 3: Was given Lasix overnight with no response (15 m. L urine output all night) 5 m. L total POD 3, and given 100 mg Lasix again today Removing Foley later today HD later today d/t labs not trending per note: • • Cr: 13. 1 (H) BUN: 71 (H) Ca: 7. 9 (L) Phos: 6. 8 (H)
References NCM: Organ Transplant Nutrition Therapy National Kidney Foundation. Pocket Guide to Nutrition Assessment of the Patient with Chronic Kidney Disease: A Concise, Practical Resource for Comprehensive Nutrition Care in CKD National Kidney Foundation (website) J. S. Gill, J. Lan, J. Dong, et al. The Survival Benefit of Kidney Transplantation in Obese Patients. American Journal of Transplantation 2013; 13: 2083 -2090. Chitra U and Sunitha Premalatha K. Nutritional Management of Renal Transplant Patients. Indian Journal of Transplantation 2013; 7(3): 88 -93
Questions?

 Sodexo dietetic internship acceptance rate
Sodexo dietetic internship acceptance rate Sodexo distance dietetic internship
Sodexo distance dietetic internship Lower south colonies
Lower south colonies Mini case study example
Mini case study example Estrategia maxi maxi
Estrategia maxi maxi Fo maxi maxi
Fo maxi maxi Analisis foda maxi mini ejemplos
Analisis foda maxi mini ejemplos Best worst and average case
Best worst and average case Sodexo energie et maintenance
Sodexo energie et maintenance Vital pass sodexo
Vital pass sodexo Accounting for catering business
Accounting for catering business Cartes sodexo perdues
Cartes sodexo perdues Crm failure case study
Crm failure case study Wave by eric walters
Wave by eric walters Sandra walters pack
Sandra walters pack Bookish crickhowell
Bookish crickhowell Walters perennials
Walters perennials Walter formula for dividend policy
Walter formula for dividend policy Discussion questions for to kill a mockingbird chapters 1-3
Discussion questions for to kill a mockingbird chapters 1-3 Robb walters
Robb walters Walters restaurant portland maine
Walters restaurant portland maine Dietetic support worker
Dietetic support worker