Midgut The derivatives of the midgut are The





- Slides: 22
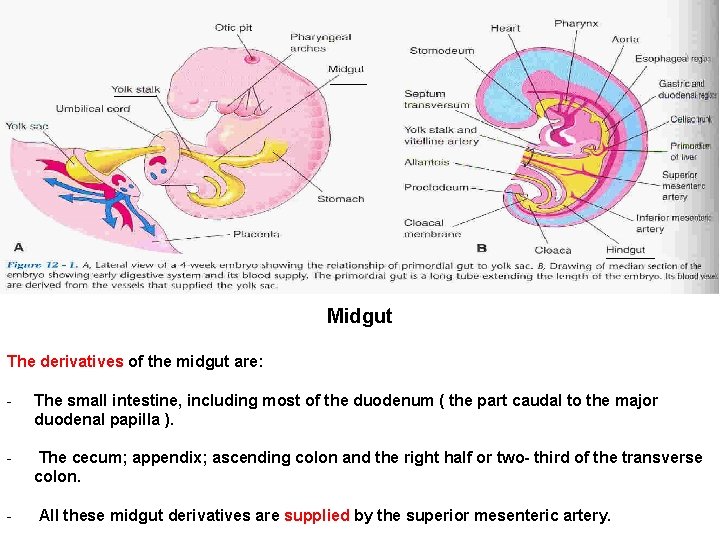
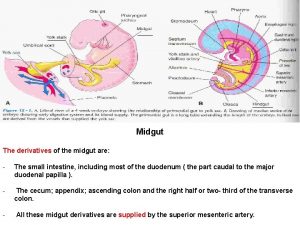
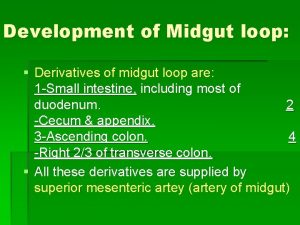
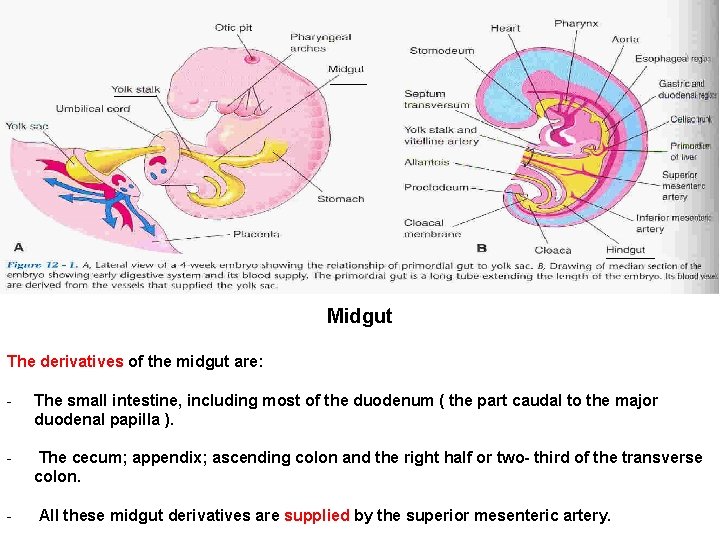
Midgut The derivatives of the midgut are: - The small intestine, including most of the duodenum ( the part caudal to the major duodenal papilla ). - The cecum; appendix; ascending colon and the right half or two- third of the transverse colon. - All these midgut derivatives are supplied by the superior mesenteric artery.

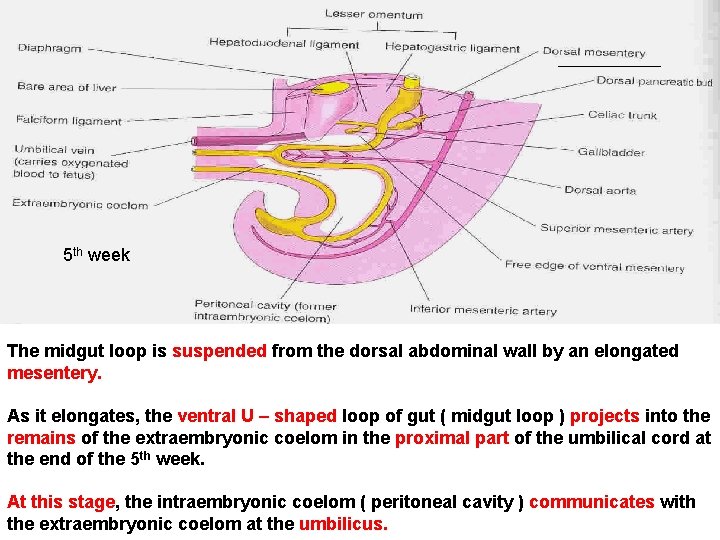
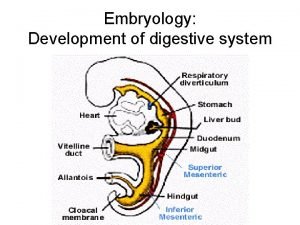
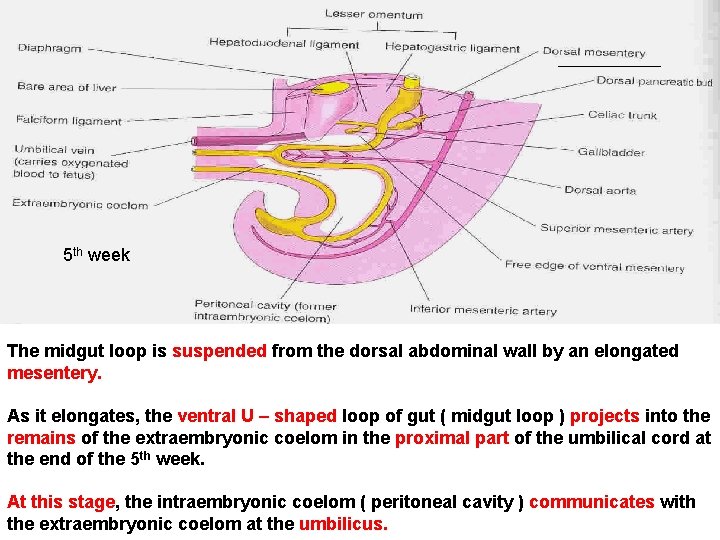
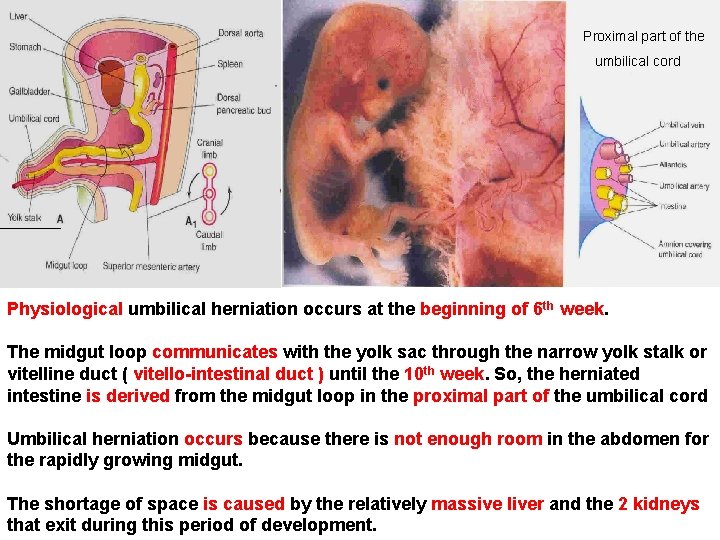
5 th week The midgut loop is suspended from the dorsal abdominal wall by an elongated mesentery. As it elongates, the ventral U – shaped loop of gut ( midgut loop ) projects into the remains of the extraembryonic coelom in the proximal part of the umbilical cord at the end of the 5 th week. At this stage, the intraembryonic coelom ( peritoneal cavity ) communicates with the extraembryonic coelom at the umbilicus.
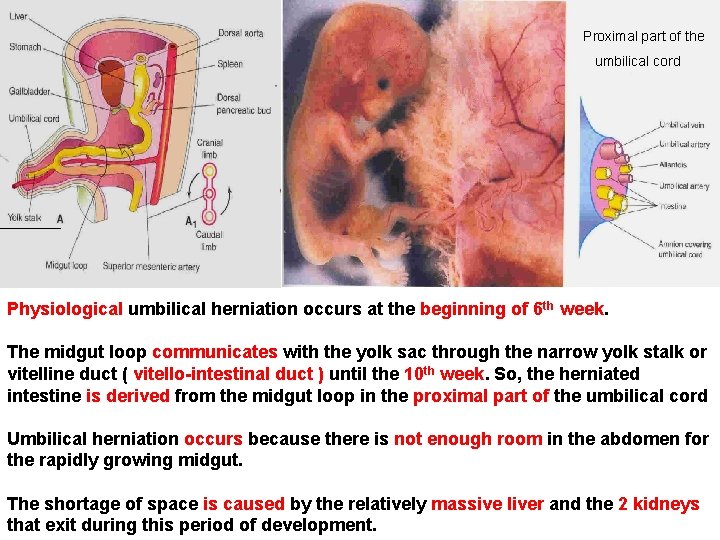
Proximal part of the umbilical cord Physiological umbilical herniation occurs at the beginning of 6 th week. The midgut loop communicates with the yolk sac through the narrow yolk stalk or vitelline duct ( vitello-intestinal duct ) until the 10 th week. So, the herniated intestine is derived from the midgut loop in the proximal part of the umbilical cord Umbilical herniation occurs because there is not enough room in the abdomen for the rapidly growing midgut. The shortage of space is caused by the relatively massive liver and the 2 kidneys that exit during this period of development.

10 week The midgut loop has a cranial limb and a caudal limb. The yolk stalk is attached to the apex of the midgut loop where the 2 limbs join. The cranial limb grows rapidly and forms small intestinal loops. The caudal limb undergoes very little change except for development of the cecal diverticulum ( the primordium of the cecum and appendix. Rotation of Midgut Loop While it is in the umbilical cord, the midgut loop rotates 90 degrees counterclockwise around the axis of the superior mesenteric artery and yolk stalk. This brings the cranial limb of the midgut loop to the right and the caudal limb to the left. During rotation the cranial limb elongates and forms jejunum & ileum ( intestinal loops ).
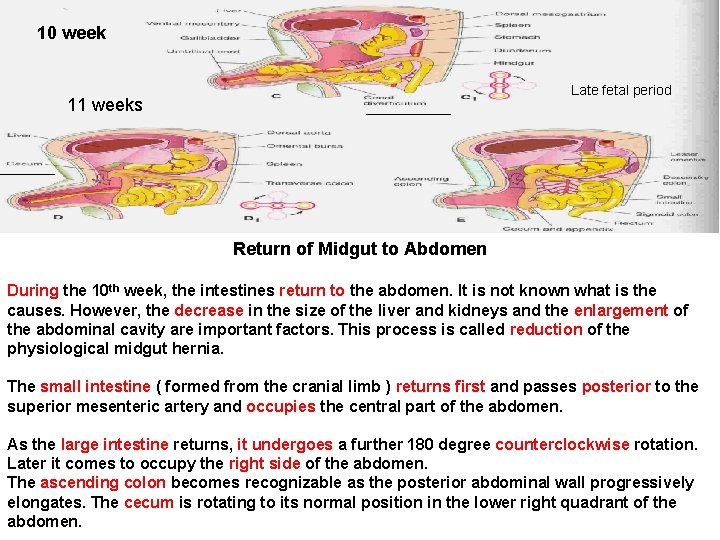
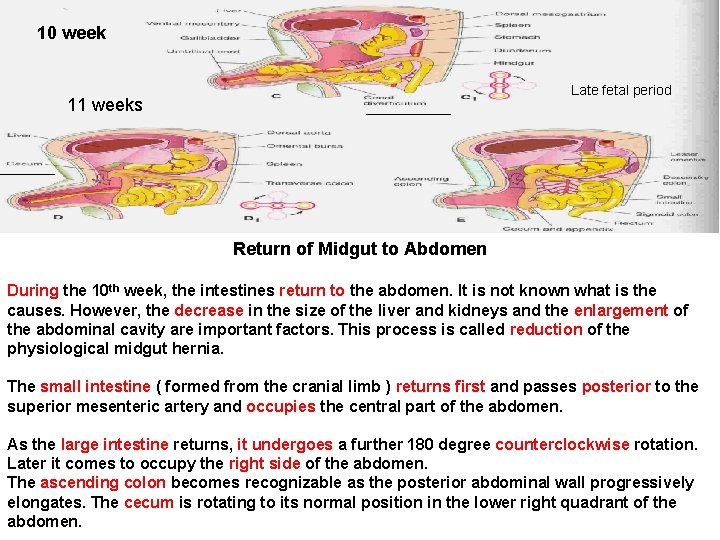
10 week Late fetal period 11 weeks Return of Midgut to Abdomen During the 10 th week, the intestines return to the abdomen. It is not known what is the causes. However, the decrease in the size of the liver and kidneys and the enlargement of the abdominal cavity are important factors. This process is called reduction of the physiological midgut hernia. The small intestine ( formed from the cranial limb ) returns first and passes posterior to the superior mesenteric artery and occupies the central part of the abdomen. As the large intestine returns, it undergoes a further 180 degree counterclockwise rotation. Later it comes to occupy the right side of the abdomen. The ascending colon becomes recognizable as the posterior abdominal wall progressively elongates. The cecum is rotating to its normal position in the lower right quadrant of the abdomen.
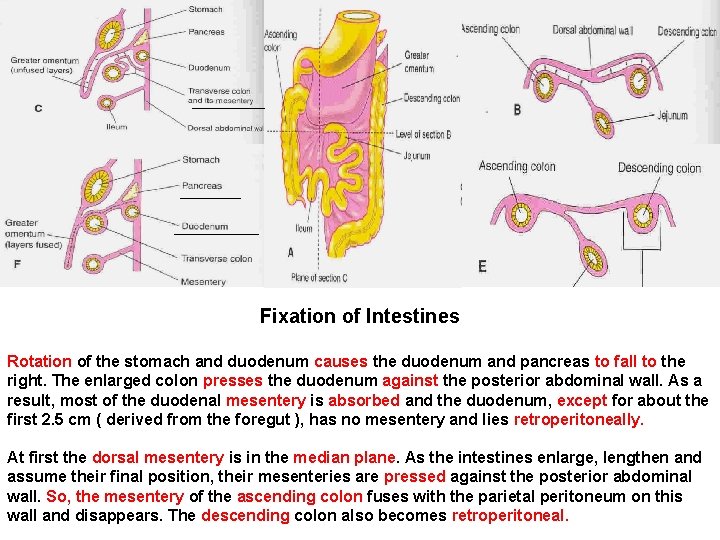
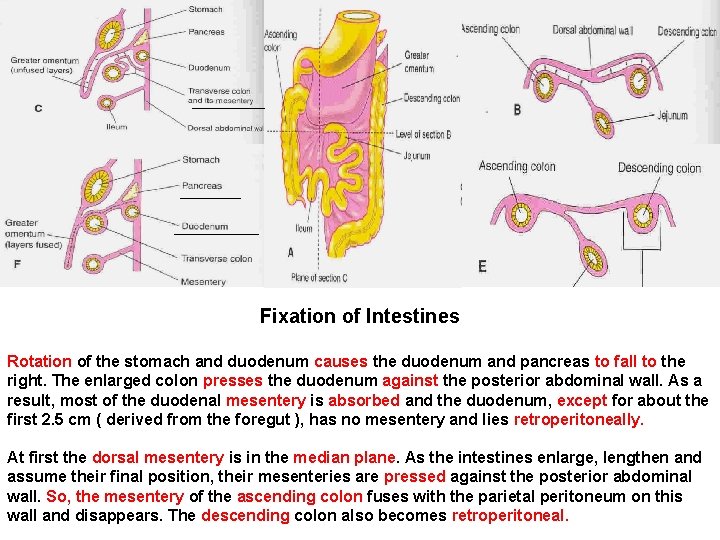
Fixation of Intestines Rotation of the stomach and duodenum causes the duodenum and pancreas to fall to the right. The enlarged colon presses the duodenum against the posterior abdominal wall. As a result, most of the duodenal mesentery is absorbed and the duodenum, except for about the first 2. 5 cm ( derived from the foregut ), has no mesentery and lies retroperitoneally. At first the dorsal mesentery is in the median plane. As the intestines enlarge, lengthen and assume their final position, their mesenteries are pressed against the posterior abdominal wall. So, the mesentery of the ascending colon fuses with the parietal peritoneum on this wall and disappears. The descending colon also becomes retroperitoneal.
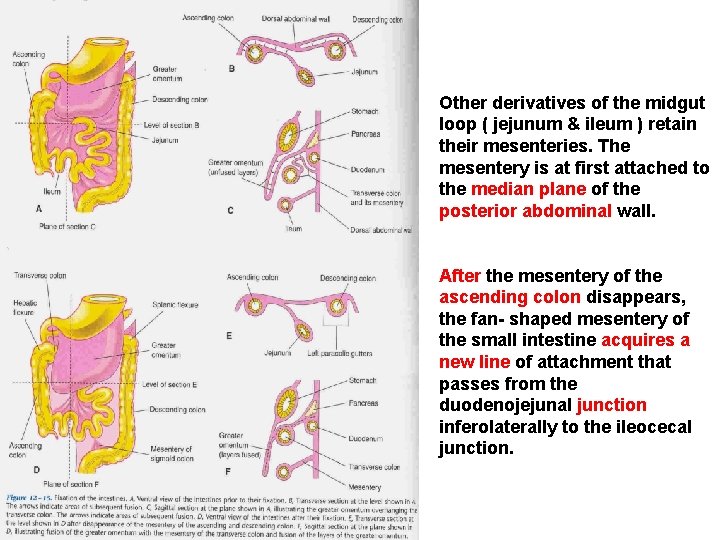
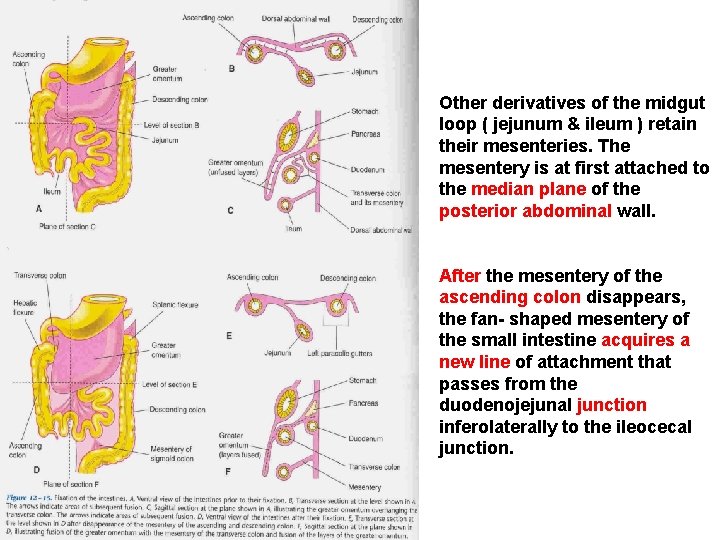
Other derivatives of the midgut loop ( jejunum & ileum ) retain their mesenteries. The mesentery is at first attached to the median plane of the posterior abdominal wall. After the mesentery of the ascending colon disappears, the fan- shaped mesentery of the small intestine acquires a new line of attachment that passes from the duodenojejunal junction inferolaterally to the ileocecal junction.
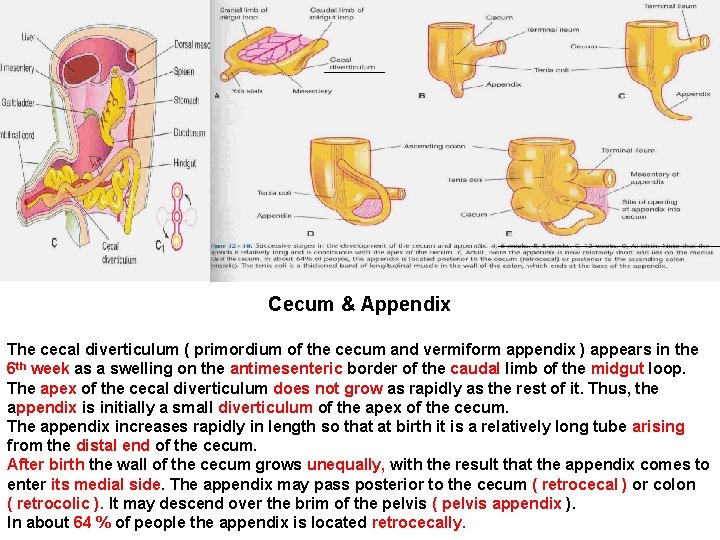
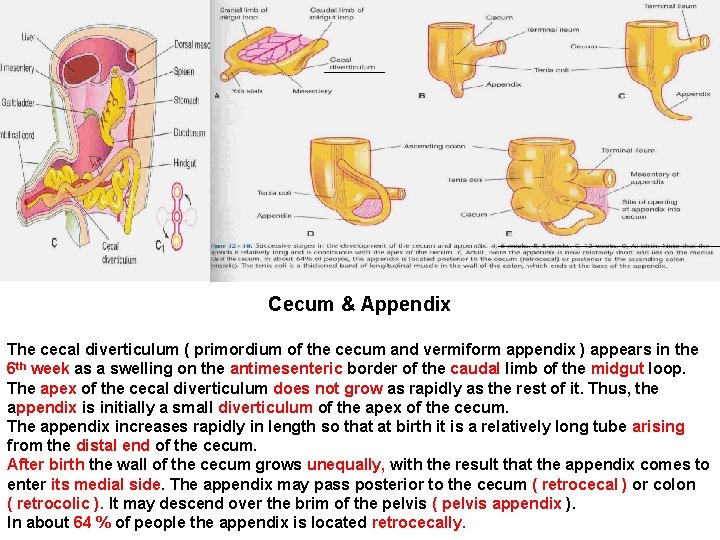
Cecum & Appendix The cecal diverticulum ( primordium of the cecum and vermiform appendix ) appears in the 6 th week as a swelling on the antimesenteric border of the caudal limb of the midgut loop. The apex of the cecal diverticulum does not grow as rapidly as the rest of it. Thus, the appendix is initially a small diverticulum of the apex of the cecum. The appendix increases rapidly in length so that at birth it is a relatively long tube arising from the distal end of the cecum. After birth the wall of the cecum grows unequally, with the result that the appendix comes to enter its medial side. The appendix may pass posterior to the cecum ( retrocecal ) or colon ( retrocolic ). It may descend over the brim of the pelvis ( pelvis appendix ). In about 64 % of people the appendix is located retrocecally.
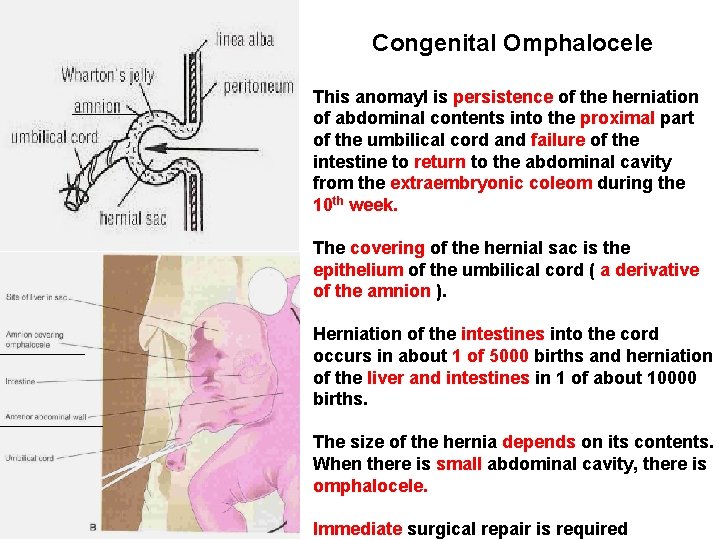
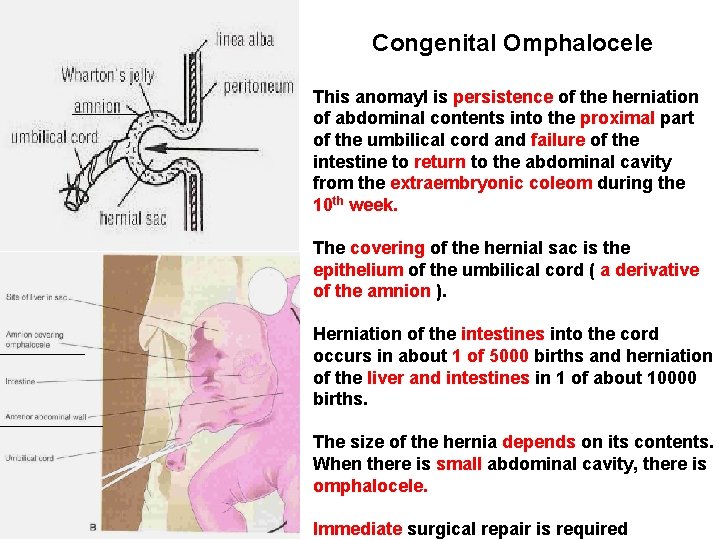
Congenital Omphalocele This anomayl is persistence of the herniation of abdominal contents into the proximal part of the umbilical cord and failure of the intestine to return to the abdominal cavity from the extraembryonic coleom during the 10 th week. The covering of the hernial sac is the epithelium of the umbilical cord ( a derivative of the amnion ). Herniation of the intestines into the cord occurs in about 1 of 5000 births and herniation of the liver and intestines in 1 of about 10000 births. The size of the hernia depends on its contents. When there is small abdominal cavity, there is omphalocele. Immediate surgical repair is required

Umbilical hernia During the 10 th week the intestine return to the abdominal cavity and then herniate through an imperfectly closed umbilicus. It is common. The protruding mass is usually the greater omentum and small intestine. It covered by subcutaneous tissue and skin. It usually does not reach its maximum size until the end of the 1 st month after birth. It usually ranges from 1 to 5 cm. The defect through which the hernia occurs is the linea alba. The protrudes during crying; straining or coughing and can be easily reduced through the fibrous ring at the umbilicus. Surgery is not persists to the age of 3 to 5 years.
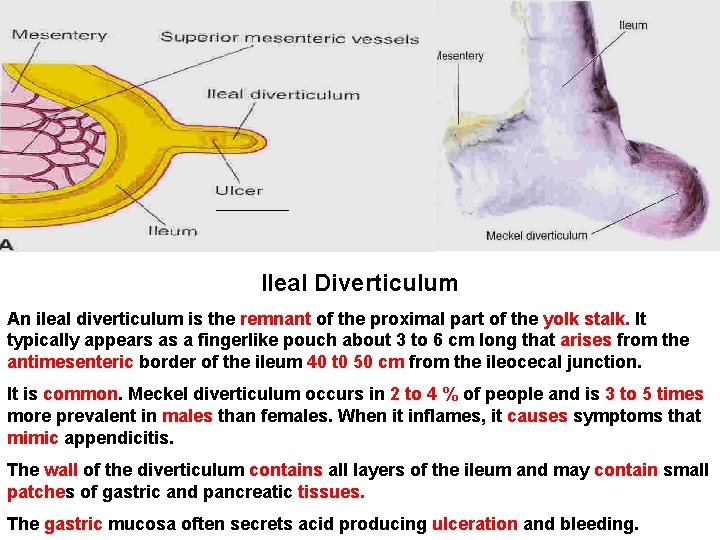
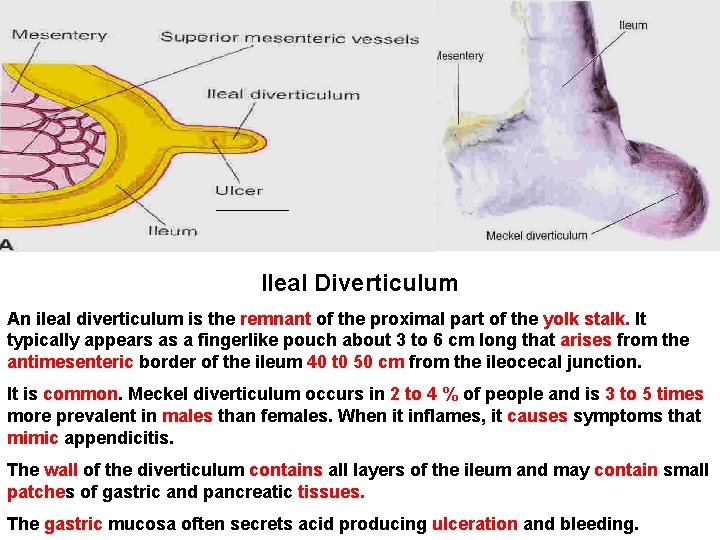
Ileal Diverticulum An ileal diverticulum is the remnant of the proximal part of the yolk stalk. It typically appears as a fingerlike pouch about 3 to 6 cm long that arises from the antimesenteric border of the ileum 40 t 0 50 cm from the ileocecal junction. It is common. Meckel diverticulum occurs in 2 to 4 % of people and is 3 to 5 times more prevalent in males than females. When it inflames, it causes symptoms that mimic appendicitis. The wall of the diverticulum contains all layers of the ileum and may contain small patches of gastric and pancreatic tissues. The gastric mucosa often secrets acid producing ulceration and bleeding.
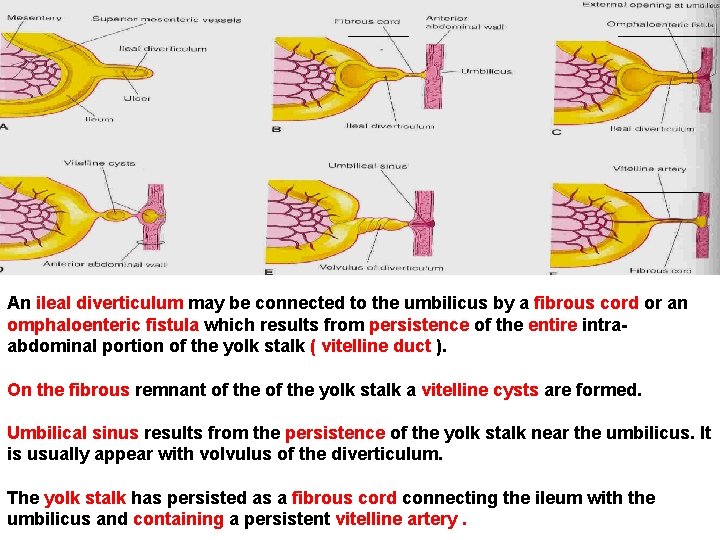
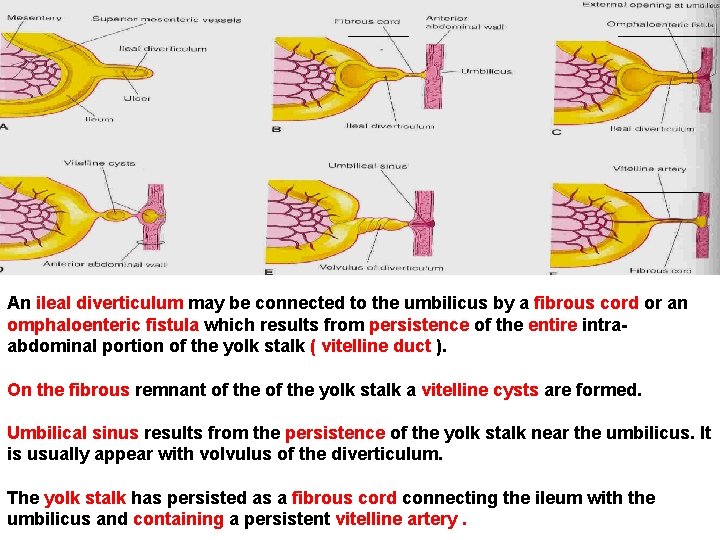
An ileal diverticulum may be connected to the umbilicus by a fibrous cord or an omphaloenteric fistula which results from persistence of the entire intraabdominal portion of the yolk stalk ( vitelline duct ). On the fibrous remnant of the yolk stalk a vitelline cysts are formed. Umbilical sinus results from the persistence of the yolk stalk near the umbilicus. It is usually appear with volvulus of the diverticulum. The yolk stalk has persisted as a fibrous cord connecting the ileum with the umbilicus and containing a persistent vitelline artery.
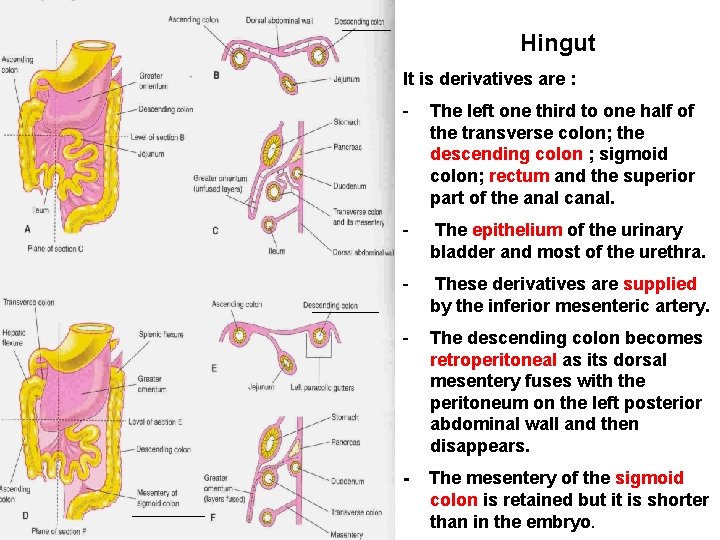
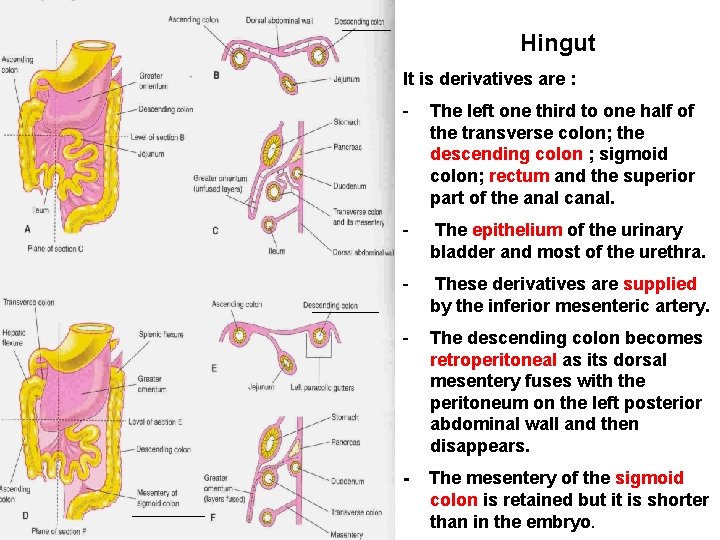
Hingut It is derivatives are : - The left one third to one half of the transverse colon; the descending colon ; sigmoid colon; rectum and the superior part of the anal canal. - The epithelium of the urinary bladder and most of the urethra. - These derivatives are supplied by the inferior mesenteric artery. - The descending colon becomes retroperitoneal as its dorsal mesentery fuses with the peritoneum on the left posterior abdominal wall and then disappears. - The mesentery of the sigmoid colon is retained but it is shorter than in the embryo.
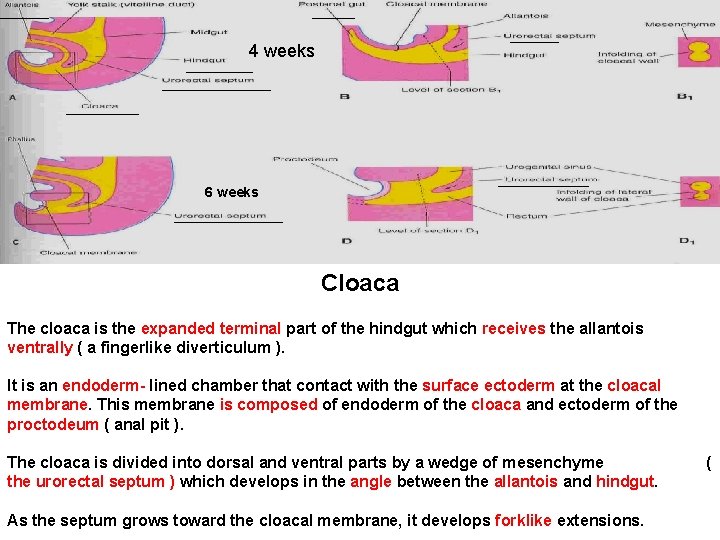
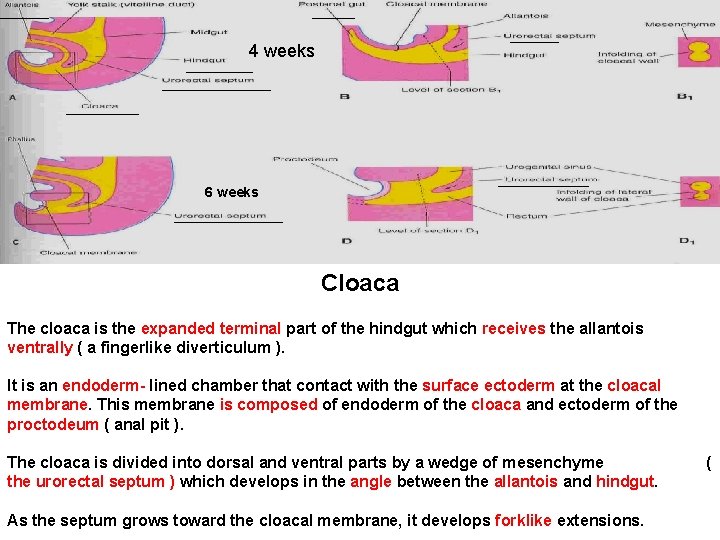
4 weeks 6 weeks Cloaca The cloaca is the expanded terminal part of the hindgut which receives the allantois ventrally ( a fingerlike diverticulum ). It is an endoderm- lined chamber that contact with the surface ectoderm at the cloacal membrane. This membrane is composed of endoderm of the cloaca and ectoderm of the proctodeum ( anal pit ). The cloaca is divided into dorsal and ventral parts by a wedge of mesenchyme the urorectal septum ) which develops in the angle between the allantois and hindgut. As the septum grows toward the cloacal membrane, it develops forklike extensions. (

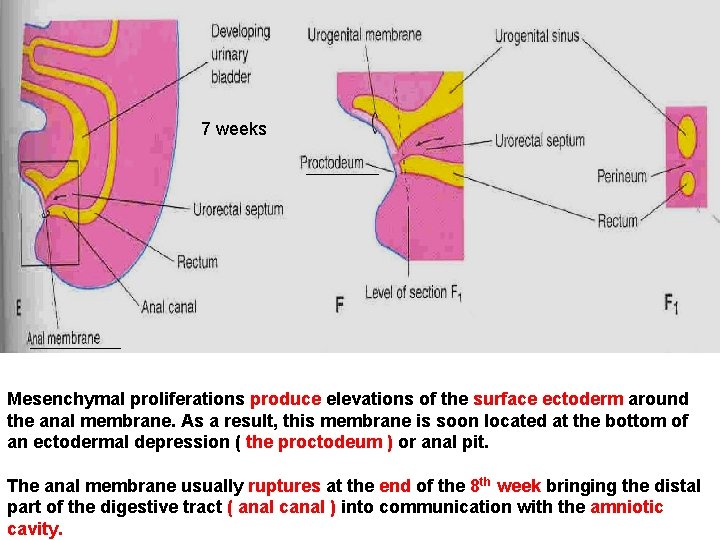
7 weeks The 2 parts are : A- Rectum and cranial part of the anal canal dorsally. B- Urogenital sinus ventrally. The postanal or tailgut degenerates and disappears as the rectum is formed. By the 7 th week, the urorectal septum has fused with the cloacal membrane, dividing it into a dorsal anal membrane and a larger ventral urogenital membrane. The area of fusion of the urorectal septum with the cloacal membrane is represented in the adult by the perineal body ( the tendinous center of the perineum ). The urorectal septum also, divides the cloacal sphincter into anterior & posterior parts. The posterior part becomes the external anal sphincter and the anterior part develops into the superficial transverse perineal ( bulbospongiosus and ischiocavernosus ) muscles. This developmental fact explains why one nerve ( pudendal nerve ) supplies all these muscles.
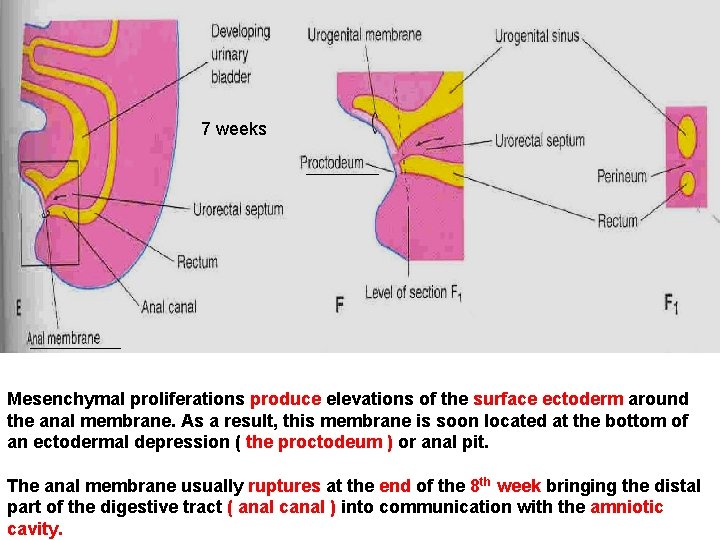
7 weeks Mesenchymal proliferations produce elevations of the surface ectoderm around the anal membrane. As a result, this membrane is soon located at the bottom of an ectodermal depression ( the proctodeum ) or anal pit. The anal membrane usually ruptures at the end of the 8 th week bringing the distal part of the digestive tract ( anal canal ) into communication with the amniotic cavity.
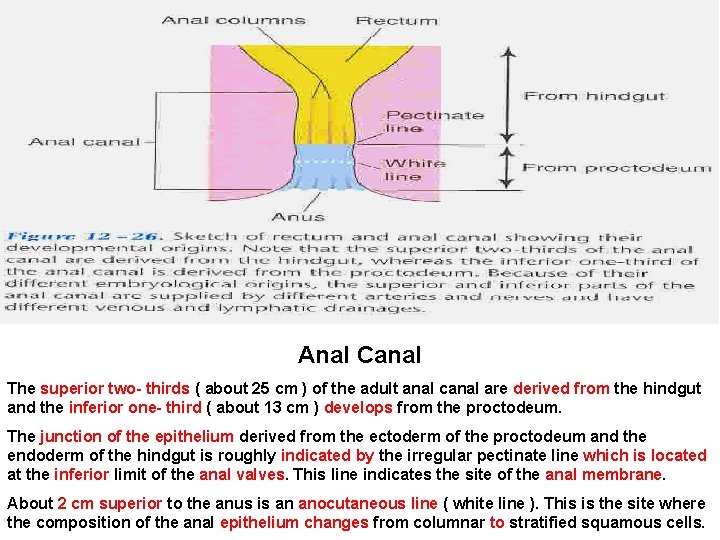
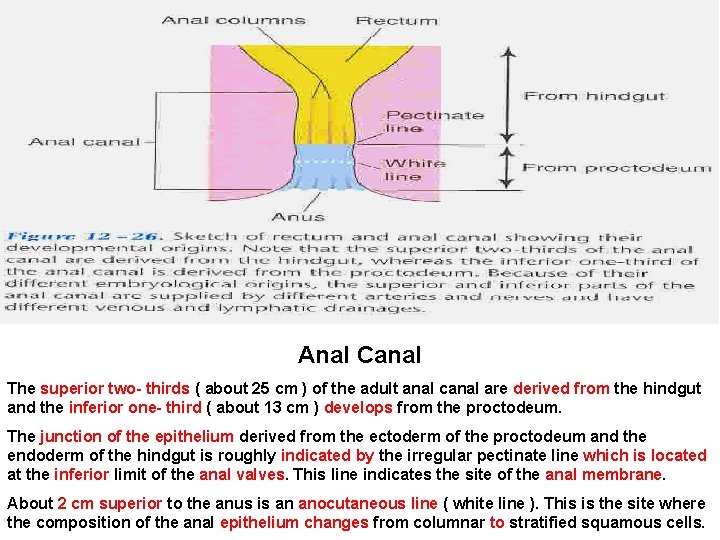
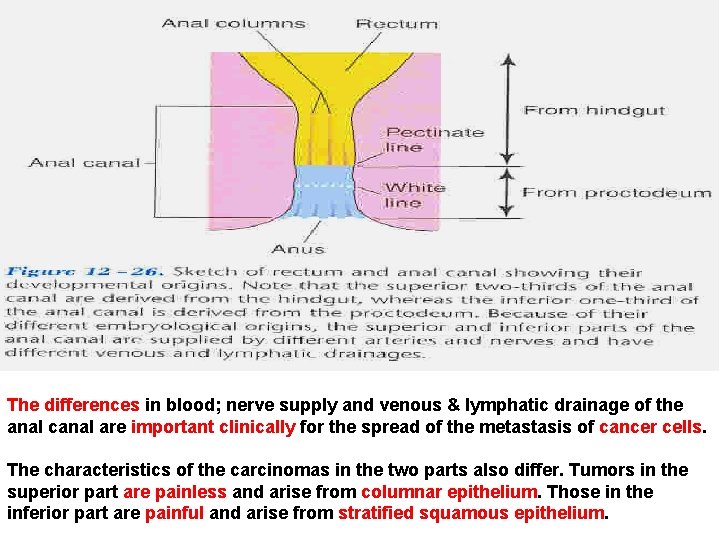
Anal Canal The superior two- thirds ( about 25 cm ) of the adult anal canal are derived from the hindgut and the inferior one- third ( about 13 cm ) develops from the proctodeum. The junction of the epithelium derived from the ectoderm of the proctodeum and the endoderm of the hindgut is roughly indicated by the irregular pectinate line which is located at the inferior limit of the anal valves. This line indicates the site of the anal membrane. About 2 cm superior to the anus is an anocutaneous line ( white line ). This is the site where the composition of the anal epithelium changes from columnar to stratified squamous cells.

At the anus, the epithelium is keratinized and continuous with the skin around the anus. The other layers of the wall of the anal canal are derived from splanchnic mesenchyme. Similar to the pyloric sphincter and the ileocecal valve ( sphincter ) the formation of the anal sphincter appears to be under genetic control. The lymphatic drainage of the superior part is to the inferior mesenteric lymph nodes. The lymphatic drainage of the inferior part of the anal canal is to the superficial inguinal lymph nodes. Its nerve supply is from the inferior rectal nerve, so, it is sensitive to pain; temperature; touch and pressure.
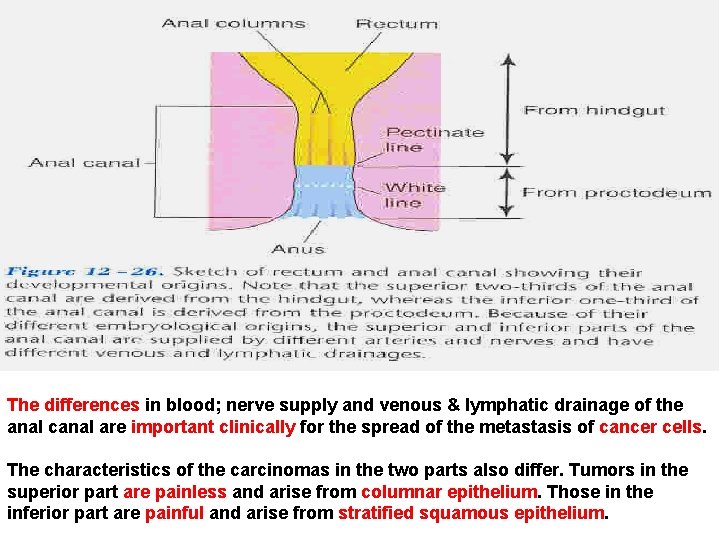
The differences in blood; nerve supply and venous & lymphatic drainage of the anal canal are important clinically for the spread of the metastasis of cancer cells. The characteristics of the carcinomas in the two parts also differ. Tumors in the superior part are painless and arise from columnar epithelium. Those in the inferior part are painful and arise from stratified squamous epithelium.
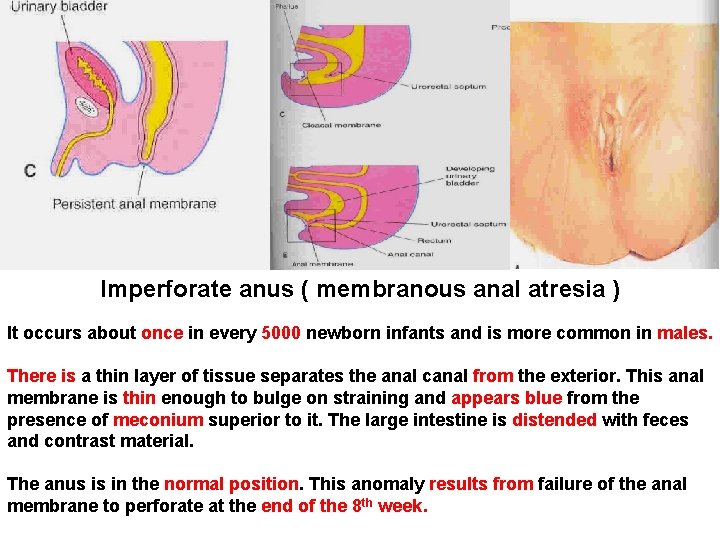
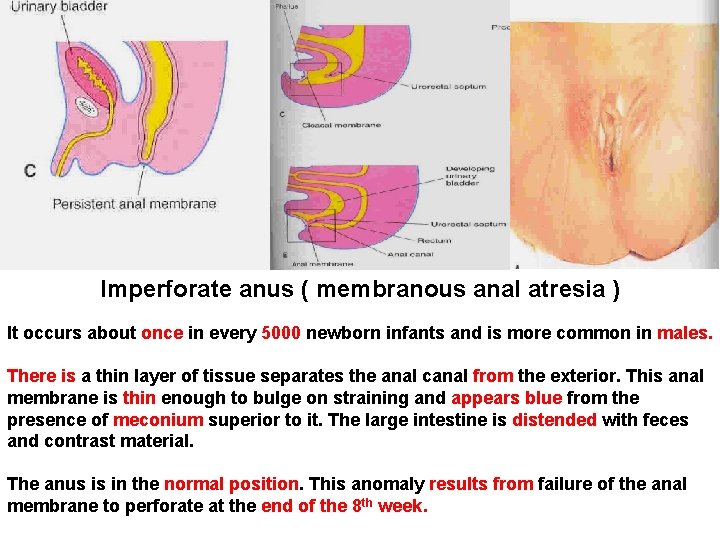
Imperforate anus ( membranous anal atresia ) It occurs about once in every 5000 newborn infants and is more common in males. There is a thin layer of tissue separates the anal canal from the exterior. This anal membrane is thin enough to bulge on straining and appears blue from the presence of meconium superior to it. The large intestine is distended with feces and contrast material. The anus is in the normal position. This anomaly results from failure of the anal membrane to perforate at the end of the 8 th week.
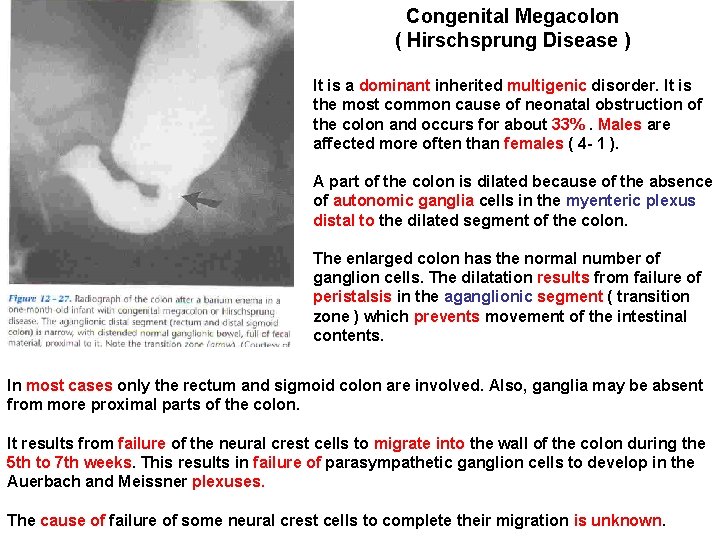
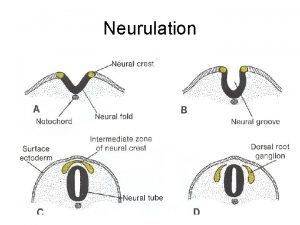
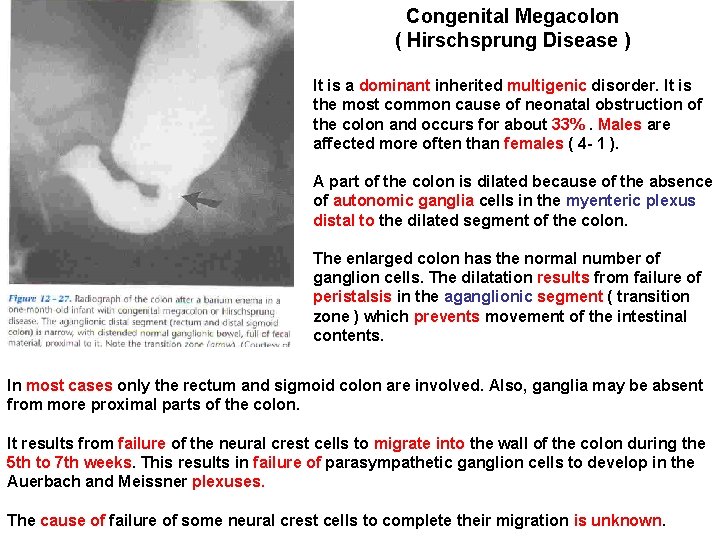
Congenital Megacolon ( Hirschsprung Disease ) It is a dominant inherited multigenic disorder. It is the most common cause of neonatal obstruction of the colon and occurs for about 33%. Males are affected more often than females ( 4 - 1 ). A part of the colon is dilated because of the absence of autonomic ganglia cells in the myenteric plexus distal to the dilated segment of the colon. The enlarged colon has the normal number of ganglion cells. The dilatation results from failure of peristalsis in the aganglionic segment ( transition zone ) which prevents movement of the intestinal contents. In most cases only the rectum and sigmoid colon are involved. Also, ganglia may be absent from more proximal parts of the colon. It results from failure of the neural crest cells to migrate into the wall of the colon during the 5 th to 7 th weeks. This results in failure of parasympathetic ganglion cells to develop in the Auerbach and Meissner plexuses. The cause of failure of some neural crest cells to complete their migration is unknown.
 Insidan region jh
Insidan region jh Derivatives of midgut
Derivatives of midgut Stomodeum and proctodeum
Stomodeum and proctodeum Midgut
Midgut Development of duodenum
Development of duodenum Rotation of gut
Rotation of gut Guttube
Guttube Embryo folding
Embryo folding Foregut, midgut hindgut adalah
Foregut, midgut hindgut adalah Tranversum
Tranversum Chain rule formula
Chain rule formula Splanchnopleuric mesoderm
Splanchnopleuric mesoderm How to find derivatives on ti 84
How to find derivatives on ti 84 Partial differentiation
Partial differentiation Hypomere and epimere
Hypomere and epimere Financial engineering derivatives and risk management
Financial engineering derivatives and risk management Non financial derivatives
Non financial derivatives Mesodermal derivatives
Mesodermal derivatives Hydrolysis of a nitrile mechanism
Hydrolysis of a nitrile mechanism Stoxx blue chip
Stoxx blue chip Embedded derivative
Embedded derivative Derivatives of inverse functions and logarithms
Derivatives of inverse functions and logarithms Derivatives formulas
Derivatives formulas