MICU Morning Report Case Presentation 48 yo male
- Slides: 18
MICU Morning Report
Case Presentation 48 yo male w/ hx HTN, DM who presents to ED with fever, cough and dyspnea for 2 days. No sick contacts No recent travel Cough productive of yellow sputum
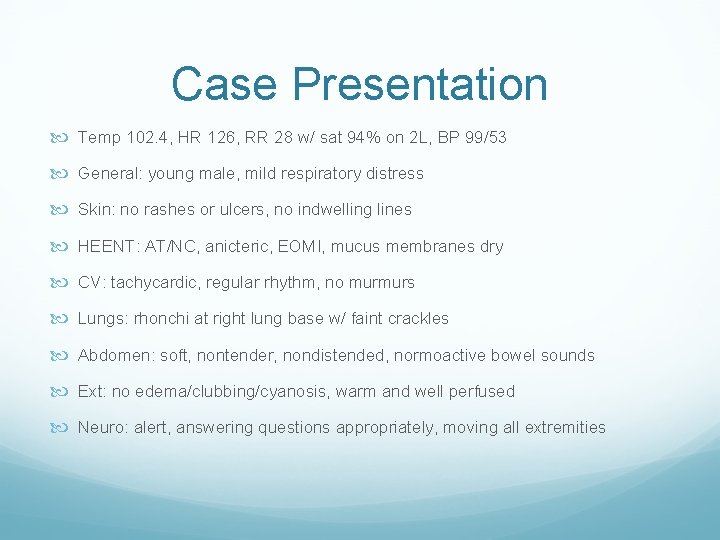
Case Presentation Temp 102. 4, HR 126, RR 28 w/ sat 94% on 2 L, BP 99/53 General: young male, mild respiratory distress Skin: no rashes or ulcers, no indwelling lines HEENT: AT/NC, anicteric, EOMI, mucus membranes dry CV: tachycardic, regular rhythm, no murmurs Lungs: rhonchi at right lung base w/ faint crackles Abdomen: soft, nontender, nondistended, normoactive bowel sounds Ext: no edema/clubbing/cyanosis, warm and well perfused Neuro: alert, answering questions appropriately, moving all extremities
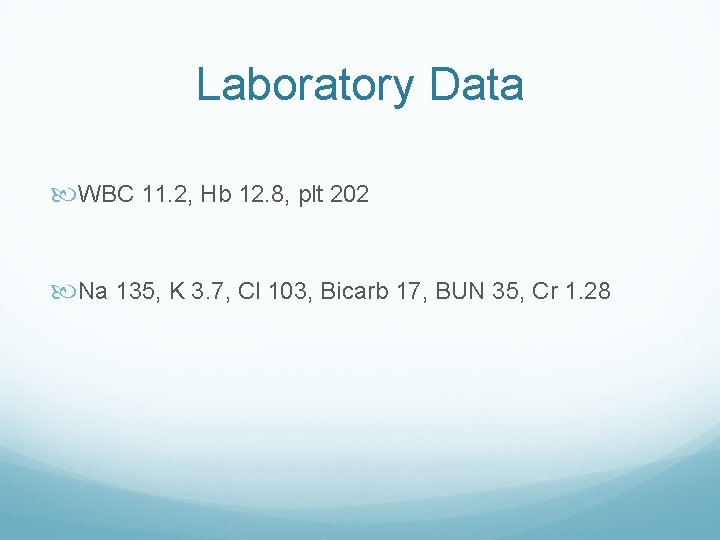
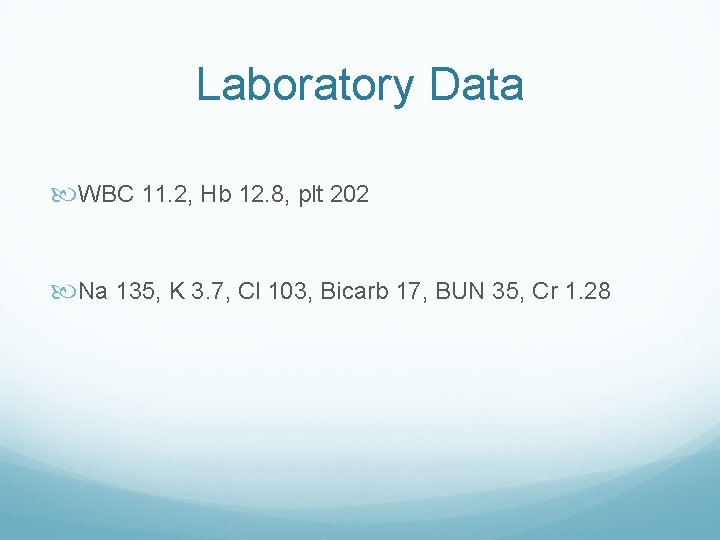
Laboratory Data WBC 11. 2, Hb 12. 8, plt 202 Na 135, K 3. 7, Cl 103, Bicarb 17, BUN 35, Cr 1. 28
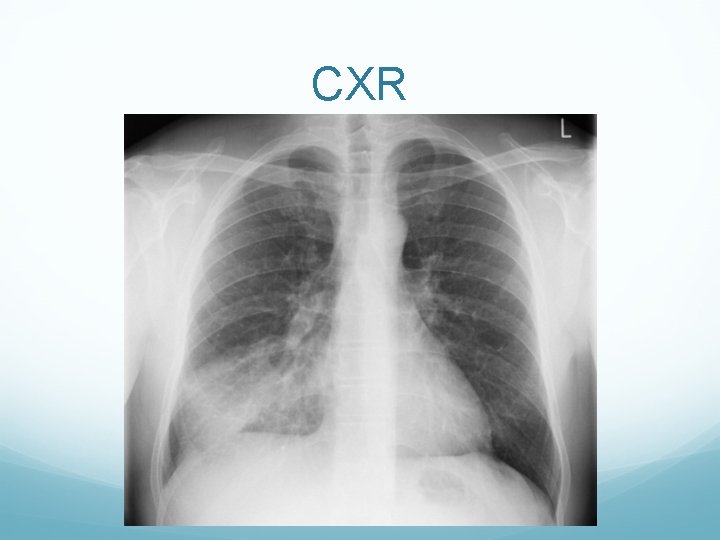
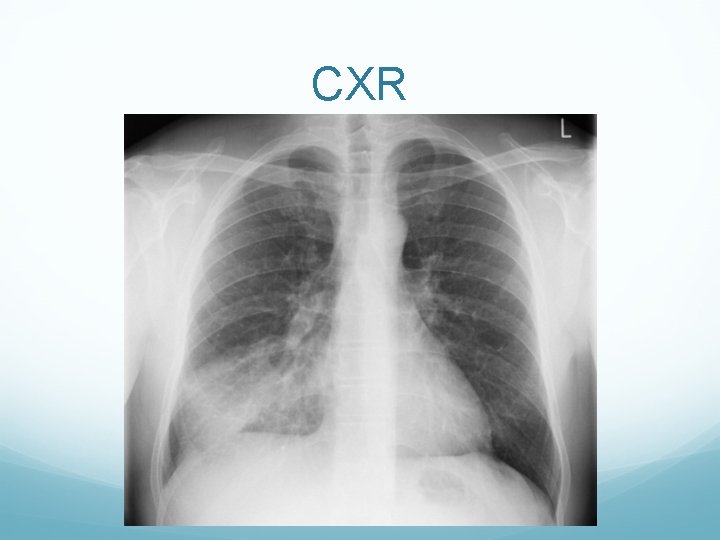
CXR
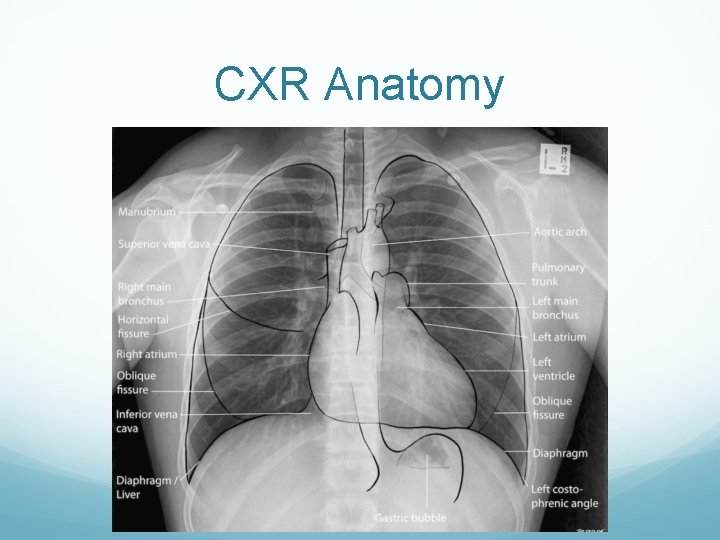
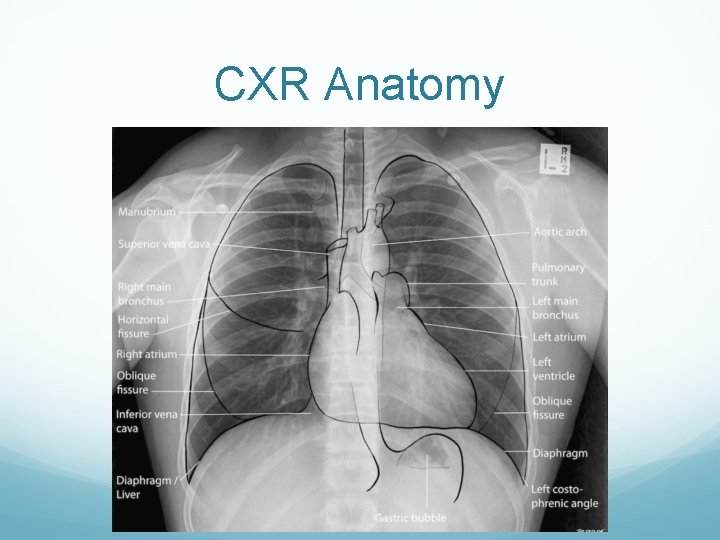
CXR Anatomy
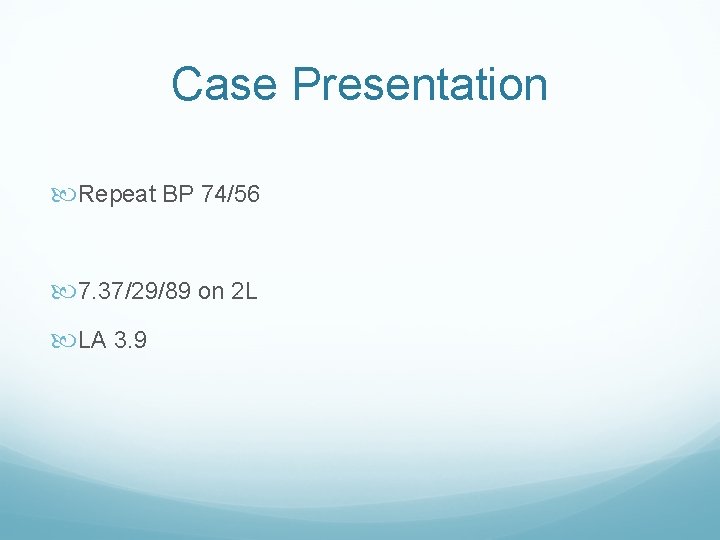
Case Presentation Repeat BP 74/56 7. 37/29/89 on 2 L LA 3. 9
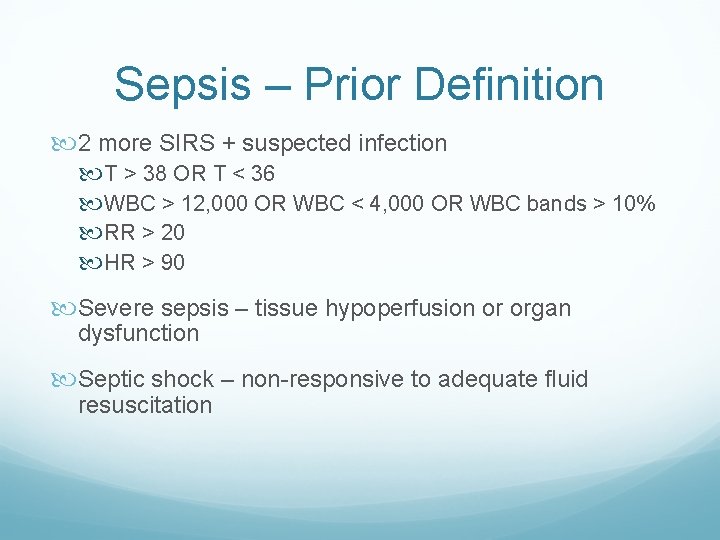
Sepsis – Prior Definition 2 more SIRS + suspected infection T > 38 OR T < 36 WBC > 12, 000 OR WBC < 4, 000 OR WBC bands > 10% RR > 20 HR > 90 Severe sepsis – tissue hypoperfusion or organ dysfunction Septic shock – non-responsive to adequate fluid resuscitation
Sepsis – Newer Definitions Life-threatening organ dysfunction caused by a dysregulated host response to infection Increase of 2 or more points in the SOFA score Severe sepsis - no longer used Septic shock despite adequate fluid resuscitation, require vasopressors to maintain MAP > 65 lactate > 2
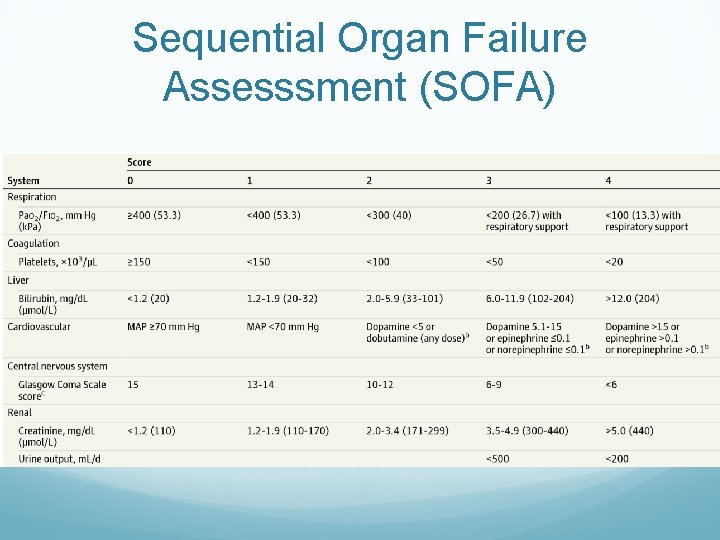
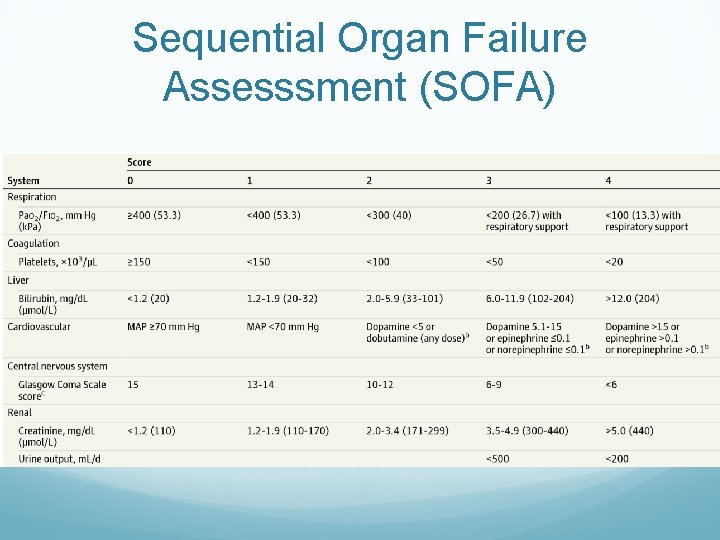
Sequential Organ Failure Assesssment (SOFA)
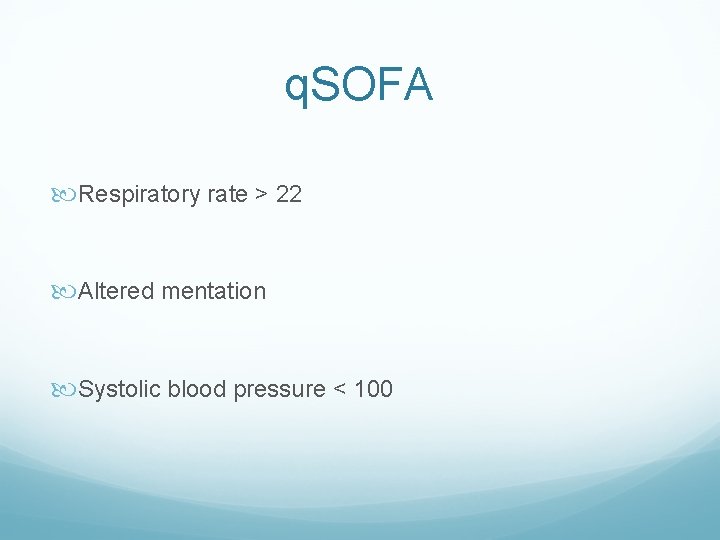
q. SOFA Respiratory rate > 22 Altered mentation Systolic blood pressure < 100
Management BP 74/56 LA 3. 9 What would you do next?
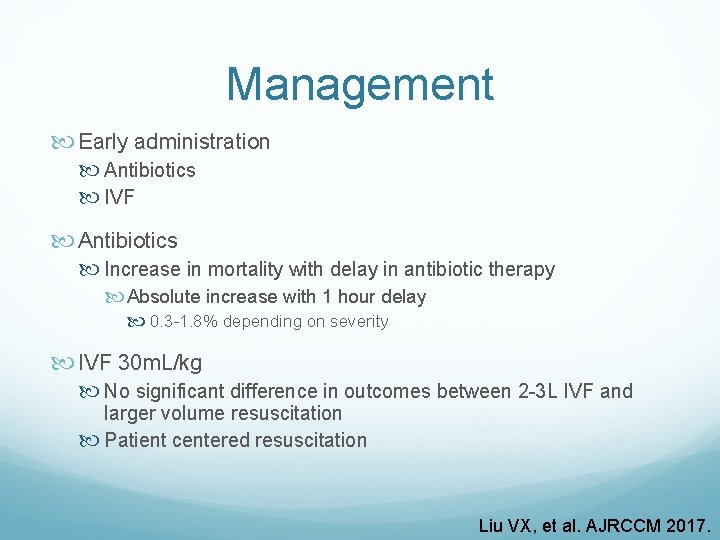
Management Early administration Antibiotics IVF Antibiotics Increase in mortality with delay in antibiotic therapy Absolute increase with 1 hour delay 0. 3 -1. 8% depending on severity IVF 30 m. L/kg No significant difference in outcomes between 2 -3 L IVF and larger volume resuscitation Patient centered resuscitation Liu VX, et al. AJRCCM 2017.
Management Early administration Antibiotics IVF Supportive care Airway management Oxygenation Assess perfusion (BP, end organ damage) Venous access
Case Presentation Patient transferred to MICU Started on ceftriaxone/azithromycin for CAP Given 3 L IVF > BP now 77/34
Vasopressors Norepinephrine is 1 st line therapy 2 nd line includes epinephrine, vasopressin, phenylephrine, dopamine Take individual patient characteristics into consideration
Vasopressors SOAP II No difference in mortality between NE and Dopa Increased rates of adverse effects (arrhythmia) with dopa Subgroup with cardiogenic shock: higher mortality with dopa compared to NE
Vasopressors VASST trial – Does addition of vasopressin to norepinephrine compared to norepinephrine alone reduce mortality at 28 days? No Resulted in lower doses of norepinephrine VANISH trial – Does early vasopressin compared to norepinephrine improve renal outcomes? No change in kidney failure-free days Used higher doses of vasopressin