Microparticle Enzyme Immunoassay MEIA Microparticle Enzyme Immunoassay MEIA


- Slides: 41

Microparticle Enzyme Immunoassay ( MEIA)
• Microparticle Enzyme Immunoassay (MEIA) is an immunoassay method that utilizes the isolation of antibody/antigen complexes on a solid phase surface of small beads called microparticles. • MEIA has been widely adapted to automate the measurement of large molecules such as markers associated with cardiac, fertility, cancer, metabolic, hepatitis, and thyroid testing.
• Chemiluminescent Magnetic Immunoassay (CMIA): Chemiluminescent label conjugated to the antibody or antigen, and it produces light when combined with it’s substrate. This method is similar to MEIA, thought the chemiluminescent reaction offers high sensitivity and ease of measurement.
• CMIA used for quantitative determination of human thyroid stimulating hormone in serum and plasma. • In ARCHITECT instrument, TSH assay is a twostep immunoassay to determine the presence of TSH in serum or plasma by CMIA technology with flexible assay protocols referred to as chemiflex.
• In the first step, sample, anti TSH antibody coated paramagnetic micro particles and TSH assay diluent are combined. TSH present in the sample binds to the anti TSH antibody coated micro particles. After washing, anti- alpha TSH acridinium labeled conjugate is added in the second step. • Pre-trigger and trigger solutions are then added to the reaction mixture: the resulting chemiluminescent reaction is measured as relative light units(RLUs).
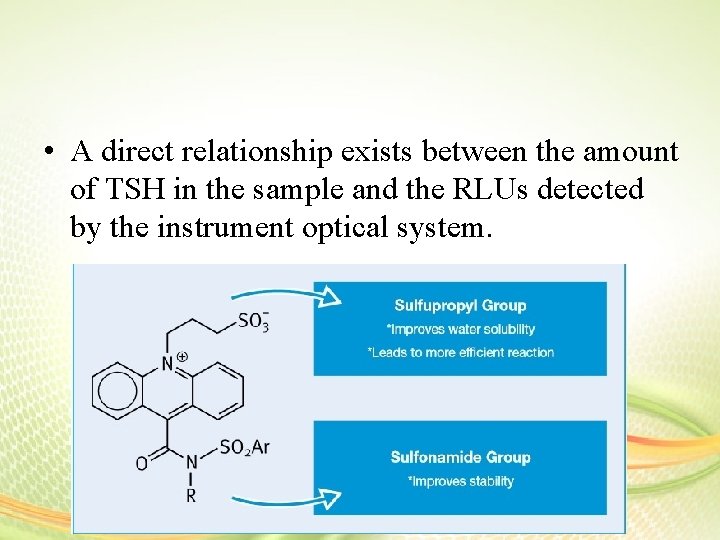
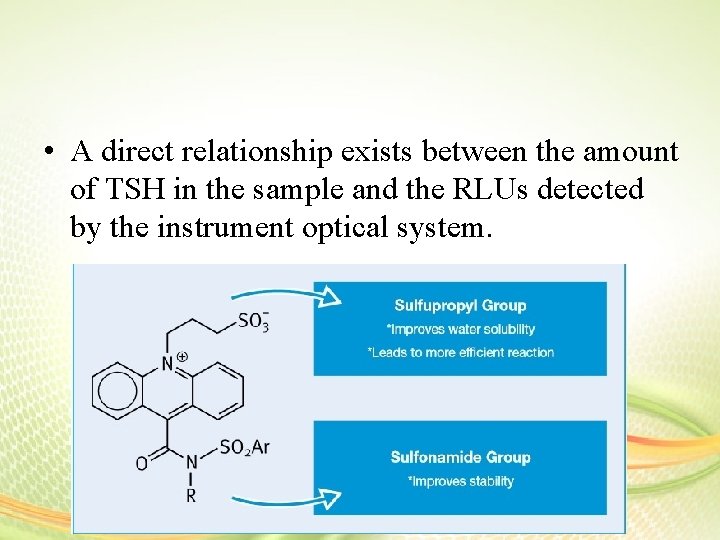
• A direct relationship exists between the amount of TSH in the sample and the RLUs detected by the instrument optical system.
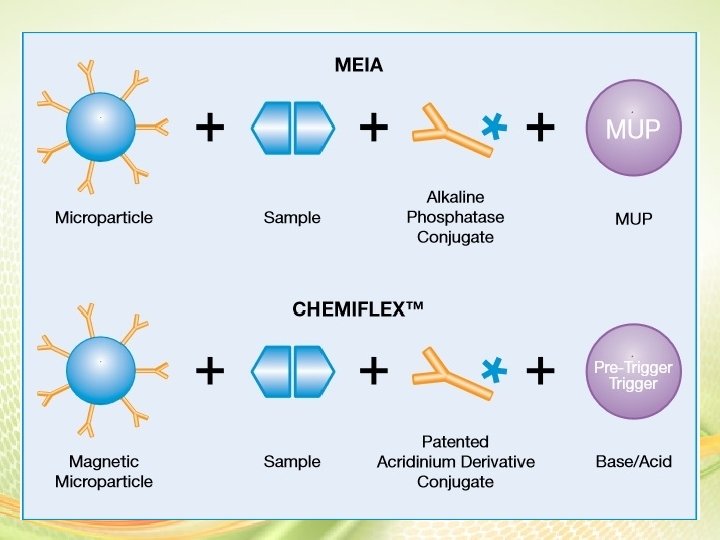
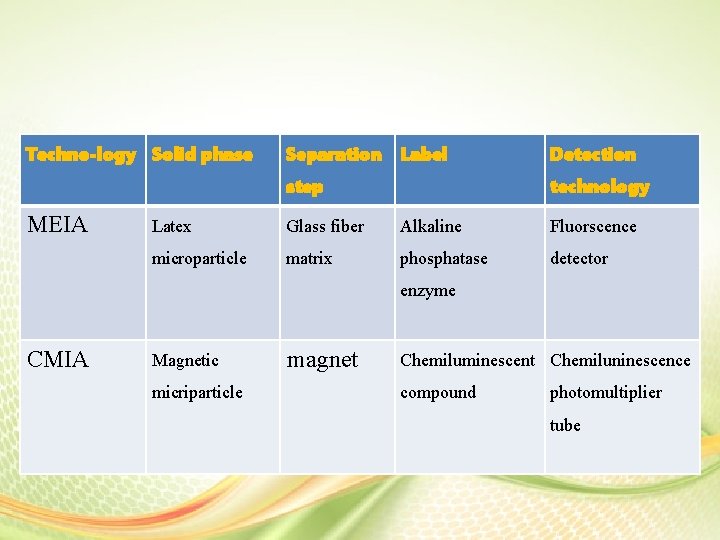
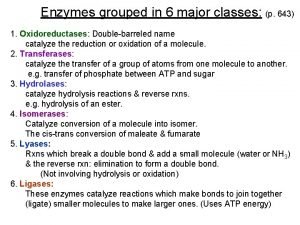
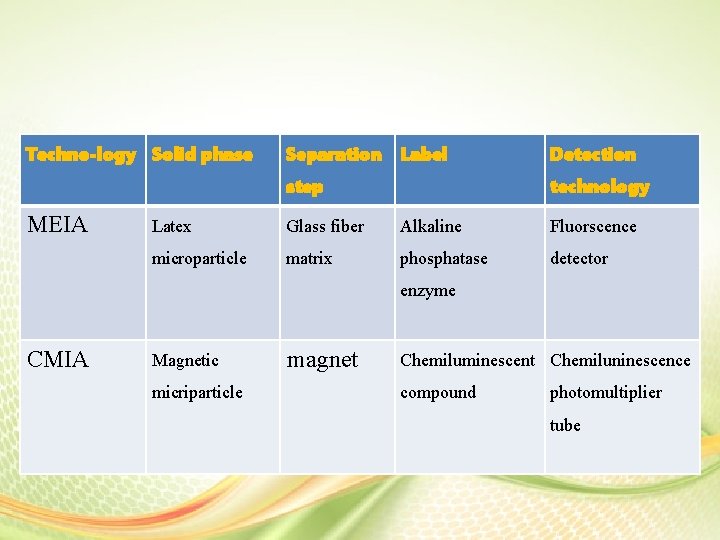
Techno-logy Solid phase Separation Label step MEIA Detection technology Latex Glass fiber Alkaline Fluorscence microparticle matrix phosphatase detector enzyme CMIA Magnetic micriparticle magnet Chemiluminescent Chemiluninescence compound photomultiplier tube
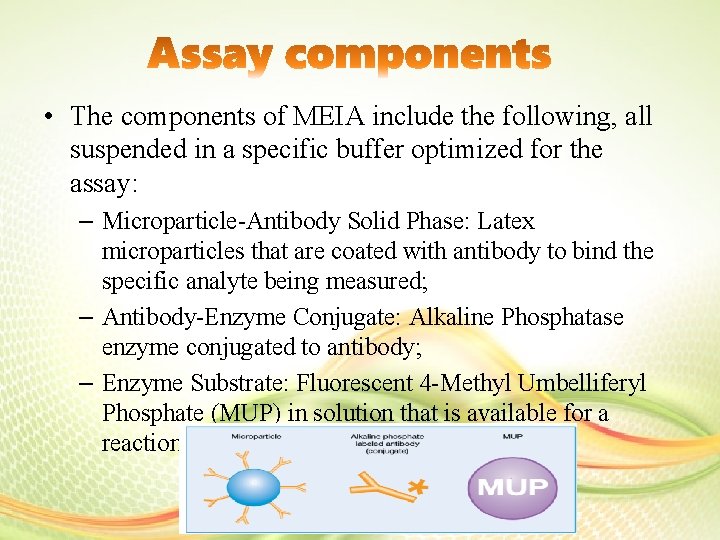
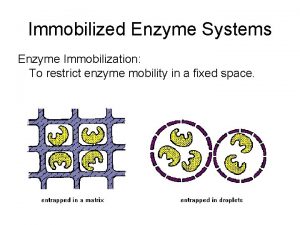
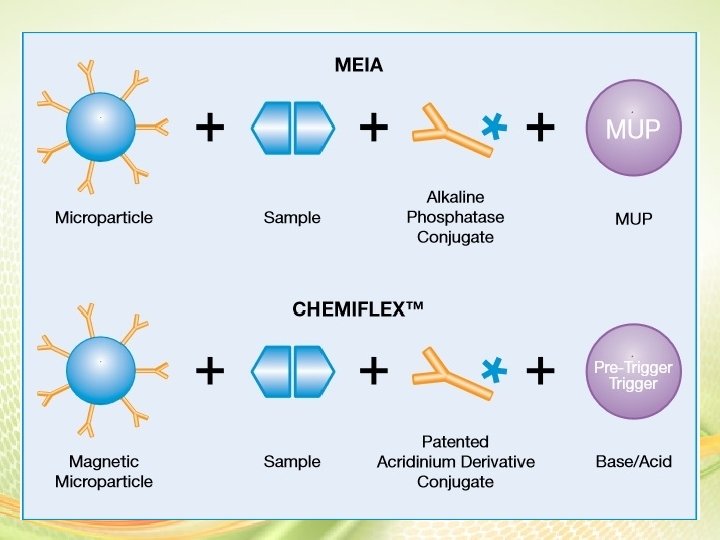
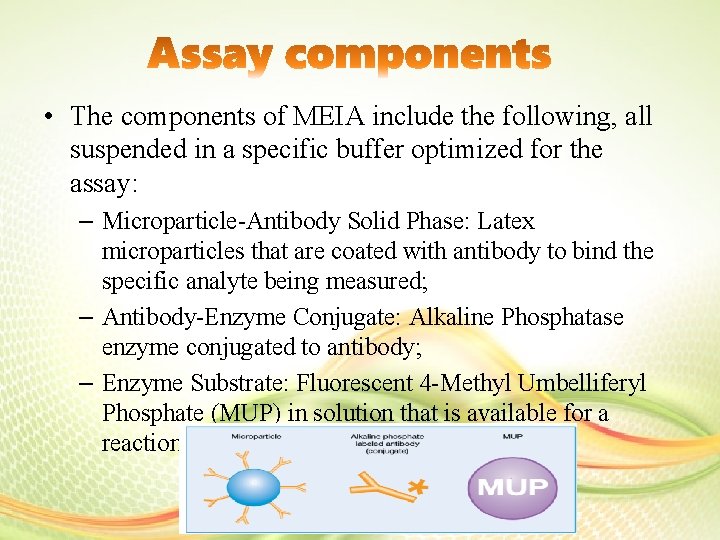
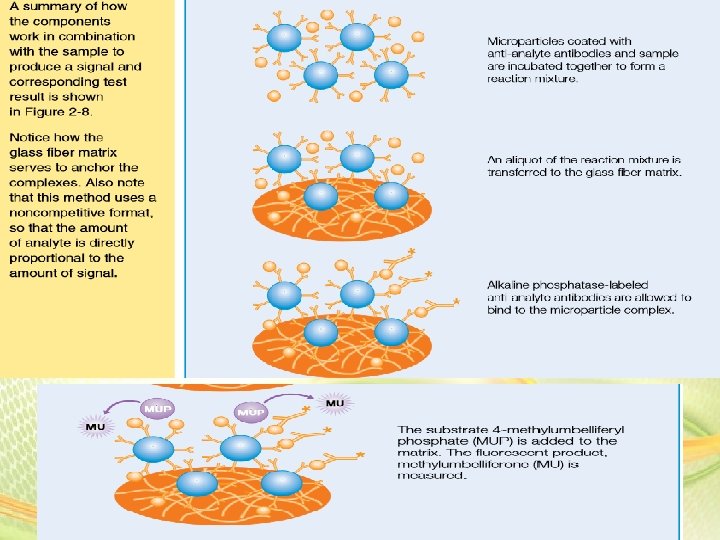
• The components of MEIA include the following, all suspended in a specific buffer optimized for the assay: – Microparticle-Antibody Solid Phase: Latex microparticles that are coated with antibody to bind the specific analyte being measured; – Antibody-Enzyme Conjugate: Alkaline Phosphatase enzyme conjugated to antibody; – Enzyme Substrate: Fluorescent 4 -Methyl Umbelliferyl Phosphate (MUP) in solution that is available for a reaction with the enzyme on the antibody.
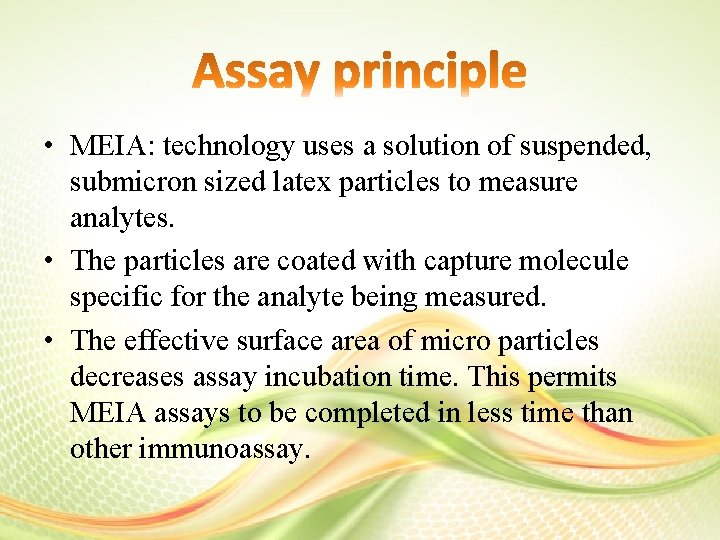
• MEIA: technology uses a solution of suspended, submicron sized latex particles to measure analytes. • The particles are coated with capture molecule specific for the analyte being measured. • The effective surface area of micro particles decreases assay incubation time. This permits MEIA assays to be completed in less time than other immunoassay.
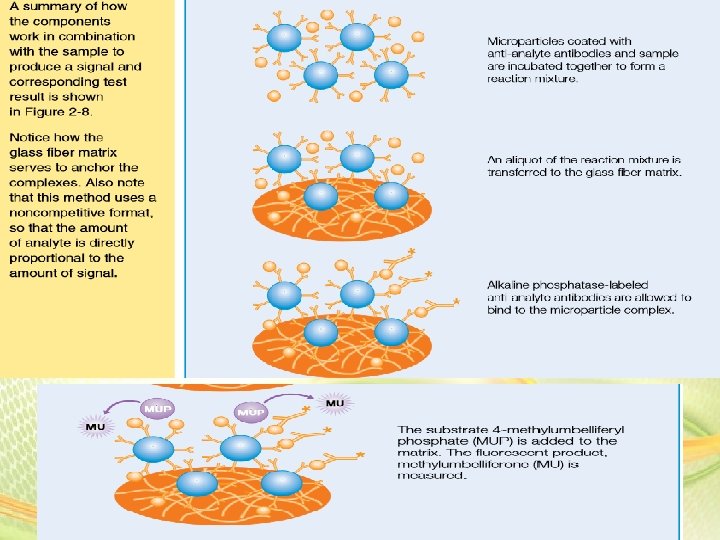
• In the sampling center, reactants and sample for one assay are transferred to a reaction vessel. The reaction vessel is transferred to the processing center where reagents and sample are incubated to allow them to come to reaction temperature. • The reagents and sample are combined and the reaction mixture is transferred to an inert glass fiber matrix. Irreversible binding of the microparticles causes the immune complex to be retained by glass fibers while the reaction mixture flows rapidly through the large pores in the matrix.
• An alkaline phosphate- labeled conjugate is added to the glass fiber matrix prior to the addition of 4 - methylumbelliferyl phosphate MUP. The conjugate catalyzes the hydrolysis of MUP to methylumbelliferone(MU). • Measurement of the fluorescent MU as it is generated on the matrix is proportional to the concentration of the analyte in the test sample.
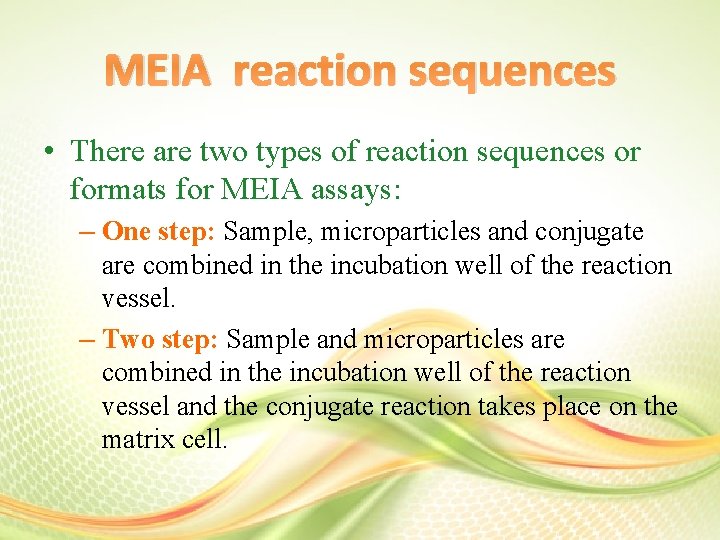
MEIA reaction sequences • There are two types of reaction sequences or formats for MEIA assays: – One step: Sample, microparticles and conjugate are combined in the incubation well of the reaction vessel. – Two step: Sample and microparticles are combined in the incubation well of the reaction vessel and the conjugate reaction takes place on the matrix cell.
Procedure 1. Analytes bind to micro particles: Samples and micro particles are combined and incubated at reaction temperature. During the incubation period analytes bind to the micro particles creating an immune complex. 2. Immune complex binds to glass fiber matrix. The processing probe aspirates the reaction vessel and dispenses it onto the matrix cell. The immune complex binds irreversibly to glass fiber matrix. A matrix cell wash removes unbound materials. The immune complex is retained by the glass fibers while the excess reaction mixture flows rapidly through the large ores in the matrix.
Thyroid hormones
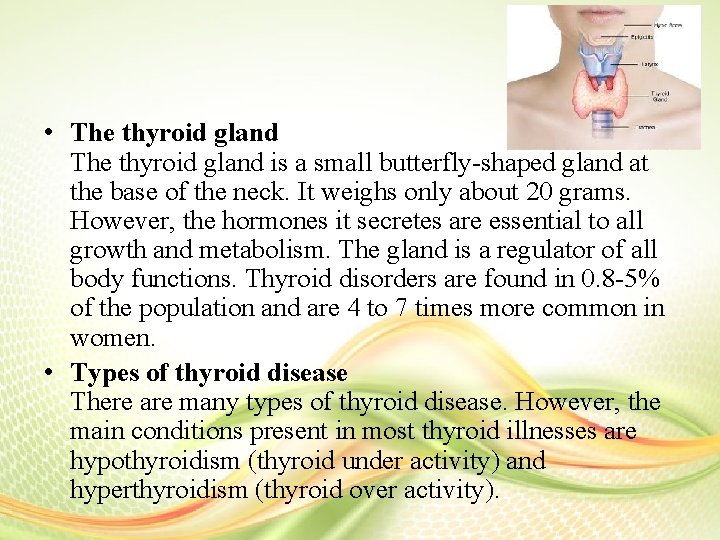
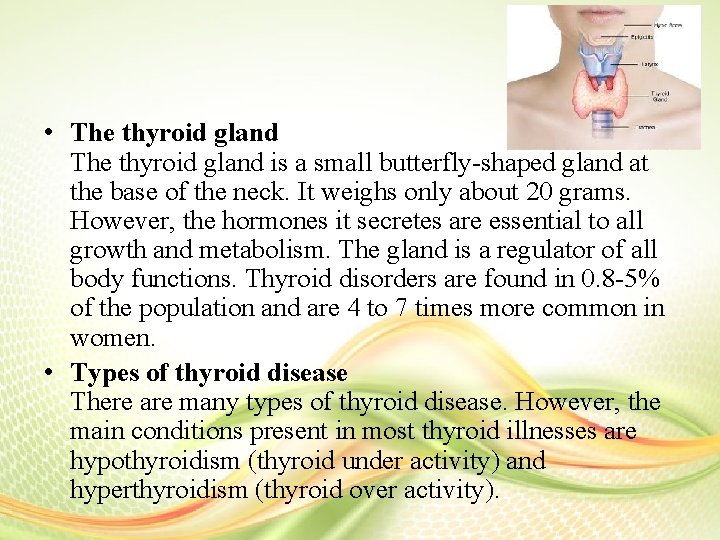
• The thyroid gland is a small butterfly-shaped gland at the base of the neck. It weighs only about 20 grams. However, the hormones it secretes are essential to all growth and metabolism. The gland is a regulator of all body functions. Thyroid disorders are found in 0. 8 -5% of the population and are 4 to 7 times more common in women. • Types of thyroid disease There are many types of thyroid disease. However, the main conditions present in most thyroid illnesses are hypothyroidism (thyroid under activity) and hyperthyroidism (thyroid over activity).
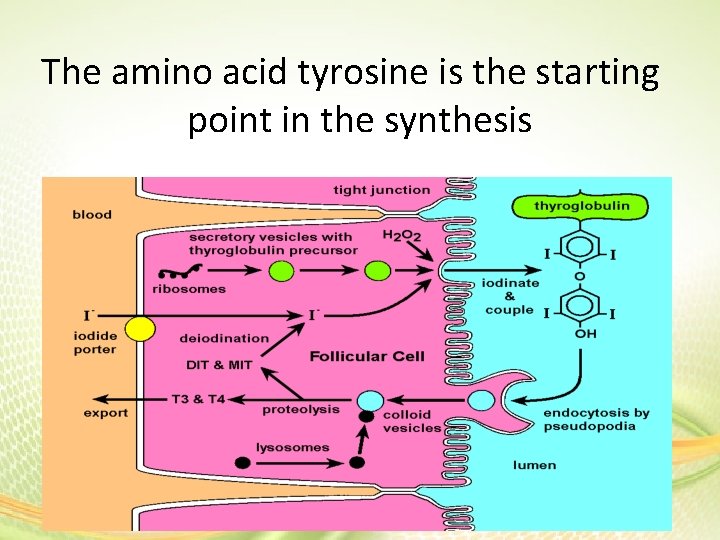
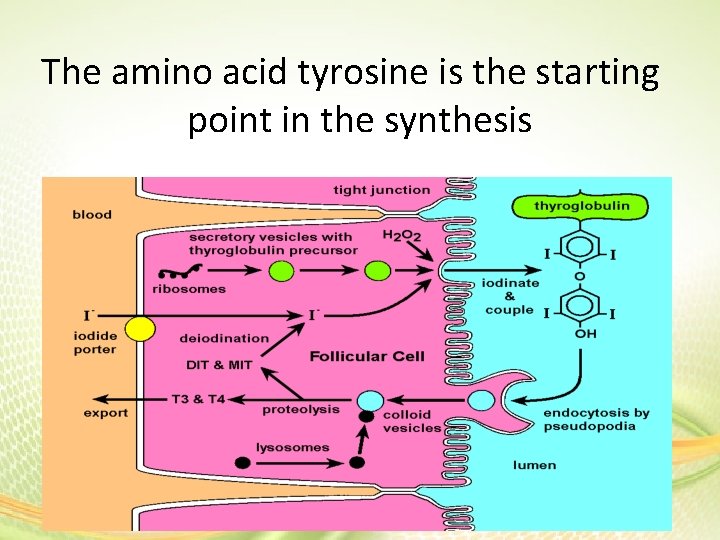
The amino acid tyrosine is the starting point in the synthesis
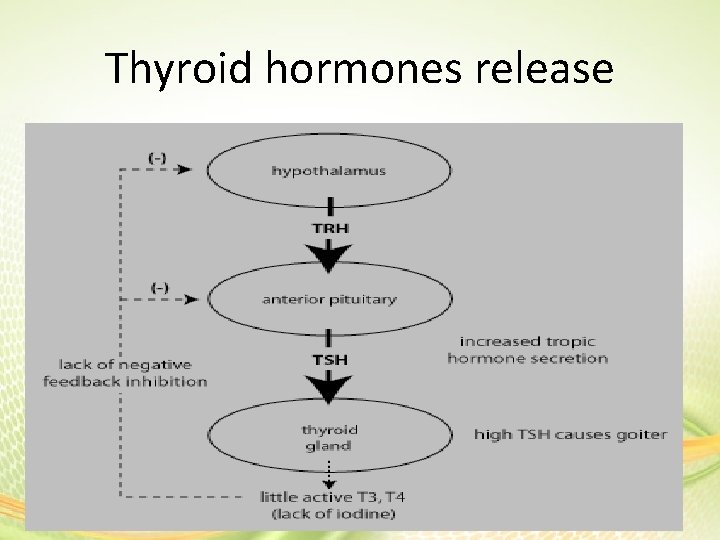
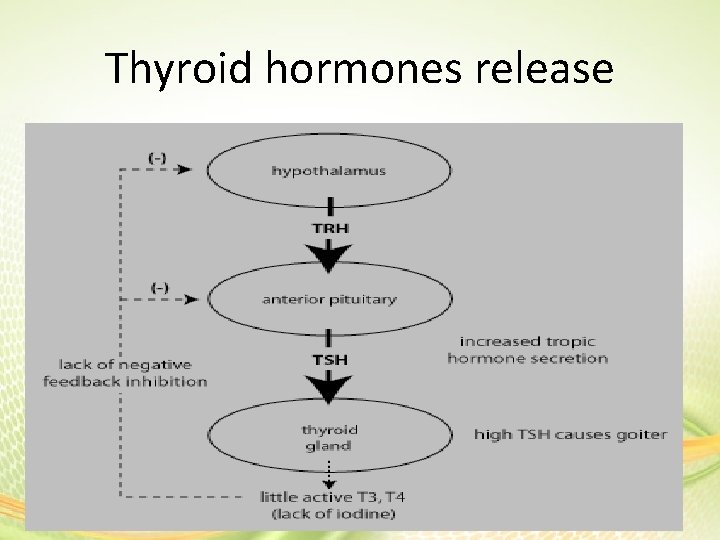
Thyroid hormones release
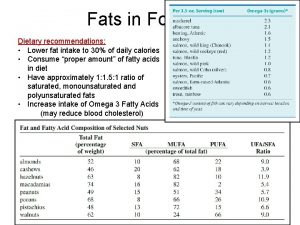
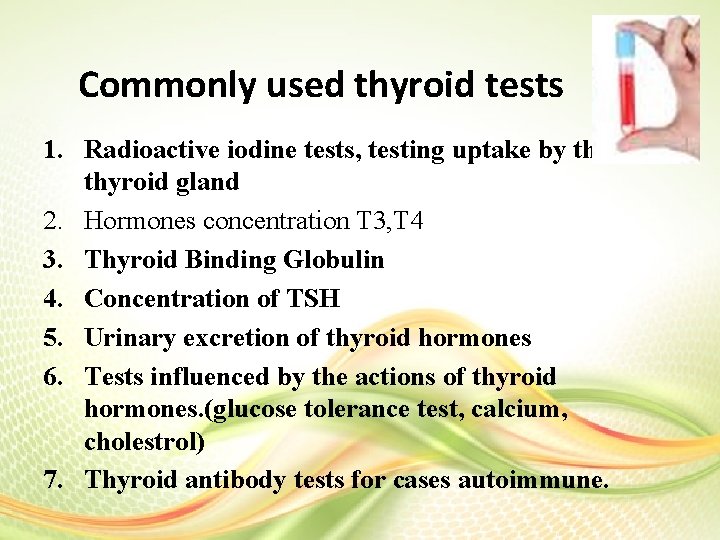
Commonly used thyroid tests 1. Radioactive iodine tests, testing uptake by the thyroid gland 2. Hormones concentration T 3, T 4 3. Thyroid Binding Globulin 4. Concentration of TSH 5. Urinary excretion of thyroid hormones 6. Tests influenced by the actions of thyroid hormones. (glucose tolerance test, calcium, cholestrol) 7. Thyroid antibody tests for cases autoimmune.
Tests for evaluate thyroid gland • The main contribution of chemical measurements to the investigation of thyroid disease is to help sub-divide patients into the categories of effects of treatment.
Thyroid hormones • It must be emphasized that a single thyroid function test is NOT absolute in diagnostic accuracy and thus, a careful selection of tests, so that their combination can give comprehensive data, would enhance the diagnostic accuracy.
• Type of sample: blood, urine or saliva • Most blood tests involving hormones measure the bound protein. However, saliva-based testing measures the free level of hormone. • Conditions for test: you should ask the patient if he/she under treatment and receive drug or made surgery thyroidectomy recently. • Preparation the patient: be kind when you deal with patient. • You should read the diagnosis status on request.
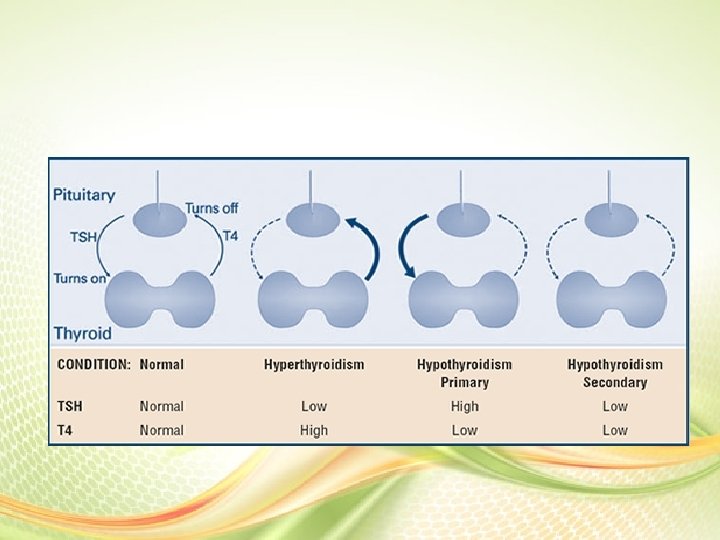
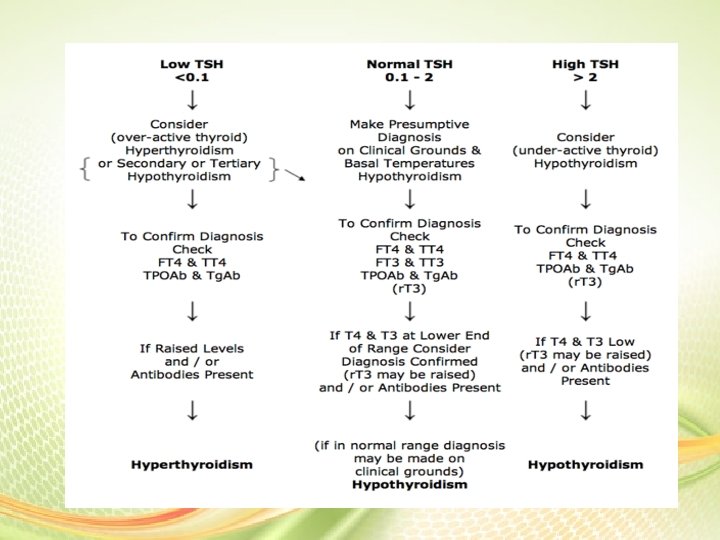
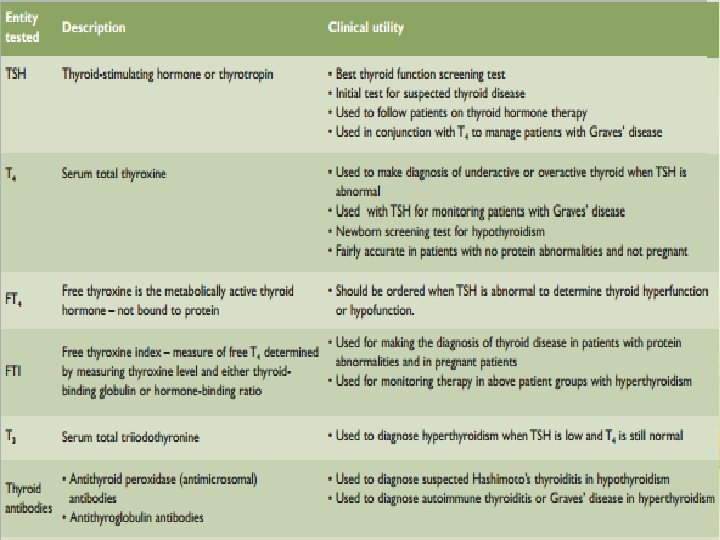
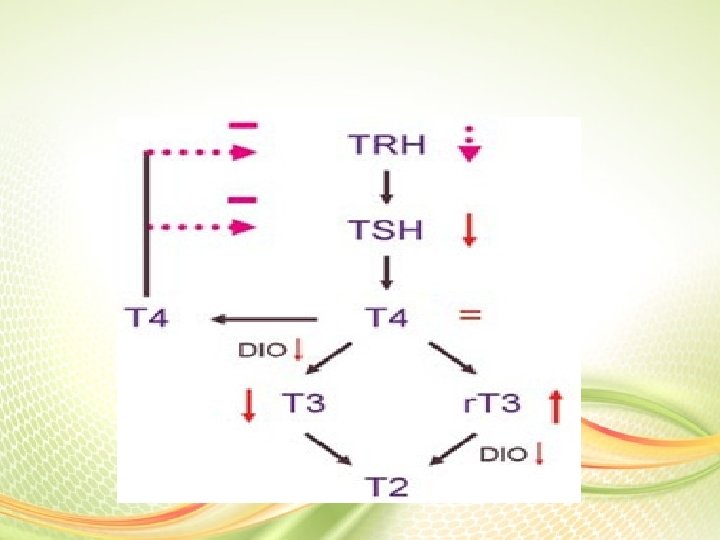
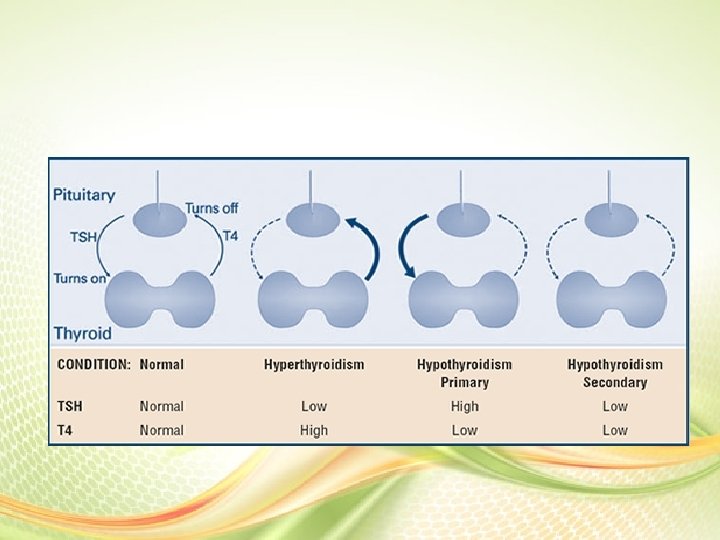
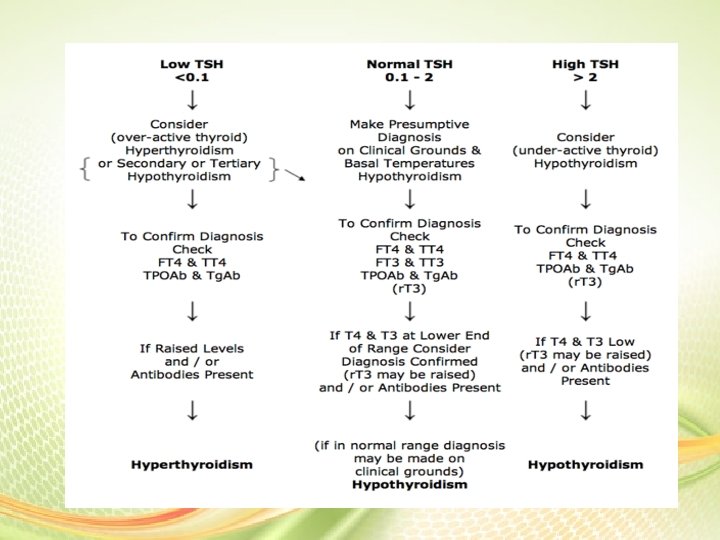
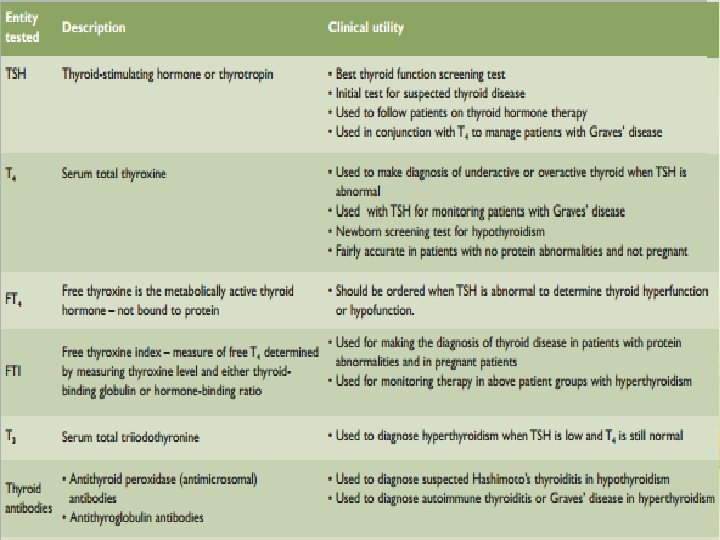
TSH • Concentrations are usually lowered in thyroxicosis, due feedback inhibition of hypothalamus and pituitary • Conversely, plasma TSH is increased in hypothyroidism, except for the rare cases of hypothyroidism secondary to pituitary disease.
TSH is the most appropriate test when monitoring patients receiving thyroxine for the treatment of hypothyroidism. It should be measured no sooner than 6 -8 weeks after the start of treatment. In the unusual situation where thyroid function needs to be assessed before this time, FT 4 should be used, as the TSH will not have plateaued at this stage.
TSH: In most situations TSH analysed using a high sensitivity assay is now accepted as the first line test for assessment of thyroid function. A TSH between 0. 4 and 4. 0 m. IU/L gives 99% exclusion of hypo- or hyperthyroidism, 12 while the TSH is considered more sensitive than FT 4 to alterations of thyroid status in patients with primary thyroid disease. Thyroglobulin: Levels are increased in all types of thyrotoxicosis, except thyrotoxicosis factitia caused by self-administration of thyroid hormone. The main role for thyroglobulin is in the follow-up of thyroid cancer patients. After total thyroidectomy and radioablation, thyroglobulin levels should be undetectable; measurable levels (>1 to 2 ng/m. L) suggest incomplete ablation or recurrent cancer.
• Thyrotropin (TSH)-secreting adenomas These rare tumors make too much thyroid-stimulating hormone (TSH), which then causes the thyroid gland to make too much thyroid hormone. This can cause symptoms of hyperthyroidism (overactive thyroid),
T 3 • Is more biologically active than T 4 but both hormones have similar actions in the body. • T 3 is not usually used in confirming the diagnosis of suspected hypothyroidism because other tests can demonstrate hypofunction of the thyroid gland. • T 3 tests are often useful to diagnosis hyperthyroidism or todetermine its severity • Sometimes, however, a patient may have clinical signs of thyrotoxicosis with a normal T 4. Measurement of the T 3 is then needed, because T 3 may be elevated in thyrotoxicosis while other thyroid tests are still the normal range. • T 3 testing rarely is helpful in the hypothyroid patient, since it is the last test to become abnormal.
• FT 3 - FT 3 has little specificity or sensitivity for diagnosing hypothyroidism and adds little diagnostic information. The main value of FT 3 is in the evaluation of the 2 to 5% of patients who are clinically hyperthyroid, but have normal FT 4. In this situation, an elevated FT 3 would be suggestive of T 3 toxicosis, in which the thyroid secretes increased amount of T 3 or there is excessive conversion of T 4 to T 3.
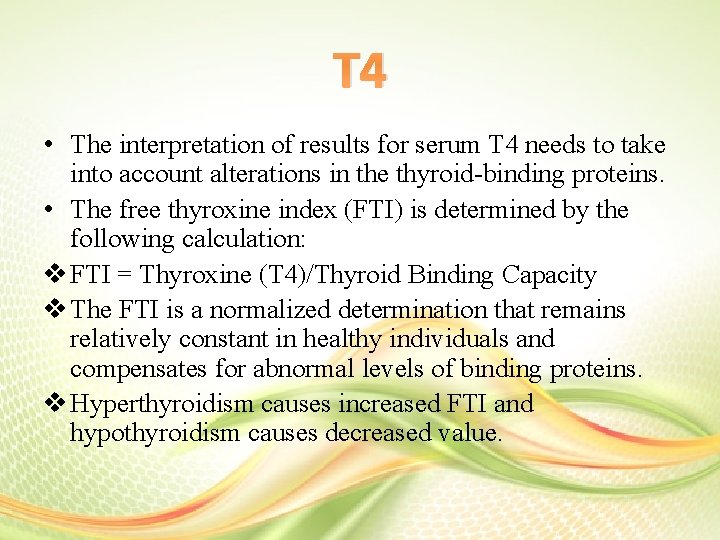
T 4 • The interpretation of results for serum T 4 needs to take into account alterations in the thyroid-binding proteins. • The free thyroxine index (FTI) is determined by the following calculation: v FTI = Thyroxine (T 4)/Thyroid Binding Capacity v The FTI is a normalized determination that remains relatively constant in healthy individuals and compensates for abnormal levels of binding proteins. v Hyperthyroidism causes increased FTI and hypothyroidism causes decreased value.
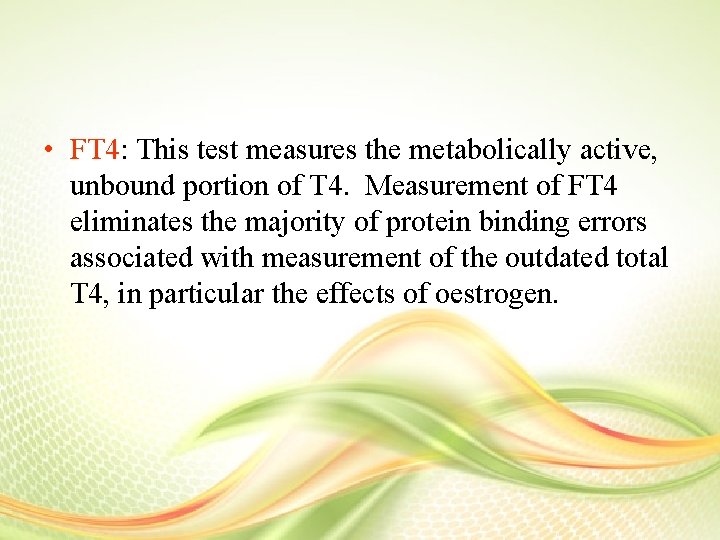
• FT 4: This test measures the metabolically active, unbound portion of T 4. Measurement of FT 4 eliminates the majority of protein binding errors associated with measurement of the outdated total T 4, in particular the effects of oestrogen.
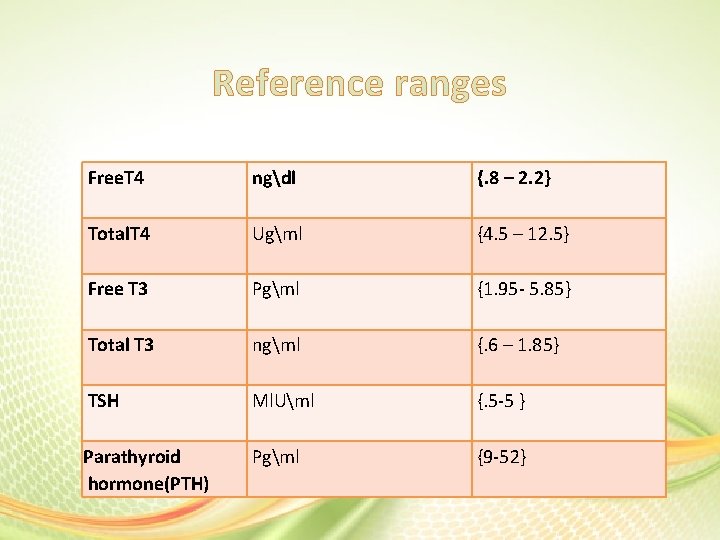
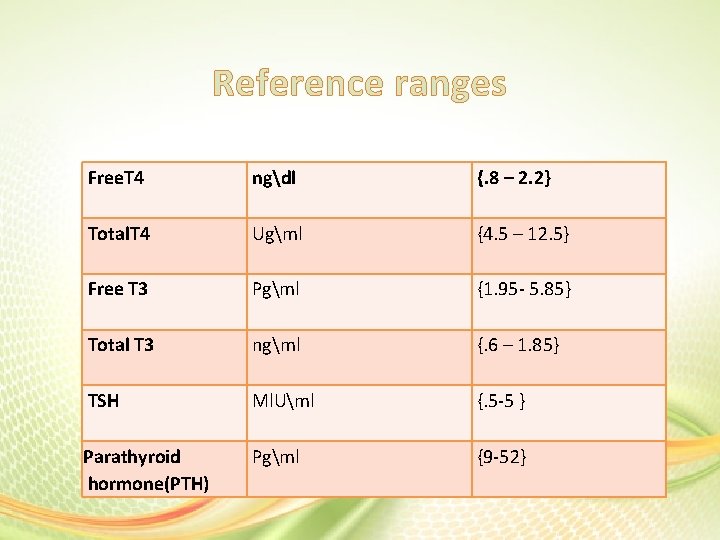
Reference ranges Free. T 4 ngdl {. 8 – 2. 2} Total. T 4 Ugml {4. 5 – 12. 5} Free T 3 Pgml {1. 95 - 5. 85} Total T 3 ngml {. 6 – 1. 85} TSH Ml. Uml {. 5 -5 } Parathyroid hormone(PTH) Pgml {9 -52}
There are marked variations in the thyroid function with age, evident in all of the vitro hormone and proteins measurements. In general thyroid function parameters in healthy subjects show little or no clinical significant gender or racial variation.
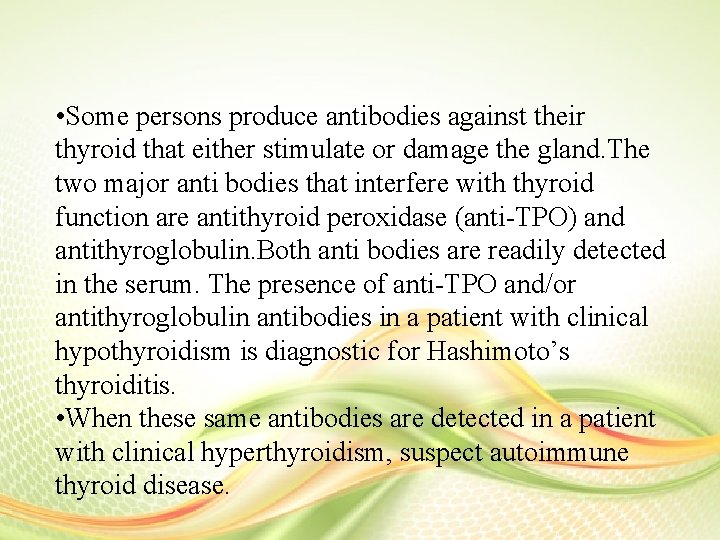
• Some persons produce antibodies against their thyroid that either stimulate or damage the gland. The two major anti bodies that interfere with thyroid function are antithyroid peroxidase (anti-TPO) and antithyroglobulin. Both anti bodies are readily detected in the serum. The presence of anti-TPO and/or antithyroglobulin antibodies in a patient with clinical hypothyroidism is diagnostic for Hashimoto’s thyroiditis. • When these same antibodies are detected in a patient with clinical hyperthyroidism, suspect autoimmune thyroid disease.
Clinical errors • Quality control, the best step for all analytical tests to have a reliable result and a voiding the errors. • Pre analytical • Analytical process • Post analytical process
Case study • A 63 -year-old woman has Hashimoto’s disease. Her thyroid laboratory values today include the following: She feels consistently run down and has dry skin that does not respond to the use of hand creams. The hormones levels: • TSH 10. 6 m. IU/L (normal (0. 5– 4. 5 m. IU/L) • A free T 4 concentration of 0. 5 ng/d. L (normal 0. 8– 1. 9 ng/d. L).

That’s all
 Meia immunoassay
Meia immunoassay What is the principle of elisa
What is the principle of elisa Labeled immunoassay
Labeled immunoassay Salto no plinto
Salto no plinto Meia vida contexto sensitiva
Meia vida contexto sensitiva Betumel
Betumel Advantage of enzyme
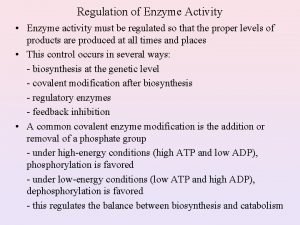
Advantage of enzyme Carboxylase enzyme class
Carboxylase enzyme class Hyaluronidase enzyme
Hyaluronidase enzyme Haemodent
Haemodent Enzyme kinetics
Enzyme kinetics Protein primary structure
Protein primary structure Oxidarion
Oxidarion Physiology of digestion and absorption
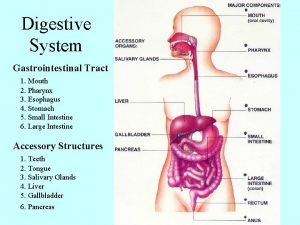
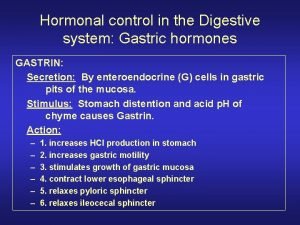
Physiology of digestion and absorption Galctosemia
Galctosemia Whiplash injury
Whiplash injury An example of prosthetic group
An example of prosthetic group Succinate dehydrogenase inhibitor malonate
Succinate dehydrogenase inhibitor malonate Enzyme ec number
Enzyme ec number Pepsin substrate and product
Pepsin substrate and product Enzyme molecule
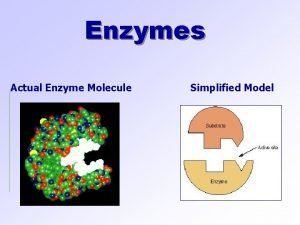
Enzyme molecule Alteration of food
Alteration of food Creatine kinase enzyme
Creatine kinase enzyme Restriction enzyme mapping
Restriction enzyme mapping Enzyme classes
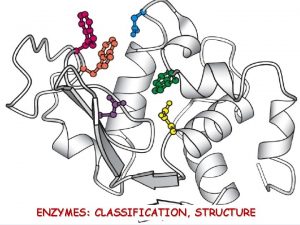
Enzyme classes Stickies-control enzyme
Stickies-control enzyme What role does dna polymerase play in copying dna?
What role does dna polymerase play in copying dna? Francis crick
Francis crick Thiamin
Thiamin Glucouronide
Glucouronide Inorganic catalyst vs enzyme
Inorganic catalyst vs enzyme Restriction enzyme analysis of dna ap bio lab
Restriction enzyme analysis of dna ap bio lab S___ux1
S___ux1 Dermatomyocytis
Dermatomyocytis Class of enzyme
Class of enzyme Enzyme activity graph
Enzyme activity graph Characteristics of enzymes
Characteristics of enzymes Non functional plasma enzymes
Non functional plasma enzymes Stickase
Stickase Hydrophilic heads
Hydrophilic heads Factors affecting enzyme activity slideshare
Factors affecting enzyme activity slideshare Enzyme-linked immunosorbent assay (elisa)
Enzyme-linked immunosorbent assay (elisa)