Microcirculation and inflammation M Jurajda Anatomy of capillary
- Slides: 21
Microcirculation and inflammation M. Jurajda
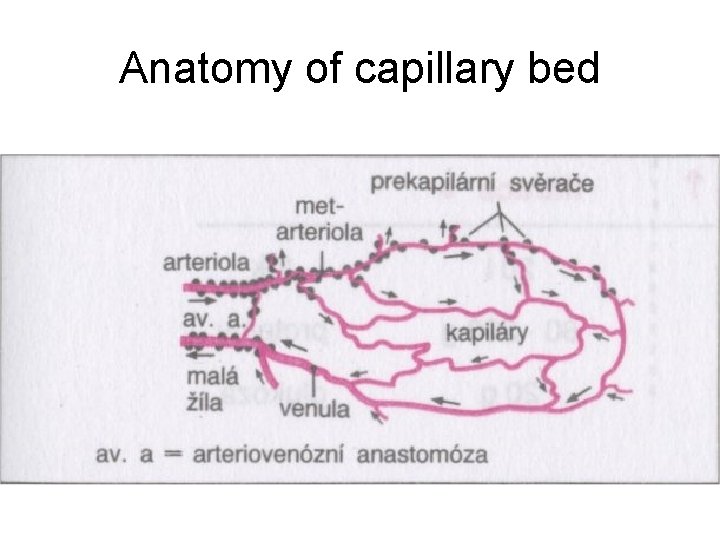
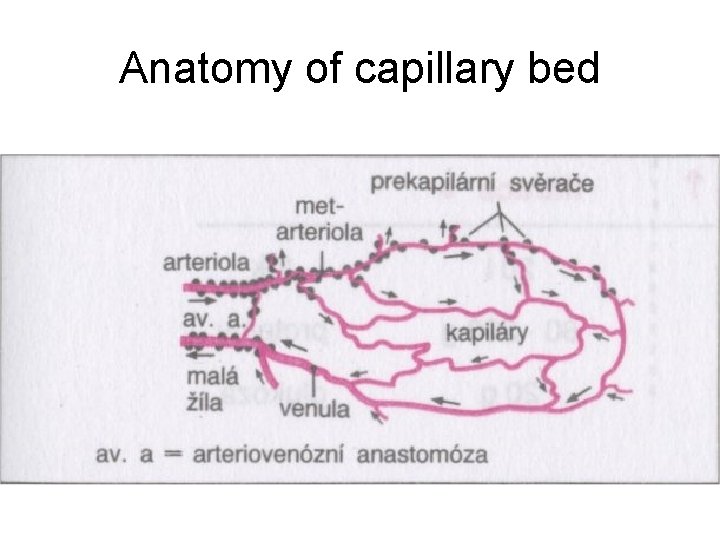
Anatomy of capillary bed
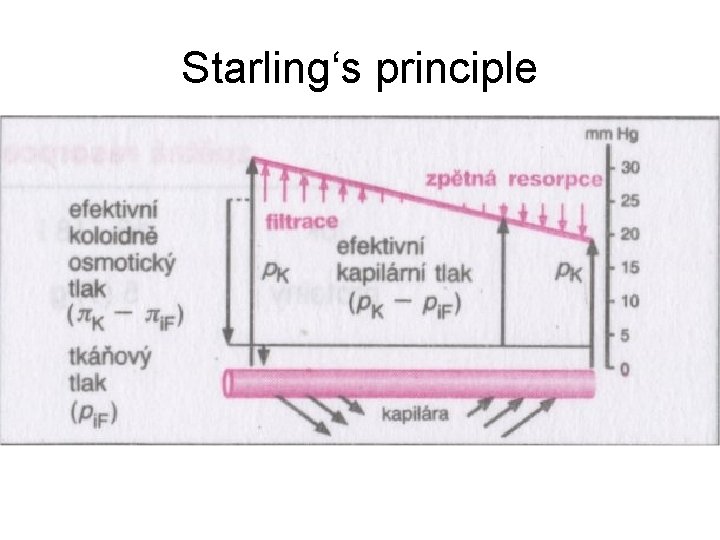
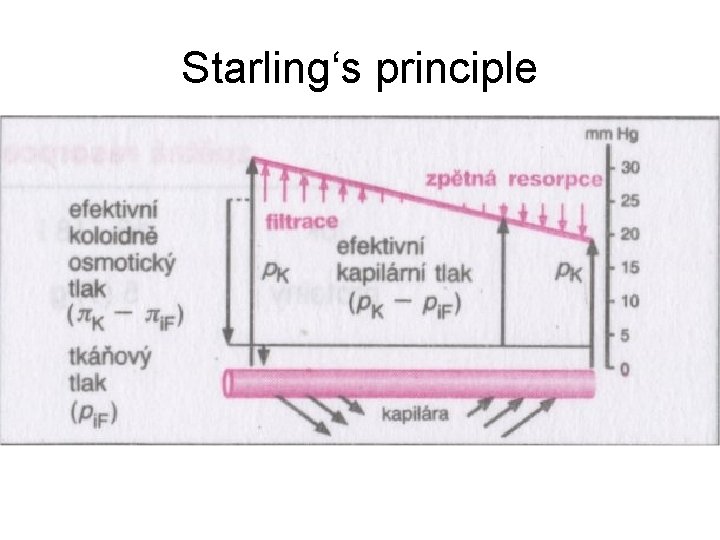
Starling‘s principle
Four signs of inflammation • Rubor et tumor cum calore et (dolore) – caused by hyperaemia of inflammed tissue • Cohenheim 1867 watched and described this events in the mesentery of the living frog
• What happens when arterioles dilate? – Systemic pressure is not affected because limited area is involved – Flow acceleration and capillary pressure rise. – Venules become distended, but capillary dilatation is minimal
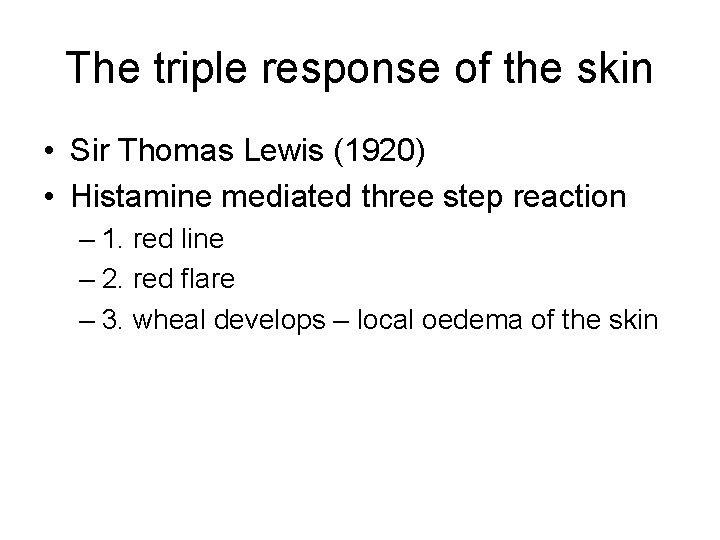
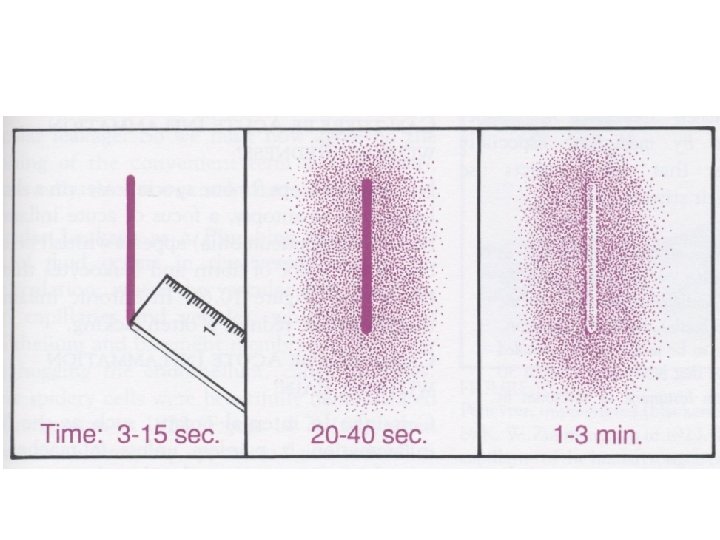
The triple response of the skin • Sir Thomas Lewis (1920) • Histamine mediated three step reaction – 1. red line – 2. red flare – 3. wheal develops – local oedema of the skin
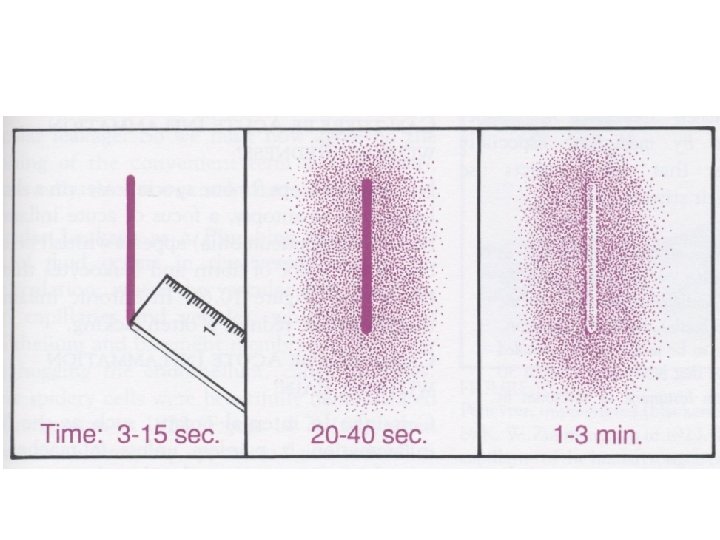
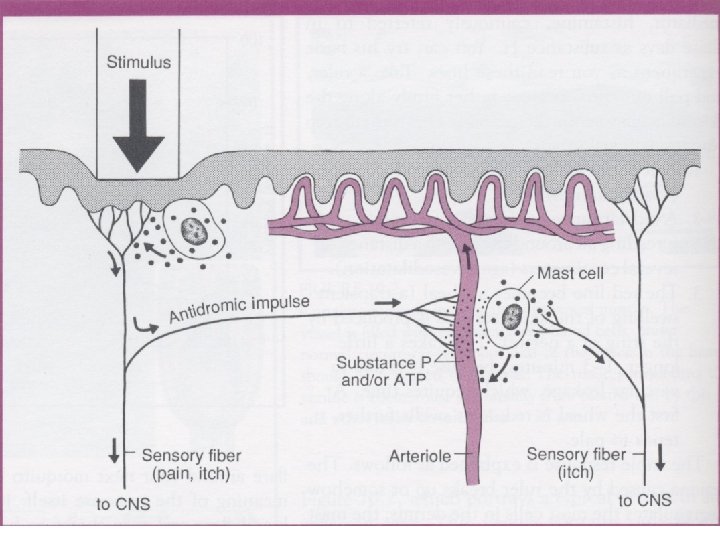
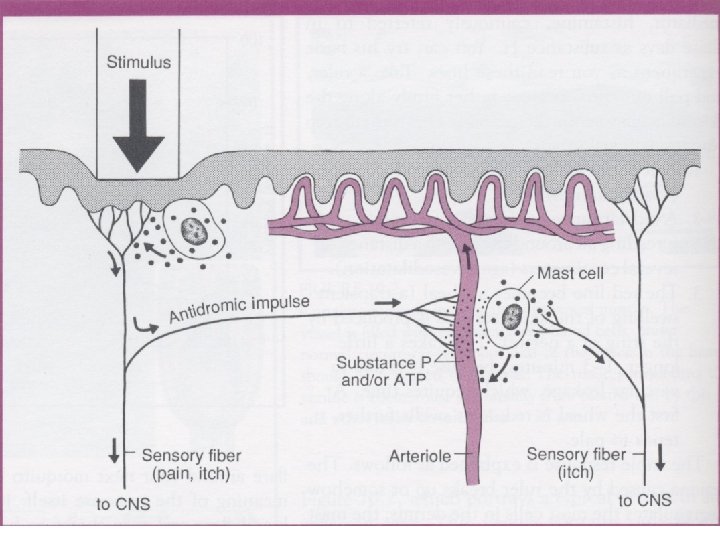
• The initial trauma to the skin releases the histamine. Histamine causes the vasodilatation and vascular leakage. The flare is caused by axon reflex.
Increased perfusion of inflammed tissue • • Dilution of noxious materials. Increased temperature. Thermotaxis? Diapedesis Exudation – antibodies escapes blood vessels
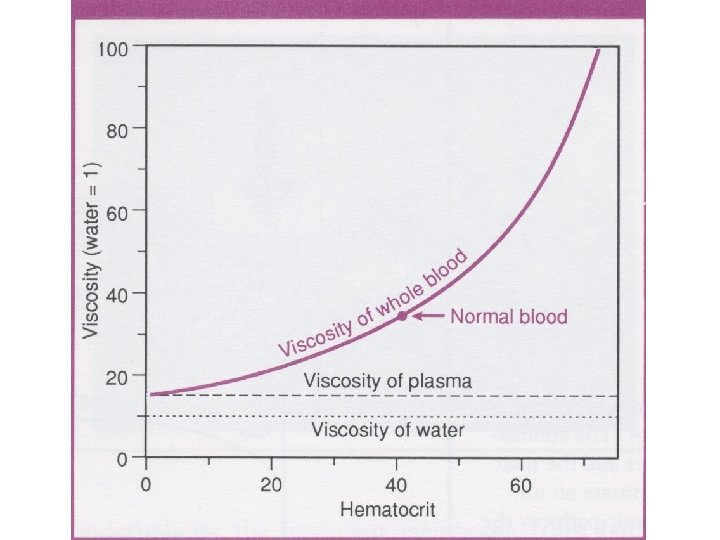
Inflammatory swelling • Vascular leakage • Filtration pressure increase • Reabsorption decrease due to protein escape into extracellular spaces
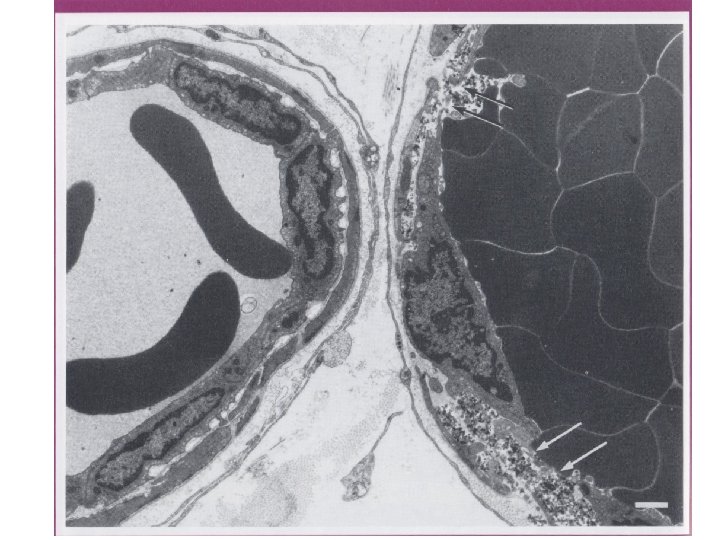
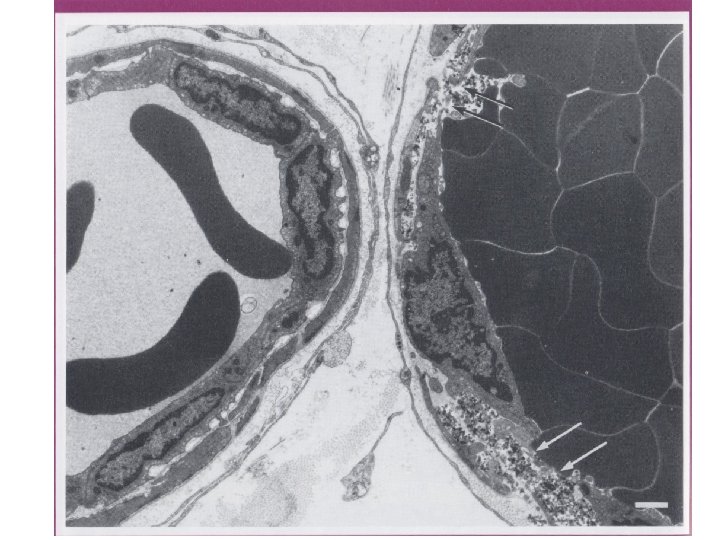
The structure of the capillary wall • Endotelium, BM, pericytes
Mechanisms of vascular leakage • Impairment of endothelial layer causes lost of permeability barrier and plasma leaks out, basement membrane (BM) holds the vessel together • Destruction of BM causes hemorrhage.
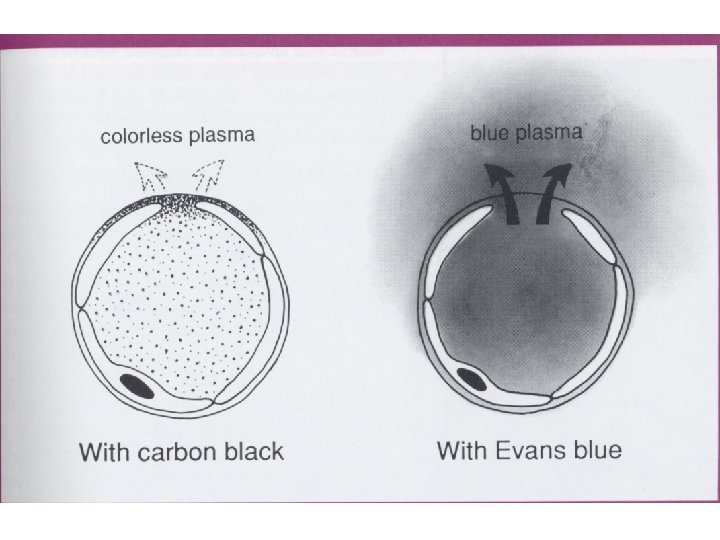
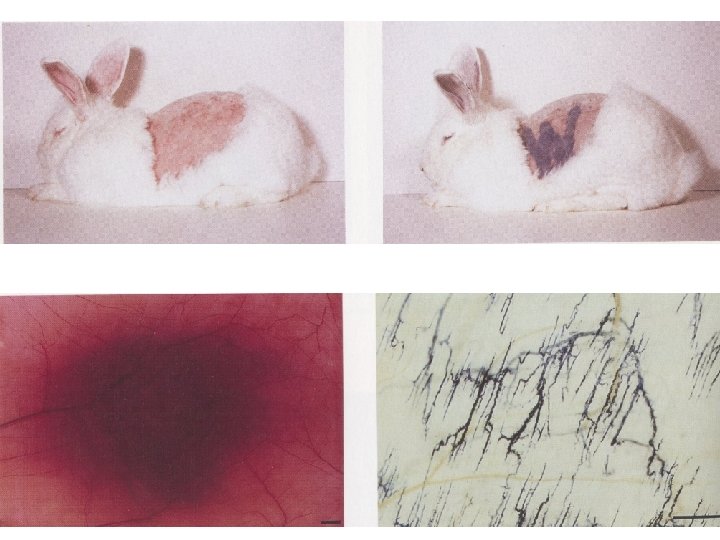
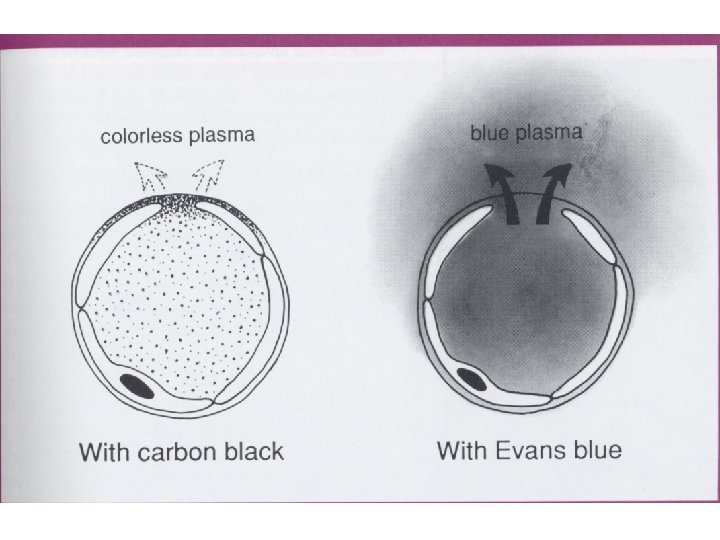
Methods for demonstrating vascular leakage • Soluble dyes • Colloidal suspensions of pigment • Bacteria in circulation tend to localize in inflammed tissue • Presence of fibrin in extracellular space is the histological sign of vascular leak
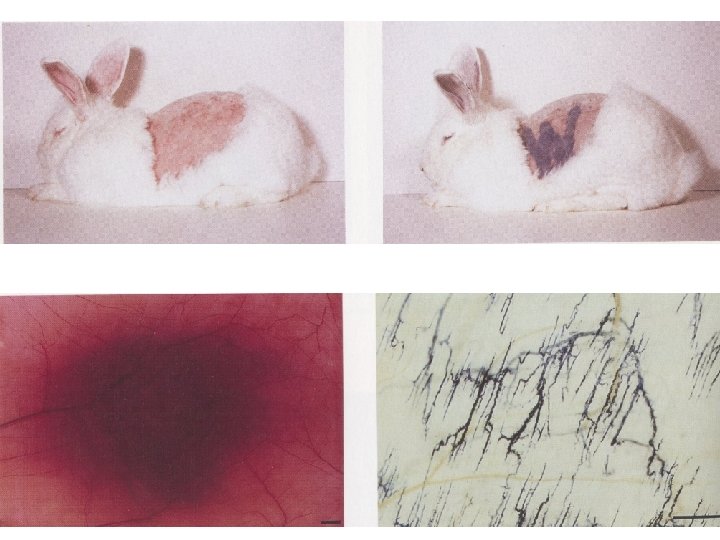
Types of vascular leakage • Direct injury of vessels – destroys endothelia in arterioles, capillaries and venules • Histamine mediated leakage – leakage is restricted only to the venules, endothelia of venules are equipped with histamine receptors and reacts by contracting itself
• Late capillary leakage develops after 12 – 18 • Probably effect of IL-1, TNF a INF-gamma • Cytoskeletal changes
• • • Direct injury Histamine Cytokines Neutrophils Prostaglandins - vasodilatation Regenerating vessels – leaky sprouts