Microbiology Nuts Bolts Opportunistic infections Dr David Garner
Microbiology Nuts & Bolts Opportunistic infections Dr David Garner Consultant Microbiologist Frimley Park Hospital NHS Foundation Trust www. microbiologynutsandbolts. co. uk
Aims & Objectives • To understand the difference between sepsis with neutropaenia and neutropaenic sepsis • To know how to manage neutropaenic sepsis • To be aware of the types of immunodeficiency syndromes • To understand what an opportunistic infection is • To consider opportunist infections in HIV infection www. microbiologynutsandbolts. co. uk
Geoff • • 43 year old On chemotherapy for malignant melanoma Presents with shortness of breath On examination – – Temperature 39. 5 o. C Crackles throughout precordium Heart Rate 120 bpm B. P. 120/75 • How should Geoff be managed? www. microbiologynutsandbolts. co. uk
Differential Diagnosis • Immediately life-threatening • Common • Uncommon • Examination and investigations explore the differential diagnosis • What would be your differential diagnosis for Geoff? www. microbiologynutsandbolts. co. uk
Differential Diagnosis • Immediately life-threatening – Severe sepsis or neutropaenic sepsis, pulmonary embolus, myocardial infarction, meningitis, encephalitis, cholangitis… • Common – Urinary tract infection (UTI), community acquired pneumonia (CAP), cellulitis, cholecystitis, URTI, gastroenteritis, etc… • Uncommon – Opportunistic infection… • How would you investigate this differential diagnosis? www. microbiologynutsandbolts. co. uk
• Full history and examination • Bloods – FBC, CRP, U&Es – Lactate – Blood Cultures • Urine – Dipstick? – MSU • Chest X-ray www. microbiologynutsandbolts. co. uk
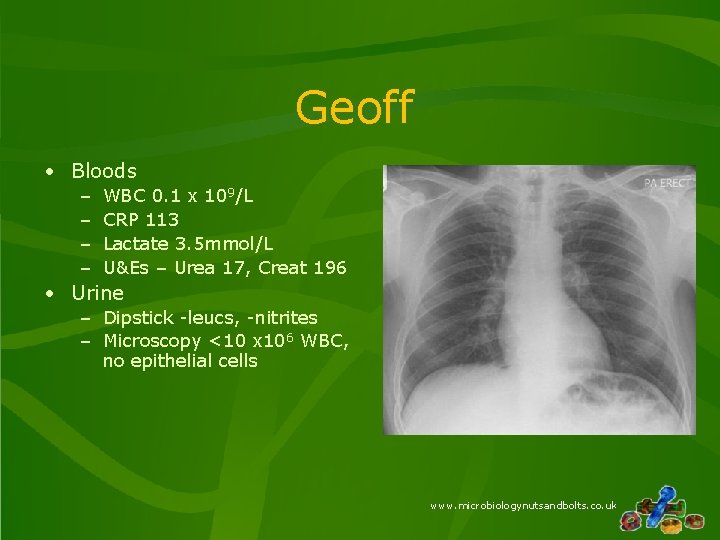
Geoff • Bloods – – WBC 0. 1 x 109/L CRP 113 Lactate 3. 5 mmol/L U&Es – Urea 17, Creat 196 • Urine – Dipstick -leucs, -nitrites – Microscopy <10 x 106 WBC, no epithelial cells www. microbiologynutsandbolts. co. uk
• • What is the diagnosis? How would you manage Geoff now? What is neutropaenic sepsis? What are the common bacterial causes of neutropaenic sepsis? www. microbiologynutsandbolts. co. uk
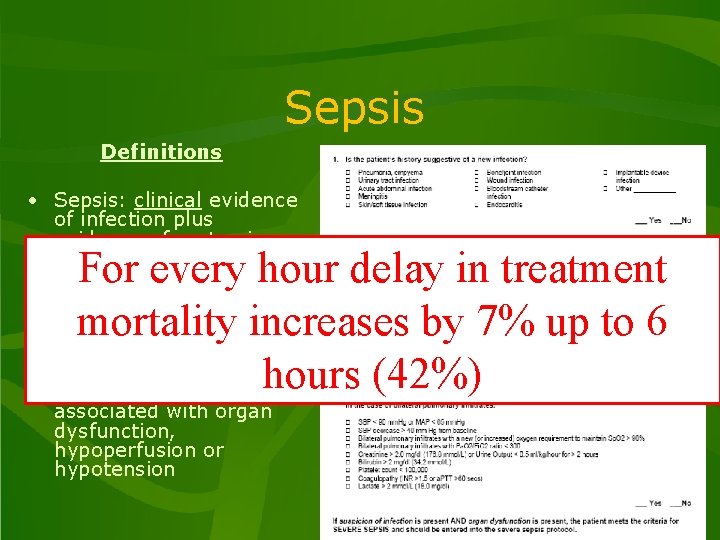
Sepsis Definitions • Sepsis: clinical evidence of infection plus evidence of systemic response to infection • • For every hour delay in treatment Sepsis syndrome: sepsis plus evidenceincreases of mortality by 7% up to 6 altered organ perfusion hours (42%) Severe sepsis: sepsis associated with organ dysfunction, hypoperfusion or hypotension www. microbiologynutsandbolts. co. uk
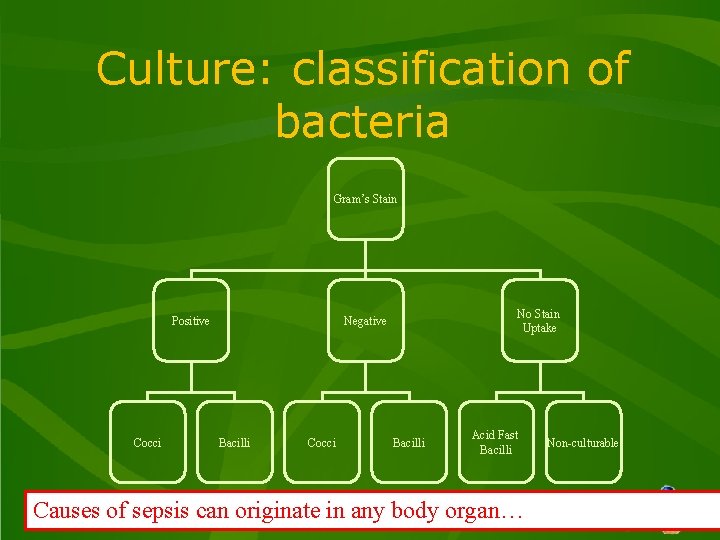
Culture: classification of bacteria Gram’s Stain Positive Cocci No Stain Uptake Negative Bacilli Cocci Bacilli Acid Fast Bacilli Non-culturable Causes of sepsis can originate in any bodywww. microbiologynutsandbolts. co. uk organ…
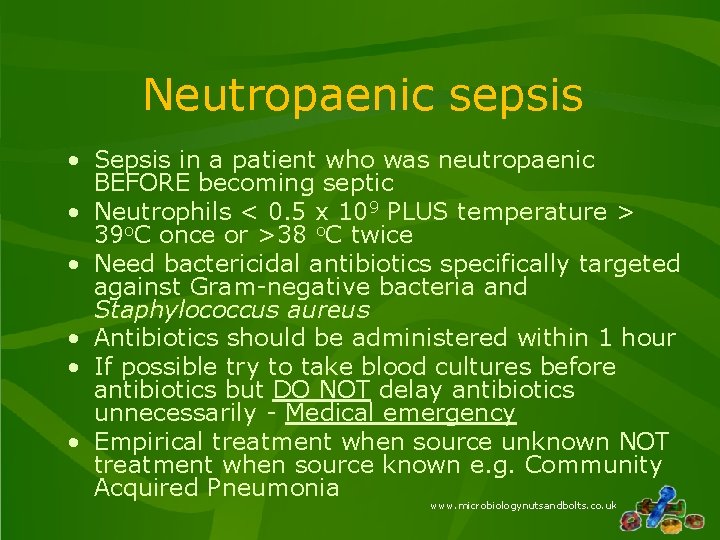
Neutropaenic sepsis • Sepsis in a patient who was neutropaenic BEFORE becoming septic • Neutrophils < 0. 5 x 109 PLUS temperature > 39 o. C once or >38 o. C twice • Need bactericidal antibiotics specifically targeted against Gram-negative bacteria and Staphylococcus aureus • Antibiotics should be administered within 1 hour • If possible try to take blood cultures before antibiotics but DO NOT delay antibiotics unnecessarily - Medical emergency • Empirical treatment when source unknown NOT treatment when source known e. g. Community Acquired Pneumonia www. microbiologynutsandbolts. co. uk
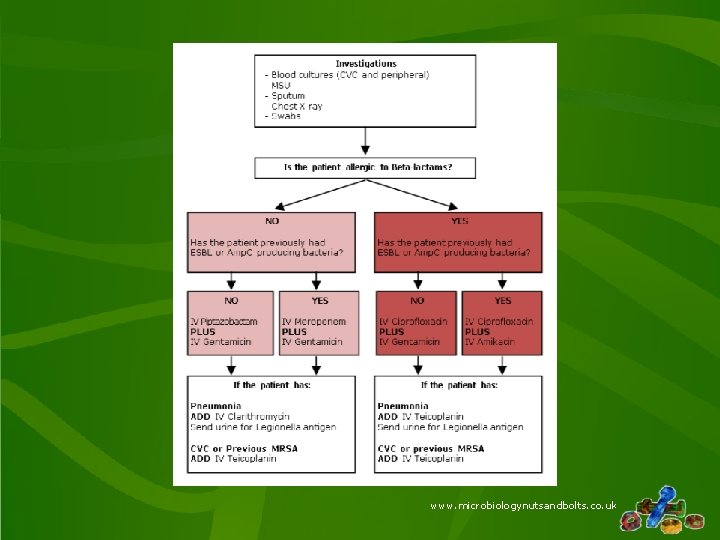
www. microbiologynutsandbolts. co. uk
Opportunist infection • An infection with a microorganism that wouldn’t normally cause an infection in a patient with a normal immune system • Can be: – New microorganism exploiting the lack of immune response – Latent microorganism escaping control of the immune response • Can be bacterial, viral, fungal or parasitic www. microbiologynutsandbolts. co. uk
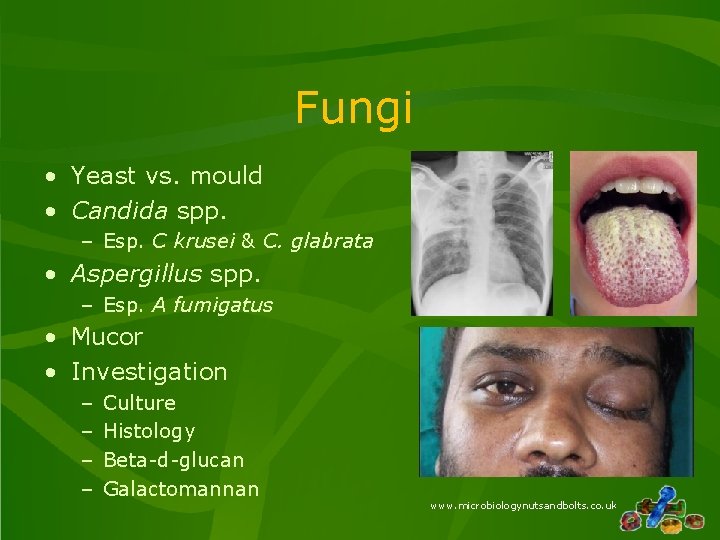
Fungi • Yeast vs. mould • Candida spp. – Esp. C krusei & C. glabrata • Aspergillus spp. – Esp. A fumigatus • Mucor • Investigation – – Culture Histology Beta-d-glucan Galactomannan www. microbiologynutsandbolts. co. uk
Viruses • Post bone marrow transplant – Months – years after! • Severe pneumonitis • High mortality • Viruses – – Respiratory syncytial virus Adenovirus Influenza Parainfluenza www. microbiologynutsandbolts. co. uk
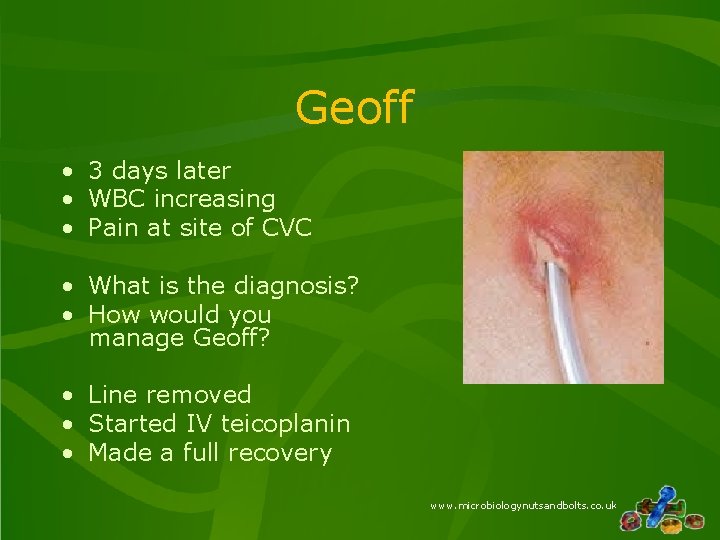
Geoff • 3 days later • WBC increasing • Pain at site of CVC • What is the diagnosis? • How would you manage Geoff? • Line removed • Started IV teicoplanin • Made a full recovery www. microbiologynutsandbolts. co. uk
Types of IV Device • • • Peripheral Venous Catheter Peripheral Arterial Catheter Short-term Central Venous Catheter (CVC) Peripherally Inserted Central Catheter (PICC) Long-term Central Venous Catheter (CVC) e. g. Broviac, Groshong, Hickman catheters Totally Implanted Catheter Pacemaker, cardioverter defibrillator IVC filters Prosthetic vascular grafts www. microbiologynutsandbolts. co. uk
IV Device Infections • Treatment – Targeted at Gram-positive bacteria e. g. Staphylococcus aureus – In immunosuppressed patients additional cover given for Gram-negative bacteria e. g. Pseudomonas aeruginosa, Klebsiella pneumoniae • Usually IV Vancomycin OR IV Teicoplanin PLUS IV Gentamicin • Remove the infected device! www. microbiologynutsandbolts. co. uk
Immunodeficiency states • Primary – Antibody deficiency – T cell deficiency • Secondary – – – Viral Drugs Haematological malignancy Metabolic Immunoglobulin loss Other e. g. splenectomy, percutaneous devices, etc. www. microbiologynutsandbolts. co. uk
Viral - HIV • Human Immunodeficiency Virus causes gradual loss of CD 4 T cells leading to immunodeficiency • Acquired Immune Deficiency Syndrome (AIDS) = group of opportunistic infections which only occur with profound reduction in immune function www. microbiologynutsandbolts. co. uk
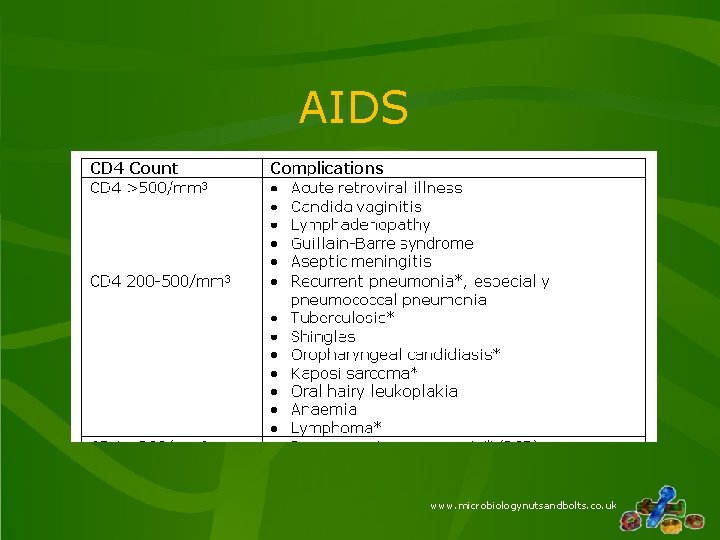
AIDS www. microbiologynutsandbolts. co. uk
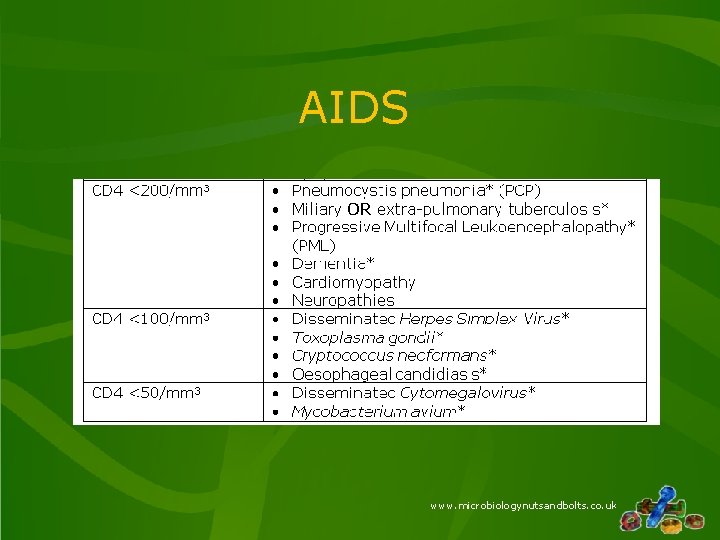
AIDS www. microbiologynutsandbolts. co. uk
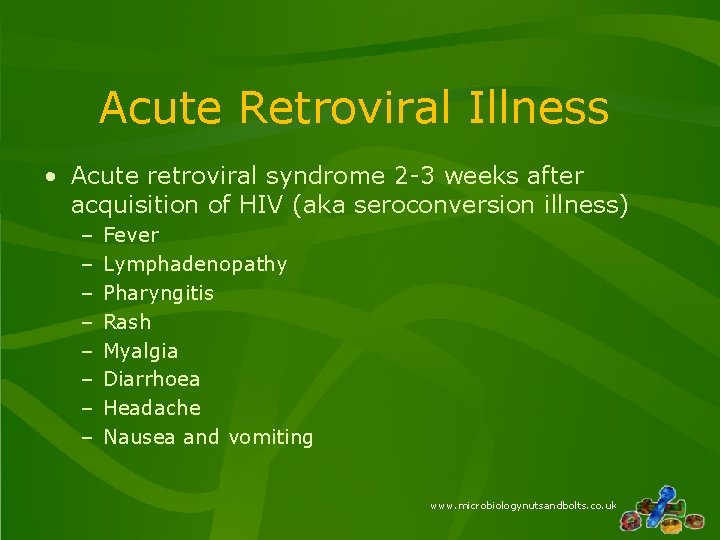
Acute Retroviral Illness • Acute retroviral syndrome 2 -3 weeks after acquisition of HIV (aka seroconversion illness) – – – – Fever Lymphadenopathy Pharyngitis Rash Myalgia Diarrhoea Headache Nausea and vomiting www. microbiologynutsandbolts. co. uk
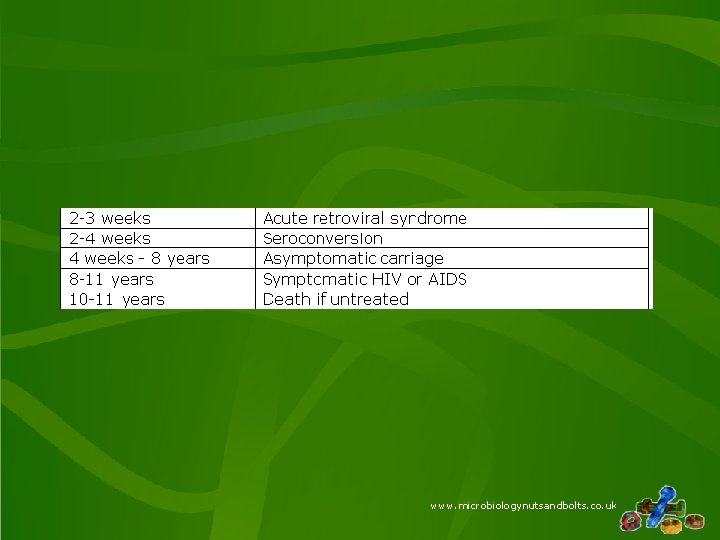
www. microbiologynutsandbolts. co. uk
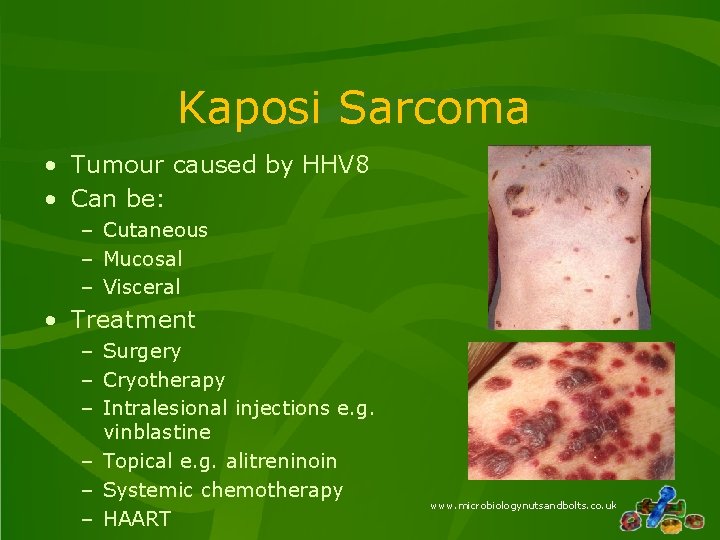
Kaposi Sarcoma • Tumour caused by HHV 8 • Can be: – Cutaneous – Mucosal – Visceral • Treatment – Surgery – Cryotherapy – Intralesional injections e. g. vinblastine – Topical e. g. alitreninoin – Systemic chemotherapy – HAART www. microbiologynutsandbolts. co. uk
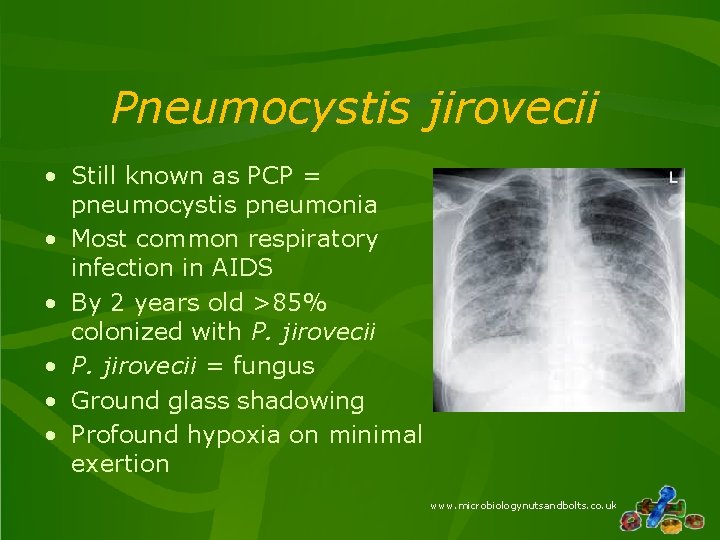
Pneumocystis jirovecii • Still known as PCP = pneumocystis pneumonia • Most common respiratory infection in AIDS • By 2 years old >85% colonized with P. jirovecii • P. jirovecii = fungus • Ground glass shadowing • Profound hypoxia on minimal exertion www. microbiologynutsandbolts. co. uk
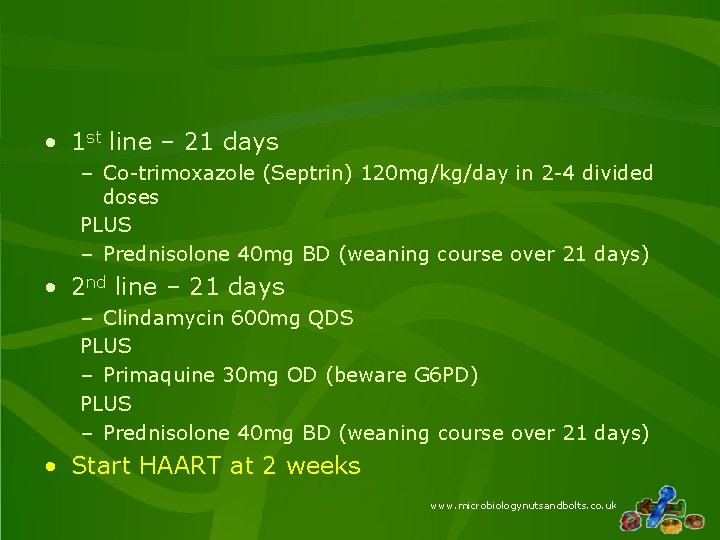
• 1 st line – 21 days – Co-trimoxazole (Septrin) 120 mg/kg/day in 2 -4 divided doses PLUS – Prednisolone 40 mg BD (weaning course over 21 days) • 2 nd line – 21 days – Clindamycin 600 mg QDS PLUS – Primaquine 30 mg OD (beware G 6 PD) PLUS – Prednisolone 40 mg BD (weaning course over 21 days) • Start HAART at 2 weeks www. microbiologynutsandbolts. co. uk
Cryptococcus neoformans • Fungus found in soil • Possible association with pigeons (gut flora? ) • Causes disseminated infection including meningoencephalitis • Worldwide approx. 1, 000 cases/year 600, 000 deaths www. microbiologynutsandbolts. co. uk
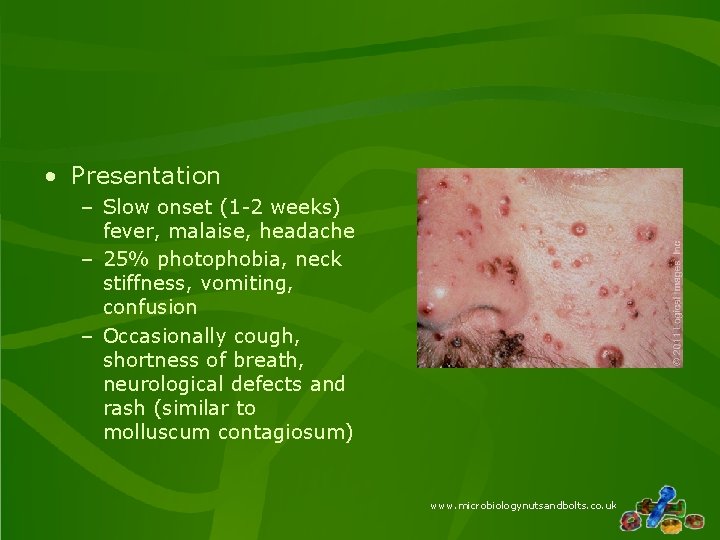
• Presentation – Slow onset (1 -2 weeks) fever, malaise, headache – 25% photophobia, neck stiffness, vomiting, confusion – Occasionally cough, shortness of breath, neurological defects and rash (similar to molluscum contagiosum) www. microbiologynutsandbolts. co. uk
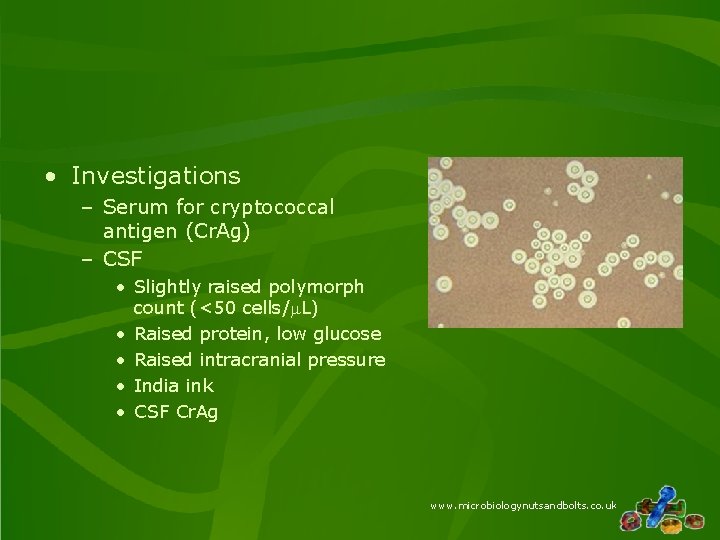
• Investigations – Serum for cryptococcal antigen (Cr. Ag) – CSF • Slightly raised polymorph count (<50 cells/m. L) • Raised protein, low glucose • Raised intracranial pressure • India ink • CSF Cr. Ag www. microbiologynutsandbolts. co. uk
• Induction ≥ 2 weeks – IV Liposomal Amphotericin B 3 -4 mg/kg/day PLUS – PO Flucytosine 25 mg/kg QDS (or Fluconazole 800 mg OD) • Consolidation 8 weeks – PO Fluconazole 400 mg OD • Maintenance ≥ 1 year – PO Fluconazole 200 mg OD • HAART 2 -10 weeks after starting treatment • Monitor CD 4 and serum Cr. Ag lifelong www. microbiologynutsandbolts. co. uk
Cytomegalovirus • • HHV 5 Latent infection Reactivates in immunosuppression Can cause: – – – Retinitis Pneumonitis Colitis Meningoencephalitis Peripheral neuropathy www. microbiologynutsandbolts. co. uk

www. microbiologynutsandbolts. co. uk
• 1 st Line – IV Ganciclovir • 2 nd Line – IV Foscarnet • Increasing role for PO Valganciclovir www. microbiologynutsandbolts. co. uk
Conclusions • Neutropaenic sepsis is sepsis that occurs in patients who are neutropaenic before septic • Neutropaenic sepsis is a medical emergency • Opportunistic infections are infections that would not occur in immunocompetent patients • Secondary infections in HIV relate to the CD 4 count • Immunosuppressed patients with infections need regular assessment until the underlying infection declares itself www. microbiologynutsandbolts. co. uk
Any Questions? www. microbiologynutsandbolts. co. uk
- Slides: 36