Microbiology Chapter 19 Microbial Diseases of the Skin
Microbiology Chapter 19 Microbial Diseases of the Skin and Wounds © 2018 Pearson Education, Inc.
Function and Components of the Integumentary System • Physical • Epidermis – stratified squamous epithelium • Dermis – sweat glands, oil glands with hair follicles, sensory nerve endings, capillaries • Immunological • Macrophages, Dendritic cells • Microbiological – resident microbiota • Staphylococcus, Micrococcus, Malassezia, Corynebacteria, Propionibacteria, Pseudomonas © 2018 Pearson Education, Inc.
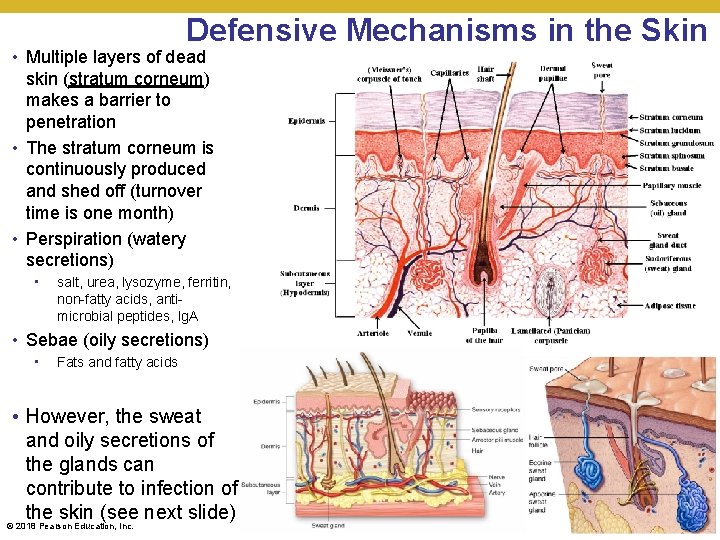
Defensive Mechanisms in the Skin • Multiple layers of dead skin (stratum corneum) makes a barrier to penetration • The stratum corneum is continuously produced and shed off (turnover time is one month) • Perspiration (watery secretions) • salt, urea, lysozyme, ferritin, non-fatty acids, antimicrobial peptides, Ig. A • Sebae (oily secretions) • Fats and fatty acids • However, the sweat and oily secretions of the glands can contribute to infection of the skin (see next slide) © 2018 Pearson Education, Inc.
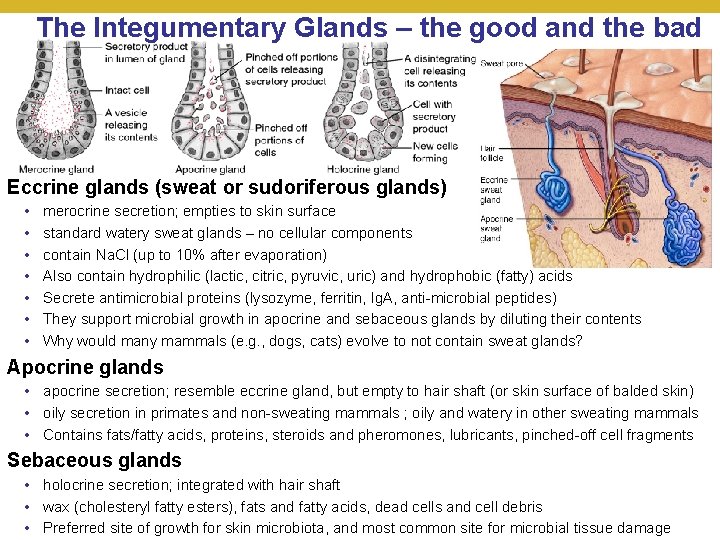
The Integumentary Glands – the good and the bad Eccrine glands (sweat or sudoriferous glands) • • merocrine secretion; empties to skin surface standard watery sweat glands – no cellular components contain Na. Cl (up to 10% after evaporation) Also contain hydrophilic (lactic, citric, pyruvic, uric) and hydrophobic (fatty) acids Secrete antimicrobial proteins (lysozyme, ferritin, Ig. A, anti-microbial peptides) They support microbial growth in apocrine and sebaceous glands by diluting their contents Why would many mammals (e. g. , dogs, cats) evolve to not contain sweat glands? Apocrine glands • apocrine secretion; resemble eccrine gland, but empty to hair shaft (or skin surface of balded skin) • oily secretion in primates and non-sweating mammals ; oily and watery in other sweating mammals • Contains fats/fatty acids, proteins, steroids and pheromones, lubricants, pinched-off cell fragments Sebaceous glands • holocrine secretion; integrated with hair shaft • wax (cholesteryl fatty esters), fats and fatty acids, dead cells and cell debris © 2018 Education, Inc. of growth for skin microbiota, and most common site for microbial tissue damage • Pearson Preferred site
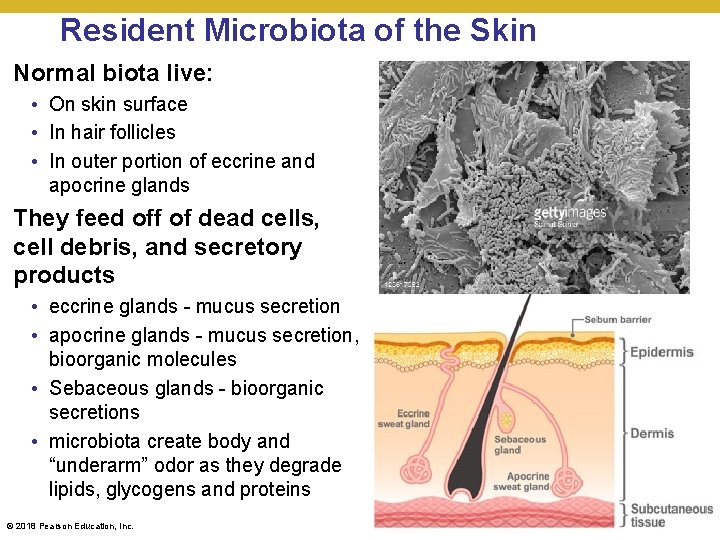
Resident Microbiota of the Skin Normal biota live: • On skin surface • In hair follicles • In outer portion of eccrine and apocrine glands They feed off of dead cells, cell debris, and secretory products • eccrine glands - mucus secretion • apocrine glands - mucus secretion, bioorganic molecules • Sebaceous glands - bioorganic secretions • microbiota create body and “underarm” odor as they degrade lipids, glycogens and proteins © 2018 Pearson Education, Inc.
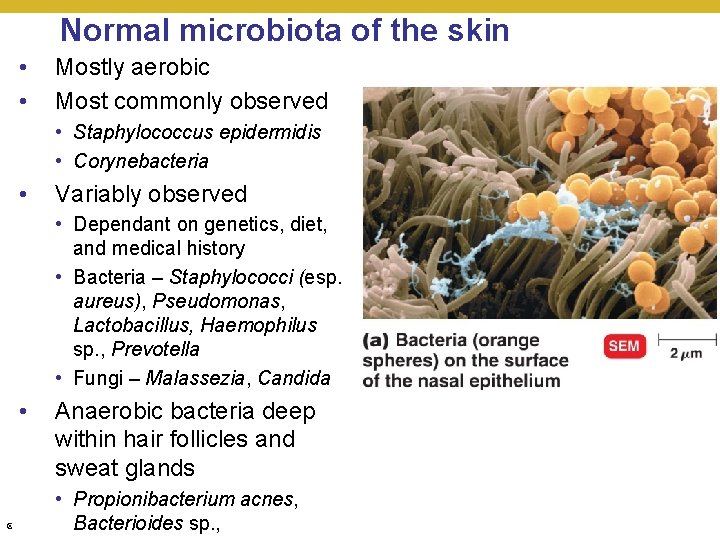
Normal microbiota of the skin • • Mostly aerobic Most commonly observed • Staphylococcus epidermidis • Corynebacteria • Variably observed • Dependant on genetics, diet, and medical history • Bacteria – Staphylococci (esp. aureus), Pseudomonas, Lactobacillus, Haemophilus sp. , Prevotella • Fungi – Malassezia, Candida • Anaerobic bacteria deep within hair follicles and sweat glands • Propionibacterium acnes, © 2018 Pearson Bacterioides Education, Inc. sp. ,
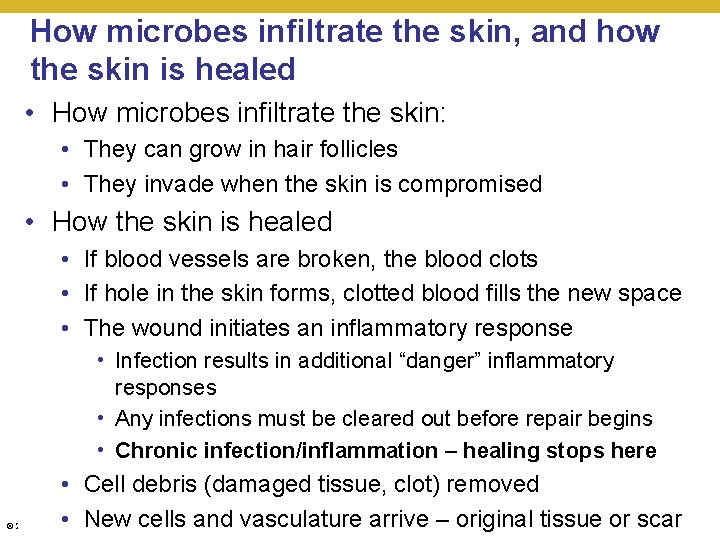
How microbes infiltrate the skin, and how the skin is healed • How microbes infiltrate the skin: • They can grow in hair follicles • They invade when the skin is compromised • How the skin is healed • If blood vessels are broken, the blood clots • If hole in the skin forms, clotted blood fills the new space • The wound initiates an inflammatory response • Infection results in additional “danger” inflammatory responses • Any infections must be cleared out before repair begins • Chronic infection/inflammation – healing stops here • Cell debris (damaged tissue, clot) removed • New cells and vasculature arrive – original tissue or scar © 2018 Pearson Education, Inc.
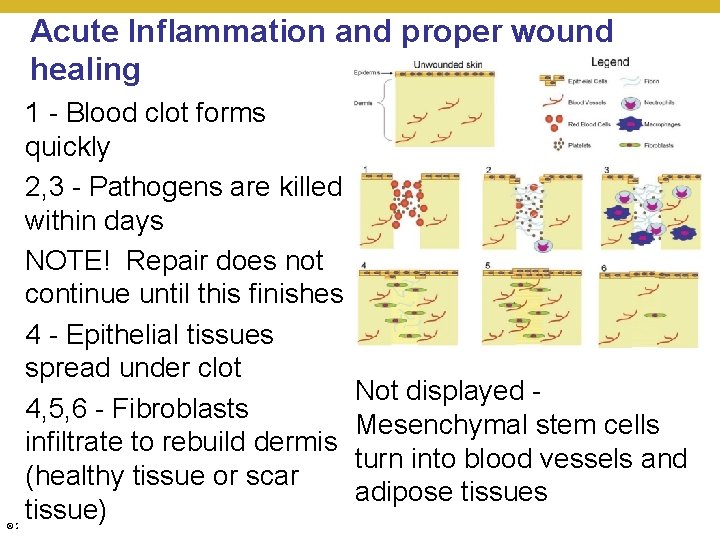
Acute Inflammation and proper wound healing 1 - Blood clot forms quickly 2, 3 - Pathogens are killed within days NOTE! Repair does not continue until this finishes 4 - Epithelial tissues spread under clot 4, 5, 6 - Fibroblasts infiltrate to rebuild dermis (healthy tissue or scar tissue) © 2018 Pearson Education, Inc. Not displayed Mesenchymal stem cells turn into blood vessels and adipose tissues
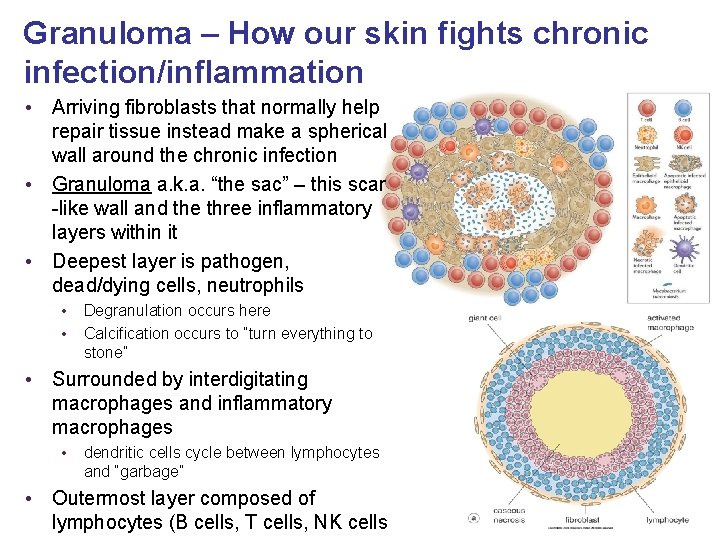
Granuloma – How our skin fights chronic infection/inflammation • Arriving fibroblasts that normally help repair tissue instead make a spherical wall around the chronic infection • Granuloma a. k. a. “the sac” – this scar -like wall and the three inflammatory layers within it • Deepest layer is pathogen, dead/dying cells, neutrophils • • Degranulation occurs here Calcification occurs to “turn everything to stone” • Surrounded by interdigitating macrophages and inflammatory macrophages • dendritic cells cycle between lymphocytes and “garbage” • Outermost layer composed of lymphocytes (B cells, T cells, NK cells
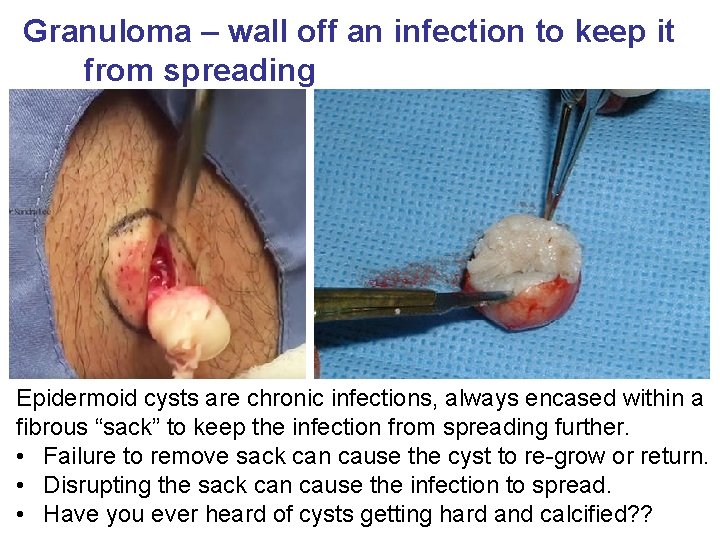
Granuloma – wall off an infection to keep it from spreading Epidermoid cysts are chronic infections, always encased within a fibrous “sack” to keep the infection from spreading further. • Failure to remove sack can cause the cyst to re-grow or return. • Disrupting the sack can cause the infection to spread. • Have you ever heard of cysts getting hard and calcified? ?
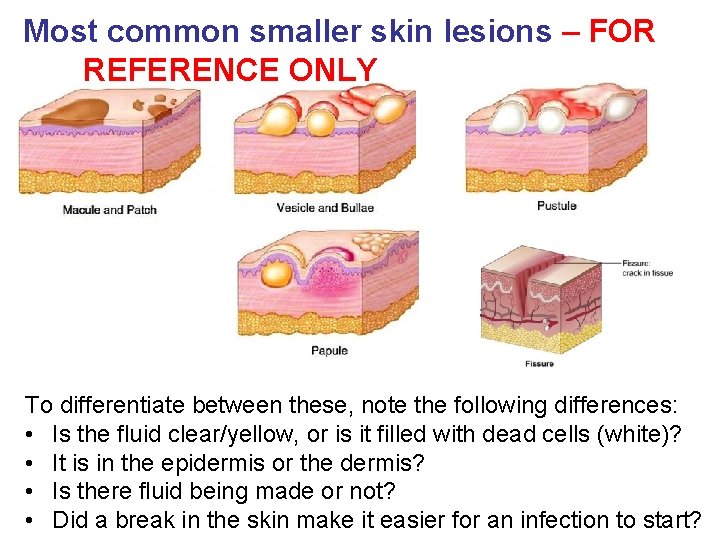
Most common smaller skin lesions – FOR REFERENCE ONLY To differentiate between these, note the following differences: • Is the fluid clear/yellow, or is it filled with dead cells (white)? • It is in the epidermis or the dermis? • Is there fluid being made or not? • Did a break in the skin make it easier for an infection to start?
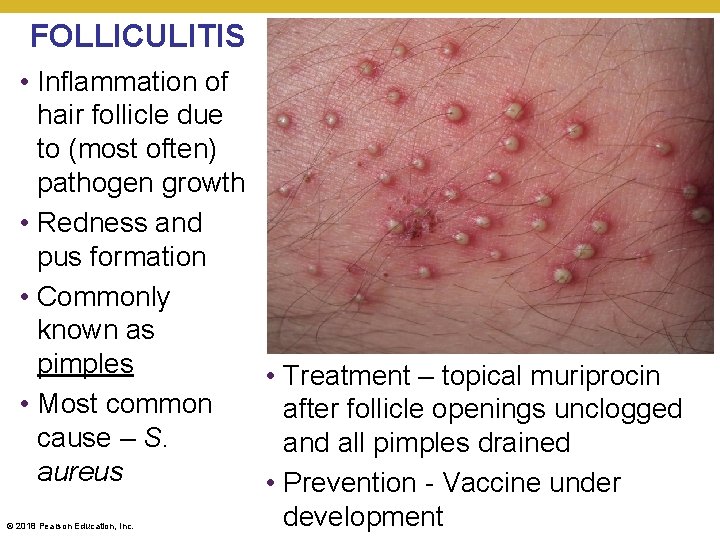
FOLLICULITIS • Inflammation of hair follicle due to (most often) pathogen growth • Redness and pus formation • Commonly known as pimples • Treatment – topical muriprocin • Most common after follicle openings unclogged cause – S. and all pimples drained aureus • Prevention - Vaccine under development © 2018 Pearson Education, Inc.
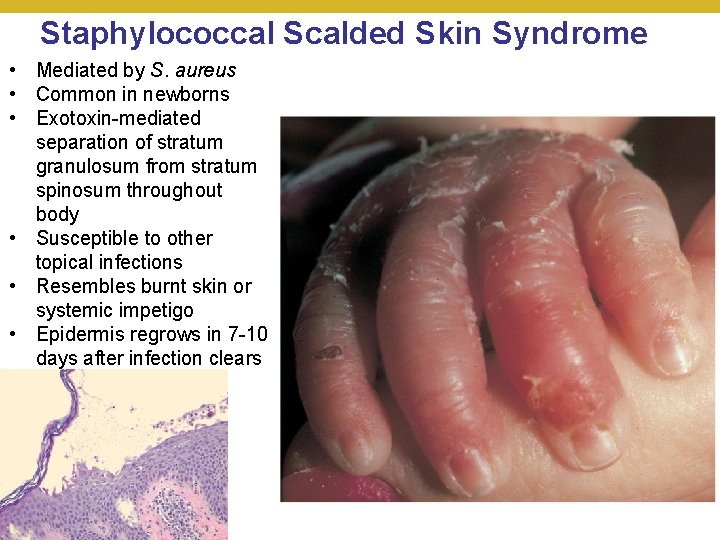
Staphylococcal Scalded Skin Syndrome • Mediated by S. aureus • Common in newborns • Exotoxin-mediated separation of stratum granulosum from stratum spinosum throughout body • Susceptible to other topical infections • Resembles burnt skin or systemic impetigo • Epidermis regrows in 7 -10 days after infection clears © 2018 Pearson Education, Inc.
Streptococcal Skin diseases – SUMMARY SLIDE • Impetigo • 80% Staphylococcus aureus • 20% Streptococcus pyogenes • Infection usually limited to the epidermis; local • Cellulitis • Same agents as impetigo • Infection spreads to the dermis; systemic • Erysipelas • Most cases involve S. pyogenes • Infection spreads into the dermis and progresses through the lymph nodes; systemic • Necrotizing fasciitis • Most cases involve S. pyogenes • Infection spreads to underlying tissues; systemic © 2018 Pearson Education, Inc.
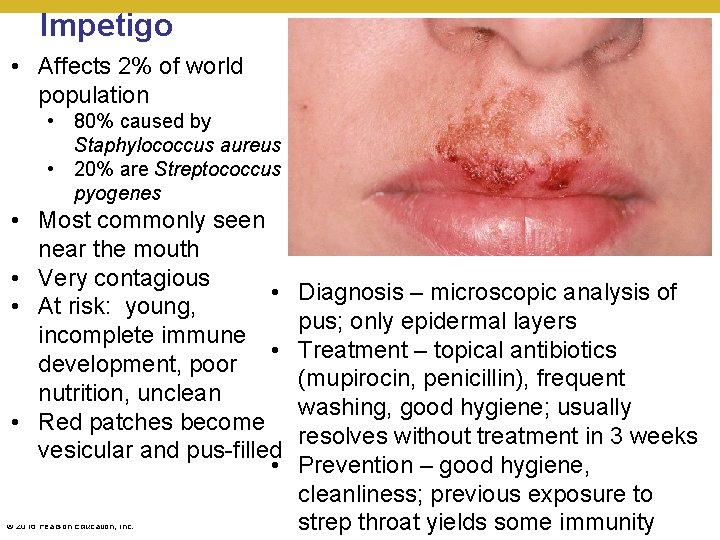
Impetigo • Affects 2% of world population • 80% caused by Staphylococcus aureus • 20% are Streptococcus pyogenes • Most commonly seen near the mouth • Very contagious • • At risk: young, incomplete immune • development, poor nutrition, unclean • Red patches become vesicular and pus-filled • © 2018 Pearson Education, Inc. Diagnosis – microscopic analysis of pus; only epidermal layers Treatment – topical antibiotics (mupirocin, penicillin), frequent washing, good hygiene; usually resolves without treatment in 3 weeks Prevention – good hygiene, cleanliness; previous exposure to strep throat yields some immunity
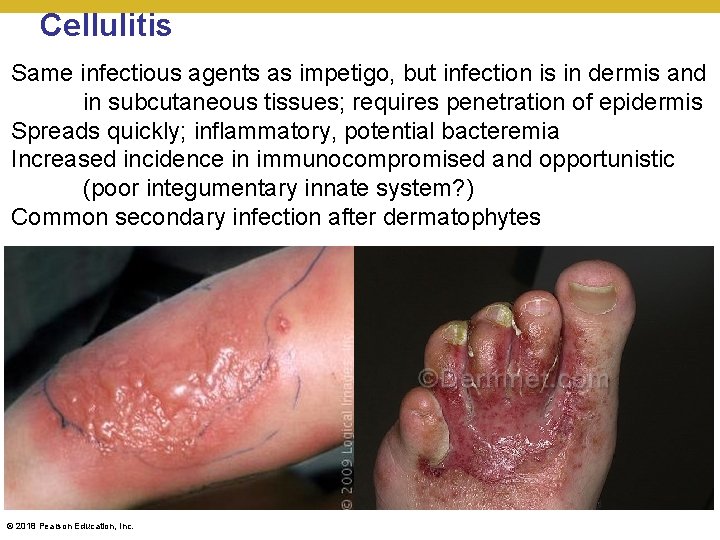
Cellulitis Same infectious agents as impetigo, but infection is in dermis and in subcutaneous tissues; requires penetration of epidermis Spreads quickly; inflammatory, potential bacteremia Increased incidence in immunocompromised and opportunistic (poor integumentary innate system? ) Common secondary infection after dermatophytes © 2018 Pearson Education, Inc.

Erysipelas • Can present with impetigo • Most common cause is substrains of Streptococcus • pyogenes with increased virulence • Migration into dermis and into lymph nodes • • Shiny red, well-defined zones of infection • • High fever, pain, soreness © 2018 Pearson Education, Inc. If left untreated: • Risk of development into acute glomerulonephritis • Mortality can approach 2 -17% (higher if young, old, or immuno-compromised) Diagnosis – microscopic analysis of skin cultures; wide-spread redness Treatment – oral clindamycin or doxycycline; usually resolves in a week • Prevention – good hygiene, cleanliness; previous exposure to strep throat yields some immunity
![Necrotizing fasciitis • A. k. a. flesh-eating [bacterial] disease • Most common cause is Necrotizing fasciitis • A. k. a. flesh-eating [bacterial] disease • Most common cause is](http://slidetodoc.com/presentation_image_h2/7640515ead02da840c461e814eb75b9c/image-18.jpg)
Necrotizing fasciitis • A. k. a. flesh-eating [bacterial] disease • Most common cause is substrains of Streptococcus pyogenes with greatly increased virulence and poor immunity • Sudden onset disease • Rapid migration into subdermal tissues • High fever, pain, soreness progresses into septic shock • Medical emergency or death is certain • Diagnosis – microscopic analysis of skin cultures; necrotic tissue • Treatment – extensive surgery and broad-spectrum combination antibiotics (clindamycin and penicillin) • Prevention – good hygiene, cleanliness; early treatment of impetigo or erysipelas © 2018 Pearson Education, Inc.
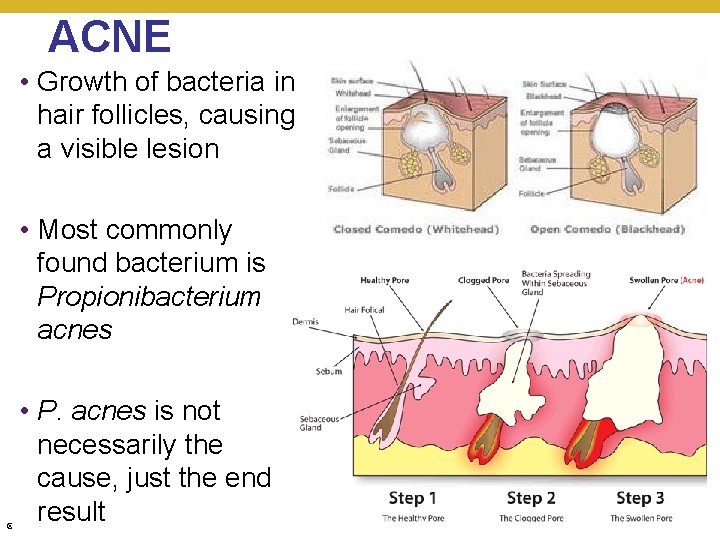
ACNE • Growth of bacteria in hair follicles, causing a visible lesion • Most commonly found bacterium is Propionibacterium acnes • P. acnes is not necessarily the cause, just the end result © 2018 Pearson Education, Inc.
Classifications of Acne • Based on severity of acne; problems additive • Comedonal (mild) acne • Growth of bacteria under anaerobic conditions • Pore clogged with skin; fully anaerobic – comedo “whitehead” • Pore “open” to air but clogged with sebum – open comedo “blackhead” • Inflammatory (moderate) acne • Lymphocytes recruited to comedo; redness (pimples) • Cystic (severe) acne • Comedo expands to deeper skin; called cyst • Becomes painful and medically dangerous (internal rupture) © 2018 Pearson Education, Inc.

Comedonal Acne • Treatment § Topical agents – azelaic acid § Salicyclic acid preparations § Retinoids (tretinoin, tazarotene, adapalene) © 2018 Pearson Education, Inc.
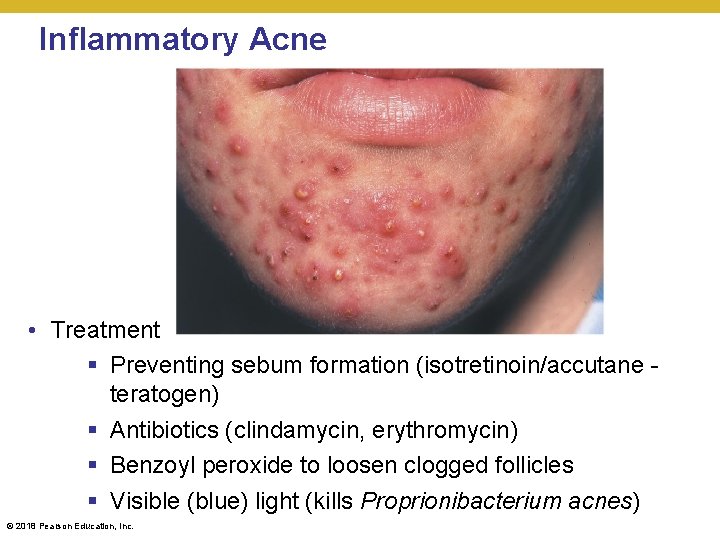
Inflammatory Acne • Treatment § Preventing sebum formation (isotretinoin/accutane teratogen) § Antibiotics (clindamycin, erythromycin) § Benzoyl peroxide to loosen clogged follicles § Visible (blue) light (kills Proprionibacterium acnes) © 2018 Pearson Education, Inc.
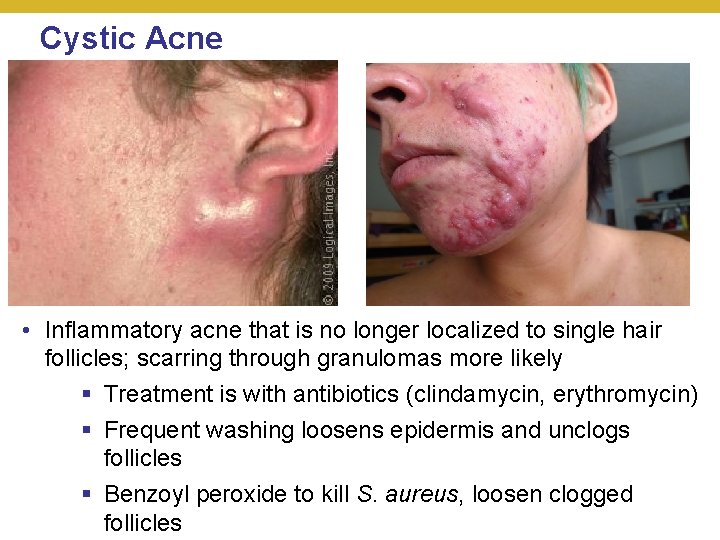
Cystic Acne • Inflammatory acne that is no longer localized to single hair follicles; scarring through granulomas more likely § Treatment is with antibiotics (clindamycin, erythromycin) § Frequent washing loosens epidermis and unclogs follicles § Benzoyl peroxide to kill S. aureus, loosen clogged follicles © 2018 Pearson Education, Inc.

Boils Resembles acne in that hair follicles are infected, but… • most common agent: Staphylococcus aureus (chronic) • furuncle (one hair follicle; surface) • carbuncle (many hair follicles; deeper) • greater chance of systemic infection and more contagious • more medically serious than acne © 2018 Pearson Education, Inc.
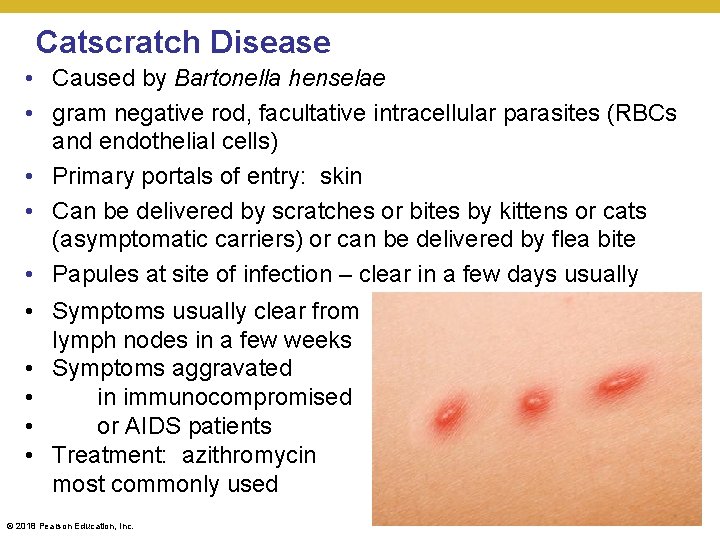
Catscratch Disease • Caused by Bartonella henselae • gram negative rod, facultative intracellular parasites (RBCs and endothelial cells) • Primary portals of entry: skin • Can be delivered by scratches or bites by kittens or cats (asymptomatic carriers) or can be delivered by flea bite • Papules at site of infection – clear in a few days usually • Symptoms usually clear from lymph nodes in a few weeks • Symptoms aggravated • in immunocompromised • or AIDS patients • Treatment: azithromycin most commonly used © 2018 Pearson Education, Inc.
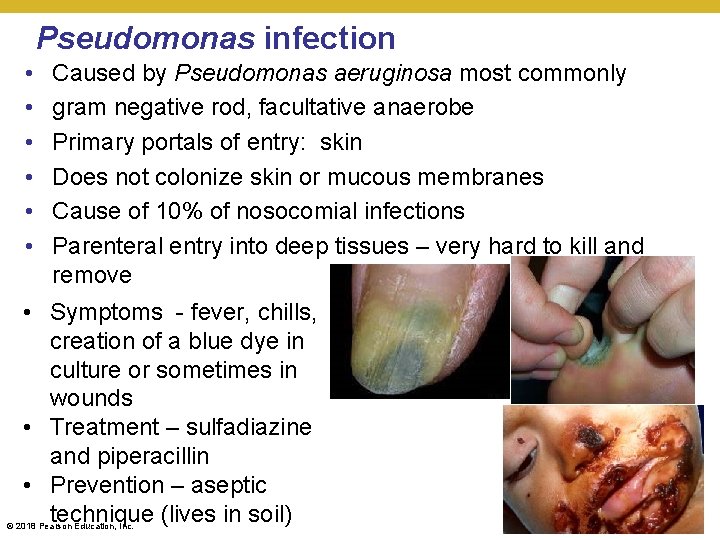
Pseudomonas infection • • • Caused by Pseudomonas aeruginosa most commonly gram negative rod, facultative anaerobe Primary portals of entry: skin Does not colonize skin or mucous membranes Cause of 10% of nosocomial infections Parenteral entry into deep tissues – very hard to kill and remove • Symptoms - fever, chills, creation of a blue dye in culture or sometimes in wounds • Treatment – sulfadiazine and piperacillin • Prevention – aseptic technique (lives in soil) © 2018 Pearson Education, Inc.

Rickettsial Spotted Fevers • Also called Rocky Mountain spotted fever • Caused by Rickettsia rickettsii • Measles-like rash, except that the rash also appears on palms and soles • Spread by a wood tick, dog tick, Lone Star tick © 2018 Pearson Education, Inc.
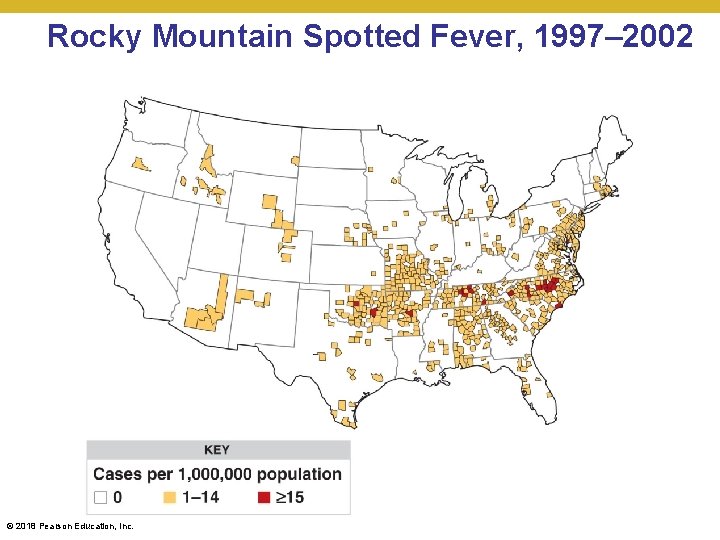
Rocky Mountain Spotted Fever, 1997– 2002 © 2018 Pearson Education, Inc.
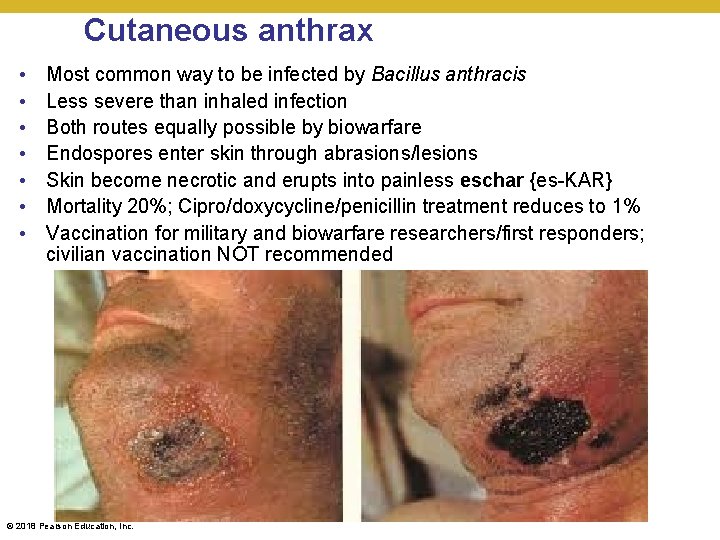
Cutaneous anthrax • • Most common way to be infected by Bacillus anthracis Less severe than inhaled infection Both routes equally possible by biowarfare Endospores enter skin through abrasions/lesions Skin become necrotic and erupts into painless eschar {es-KAR} Mortality 20%; Cipro/doxycycline/penicillin treatment reduces to 1% Vaccination for military and biowarfare researchers/first responders; civilian vaccination NOT recommended © 2018 Pearson Education, Inc.
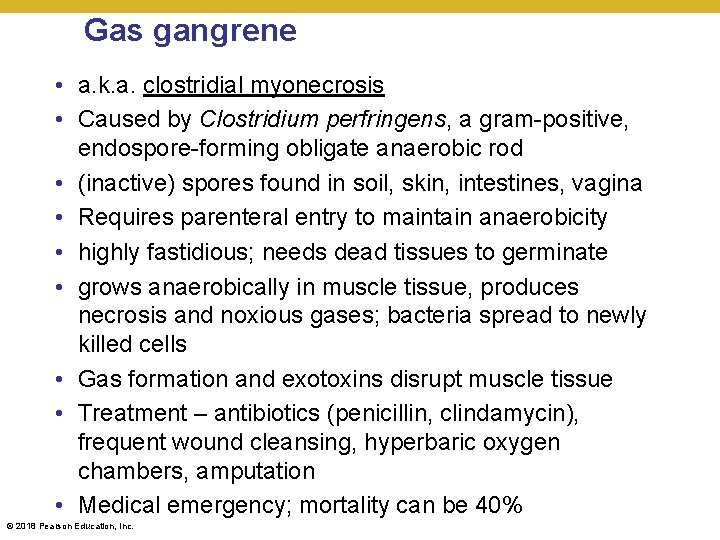
Gas gangrene • a. k. a. clostridial myonecrosis • Caused by Clostridium perfringens, a gram-positive, endospore-forming obligate anaerobic rod • (inactive) spores found in soil, skin, intestines, vagina • Requires parenteral entry to maintain anaerobicity • highly fastidious; needs dead tissues to germinate • grows anaerobically in muscle tissue, produces necrosis and noxious gases; bacteria spread to newly killed cells • Gas formation and exotoxins disrupt muscle tissue • Treatment – antibiotics (penicillin, clindamycin), frequent wound cleansing, hyperbaric oxygen chambers, amputation • Medical emergency; mortality can be 40% © 2018 Pearson Education, Inc.
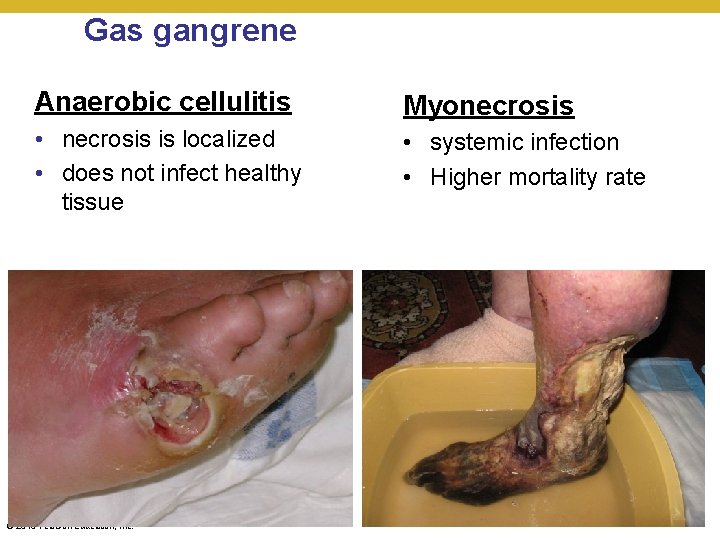
Gas gangrene Anaerobic cellulitis Myonecrosis • necrosis is localized • does not infect healthy tissue • systemic infection • Higher mortality rate © 2018 Pearson Education, Inc.
Viral skin diseases – SUMMARY SLIDE Poxviruses Herpesviruses Papillomaviruses Chickenpox/Shingles Rubella Measles Other childhood diseases Erythema Infectiosum Roseola © 2018 Pearson Education, Inc.

Smallpox Viruses • Smallpox (variola) § Smallpox virus (orthopox virus) • Variola major has 20% mortality • Variola minor has <1% mortality § Eradicated by vaccination by 1979 § Pre-2001, last vaccinations done in 1970 s § ACAM 2000 is military-only vaccine for smallpox biowarfare responders; significant side effects • Monkeypox § Monkey version of small pox § Transmitted through prairie dogs and African rats § Prevention by smallpox vaccination © 2018 Pearson Education, Inc.
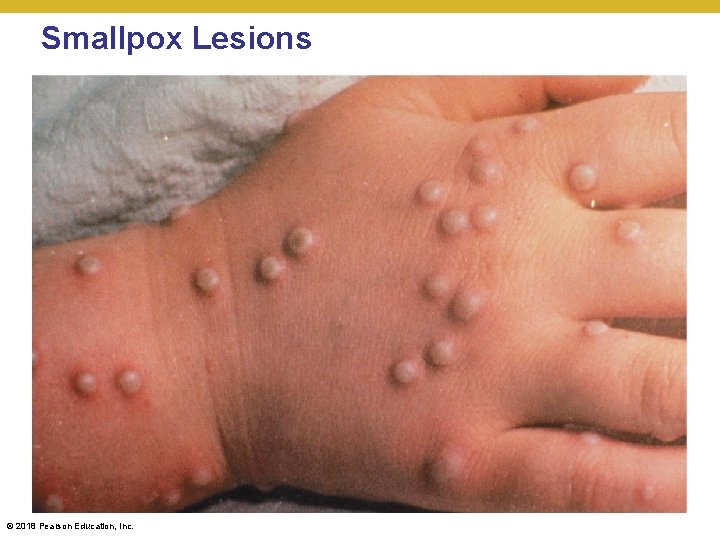
Smallpox Lesions © 2018 Pearson Education, Inc.

HSV-1/HHV-1 infection • Oral Herpes • Signs and symptoms • Presence of cold sores near lips, where nerve density is highest and skin flexing greatest • Pathogen and pathogenesis • 80% by human herpesvirus 1 (HHV-1); remainder HHV-2 • Virions form syncytia to avoid host’s immune system • Latency established in the trigeminal nerve ganglion • Epidemiology • Infections occur by casual contact in childhood (parent to child most often) • 80% of population has HHV-1 antibodies by age 2 • Later onset usually due to HHV-2 • Primary infections are usually asymptomatic; subsequent reinfections are less symptomatic © 2018 Pearson Education, Inc.

Figure 23. 12 Oral herpes lesion. © 2018 Pearson Education, Inc.
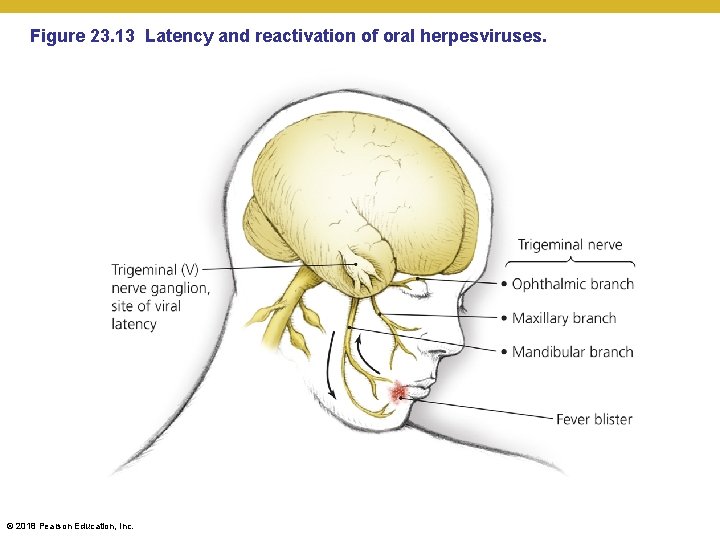
Figure 23. 13 Latency and reactivation of oral herpesviruses. © 2018 Pearson Education, Inc.

Viral Diseases of the Digestive System • Oral Herpes • Diagnosis, treatment, and prevention • Diagnosis is based on characteristic lesions • Topical penciclovir, acyclovir, or valacyclovir limits duration of lesions • Avoid direct contact with infected individuals • Acute breakouts usually self-resolve • Stress or immunosuppressive drugs can promote herpetic breakouts © 2018 Pearson Education, Inc.

Figure 24. 10 Sites of events in genital herpesvirus infections. • Note that the virus causing each of these diseases can be the same • It only varies based on which nerve ganglion it resides • It spreads to other ganglia only though skin-to-skin contact • dentists/oral hygienists working without gloves • Thumb-sucking/nail biting • Rubbing eyes or skin without hygiene © 2018 Pearson Education, Inc.
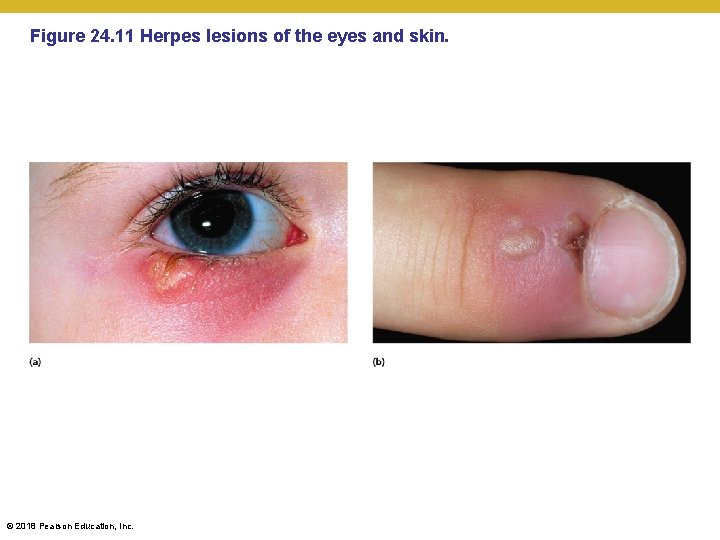
Figure 24. 11 Herpes lesions of the eyes and skin. © 2018 Pearson Education, Inc.
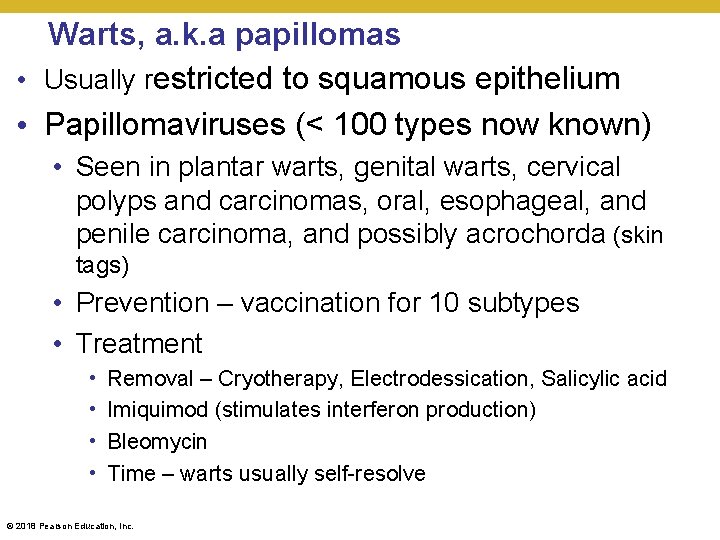
Warts, a. k. a papillomas • Usually restricted to squamous epithelium • Papillomaviruses (< 100 types now known) • Seen in plantar warts, genital warts, cervical polyps and carcinomas, oral, esophageal, and penile carcinoma, and possibly acrochorda (skin tags) • Prevention – vaccination for 10 subtypes • Treatment • • Removal – Cryotherapy, Electrodessication, Salicylic acid Imiquimod (stimulates interferon production) Bleomycin Time – warts usually self-resolve © 2018 Pearson Education, Inc.
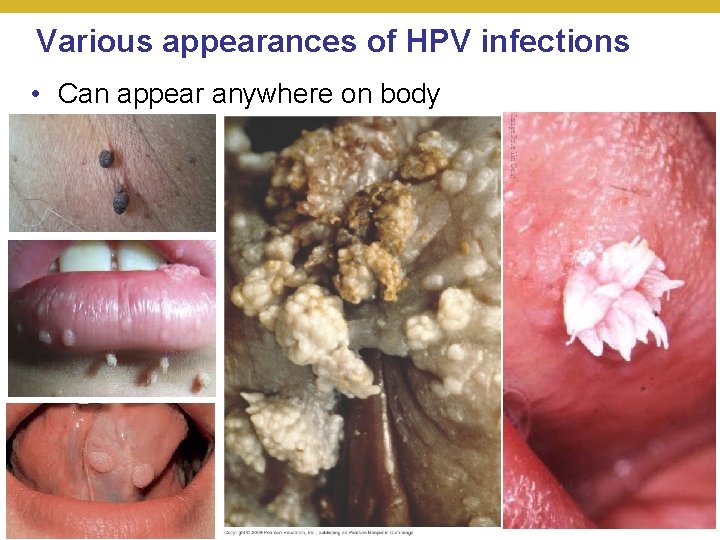
Various appearances of HPV infections • Can appear anywhere on body © 2018 Pearson Education, Inc.
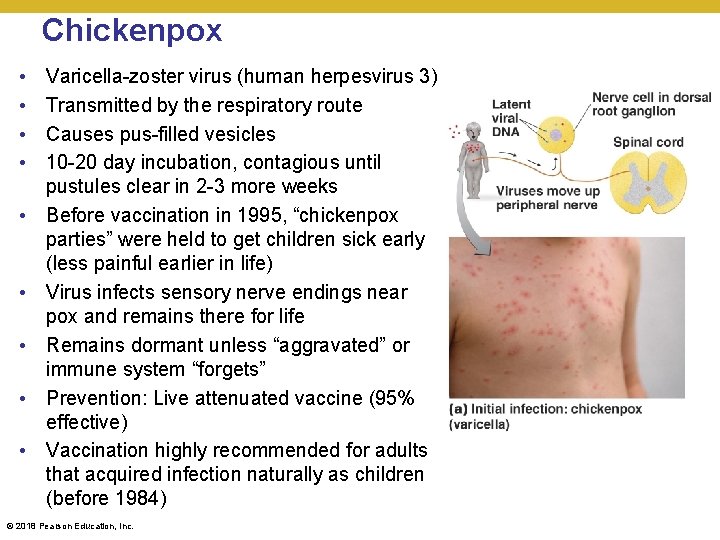
Chickenpox • • • Varicella-zoster virus (human herpesvirus 3) Transmitted by the respiratory route Causes pus-filled vesicles 10 -20 day incubation, contagious until pustules clear in 2 -3 more weeks Before vaccination in 1995, “chickenpox parties” were held to get children sick early (less painful earlier in life) Virus infects sensory nerve endings near pox and remains there for life Remains dormant unless “aggravated” or immune system “forgets” Prevention: Live attenuated vaccine (95% effective) Vaccination highly recommended for adults that acquired infection naturally as children (before 1984) © 2018 Pearson Education, Inc.

Latent Chickenpox • Breakthrough varicella in vaccinated people from incomplete protection (artificial vs. natural immunity) • Improperly stored vaccine; immunodeficiency; vaccine protection wore out (> 6 years) • Attenuated virus used for vaccine (Oka strain) less immunogenic than fully active virus • Because vaccine is still partially effective, breakthrough varicella is less severe than chickenpox • Virus reactivation and reemergence in later life known as shingles • Booster now recommended even in adults who were exposed naturally to chickenpox to prevent re-emergence • Pro. Quad = Oka + MMR for children, MMRV, young adults • Zostavax for adults 60+ © 2018 Pearson Education, Inc.

Shingles • Reactivation of latent HHV-3 releases viruses that move along peripheral nerves to skin • Semi-localized pattern corresponds to sensory innervation (dermatomes) • Painful vesicles; nerve pain • Months to resolve • Postherapeutic neuralgia • Prevention: Live attenuated vaccine (Zostavax) • Acyclovir may lessen symptoms © 2018 Pearson Education, Inc.

Rubella (German Measles) • Rubella virus • Macular rash and fever • Congenital rubella syndrome causes severe fetal damage; deformities • Prevented by vaccination (MMR) • Must ensure preexpectant mothers are vaccinated, not recommended for expectant mothers (why? ) © 2018 Pearson Education, Inc.
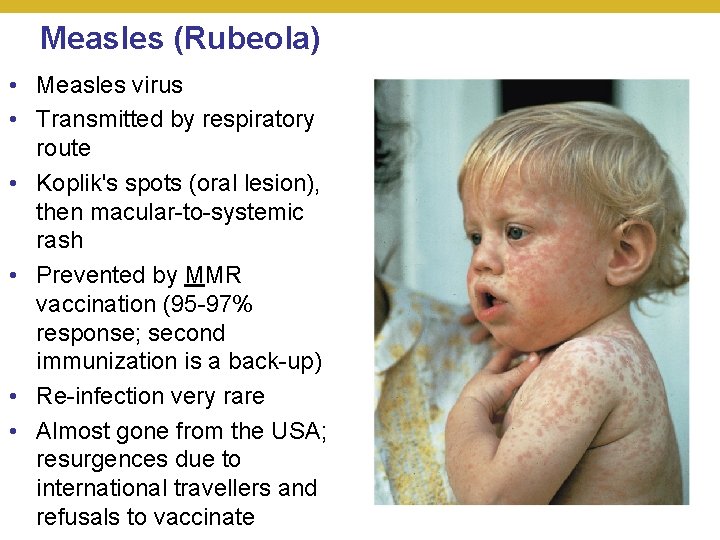
Measles (Rubeola) • Measles virus • Transmitted by respiratory route • Koplik's spots (oral lesion), then macular-to-systemic rash • Prevented by MMR vaccination (95 -97% response; second immunization is a back-up) • Re-infection very rare • Almost gone from the USA; resurgences due to international travellers and refusals to vaccinate © 2018 Pearson Education, Inc.

Complications from Measles • With improved diet and overall health in last 100 years, complications and fatalities from measles became very uncommon (pneumonia, encephalitis from cytokine response to infection in 1: 100 cases) • Secondary infection – H. influenza, S. pneumonia – leads to pneumonia, URI • Subacute sclerosing panencephalitis in 1, 000 cases – relapse by defective virus that is fatal © 2018 Pearson Education, Inc.

Reported U. S. Cases of Measles 1944– 2005 2° vac. rec’d vaccine licensed 1995 © 2018 Pearson Education, Inc.

Resurgence of Measles 2001– 2019 data is January to April 2019 cases expected to peak over 1500 © 2018 Pearson Education, Inc.
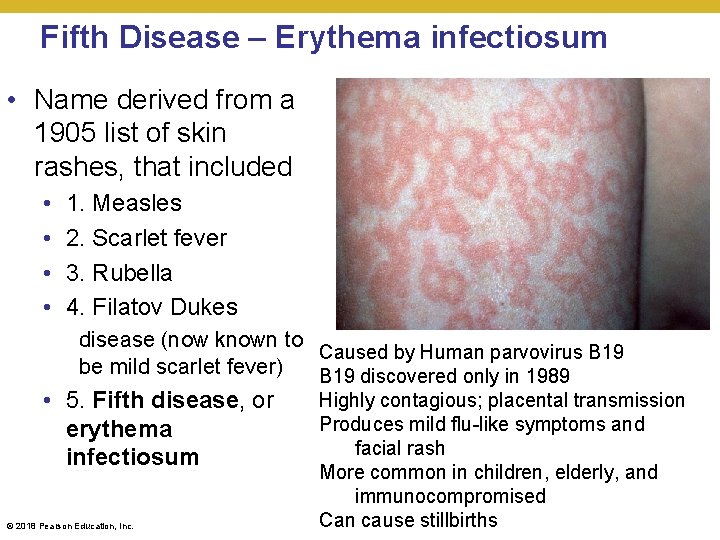
Fifth Disease – Erythema infectiosum • Name derived from a 1905 list of skin rashes, that included • • 1. Measles 2. Scarlet fever 3. Rubella 4. Filatov Dukes disease (now known to Caused by Human parvovirus B 19 be mild scarlet fever) B 19 discovered only in 1989 • 5. Fifth disease, or erythema infectiosum © 2018 Pearson Education, Inc. Highly contagious; placental transmission Produces mild flu-like symptoms and facial rash More common in children, elderly, and immunocompromised Can cause stillbirths
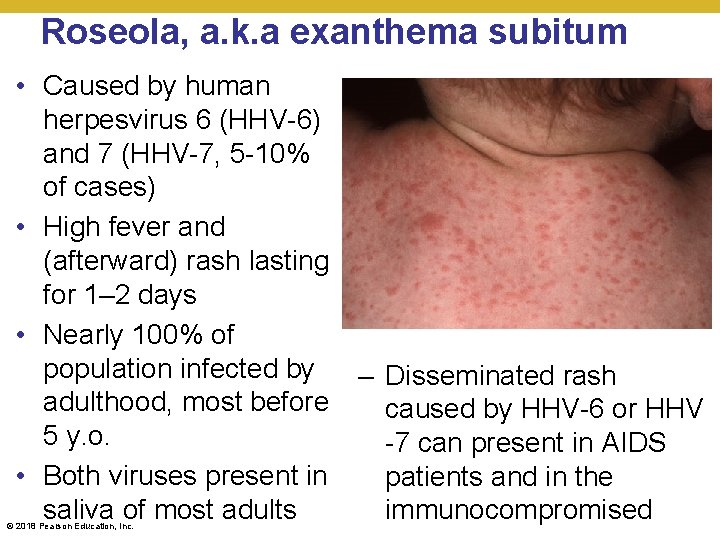
Roseola, a. k. a exanthema subitum • Caused by human herpesvirus 6 (HHV-6) and 7 (HHV-7, 5 -10% of cases) • High fever and (afterward) rash lasting for 1– 2 days • Nearly 100% of population infected by adulthood, most before 5 y. o. • Both viruses present in saliva of most adults © 2018 Pearson Education, Inc. – Disseminated rash caused by HHV-6 or HHV -7 can present in AIDS patients and in the immunocompromised
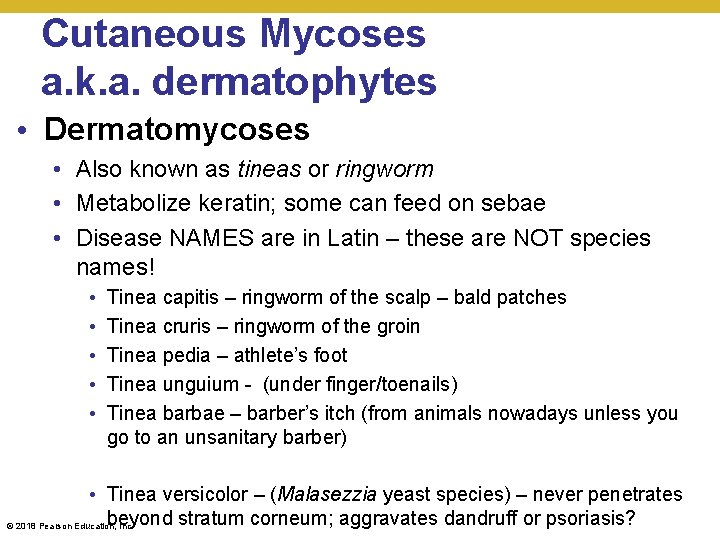
Cutaneous Mycoses a. k. a. dermatophytes • Dermatomycoses • Also known as tineas or ringworm • Metabolize keratin; some can feed on sebae • Disease NAMES are in Latin – these are NOT species names! • • • Tinea capitis – ringworm of the scalp – bald patches Tinea cruris – ringworm of the groin Tinea pedia – athlete’s foot Tinea unguium - (under finger/toenails) Tinea barbae – barber’s itch (from animals nowadays unless you go to an unsanitary barber) • Tinea versicolor – (Malasezzia yeast species) – never penetrates beyond stratum corneum; aggravates dandruff or psoriasis? © 2018 Pearson Education, Inc.
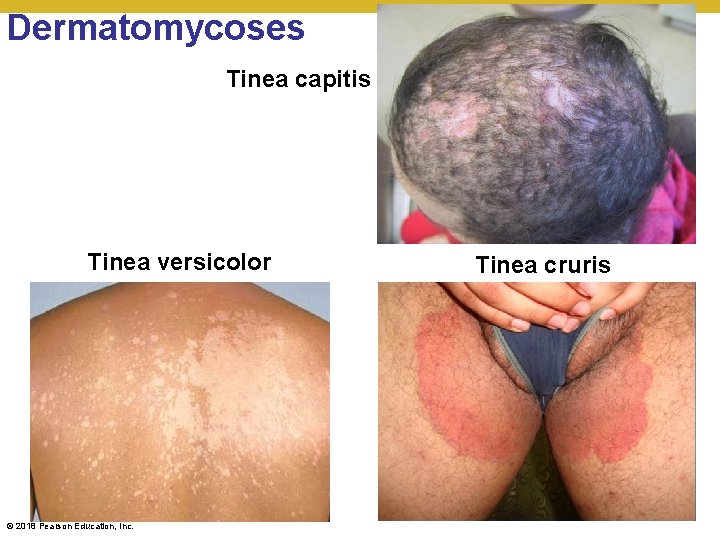
Dermatomycoses Tinea capitis Tinea versicolor © 2018 Pearson Education, Inc. Tinea cruris

Dermatomycoses (c)Tinea unguium © 2018 Pearson Education, Inc. (d)Tinea barbae
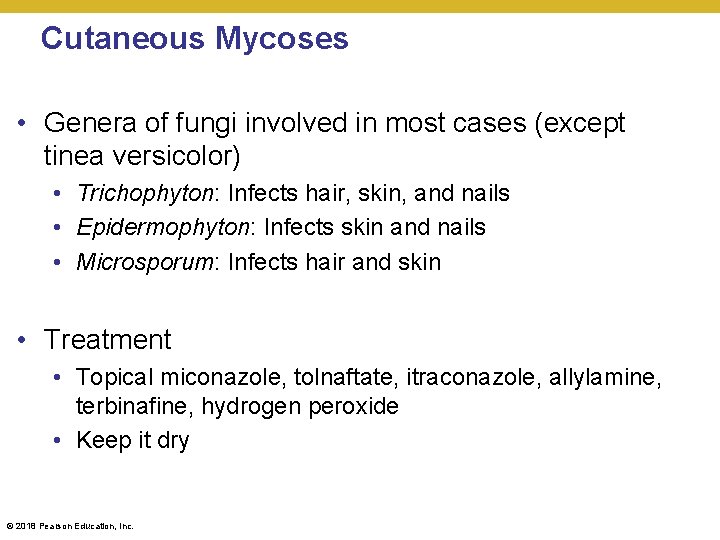
Cutaneous Mycoses • Genera of fungi involved in most cases (except tinea versicolor) • Trichophyton: Infects hair, skin, and nails • Epidermophyton: Infects skin and nails • Microsporum: Infects hair and skin • Treatment • Topical miconazole, tolnaftate, itraconazole, allylamine, terbinafine, hydrogen peroxide • Keep it dry © 2018 Pearson Education, Inc.
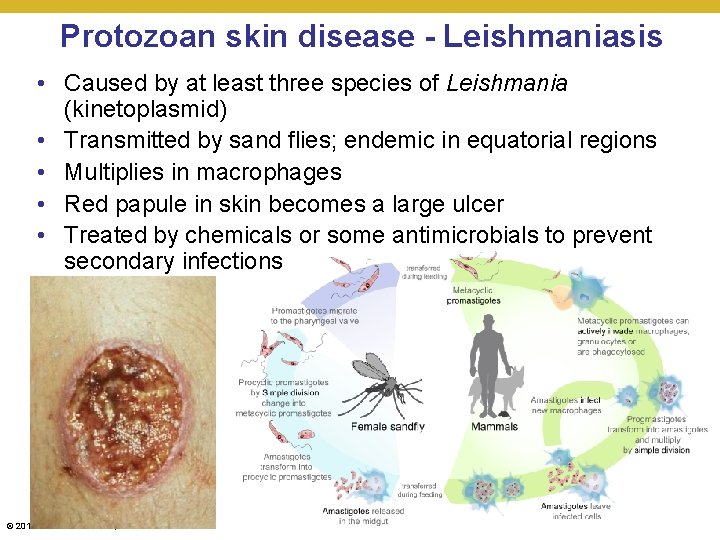
Protozoan skin disease - Leishmaniasis • Caused by at least three species of Leishmania (kinetoplasmid) • Transmitted by sand flies; endemic in equatorial regions • Multiplies in macrophages • Red papule in skin becomes a large ulcer • Treated by chemicals or some antimicrobials to prevent secondary infections © 2018 Pearson Education, Inc.

Scabies • Mite infection of skin tissues • Larvae feed on epidermis and trigger inflammatory response • Person-to-person spreading through sharing clothes, bedding or towels • More common in concentrated and dirty areas • May also be spread through insect bites (mechanical vector) • Diagnosis – difficult – very few microscopic (0. 3 mm length) adults • Prevention – clean clothing, hygiene, vaccination not possible © 2018 Pearson Education, Inc.
- Slides: 58