Microbial ToxinBIOC 422 Lecture7 1 Bacterial Toxins Exotoxins
Microbial Toxin-BIOC 422 Lecture-7
1 - Bacterial Toxins
Exotoxins 1. Cytotoxin : Diphtheria Toxin § Corynebacterium diphtheria § Diphtheria 2. Neurotoxin: Tetanospasmin § Clostridium tetani § Tetanus

4 - Production of toxins : Exotoxins 3)- Enterotoxin EXAMPLES: i. Cholera toxin “Ct” >> Cholera What is Vibrio cholerae ?
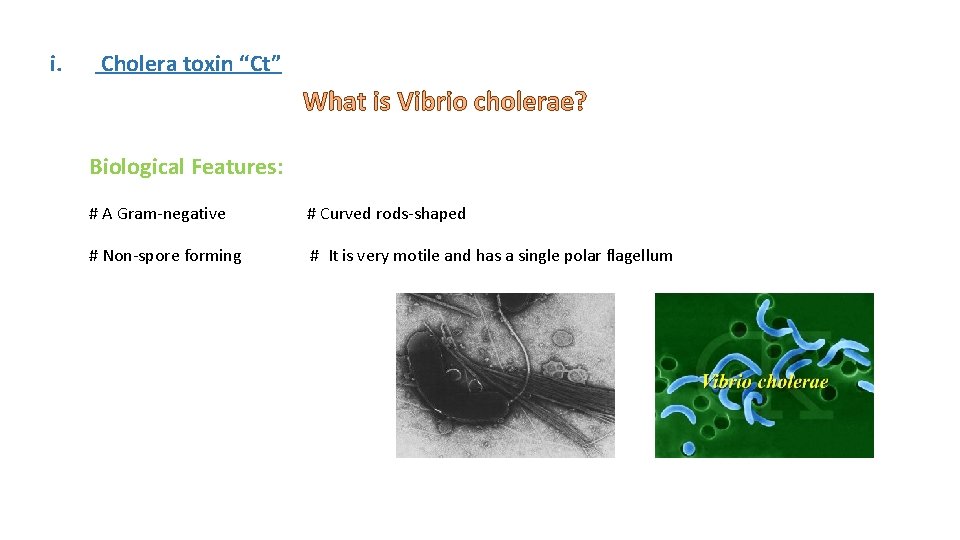
i. Cholera toxin “Ct” What is Vibrio cholerae? Biological Features: # A Gram-negative # Curved rods-shaped # Non-spore forming # It is very motile and has a single polar flagellum
i. Cholera toxin “Ct” What is cholera? • Cholera is an infection of the small intestine by some strains of the bacterium Vibrio cholera • It is one of the most devastating human diseases, with a rapid onset of diarrhea and vomiting within several hours to 2 -3 days of ingestion. • Due to massive fluid losses (15 -20 liters/day), the untreated mortality rate is in excess of 60%. However, rehydration therapy brings the mortality rate to below 1%.
Cholera History: • During the 19 th century, The first 2 cholera pandemic occurred in the Bengal region of India, near Calcutta starting in 1817 through 1824. • The disease spersed from India by trade 3 routes (land sea) to Southeast Asia, the Middle East, Europe, Eastern Africa… and from Europe to North America and the rest of the world. 1 4 5 6 7 8
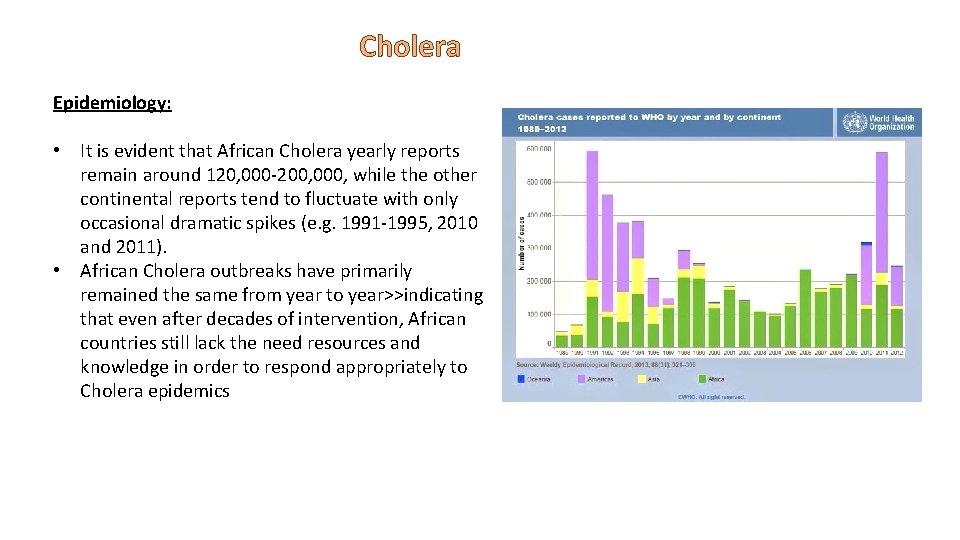
Cholera Epidemiology: • It is evident that African Cholera yearly reports remain around 120, 000 -200, 000, while the other continental reports tend to fluctuate with only occasional dramatic spikes (e. g. 1991 -1995, 2010 and 2011). • African Cholera outbreaks have primarily remained the same from year to year>>indicating that even after decades of intervention, African countries still lack the need resources and knowledge in order to respond appropriately to Cholera epidemics
Cholera Pandemics First, 1816– 26 Fourth, 1863– 1875 Second, 1829– 51 Fifth, 1881– 1896 Third, 1852– 1860 Sixth, 1899– 1923 Seventh, 1961– 1975 Notable outbreaks (1991– 2009): • 1991 – : Outbreak in South America, apparently initiated when a Chinese ship discharged ballast water. Beginning in Peru, there were 1. 04 million identified cases and almost 10, 000 deaths. • In 2000: some 140, 000 cholera cases were officially reported to WHO. Countries in Africa accounted for 87% of these cases. • In 2007: A lack of clean drinking water in IRAQ led to an outbreak of cholera. Notable outbreaks (2010–present): • Haiti and Dominican Republic: Late in October 2010, an outbreak was reported in Haiti. The number of dead was 1, 034, with hospitalizations for cholera symptoms totalling over 16, 700. • By November 2010, the disease had spread into the neighboring Dominican Republic. As of August 2016, the epidemic has officially sickened at least 790000 people and killed more than 9, 000 in Haiti, but the real burden is probably much higher. In the neighboring Dominican Republic, there have been at least 32, 000 suspected cases and 500 related deaths.
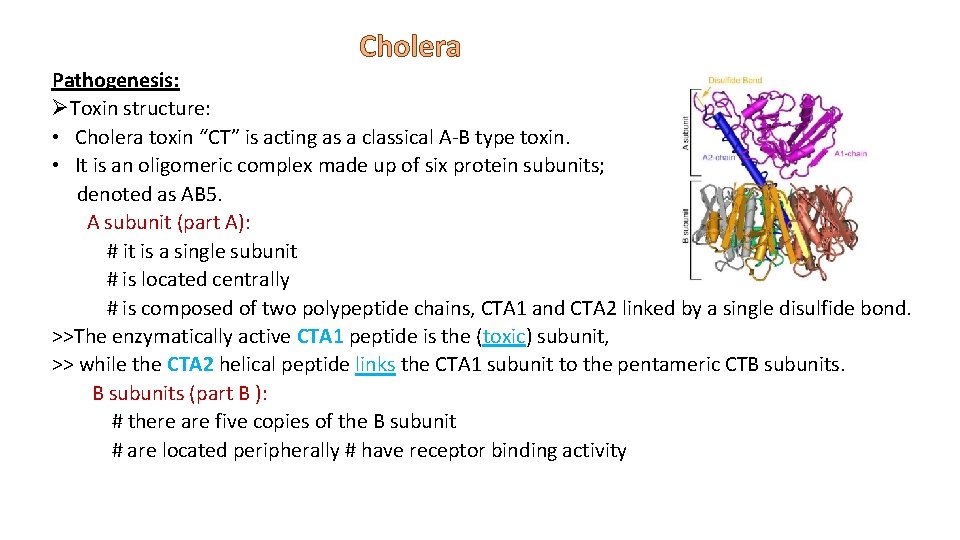
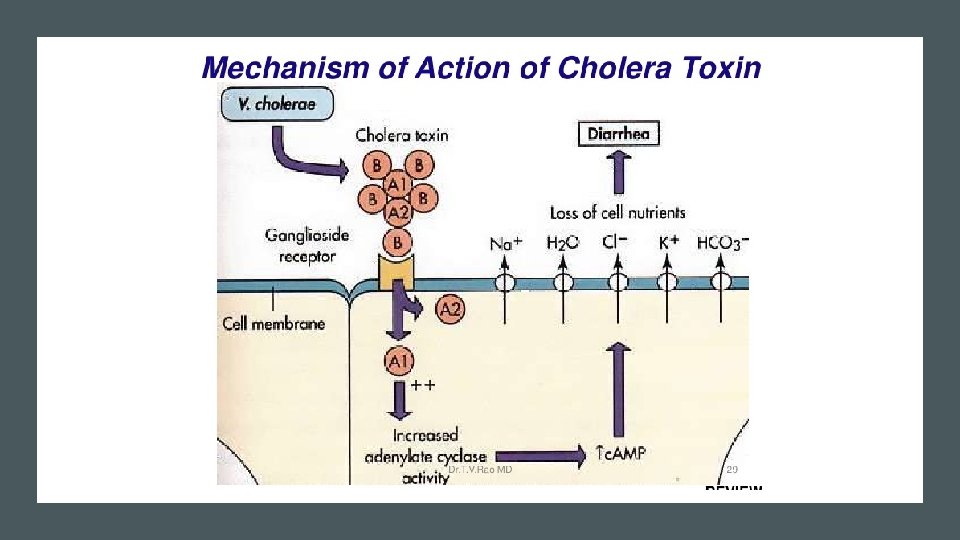
Cholera Pathogenesis: ØToxin structure: • Cholera toxin “CT” is acting as a classical A-B type toxin. • It is an oligomeric complex made up of six protein subunits; denoted as AB 5. A subunit (part A): # it is a single subunit # is located centrally # is composed of two polypeptide chains, CTA 1 and CTA 2 linked by a single disulfide bond. >>The enzymatically active CTA 1 peptide is the (toxic) subunit, >> while the CTA 2 helical peptide links the CTA 1 subunit to the pentameric CTB subunits (part B ): # there are five copies of the B subunit # are located peripherally # have receptor binding activity
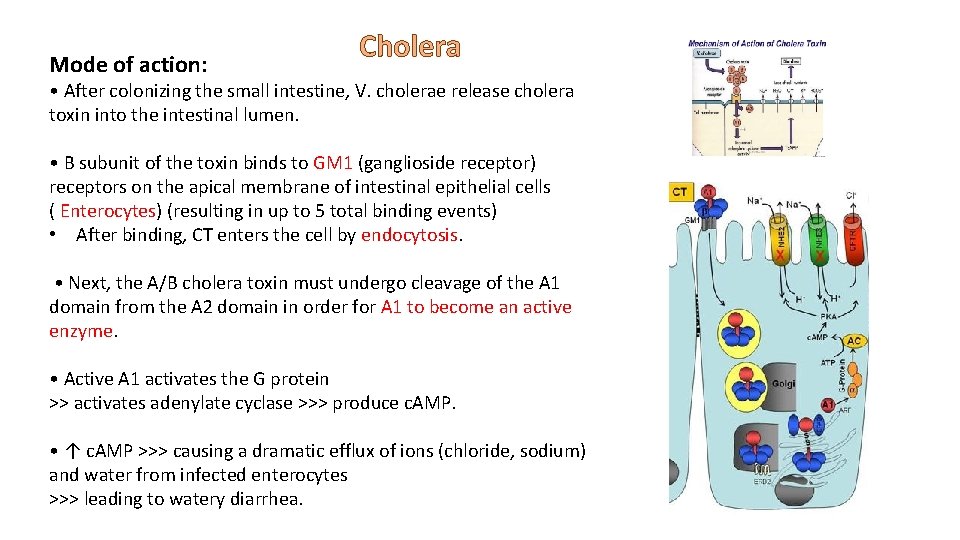
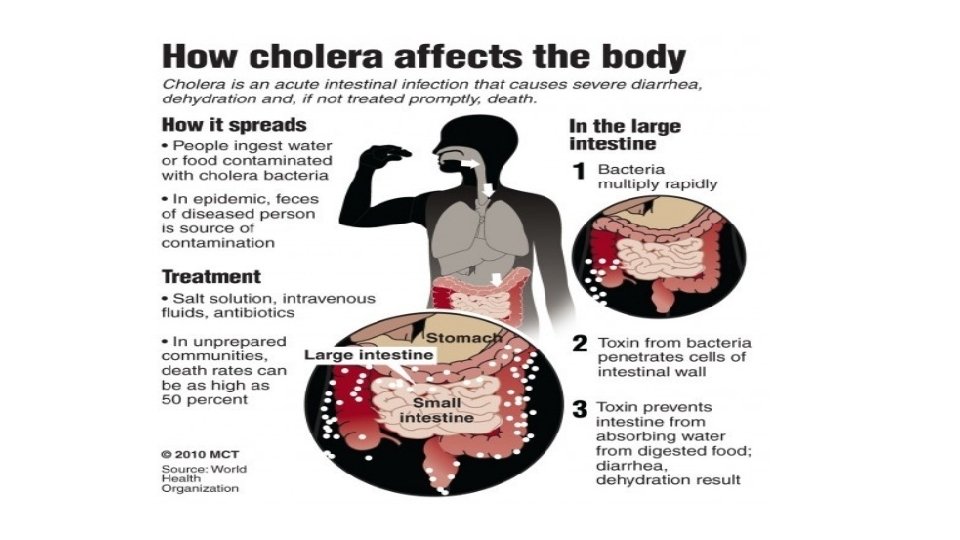
Mode of action: Cholera • After colonizing the small intestine, V. cholerae release cholera toxin into the intestinal lumen. • B subunit of the toxin binds to GM 1 (ganglioside receptor) receptors on the apical membrane of intestinal epithelial cells ( Enterocytes) (resulting in up to 5 total binding events) • After binding, CT enters the cell by endocytosis. • Next, the A/B cholera toxin must undergo cleavage of the A 1 domain from the A 2 domain in order for A 1 to become an active enzyme. • Active A 1 activates the G protein >> activates adenylate cyclase >>> produce c. AMP. • ↑ c. AMP >>> causing a dramatic efflux of ions (chloride, sodium) and water from infected enterocytes >>> leading to watery diarrhea.
Cholera Signs and symptoms • Cholera is one of the most devastating human diseases, with a rapid onset of diarrhea and vomiting within several hours to 2 -3 days of ingestion. • Due to massive fluid losses (15 -20 liters/day), the untreated mortality rate is in excess of 60%. However, rehydration therapy brings the mortality rate to below 1%. .
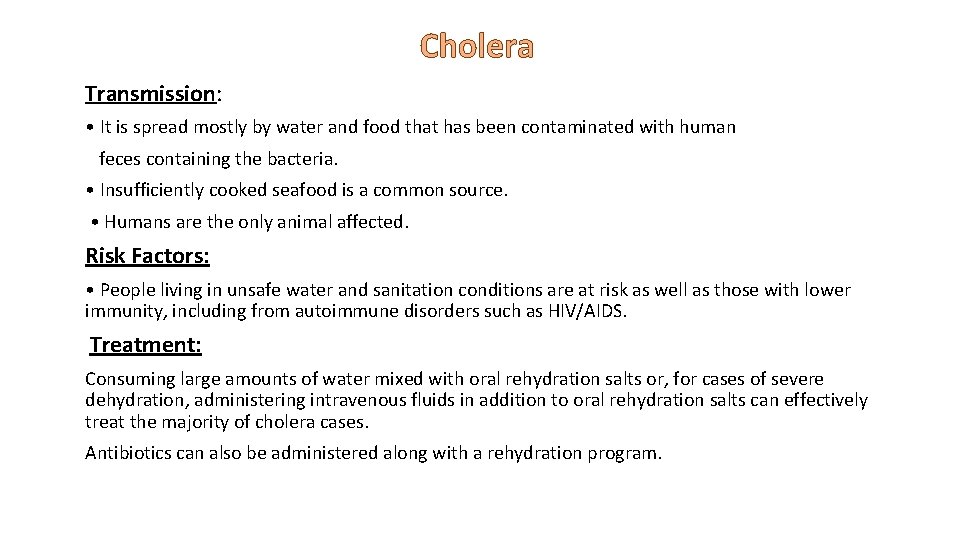
Cholera Transmission: • It is spread mostly by water and food that has been contaminated with human feces containing the bacteria. • Insufficiently cooked seafood is a common source. • Humans are the only animal affected. Risk Factors: • People living in unsafe water and sanitation conditions are at risk as well as those with lower immunity, including from autoimmune disorders such as HIV/AIDS. Treatment: Consuming large amounts of water mixed with oral rehydration salts or, for cases of severe dehydration, administering intravenous fluids in addition to oral rehydration salts can effectively treat the majority of cholera cases. Antibiotics can also be administered along with a rehydration program.
Cholera Vaccine: Cholera has been a burden to human health for centuries and has spread globally in the past 200 years. For the past 15 years, the World Health Organization has called for the development of oral cholera vaccines. While previously, researchers focused on creating vaccines using inactivated CT, it is now understood through animal model and human studies that anti-CT immunity that developed from treatment by the vaccine is not nearly as effective at protecting the patient from cholera. Prevention: It involves improved sanitation and access to clean water.
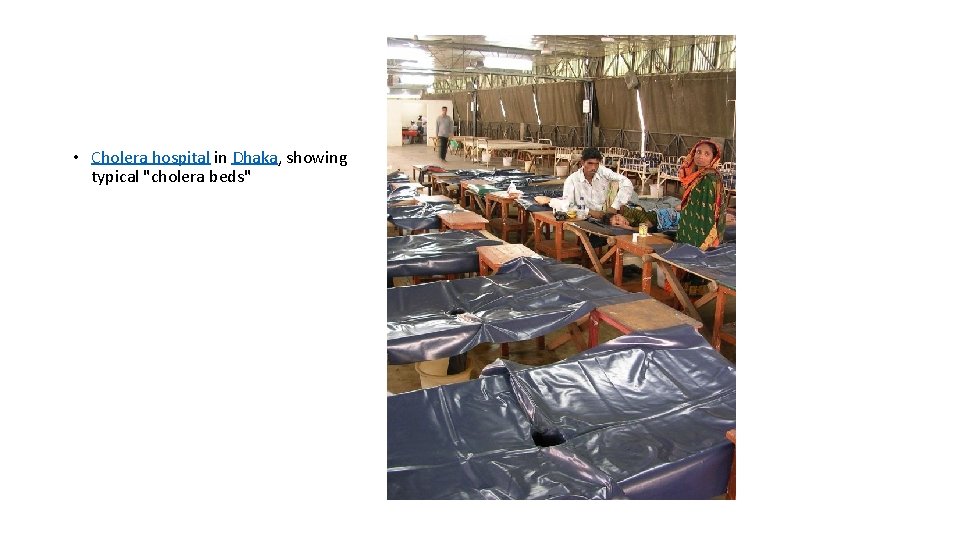
• Cholera hospital in Dhaka, showing typical "cholera beds"

- Slides: 19