Metabolic Syndrome Dr Hasan AYDIN Metabolic Syndrome Clustering
Metabolic Syndrome Dr. Hasan AYDIN
Metabolic Syndrome Clustering of cardiovascular risk factors Central obesity Diabetes Hypertension Dyslipidemia
Definition
First report The degree of masculine differentiation to obesity: a factor determining predisposition to diabetes, atherosclerosis, gout and uric calculus disease. (Vague Am J Clin Nutr 4: 20, 1956)
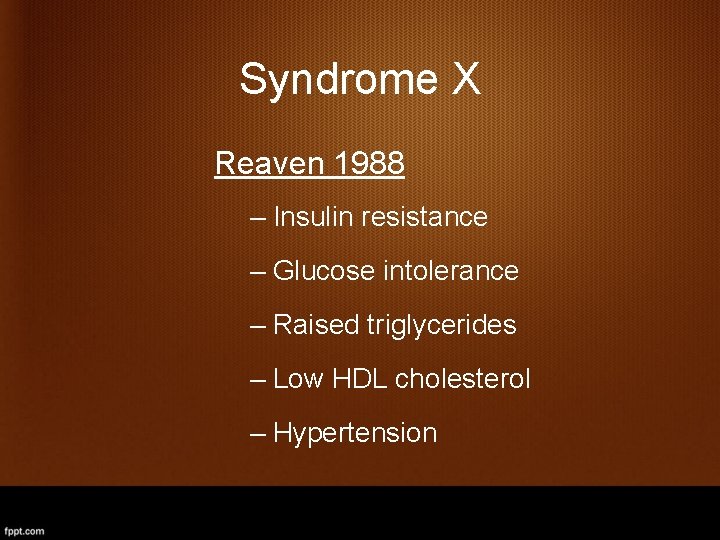
Syndrome X Reaven 1988 – Insulin resistance – Glucose intolerance – Raised triglycerides – Low HDL cholesterol – Hypertension
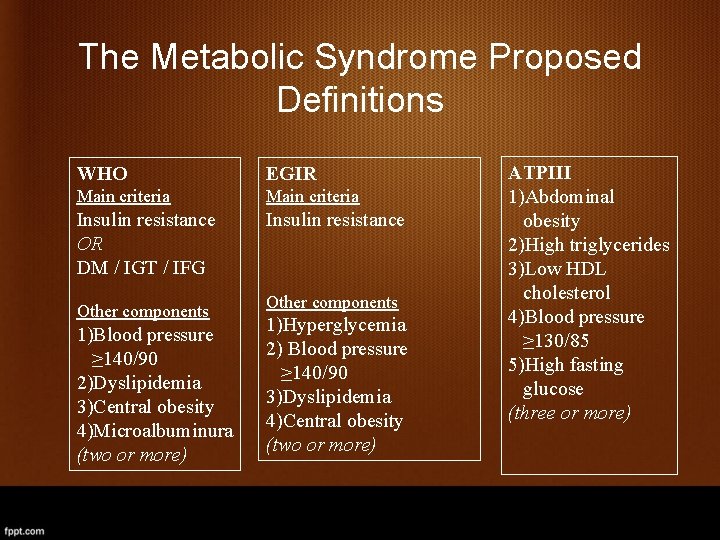
The Metabolic Syndrome Proposed Definitions WHO EGIR Main criteria Insulin resistance OR DM / IGT / IFG Insulin resistance Other components 1)Blood pressure ≥ 140/90 2)Dyslipidemia 3)Central obesity 4)Microalbuminura (two or more) Other components 1)Hyperglycemia 2) Blood pressure ≥ 140/90 3)Dyslipidemia 4)Central obesity (two or more) ATPIII 1)Abdominal obesity 2)High triglycerides 3)Low HDL cholesterol 4)Blood pressure ≥ 130/85 5)High fasting glucose (three or more)
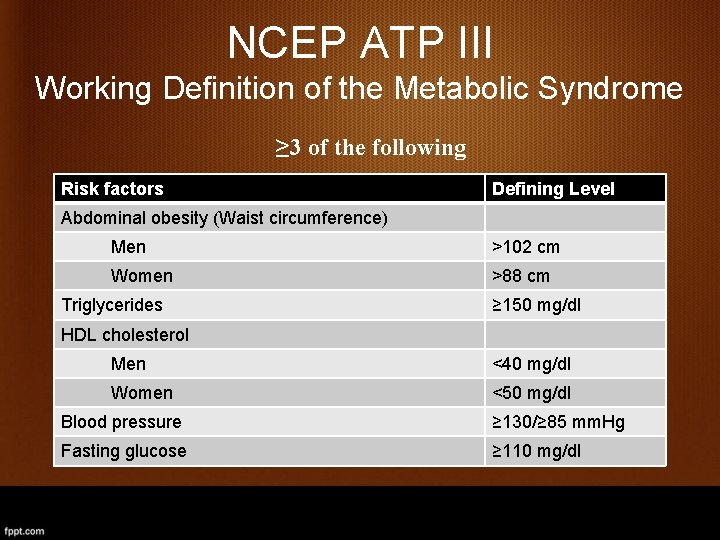
NCEP ATP III Working Definition of the Metabolic Syndrome ≥ 3 of the following Risk factors Defining Level Abdominal obesity (Waist circumference) Men >102 cm Women >88 cm Triglycerides ≥ 150 mg/dl HDL cholesterol Men <40 mg/dl Women <50 mg/dl Blood pressure ≥ 130/≥ 85 mm. Hg Fasting glucose ≥ 110 mg/dl
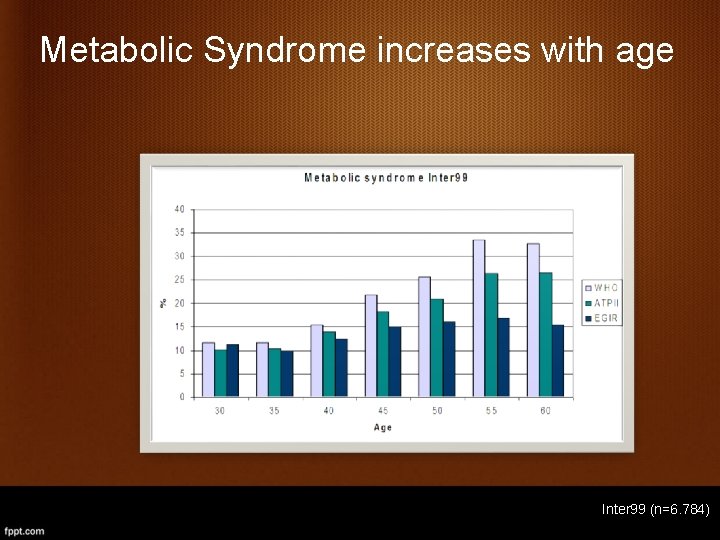
Metabolic Syndrome increases with age Inter 99 (n=6. 784)
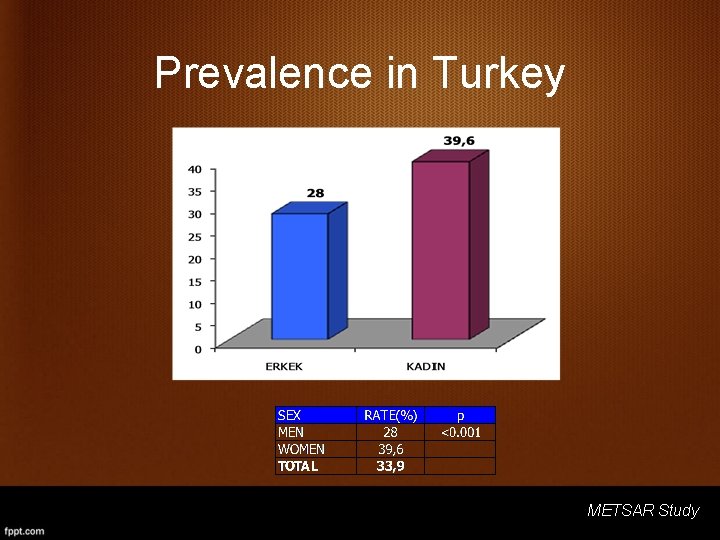
Prevalence in Turkey METSAR Study
Waist Measurements (cm) METSAR Study
Waist Measurements Age Groups METSAR Study
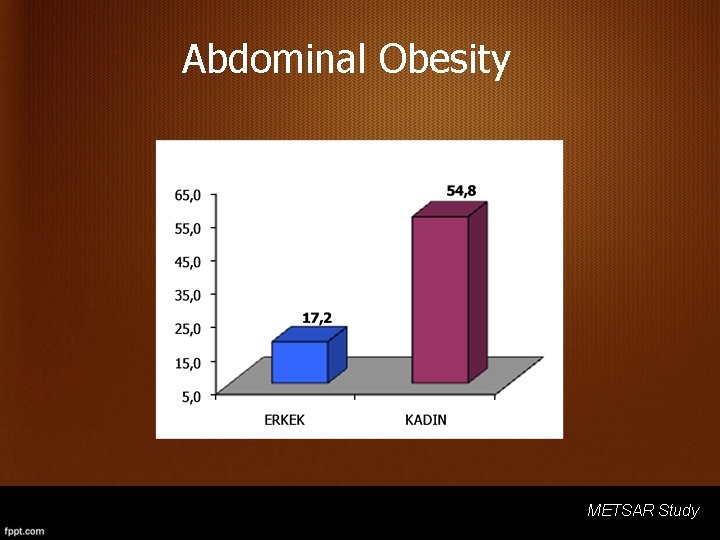
Abdominal Obesity METSAR Study
What causes metabolic syndrome? • Genetic predisposition • Ethnicity • Lifestyle and culture of inactivity and obesity • Aging
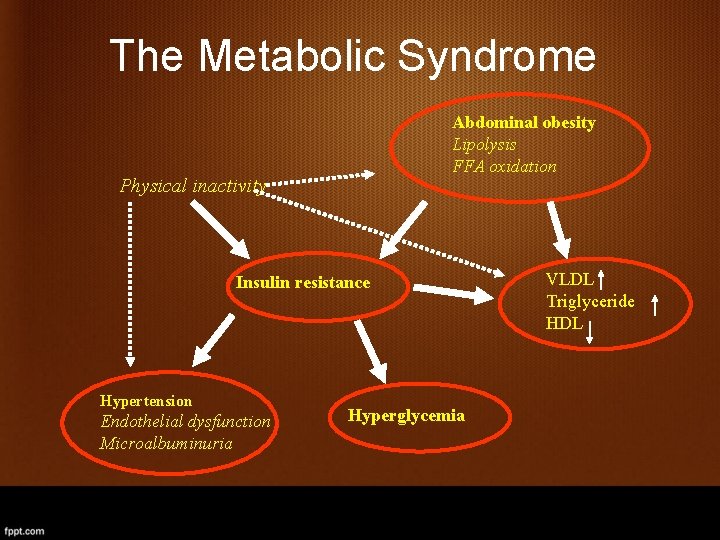
The Metabolic Syndrome Abdominal obesity Lipolysis FFA oxidation Physical inactivity Insulin resistance Hypertension Endothelial dysfunction Microalbuminuria Hyperglycemia VLDL Triglyceride HDL
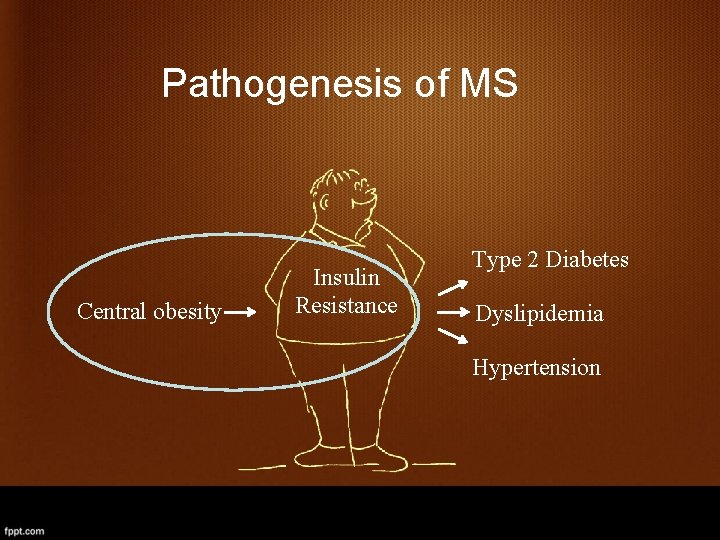
Pathogenesis of MS Central obesity Insulin Resistance Type 2 Diabetes Dyslipidemia Hypertension
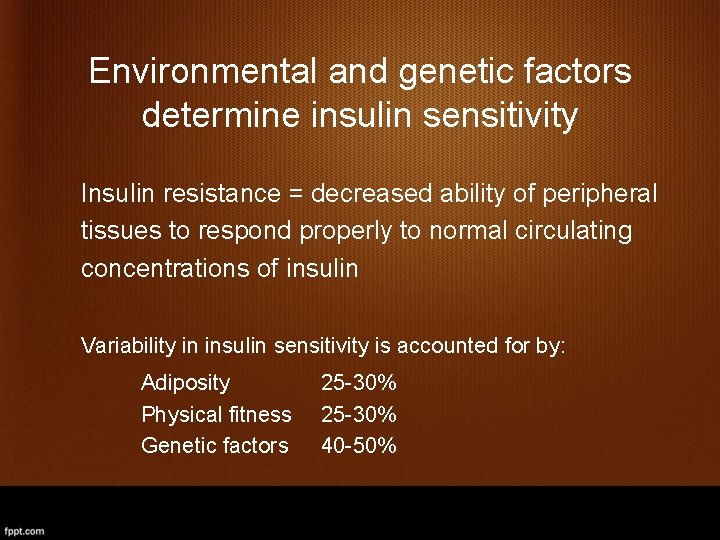
Environmental and genetic factors determine insulin sensitivity Insulin resistance = decreased ability of peripheral tissues to respond properly to normal circulating concentrations of insulin Variability in insulin sensitivity is accounted for by: Adiposity Physical fitness Genetic factors 25 -30% 40 -50%
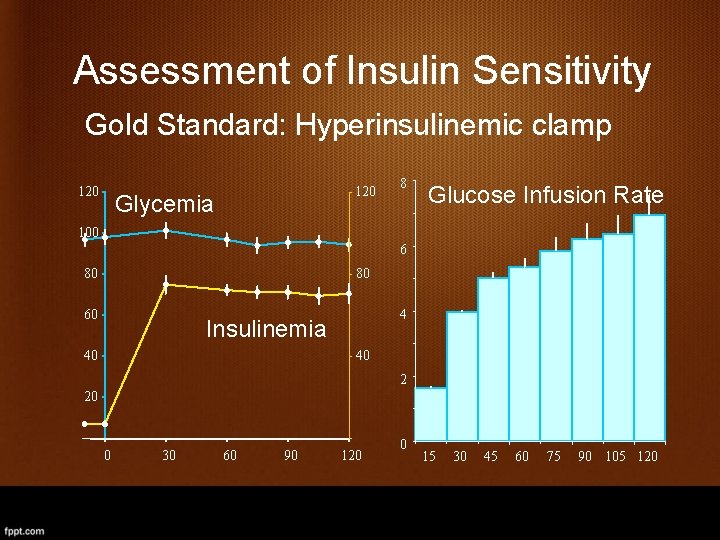
Assessment of Insulin Sensitivity Gold Standard: Hyperinsulinemic clamp 120 Glycemia 8 Glucose Infusion Rate 100 6 80 80 60 4 Insulinemia 40 40 2 20 0 30 60 90 120 0 15 30 45 60 75 90 105 120
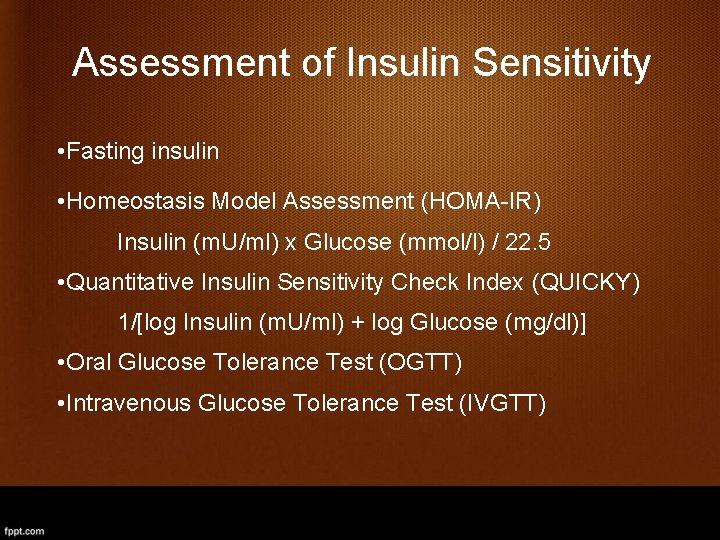
Assessment of Insulin Sensitivity • Fasting insulin • Homeostasis Model Assessment (HOMA-IR) Insulin (m. U/ml) x Glucose (mmol/l) / 22. 5 • Quantitative Insulin Sensitivity Check Index (QUICKY) 1/[log Insulin (m. U/ml) + log Glucose (mg/dl)] • Oral Glucose Tolerance Test (OGTT) • Intravenous Glucose Tolerance Test (IVGTT)
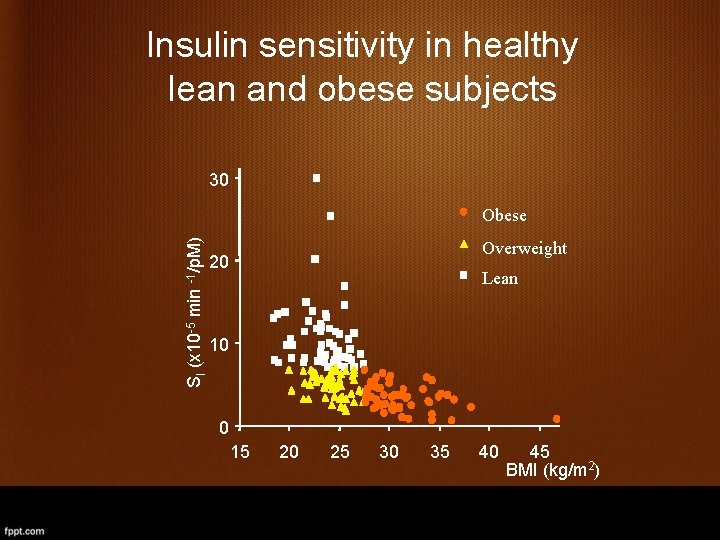
Insulin sensitivity in healthy lean and obese subjects 30 SI (x 10 -5 min -1/p. M) Obese Overweight 20 Lean 10 0 15 20 25 30 35 40 45 BMI (kg/m 2)
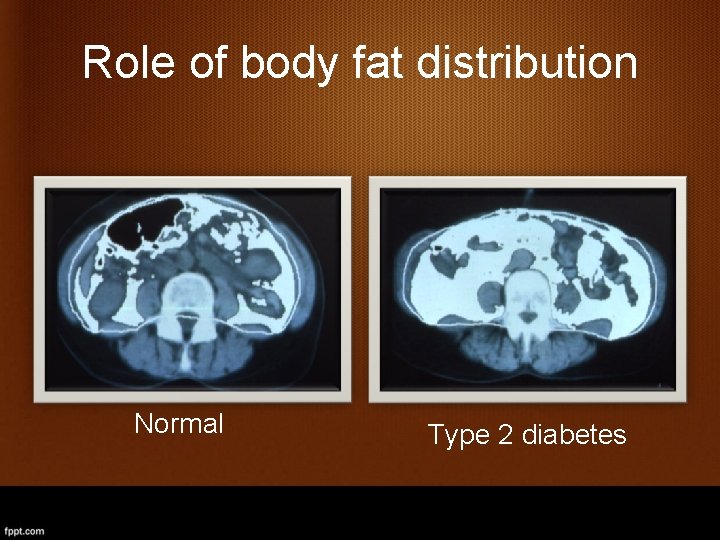
Role of body fat distribution Normal Type 2 diabetes
Question Do lean insulin sensitive, lean insulin resistant, and obese insulin resistant subjects have similar abdominal fat distribution?

Body Mass Index and Insulin Sensitivity **, ˆ SI (x 10 -5 min-1/p. M) BMI (kg/m 2) 30 20 10 7. 5 **, ˆ 2. 5 0 LIS LIR OIR (Cnop et al. Diabetes 51: 1005, 2002)
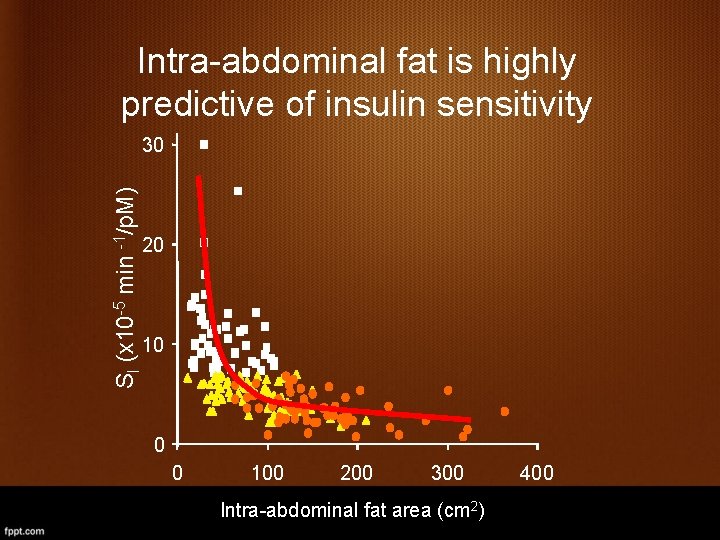
Intra-abdominal fat is highly predictive of insulin sensitivity SI (x 10 -5 min -1/p. M) 30 20 10 0 0 100 200 300 Intra-abdominal fat area (cm 2) 400
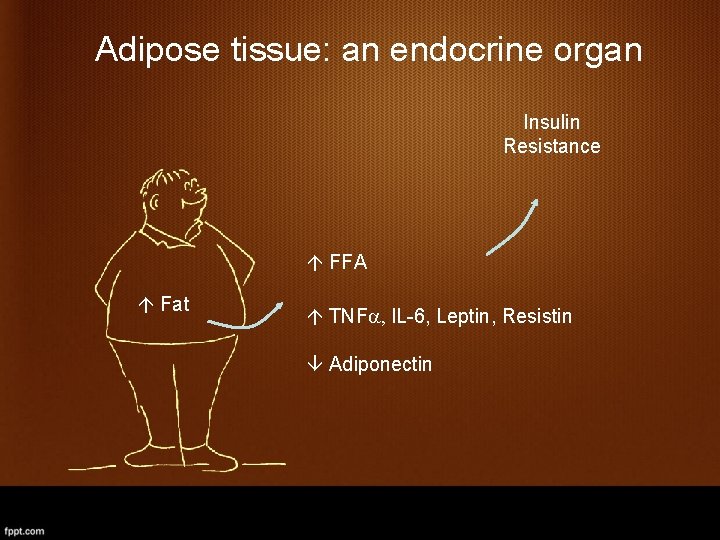
Adipose tissue: an endocrine organ Insulin Resistance FFA Fat TNFa, IL-6, Leptin, Resistin Adiponectin
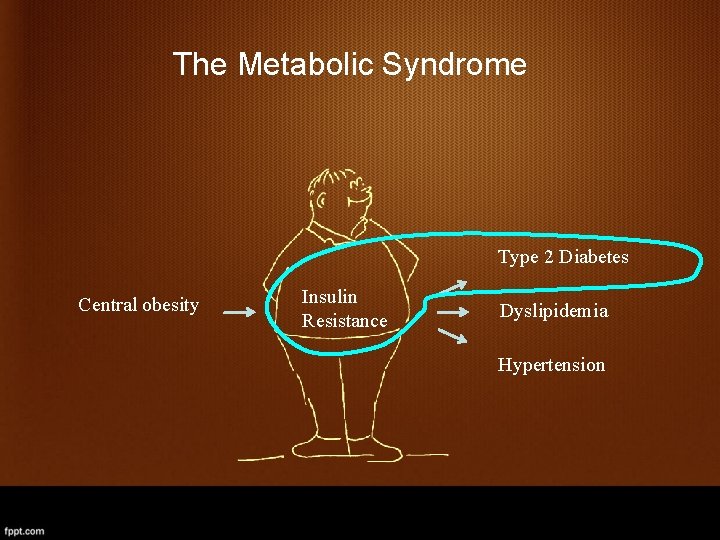
The Metabolic Syndrome Type 2 Diabetes Central obesity Insulin Resistance Dyslipidemia Hypertension
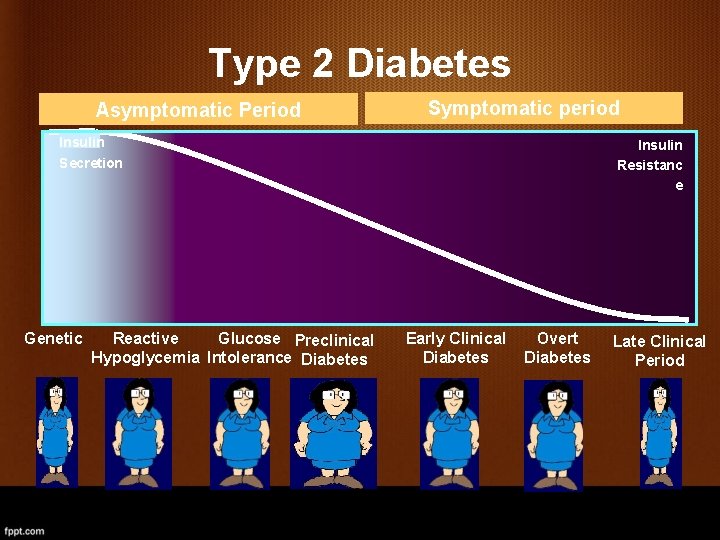
Type 2 Diabetes Asymptomatic Period Symptomatic period Insulin Secretion Genetic Reactive Glucose Preclinical Hypoglycemia Intolerance Diabetes Insulin Resistanc e Early Clinical Diabetes Overt Diabetes Late Clinical Period

Does the metabolic syndrome predict incident diabetes? N Follow up Definition Development of diabetes SAHS 1, 734 7 -8 years NCEP OR=3. 3 Strong Heart study 2, 283 7. 8 years NCEP √ Kuopio (men only) 1, 005 4 years WHO NCEP OR=8. 0 OR=5. 0 Mauritius 2, 605 5 years Other √
Does hyperinsulinemia predict diabetes? Percent (%) Tertile of HOMA-IR Resnick H et al. Diabetes Care 2003
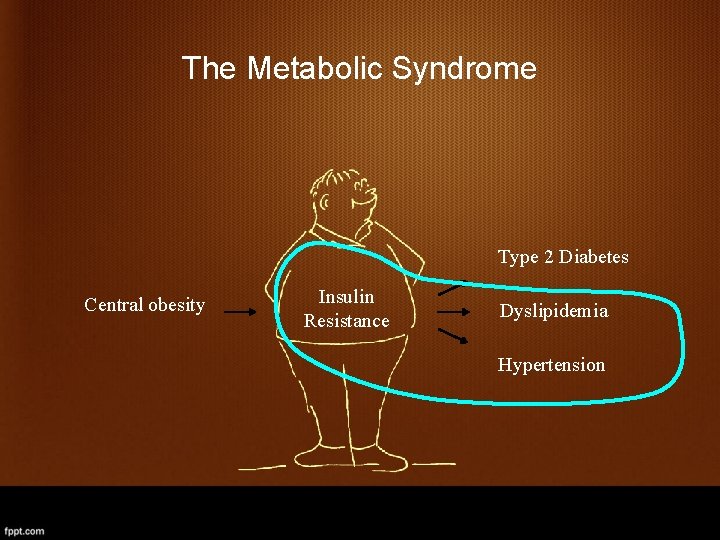
The Metabolic Syndrome Type 2 Diabetes Central obesity Insulin Resistance Dyslipidemia Hypertension
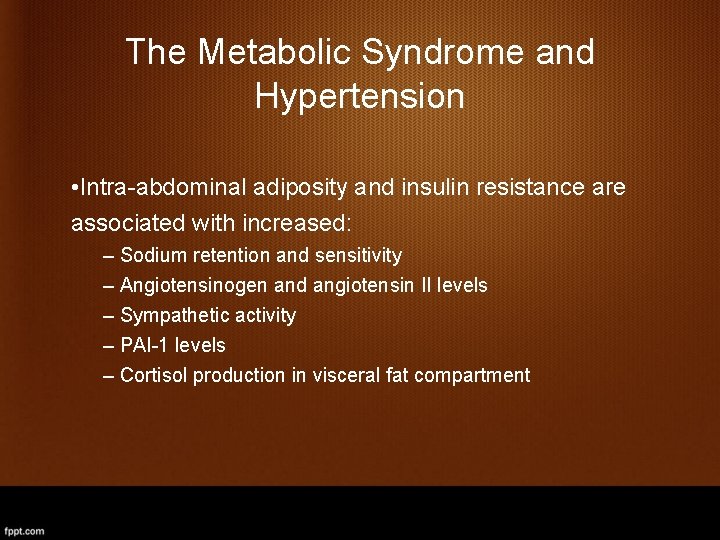
The Metabolic Syndrome and Hypertension • Intra-abdominal adiposity and insulin resistance are associated with increased: – Sodium retention and sensitivity – Angiotensinogen and angiotensin II levels – Sympathetic activity – PAI-1 levels – Cortisol production in visceral fat compartment
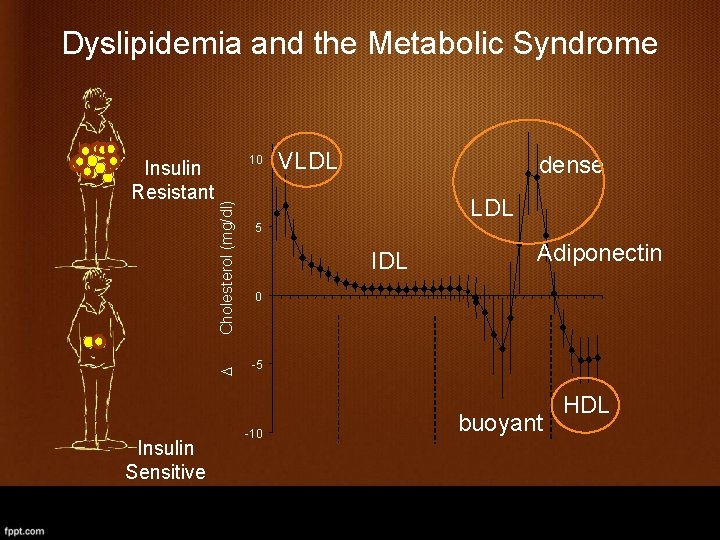
Dyslipidemia and the Metabolic Syndrome Cholesterol (mg/dl) 10 D Insulin Resistant Insulin Sensitive VLDL dense LDL 5 IDL Adiponectin 0 -5 -10 buoyant HDL
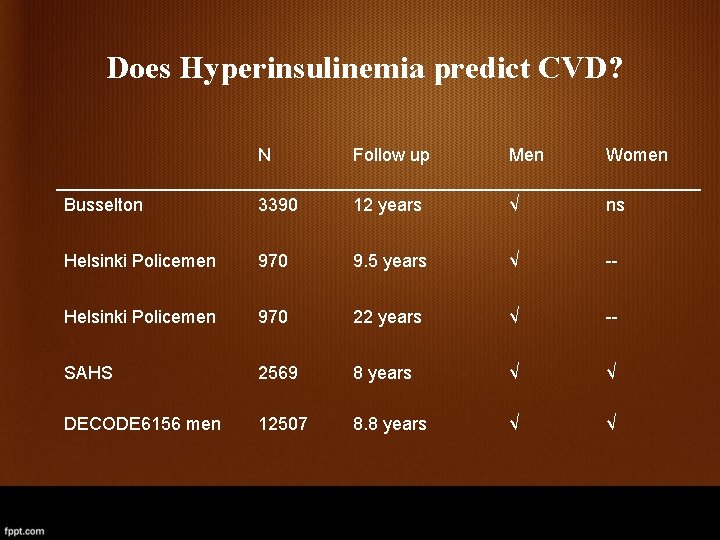
Does Hyperinsulinemia predict CVD? N Follow up Men Women Busselton 3390 12 years √ ns Helsinki Policemen 970 9. 5 years √ -- Helsinki Policemen 970 22 years √ -- SAHS 2569 8 years √ √ DECODE 6156 men 12507 8. 8 years √ √
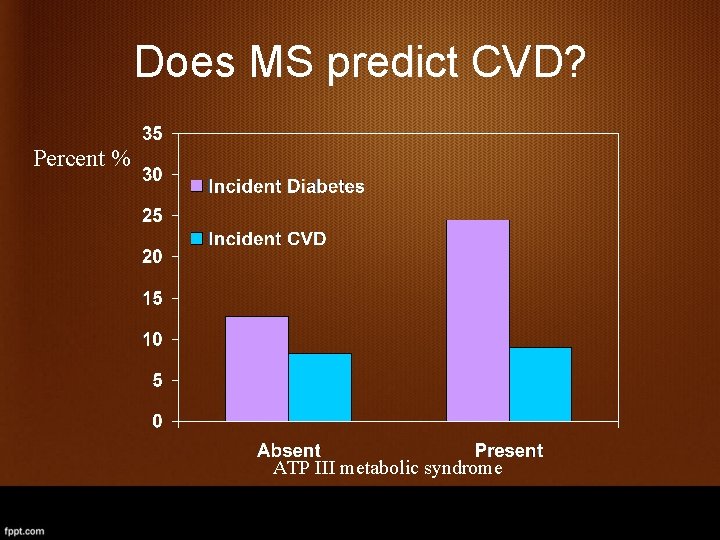
Does MS predict CVD? Percent % ATP III metabolic syndrome
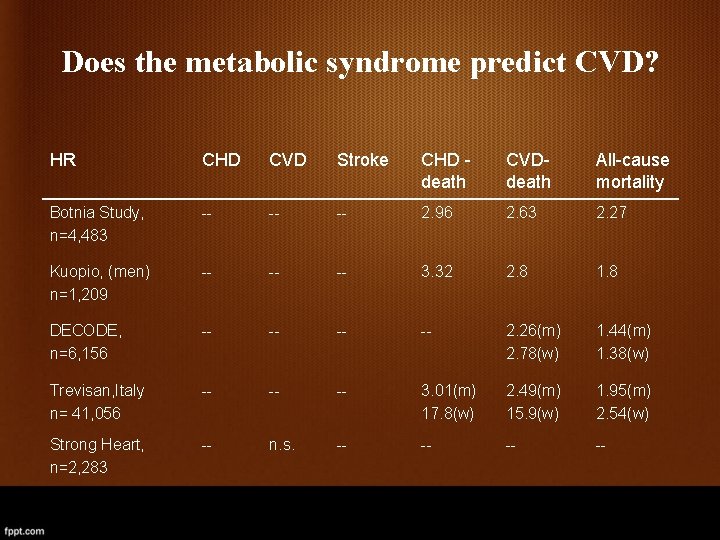
Does the metabolic syndrome predict CVD? HR CHD CVD Stroke CHD death CVDdeath All-cause mortality Botnia Study, n=4, 483 -- -- -- 2. 96 2. 63 2. 27 Kuopio, (men) n=1, 209 -- -- -- 3. 32 2. 8 1. 8 DECODE, n=6, 156 -- -- 2. 26(m) 2. 78(w) 1. 44(m) 1. 38(w) Trevisan, Italy n= 41, 056 -- -- -- 3. 01(m) 17. 8(w) 2. 49(m) 15. 9(w) 1. 95(m) 2. 54(w) Strong Heart, n=2, 283 -- n. s. -- --
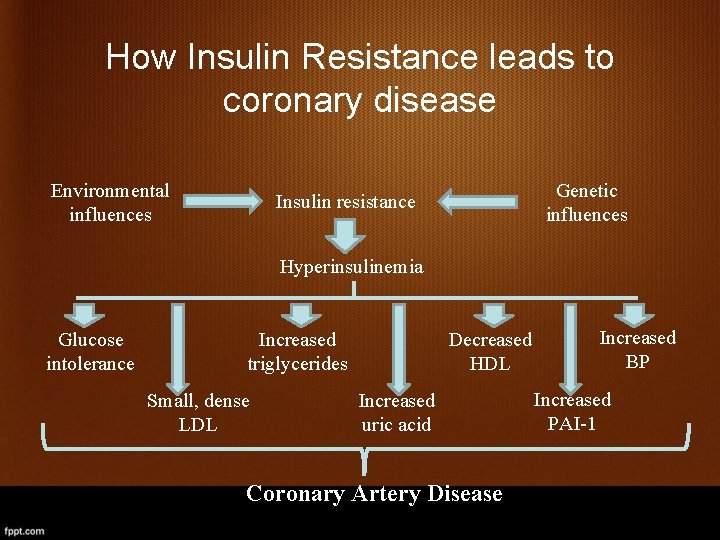
How Insulin Resistance leads to coronary disease Environmental influences Genetic influences Insulin resistance Hyperinsulinemia Glucose intolerance Increased triglycerides Small, dense LDL Decreased HDL Increased uric acid Coronary Artery Disease Increased BP Increased PAI-1
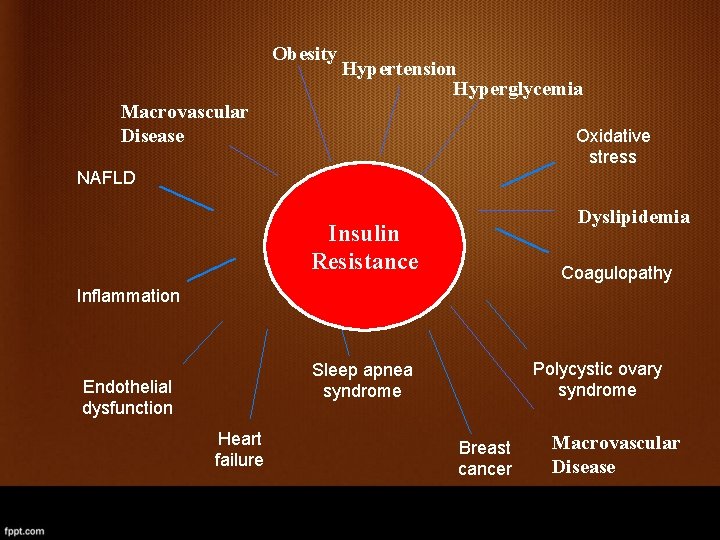
Obesity Hypertension Hyperglycemia Macrovascular Disease Oxidative stress NAFLD Dyslipidemia Insulin Resistance Coagulopathy Inflammation Polycystic ovary syndrome Sleep apnea syndrome Endothelial dysfunction Heart failure Breast cancer Macrovascular Disease
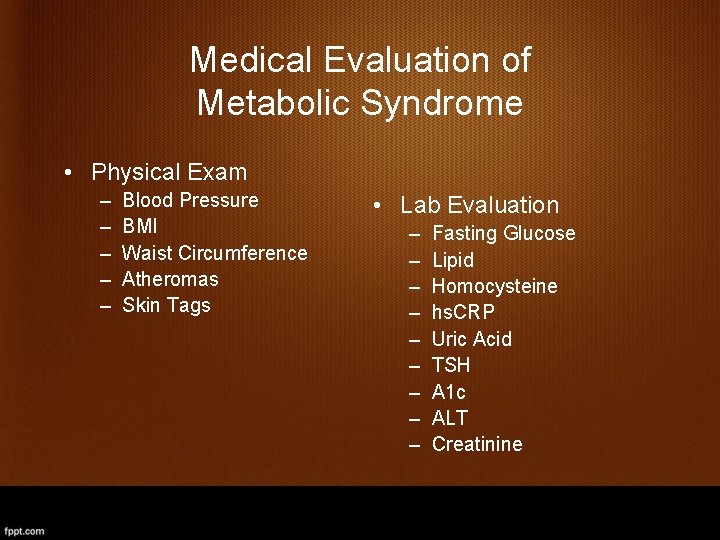
Medical Evaluation of Metabolic Syndrome • Physical Exam – – – Blood Pressure BMI Waist Circumference Atheromas Skin Tags • Lab Evaluation – – – – – Fasting Glucose Lipid Homocysteine hs. CRP Uric Acid TSH A 1 c ALT Creatinine
Treatment
Therapy for Insulin Resistance Nonpharmacologic / Pharmacologic • Exercise • Weight control • Diet • Smoking cessation
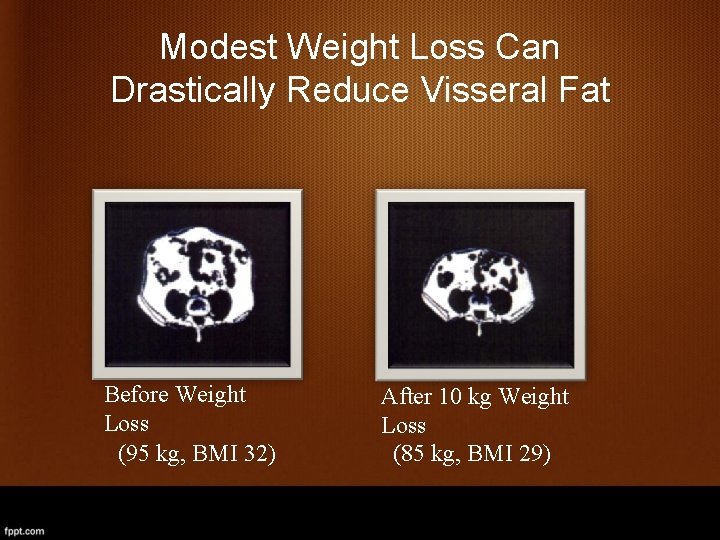
Modest Weight Loss Can Drastically Reduce Visseral Fat Before Weight Loss (95 kg, BMI 32) After 10 kg Weight Loss (85 kg, BMI 29)
NCEP/ATP III Guidelines Clinical Management of the Metabolic Syndrome Management of underlying cause – Weight control enhances LDL lowering and reduces all risk factors – Physical activity reduces VLDL, increases HDL, and may lower LDL Management of lipid and nonlipid risk factors – Treat hypertension – Use of aspirin in CHD patients – Treat elevated triglycerides and low HDL
Dietary Interventions • • • Reduce calories Reduce saturated fat Increase whole grains Increase fruits and vegetables Eat fish 1 -2 times per week Use monounsaturated or polyunsaturated oils – Olive, Canola, and Peanuts – Safflower, Sunflower or Sesame seed, Corn, or Soy
Exercise Interventions • Goal for Patients: 240 minutes of purposeful activity per week • Write exercise prescription • 10, 000 steps per day
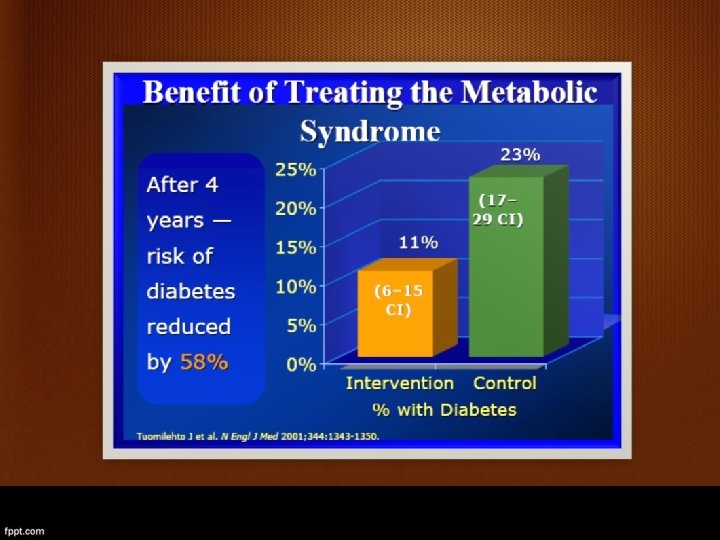
Treatment: Lifestyle • Finnish Diabetes Prevention Study • STOP-NIDDM Trial • US Diabetes Prevention Program • 7% weight loss • 150 min/week exercise • Reduction of diabetes incidence by 60% • Compared to 25 -30% reduction for pharmacological intervention
Pharmacologic Management • Aggressive Treatment of Hypertension – ACE Inhibitor is the drug of choice – Beta Blockers promote weight gain – Thiazide diuretics increase insulin resistance • • Metformin 500 mg BID—diabetes prevention Lipid—Statin medication or combination Aspirin for Everyone!!! Excellent Candidates for Aggressive Weight loss intervention – Healthy Ways – Weight Loss Meds: Sibutramine, Orlistat – Aggressive Dietary Intervention: VLCD if BMI>27
Treatment: Drugs • Underlying conditions (hypertension, diabetes, lipid disorders) should be treated. • An aggressive and early treatment strategy has been proposed. • Therapeutic agents might include fibrates, statins, metformin, thiazolidinediones, and, possibly, dual PPAR-a and g agonists. • No consensus optimal treatment targets have been determined and pharmacotherapy remains at present unproven.
Does Treating the Metabolic Syndrome Make a Difference? Finnish Diabetes Prevention Study
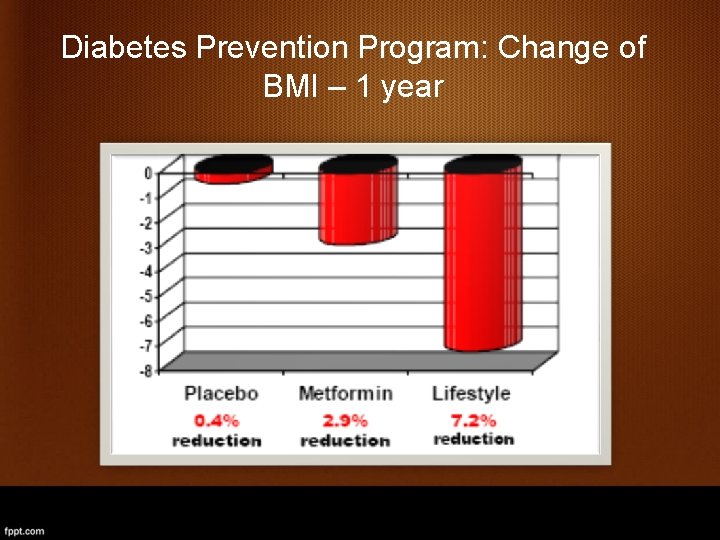
Diabetes Prevention Program: Change of BMI – 1 year
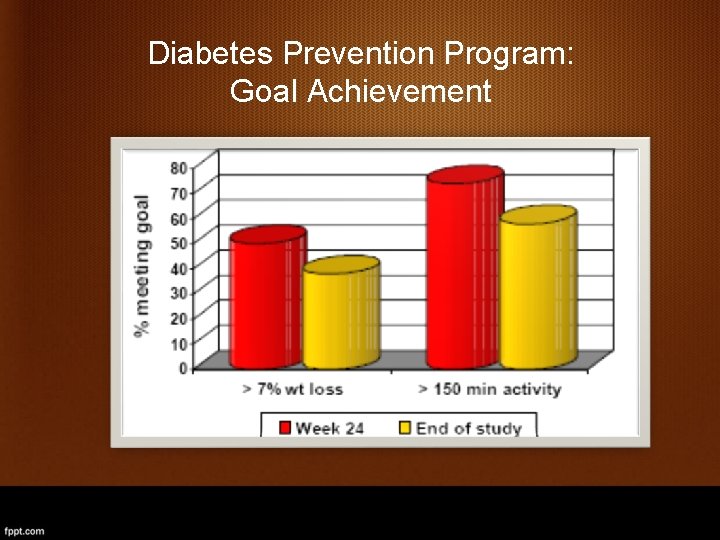
Diabetes Prevention Program: Goal Achievement
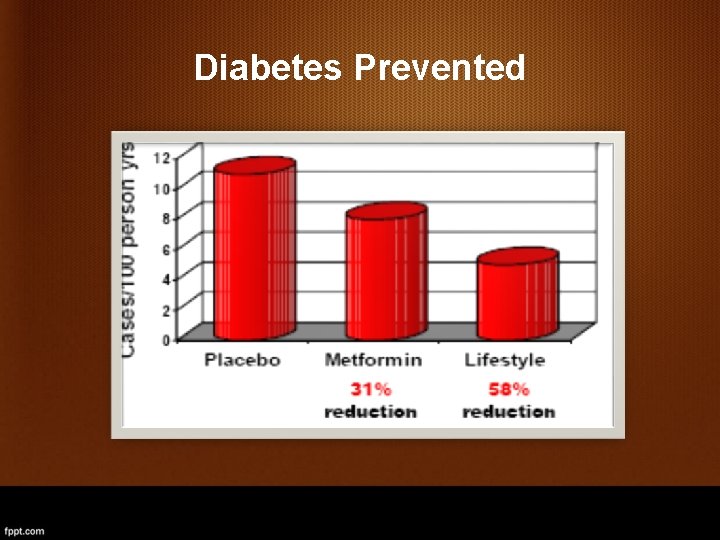
Diabetes Prevented
In Summary—Be Aggressive! • Identify patients with Metabolic Syndrome • Aggressive Lifestyle Intervention • Aggressive Pharmacologic Intervention – – – BP Lipid Metformin Aspirin Weight Loss Therapies
Thank you
- Slides: 53